Grade 4 placenta
Placenta praevia | Pregnancy Birth and Baby
Placenta praevia | Pregnancy Birth and Baby beginning of content4-minute read
Listen
The placenta develops at the same time as your baby and is attached to the lining of your uterus (womb) during pregnancy. It allows for oxygen and nutrients to pass from you to your baby as well as producing hormones that support your pregnancy.
The fertilised ovum (egg) implants into the lining of your uterus and the placenta grows from there. As your pregnancy progresses and your baby and placenta increase in size, your womb expands and this affects the placenta's position. The area where the placenta is usually attached stretches upwards, moving the placenta away from your cervix.
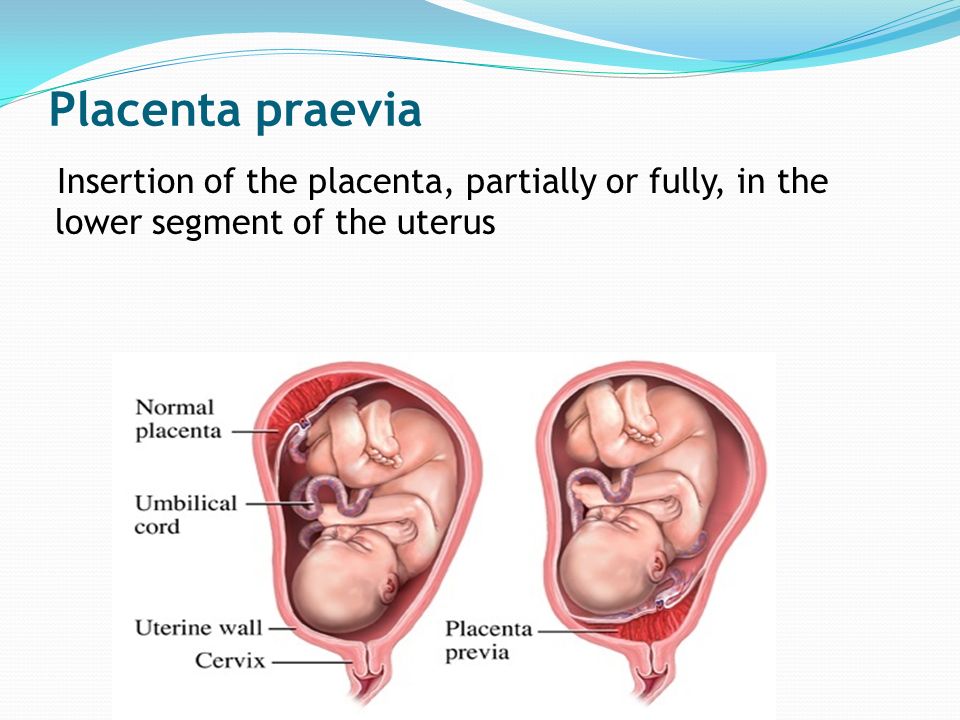
If the placenta stays low in your womb, near to or covering your cervix, it may block the baby's way out. This is called 'low-lying placenta' or 'placenta praevia'.
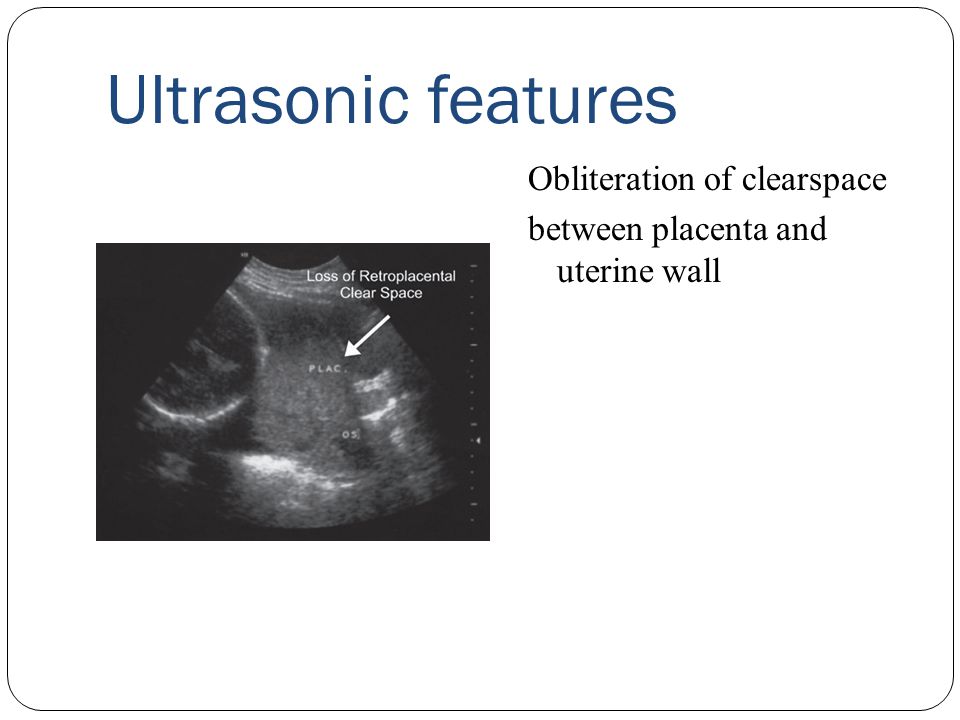
The position of your placenta will be recorded at your 18-22 week ultrasound scan. If your placenta is significantly low, you'll be offered an extra ultrasound scan later in your pregnancy (usually at about 32 weeks) to check its position again. For most women, the placenta will have moved into the upper part of the womb by this stage.
What causes placenta praevia?
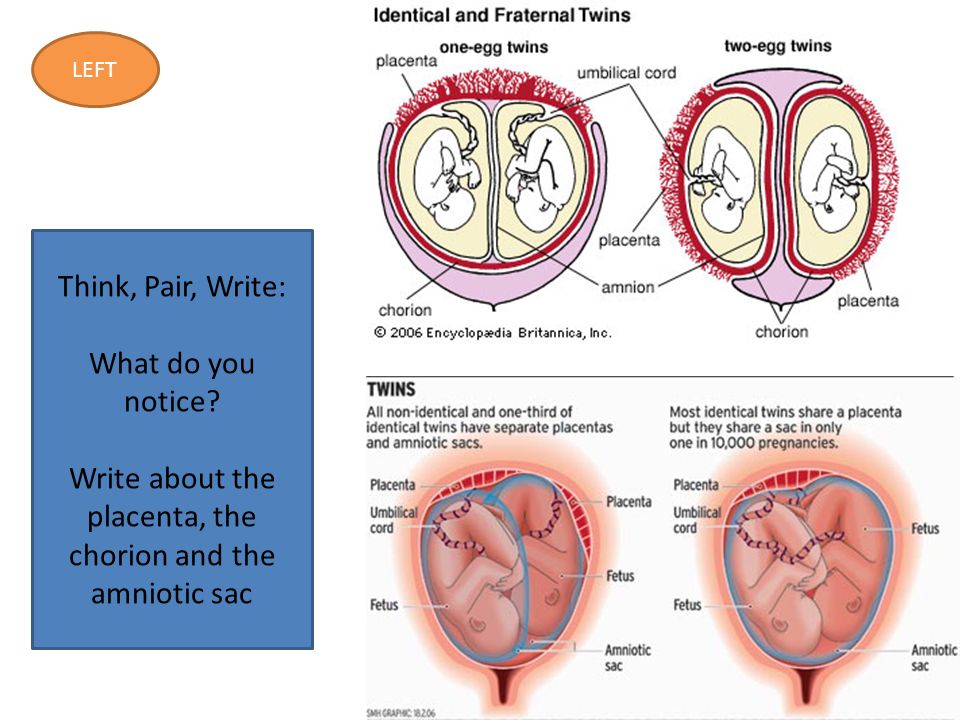
There is no obvious cause for placenta praevia. It may be that there is a larger placenta area (such as, if you are having twins) or there could be scar tissue from a previous caesarean or curette. There are several factors that can increase your risk of placenta praevia, including having had a caesarean section in the past (especially if your last baby was born by caesarean), and older age in the mother.
There is nothing you can do to prevent placenta praevia.
Placenta praevia symptoms
Signs that the placenta could be low-lying include painless, bright red bleeding from the vagina (either spontaneously or after sex) any time after 20 weeks of pregnancy.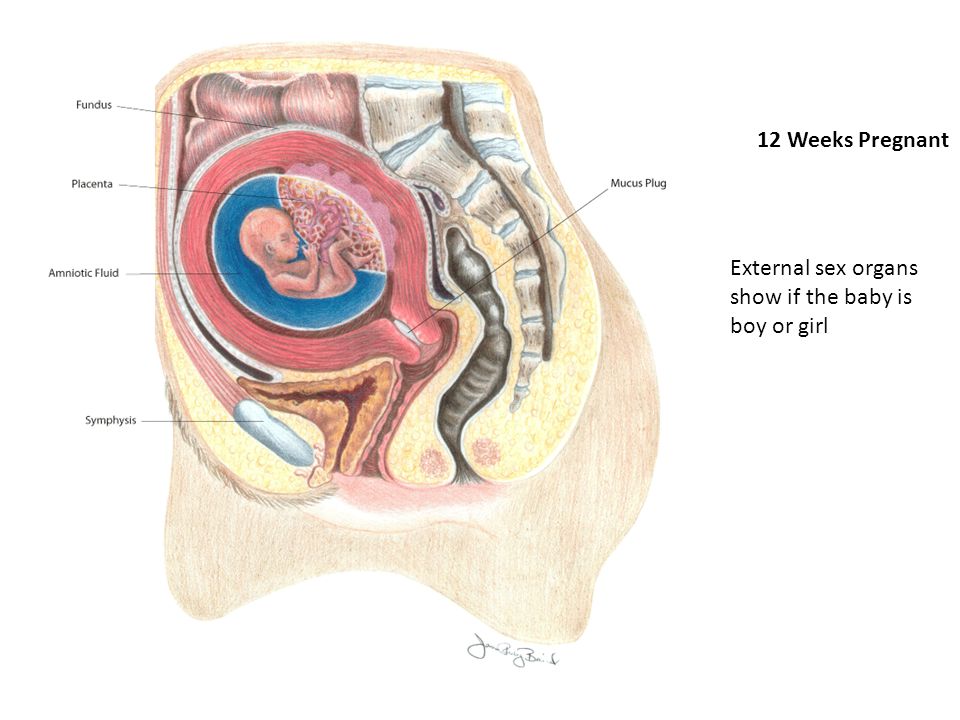 Placenta praevia is the most common cause of painless bleeding in the last trimester of pregnancy.
Placenta praevia is the most common cause of painless bleeding in the last trimester of pregnancy.
You may also experience:
- cramping in your uterus with bleeding
- bleeding during labour
If you experience bleeding during your pregnancy, contact your midwife or doctor immediately.
Placenta praevia treatment
Placenta praevia is graded into 4 categories from minor to major. If you have grade 1 or 2 it may still be possible to have a vaginal birth, but grade 3 or 4 will require a caesarean section.
Any grade of placenta praevia will require you to live near or have easy access to the hospital in case you start bleeding. Heavy bleeding may mean you need to be admitted to hospital for the remainder of your pregnancy.
When you are in hospital, your blood will be taken to make sure an exact donor blood match is available in case you need a blood transfusion. You may also need to take iron tablets if you have anaemia (low blood haemoglobin level).
If you have bleeding during your pregnancy and have Rh negative blood, you will need an injection of Anti D so your baby is not affected by the bleeding.
Your baby may also be monitored with a cardiotocograph (CTG) to make sure they are not distressed. The CTG records your baby's heart rate and response to movements and contractions.
Being in hospital doesn't stop you from bleeding, but your baby can be delivered more quickly if needed. Your doctor or midwife will discuss any test results with you and what steps may be needed to ensure you and your baby's wellbeing.
As well as speaking to your doctor or midwife for advice, you can get help and information from:
- Pregnancy, Birth and Baby — call 1800 882 436 to speak to a maternal child health nurse (7 days a week, 7am to midnight AET).
- The Australian Birth Trauma Association offers advice, resources and a peer-to-peer support service.
- The Centre of Perinatal Excellence (COPE) provides information and a list of support services.
- Perinatal Anxiety & Depression Australia (PANDA) — call 1300 726 306 to speak with a counsellor (Mon to Fri, 9am to 7.30pm AET).
Sources:
RANZCOG (Placenta praevia, placenta praevia accreta and vasa praevia: diagnosis and management), Women's and Children's Health Network (Placenta praevia), March of Dimes (Placenta previa)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2019
Back To Top
Related pages
- Placenta complications in pregnancy
- What is the placenta?
Need more information?
Placenta previa - Better Health Channel
betterhealth.vic.gov.au
Read more on Better Health Channel website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.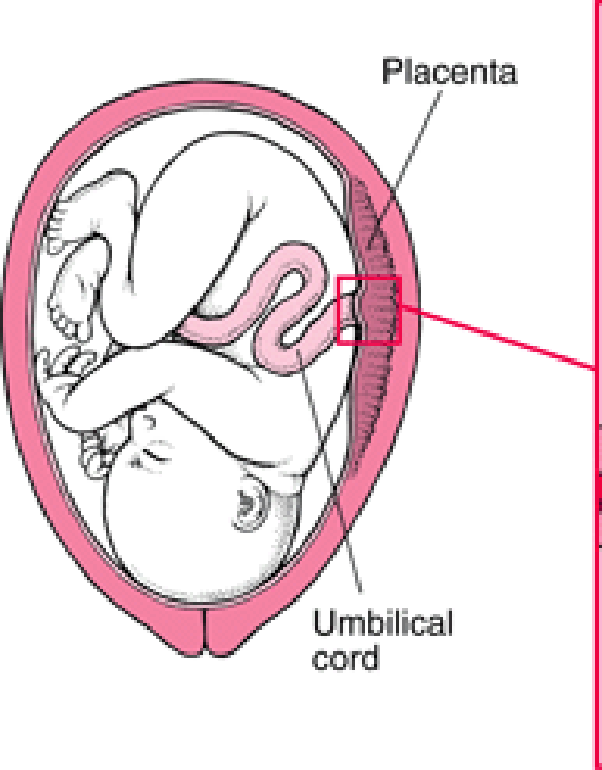
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Ageing or calcification of the placenta
In this article
- What does an 'ageing placenta' or 'calcification of the placenta' mean?
- How is the calcification or age of the placenta measured?
- How will an ageing or calcified placenta affect my delivery?
- Is it harmful to my baby if my placenta calcifies or ages too soon?
- Is there anything I can do to prevent early calcification or ageing of the placenta?
What does an 'ageing placenta' or 'calcification of the placenta' mean?
Placental calcification is the medical term for some of the changes that happen to the placenta, as pregnancy progresses.
Many researchers regard placental calcification as a normal ageing process, rather than a change related to a disease or ailment.
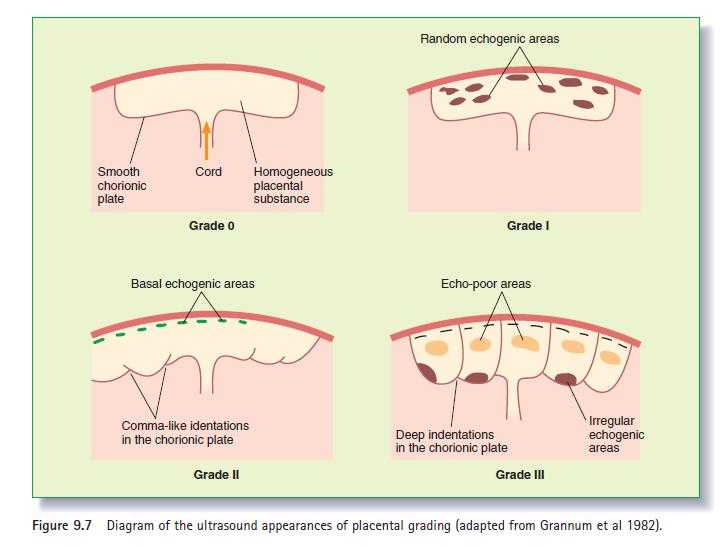
The placenta is usually described as going through four grades, from 0 (most immature) to III (most mature).
All placentas start at grade zero in early pregnancy. Changes can be seen from 12 weeks onwards. As pregnancy progresses, the placenta matures and calcifies.
It is classified into the following grades at different stages in pregnancy, at approximately the following times:
- Grade 0. Before 18 weeks of pregnancy.
- Grade I. Around 18 to 29 weeks of pregnancy.
- Grade II. Around 30 to 38 weeks of pregnancy.
- Grade III. Around 39 weeks of pregnancy. It is usually not seen before 38 weeks. A grade III placenta is known as a severely calcified placenta. At this stage, a formation of indentations or ring-like structures can be seen within the placenta.
How is the calcification or age of the placenta measured?
There is some uncertainty about whether changes in the placenta can be measured accurately as it can be difficult to grade the placenta objectively.
A lot depends on the interpretation of the ultrasound images by the ultrasound doctor. Some differences may also arise as it depends on how a doctor interprets the result.
How will an ageing or calcified placenta affect my delivery?
The effect of an ageing placenta on labour and delivery is difficult to say. Experts seem to have different opinions on the significance of a calcified placenta on delivery due to the lack of conclusive evidence.
Some placental changes during late pregnancy are considered a normal part of pregnancy and not thought to be of concern. However, in cases where changes occur earlier than expected, there is some disagreement regarding their significance.
Some risks that are known to be associated with placental calcification at each stage of pregnancy are listed below.
Changes between 28 and 36 weeks
One study suggests that women in high-risk pregnancies who develop a calcified placenta between 28 and 34 weeks need closer monitoring.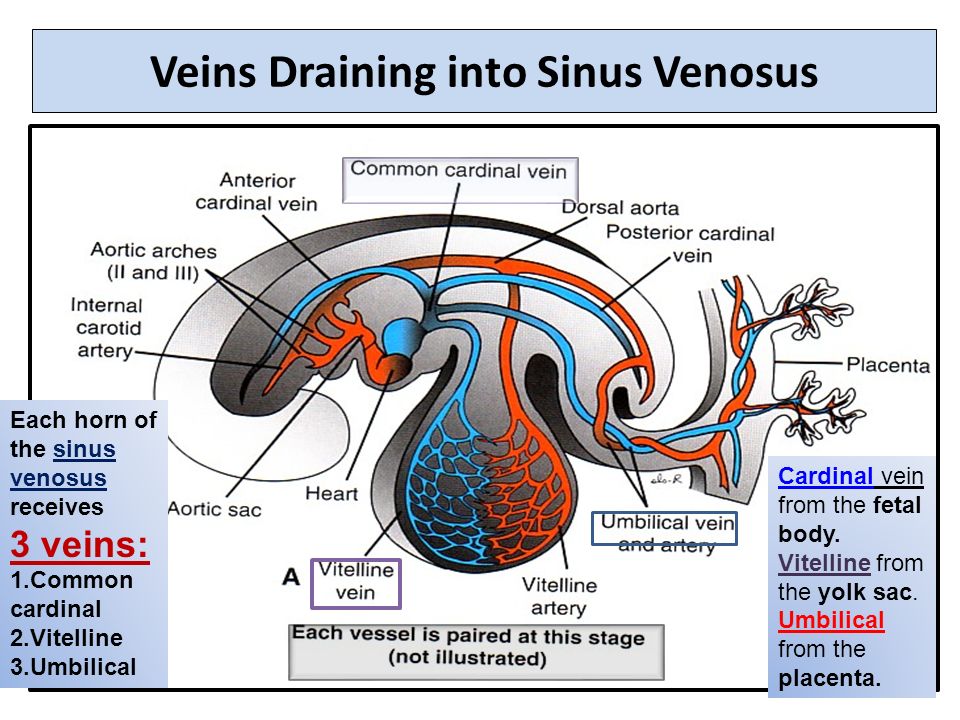 Some examples of high-risk pregnancies include pregnancies complicated by placenta praevia, diabetes, high blood pressure or severe anaemia.
Some examples of high-risk pregnancies include pregnancies complicated by placenta praevia, diabetes, high blood pressure or severe anaemia.
Calcification of placenta before 32 weeks of pregnancy is called an "early preterm placental calcification". It is known to be associated with a higher risk of pregnancy and birth complications, such as
- heavy bleeding after birth or postpartum haemorrhage
- placental abruption
- premature baby
- having a baby with a low Apgar score
- stillbirth
Changes from 36 weeks
One study has suggested that having a grade III placenta at 36 weeks is associated with an increased risk of pregnancy-related high blood pressure and having a low-birth-weight baby.
Hence, ultrasound scans that show placental calcification at 36 weeks may help in identifying high-risk pregnancies.
Changes from 37 to 42 weeks
A grade III calcified placenta from 37 weeks onwards is found in about 20 to 40 per cent of normal pregnancies.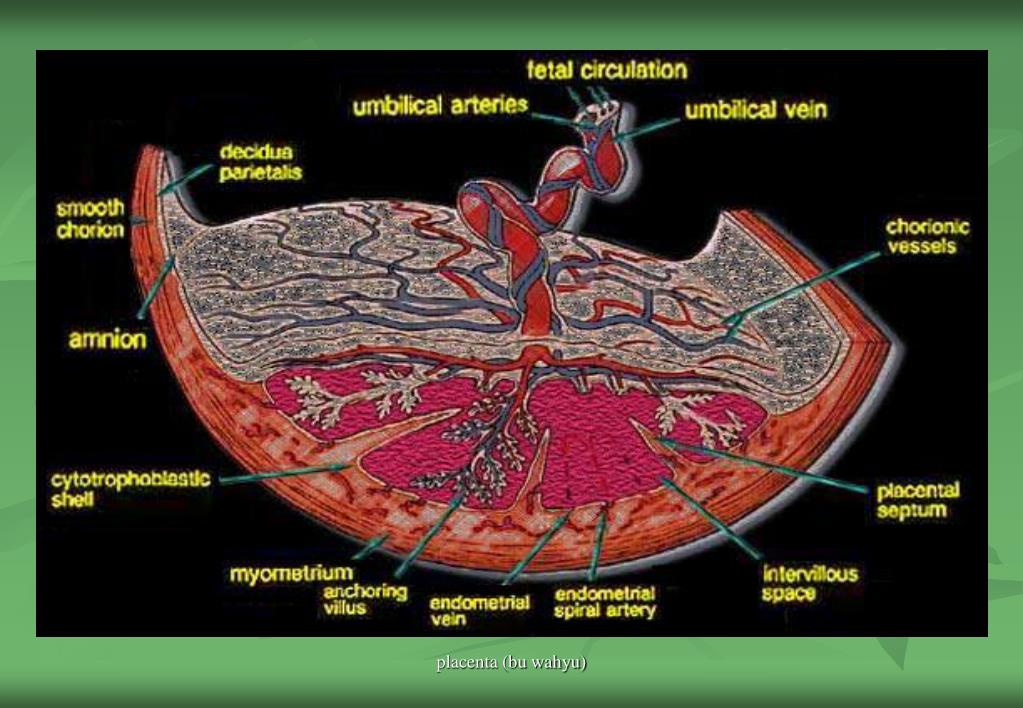 However, it is thought to of little clinical significance.
However, it is thought to of little clinical significance.
The effects of calcified placenta probably need to be evaluated on a case-to-case basis, depending on:
- how early the changes are seen
- how severe they are
- whether it is a high-risk pregnancy or not
- your doctor's opinion
Is it harmful to my baby if my placenta calcifies or ages too soon?
Preterm calcification of the placenta can be harmful to a baby in the womb, but it also depends on the grade and stage of pregnancy.
Some studies suggest that placental calcification before 32 weeks of pregnancy can result in low birth weight babies, babies with a low Apgar score and even stillbirth.
Some studies have shown that having a grade II placenta between 30 and 34 weeks can predict a low birth weight baby. But this is only among women who smoke during pregnancy.
Is there anything I can do to prevent early calcification or ageing of the placenta?
The exact causes of an ageing placenta are still not very clear, so it is difficult to say what would prevent it.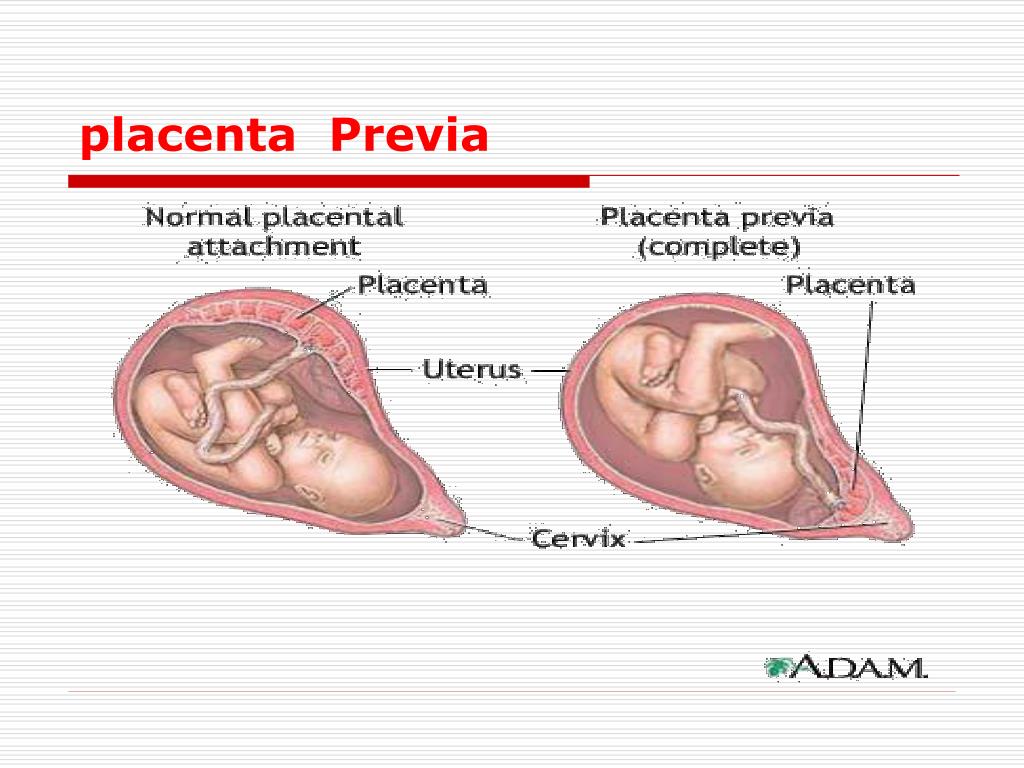 However, some research suggests that placental calcification is more likely in:
However, some research suggests that placental calcification is more likely in:
- younger women
- first-time pregnancies
- women who smoke during their pregnancy
Your doctor will be monitoring your health throughout your pregnancy. So, make sure you don’t miss any antenatal check-ups and your ultrasound scan appointments.
यह लेख हिंदी में पढ़ें!
Read more on:
- Scans to check the position of the placenta
- Low amniotic fluid (oligohydramnios)
- Dizziness in pregnancy
References
Abramowicz JS, Sheiner E. 2007. In utero imaging of the placenta: Importance for diseases of pregnancy. Placenta. 21(Suppl A):S14–S22.
Bricker L, Neilson JP, Dowswell T. Routine ultrasound in late pregnancy (after 24 weeks' gestation). Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No.: CD001451. DOI: 10.1002/14651858.CD001451.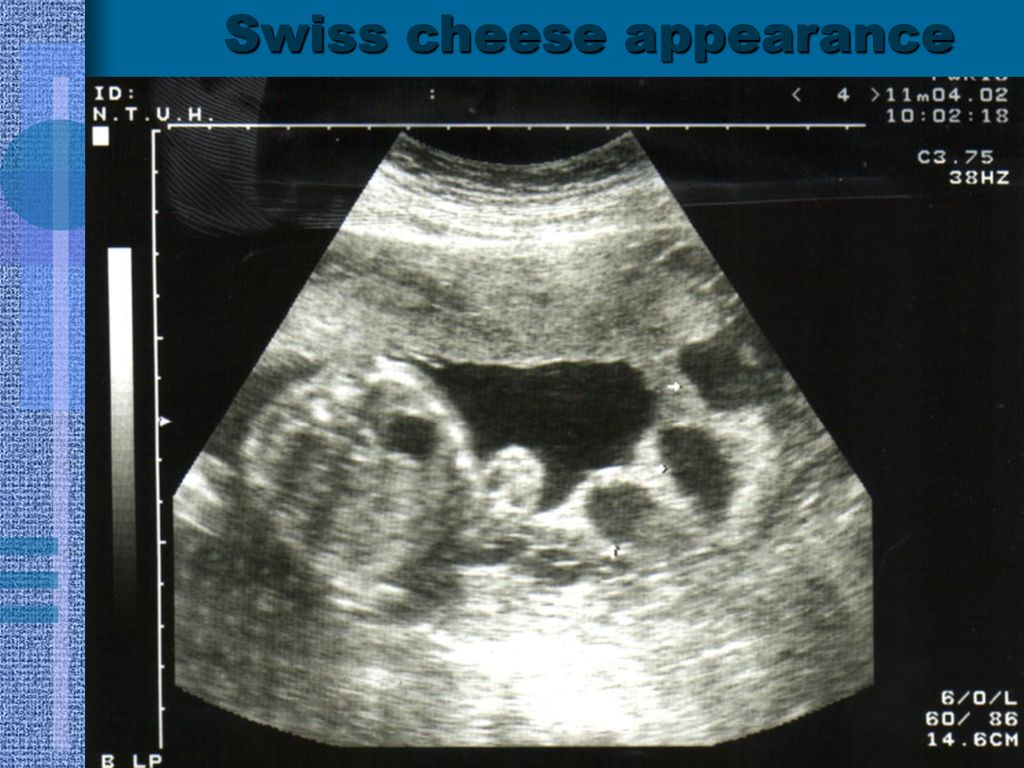 pub3.
pub3.
Chen KH, Chen LR, Lee YH. 2012. The role of preterm placental calcification in high-risk pregnancy as a predictor of poor uteroplacental blood flow and adverse pregnancy outcome. Ultrasound Med Biol. 38(6):1011-8. Online first 3 Apr.
Grannum PA, Berkowitz RL, Hobbins JC. 1979. The ultrasonic changes in the maturing placenta and their relation to fetal pulmonary maturity. American Journal of Obstetrics and Gynecology. 133:915–22.
Hill LM. Breckle R. Ragozzino MW. Wolfgram KR. O'Brien PC. Grade 3 placentation: incidence and neonatal outcome. Obstetrics & Gynecology. 61(6):728-32, 1983 Jun. Abstract. Full text available to Fellows, Members and Trainees.
Hills D. Irwin GA. Tuck S. 1984. Distribution of placental grade in high-risk gravidas. AJR. American Journal of Roentgenology. 143(5):1011-3.
Kazzi GM, Gross TL, et al. 1984. The relationship of placental grade, fetal lung maturity, and neonatal outcome in normal and complicated pregnancies. Am J Obstet Gynecol.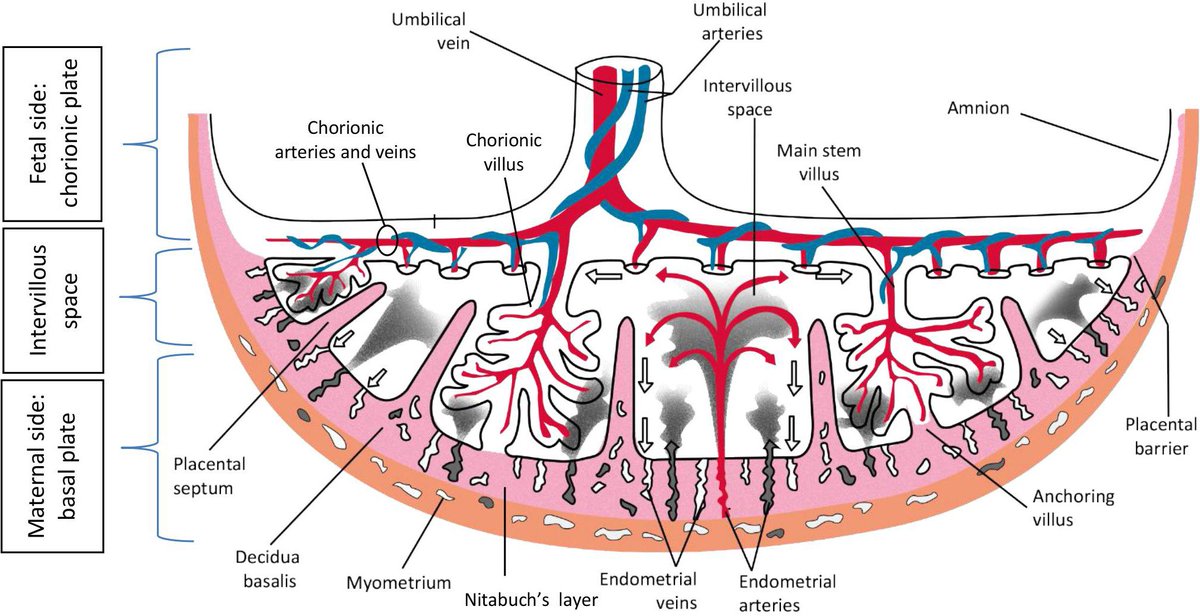 ;148(1):54-8
;148(1):54-8
McKenna D, Tharmaratnam S, Mahsud S, 2005. Ultrasonic evidence of placental calcification at 36 weeks' gestation: maternal and fetal outcomes. Acta Obstet Gynecol Scand. 84(1):7-10.
Miller JM Jr, Brown HL, Kissling GA, Gabert HA. The relationship of placental grade to fetal size and growth at term. Am J Perinatol 1988; 5: 19–21.
Moran M, Ryan J, Higgins M, et al. 2011. Poor agreement between operators on grading of the placenta. J Obstet Gynaecol. 31(1):24-8.
Proud J, Grant AM. 1987. Third trimester placental grading by ultrasonography as a test of fetal wellbeing. BMJ 294: 1641–4.
Smith R, Maiti K, Aitken RJ. 2013. Unexplained antepartum stillbirth: a consequence of placental aging? Placenta. 34(4):310-3. Online first 26 Feb.
Szymanowski K, Chmaj-Wierzchowska K, Florek E,et al. 2007. Does calcification of placenta reveal only maternal cigarette smoking? Przegl Lek. 2007;64(10):879-81.
Walker MG, Hindmarsh PC, Geary M, et al. 2010. Sonographic Maturation of the Placenta at 30 to 34 Weeks Is Not Associated With Second Trimester Markers of Placental Insufficiency in Low-risk Pregnancies. J Obstet Gynaecol. 32(12):1134.– 39.
Sonographic Maturation of the Placenta at 30 to 34 Weeks Is Not Associated With Second Trimester Markers of Placental Insufficiency in Low-risk Pregnancies. J Obstet Gynaecol. 32(12):1134.– 39.
Yin TT, Loughna P, Ong SS, et al. 2009. No correlation between ultrasound placental grading at 31-34 weeks of gestation and a surrogate estimate of organ function at term obtained by stereological analysis. Placenta. 30(8):726-30. Online first 12 Jun.
Show references Hide references
what is premature maturation of the placenta and how it threatens
Premature maturation of the placenta means the appearance of signs of maturity of the placental tissue before the gestational age, for which such changes are physiological. This condition does not manifest itself in any way and is detected on ultrasound screening.
Premature aging of the placenta is dangerous because the child will not receive adequate nutrition and oxygen. This can lead not only to fetal growth retardation, intrauterine hypoxia and premature birth, but also to the death of the child.
The placenta (from Latin Placenta - cake) is also called a children's place, which is the link between the baby and the mother. It is this temporary organ that ensures the delivery of nutrition and oxygen to the fetus, and also protects it from external influences.
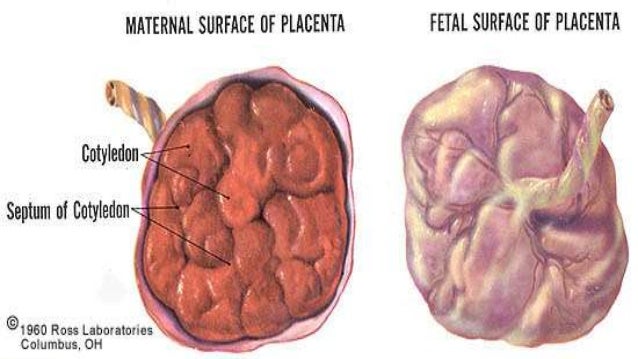
Placental tissue has a spongy structure. On one side, it is adjacent to the uterine wall, from where it receives blood thanks to common vessels, the other is connected to the child through the umbilical cord.
The child's place plays the role of a barrier that prevents the mixing of the blood of the mother and fetus. Through it, fresh blood, enriched with vitamins and minerals, enters the latter through a vein inside the umbilical cord.
The metabolic products of the fetus - urea, carbon dioxide, creatinine - are excreted through 2 umbilical arteries.
The placenta synthesizes important hormones for the pregnant woman.
How the placenta develops
A week after ovulation, the fetal egg enters the uterus and is introduced into its wall due to the chorionic membrane, which literally grows into the endometrium by dissolving epithelial cells.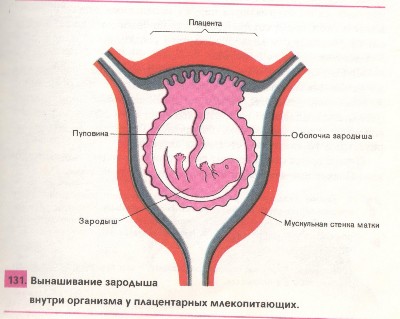 At the site of attachment, a chorion is formed, which gradually transforms into the placenta, and by 14-16 weeks this process is completed. But the final form of the child's place takes on only by the 20th week.
At the site of attachment, a chorion is formed, which gradually transforms into the placenta, and by 14-16 weeks this process is completed. But the final form of the child's place takes on only by the 20th week.
Until the middle of pregnancy, the young placental tissue increases and expands more and more, in the later stages it only adds a little in thickness.
The functionality of the placenta decreases along with the duration of pregnancy. It gradually develops its resource and grows old. At first, its membranes take on a wave-like shape, later point blotches appear in the placental tissue, consisting of deposits of calcium salts.
Further, these deposits increase, the sponginess is more and more smoothed out, giving density to the children's place, which at the same time becomes thinner. But all the described processes are physiological as long as they coincide in time with generally accepted standards.
There are 4 degrees of maturity of the placenta, which replace each other at a time determined by nature. If these deadlines are met, the child is not in danger. Otherwise, with a more rapid "fading" of the placental structure, we are talking about early aging. During a remote consultation, our doctors will connect independent doctors to provide a second opinion, make a list of tests, and analyze the reasons.
If these deadlines are met, the child is not in danger. Otherwise, with a more rapid "fading" of the placental structure, we are talking about early aging. During a remote consultation, our doctors will connect independent doctors to provide a second opinion, make a list of tests, and analyze the reasons.
How the placenta ages: maturity grades
The placenta during pregnancy matures in 4 stages, each of which has its own distinctive ultrasound signs:
| The degree of maturity of the placenta | Terms, weeks | Peculiarities |
| Zero | up to 30 | There are no inclusions, placental tissue is homogeneous, tends to increase in mass and volume |
| First | 30-34 | There are a small number of echogenic inclusions due to the compaction of the stroma, slight waviness of the chorionic plate. |
| Second | 35-39 | The waviness of the chorionic membrane is more pronounced, fragmentary thinning of the placental tissue is noted, its structure becomes denser, calcium deposits appear |
| Third | 37 and more | 3 degree of maturity of the placenta is manifested by the tortuosity of the chorionic plate. The previously smooth structure becomes lobulated and looks like a cluster of round lobules with rarefaction in the middle. Calcium deposits are clearly visible. The size and exchange area of placental tissue are reduced |
What does old placenta mean
We can talk about premature maturation of placental tissue if:
- signs of the 1st degree of maturity occur before 27 weeks;
- signs of maturity of the placenta of the 2nd degree appear up to 32 weeks;
- the third degree of maturity of the placenta is fixed up to 36 weeks.
Such a development of events indicates a high risk of a functional deficiency of placental tissue and decompensation of the adaptive capabilities of the "woman-child" system.
Attention! Normally, the 3rd degree of maturity of the child's place is noted almost before the very birth, in the last weeks, and sometimes days before the onset of labor.
Early aging of the placenta during pregnancy: causes
The placental structure begins to age prematurely due to various reasons that can lead to increased work of the “woman-child” complex. The mechanism of early aging can be triggered by external and internal factors due to the pathological course of pregnancy.
Why does the placenta age early?
- a pregnant woman suffers from common diseases - for example, diabetes mellitus, hypertension, thyroid and kidney dysfunction. The cause of aging is the change in microcirculation and increased load on weakened organs;
- a woman has urogenital infections from the category of STIs - chlamydia, ureaplasmosis, herpes or mycoplasmosis;
- the mother suffered during pregnancy a viral disease - rubella, colds, flu;
- due to gestosis, which takes a long time.
 With short-term gestosis, nothing threatens the child's place, since the normal blood supply to the fetus is maintained due to the compensatory resources of the body. If toxicosis lasts a long time, accelerated growth of placental tissue begins, so it matures and ages faster;
With short-term gestosis, nothing threatens the child's place, since the normal blood supply to the fetus is maintained due to the compensatory resources of the body. If toxicosis lasts a long time, accelerated growth of placental tissue begins, so it matures and ages faster; - there is an isoserological conflict between the mother and the fetus, which have the opposite Rh factor. In particular, a child with hemolytic disease due to AB0 or Rh incompatibility requires an increased supply of nutrients and oxygen. As a result, the load on the placental tissue increases, which is why it becomes old faster.
It is in the power of a woman to protect herself from many factors that are fraught with problems with a child's place: stop drinking alcohol, smoking and be especially careful when taking medication. If you have any questions, please contact our doctors. At a remote consultation, they will select analogues of drugs, they will be in touch at any time of the day.
Risk factors
Aging of the placenta during pregnancy occurs faster under the influence of radiation, chemical, temperature effects in everyday life and at work. The likelihood of such an outcome is increased by factors such as:
- the presence of bad habits - smoking, taking psychoactive substances;
- excess / lack of body weight;
- hypodynamia;
- unbalanced, poor nutrition.
Attention! Early aging of the placenta is more common in multiple pregnancies and hormonal disruptions.
Consequences
Premature aging of the placenta in itself is not dangerous for the mother and child. It becomes a threat if the condition of the fetus worsens. It is important to understand that really serious deviations in the “age” of the placental tissue are cause for concern, since this organ is able to fully function even with partial damage or detachment.
The alarm should be sounded in case of a clear lag in the development of the fetus. In order not to miss it, it is necessary to periodically do unscheduled ultrasounds.
Case study:
Ultrasound at 29 weeks showed signs of early maturation of the placenta. The woman donated blood for a coagulogram and platelets, according to the results of the examination, Curantyl was prescribed. Dopplerometry showed no abnormalities. The doctor recommended a second ultrasound in a month and assured me that complications were unlikely.
The symptoms of suffering in a child are as follows:
- developmental delay;
- disorder of placental circulation;
- signs of Rhesus conflict;
- persistent maternal hypertension;
- diabetes mellitus in the stage of decompensation in a pregnant woman.
These symptoms are an indication for medical intervention with possible hospitalization, up to urgent delivery.
If signs of early aging of the placenta occur at 22-26 weeks of gestation, then the likelihood of significant developmental delay and intrauterine fetal hypoxia is very high.
With an early manifestation of the pathology, accompanied by dystrophic and sclerotic changes, early discharge of water and detachment of the placenta, as well as premature birth, are often noted.
Attention! In severe cases, intrauterine death of the child is not excluded.
Treatment
If early aging of the placental tissue is detected at any time, the main pathology is treated, first of all, regardless of its type. To do this, drugs of various drug groups are used, including antibiotics, immunomodulators, steroids, cardiac drugs.
Specific therapy is aimed at improving the blood supply to the fetus. Antithrombotic, vasodilator drugs, amino acid complexes, hepatoprotectors cope with this task.
Of great importance are non-drug methods - dosed physical activity, a balanced diet, an optimal mode of work and rest.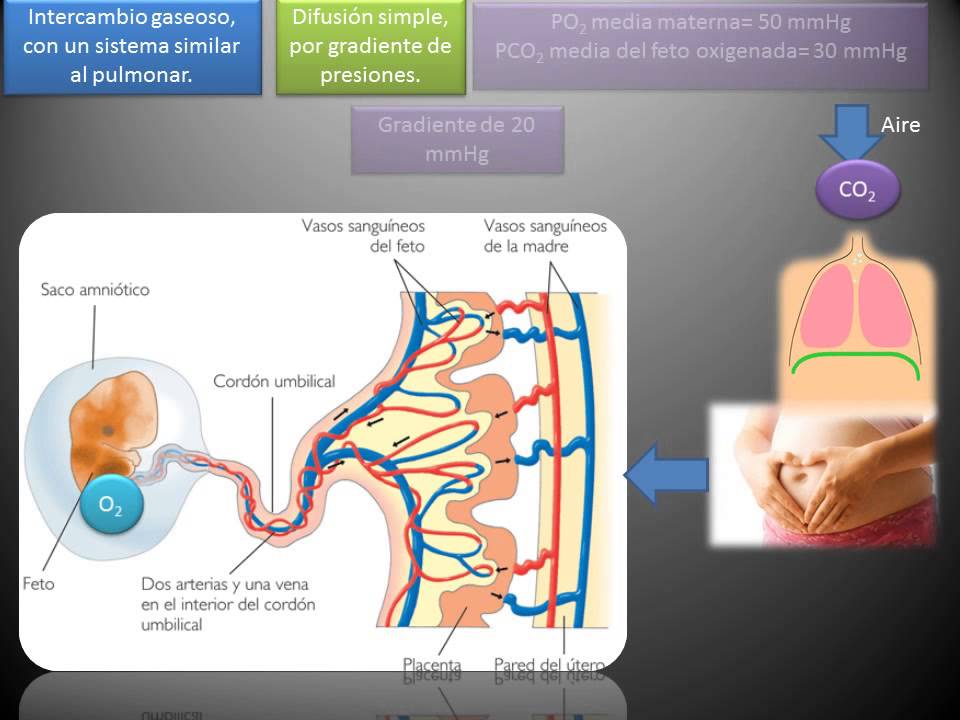
Case study:
A woman at 36.2 weeks of pregnancy was diagnosed with "premature aging of the placenta of the 2nd degree." The thickness of the placental tissue is 32 mm, multiple persificates. The development of the fetus corresponds to the gestational age, the blood flow is not disturbed, there is a single entanglement of the umbilical cord in the neck. Presumably, percificates and entanglement are a consequence of the transferred ARVI, which at such a time is no longer dangerous. This did not affect the child, since the blood flow and all parameters are normal.
FAQ
What drugs are used for treatment?
+
The standard treatment regimen includes antispasmodics (No-shpa, Papaverine) to reduce uterine contractility, agents to improve microcirculation (Kurantil, Actovegin), vitamin complexes. If fetal hypoxia is suspected, oxygen cocktails may be prescribed to a woman.
What are the indications for emergency delivery?
+
The lack of effectiveness of the treatment and the presence of negative dynamics of the state of the baby.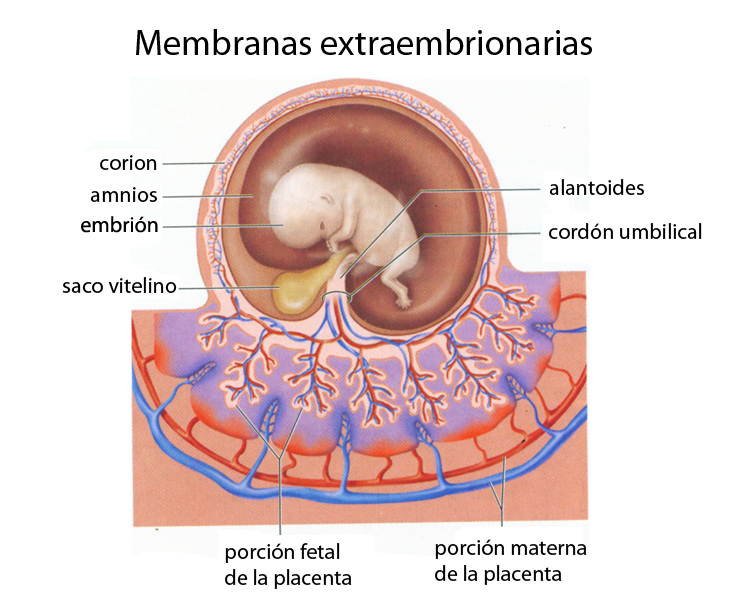
How many weeks of pregnancy is considered safe for an emergency delivery?
+
31-33 weeks. The indication may be a critical violation of the umbilical blood flow, CTG signs of oxygen starvation of the fetus, cessation of its growth, a sharp drop in the volume of amniotic water, as well as the presence of other conditions that threaten the health of the child.
Is it true that an old placenta can cause pregnancy to fail?
+
Yes, at maturity up to 25 weeks.
What tests are ordered to confirm the diagnosis?
+
Blood test for trophoblastic β-globulin, placental lactogen. If the level of these proteins is not reduced, then the placenta is functioning normally. However, these studies are not specific and are not significant diagnostic criteria.
What are the main ultrasound signs of an old placenta?
+
First of all, this is its thickening of more than 35 mm, the appearance of calcium deposits, increased waviness of the chorionic plate.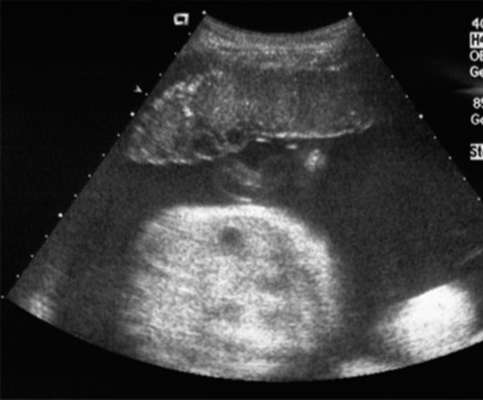
Expert opinion
Premature aging of the placenta requires a strictly individual approach, taking into account the underlying disease. Subject to the timely detection and adequate treatment of pathology, the risk of placental insufficiency can be reduced and the pregnancy can be extended to a time that is safe for the birth of a baby.
We publish only verified information
Article author
Menshikova Maria Viktorovna obstetrician-gynecologist
Experience 38 years
Consultations 1816
Articles 46
Specialist with extensive practical experience. He has a certificate of a mammologist, a certificate of professional certification. Participates in foreign business trips and individual training programs (Los Angeles).
He has a certificate of a mammologist, a certificate of professional certification. Participates in foreign business trips and individual training programs (Los Angeles).
- 1982 - 1986 NPO MONIIAG - obstetrician-gynecologist
- 1987 - 1989 VNITs OZMIR - obstetrician-gynecologist
- 1989 - 1992 departmental polyclinic st. Moscow - Kurskaya - obstetrician-gynecologist
- 1992 - 2001 NPO MONIIAG - obstetrician-gynecologist
- 2007 - 2008 NP KMIKM - doctor administrator
- 2009 - 2013 Pereslavl Central District Hospital, women's consultation - obstetrician-gynecologist
- 2020 to present Teledoctor24 LLC - doctor - consultant (gynecologist)
what is premature maturation of the placenta and what does it threaten
Premature maturation of the placenta means the appearance of signs of maturity of the placental tissue before the gestational age, for which such changes are physiological. This condition does not manifest itself in any way and is detected on ultrasound screening.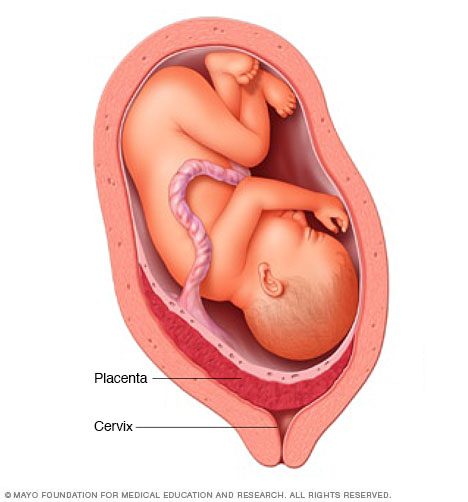
Premature aging of the placenta is dangerous because the child will not receive adequate nutrition and oxygen. This can lead not only to fetal growth retardation, intrauterine hypoxia and premature birth, but also to the death of the child.
The placenta (from Latin Placenta - cake) is also called a children's place, which is the link between the baby and the mother. It is this temporary organ that ensures the delivery of nutrition and oxygen to the fetus, and also protects it from external influences.
Placental tissue has a spongy structure. On one side, it is adjacent to the uterine wall, from where it receives blood thanks to common vessels, the other is connected to the child through the umbilical cord.
The child's place plays the role of a barrier that prevents the mixing of the blood of the mother and fetus. Through it, fresh blood, enriched with vitamins and minerals, enters the latter through a vein inside the umbilical cord.
The metabolic products of the fetus - urea, carbon dioxide, creatinine - are excreted through 2 umbilical arteries.
The placenta synthesizes important hormones for the pregnant woman.
How the placenta develops
A week after ovulation, the fetal egg enters the uterus and is introduced into its wall due to the chorionic membrane, which literally grows into the endometrium by dissolving epithelial cells. At the site of attachment, a chorion is formed, which gradually transforms into the placenta, and by 14-16 weeks this process is completed. But the final form of the child's place takes on only by the 20th week.
Until the middle of pregnancy, the young placental tissue increases and expands more and more, in the later stages it only adds a little in thickness.
The functionality of the placenta decreases along with the duration of pregnancy. It gradually develops its resource and grows old. At first, its membranes take on a wave-like shape, later point blotches appear in the placental tissue, consisting of deposits of calcium salts.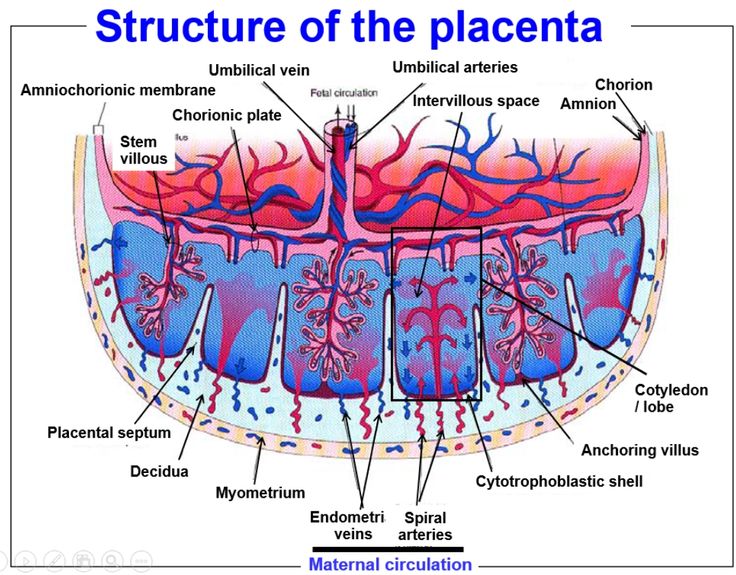
Further, these deposits increase, the sponginess is more and more smoothed out, giving density to the children's place, which at the same time becomes thinner. But all the described processes are physiological as long as they coincide in time with generally accepted standards.
There are 4 degrees of maturity of the placenta, which replace each other at a time determined by nature. If these deadlines are met, the child is not in danger. Otherwise, with a more rapid "fading" of the placental structure, we are talking about early aging. During a remote consultation, our doctors will connect independent doctors to provide a second opinion, make a list of tests, and analyze the reasons.
How the placenta ages: maturity grades
The placenta during pregnancy matures in 4 stages, each of which has its own distinctive ultrasound signs:
| The degree of maturity of the placenta | Terms, weeks | Peculiarities |
| Zero | up to 30 | There are no inclusions, placental tissue is homogeneous, tends to increase in mass and volume |
| First | 30-34 | There are a small number of echogenic inclusions due to the compaction of the stroma, slight waviness of the chorionic plate. |
| Second | 35-39 | The waviness of the chorionic membrane is more pronounced, fragmentary thinning of the placental tissue is noted, its structure becomes denser, calcium deposits appear |
| Third | 37 and more | 3 degree of maturity of the placenta is manifested by the tortuosity of the chorionic plate. The previously smooth structure becomes lobulated and looks like a cluster of round lobules with rarefaction in the middle. Calcium deposits are clearly visible. The size and exchange area of placental tissue are reduced |
What does old placenta mean
We can talk about premature maturation of placental tissue if:
- signs of the 1st degree of maturity occur before 27 weeks;
- signs of maturity of the placenta of the 2nd degree appear up to 32 weeks;
- the third degree of maturity of the placenta is fixed up to 36 weeks.
Such a development of events indicates a high risk of a functional deficiency of placental tissue and decompensation of the adaptive capabilities of the "woman-child" system.
Attention! Normally, the 3rd degree of maturity of the child's place is noted almost before the very birth, in the last weeks, and sometimes days before the onset of labor.
Early aging of the placenta during pregnancy: causes
The placental structure begins to age prematurely due to various reasons that can lead to increased work of the “woman-child” complex. The mechanism of early aging can be triggered by external and internal factors due to the pathological course of pregnancy.
Why does the placenta age early?
- a pregnant woman suffers from common diseases - for example, diabetes mellitus, hypertension, thyroid and kidney dysfunction. The cause of aging is the change in microcirculation and increased load on weakened organs;
- a woman has urogenital infections from the category of STIs - chlamydia, ureaplasmosis, herpes or mycoplasmosis;
- the mother suffered during pregnancy a viral disease - rubella, colds, flu;
- due to gestosis, which takes a long time.
 With short-term gestosis, nothing threatens the child's place, since the normal blood supply to the fetus is maintained due to the compensatory resources of the body. If toxicosis lasts a long time, accelerated growth of placental tissue begins, so it matures and ages faster;
With short-term gestosis, nothing threatens the child's place, since the normal blood supply to the fetus is maintained due to the compensatory resources of the body. If toxicosis lasts a long time, accelerated growth of placental tissue begins, so it matures and ages faster; - there is an isoserological conflict between the mother and the fetus, which have the opposite Rh factor. In particular, a child with hemolytic disease due to AB0 or Rh incompatibility requires an increased supply of nutrients and oxygen. As a result, the load on the placental tissue increases, which is why it becomes old faster.
It is in the power of a woman to protect herself from many factors that are fraught with problems with a child's place: stop drinking alcohol, smoking and be especially careful when taking medication. If you have any questions, please contact our doctors. At a remote consultation, they will select analogues of drugs, they will be in touch at any time of the day.
Risk factors
Aging of the placenta during pregnancy occurs faster under the influence of radiation, chemical, temperature effects in everyday life and at work. The likelihood of such an outcome is increased by factors such as:
- the presence of bad habits - smoking, taking psychoactive substances;
- excess / lack of body weight;
- hypodynamia;
- unbalanced, poor nutrition.
Attention! Early aging of the placenta is more common in multiple pregnancies and hormonal disruptions.
Consequences
Premature aging of the placenta in itself is not dangerous for the mother and child. It becomes a threat if the condition of the fetus worsens. It is important to understand that really serious deviations in the “age” of the placental tissue are cause for concern, since this organ is able to fully function even with partial damage or detachment.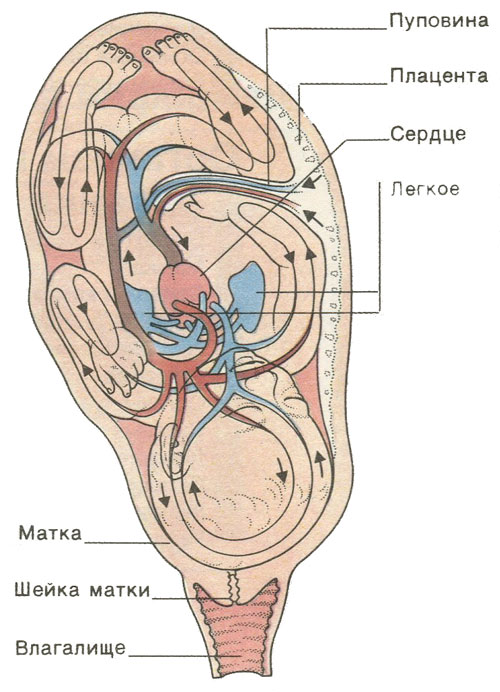
The alarm should be sounded in case of a clear lag in the development of the fetus. In order not to miss it, it is necessary to periodically do unscheduled ultrasounds.
Case study:
Ultrasound at 29 weeks showed signs of early maturation of the placenta. The woman donated blood for a coagulogram and platelets, according to the results of the examination, Curantyl was prescribed. Dopplerometry showed no abnormalities. The doctor recommended a second ultrasound in a month and assured me that complications were unlikely.
The symptoms of suffering in a child are as follows:
- developmental delay;
- disorder of placental circulation;
- signs of Rhesus conflict;
- persistent maternal hypertension;
- diabetes mellitus in the stage of decompensation in a pregnant woman.
These symptoms are an indication for medical intervention with possible hospitalization, up to urgent delivery.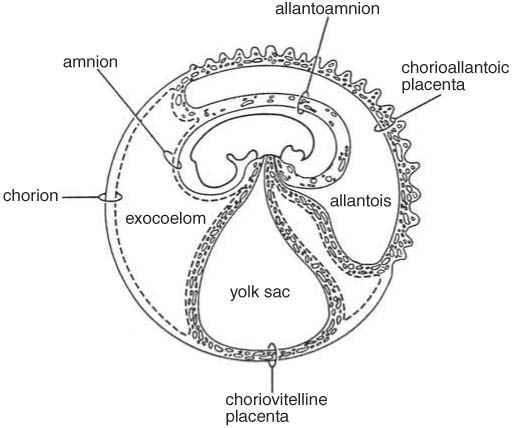
If signs of early aging of the placenta occur at 22-26 weeks of gestation, then the likelihood of significant developmental delay and intrauterine fetal hypoxia is very high.
With an early manifestation of the pathology, accompanied by dystrophic and sclerotic changes, early discharge of water and detachment of the placenta, as well as premature birth, are often noted.
Attention! In severe cases, intrauterine death of the child is not excluded.
Treatment
If early aging of the placental tissue is detected at any time, the main pathology is treated, first of all, regardless of its type. To do this, drugs of various drug groups are used, including antibiotics, immunomodulators, steroids, cardiac drugs.
Specific therapy is aimed at improving the blood supply to the fetus. Antithrombotic, vasodilator drugs, amino acid complexes, hepatoprotectors cope with this task.
Of great importance are non-drug methods - dosed physical activity, a balanced diet, an optimal mode of work and rest.
Case study:
A woman at 36.2 weeks of pregnancy was diagnosed with "premature aging of the placenta of the 2nd degree." The thickness of the placental tissue is 32 mm, multiple persificates. The development of the fetus corresponds to the gestational age, the blood flow is not disturbed, there is a single entanglement of the umbilical cord in the neck. Presumably, percificates and entanglement are a consequence of the transferred ARVI, which at such a time is no longer dangerous. This did not affect the child, since the blood flow and all parameters are normal.
FAQ
What drugs are used for treatment?
+
The standard treatment regimen includes antispasmodics (No-shpa, Papaverine) to reduce uterine contractility, agents to improve microcirculation (Kurantil, Actovegin), vitamin complexes. If fetal hypoxia is suspected, oxygen cocktails may be prescribed to a woman.
What are the indications for emergency delivery?
+
The lack of effectiveness of the treatment and the presence of negative dynamics of the state of the baby.
How many weeks of pregnancy is considered safe for an emergency delivery?
+
31-33 weeks. The indication may be a critical violation of the umbilical blood flow, CTG signs of oxygen starvation of the fetus, cessation of its growth, a sharp drop in the volume of amniotic water, as well as the presence of other conditions that threaten the health of the child.
Is it true that an old placenta can cause pregnancy to fail?
+
Yes, at maturity up to 25 weeks.
What tests are ordered to confirm the diagnosis?
+
Blood test for trophoblastic β-globulin, placental lactogen. If the level of these proteins is not reduced, then the placenta is functioning normally. However, these studies are not specific and are not significant diagnostic criteria.
What are the main ultrasound signs of an old placenta?
+
First of all, this is its thickening of more than 35 mm, the appearance of calcium deposits, increased waviness of the chorionic plate.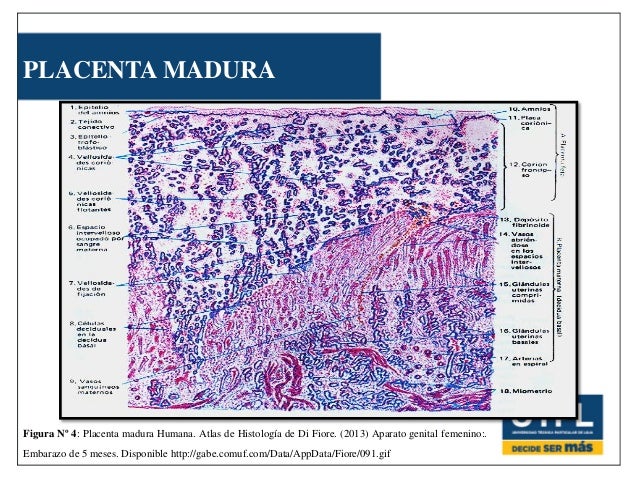
Expert opinion
Premature aging of the placenta requires a strictly individual approach, taking into account the underlying disease. Subject to the timely detection and adequate treatment of pathology, the risk of placental insufficiency can be reduced and the pregnancy can be extended to a time that is safe for the birth of a baby.
We publish only verified information
Article author
Menshikova Maria Viktorovna obstetrician-gynecologist
Experience 38 years
Consultations 1816
Articles 46
Specialist with extensive practical experience.
 Child seat growth stops
Child seat growth stops 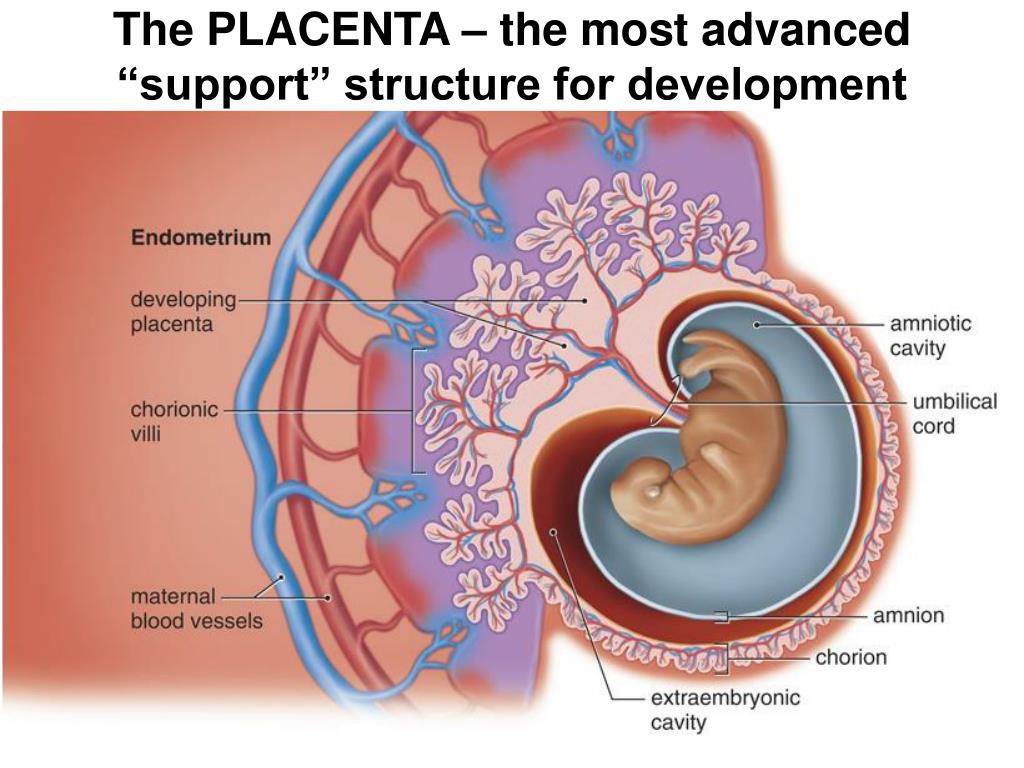 Child seat growth stops
Child seat growth stops