Legs hurting in early pregnancy
Aching, Painful, Or Heavy Legs During Pregnancy
Having aching legs during pregnancy is the icing on the cake of all of your physical ailments. But contrary to cake, heavy or aching legs are not something to be desired. While things like morning sickness and fatigue can be expected, when leg pain hits, it might catch you off guard.
To help make your leg troubles a little more bearable, we’ll give you some basic information and help you identify the signs, causes, and treatments for your aching and heavy legs.
Blood Circulation And Heavy Or Aching Legs During Pregnancy
Pregnancy is a period during which the risk of circulatory disruptions becomes particularly high. These disruptions are the consequence of the related increase in body weight and hormonal changes, as seen below:
- As early as the first trimester, the increase in hormones creates circumstances in which the blood in the veins can easily stagnate, weakening vein walls and the firmness of blood vessels.
Estrogen levels can lead to inflammation (edema), and progesterone modifies the vein walls and vessel dilation.
- Throughout pregnancy, the increased volume of the uterus leads to increased pressure on the main vein responsible for returning blood to the heart.
- Finally, an increase in blood weight and volume (of 20% to 30%) contributes to increased pressure on the leg veins, which is doubled or tripled. The valves are separated further from each other by distension of the veins and no longer play their role of impeding blood return.
Blood circulation in the leg veins can be considerably disrupted. The symptoms vary significantly from woman to woman and pregnancy to pregnancy, ranging from simple discomfort to disabling pain.
After delivery, these impairments most often go away on their own within a few weeks.
The Role Of Veins And Vascular Insufficiency
In their normal state, arteries supply the body’s tissues and organs with essential substances for their healthy functioning, such as oxygen. Veins, on the other hand, return blood to the heart.
Veins, on the other hand, return blood to the heart.
Blood pressure and the firmness of vein walls allow blood to flow from the lower to the upper portion of the legs. This blood flow through the veins and back up to the heart is called venous return.
Valves, acting as small flaps, are positioned every 2 to 5 centimeters (0.8 to 2 inches) in the veins. These valves ensure that blood always flows in the same direction without ever “falling” back down the other way.
The calf muscles and compression of the instep also play a role in blood flow, particularly when walking.
Contributing Factors
Several factors can increase the risk of vascular insufficiency during pregnancy:
- Heredity: If your mom has had circulatory issues, you run a higher risk of experiencing them yourself.
- Working in a standing position and shuffling. Prolonged sitting can also disrupt venous return.
- A sedentary lifestyle and lack of physical exercise.
- Excess body weight prior to pregnancy, or significant weight gain during pregnancy.
- Previous pregnancies: The risk of venous insufficiency increases with the number of previous pregnancies carried to term — 23 percent for the first pregnancy and 31 percent for the fourth.
Healthy Habits
To avoid circulatory impairments during pregnancy, prevention is essential. If you need to, try to lose weight before getting pregnant and then limit your weight gain during pregnancy.
Here are some other healthy habits to help you avoid vascular insufficiency:
- Take walks or do light exercise, which boosts blood flow
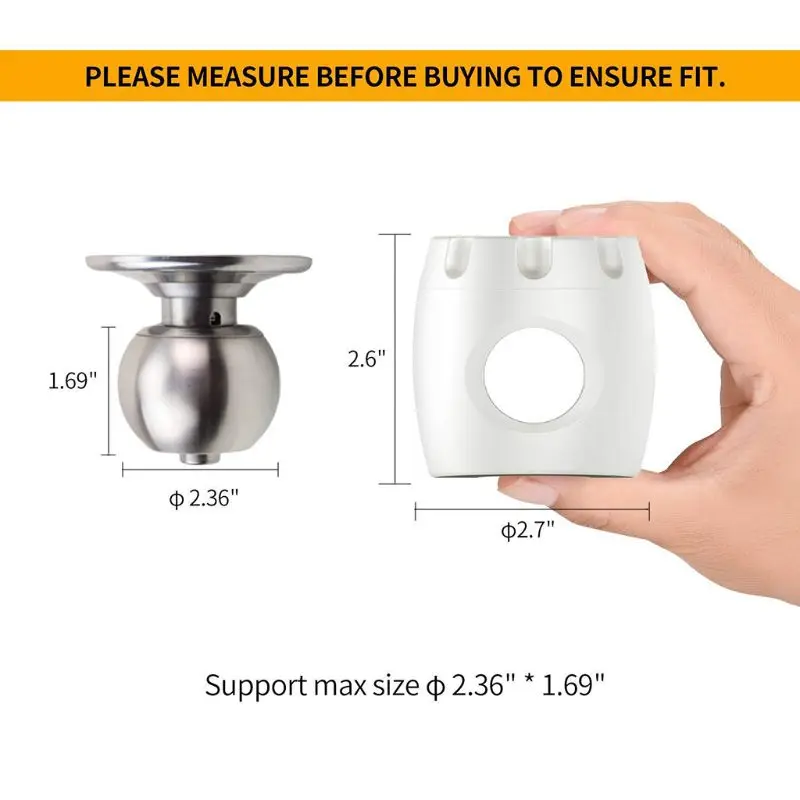
- Wear shoes with a small heel that is neither too high nor too flat (3 to 4 cm or 1 to 1.5 inches)
- Avoid tight-fitting clothes and constricting socks
- If you suffer from any plantar arch problems, wear corrective insoles
- In certain cases, wearing compression stockings and taking venotonics may be recommended during pregnancy, starting in the second month
If you experience the sensation of heavy legs despite these measures, try some of these tips to help ease the discomfort:
- Raise your feet from the foot of your bed
- At the end of each shower, spray cold water over your legs in an upward motion from the ankles to the thighs
- Avoid sources of heat (prolonged exposure to the sun, high-temperature baths, underfloor heating, etc.
 )
) - Massage your legs every day, from the ankles to the knees, using a specific treatment cream to increase blood return and stimulate blood flow
Signs Of Heavy Or Aching Legs
Aching or heavy legs first appear as a sensation of discomfort, fatigue, and heaviness in the legs. These sensations can be the first sign of an actual circulation impairment alongside other characteristics, such as having pain:
- In the interior and posterior area of the calf that radiates up the leg toward the inside of the knee
- Most often felt towards the end of the day
- If you remain standing for a long time or if you are in contact with heat (summer temperatures, hot baths, hot-wax treatments, etc.)
- Increase as the pregnancy progresses
- Relieved by cold temperatures, winter climates, rest, elevation of the legs, and walking
- Accompanied by cramps at night, restlessness of the legs (painful discomfort that requires that one move one’s legs for relief), inflammation (edema of the ankles), varicosities, and even varicose veins
If you are experiencing any of these symptoms, talk about it with your doctor at your next visit. Your doctor may be able to prescribe a suitable treatment for you.
Your doctor may be able to prescribe a suitable treatment for you.
Causes Of Aching Or Heavy Legs
Like most expecting moms, you’re probably wondering what’s causing your aching or heavy legs. The sensation of heavy or aching legs is related to a loss of firmness and elasticity of the vein walls, which causes a slowing of blood circulation in the veins. Because of this, the veins dilate and blood pressure increases.
Valves — the small flaps that normally keep blood from flowing back down the leg veins — have difficulty maintaining this pressure and progressively become deficient.
Resistance to leaks weakens and blood stagnates in the lower portion of the veins, which further impairs vein walls. A vicious cycle takes hold.
On top of this, other factors could be causing your aching legs, such as:
- Nerve pressure: When your uterus expands, it puts pressure on certain nerves, which can trigger spasms and cause pain in your legs.
- Dehydration: If your body doesn’t get the right amount of hydration during your pregnancy — and it needs a lot! — it can really suffer.
 Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route!
Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route! - Increase in your weight: Your legs are carrying around more weight than they’re used to. They’re having to work a little harder each day, so at the end of the day, they’re tired just like you.
- Swelling: Swelling is no stranger to pregnancy, especially in the heat. When your ankles and feet start to swell in the heat, as we’ve mentioned above, circulation gets restricted. This is when your legs start to ache and get heavy. (Note: If you notice consistent swelling in your legs and feet, or your leg starts to feel warm, reach out to your obstetrician right away.)
- Changes in your posture as your baby grows: Throughout stages of your pregnancy, your baby has taken different positions inside your uterus. This can take a toll on your body, especially your back.
 Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them.
Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them. - Fluid retention: Your growing uterus puts pressure on the veins that carry blood back from your lower body, which partially blocks blood flow. As a result, fluid remains in your legs and feet.
- Joint laxity: As we’ve discussed, when you’re carrying the extra weight from your precious baby, it’s a lot for your legs — but it’s also a lot for your joints. Your joints can easily become stressed from the added pressure. Your joints may seem a little loose and you might even waddle when you walk!
At-Home Treatment
Most often, your leg aches can be relieved at home. That’s something to shout about because we know leg aches can really be a Debby Downer as you wrap up your day!
Here are a few ideas to relieve your leg aches and heavy legs at the end of the day:
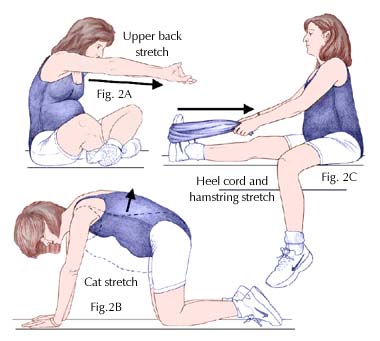
- Stretch your calf muscles by flexing and releasing each foot a few times
- Take short walks throughout the day to boost blood flow
- Avoid standing or sitting with your legs crossed for long periods
- Take a warm bath before bed (After getting out of a relaxing bath, don’t forget to apply Stretch Marks Oil to help limit the appearance of stretch marks! It leaves your skin restored, refreshed, and noticeably smoother.
 )
) - Massage your legs throughout the day and especially before bed (Try using our Body Firming Gel to give your legs a little massage. It hydrates your skin, giving it a firmer look and overall feel.)
- Take a calcium supplement (with the go-ahead from your doctor)
- Drink a glass of milk before bed
- Prop your legs up on a pillow (make sure your legs are elevated above your heart)
- Wear compression leggings or socks
- Increase your potassium intake
Medical Treatment
If your legs are painful and you see no improvement after trying the recommended measures outlined in the previous section, do not hesitate to see a doctor. They can prescribe suitable treatment for your condition.
Various methods — from medicinal to physical to surgical — may be considered, depending on the severity of your circulatory impairments:
- Compression via pantyhose, stockings, or socks is the basic treatment for anyone experiencing venous insufficiency.
 Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement.
Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement. - Venotonics have anti-inflammatory properties, stimulating muscle tone and protecting the elasticity of the vein walls. They must be taken for an extended period of time in order to be effective.
- Kinesitherapy and exercises to build up the leg muscle also have a role to play. Walking, swimming and biking are the best types of activity. Spa treatments, massages, and manual lymphatic drainage can also provide valuable relief.
- If varicose veins developed during your pregnancy and are still present after delivery, vein sclerotherapy or surgery may be considered. These techniques can be performed under local anesthesia, requiring neither an epidural nor general anesthesia, and the patient can go home the same day as treatment, or the following day.

A Comfortable Pregnancy
Aching and heavy legs can be caused by a variety of factors, as we listed above. Although these unpleasant sensations usually disappear on their own after delivery, they should not be taken lightly.
Heavy legs can turn into vascular pathologies that can sometimes be disabling. Monitor your heavy legs closely and give them the appropriate care from the very first signs to limit the risk of complications.
But keep in mind that most often, it’s not a cause for concern or harmful to your baby. Use at-home treatments to ease your leg aches and heavy legs. You may have to try a few before you find what works for you.
And while you’re at it, continue taking care of yourself during your pregnancy by treating your skin. Using the right products that have been clinically proven to effectively help expecting mothers, like our Stretch Marks Cream, will make for one comfortable pregnancy!
Leg cramps during pregnancy | Pregnancy Birth and Baby
Leg cramps during pregnancy | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Leg pain can sometimes be a sign of a blood clot. If pain in your leg doesn’t go away, or if your leg is red, warm or swollen, see your doctor immediately.
If pain in your leg doesn’t go away, or if your leg is red, warm or swollen, see your doctor immediately.
Key facts
- Up to 3 in 10 people who are pregnant get leg cramps.
- Cramps are most common in your calf muscles.
- Cramps commonly happen at night in late pregnancy.
- To prevent leg cramps, try stretching your leg muscles before you go to bed and drink plenty of water.
- To ease a cramp, pull your toes up towards your ankle, rub the muscle, walk around or apply a heat pack.
What are leg cramps?
Leg cramps (pains) affect up to 3 in 10 people who are pregnant. They usually occur in your calf muscles, but can also occur in your thighs or feet. A cramp is a sign that your muscles are contracting very tightly when they shouldn’t be. This happens when acid builds up in your muscles.
Cramps usually happen at night. They are more common in your second and third trimesters.
Leg cramps are not the same as pelvic cramps.
What causes leg cramps during pregnancy?
There are many reasons suggested for cramps while you’re pregnant, such as changes to your metabolism, having a vitamin deficiency, being too active or not being active enough. However, nobody really knows why they occur in pregnancy.
How can I get rid of cramps?
To ease a leg cramp, you can try:
- stretching the muscle by pulling your toes hard up towards the front of your ankle
- rubbing the muscle firmly
- walking around
- a heat pack
If you have a partner, you could ask them to help.
If your muscles are still sore after the cramp has gone, you can take paracetamol for pain relief.
How can I prevent leg cramps?
Things you can try that might help prevent cramps include:
- stretching your calf muscles before you go to bed
- drinking plenty of water
- having a warm bath before you go to bed
- eating a balanced diet
- avoiding stretching your leg while pointing your toes
Magnesium, calcium, vitamin B and vitamin C have been suggested as a treatment for cramps. It’s not clear whether any of these supplements work, but people often try magnesium and calcium. If you’re interested in trying supplements, talk to your doctor or midwife about whether they might be suitable for you.
It’s not clear whether any of these supplements work, but people often try magnesium and calcium. If you’re interested in trying supplements, talk to your doctor or midwife about whether they might be suitable for you.
When should I talk to my doctor or midwife about cramps?
If leg cramps are bothering you, talk to your doctor or midwife.
Leg pain can sometimes be a sign of a blood clot. If pain in your leg doesn’t go away, or if your leg is red, warm or swollen, see your doctor immediately.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Therapeutic Guidelines (Muscle cramps, including leg cramps in pregnant women), NSW Government (Having a baby), Queensland Health (6 weird things that may happen to your body during pregnancy), King Edward Memorial Hospital (Minor Symptoms or Disorders in Pregnancy King Edward Memorial Hospital Clinical Guidelines: Obstetrics & Midwifery), Queensland Health (VTE in pregnancy (a blood clot in the vein)), NPS (Magnesium, a treatment for leg cramps?), Royal Women’s Hospital (Common concerns in early pregnancy)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- Swelling during pregnancy
- Varicose veins
- Common discomforts during pregnancy
Need more information?
Pregnancy at week 28
You are now in the third trimester and you'll probably be feeling many of the common discomforts of pregnancy, like a sore back, swelling, heartburn or cramps.
Read more on Pregnancy, Birth & Baby website
Common discomforts during pregnancy
Your body has a great deal to do during pregnancy. Sometimes the changes taking place will cause irritation or discomfort, and on occasions they may seem quite alarming.
Read more on Pregnancy, Birth & Baby website
Am I having a miscarriage? - Miscarriage Australia
We describe the common signs or symptoms of miscarriage.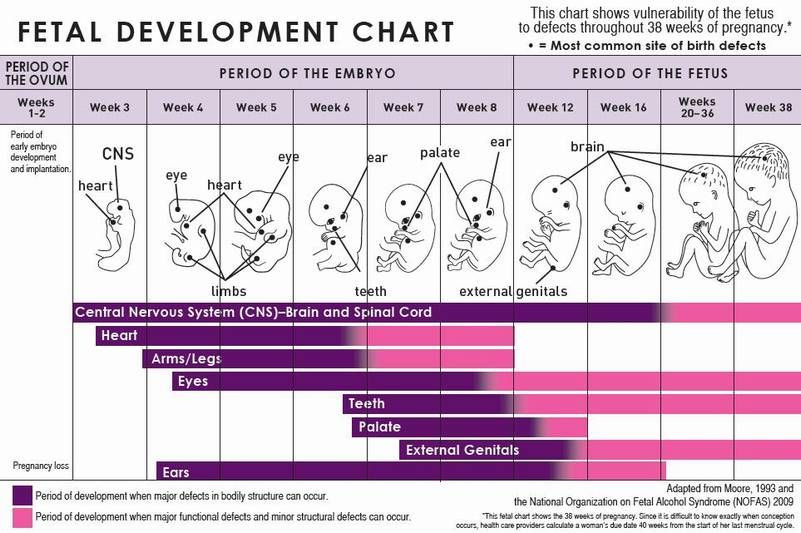 Sometimes there are symptoms, but sometimes there aren't.
Sometimes there are symptoms, but sometimes there aren't.
Read more on Miscarriage Australia website
Having a miscarriage - Miscarriage Australia
Here you can find information about the common symptoms of miscarriage, what happens during a miscarriage, and where to go for help.
Read more on Miscarriage Australia website
Pregnancy health problems & complications | Raising Children Network
Many pregnancy health problems are mild, but always call your doctor if you’re worried about symptoms. A healthy lifestyle can help you avoid health problems.
Read more on raisingchildren.net.au website
Pregnancy - signs and symptoms - Better Health Channel
All women experience pregnancy differently, and you will experience different symptoms at different stages of your pregnancy.
Read more on Better Health Channel website
Sleep during pregnancy
Sleep can become a problem when you're pregnant. Here are some tips to help you get as much sleep as possible so you’re ready for your baby's arrival.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 33
Your baby's brain and nervous system are now fully developed, and the baby is continuing to gain weight. You'll probably also be feeling sore and tired.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 25
As you are approaching the end of the second trimester, you might be starting to feel a bit uncomfortable as your baby continues to grow.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 26
Your baby is starting to put on fat and muscle and as your baby grows, your centre of gravity will shift, so you might find that you are starting to walk differently and maybe even a little clumsy.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Pulling legs during early pregnancy - Articles - The official website of Intex
The situation in which pulling the leg during pregnancy in the later stages is rarely surprising. At this time, the legs have a large load that overloads the muscles of the legs, and the pregnant uterus compresses the deep veins of the legs, provoking blood stasis and associated discomfort in the legs. In this article, we will analyze why the legs are pulled during early pregnancy , and we will explain how to alleviate the condition if the leg is pulled at the beginning of pregnancy.
At this time, the legs have a large load that overloads the muscles of the legs, and the pregnant uterus compresses the deep veins of the legs, provoking blood stasis and associated discomfort in the legs. In this article, we will analyze why the legs are pulled during early pregnancy , and we will explain how to alleviate the condition if the leg is pulled at the beginning of pregnancy.
Why does leg pull during early pregnancy?
Discomfort, swelling and feeling of heaviness in the legs in the first weeks of pregnancy most often accompany early toxicosis of pregnant women, which includes all pathological changes in the body of a pregnant woman. Early toxicosis manifests itself in feelings of nausea, skin irritations, muscle cramps, asthma and other painful manifestations. Most often, early toxicosis of pregnant women provokes diseases of the gastrointestinal tract, thyroid gland and liver, bacterial and viral infections. To exclude manifestations of early toxicosis, in the first trimester of pregnancy, at the first signs of discomfort in the legs, you need see a doctor . The first manifestations of varicose veins are the second common reason why the left leg aches at the beginning of pregnancy. During pregnancy, the body increases the synthesis of the hormone progesterone, the main task of which is to relax the smooth muscle of the uterus. Since, at the same time, the smooth muscle of the walls of the venous vessels relaxes, the vessels begin to stretch . The valves of the veins weakened by progesterone cannot withstand the pressure of the blood. Under the influence of gravity, blood begins to seep through the valves of the veins and return back to the superficial veins of the legs. Pressure increases inside the veins, and the liquid part of the blood begins to be forced out through the walls of the vessels into the muscles and subcutaneous tissue. Because of this, pregnant women, even in the early stages of pregnancy, may experience varicose edema.
How to relieve nagging pain in the legs in the first trimester of pregnancy?
First of all, you need to see a doctor observing pregnancy as soon as possible. The doctor will be able to exclude early toxicosis and concomitant diseases. If necessary, the doctor will refer to a phlebologist , a specialist dealing with problems of the circulatory system. If the phlebologist detects signs of incipient varicose veins, it is important to start treatment as early as possible. If therapy is neglected, varicose veins can persist even after childbirth. Treatment of varicose veins in the first trimester of pregnancy is reduced to physiotherapy, massage and wearing compression garments. Use of drugs in pregnant women is not allowed, because it can harm the baby. In the first trimester of pregnancy, compression stockings or tights "Intex" for pregnant women of the 1st compression class help relieve pain in the legs. Elastic products create a distributed pressure on the legs in the range of 18-22 mm Hg. This pressure is enough to reduce the negative effect of progesterone on the veins: relieve discomfort in the legs, reduce swelling and prevent varicose veins in the legs .
The doctor will be able to exclude early toxicosis and concomitant diseases. If necessary, the doctor will refer to a phlebologist , a specialist dealing with problems of the circulatory system. If the phlebologist detects signs of incipient varicose veins, it is important to start treatment as early as possible. If therapy is neglected, varicose veins can persist even after childbirth. Treatment of varicose veins in the first trimester of pregnancy is reduced to physiotherapy, massage and wearing compression garments. Use of drugs in pregnant women is not allowed, because it can harm the baby. In the first trimester of pregnancy, compression stockings or tights "Intex" for pregnant women of the 1st compression class help relieve pain in the legs. Elastic products create a distributed pressure on the legs in the range of 18-22 mm Hg. This pressure is enough to reduce the negative effect of progesterone on the veins: relieve discomfort in the legs, reduce swelling and prevent varicose veins in the legs .
Pregnancy and your feet article on the site of the Preobrazhenskaya Clinic
Pregnancy causes many different changes in a woman's body. Many women during pregnancy present the same complaints.
One of these complaints, which is practically not taken into account, is the complaint of pain in the legs.
Due to the natural weight gain during pregnancy, the body's center of gravity shifts forward. This causes a redistribution of the load on the limbs and an increase in pressure in the knee joints and feet.
Pregnant women have two main problems, they are excessive pronation of the foot and swelling of the legs.
These changes can cause pain in the heels, arch, or metatarsus. Many women experience leg cramps and varicose veins. Therefore, all pregnant women need to have the necessary information about their health and, in particular, about the function of the legs, so that the nine-month pregnancy period is more comfortable for them.
Reason:
Excessive stress on the feet and swelling of the legs are the most common problems during pregnancy.
Overload occurs because the arch of the foot flattens under the weight. This can cause congestion and inflammation of the plantar fascia that runs from the heel to the toes.
Excessive stress on the feet can make walking painful due to increased stress on the legs, calves and spine.
Edema, or swelling of the legs, usually occurs in the second half of pregnancy.
Edema is caused by obstruction of the outflow of blood due to the pressure of the enlarging uterus on the veins of the lower extremities. In a woman's body, the total volume of fluid in the body remains the same as before pregnancy, but its distribution changes. Swollen legs become bluish.
During pregnancy, an extra volume of fluid accumulates in the body, which contributes to an increase in edema.
If the hands or face swell, the pregnant woman should immediately consult a doctor.
Treatment
There are effective ways to deal with deformity and swelling of the feet during pregnancy.
Foot deformities can be treated with ready-made orthotics . These orthotics must have sufficient arch and hindfoot support. It remains important to choose the right shoes. A pregnant woman should choose comfortable shoes with proper foot support and cushioning.
Foot deformity should be treated not only to relieve pain, but also to avoid complications such as plantar fasciitis, heel spurs, tibialis posterior inflammation or toe deformities.
Pregnant women can be given the following advice:
- Raise your legs as often as possible. If you have to stay in a sitting position for a long time, set up a small stool and place your feet on it.
- Wear rational footwear. Too narrow and short shoes impede blood flow in the lower extremities.
- Measure the circumference of the lower leg and thigh, as well as the size of the foot, several times during pregnancy. These numbers are subject to change.
- Wear seamless socks that don't restrict blood flow.