Leg cramp during early pregnancy
Leg cramps during pregnancy | Pregnancy Birth and Baby
Leg cramps during pregnancy | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Leg pain can sometimes be a sign of a blood clot. If pain in your leg doesn’t go away, or if your leg is red, warm or swollen, see your doctor immediately.
Key facts
- Up to 3 in 10 people who are pregnant get leg cramps.
- Cramps are most common in your calf muscles.
- Cramps commonly happen at night in late pregnancy.
- To prevent leg cramps, try stretching your leg muscles before you go to bed and drink plenty of water.
- To ease a cramp, pull your toes up towards your ankle, rub the muscle, walk around or apply a heat pack.
What are leg cramps?
Leg cramps (pains) affect up to 3 in 10 people who are pregnant. They usually occur in your calf muscles, but can also occur in your thighs or feet. A cramp is a sign that your muscles are contracting very tightly when they shouldn’t be. This happens when acid builds up in your muscles.
Cramps usually happen at night. They are more common in your second and third trimesters.
Leg cramps are not the same as pelvic cramps.
What causes leg cramps during pregnancy?
There are many reasons suggested for cramps while you’re pregnant, such as changes to your metabolism, having a vitamin deficiency, being too active or not being active enough. However, nobody really knows why they occur in pregnancy.
How can I get rid of cramps?
To ease a leg cramp, you can try:
- stretching the muscle by pulling your toes hard up towards the front of your ankle
- rubbing the muscle firmly
- walking around
- a heat pack
If you have a partner, you could ask them to help.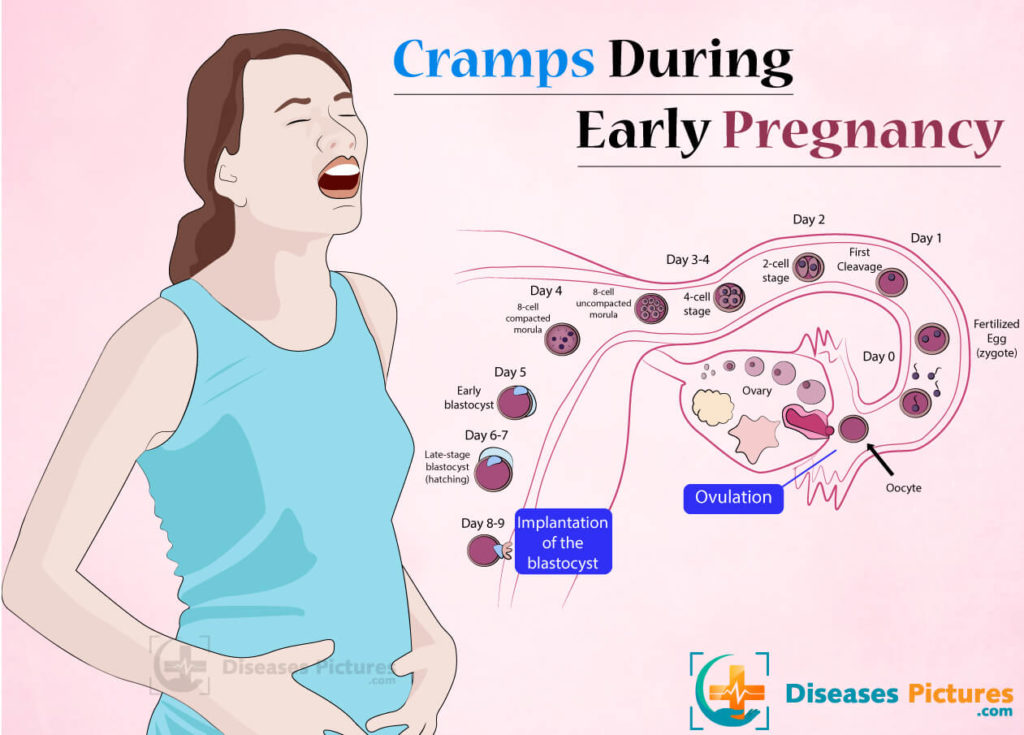
If your muscles are still sore after the cramp has gone, you can take paracetamol for pain relief.
How can I prevent leg cramps?
Things you can try that might help prevent cramps include:
- stretching your calf muscles before you go to bed
- drinking plenty of water
- having a warm bath before you go to bed
- eating a balanced diet
- avoiding stretching your leg while pointing your toes
Magnesium, calcium, vitamin B and vitamin C have been suggested as a treatment for cramps. It’s not clear whether any of these supplements work, but people often try magnesium and calcium. If you’re interested in trying supplements, talk to your doctor or midwife about whether they might be suitable for you.
When should I talk to my doctor or midwife about cramps?
If leg cramps are bothering you, talk to your doctor or midwife.
Leg pain can sometimes be a sign of a blood clot. If pain in your leg doesn’t go away, or if your leg is red, warm or swollen, see your doctor immediately.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Therapeutic Guidelines (Muscle cramps, including leg cramps in pregnant women), NSW Government (Having a baby), Queensland Health (6 weird things that may happen to your body during pregnancy), King Edward Memorial Hospital (Minor Symptoms or Disorders in Pregnancy King Edward Memorial Hospital Clinical Guidelines: Obstetrics & Midwifery), Queensland Health (VTE in pregnancy (a blood clot in the vein)), NPS (Magnesium, a treatment for leg cramps?), Royal Women’s Hospital (Common concerns in early pregnancy)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- Common discomforts during pregnancy
- Swelling during pregnancy
- Varicose veins
Need more information?
Pregnancy at week 28
You are now in the third trimester and you'll probably be feeling many of the common discomforts of pregnancy, like a sore back, swelling, heartburn or cramps.
Read more on Pregnancy, Birth & Baby website
Common discomforts during pregnancy
Your body has a great deal to do during pregnancy. Sometimes the changes taking place will cause irritation or discomfort, and on occasions they may seem quite alarming.
Read more on Pregnancy, Birth & Baby website
Pregnancy health problems & complications | Raising Children Network
Many pregnancy health problems are mild, but always call your doctor if you’re worried about symptoms. A healthy lifestyle can help you avoid health problems.
A healthy lifestyle can help you avoid health problems.
Read more on raisingchildren.net.au website
Pregnancy - signs and symptoms - Better Health Channel
All women experience pregnancy differently, and you will experience different symptoms at different stages of your pregnancy.
Read more on Better Health Channel website
Sleep during pregnancy
Sleep can become a problem when you're pregnant. Here are some tips to help you get as much sleep as possible so you’re ready for your baby's arrival.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 33
Your baby's brain and nervous system are now fully developed, and the baby is continuing to gain weight. You'll probably also be feeling sore and tired.
You'll probably also be feeling sore and tired.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 25
As you are approaching the end of the second trimester, you might be starting to feel a bit uncomfortable as your baby continues to grow.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 26
Your baby is starting to put on fat and muscle and as your baby grows, your centre of gravity will shift, so you might find that you are starting to walk differently and maybe even a little clumsy.
Read more on Pregnancy, Birth & Baby website
Pregnancy and your mental health - Better Health Channel
Finding out you are pregnant can be a very exciting time. But it can also make you feel uncomfortable, unwell, worried and make you wonder how you are going to cope. And it doesn’t stop when the baby arrives. Some mums find it easy to adjust to life with a new baby. But others don’t!
But it can also make you feel uncomfortable, unwell, worried and make you wonder how you are going to cope. And it doesn’t stop when the baby arrives. Some mums find it easy to adjust to life with a new baby. But others don’t!
Read more on Better Health Channel website
Sclerotherapy - MyDr.com.au
Sclerotherapy is a treatment that involves the injection of a chemical solution into blood vessels, usually spider veins or superficial (surface) varicose veins on the legs.
Read more on myDr website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Treatment, Home Remedies, and Prevention
Pregnancy isn’t always a cakewalk. Sure, we hear how beautiful it is (and it is!), but your first months may have been filled with morning sickness and heartburn. And just when you think you’re out of the woods, leg cramps come along.
Leg cramps are a common pregnancy symptom that usually occurs in the second and third trimester. In fact, nearly half of all pregnant women report muscle spasms by the third trimester.
In fact, nearly half of all pregnant women report muscle spasms by the third trimester.
You may experience these cramps mainly at night — just when you’d like to get the sleep you’re probably craving — and feel tightness in your calf, foot, or both areas. Some women also experience them after sitting in one position for an extended amount of time.
It may not be possible to entirely prevent leg cramps. But preventative and relief measures like stretching, staying active, and drinking plenty of water may help ease your symptoms and get your mind back on the true joys of pregnancy.
Let’s start by talking about what causes these cramps, because knowledge is power when it comes to getting relief.
Circulation changes
During pregnancy, circulation slows — this is totally normal and not a reason to worry. It’s due in part to overactive hormones. (You probably know by now that hormones are gifts that keep on giving for the whole 40 weeks — and beyond.)
During later trimesters, your body also experiences an increase in blood volume, which also contributes to slow circulation. This can lead to swelling and cramping in your legs.
This can lead to swelling and cramping in your legs.
Tips for improving circulation while pregnant
- Try sleeping on your left side.
- Elevate your legs as often as possible — literally, find the time to put your feet up and relax if you can.
- At night, place a pillow under or between your legs.
- During the day, stand up and walk around every hour or two — especially if you have a job that keeps you at a desk all day.
Dehydration
Quick check: Are you drinking enough water?
During pregnancy, you’re ideally drinking 8 to 12 cups of water each day. Watch out for symptoms of dehydration, like dark yellow pee (it should be clear or nearly clear).
Dehydration can cause and worsen leg cramps. If you’re experiencing them, try upping your daily water intake.
Weight gain
The pressure from your growing baby can take a toll on your nerves and blood vessels, including the ones that go to your legs. This is why you’re more likely to experience leg cramps as your pregnancy progresses, especially in the third trimester.
Gaining a healthy amount of weight and staying active during your pregnancy may help prevent leg cramps. Talk to your healthcare provider if you’re concerned.
Fatigue
It’s the norm to feel tired during pregnancy — you’re growing a tiny human! — and this is especially true as you gain more weight in the second and third trimester. As your muscles get fatigued from the added pressure, too, it can lead to leg cramps.
Try drinking plenty of water, going for a walk during the day, and stretching before bed to prevent leg cramps due to muscle fatigue.
Calcium or magnesium deficiency
Having too little calcium or magnesium in your diet may contribute to leg cramps.
But if you already take a prenatal vitamin, you likely don’t need to take an additional supplement. A 2015 review of studies of 390 pregnant women found that taking magnesium or calcium supplements made little to no difference when it came to experiencing leg cramps.
If you’re concerned you aren’t getting enough of these nutrients, speak to your doctor. You’re probably getting labs done occasionally anyway, so it doesn’t hurt to have these levels checked.
You’re probably getting labs done occasionally anyway, so it doesn’t hurt to have these levels checked.
DVT blood clot
A deep vein thrombosis (DVT) blood clot can occur in the legs, thigh, or pelvis. Pregnant women are 5 to 10 times more likely to develop a DVT than non-pregnant women. While there’s no need to panic that you’ll get one — it’s pretty uncommon to start with — we can’t say enough that knowledge is power.
Bottom line: Keep moving. We’re not talking marathons here, but the best way to prevent DVT during pregnancy is to avoid hours at a time of inactivity.
If your job requires a lot of sitting, you could set a quiet alarm on your phone to go off every hour to remind you to get up and walk — perhaps to the water cooler to add to your water intake for the day! Two birds, one stone.
Also take extra care to get up during long flights. You may want to check with your doctor before flying while pregnant.
Symptoms of a blood clot are similar to leg cramps, but a DVT blood clot is a medical emergency. Seek medical care right away if you experience symptoms like:
Seek medical care right away if you experience symptoms like:
- a lot of pain in your legs when you’re standing or moving around
- severe swelling
- warm-to-the-touch skin near the affected area
Stretching before bed
Performing a calf stretch before getting into bed at night may help prevent or ease leg cramps. Follow these steps:
- Stand facing a wall, an arm’s length away.
- Place your hands on the wall in front of you.
- Step your right foot back. Keep your heels on the floor the whole time and bend your left knee while keeping your right leg straight. Keep your left knee bent as so you feel the stretch in your right calf muscle.
- Hold for up to 30 seconds. Switch legs, if needed.
Staying hydrated
Drinking plenty of water during pregnancy is important to prevent dehydration — and dehydration can also lead to those awful leg cramps.
Try to drink 8 to 12 cups of water each day during pregnancy.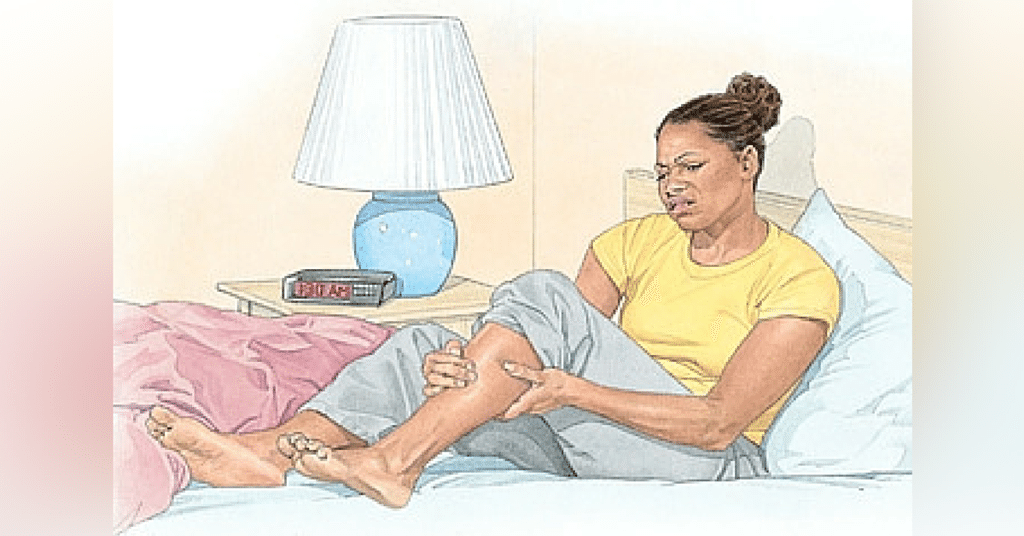 Easier said than done, sure — but super important for a lot of good reasons.
Easier said than done, sure — but super important for a lot of good reasons.
Applying heat
Try applying heat to your cramping muscle. It may help loosen up the cramp. No need to buy a fancy heating pad: You can also use a microwave-safe cloth bag (or a sock) filled with rice.
Massaging the area
When you get a leg cramp, performing a self-massage may help ease your pain. Use one hand to gently massage your calf or wherever your leg is cramping. Perform this self-massage for 30 seconds to a minute to ease your cramp.
You can also get a prenatal massage, which can be a positively divine experience. Look for an experienced therapist in your area who specializes in working with pregnant women.
Exercising
It’s a smart idea to stay active throughout your pregnancy, even though you don’t want to overdo it.
With your doctor’s OK, pregnancy-safe activities like prenatal yoga, walking, and swimming can benefit you and your baby-to-be.
Staying active can prevent excess weight gain, promote circulation, and yes — help prevent leg cramps. Always stretch and warm up before and after exercising so your muscles don’t cramp up afterward, though.
Always stretch and warm up before and after exercising so your muscles don’t cramp up afterward, though.
Avoiding inactivity
So, perhaps you don’t have the time or energy for a challenging hike or run. That is more than OK — you need to listen to your body and know your limits, especially during pregnancy.
But sitting for long periods of time can lead to leg and muscle cramps. To avoid this, make sure you stand up and walk around every hour or two. Set a timer on your phone or watch if you tend to forget to get up during the day.
Leg cramps are a common pregnancy symptom. (That doesn’t make having them any easier, but hopefully it turns down the stress dial a bit.)
If you’re concerned about your pain or they’re causing too much lost shut-eye, mention it at your next prenatal checkup.
Also call your doctor and let them know if your leg cramps are severe, persistent, or worsening. You may need supplements or medication.
Seek medical help immediately if you experience severe swelling in one or both legs, pain walking, or enlarged veins. These may be symptoms of a blood clot.
These may be symptoms of a blood clot.
The straight answer here is that there is no straight answer. (Great.)
Leg cramps are most common in the second and third trimester of pregnancy, not the first. But changing symptoms are a valid reason to wonder if you’re pregnant.
Some women do report aches and pains during the first trimester. This is likely due to your hormonal changes and your expanding uterus.
Leg cramps alone can’t tell you if you’re pregnant. If you suspect you’re pregnant or miss your period, take an at-home pregnancy test or see your doctor to confirm.
To prevent leg cramps, try the following:
- Drink between 8 and 12 cups of water per day.
- Stay active throughout your pregnancy.
- Stretch out your calf muscles.
- Wear comfortable shoes — leave the heels at home!
- Eat a balanced diet with calcium- and magnesium-rich foods like yogurt, leafy greens, whole grains, dried fruit, nuts, and seeds
Experiencing leg cramps during pregnancy isn’t pleasant. But it’s a common symptom, especially at night. Try our tips — we think they’ll help.
But it’s a common symptom, especially at night. Try our tips — we think they’ll help.
And as always, let your doctor know if you have any related worries. Never feel bad or self-conscious about phoning or emailing your clinic — helping you through a healthy pregnancy is the number one concern of OB doctors and nurses.
Interventions for leg cramps during pregnancy
What is the problem?
Leg cramps manifest themselves as sudden, intense involuntary contractions of the leg muscles. This is a common problem during pregnancy, especially in the third trimester. They are painful and can interfere with daily activities, disrupt sleep, and reduce quality of life. Various types of interventions are used to treat leg cramps during pregnancy, including medications, electrolytes (magnesium, calcium, sodium) and vitamins, as well as non-drug therapies such as muscle stretching.
Why is this important?
The aim of this review was to find out which treatment for leg cramps during pregnancy is effective and safe.
What evidence did we find?
In September 2019, we searched for evidence and identified eight randomized controlled trials in 576 women 14 to 36 weeks pregnant comparing magnesium, calcium, calcium with vitamin D or B vitamins versus placebo or no treatment, and compared vitamin C with calcium. All drugs were given as tablets to chew or swallow.
Magnesium supplements may reduce the incidence of leg cramps in women compared with placebo or no treatment, although studies have not been consistent. Different studies have assessed the effect of magnesium supplementation differently. Some studies have shown magnesium to help reduce the incidence of leg cramps, while others have shown little or no effect. Data on the effect of magnesium on pain reduction was also inconclusive, with only one study showing a reduction in pain intensity, while others showed no difference. Differences in the occurrence of side effects such as nausea and diarrhea were negligible or non-existent.
Differences in the occurrence of side effects such as nausea and diarrhea were negligible or non-existent.
Calcium did not always reduce the incidence of leg cramps in women after treatment compared to those who did not receive any treatment. It also found that the evidence was of very low quality, so we cannot be sure of the results.
More women who received B-vitamin supplements made a full recovery compared to those who received no treatment; however, these results were based on a small sample size and the study had design limitations.
Frequency of leg cramps did not differ between women receiving calcium and women receiving vitamin C. with placebo.
What does this mean?
The quality of the evidence was low to very low. This was mainly due to small study sample sizes and study design weaknesses. Four studies were well-conducted and presented their reports. The remaining four had flaws in their design: in several studies, women were not best assigned to different treatment groups, and in two studies, women knew whether they were receiving treatment or not. Adverse effects, such as the effect of treatment on complications of pregnancy, childbirth and child, were not reported. Several studies have focused primarily on serum calcium and magnesium levels. The frequency and intensity of seizures and duration of pain were not uniformly reported, and there was often no information on whether they were assessed during treatment, at the end of treatment, or after treatment was discontinued.
Adverse effects, such as the effect of treatment on complications of pregnancy, childbirth and child, were not reported. Several studies have focused primarily on serum calcium and magnesium levels. The frequency and intensity of seizures and duration of pain were not uniformly reported, and there was often no information on whether they were assessed during treatment, at the end of treatment, or after treatment was discontinued.
It is not clear from the evidence reviewed whether any oral interventions (magnesium, calcium, calcium with vitamin D, B vitamins, vitamin D, or vitamin C) are an effective and safe treatment for leg cramps during pregnancy. Supplements can have different effects depending on how women usually take them. None of the trials looked at forms of treatment such as muscle stretching, massage, relaxation, or heat therapy.
Translation notes:
Translation: Luzan Maria Alexandrovna. Editing: Yudina Ekaterina Viktorovna. Russian translation project coordination: Cochrane Russia - Cochrane Russia, Cochrane Geographic Group Associated to Cochrane Nordic. For questions related to this transfer, please contact us at: [email protected]
For questions related to this transfer, please contact us at: [email protected]
〚 Why do pregnant women have cramps at night and should I be worried about it? 〛|| Blog BABYSTART
March 13, 2020
Pregnancy is a natural state for a woman. However, her body at this time is subject to increased stress, which sometimes causes various ailments. These include leg cramps, which disturb the expectant mother, as a rule, during a night's sleep. Why they arise and whether it is worth sounding the alarm, let's look at this article.
Spasm - a sharp and painful spasm of a muscle (or a series of contractions). It comes suddenly and does not depend on the will of man. Everyone has experienced this phenomenon at least once in their life, but especially pregnant women experience convulsions. Leg cramps at night, usually in the calf muscle. A spasm can portend a feeling of heaviness or fullness in the leg.
This causes pain, the nature of which can be called aching. Localization of convulsions - in the place of the greatest rigidity of the muscle. It does not last long - as a rule, no more than two minutes, but the woman feels quite significant discomfort. After the experience of pain, she often cannot sleep.
Localization of convulsions - in the place of the greatest rigidity of the muscle. It does not last long - as a rule, no more than two minutes, but the woman feels quite significant discomfort. After the experience of pain, she often cannot sleep.
Why muscle contractions occur
During pregnancy, a number of factors can contribute to the occurrence of leg cramps at night:
- Slowing of blood circulation at night.
- Accumulation of lactic acid in the muscles during the day, which provokes cramps in the calves when they relax.
- Decreased hemoglobin. When there are few red blood cells in the body, muscle fibers do not receive enough oxygen, and, in addition to convulsions, a pregnant woman often experiences bouts of weakness and dizziness.
- Increased load on the lower limbs, which is often noted in the later stages. The problem is exacerbated by wearing tight, uncomfortable clothes and shoes with heels, prolonged stay on the feet due to the profession.

- Insufficient fluid intake in the body. This happens not only because a woman drinks little water. Overheating in the sun, drinking coffee, alcohol and nicotine can lead to dehydration. As a result, toxins settle in the muscles and can cause them to contract involuntarily.
- Excessive compression of the inferior vena cava by the growing uterus, which occurs if the expectant mother often sleeps on her back. The muscles of the legs suffer from oxygen starvation, to which they react with repeated convulsions.
- Deficiency of important vitamins and microelements, primarily potassium, calcium and magnesium, vitamin B6. At the same time, a pregnant woman has concomitant symptoms - brittle nails, hair loss, dental caries, problems with stools, chronic fatigue and depression.
- Varicose veins. This, unfortunately, is a frequent companion of pregnancy. Often, the disease first manifests itself or worsens precisely during the period of bearing a child. Cramps in the calf muscles in this case are caused by circulatory disorders.
- Changes in blood sugar levels. If a woman eats irregularly, and eats rarely and in large portions, then the concentration of glucose in the blood will constantly change dramatically, which is fraught with convulsions.
When you need to see a doctor immediately
Most often, leg cramps in pregnant women are a common occurrence and do not mean any pathology. However, there are cases when they indicate serious health problems, such as:
- Eclampsia. This is the most severe form of late pregnancy toxicosis. It is expressed by a dangerous increase in pressure, threatening the life of both the mother and the fetus. Convulsions in eclampsia are accompanied by numbness of the legs and their pronounced edema. With this condition, a woman needs emergency medical care.
- Deep vein thrombosis of the lower extremities. Circulatory failure and convulsions occur due to blockage of large blood vessels by a blood clot.
- Serious vitamin deficiency.