Reason for premature birth
Premature birth - Symptoms and causes
Overview
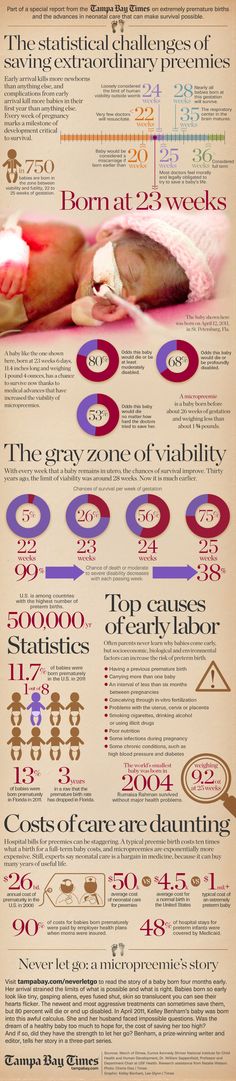
A premature birth is a birth that takes place more than three weeks before the baby's estimated due date. In other words, a premature birth is one that occurs before the start of the 37th week of pregnancy.
Premature babies, especially those born very early, often have complicated medical problems. Typically, complications of prematurity vary. But the earlier your baby is born, the higher the risk of complications.
Depending on how early a baby is born, he or she may be:
- Late preterm, born between 34 and 36 completed weeks of pregnancy
- Moderately preterm, born between 32 and 34 weeks of pregnancy
- Very preterm, born at less than 32 weeks of pregnancy
- Extremely preterm, born at or before 25 weeks of pregnancy
Most premature births occur in the late preterm stage.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Mayo Clinic Guide to Your Baby's First Years
Symptoms
Your baby may have very mild symptoms of premature birth, or may have more-obvious complications.
Some signs of prematurity include the following:
- Small size, with a disproportionately large head
- Sharper looking, less rounded features than a full-term baby's features, due to a lack of fat stores
- Fine hair (lanugo) covering much of the body
- Low body temperature, especially immediately after birth in the delivery room, due to a lack of stored body fat
- Labored breathing or respiratory distress
- Lack of reflexes for sucking and swallowing, leading to feeding difficulties
The following tables show the median birth weight, length and head circumference of premature babies at different gestational ages for each sex.
| Weight, length and head circumference by gestational age for boys | |||
|---|---|---|---|
| Gestational age | Weight | Length | Head circumference |
| 40 weeks | 7 lbs. , 15 oz. , 15 oz.(3.6 kg) | 20 in. (51 cm) | 13.8 in. (35 cm) |
| 35 weeks | 5 lbs., 8 oz. (2.5 kg) | 18.1 in. (46 cm) | 12.6 in. (32 cm) |
| 32 weeks | 3 lbs., 15.5 oz. (1.8 kg) | 16.5 in. (42 cm) | 11.6 in. (29.5 cm) |
| 28 weeks | 2 lbs., 6.8 oz. (1.1 kg) | 14.4 in. (36.5 cm) | 10.2 in. (26 cm) |
| 24 weeks | 1 lb., 6.9 oz. (0.65 kg) | 12.2 in. (31 cm) | 8.7 in. (22 cm) |
| Weight, length and head circumference by gestational age for girls | |||
|---|---|---|---|
| Gestational age | Weight | Length | Head circumference |
| 40 weeks | 7 lbs. , 7.9 oz. , 7.9 oz.(3.4 kg) | 20 in. (51 cm) | 13.8 in. (35 cm) |
| 35 weeks | 5 lbs., 4.7 oz. (2.4 kg) | 17.7 in. (45 cm) | 12.4 in. (31.5 cm) |
| 32 weeks | 3 lbs., 12 oz. (1.7 kg) | 16.5 in. (42 cm) | 11.4 in. (29 cm) |
| 28 weeks | 2 lbs., 3.3 oz. (1.0 kg) | 14.1 in. (36 cm) | 9.8 in. (25 cm) |
| 24 weeks | 1 lb., 5.2 oz. (0.60 kg) | 12.6 in. (32 cm) | 8.3 in. (21 cm) |
Special care
If you deliver a preterm baby, your baby will likely need a longer hospital stay in a special nursery unit at the hospital. Depending on how much care your baby requires, he or she may be admitted to an intermediate care nursery or the neonatal intensive care unit (NICU). Doctors and a specialized team with training in taking care of preterm babies will be available to help care for your baby. Don't hesitate to ask questions.
Doctors and a specialized team with training in taking care of preterm babies will be available to help care for your baby. Don't hesitate to ask questions.
Your baby may need extra help feeding, and adapting immediately after delivery. Your health care team can help you understand what is needed and what your baby's care plan will be.
Request an Appointment at Mayo Clinic
Risk factors
Often, the specific cause of premature birth isn't clear. However, there are known risk factors of premature delivery, including:
- Having a previous premature birth
- Pregnancy with twins, triplets or other multiples
- An interval of less than six months between pregnancies
- Conceiving through in vitro fertilization
- Problems with the uterus, cervix or placenta
- Smoking cigarettes or using illicit drugs
- Some infections, particularly of the amniotic fluid and lower genital tract
- Some chronic conditions, such as high blood pressure and diabetes
- Being underweight or overweight before pregnancy
- Stressful life events, such as the death of a loved one or domestic violence
- Multiple miscarriages or abortions
- Physical injury or trauma
For unknown reasons, black women are more likely to experience premature birth than are women of other races. But premature birth can happen to anyone. In fact, many women who have a premature birth have no known risk factors.
But premature birth can happen to anyone. In fact, many women who have a premature birth have no known risk factors.
Complications
While not all premature babies experience complications, being born too early can cause short-term and long-term health problems. Generally, the earlier a baby is born, the higher the risk of complications. Birth weight plays an important role, too.
Some problems may be apparent at birth, while others may not develop until later.
Short-term complications
In the first weeks, the complications of premature birth may include:
-
Breathing problems. A premature baby may have trouble breathing due to an immature respiratory system. If the baby's lungs lack surfactant — a substance that allows the lungs to expand — he or she may develop respiratory distress syndrome because the lungs can't expand and contract normally.
Premature babies may also develop a lung disorder known as bronchopulmonary dysplasia.
 In addition, some preterm babies may experience prolonged pauses in their breathing, known as apnea.
In addition, some preterm babies may experience prolonged pauses in their breathing, known as apnea. - Heart problems. The most common heart problems premature babies experience are patent ductus arteriosus (PDA) and low blood pressure (hypotension). PDA is a persistent opening between the aorta and pulmonary artery. While this heart defect often closes on its own, left untreated it can lead to a heart murmur, heart failure as well as other complications. Low blood pressure may require adjustments in intravenous fluids, medicines and sometimes blood transfusions.
- Brain problems. The earlier a baby is born, the greater the risk of bleeding in the brain, known as an intraventricular hemorrhage. Most hemorrhages are mild and resolve with little short-term impact. But some babies may have larger brain bleeding that causes permanent brain injury.
-
Temperature control problems.
 Premature babies can lose body heat rapidly. They don't have the stored body fat of a full-term infant, and they can't generate enough heat to counteract what's lost through the surface of their bodies. If body temperature dips too low, an abnormally low core body temperature (hypothermia) can result.
Premature babies can lose body heat rapidly. They don't have the stored body fat of a full-term infant, and they can't generate enough heat to counteract what's lost through the surface of their bodies. If body temperature dips too low, an abnormally low core body temperature (hypothermia) can result.Hypothermia in a premature baby can lead to breathing problems and low blood sugar levels. In addition, a premature infant may use up all of the energy gained from feedings just to stay warm. That's why smaller premature infants require additional heat from a warmer or an incubator until they're larger and able to maintain body temperature without assistance.
- Gastrointestinal problems. Premature infants are more likely to have immature gastrointestinal systems, resulting in complications such as necrotizing enterocolitis (NEC). This potentially serious condition, in which the cells lining the bowel wall are injured, can occur in premature babies after they start feeding.
 Premature babies who receive only breast milk have a much lower risk of developing NEC.
Premature babies who receive only breast milk have a much lower risk of developing NEC. -
Blood problems. Premature babies are at risk of blood problems such as anemia and newborn jaundice. Anemia is a common condition in which the body doesn't have enough red blood cells. While all newborns experience a slow drop in red blood cell count during the first months of life, the decrease may be greater in premature babies.
Newborn jaundice is a yellow discoloration in a baby's skin and eyes that occurs because the baby's blood contains excess bilirubin, a yellow-colored substance, from the liver or red blood cells. While there are many causes of jaundice, it is more common in preterm babies.
- Metabolism problems. Premature babies often have problems with their metabolism. Some premature babies may develop an abnormally low level of blood sugar (hypoglycemia). This can happen because premature infants typically have smaller stores of stored glucose than do full-term babies.
 Premature babies also have more difficulty converting their stored glucose into more-usable, active forms of glucose.
Premature babies also have more difficulty converting their stored glucose into more-usable, active forms of glucose. - Immune system problems. An underdeveloped immune system, common in premature babies, can lead to a higher risk of infection. Infection in a premature baby can quickly spread to the bloodstream, causing sepsis, an infection that spreads to the bloodstream.
Long-term complications
In the long term, premature birth may lead to the following complications:
- Cerebral palsy. Cerebral palsy is a disorder of movement, muscle tone or posture that can be caused by infection, inadequate blood flow or injury to a newborn's developing brain either early during pregnancy or while the baby is still young and immature.
- Impaired learning. Premature babies are more likely to lag behind their full-term counterparts on various developmental milestones. Upon school age, a child who was born prematurely might be more likely to have learning disabilities.

- Vision problems. Premature infants may develop retinopathy of prematurity, a disease that occurs when blood vessels swell and overgrow in the light-sensitive layer of nerves at the back of the eye (retina). Sometimes the abnormal retinal vessels gradually scar the retina, pulling it out of position. When the retina is pulled away from the back of the eye, it's called retinal detachment, a condition that, if undetected, can impair vision and cause blindness.
- Hearing problems. Premature babies are at increased risk of some degree of hearing loss. All babies will have their hearing checked before going home.
- Dental problems. Premature infants who have been critically ill are at increased risk of developing dental problems, such as delayed tooth eruption, tooth discoloration and improperly aligned teeth.
- Behavioral and psychological problems. Children who experienced premature birth may be more likely than full-term infants to have certain behavioral or psychological problems, as well as developmental delays.

- Chronic health issues. Premature babies are more likely to have chronic health issues — some of which may require hospital care — than are full-term infants. Infections, asthma and feeding problems are more likely to develop or persist. Premature infants are also at increased risk of sudden infant death syndrome (SIDS).
Prevention
Although the exact cause of preterm birth is often unknown, there are some things that can be done to help women — especially those who have an increased risk — to reduce their risk of preterm birth, including:
- Progesterone supplements. Women who have a history of preterm birth, a short cervix or both factors may be able to reduce the risk of preterm birth with progesterone supplementation.
-
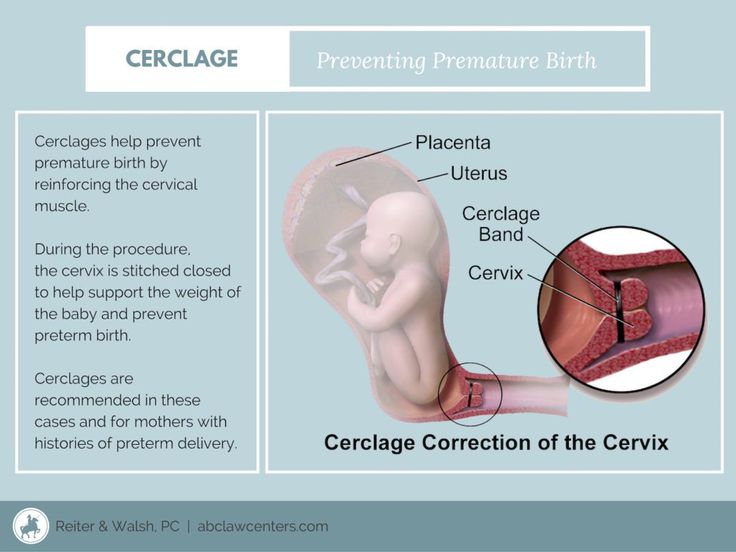
Cervical cerclage. This is a surgical procedure performed during pregnancy in women with a short cervix, or a history of cervical shortening that resulted in a preterm birth.
During this procedure, the cervix is stitched closed with strong sutures that may provide extra support to the uterus. The sutures are removed when it's time to deliver the baby. Ask your doctor if you need to avoid vigorous activity during the remainder of your pregnancy.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Why Are Babies Born Early? (for Parents)
Reviewed by: Thinh Phu Nguyen, MD
Fetal Medicine at Nemours Children's Health
en español ¿Por qué algunos bebés nacen antes de tiempo?
Most babies are born healthy at or near their due date. Sometimes, though, babies are born early and might have health problems.
Why Are Some Babies Born Early?
Babies born before 37 weeks are premature. A premature birth is more likely to happen when a mother has a health problem — like diabetes — or does harmful things during her pregnancy, like smoke or drink. If she lives with a lot of stress, that also can make her baby be born too early.
If she lives with a lot of stress, that also can make her baby be born too early.
Many things can cause a baby to be born early or with health problems. Some of these things can be controlled, but others can't.
Here's what you can do to have a healthy pregnancy.
How Can I Stay Healthy During Pregnancy?
During pregnancy, help your baby grow strong and healthy. Be sure to:
- Start prenatal care as soon as you think you're pregnant. Prenatal care is the health care that you get during pregnancy. All pregnant women should see a health care professional as soon as they think they're pregnant, and should plan regular prenatal visits throughout pregnancy.
- Get health problems treated. It's best to have any health problems (like diabetes, depression, or high blood pressure) under control before becoming pregnant. But if you don't, talk to your doctor right away about a treatment plan.
- Eat a healthy diet.
 It's important to eat a variety of healthy foods before and during pregnancy. Take a prenatal vitamin to be sure you're getting enough folic acid, iron, and other important nutrients.
It's important to eat a variety of healthy foods before and during pregnancy. Take a prenatal vitamin to be sure you're getting enough folic acid, iron, and other important nutrients. - Gain the right amount of weight. How much weight you should gain depends on how much you weighed before you were pregnant. Most women who are at a healthy weight should gain about 25 to 35 pounds during pregnancy. Overweight women should probably gain less.
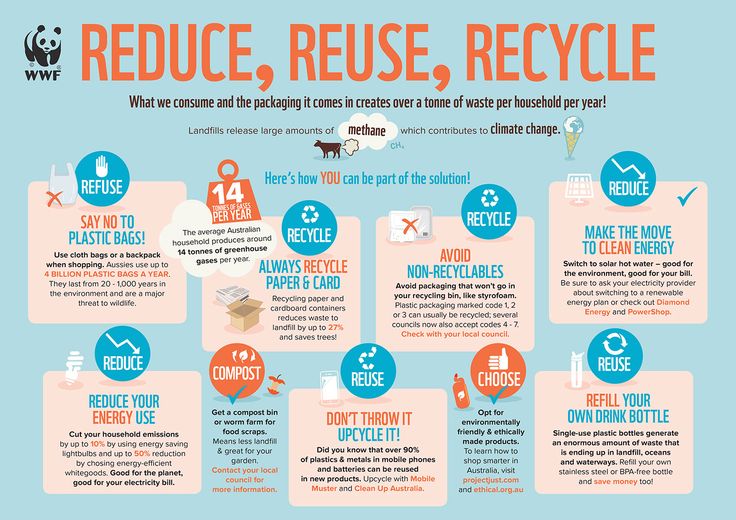
- Don't smoke, drink alcohol, or take illegal drugs. Staying away from tobacco, alcohol, and drugs can help you and your baby avoid many serious health problems, like fetal alcohol syndrome and neonatal abstinence syndrome (NAS). If you do any of these things, get help to quit.
- Wait at least 12 months between pregnancies. Increasing the time between pregnancies may lower the chances of preterm birth, especially if you had a premature baby before.
Things You Can't Control During Pregnancy
Some things that may increase the chances of a premature birth are out of your control. This doesn't mean that your baby will be born sick or too early. Remember, most babies are born healthy.
This doesn't mean that your baby will be born sick or too early. Remember, most babies are born healthy.
Here are some things you can't control during pregnancy:
- Your age. Mothers who are 17 or younger or 35 or older are more likely to have a premature baby. Teen moms are more likely to get high blood pressure during pregnancy and less likely to get the health care they need. Older women are more likely to have health problems before they get pregnant.
- The number of babies (multiples). The chances of having a premature baby go up if the mother is pregnant with twins, triplets, or more. More than half of all twins are born early.
- Your health. Moms with problems like diabetes, depression, or high blood pressure may need to see their health care professional more often to keep these conditions under control.
- Problems with an earlier pregnancy. A woman who has had a previous early delivery, or a baby born with health problems or a birth defect, is more likely to have problems in future pregnancies too.

- Other factors. It's not clear why, but black women are more likely to have premature babies than white and Hispanic women.
If you're pregnant or are planning to be, talk with your health care professional. Women who get regular prenatal care are more likely to have a healthier pregnancy and baby.
Reviewed by: Thinh Phu Nguyen, MD
Date reviewed: August 2022
Premature birth - Juno
Premature birth: content of the article
What is preterm birth
The birth of a baby weighing more than 0.5 kg from 22 to 37 weeks is considered early. According to statistics, 15 million babies are born prematurely around the world.
In our country, until 2012, babies were registered who were born at 28 weeks, and all those born earlier - a week later. The development of obstetrics made it possible to nurse critically premature babies and increased their survival statistics.
Who is at risk
Any pregnant woman can give birth prematurely. Some expectant mothers have a higher chance of preterm birth. The risk zone includes pregnant women:
Some expectant mothers have a higher chance of preterm birth. The risk zone includes pregnant women:
- under 17 and over 35;
- have more than one fetus;
- have structural features of the uterus or its cervix;
- use harmful substances - drugs, alcohol, smoke;
- have heavy physical activity;
- have a history of preterm birth;
- work in hazardous production;
- are subjected to sexual, emotional abuse, stress, mental stress.
At risk are expectant mothers who are not registered during the gestation period or ignore ultrasound, screenings, laboratory tests.
The threat of early preterm birth is more common with diagnoses: diabetes mellitus, anemia, hypertension, genitourinary infections, hypothyroidism, problems with weight before conception (deficiency or obesity), thrombophilia, vaginal bleeding. There is also a risk when conceiving through IVF, with congenital malformations of the fetus.
If a woman has previously given birth to a child ahead of schedule, the chances of premature birth remain in subsequent pregnancies. The same applies to the weight of the crumbs: if the firstborn was born with a lack of body weight, then his brother or sister may be underweight.
Risk factors
Doctors point to a number of factors that take place long before the conception of a child. These include:
- Gynecological diseases suffered in childhood or adolescence;
- Early initiation of intimate life;
- Hereditary factor;
- Pathologies of previous pregnancy: preeclampsia, fetoplacental insufficiency, premature birth;
- Excessive uterine distension in multiple pregnancies, polyhydramnios;
- Threat of early miscarriage.
Another risk factor is surgery or trauma to the abdominal organs during the gestation period.
Risk of preterm birth at different terms
The birth of a child prematurely has many negative consequences for him. It depends on the trimester in which the pregnancy ended.
It depends on the trimester in which the pregnancy ended.
The most severe consequence is the death of the infant. With early preterm birth in the period of 22-24 weeks, the threat is the highest - up to 80% of babies die. This occurs against the background of intracranial hemorrhage of 3-4 degrees, cardiopulmonary insufficiency, intrauterine infection of the fetus.
Among those born in the period of 25 - 26 weeks, 40% of babies die, in 27 - 28 - about 20%, in 29 - 32 - no more than 10%, and in 33 - 34 - 2% of newborns are at risk.
Modern medicine is able to provide care for a premature baby and save his life. But no one can guarantee a full healthy life. Such a child can subsequently be given disappointing diagnoses: cerebral palsy, mental retardation, retinopathy of prematurity. He may suffer all his life from problems with the digestive and respiratory systems, impaired vision, hearing, delayed mental and physical development. Diagnosis implies disability.
For a woman in labor, preterm labor is usually not dangerous. Without concomitant pathologies, the mother's body does not care how long the child is born. There are only psychological problems: stress, fear and worries about the baby. It is better for a mother to tune in that her child, in case of severe prematurity, will be taken to the intensive care unit for nursing, so she will not see him immediately.
A newly minted mother needs rehabilitation. Therapy is prescribed, depending on the cause of the pathology: a complex of vitamins, antioxidants, hormones.
Why preterm birth is dangerous
Infants are immature: their body is covered with a large amount of cheese-like lubricant, there is a deficiency of subcutaneous fatty tissue, few hairs on the head and fluff on the body, cartilage on the ears and nose are soft, the nails do not go beyond the fingertips, the navel is located closer to the pubis.
Babies are underweight. Depending on the weight of the crumbs, 4 degrees of prematurity are distinguished: at the 1st degree, the baby weighs from 2500 to 2001 g, the 2nd - from 2000 to 1500 g, the 3rd - from 1500 to 1001 g, the 4th - 1000 g and below .
The development of the genital organs has not been completed: the testicles in boys are not lowered into the scrotum, and in girls the large labia do not cover the small and clitoris.
Children have immature lungs. They cannot breathe adequately - often they need help. The cry is weak. There are also problems with digestion. The body cannot absorb all the components from mother's milk.
Extrauterine life for children becomes a strong stress. It's hard to deal with him. They poorly resist infections, quickly lose heat, thermoregulation is impaired. They are subject to hemorrhages against the background of fragile vessels. Especially dangerous are hemorrhages in the cervical spinal cord and ventricles of the brain.
Among the complications of preterm birth are intracranial hemorrhages, asphyxia, intrauterine growth retardation.
Types of preterm birth
Several classifications have been adopted. Let's consider them.
- By term: critically early - up to 28 weeks, significantly early - from 28 to 32 weeks, moderately early or late - from 32 to 37 weeks;
- By the mechanism of attack: induced and spontaneous.
 Induced cause artificially for medical reasons. Occurs in 40% of cases. Spontaneous in 60% of cases begin with contractions, in 40% - with a rupture of the membranes;
Induced cause artificially for medical reasons. Occurs in 40% of cases. Spontaneous in 60% of cases begin with contractions, in 40% - with a rupture of the membranes; - By the nature of the course: spontaneous, with regular labor activity, without it and artificially provoked. In 80% of cases, preterm labor begins spontaneously. At the same time, the fetal bladder can be intact - and then the contractions are regular, growing. Or amniotic fluid may pour out, labor activity is chaotic. For medical reasons, early delivery can be artificially induced. For example, in case of danger to the life of the mother, intrauterine death of the fetus, or defects that are incompatible with life;
- According to symptoms: threatening, incipient and incipient. With threatening early premature birth, the lower abdomen and lower back hurt, the tone rises. Her neck remains unchanged, the external os is closed. When the process begins, pains appear in the lower abdomen. Regular contractions may begin.
 The neck is flattened or shortened. The main symptom of the onset of preterm labor is regular labor activity. The cervix opens by 2 - 3 cm, it happens quickly.
The neck is flattened or shortened. The main symptom of the onset of preterm labor is regular labor activity. The cervix opens by 2 - 3 cm, it happens quickly.
In 40% of women in labor, water breaks, 35% gave birth quickly and quickly. The active phase lasts less than when the baby appears on time. The contractions are monotonous, long and painful, the pauses between them are small.
Causes of preterm birth
Doctors indicate the main causes of the pathology:
- Early activity of the fetal endocrine system;
- Infections and inflammatory processes - ureaplasmosis, mycoplasmosis, pyelonephritis, bacterial vaginosis. They stimulate the production of prostaglandins. Hormones affect the uterine muscles - cause contractions and premature birth;
- Placental bleeding. They occur with incorrect presentation or detachment. The situation is serious, there is a threat to the life of the mother. Therefore, with presentation, hospitalization is indicated;
- Neck weakness.
 In 20% of cases, it leads to preterm birth. This also includes such factors: the interval between the current and previous gestation is less than 2 years, the woman is expecting 4 children or more;
In 20% of cases, it leads to preterm birth. This also includes such factors: the interval between the current and previous gestation is less than 2 years, the woman is expecting 4 children or more; - Isthmic-cervical insufficiency. The cervix opens itself - a miscarriage or premature birth occurs. It is possible to open mechanically - when scraping after a miscarriage, IVF, abortion;
- Pathologies on the part of the baby - intrauterine infection, malformations of internal organs.
Chronic ailments, dental problems, tonsillitis, the state of health during the gestation period, the genetic factor are all common reasons for early delivery. Sometimes it is impossible to determine. Although this is important for the development of effective means of preventing pathology.
Symptoms of preterm labor
We list the signs by which you may suspect that the baby is in a hurry to be born ahead of time.
Spasms over the pubis. They are similar to pain during menstruation.
Pain, pressure and discomfort in the genitals, thighs, pelvis. There is a dull pain in the lumbar region.
Feeling of pressure, pressure in the back.
Diarrhea, spasms and pain in the intestines.
Vaginal discharge - they get worse. May be watery, pink, brown, bloody.
Contractions of varying intensity. Touch your stomach with your fingertips - you will feel the contraction and relaxation of the uterus. Counted more than 4 contractions in 60 minutes? Call an ambulance - you need an urgent examination by an obstetrician.
The following symptoms are also dangerous: sudden blurred vision, flashes and “flies” before the eyes, incessant migraine, swelling of the face or hands, temperature of 38º C and above, painful urination, abdominal trauma, decreased fetal activity in the 3rd trimester (less than 10 movements in 12 hours).
Any of the above symptoms indicate the risk of preterm birth. Seek medical attention.
Diagnosis of preterm birth
Includes several stages.
Transvaginal ultrasound. The length of the cervix is measured, fetal fibronectin is determined - a kind of "biological glue" that binds the fetal sac to the uterine mucosa.
Gynecological examination. Allows you to assess the degree of opening of the neck, its length.
Rapid test for the determination of phosphorylated protein-1. The test determines the possibility of preterm birth. In the future, this helps prevent iatrogenic complications.
When diagnosing, 2 parameters are evaluated:
- Regularity of contractions;
- Neck changes - shortening and smoothing. informative method. For example, with a neck length of 3 cm, the risk of preterm birth in the next week is 1%. The patient is not admitted to the hospital, there is no danger to her and the fetus.
Differential diagnosis
Its goal is to correctly diagnose. The early birth of a baby is accompanied by cramps in the lower abdomen, diarrhea, pain in the lumbar region. These same symptoms are characteristic of other conditions: appendicitis, colitis, cystitis, pyelonephritis.
These same symptoms are characteristic of other conditions: appendicitis, colitis, cystitis, pyelonephritis.
When complaining of pain in the lower abdomen, the patient is examined for the consistency of the scar after the previous cesarean section, for example. When the temperature rises, flu, sore throat, viral infection are excluded.
Diagnosis
Preterm birth is stated based on the clinical picture. Doctors are guided by such markers.
The first is the length of the neck - less than 2 - 2.5 cm.
The second is the determination of phosphorylated protein-1.
The third is the regularity of contractions. There should be at least 4 in 20 minutes.
Fourth - neck changes in dynamics.
Fifth - assessment of the degree of maturity of the neck. Determined by the level of PSIFR-1 in the cervical canal.
Usually the process begins rapidly, suddenly and intensely.
Treatment for preterm birth
The goal is to reduce the tone of the myometrium, reduce uterine contractions.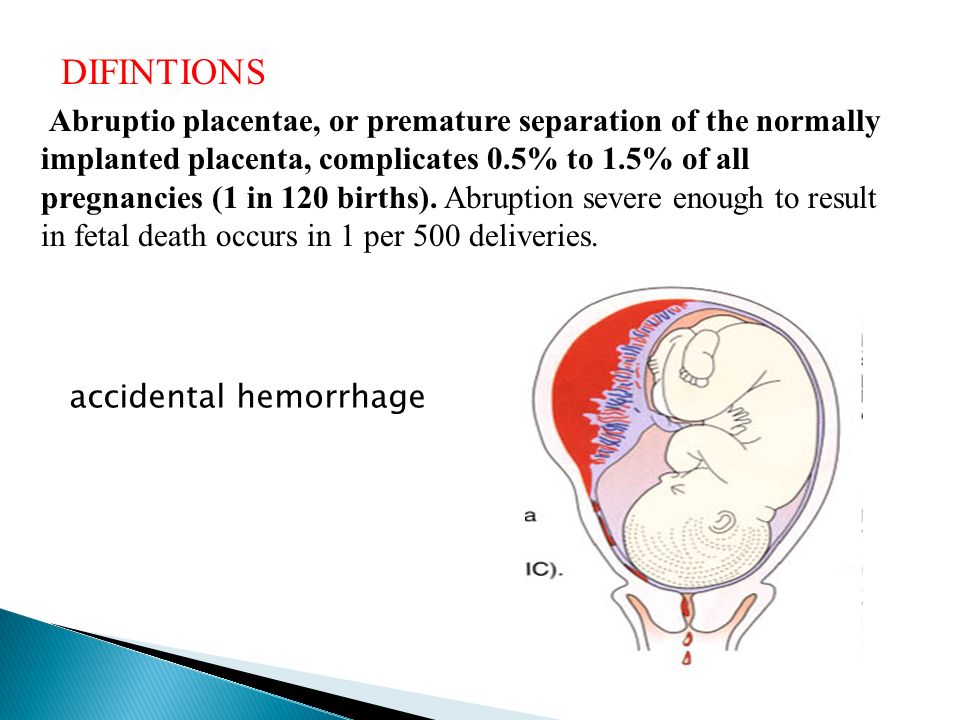 This is achieved by blocking oxytocin receptors - it is the hormone oxytocin that triggers the birth process.
This is achieved by blocking oxytocin receptors - it is the hormone oxytocin that triggers the birth process.
Such antagonists of oxytocin receptors are tocolytics. One of the modern representatives of this group of drugs is atosiban.
The remedy is effective, but has contraindications. It is forbidden to treat pregnant women for less than 24 and more than 33 weeks, with uterine bleeding, growth retardation, distress or fetal death, severe preeclampsia, with rupture of the fetal membrane after 30 weeks, placenta previa or its detachment.
5 stages of preterm labor
The first stage is forecasting their onset. Depends on the situation: the process is starting, has begun, or it is a threat.
Stage two - prevention of respiratory distress syndrome in a child. Doctors stimulate the maturation of the lungs. Apply funds from the group of glucocorticoids.
Stage three - prolongation of pregnancy. Doctors try to delay preterm labor by giving the baby's lungs and placenta time to mature. For this, tocolytics are used - they inhibit the contractile activity of the uterus. Usually prophylaxis is carried out - tocolysis is carried out before contractions. When started, therapy is ineffective. The duration of treatment is a maximum of 48 hours.
For this, tocolytics are used - they inhibit the contractile activity of the uterus. Usually prophylaxis is carried out - tocolysis is carried out before contractions. When started, therapy is ineffective. The duration of treatment is a maximum of 48 hours.
Stage four - preparation for the birth of a premature baby. The woman in labor is transferred to a higher-level hospital. The physiology of preterm labor does not differ from the birth of a child at term. But close attention is required from doctors to minimize complications for mom and baby.
The fifth stage is the prevention of infections and their complications. At risk are women in labor whose waters have broken. If the patient gives birth before 34 weeks, she can be pierced with a course of dexamethasone. It accelerates the maturation of the placenta and internal organs of the baby, reduces the risk of complications.
OB sequence
When registering a patient with preterm birth, the doctor gets acquainted with the exchange card, studies the general, gynecological and infectious anamnesis, and the results of examinations. Clarifies complaints and evaluates the condition of the woman in labor. He examines her, measures the pulse and respiration rate, temperature, pressure, abdominal circumference and the height of the uterus.
Clarifies complaints and evaluates the condition of the woman in labor. He examines her, measures the pulse and respiration rate, temperature, pressure, abdominal circumference and the height of the uterus.
Clarifies data on the fetus: movements, measures heart rate by auscultation - listening to the heart through the mother's stomach through the device. To assess the condition of the crumbs, the doctor performs cardiotocography. The device records the heart rate.
Ultrasound is performed to assess the condition of the child and mother's organs.
A gynecological examination is carried out: with intact membranes - external, with their rupture - internal. This is necessary to determine the position and position of the child, to assess the degree of disclosure.
Conduct a laboratory examination. They take a smear from the vagina: culture for β-hemolytic streptococcus, bacteriological culture, take blood and urine for a general analysis.
According to the results of the examination, the obstetrician confirms or refutes preterm birth, their stage.
The expectant mother is informed about her condition, forecasts for the child. At the slightest opportunity, they try to prolong the pregnancy. If the child is ready to be born in the near future, the doctor determines the tactics of assistance, coordinates the issue of anesthesia with the woman in labor.
In the absence of indications for a caesarean section, they give birth naturally. This is the best way - it is less traumatic for the baby. A gentle approach is what a weak newborn needs.
Preterm birth care policy
The woman in labor is provided with continuous psychological support. Describe the current obstetric situation.
With head presentation, they give birth naturally.
With pelvic - take into account clinical indications. Caesarean section is not the only effective method in this case. The operation does not improve the prognosis for a premature baby, but it puts an additional burden on the mother's body: it increases infection, morbidity, and complications.
With foot presentation, only a caesarean section is done.
Anesthesia is carefully selected. Avoid opiates - they depress the respiratory center, which is dangerous for premature babies.
At the birth of a baby before 34 weeks, vacuum aspiration is prohibited. It increases the risk of neonatal morbidity. Dosed episiotomy, exit forceps for the birth of the head and epidural anesthesia are performed.
The umbilical cord is clamped at least 1 minute after the baby is born. This tactic reduces the frequency of intraventricular hemorrhage in preterm pregnancies up to 37 weeks of gestation.
Control the state of the crumbs. CTG is done every hour for 40 minutes, auscultation - periodically.
General recommendations for prevention
You need to think about it from the first trimester. If you want to inform the baby, follow the advice of gynecologists.
- Take care of yourself. Rest, avoid nervous overload.
 Sleep at least 7 hours;
Sleep at least 7 hours; - Eat well. Eat foods rich in vitamins, exclude fast food, fatty, fried, spicy and salty foods from the diet. Give up coffee and strong tea;
- Observe the drinking regimen. Try not to feel thirsty - drink water every 2 hours. If you don't want to - don't force yourself;
- Avoid physical activity. Active training, hard work, general cleaning alone are taboo for a pregnant woman. Try not to go outside on ice - you may fall, you will strain your muscles - this can increase your tone and provoke premature birth;
- Maintain personal hygiene. Wash your face after a bowel movement. Always wash and dry from front to back. This way you will not bring bacteria from the intestine into the vagina. Infections are provocateurs of premature birth;
- Lead a healthy lifestyle. Alcohol and cigarettes are taboo. Smoking pregnant women are predisposed to preterm labor. If you take medications on a regular basis, tell your gynecologist about it.
 Walk outdoors. Cancel active workouts in favor of leisurely walks in the park;
Walk outdoors. Cancel active workouts in favor of leisurely walks in the park; - Register at the antenatal clinic in the first trimester - at 6 ‒ 8 weeks. Visit a gynecologist, listen to him, take tests, undergo ultrasound, screenings;
- Be careful with sex. In the first trimester, it is better to limit or abstain from it as much as possible - the embryo must be fixed. With placenta previa and other pathologies, the gynecologist may forbid you to have intimate contacts - listen to him;
- Learn to understand your body. In the 2nd trimester, start listening to the baby: his movements, activity. Fix any changes, strange and unpleasant sensations - and talk about them to the doctor. In case of acute pain, contractions, spasms, blood, urgently call an ambulance - this may be a premature birth;
- Maintain bed rest. A gynecologist can advise you to rest. For example, with increased uterine contractions, tone;
- Rest every hour. Sit in a chair, lift your legs up.
 This will relax the muscles, eliminate swelling;
This will relax the muscles, eliminate swelling; - Be aware of the signs of preterm labor. In case of their threat, you will not miss a moment and consult a doctor. Perhaps the process can be stopped with the help of drugs. Treatment minimizes complications in the premature baby.
Preterm birth prevention
It is divided into 2 stages: before conception and after.
Preventive measures before conception
It is advisable to carry them out to mothers from the risk zone. The gynecologist limits intrauterine manipulations, such as curettage. During IVF, the number of embryos for transfer is regulated taking into account the age of the future mother and her health. Inform about the possibility of premature birth at conception through reproductive technologies.
Hydration is shown - enhanced drinking regimen. It improves fetoplacental blood flow and reduces the risk of preterm birth.
Eliminate infections. It is advisable to do this at the planning stage, since antibiotic treatment during gestation harms the fetus.
It is recommended to postpone the conception of a child soon after the birth of an older brother or sister. Mommy's body needs to recover from the previous pregnancy. It takes him at least 2 years to do this. During this time, the uterus will return to its previous state, strength, vitamin reserves and body reserves will be restored.
Vitamin complexes are prescribed for predisposition to preterm birth for planning and expectant mothers. Protein-rich dietary supplements are helpful. They strengthen the immune system, improve blood circulation, protect the pregnant woman from infections - and hence the child.
Secondary prevention of early delivery
With the threat of premature birth, the condition of the pregnant woman is monitored at critical periods: from 2 to 12 and from 18 to 22 weeks. During these periods, it is better to stay in the hospital of the perinatal center. Doctors prescribe drugs to maintain and prolong pregnancy.
Therapy is selected on an individual basis.
With a short neck from 1 to 2.5 cm, progesterone suppositories are prescribed vaginally. The hormone is also shown in previous preterm births. This tactic reduces their risk by 35%. This is a natural hormone. It is efficient and safe. It is prescribed in the first trimester. Synthetic hormone is harmful: it can provoke gestational diabetes.
If there is a threat of early birth of the crumbs, sutures are placed on the neck. The expectant mother is out of the risk zone in this situation, stitches may not be applied.
Another option is to install a pessary on the neck.
These methods reduce the statistics of premature births. But the mortality rate of newborns is not affected.
When carrying twins, circular or U-shaped sutures can be applied. In most cases, such tactics with a short neck in multiple pregnancies can provoke preterm labor. Vaginal progesterone is not prescribed.
For infections (for example, bacteriuria, gonococcus, syphilis, β-hemolytic streptococcus, bacterial vaginosis, chlamydia), antibiotic prophylaxis is prescribed. Depending on the diagnosis, penicillin, ampicillin, metronidazole, erythromycin, ceftriaxone, josamycin may be prescribed.
Depending on the diagnosis, penicillin, ampicillin, metronidazole, erythromycin, ceftriaxone, josamycin may be prescribed.
Terminals
Premature birth is one of the fears of many expectant mothers. Nobody is immune from this. But you can minimize the risks. Follow the recommendations of the gynecologist, take care of yourself, listen to your body, do not refuse to stay in the perinatal center.
Don't think bad. Modern medicine successfully nurses premature babies, reduces the risks of complications and consequences.
Makarov I.O. • Preterm birth
RS80 ultrasound scanner
Setting new standards! Unparalleled clarity, resolution, ultra-fast data processing, and a comprehensive suite of state-of-the-art ultrasound technologies to meet the most demanding diagnostic challenges.
Premature births are those that occur between 28 and 37 weeks of gestation and the fetus weighs between 1000 and 2500 g. and the fetal weight is 500 g or more, and the newborn survives for 7 days, then the birth is considered premature with an extremely low fetal weight.
Causes of preterm birth
Risk factors for preterm birth are: low socioeconomic status; unsettled family life; young age; abuse of nicotine, alcohol, drugs; previous abortions, premature births and spontaneous miscarriages; urinary tract infections; inflammatory diseases of the genital organs; severe somatic diseases; violations of the structure and function of the genital organs. The complicated course of this pregnancy also plays an important role in the occurrence of premature birth. Particular attention should also be paid to infectious diseases suffered during this pregnancy.
Prematurity, which occurs at 22-27 weeks, is 5% of their total. First of all, these births are caused by isthmic-cervical insufficiency, infection of the fetal membranes by their premature rupture. In this situation, the lungs of the fetus do not yet reach the necessary maturity, which does not allow to adequately provide the respiratory function of the newborn. It is not always possible to achieve acceleration of lung maturation with the help of drugs. As a result, the outcome of childbirth for a newborn in such a situation is the most unfavorable.
As a result, the outcome of childbirth for a newborn in such a situation is the most unfavorable.
Preterm birth at 28-33 weeks' gestation has a wider range of causes. The lungs of the fetus in these terms are also not yet mature enough, however, the appointment of certain medications in a number of cases makes it possible to accelerate their maturation. In this regard, accordingly, the outcome of childbirth for a newborn in these terms of pregnancy may be more favorable. The prognosis of more favorable outcomes of preterm birth increases at 34-37 weeks of gestation.
Symptoms of preterm labor
Distinguish between threatening, incipient and incipient preterm labor. Threatening preterm birth is characterized by intermittent pain in the lower back and lower abdomen against the background of increased uterine tone. In this case, the cervix remains closed. When starting premature birth, there are usually cramping pains in the lower abdomen, accompanied by a regular increase in the tone of the uterus (contractions). The cervix is shortened and opened. Often there is a premature rupture of amniotic fluid.
The cervix is shortened and opened. Often there is a premature rupture of amniotic fluid.
Premature birth is characterized by: untimely discharge of amniotic fluid; weakness of labor activity, discoordination or excessively strong labor activity; fast or rapid childbirth or, conversely, an increase in the duration of labor; bleeding due to placental abruption; bleeding in the afterbirth and early postpartum periods due to retention of parts of the placenta; inflammatory complications, both during childbirth and in the postpartum period; fetal hypoxia.
Treatment of pregnant women
If symptoms appear that indicate the possibility of preterm labor, treatment should be differentiated, since in the beginning of labor, treatment can be carried out aimed at maintaining the pregnancy, and with the onset of labor, such treatment is no longer effective. To reduce the excitability of the uterus and reduce its contractile activity, the following is prescribed: bed rest; sedatives; antispasmodic drugs. To reduce the direct contractile activity of the uterus, magnesium sulfate and ?-mimetics (partusisten, ginipral) are prescribed.
To reduce the direct contractile activity of the uterus, magnesium sulfate and ?-mimetics (partusisten, ginipral) are prescribed.
For the treatment of pregnant women who have threatened preterm labor, non-drug physiotherapy can also be used, such as electrorelaxation of the uterus by exposing it to an alternating sinusoidal current with a frequency in the range from 50 to 500 Hz and a current strength of up to 10 mA. Electrorelaxation is carried out using the apparatus "Amplipulse-4". This one is highly effective and is considered safe for mother and fetus. With threatening premature birth, acupuncture is also successfully used as an independent method in combination with drugs. With the threat of preterm birth, it is also important to prevent respiratory disorders (respiratory distress syndrome) in newborns by prescribing glucocorticoid drugs to the pregnant woman. The fact is that in premature newborns, respiratory problems occur due to a lack of surfactant in the immature lungs. Surfactant is a substance that coats the alveoli of the lungs, promotes their opening during inhalation and prevents the alveoli from collapsing during exhalation. A small amount of surfactant is produced already from 22-24 weeks of intrauterine life, however, it is very quickly consumed after preterm birth, and its more or less adequate reproduction is possible only after 35 weeks under the influence of glucocorticoids administered to the pregnant woman or acceleration of surfactant synthesis is observed. Contraindications for the appointment of dexamethasone are: peptic ulcer of the stomach and duodenum, circulatory failure III degree, endocarditis, nephritis, active form of tuberculosis, severe forms of diabetes mellitus, osteoporosis, severe preeclampsia. Such prevention of respiratory disorders makes sense at gestational ages of 28-35 weeks. Prevention is repeated after 7 days 2-3 times.
Surfactant is a substance that coats the alveoli of the lungs, promotes their opening during inhalation and prevents the alveoli from collapsing during exhalation. A small amount of surfactant is produced already from 22-24 weeks of intrauterine life, however, it is very quickly consumed after preterm birth, and its more or less adequate reproduction is possible only after 35 weeks under the influence of glucocorticoids administered to the pregnant woman or acceleration of surfactant synthesis is observed. Contraindications for the appointment of dexamethasone are: peptic ulcer of the stomach and duodenum, circulatory failure III degree, endocarditis, nephritis, active form of tuberculosis, severe forms of diabetes mellitus, osteoporosis, severe preeclampsia. Such prevention of respiratory disorders makes sense at gestational ages of 28-35 weeks. Prevention is repeated after 7 days 2-3 times.
Management of preterm labor
Adequate analgesia is essential in the management of preterm labor. Due to the fact that most complications in preterm birth, both in the mother and the fetus, are due to a violation of the contractile activity of the uterus, constant monitoring of uterine contractions and the condition of the fetus is mandatory. The duration of preterm labor is usually less than timely labor due to the increased rate of cervical dilatation. This is mainly due to the fact that in such situations isthmic-cervical insufficiency occurs more often, and with a small mass of the child, high uterine activity and intensity of contractions are not required for his birth. If the contractile activity of the uterus during preterm labor is normal, then expectant tactics are used in the management of labor. Prevention of fetal hypoxia is regularly carried out, epidural anesthesia is used. In order to reduce birth trauma during the period of exile, they provide benefits without perineal protection.
Due to the fact that most complications in preterm birth, both in the mother and the fetus, are due to a violation of the contractile activity of the uterus, constant monitoring of uterine contractions and the condition of the fetus is mandatory. The duration of preterm labor is usually less than timely labor due to the increased rate of cervical dilatation. This is mainly due to the fact that in such situations isthmic-cervical insufficiency occurs more often, and with a small mass of the child, high uterine activity and intensity of contractions are not required for his birth. If the contractile activity of the uterus during preterm labor is normal, then expectant tactics are used in the management of labor. Prevention of fetal hypoxia is regularly carried out, epidural anesthesia is used. In order to reduce birth trauma during the period of exile, they provide benefits without perineal protection.
Detection of premature rupture of membranes in preterm pregnancy can be somewhat difficult due to oligohydramnios and due to heavy discharge due to concomitant colpitis. In this regard, it is advisable to use the express method - amnitest. In case of premature rupture of membranes, expectant management is usually followed, controlling the possible development of infection, since the most important fact to be taken into account in such a situation is, first of all, the possibility of infection, which has a decisive influence on the management of pregnancy. Expectant tactics are most preferable at small terms of pregnancy.
In this regard, it is advisable to use the express method - amnitest. In case of premature rupture of membranes, expectant management is usually followed, controlling the possible development of infection, since the most important fact to be taken into account in such a situation is, first of all, the possibility of infection, which has a decisive influence on the management of pregnancy. Expectant tactics are most preferable at small terms of pregnancy.
If a premature rupture of the membranes is detected in the case of a premature pregnancy, the pregnant woman is hospitalized. The patient needs bed rest with a daily change of linen and good nutrition. Doctors exercise strict control over the health of the mother and fetus. They measure the circumference of the abdomen and the height of the fundus of the uterus above the womb, assess the quantity and quality of leaking water, determine the pulse rate, body temperature and heart rate of the fetus every 4 hours. It is necessary to determine the content of leukocytes every 12 hours with an analysis of the leukocyte blood count. Cervical cultures and vaginal swabs are monitored every 5 days. Tocolytic drugs are usually prescribed for premature rupture of the membranes in the case of threatened and incipient preterm labor. If labor activity has already begun on its own, then it is not advisable to suppress it. Antibiotics for premature rupture of the membranes are used in case of a risk of developing inflammatory complications, as well as with prolonged use of glucocorticoids, with isthmic-cervical insufficiency, if a pregnant woman has anemia, pyelonephritis and other chronic infectious diseases.
Cervical cultures and vaginal swabs are monitored every 5 days. Tocolytic drugs are usually prescribed for premature rupture of the membranes in the case of threatened and incipient preterm labor. If labor activity has already begun on its own, then it is not advisable to suppress it. Antibiotics for premature rupture of the membranes are used in case of a risk of developing inflammatory complications, as well as with prolonged use of glucocorticoids, with isthmic-cervical insufficiency, if a pregnant woman has anemia, pyelonephritis and other chronic infectious diseases.
Peculiarities of premature newborns
A child, after premature birth, has signs of immaturity: a lot of cheesy lubrication, insufficient development of subcutaneous fat, fluff on the body, short hair on the head, soft ear and nasal cartilages, nails do not go beyond the fingertips, the umbilical ring is located closer to the pubis, in boys the testicles are not lowered into the scrotum, in girls the clitoris and labia minora are not covered by large ones, the cry of the child is weak.