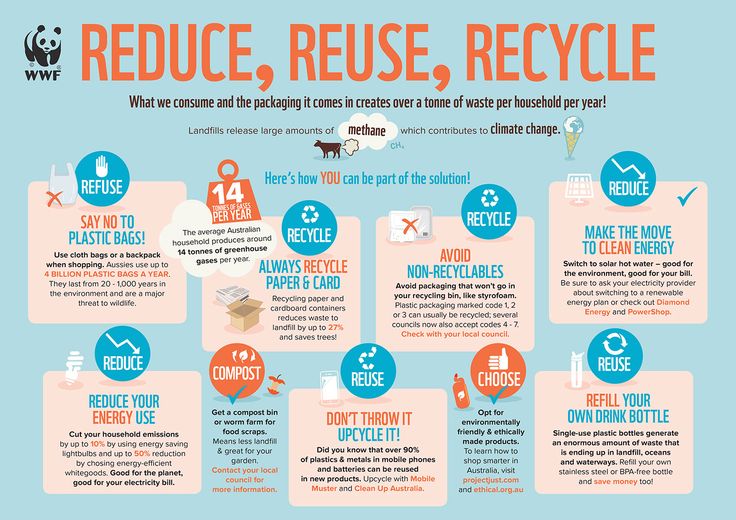
Soft spot on top of skull
Fontanelles - bulging Information | Mount Sinai
Soft spot - bulging; Bulging fontanelles
A bulging fontanelle is an outward curving of an infant's soft spot (fontanelle).
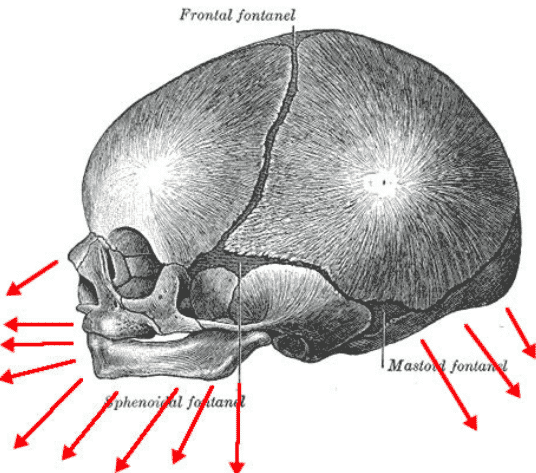
The sutures or anatomical lines where the bony plates of the skull join together can be easily felt in the newborn infant. The diamond shaped space on the top of the skull and the smaller space further to the back are often referred to as the soft spot in young infants.
A tense or bulging fontanelle occurs when fluid accumulates in the skull cavity or when pressure increases in the brain. Common causes are hydrocephalus or increased intracranial pressure due to illness.
Considerations
The skull is made up of many bones, 8 in the skull itself and 14 in the face area. They join together to form a solid, bony cavity that protects and supports the brain. The areas where the bones join together are called the sutures.
The bones are not joined together firmly at birth. This allows the head to change shape to help it pass through the birth canal. The sutures get minerals added to them over time and harden, firmly joining the skull bones together.
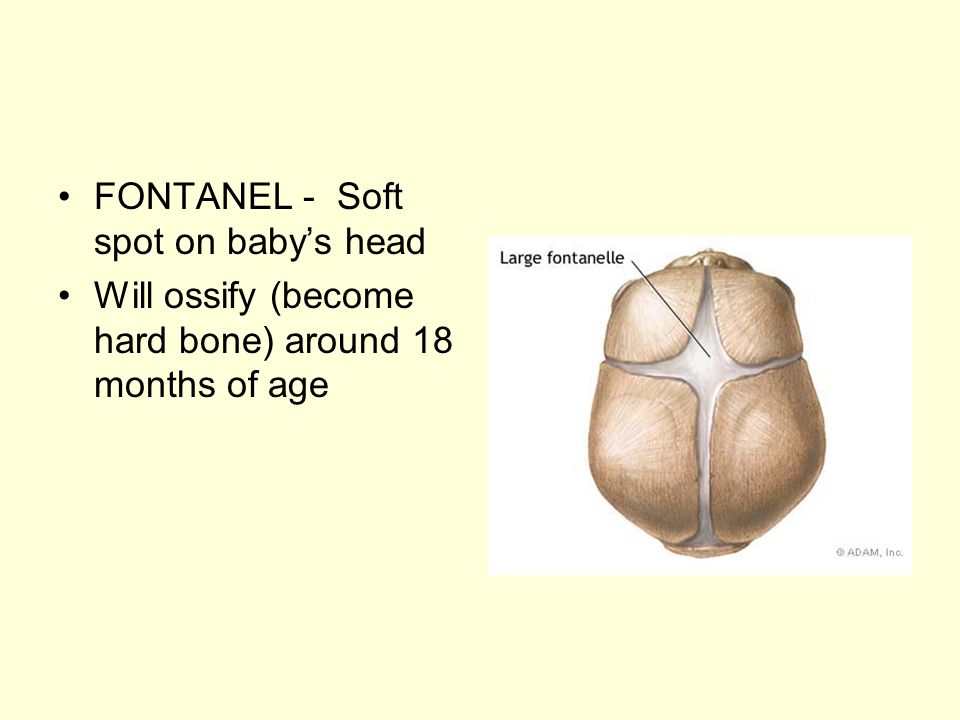
In an infant, the space where 2 sutures join forms a membrane-covered "soft spot" called a fontanelle (fontanel). The fontanelles allow for growth of the brain and skull during an infant's first year.
There are normally several fontanelles on a newborn's skull. They are located mainly at the top, back, and sides of the head. Like the sutures, fontanelles harden over time and become closed, solid bony areas.
- The fontanelle in the back of the head (posterior fontanelle) most often closes by the time an infant is 1 to 2 months old.
- The fontanelle at the top of the head (anterior fontanelle) most often closes between 7 to 19 months.
The fontanelles should feel firm and very slightly curved inward to the touch. A tense or bulging fontanelle occurs when fluid builds up in the brain or the brain swells, causing increased pressure inside the skull.
When the infant is crying, lying down, or vomiting, the fontanelles may look like they are bulging. However, they should return to normal when the infant is in a calm, head-up position.
Causes
Reasons a child may have bulging fontanelles include:
- Encephalitis.
 Swelling (inflammation) of the brain, most often due to infections.
Swelling (inflammation) of the brain, most often due to infections. - Hydrocephalus. A buildup of fluid inside the skull.
- Increased intracranial pressure.
- Meningitis. Infection of the membranes covering the brain.
Home Care
If the fontanelle returns to normal appearance when the child is calm and head-up, it is not a truly bulging fontanelle.
When to Contact a Medical Professional
Immediate, emergency care is needed for any infant who has a truly bulging fontanelle, especially if it occurs along with fever or excess drowsiness.
What to Expect at Your Office Visit
The health care provider will perform a physical exam and ask questions about the child's medical history, such as:
- Does the "soft spot" return to normal appearance when the infant is calm or head-up?
- Does it bulge all the time or does it come and go?
- When did you first notice this?
- Which fontanelles bulge (top of the head, back of the head, or other)?
- Are all the fontanelles bulging?
- What other symptoms are present (such as fever, irritability, or lethargy)?
Diagnostic tests that may be done are:
- CT scan of the head
- MRI scan of the head
- Spinal tap (lumbar puncture)
Goyal NK.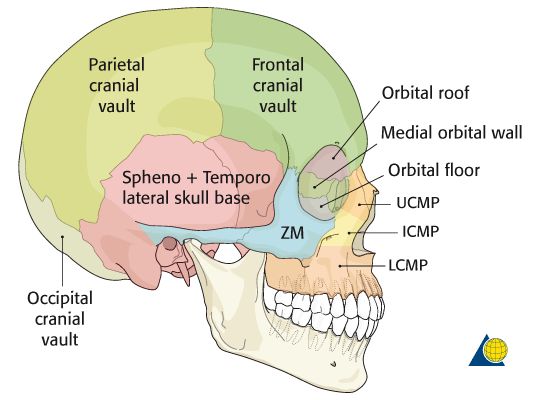 The newborn infant. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 113.
The newborn infant. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 113.
Rosenberg GA. Brain edema and disorders of cerebrospinal fluid circulation. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 88.
Somand DM, Meurer WJ. Central nervous system infections. In: Walls RM, Hockberger RS, Gausche-Hill M, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 99.
Last reviewed on: 2/2/2021
Reviewed by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
5 Warning Signs From Your Baby’s Soft Spot – Cleveland Clinic
When you’re a new parent, you learn that you need to protect that soft spot, or fontanelle, on your baby’s head. It rarely requires much attention, but it reminds you just how fragile your infant is.
It rarely requires much attention, but it reminds you just how fragile your infant is.
That’s why, if something changes — is the soft spot sunken in a little? — you may worry there’s something wrong.
A change in the fontanelle isn’t always a major problem, but it can sometimes reveal internal issues, says Violette Recinos, MD, Section Head of Pediatric Neurosurgery at Cleveland Clinic.
“It is a good indicator of the baby’s potential hydration status and brain status,” she says. “It’s like an automatic pressure sensor.”
What is the fontanelle?
The fontanelle is the space between different plates of a baby’s skull that will eventually come together. This aspect of an infant’s skull structure typically allows for easy delivery through the birth canal and for rapid head growth during the first year of life, Dr. Recinos says.
There are actually two soft spots — one at the back of the head and another on top. The posterior one closes within a few months of birth, while the top fontanelle typically remains until just past a child’s first birthday.
Dr. Recinos explains what changes in the fontanelle can tell you about your infant’s health.
Sunken in soft spot
This is often a sign of dehydration, she says. It may occur if your child is sick and not getting enough fluids.
What you should do: See your pediatrician if the sunken appearance persists and you can’t get your baby to take in more fluids.
Advertising Policy
Swollen soft spot
After a fall, a swollen soft spot (particularly if it’s accompanied by vomiting) is sometimes a sign of head trauma.
What you should do: Seek medical treatment right away.
Bulging soft spot
Fluid buildup (hydrocephalus) can cause rapid head growth and can make the soft spot look “full,” Dr. Recinos says.
A bulging fontanelle also might signal internal bleeding or a tumor or mass causing pressure in the head.
What you should do: If their soft spot is bulging, that’s a reason to seek care from your pediatrician, she says.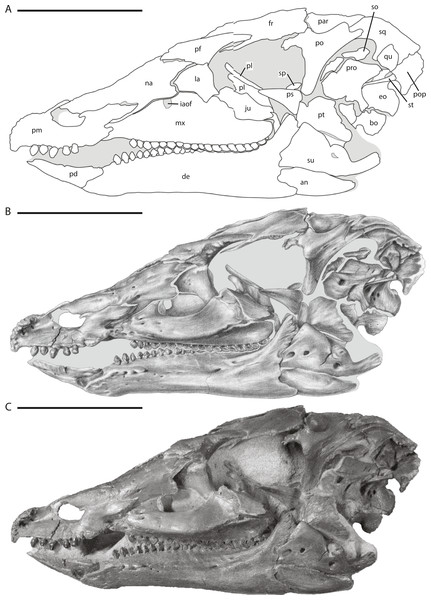
Seek emergency care if your infant exhibits fatigue, vomiting or unusual mental status along with the fontanelle’s fullness. Treatment for these conditions may include surgery to insert a shunt that relieves fluid buildup or to remove any underlying mass, Dr. Recinos says.
Disappearing soft spot
Most of the time the soft spot is obvious, particularly on a newborn. But at times it can seem to disappear quickly.
This may scare parents, but it typically means it’s just a “quiet fontanelle,” not that it has fused together prematurely, Dr. Recinos says.
Advertising Policy
As long as your child’s head is growing normally, all is probably well, she says. But your pediatrician may suggest an imaging test to make sure the fontanelle is still open.
Occasionally, though, the skull bones do close earlier than normal on one side, causing craniosynostosis. Depending on which bones fused, the baby may develop an abnormal head shape. For example, sagittal craniosynostosis, the most common form, results in a longer head that is shaped somewhat like a football.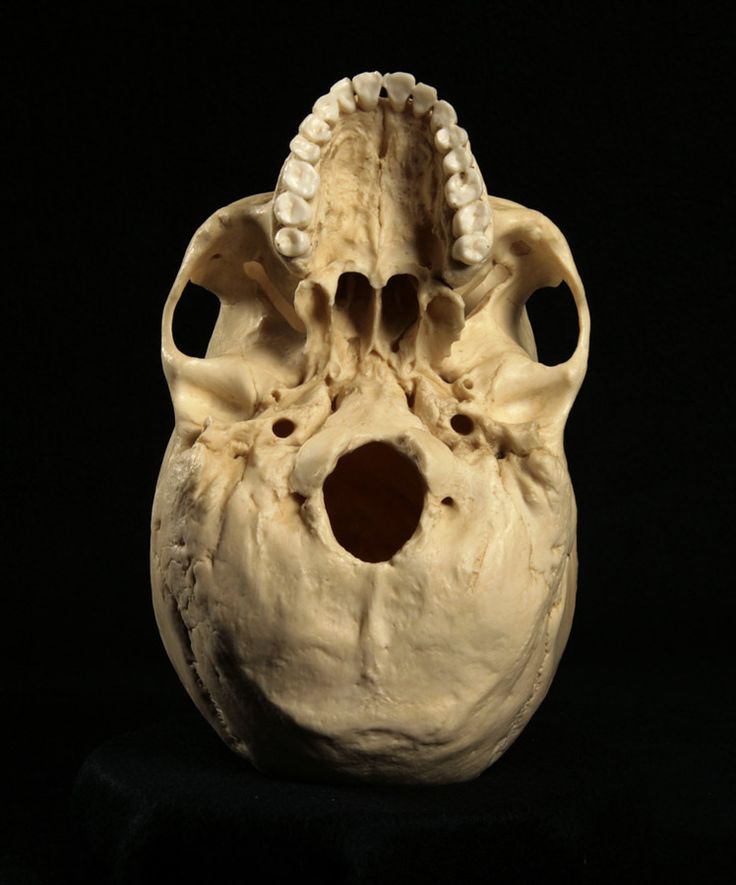
What you should do: Children with craniosynostosis may need surgery to open the fused bones and reshape the skull. In some cases, the child will wear a helmet afterward until the site heals and the head shape normalizes.
Soft spot that doesn’t close
If the soft spot stays big or doesn’t close after about a year, it is sometimes a sign of a genetic condition such as congenital hypothyroidism.
What you should do: Talk to your doctor about treatment options.
The bottom line? If you have any questions or concerns about your baby’s soft spot, it’s a good idea to check in with your pediatrician to make sure all is well.
6 types of headache: diagnosis and treatment
We are often asked what research is best done for headaches. It all depends on what is causing the problem. Even the most experienced doctor without a diagnosis (and in the case of a headache it is always an MRI) will not tell you the cause with 100% accuracy.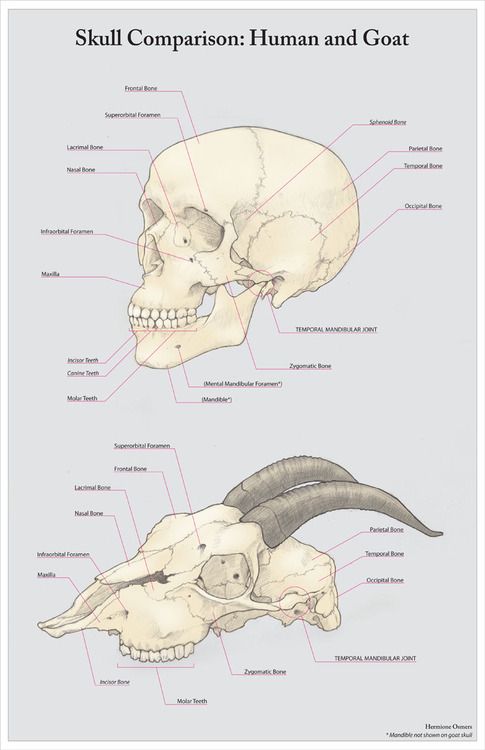 However, he can understand from your symptoms exactly where to look for the root of all troubles.
However, he can understand from your symptoms exactly where to look for the root of all troubles.
There are 6 main types of pain:
1. Sinus.
This is a sharp, severe pain in the region of the brow ridges, nose and cheekbones. Often appears in conjunction with a cold, flu, or seasonal allergies.
Cause in the sinuses - they are irritated, inflamed, swollen and/or filled with mucus, hence the discomfort. The pain will disappear after recovery.
People with similar symptoms are usually referred to an ENT. He will prescribe an MRI of the sinuses, according to the results, he will prescribe a course of antibiotics, antihistamines and decongestants. And if the disease has already progressed greatly, and pus has accumulated in the sinuses, then it can make a puncture and remove all the “trash” manually.
2. Cluster.
Rare, affecting only 1 in 1,000 people, and more common in men than women. This is an attack of very severe pain or burning in the eye area that lasts from 30 minutes to 3 hours. It repeats every day at the same time.
It repeats every day at the same time.
The torment may pass in a week, may linger for 3 months, and sometimes last for years. Fortunately, there are medications that can help. Special breathing and relaxation techniques can also relieve pain and have been shown to increase the time between attacks and make them less frequent.
The source of problems is hidden deep in the brain. This is a pair of symmetrical trigeminal nerves that are responsible for sensations of heat or pain in the face. The root of the nerve is located on the side of the eye, and branches run along the forehead, cheek, and from the chin to the area above the ear on one side of the face. To diagnose problems with the trigeminal nerves, your doctor will refer you to an MRI scan called "neurovascular conflict."
3-4. Headache from stress and tension.
As the name implies, this pain is caused by stress or tension (usually in the neck and shoulders). It is associated with strong psychological stress, poor posture, the habit of clenching your jaw and grinding your teeth, bright lights and, which is completely unfair, sitting at a computer for a long time.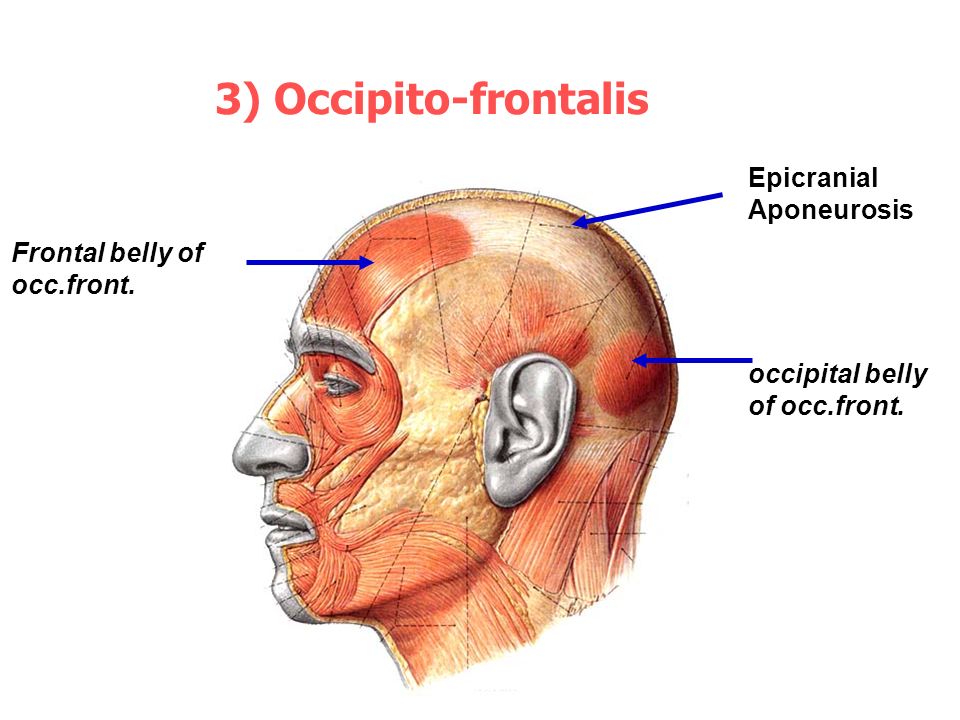
You can recognize this headache by the following signs:
1. It is symmetrical, that is, it is felt on both sides of the head or neck.
2. It is dull and obsessive, but not very strong, rather medium or even weak in intensity.
3. As if something is pressing or squeezing the hoop on the head, especially in the region of the forehead and the back of the head.
4. Normal movement of the head prevents pain and discomfort in the muscles.
5. Sensitivity to light and noise.
6. Insomnia and distraction.
7. Often occurs against the background of depression and feelings of longing.
This pain is relatively easy to manage. Rest, physical and mental, massages, posture correction will help to correct the situation. However, first you need to exclude some serious diseases with similar symptoms and understand whether it is stress or a problem with the cervical spine. As a rule, in this case, neurologists refer patients to the "Head and Neck" complex, which includes as many as 5 studies: the brain, arteries and veins of the brain, cervical region and arteries of the neck.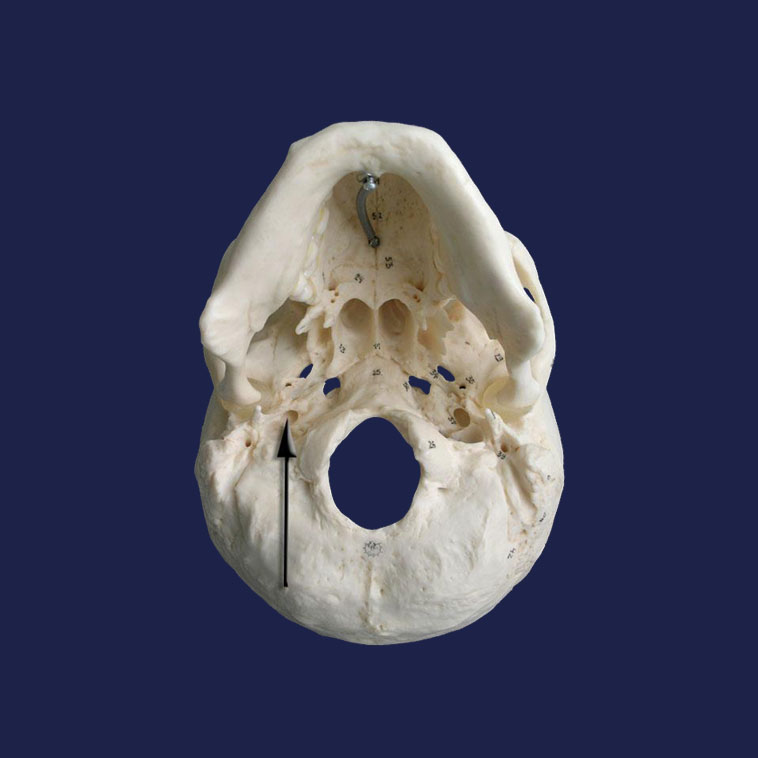
5. Migraine.
Severe throbbing pain - usually in one side of the head. Often accompanied by nausea, vomiting, and sensitivity to light and noise.
Migraine lasts for hours or even days and is so unbearable that the person cannot even get out of bed.
The aura often becomes a harbinger of seizures. These are flashes of light, blind spots or tingling/numbness in the face, arm or leg, loss of smell.
Migraine is now treated with medication and lifestyle changes. To make a diagnosis and prescribe medication, the doctor will ask you to bring the results of the MRI complex "brain + brain arteries + brain veins".
6. TMJ syndrome.
Headaches are a side effect of problems with the temporomandibular joint, which connects the lower jaw to the skull. Thanks to this joint, we can move the jaw up and down and left and right, speak, chew and yawn.
TMJ syndrome can be identified by the following signs:
1. Pain or discomfort in the jaw, around the ear, in the neck and shoulders when you eat, speak or open your mouth wide.
2. It is difficult to open or close the mouth, when chewing there is a feeling as if the lower and upper jaw do not match.
3. Clicks or grinding when moving the jaw.
4. Swelling on one side of the face.
In some cases, any of the above may be accompanied by toothache or pain in the neck and shoulders, pain and ringing in the ears, dizziness, hearing loss. Diagnosis of the syndrome is carried out using MRI of the temporomandibular joint.
Whichever of these types of pain you suspect, you should not self-medicate. There are many nuances in neurology that only a professional can take into account. In the event that you do not have your own proven doctor or if you want to get a second opinion, neurologists with 20 years of experience (including a candidate of sciences) work in the Moscow MRI Centers.
Health and good luck!
Head Injuries: Causes, Symptoms, Treatment | doc.ua
Causes
Head injury can be closed or open. The closed type is characterized by trauma to the brain through the bones and tissues of the skull, and is sometimes accompanied by a closed fracture of the bones of the skull. In the latter case, it is a closed craniocerebral injury. This also includes damage to the soft tissues of the skull without fracture of the bones. That is, we mean such a craniocerebral injury in which the intracranial cavity remains closed.
The closed type is characterized by trauma to the brain through the bones and tissues of the skull, and is sometimes accompanied by a closed fracture of the bones of the skull. In the latter case, it is a closed craniocerebral injury. This also includes damage to the soft tissues of the skull without fracture of the bones. That is, we mean such a craniocerebral injury in which the intracranial cavity remains closed.
Open traumatic brain injury can be non-penetrating and penetrating. With non-penetrating, the hard shell of the brain remains intact, with penetrating - it is damaged. With a penetrating wound, there is a risk of developing meningoencephalitis, purulent meningitis, and a brain abscess.
Consequences of a penetrating trauma of the skull in the brain and its membrane are complex pathological processes that are associated with disorders of both the brain itself and disorders of the liquor and blood circulation, swelling and swelling of the brain, infection. This complex is called traumatic brain disease. It is divided into five periods:
It is divided into five periods:
- acute (initial) - the first three days;
- early reactions and complications - from 3 days to 1 month;
- elimination of early complications and restriction of the infectious focus - from the second month to six months;
- complications - last up to 2-3 years;
- long-term consequences of traumatic brain injury - many years after the injury.
Symptoms
The main feature of injuries is a disorder of consciousness. If it continues for a long time, then there is a real threat to the life of the patient. To assess the severity of the patient's condition, the following scheme is used during his first examination:
- full consciousness after its short-term loss: the victim orients himself in the place of stay, time and situation, he adequately reacts to the environment;
- partial loss of consciousness: lethargy is observed in the behavior of the victim, he is drowsy, but he fulfills insistent demands;
- severe stupor: the victim performs elementary tasks only after insistent demands;
- medium stupor: the victim performs more complex tasks, answers the doctor's questions in monosyllables;
- slight stupor: the victim is slightly disoriented, responds slowly to questions;
- in the soporous state (hibernation), the victim retained only the main reflexes (corneal, corneal, bronchial and swallowing).
 The injured person reacts to pain stimuli with a grimace of pain or jerking of the limbs. Autonomic reactions to pain persist - rapid breathing and pulse, intermittent pupillary reactions, vasomotor disorders;
The injured person reacts to pain stimuli with a grimace of pain or jerking of the limbs. Autonomic reactions to pain persist - rapid breathing and pulse, intermittent pupillary reactions, vasomotor disorders; - coma - in this state, the victim does not respond to either external or internal stimuli. Motor activity is completely stopped. With increasing coma, all reflexes disappear, muscle tone decreases, sphincters relax. At the same time, respiratory function is disturbed, heart failure develops. Pupils dilate, pupillary reactions disappear. These symptoms are characteristic of atonic coma.
Often, head injuries associated with loss of consciousness are accompanied by retrograde amnesia: patients do not remember the moment of injury, they do not know about the loss of consciousness and its duration. The cardiovascular system responds by slowing down the heart rate. In parallel, irritation of the nuclei of the vagus nerve is observed, which then happens in various states. leading to high intracranial pressure. The pulse quickens due to irritation of the sympathetic nuclei of the trunk. At times, paroxysmal tachycardia joins the symptoms. There is a fluctuation in blood pressure and regional blood flow disorders. Cardiovascular disorders are accompanied by violations of the depth, frequency, rhythm of breathing. This is due to the direct connection of the systems with lesions of the parasympathetic and sympathetic nuclei of the brainstem.
leading to high intracranial pressure. The pulse quickens due to irritation of the sympathetic nuclei of the trunk. At times, paroxysmal tachycardia joins the symptoms. There is a fluctuation in blood pressure and regional blood flow disorders. Cardiovascular disorders are accompanied by violations of the depth, frequency, rhythm of breathing. This is due to the direct connection of the systems with lesions of the parasympathetic and sympathetic nuclei of the brainstem.
Vomiting is a clear sign of injury. It occurs immediately after the impact. It causes irritation of the IV ventricle, vestibular disorders, irritation of the meninges, as well as high intracranial pressure caused by edema and swelling of the brain. The vestibular apparatus responds with dizziness, a sensation of movement of objects around the injured person, spontaneous nystagmus, a violation of the sense of balance, labyrinthine deceptions that attack paroxysmal, dizziness and loss of consciousness. Often after a blow, a divergent strabismus is diagnosed, as well as a violation of convergence.
Symptoms of moderate and severe craniocerebral trauma make themselves felt with headaches resembling migraines or spasms - the patient complains of pressure in the temples, aching, burning and heaviness of the head, feel a painful pulsation. If there is no subarachnoid hemorrhage, then the headache is rarely severe. Pupillary reflexes are sluggish. Focal symptoms are the result of injury to various areas of the brain. Depending on the regular occurrence of the same manifestations or their combination, it is possible to determine which part of the brain is damaged. It does not necessarily coincide with external damage to the tissues of the skull.
Thus, paralysis, Jackson-type seizures and paresis are characteristic of the blockade of the functions of the motor center, compressed as a result of a fracture. Increasing paresis indicates the formation of a hematoma, arterial thrombosis, or the spread of phlebothrombosis. An equally important symptom is a speech disorder. The consequences of traumatic brain injury may include: post-traumatic arachnoiditis, brain atrophy, pachymeningitis, liquor fistula, chronic hematoma, etc.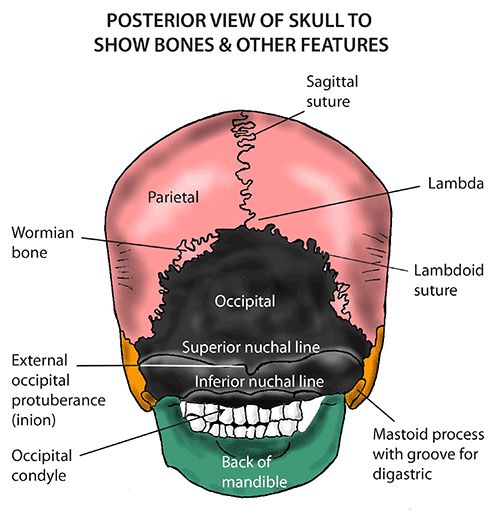
In the presence of any alarming symptoms, it is important to consult a traumatologist or surgeon in a timely manner. You can choose the right specialist in the list of doctors from the catalog of our website.
Cerebral concussion
Cerebral concussion is a complex of symptoms that occurs after a skull injury and develops as functional disorders. First of all, we are talking about vegetative disorders. This is the simplest form of injury of this kind. From the point of view of physiology, this is a syndrome of sudden paralysis or paresis of vasomotor, respiratory, reflex, and other brain activities resulting from injury against the background of loss of consciousness. Such a symptom complex is not accompanied by morphological changes in the membrane and tissues of the brain; this does not apply to other injuries of the skull. Signs of a concussion are:
- impaired consciousness ranging from stupor to stupor, which can be measured in seconds or minutes;
- retrograde amnesia, which covers events immediately before the injury, as well as anterograde amnesia, which covers a narrow period of time after the injury;
- after regaining consciousness, the victim complains of headaches, dizziness, weakness, noise and ringing in the ears.
 Hot flushes to the face, sleep disturbance, sweating and a number of other vegetative manifestations are observed. There are also pains in the region of the eyeballs and forehead during the movement of the open eyes, vestibular hyperesthesia develops, an oculostatic phenomenon, divergence of the eyeballs during reading;
Hot flushes to the face, sleep disturbance, sweating and a number of other vegetative manifestations are observed. There are also pains in the region of the eyeballs and forehead during the movement of the open eyes, vestibular hyperesthesia develops, an oculostatic phenomenon, divergence of the eyeballs during reading; - breathing becomes shallow, its frequency changes, but without arrhythmia, then it quickly returns to normal;
- the pulse corresponds to the physiological norm, but immediately after the injury it speeds up or slows down a little;
- a single vomiting is possible immediately after the impact;
- the face may turn pale, after which its hyperemia is observed;
- in some cases, concussion is accompanied by asymmetry of the mimic muscles of the face, tendon and skin reflexes. They disappear on the third day after the injury;
- CSF pressure is sometimes lowered.
These patients usually recover within a week of injury, provided adequate concussion treatment is provided .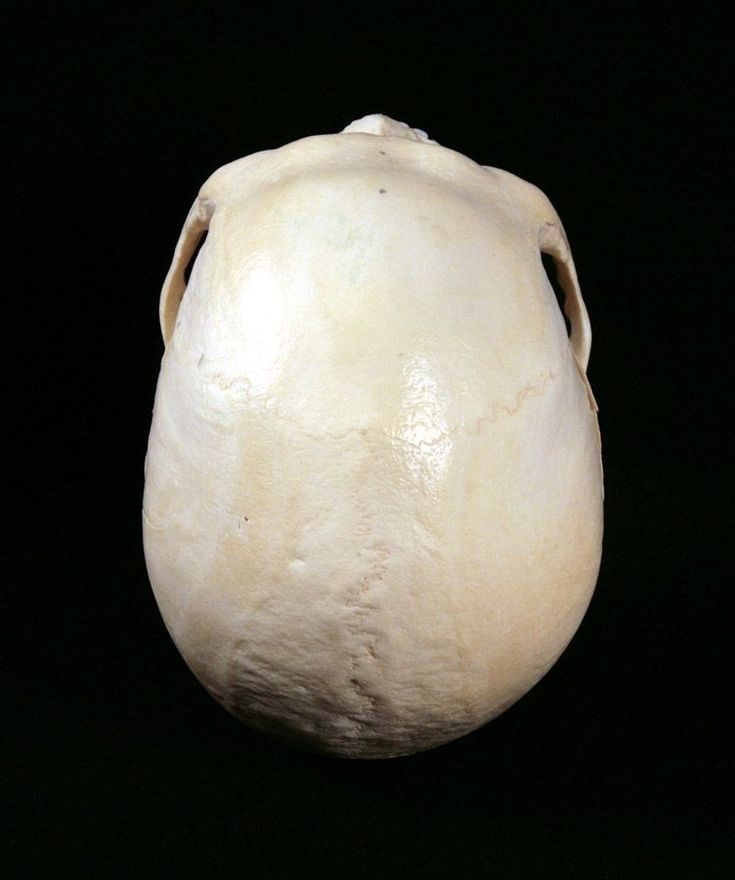
Brain contusion
This type of injury is characterized by focal symptoms. An absolute sign of a bruise of any degree is a fracture of the base and calvaria or the presence of impurities in the cerebrospinal fluid.
Brain contusion may be accompanied by mild or severe anisocoria. Severe anisocoria cannot be confused with Horner's syndrome - it manifests itself in the form of miosis, enophthalmos or ptosis, which is sometimes regarded as mydriasis on the opposite side. These forms of pupillary disorders must be distinguished, since Horner's syndrome is caused by damage to the synaptic plexus, in particular, the stellate ganglion. An increasingly pronounced pupil dilation in some cases indicates direct compression of the optic nerve. This should cause concern, since intracranial hematoma may compress the homolateral hemisphere. Mild contusion: symptoms are characterized by reflex asymmetry.
For a moderate contusion, more pronounced focal symptoms of CNS damage are characteristic - hemiplegia or hemiparesis, aphasia, hypoesthesia, damage to the cranial nerves (trigeminal, auditory, facial, oculomotor). In the acute period, the symptoms resemble cerebral ones, but after the restoration of consciousness, the first ones are more expressive.
In the acute period, the symptoms resemble cerebral ones, but after the restoration of consciousness, the first ones are more expressive.
Severe contusion includes trauma to the base of the brain, mediobasal regions, diencephalic region. This condition can be fatal. It is characterized by a long-term soporous-coma state, especially with a primary lesion of the brain stem, often accompanied by a disorder of vital functions, gross neurological disorders - both cerebral and local, profound disorders of metabolism, blood flow, etc. If intracranial pressure rises, congestive optic discs are present. After coming out of a coma, patients remain in a state of stupor or stupor for a long time, disorientation is noted.
Diagnosis
Diagnosis includes a series of examinations of the patient's brain disease. In particular, they include lumbar puncture to study pressure, transparency and composition of cerebrospinal fluid, angiography of cerebral vessels, encephalography. Angiography allows you to determine the topic and nature of the damage.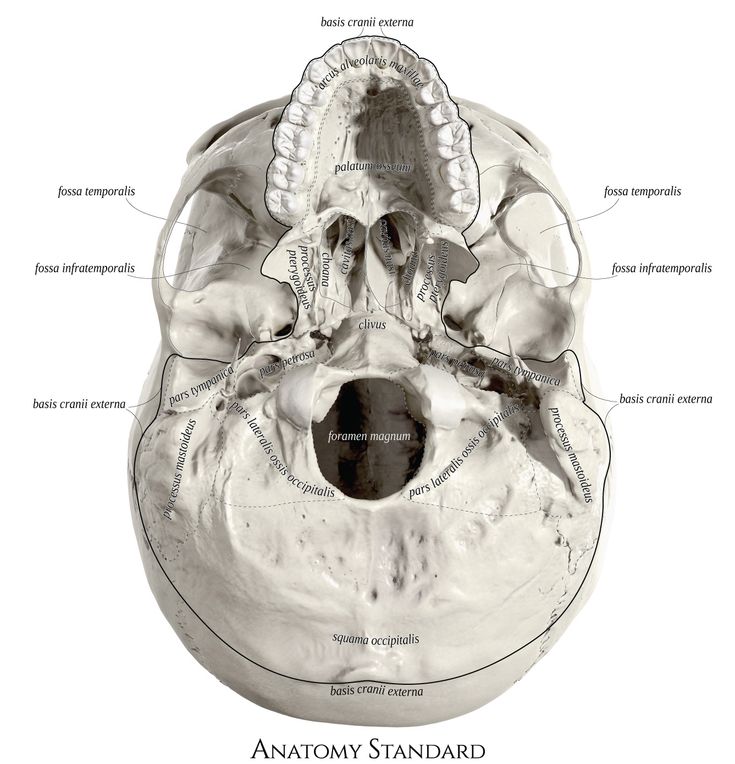 Trial trepanation of the skull is widespread. Such a study allows you to get the most accurate information about the injury and the cranial cavity.
Trial trepanation of the skull is widespread. Such a study allows you to get the most accurate information about the injury and the cranial cavity.
You can deliver the patient to the clinic using the "Honey Taxi" service.
Treatment
Treatment of traumatic brain injury involves a set of measures. Upon admission of a patient with a severe skull injury, a number of resuscitation measures are carried out - they restore cardiopulmonary activity, brain activity. With a closed injury, accompanied by a depressed fracture of the cranial vault, surgical treatment of the wound is performed. It consists in the removal of bone fragments, the imposition of a blind suture on soft tissues. At the same time, if the patient feels satisfactory, primary cranioplasty can be performed. If the patient is in serious condition, the procedure is postponed.
In case of open head injuries, surgical treatment of the wound is performed - excision of soft tissues, removal of bone fragments, blood clots and brain detritus, suturing.