Can pregnancy cause fever blisters
Cold sores in pregnancy | Pregnancy Birth and Baby
Cold sores in pregnancy | Pregnancy Birth and Baby beginning of content6-minute read
Listen
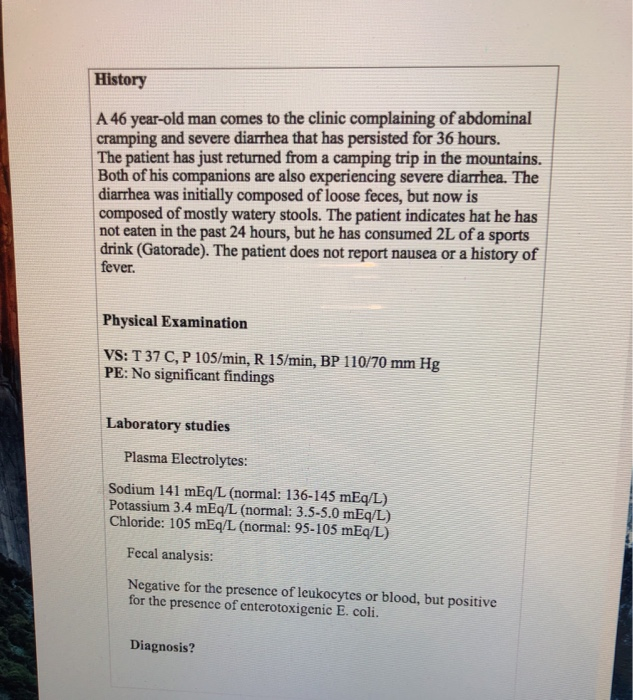
What is HSV?
If you or your partner has the virus that causes cold sores or genital herpes, you might be worried about what could happen when you're pregnant or have a new baby. Here's what you need to know about herpes simplex virus (HSV), and how to protect your baby from infection.
The herpes simplex virus is a very common virus carried by most people. Sometimes it causes cold sores or genital herpes.
Cold sores are blisters that form on the lips, around the mouth and nose. Genital herpes is blisters or sores around the genitals or anus. The blisters may form a crust after about 3 days. The sores go away by themselves within 2 weeks.
There are two main types of HSV:
- HSV-1 causes mostly cold sores on the face and lips, and sometimes on the genitals
- HSV-2 causes mostly genital herpes
Both viruses are transferred though contact of the skin, saliva or genitals, and the viruses stay in the body for life. The viruses do not always cause symptoms, so you can carry the virus without knowing it.
HSV-1 is very common, with about 8 in 10 Australians carrying it in their bloodstream. But only 1 in 3 people with the virus has ever had a cold sore. HSV-2 is less common.
It is common for women who have had cold sores in the past to experience an outbreak while pregnant.
What happens if I get cold sores or genital herpes during pregnancy?
Having the HSV virus does not affect your chance of becoming pregnant.
It is quite common for women to have a cold sore during their pregnancy, even if they haven’t had one for a long time. Cold sores should not affect your unborn baby. But they are infectious, so it’s a good idea to treat them.
But they are infectious, so it’s a good idea to treat them.
Genital herpes should not affect the baby if you have your first outbreak or it comes back in the first 34 weeks. But it can be transferred to your baby during the birth, especially if it’s your first outbreak.
If you've ever had a cold sore or genital herpes and you become pregnant, or you develop these conditions during pregnancy, it's important to tell your doctor or midwife about it. Together you can make a plan for managing herpes during pregnancy and birth.
How is HSV treated during pregnancy or breastfeeding?
You can treat cold sores and genital herpes with:
- aciclovir cream, available from a pharmacist without prescription
- aciclovir or valaciclovir tablets, for which you need a prescription
These 'antiviral' drugs are known to be safe for pregnant and breastfeeding women and are effective most of the time.
Famciclovir tablets are not recommended to take during pregnancy.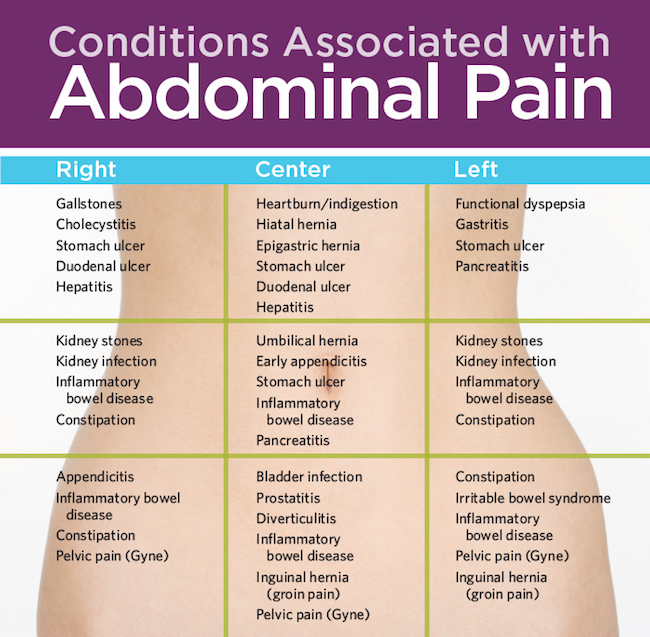 Speak to your doctor if the cold sore is severe.
Speak to your doctor if the cold sore is severe.
How is genital herpes treated during pregnancy?
You should take acyclovir or valaciclovir tablets, as above.
If it's your first outbreak of genital herpes, your baby may be more at risk because you haven't had time to develop immune protection against the virus, which also helps protect the baby.
Some women experiencing an outbreak of genital herpes might be advised to have a caesarean. This would prevent the herpes virus passing from mother to baby during a vaginal birth. But most women in Australia with genital herpes do give birth safely to healthy babies vaginally.
It's often recommended that women who have ever had genital herpes take antiviral tablets prior to the birth, even if the herpes isn't active at the time.
Talk to your doctor or midwife about the best course of action for your situation.
How do I protect my baby from herpes?
Herpes can cause serious problems in a baby, such as infections to the eyes and throat, brain damage and even death.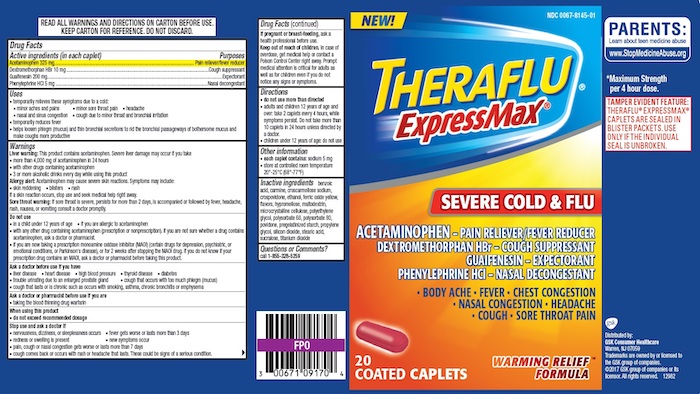
A newborn baby can catch HSV-1 and HSV-2 from being kissed or touched by someone with cold sores, or during childbirth.
Fortunately, most babies born to women who carry the virus are not affected. But if you or your partner has a cold sore or genital herpes, talk to your doctor about keeping it under control during the pregnancy and after the birth. It is also important to treat these conditions aggressively while you are breastfeeding.
It's important to maintain strict hygiene habits when caring for a new baby if you, or anyone in close contact with the baby, have cold sores.
If you have cold sores, you should:
- cover cold sores when you're around the baby
- avoid kissing your baby until the sores are completely healed
- avoid touching the cold sores then touching your baby
- wash your hands thoroughly before touching your baby
What if I have a cold sore while breastfeeding?
If you have cold sores, it is safe to breastfeed your baby as long as the cold sores are not on the breast or nipple.
If they are, it may be wise to breastfeed from the unaffected nipple only until the lesions have cleared up. You would express and dispose of breastmilk from the affected nipple. Breastmilk itself doesn't contain the herpes virus but it can be contaminated through the skin lesions.
Talk to your doctor or midwife as soon as you notice any cold sores on your breast or nipple.
What happens if my baby gets herpes?
It is very important that herpes in a newborn is recognised and treated by a doctor in hospital immediately. Signs of herpes in a newborn include:
- blisters on the skin
- fever
- irritability
- tiredness
- lack of appetite
If you think your baby might have the herpes virus, don't wait to see if they get better — seek medical help. Tell medical staff if you or your partner carry the herpes virus.
Resource and Support
If you are worried about your baby, see a doctor or midwife, or take them to the hospital.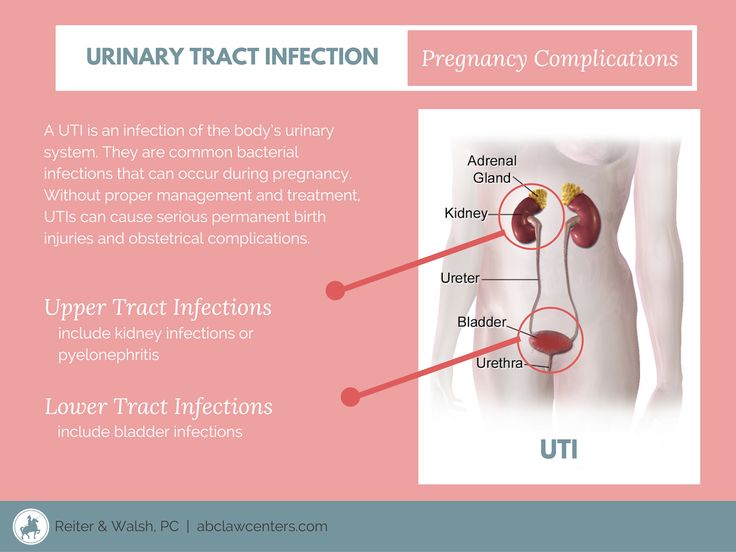
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
If you're not sure what to do or want more information, you call Pregnancy Birth Baby on 1800 882 436 to speak with a maternal child nurse.
Sources:
Family Planning NSW (Genital herpes), The Royal Woman’s Hospital (Genital herpes), Mothersafe (Cold sores in pregnancy and breastfeeding), Queensland Government Health (Genital Herpes and Pregnancy), SA Health (Cold sores (herpes simplex type 1) - including symptoms, treatment and prevention), Safer Care Victoria (Herpes simplex virus in neonates)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Need more information?
Genital Herpes (HSV) | Body Talk
Genital herpes is a common STI caused by the Herpes Simplex Virus (HSV). Find out all the facts about Genital Herpes here.
Find out all the facts about Genital Herpes here.
Read more on Body Talk website
Cold sores - Better Health Channel
Cold sores are blisters around the mouth and nose, caused by the herpes simplex virus.
Read more on Better Health Channel website
Cold sores overview - MyDr.com.au
A cold sore is a skin infection that is caused by the herpes simplex virus (HSV). Cold sores usually occur on or around the lips or nose and are very common. They have nothing to do with colds.
Read more on myDr website
Cold sores: self-care - MyDr.com.au
Cold sores are caused by the herpes simplex type 1 virus. Most people carry this virus in their bodies.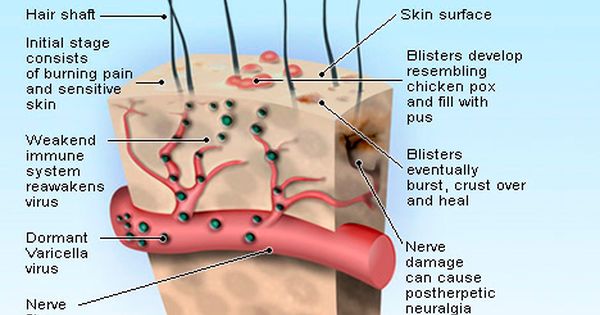 Find out what products are available for cold sores.
Find out what products are available for cold sores.
Read more on myDr website
Cold sores | SA Health
Herpes simplex virus type 1 (HSV1) causes cold sores on the face or lips - it is spread by skin or mucous membrane contact with infected saliva
Read more on SA Health website
Cold sore infections - MyDr.com.au
Find the answers to common questions about cold sores, irritating blisters which are caused by the herpes simplex type 1 virus and can be triggered by stress, fatigue or exposure to sunlight.
Read more on myDr website
Cold sores: children & teens | Raising Children Network
Cold sores are quite common in older children and teenagers. Cold sores usually clear up by themselves, but see your GP if you’re concerned.
Cold sores usually clear up by themselves, but see your GP if you’re concerned.
Read more on raisingchildren.net.au website
Genital Herpes and Pregnancy
If you are pregnant and you get genital herpes, it is important to tell your midwife or obstetrician.
Read more on Queensland Health website
Genital herpes
Genital herpes is a sexually transmitted infection (STI) which shows as blisters or sores on the genitals. This is caused by the herpes simplex virus (HSV).
Read more on WA Health website
Genital herpes: what is it? - MyDr.com.au
Genital herpes is a viral infection characterised by outbreaks of blisters and sores around your genital area.
Read more on myDr website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.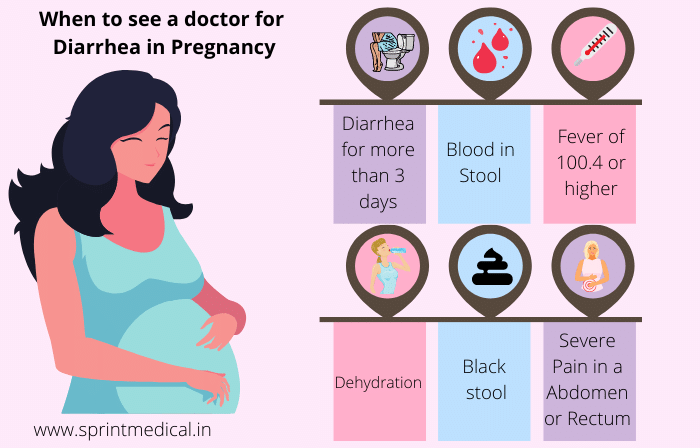
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Affect on Baby and Safe Treatments
If you’ve ever had cold sores — those annoying, painful, tiny, fluid-filled blisters that usually form around your mouth and on your lips — you know how inconvenient they can be.
But also if you’ve ever had cold sores (and therefore already have the virus that causes them), did you know they can recur, especially when you’re under stress or are undergoing hormonal fluctuations?
Stress and hormonal changes. That sounds an awful lot like pregnancy.
Cold sores in pregnancy aren’t unheard of, and they don’t usually have any impact on your growing baby. So first, let out a deep sigh of relief. Next, read on — because there are still important things to know about cold sores if you’re expecting.
Cold sores are caused by a virus — the herpes simplex virus (HSV). Of the two types of HSV, cold sores are generally caused by HSV-1, whereas genital herpes is usually a result of exposure to HSV-2. There have been a few instances where HSV-1 sores have been found in the genitals and vice versa.
Once you’ve had a cold sore (oral herpes), the virus remains in your system for life — it’s just not active unless you have a current outbreak.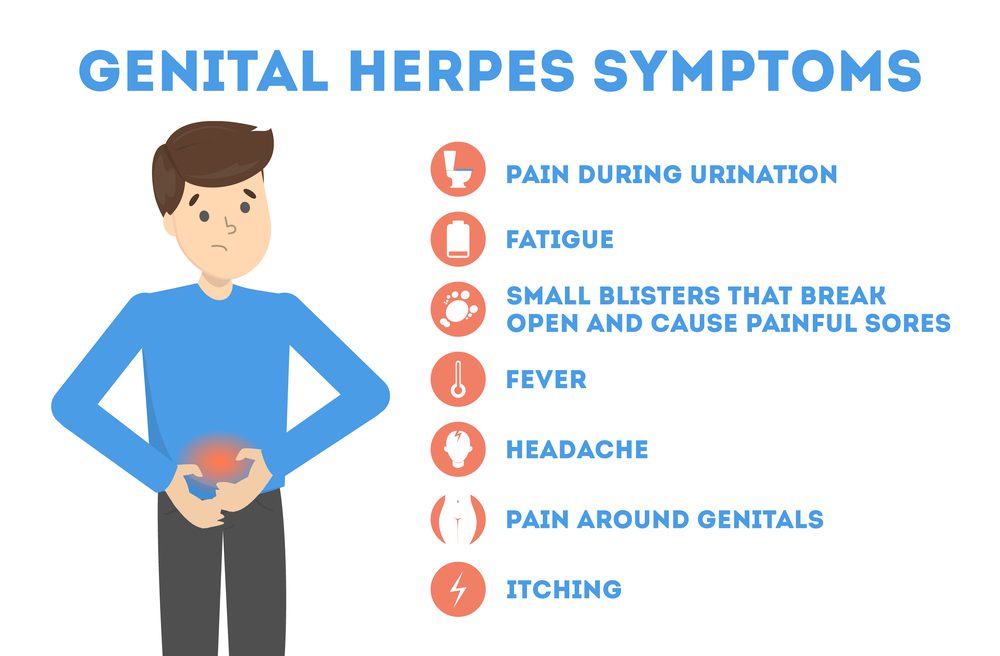
But when we say that stress and hormones can cause the virus to reactivate, it’s important to know that stress and hormones don’t cause the virus in the first place.
If you’ve never had HSV, you can only get it through contact with someone who has. When it comes to a first-time cold sore infection, this can happen via activities like:
- kissing
- sharing food or utensils
- using someone else’s ChapStick or lip gloss
- oral sex
Here’s the really good news: If you already have the virus that causes cold sores, and you have an outbreak of oral herpes during pregnancy, it’s most likely not going to have any impact on your growing baby.
Cold sores are a localized infection, usually around the mouth area. They don’t typically cross the placenta and reach your baby.
The highest risk scenario is if you get HSV for the first time during your third trimester of pregnancy.
When you get the virus for the first time, your body hasn’t developed any protective antibodies to it yet. And while HSV-1 is usually associated with oral herpes, it can cause a genital herpes outbreak, which can be dangerous to your baby — especially as they pass through the birth canal.
And while HSV-1 is usually associated with oral herpes, it can cause a genital herpes outbreak, which can be dangerous to your baby — especially as they pass through the birth canal.
Birth-acquired herpes is serious. However, it’s a concern with genital rather than oral herpes. That being said, because the same virus can cause both, it’s important to talk to your OB about any cold sores during pregnancy.
The most common treatment for cold sores is docosanol (Abreva), an over-the-counter topical cream. But the Food and Drug Administration hasn’t evaluated it for safety in pregnancy.
While some research has determined that it’s “likely safe” during pregnancy, at least one pharmaceutical company that manufactures the drug warns against using it unless it’s definitely needed — which really means you need to check with your doctor. There may be other treatments you should try first.
If you’ve had herpes in the past, your doctor may recommend antivirals — like acyclovir or valacyclovir — starting at week 36 and continuing until delivery of your baby, even if you don’t have a current outbreak of lesions around the genital area. This helps prevent reactivation and spread of the virus to the genital area.
This helps prevent reactivation and spread of the virus to the genital area.
This precaution is because you shouldn’t expose your baby to herpes in the vaginal area during delivery.
Alternatively, your doctor may suggest a cesarean delivery, which avoids the birth canal altogether — something that’s especially important if you have a current outbreak of genital herpes.
Cold sores are highly contagious, despite the fact that they won’t affect your baby in the womb. If you have them after your baby is born, avoid kissing those adorable little cheeks or touching any sores and then touching your newborn without first washing your hands with soap.
In the extremely rare event that you have cold sores on either breast, avoid breastfeeding from that breast while you’re still contagious.
Your cold sores are contagious until they crust over, at which point they’ll start to heal.
If you do pass a cold sore infection on to your newborn, it’s known as neonatal herpes.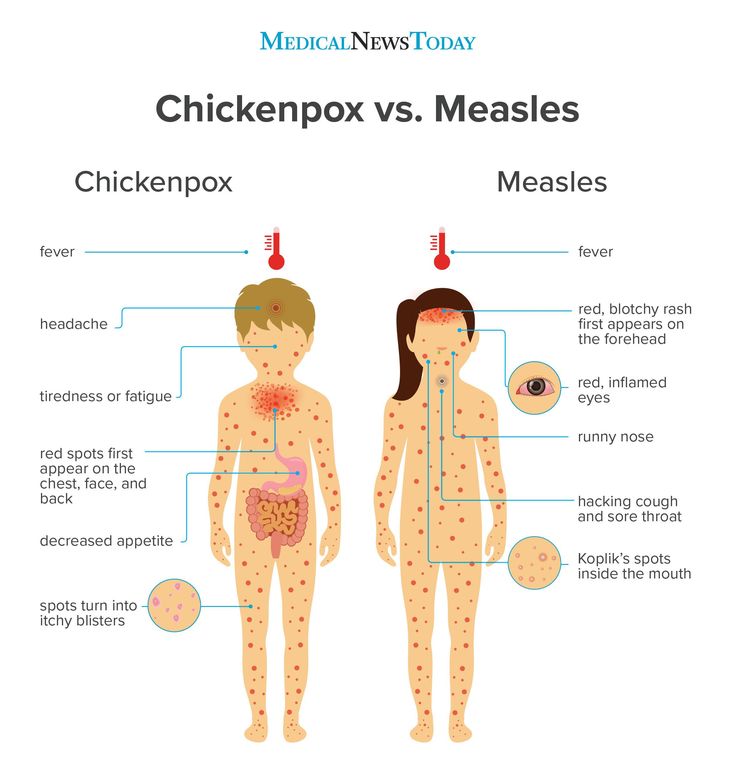 While not as serious as the birth-acquired version, it can still cause serious complications in a baby who hasn’t yet developed a robust immune system.
While not as serious as the birth-acquired version, it can still cause serious complications in a baby who hasn’t yet developed a robust immune system.
The cold sore on your mouth is likely to be more of an annoyance to you than a serious risk to your developing baby, particularly in your first two trimesters of pregnancy and especially if you’ve had one before. But you should still let your OB know about it.
The virus that causes cold sores — usually HSV-1 — can also cause genital herpes, which is more of a risk to your pregnancy and growing little one.
If you have an outbreak in your third trimester — or if you acquire the virus for the first time in your third trimester — your doctor may want you to follow certain treatment or precautionary guidelines, like antivirals or a cesarean delivery.
Fever during pregnancy: causes, risks, treatments
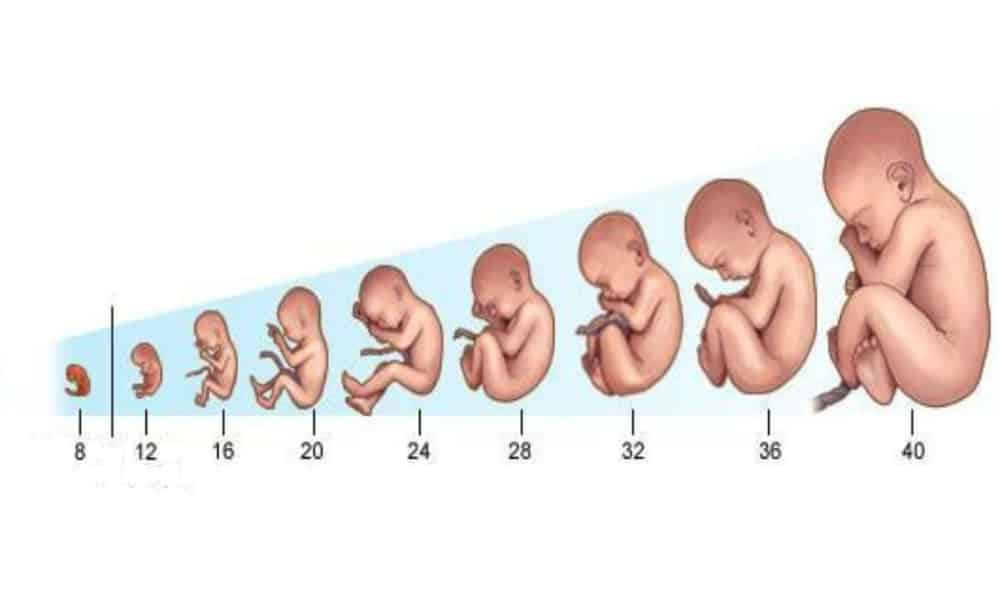
During pregnancy, the level of hormones in a woman's body increases, as a result of which the temperature rises slightly in the early stages, and this is normal. High body temperature during pregnancy can be dangerous complications, and in the early stages it increases the risk of developing neural tube defects in a child.
High body temperature during pregnancy can be dangerous complications, and in the early stages it increases the risk of developing neural tube defects in a child.
Natalya Chebakova
legion-media
Various viral and bacterial infections, from which even a pregnant woman is not immune, can cause body temperature to rise above 38 degrees. This condition is considered dangerous. Studies have proven the association of fever with the risk of developing anomalies in a child.
Contents of the article
Do not self-medicate! In our articles, we collect the latest scientific data and the opinions of authoritative health experts. But remember: only a doctor can diagnose and prescribe treatment.
What can cause fever during pregnancy?
In fact, during pregnancy, a woman is more susceptible to all diseases due to a suppressed immune system. Fever can be caused by a bacterial or viral infection, such as a cold or flu, food poisoning, or a urinary tract infection.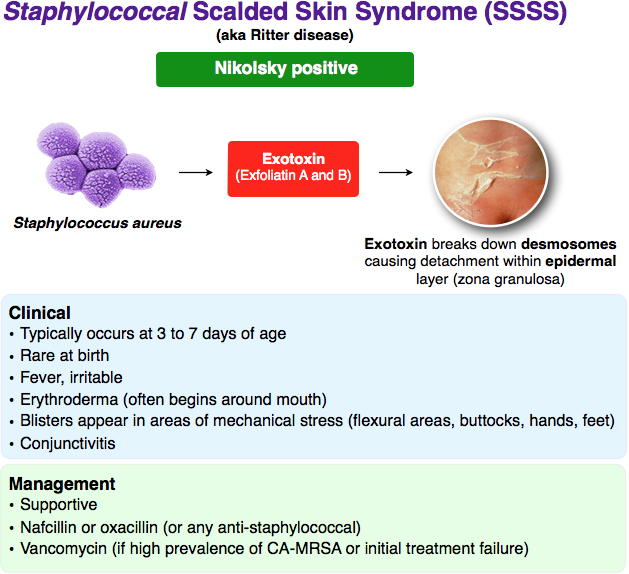
A temperature above 38 degrees Celsius is considered a fever.
Can fever during pregnancy harm the baby?
25% of pregnant women have a fever at least once during pregnancy, and the vast majority of them have healthy children.
If the temperature does not rise above 38.3 degrees and does not last long, it is the least of concern. High body temperature that persists for a long time can have serious consequences for the child.
This aspect is still being studied. Previously conducted studies have shown that the fever during pregnancy can cause:
- Nervous tube defects (DNT)
- miscarriage
- Congenital heart defects
- Defects in the abdominal wall
- Penettlete
However, not all studies confirm the negative impact of fever on child development. Thus, in Denmark, observations of more than 77,000 pregnant women and their children born between 1996 to 2002 showed no association between maternal fever during pregnancy and the risk of birth defects.
Is high fever dangerous in early pregnancy?
Fever in very early pregnancy can be more dangerous as fetal structures are just forming. The risk of developing neural tube defects in a child, such as anencephaly, encephalocele, craniocerebral hernia and spinal hernia, increases. This is because the neural tube that forms the baby's spinal cord develops during the first six weeks of pregnancy.
Once the neural tube closes at the beginning of the sixth week, the baby is no longer susceptible to fever-induced NTDs.
Experts say you can reduce your risk of developing neural tube defects, even when you have a fever, by taking prenatal vitamins with at least 400 mcg of folic acid.
Folic acid is a scientifically developed water-soluble analogue of vitamin B9, essential for the proper development of the human circulatory and immune systems.
Fetal NTD screening is done in the second trimester of pregnancy using blood tests and ultrasound.
Can fever be a sign of pregnancy?
Many women experience a slight increase in body temperature along with an increase in progesterone levels in early pregnancy.
The temperature rise is a small, normal spike that stays well below the fever threshold of 38 degrees. Fever cannot be a sign of pregnancy.
Does fever during pregnancy increase the risk of autism, ADHD or developmental delay?
Scientists have not yet fully studied the answer to this question. However, there have been some studies linking fever during pregnancy with an increased risk of autism spectrum disorder (ASD), attention deficit hyperactivity disorder (ADHD), and developmental delay.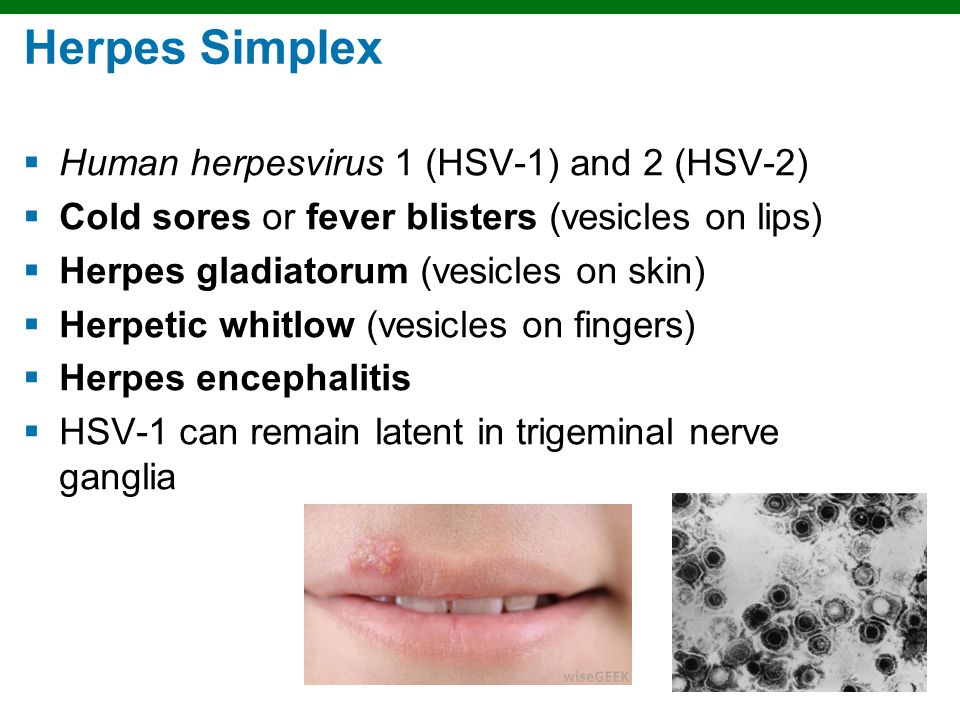
Important to know! Retrospective studies, when subjects are asked to report symptoms in the distant past, appear to be less reliable than prospective studies that collect information in real time.
1. One retrospective study analyzed data from more than 500 children with ASD and more than 160 children with ADHD and found an association between maternal fever and both conditions.
It was also found that the risk of ASD was lower among mothers who took medication to reduce fever.
2. A prospective Norwegian study of more than 114,000 children found an association between intrauterine fever and an increased risk of ASD, especially (but not exclusively) in the second trimester.
These investigators concluded that the risk increased markedly with the frequency of fever (three or more episodes), especially after 12 weeks of gestation.
Data from the same study showed that maternal fever in early pregnancy may be a risk factor for ADHD and especially inattention problems.
3. A large, multicenter, retrospective study of children with ASD and developmental delay born in the United States between 2003 and 2006 showed that women who had an infection accompanied by fever in the second trimester of pregnancy were more likely to have children with ASD.
4. A prospective study of the motor development of children whose mothers had a fever during pregnancy found a significant association between maternal fever during pregnancy and dyspraxia in 7-year-old children (clumsiness, poor coordination, clumsiness of hand movements, inaccuracy of articulation, difficulties in writing).
Although the results of these studies may be worrying, the absolute risk of developing these disorders is quite low.
Medicines for fever during pregnancy
In order to reduce the temperature during pregnancy, you need to see a doctor. Only a doctor can prescribe a drug that is safe for the expectant mother and child.
In addition, the drug should be taken in strictly recommended dosages. Taking too much medication can be harmful to a woman's liver and her baby's liver.
Other treatments for fever during pregnancy
In addition to taking medication, there are some things that can help bring down the temperature:
- Lie down in a comfortable position with a cool, damp towel over your forehead.
- Take a warm bath. It is important to avoid using cold water, as it can cause chills, leading to a temperature spike. Warm water will do - the fever will subside when the water evaporates from the skin.
Rubbing with rubbing alcohol or vinegar does not bring down the fever, but can lead to too rapid cooling, and later to a higher temperature jump.
- Drink plenty of fluids to stay hydrated.
- Ventilate the room where a pregnant woman is.
When should I call a doctor?
Call a doctor or an ambulance if:
- fever lasts more than two days during pregnancy;
- chest pain or shortness of breath;
- cough lasts more than 7 days;
- have diarrhea or bloody diarrhea;
- back pain, abdominal pain, nausea or vomiting.
How to protect yourself from infection?
Preventive measures such as frequent handwashing, avoiding contact with people who are sick, and flu and COVID-19 vaccinations can help minimize the chance of contracting infections that cause fever.
To avoid intestinal infections, it is important to thoroughly wash food before eating, and do not eat undercooked meat and eggs.
youtube
Click and watch
Did you have a fever during pregnancy?
Threatening conditions during pregnancy ⚕️ Article Med-Atlant
Pregnancy is a wonderful and amazing period in a woman's life. With its physiological course, the pregnant woman has the opportunity to enjoy every day of nine wonderful months. However, pregnancy does not always proceed normally, sometimes pregnant women experience conditions that are threatening for her and for her child. Every pregnant woman should be aware of these symptoms and, if they occur, seek immediate medical attention.
Bloody discharge. Normally there should be no bloody discharge from the vagina at all. Threatening are any: from minor spotting to heavy bleeding. They may indicate the onset of a spontaneous miscarriage or premature birth, premature detachment of the placenta (a condition that threatens both the fetus and the woman and may require an immediate caesarean section).
Change in the nature of discharge. In addition to bloody, watery discharge from the vagina up to 37 weeks of gestation is also dangerous, which may indicate premature discharge of amniotic fluid. In this case, hospitalization is necessary for a complex of diagnostic and therapeutic measures. Only a doctor with the help of special tests can distinguish amniotic fluid from urine, mucous plug or inflammatory discharge. The latter are also dangerous and require treatment, in particular, greenish, yellowish, cheese-like, odorous discharge, accompanied by discomfort, itching. They may indicate the presence of an infection that threatens the infection of the fetus or premature birth.
High fever in pregnant women. In the normal course of pregnancy, due to changes in the hormonal background of a woman, the temperature may rise to 37.3-37.5 ° C, but not always. If the temperature rises above 37.5 ° C, medical attention should be sought. Given the Covid 19 pandemic, any increase in temperature and deterioration in general condition should be reported to your OB/GYN and family doctor. A high temperature may also indicate other diseases dangerous for pregnant women, such as influenza, respiratory viral infections, inflammation of the kidneys, ENT organs, appendicitis, etc.
A high temperature may also indicate other diseases dangerous for pregnant women, such as influenza, respiratory viral infections, inflammation of the kidneys, ENT organs, appendicitis, etc.
Change in the nature of fetal movements. As you know, during the first pregnancy, a woman begins to feel the movement of the baby from 20-21 weeks, with a second pregnancy - even from 16-17 weeks. Until the 28th week, it is important to have the movements of the child during the day, later the woman should feel more than 10 sets of movements per day and count them. To do this, every pregnant woman must complete the so-called "fetal movement test", which allows her to suspect and respond in time to the deterioration of the baby's condition. If there are doubts about the movements, if the woman has less than 10 sets of movements within 12 hours, or, conversely, the movements are too active and painful, it is necessary to consult a doctor.
Dangerous during pregnancy are also excessive vomiting, diarrhea, pain when urinating, sudden significant swelling of the hands, feet, face, headache, especially in combination with high blood pressure, blurred vision, convulsive twitching of the limbs.