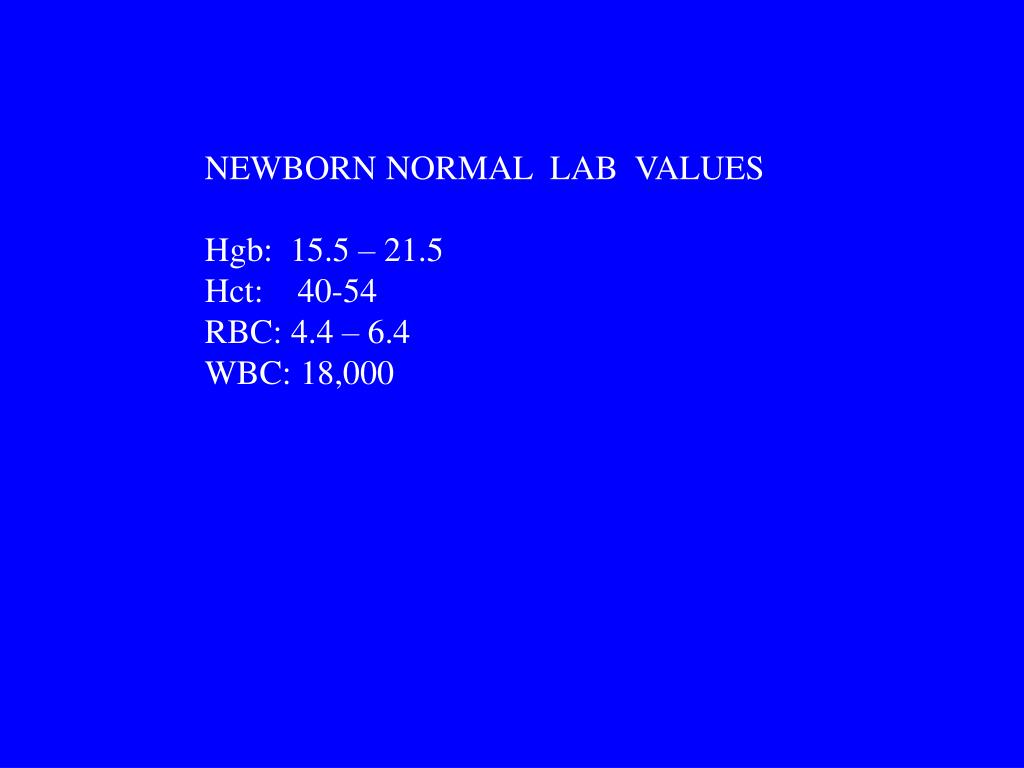
Lab values for newborn
Critical Values for Infants | Department of Pathology | School of Medicine
Laboratory values in the critical range will be reported by telephone immediately.
On inpatients, the laboratory will attempt to phone the physician first; however, if the physician listed as the ordering physician is incorrect or does not respond within 10 minutes, the patient’s nurse will be notified.
Results will be reported only to a physician or nurse unless the location of the patient is in the recovery room, operating room, or labor and delivery and a physician or nurse cannot come to the phone.
Critical value laboratory test results will be phoned immediately to non-UC Irvine Pathology Referral Services clients. These results can be released to a clinical laboratory scientist at the referral client location when the ordering physician is unavailable.
The urgency of the contact will be emphasized to the individual accepting the phoned report, as well as the importance of contacting the appropriate physician.
Inability to contact the requesting physician, clinic, or office after two attempts will be followed up with an attempt to reach the pathology resident on call, the clinical pathology attending on call, or the director of the specific laboratory section in which the laboratory results occurred.
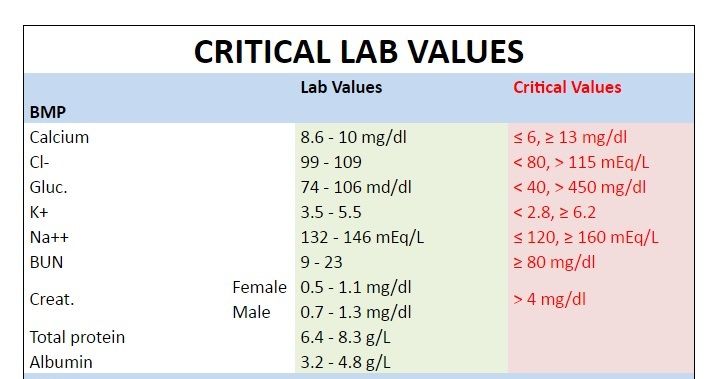
| Test | Critical Low Value | Critical High Value |
| Albumin | <2.0 g/dL | ----- |
| ALT (SGPT) | >100 IU/L | |
| Ammonia | >100 mcmol/L | |
| Ammonia Nitrogen (arterial) | ----- | >150 ug/dL |
| Bicarbonate | <14 mmol/L | >35 mmol/L |
| Bilirubin, direct | ----- | >1.5 mg/dL |
| Bilirubin, micro: | 1 day: >6 mg/dL 2 days:>10 mg/dL 5 days-12 mos: >15 mg/dL | |
| Bilirubin, Total | ----- | >15 mg/dL |
| Blood culture | ----- | Positive |
| Calcium, plasma | <6. 5 mg/dL 5 mg/dL | >12 mg/dL |
| Calcium, ionized | Birth to 1 month: >1 month to ≤12 months old: | >1 month to ≤12 months: >1.5 mmol/L |
| Carbon Dioxide (CO2) | <12 mEq/L | ----- |
| Chloride | <80 mEq/L | >117 mEq/L |
| COVID-19 (SARS-CoV-2) | ----- | Detected |
| Creatinine | ----- | >2.0 mg/dL |
| Creatine phosphokinase (CK) | ----- | >1,200 U/L |
| CSF, culture or Gram stain | ----- | Positive |
| ESR (Ophthalmology) TOPHT, TEYES, ZOPHT | ----- | >10 mm/hr |
| Fibrinogen | <100mg/dL | ----- |
| Gamma-Glutamyl Trans (GGT): | ----- | >300 U/L |
| Glucose (Blood) | <45 mg/dL | >250 mg/dL |
| Hemoglobin | <7.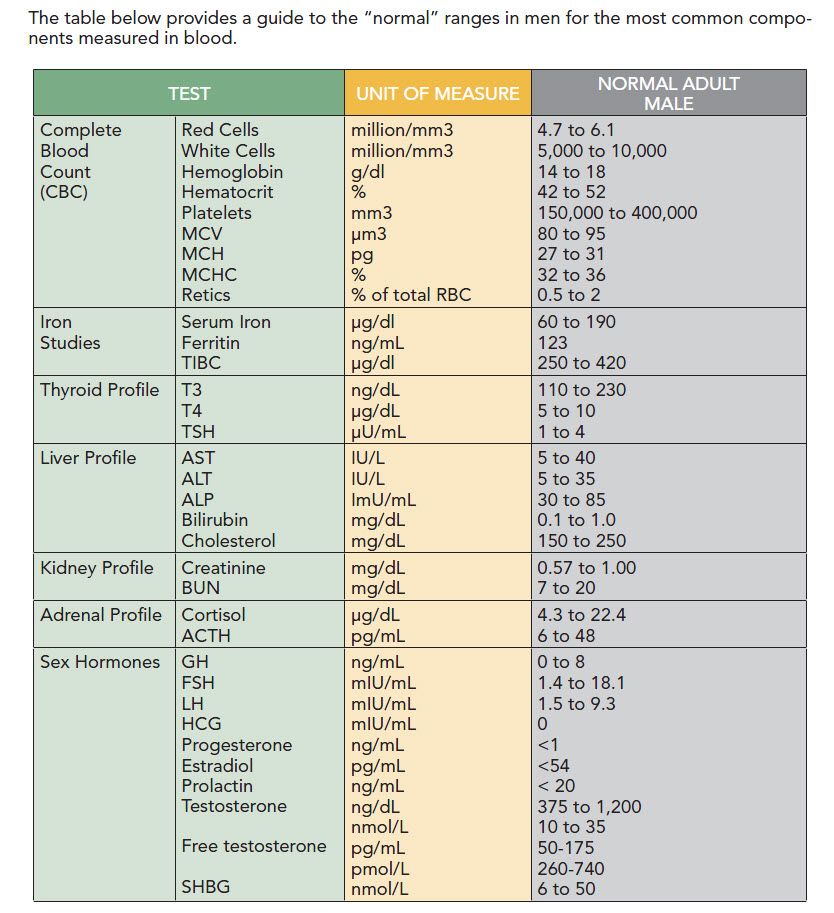 0 gm/dL 0 gm/dL | >22.0 gm/dL |
| Hematocrit | <21% | >65% |
| Lactate dehydrogenase (LDH) | ----- | >3,000 U/L |
| Lactic acid, plasma: | >3.0 mmol/L | |
| Lead | ----- | ≥10 mcg/dL |
| Low Molecular Weight Heparin (LMWH) | ----- | ≥2.0 IU/mL |
| Magnesium (blood) | <1.2 mg/dL | >3.0 mg/dL |
| Metabolic Error Screen | ----- | any positive |
| Nucleated cells (CSF) | ----- | > 5 cells present |
| Osmolality | ----- | > 300 mOsm/L |
| Base Excess Neonates (arterial or capillary) | <-10 mEq/L | ----- |
| pH | <7.25 | >7.60 |
| pCO2 | ----- | >75 mm Hg |
| pO2 | <50 mm Hg | >100 mm Hg |
| Phosphorus | <3 mg/dL | >8 mg/dL |
| Platelet Count | ≤50,000 /mm3 | >1,000,000 /mm3 |
| Prothrombin Time (PT) | ----- | >4. 0 INR 0 INR |
| Partial Thromboplastin Time (PTT) | ----- | ≥90.0 seconds |
| Sodium | <125 mEq/dL | >150 mEq/dL |
| Unfractionated Heparin | ----- | ≥0.8 IU/mL |
| Urea Nitrogen | ----- | >60 mg/dL |
| Uric acid | ----- | >12 mg/dL |
| WBC Peripheral Blood | ≤2,000 /mm3 | ≥35,000 /mm3 |
| % Bands | ----- | >25 % |
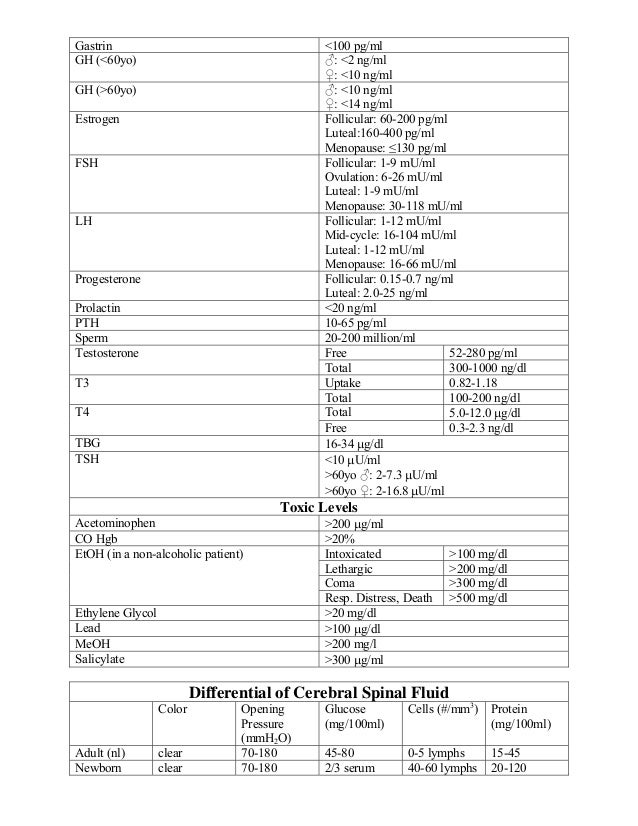
| Therapeutic Drug Levels | ||
| Acetaminophen | ----- | >150 mcg/mL |
| Amikacin | ----- | Peak: >30.0 mcg/mL Trough: >10.0 mcg/mL |
| Carbamazepine | ----- | >15.0 mcg/mL |
| Cyclosporin | ----- | >450 ng/mL |
| Digoxin | ----- | >2. 1 ng/mL 1 ng/mL |
| Dilantin | ----- | >20.0 mcg/mL |
| Gentamicin | ----- | Peak: >12.0 mcg/mL Trough: >2.0 mcg/mL |
| Lithium | ----- | >1.5 mEq/L |
| Phenobarbital | ----- | >50 mcg/mL |
| Salicylate | ----- | >30 mg/mL |
| Sirolimus | ----- | >25 ng/mL: Liver Transplantation |
| Tacrolimus | ----- | >7.5 ng/mL |
| Theophylline | ----- | >20.0 mcg/mL |
| Tobramycin | ----- | Peak: >12.0 mcg/mL Trough: >2.0 mcg/mL |
| Valproic acid | ----- | >120 mcg/mL |
| Vancomycin | ----- | Peak: > 60.0 mcg/mL Trough: <5.0 mcg/mL or >15.0 mcg/mL |
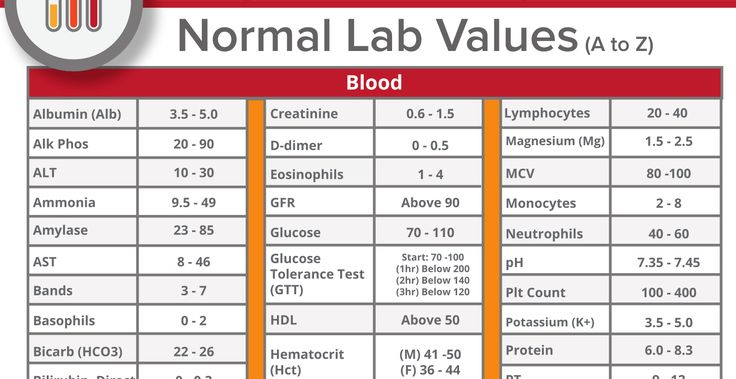
Pediatric Reference Ranges
Listed in this appendix are pediatric normal ranges for some of the more common hematology and chemistry tests along with the references from which they were obtained.
|
Hematology |
|||
| Test | Age | Range | Units |
| Red Cell Count | 0-1 month 1-2 months 2-3 months 3-6 months 6 months-1 year |
3.90-5.90 3.10-5.30 2.70-4.50 3.10-5.10 3.90-5.50 |
millions/mm3 |
| Hematocrit | 0-1 month 1-2 months 2-3 months 3-6 months 6 months-1 year |
42-65 33-55 28-41 29-41 31-41 |
% |
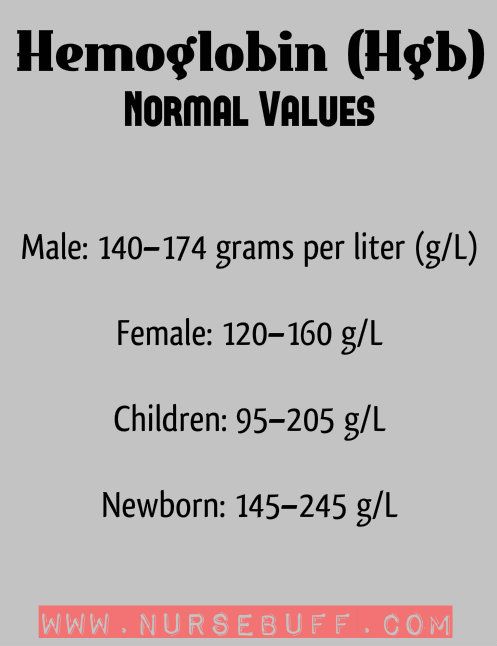
| Hemoglobin | 0-1 month 1-2 months 2-3 months 3-6 months 6 months-1 year |
13. 4-19.9 4-19.910.7-17.1 9.0-14.1 9.5-14.1 11.3-14.1 |
gm/dL |
| MCH | 0-1 month 1-3 months 3-6 months 6 months-1 year |
31-37 27-36 25-35 23-31 |
pg |
| MCHC | 0-6 months 6 months-1 year |
28-36 32-36 |
g/dL RBC |
| MCV | 0-1 month 1-3 months 3-6 months 6 months-1 year |
88-123 91-112 74-108 70-85 |
femtoliters |
| White Cell Count | 0-1 month 1-3 months 3 months-1 year 1-2 years 2-4 years |
9000-30000 5000-19500 6000-17500 6000-17000 5500-15500 |
mm3 |
| Differential (manual) Neutrophils | 0-1 month 1-3 months 3-6 months 6 months-5 years 5-18 years |
1000-20000 1000-9000 1000-8500 1500-8500 1700-7500 |
mm3 |
| Lymphocytes | 0-1 month 1-3 months 3-6 months 6 months-1 year 1-2 years 2-5 years 5-18 years 18+ years |
2000-11000 2500-16500 4000-13500 4000-10500 3000-9500 2000-8000 1250-7000 875-3300 |
mm3 |
| Monocytes | 0-1 month 1-3 months 3-12 months 1-2 years 2-5 years 5-18 years 18+ years |
540-1800 350-1365 300-875 300-850 275-775 28-825 130-860 |
mm3 |
| Eosinophils | 0-1 month |
270-900 150-585 180-525 180-510 165-465 40-650 40-390 |
mm3 |
| Basophils | 0-1 month 1 month-5 years 5-18 years 18+ years |
0-400 0-140 7-140 10-136 |
mm3 |
These ranges were extrapolated from published ranges in the following references.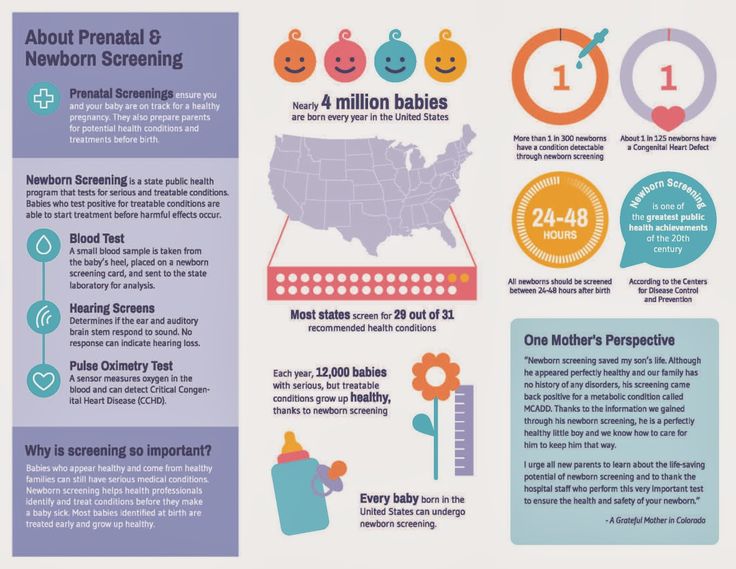
Chemistry - Assays with Separate Male/Female Ranges |
||||
| Test | Age | Male | Female | Units |
| Albumin | 0-4 days 4 days-14 years 14-18 years |
2.8-4.4 3.8-5.4 3.2-4.5 |
2.8-4.4 3.8-5. 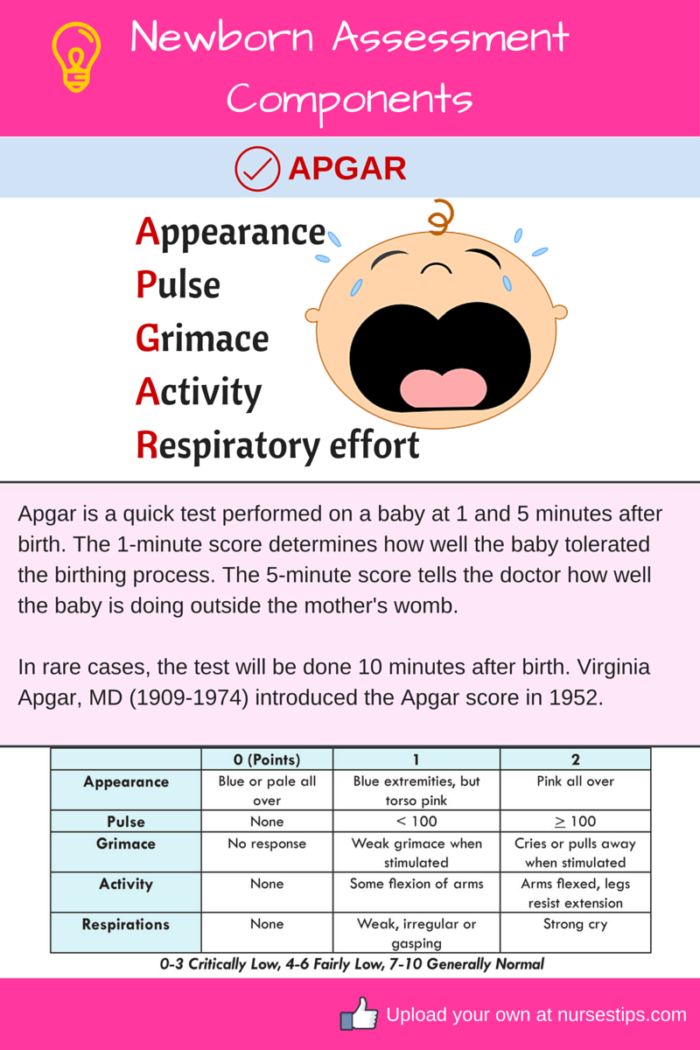 4 43.2-4.5 |
g/dL g/dL g/dL |
| Alpha Fetoprotein, Non-Pregnant | 0-13 days 14-30 days 1 month 2 months 3 months 4 months 5 months 6-11 months 1 year 2 years 3+ years |
5,000-105,000 300-60,000 100-10,000 40-1,000 11-300 5-200 0-90 0-60 0-17 0-12 0-9 |
5,000-105,000 300-60,000 100-10,000 40-1,000 11-300 5-200 0-90 0-97 0-41 0-12 0-9 |
ng/mL ng/mL ng/mL ng/mL ng/mL ng/mL ng/mL ng/mL ng/mL ng/mL ng/mL |
| Calcium (Total) | Birth-30 days 31 days-1 year 1-6 years 7-12 years 13-15 years 16-18 years |
8. 5-10.6 5-10.68.7-10.5 8.8-10.6 8.7-10.3 8.5-10.2 8.4-10.3 |
8.4-10.6 8.9-10.5 8.5-10.5 8.5-10.3 8.4-10.2 8.6-10.3 |
mg/dL mg/dL mg/dL mg/dL mg/dL mg/dL |
| Phosphatase, Alkaline | 1-30 days 31 days-1 year 1-3 years 4-6 years 7-9 years 10-12 years 13-15 years 16-18 years |
75-316 82-383 104-345 93-309 86-315 42-362 74-390 52-171 |
48-406 124-341 108-317 96-297 69-325 51-332 50-162 47-119 |
U/L U/L U/L U/L U/L U/L U/L U/L |
| Progesterone | < 2 years old 2-9 years old 10-17 years old |
0. 87-3.37 87-3.37< 0.2 adult levels generally achieved by puberty |
0.87-3.37 0.20-0.24 adult levels generally achieved by puberty |
ng/mL ng/mL |
| Test | Age | Range | Units |
| Testosterone, Total (Male) | <1 month 1-5 months 6-24 months 2-5 years 6-9 years 10-11 years 12-13 years 14-15 years 16-18 years Tanner stage 1 |
75-400 14-363 < 37 < 19 < 13 3-327 29-432 40-778 238-1048 < 15 |
ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL |
| Testosterone, Total (Female) | Up to 30 days 1-5 months 6-24 months 2-3 years 4-5 years 6-7 years 8-9 years 10-11 years 12-13 years 14-15 years 16-18 years Tanner stage 1 |
20-64 < 20 < 9 < 20 < 30 < 13 1-8 3-32 3-50 6-52 9-58 < 17 |
ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL ng/dL |
| Test | Age | Male | Female | Units |
| Iron (Transferrin) Saturation | 20-50 | 15-50 | % | |
| Total Protein | Birth-31 days 1-6 months 6 months-1 year 1-18 years |
4. 1-6.3 1-6.34.7-6.7 5.5-7.0 5.7-8.0 |
4.2-6.2 4.4-6.6 5.6-7.9 5.7-8.0 |
g/dL g/dL g/dL g/dL |
|
Chemistry - Assays with Genderless Ranges |
|||
| Test |
Age |
Range |
Units |
| Carbon dioxide (CO2 content=bicarb+dissolved CO2) |
Cordblood Child |
15-20 18-27 |
mEq/L mEq/L |
Creatinine Note: There are gender-specific ranges only for ages 16 years and older. |
Premature Neonates 2-12 months 1-2 years 3-4 years 5-6 years 7-8 years 9-10 years 11-12 years 13-15 years Males 16 years + |
0.3-1.o 0.2-0.9 0.2-0.4 0.2-0.5 0.3-0.7 0.3-0.7 0.2-0.6 0.3-0.7 0.3-0.9 0.4-0.9 0.6-1.2 |
mg/dL mg/dL mg/dL mg/dL mg/dL mg/dL mg/dL mg/dL mg/dL mg/dL mg/dL |
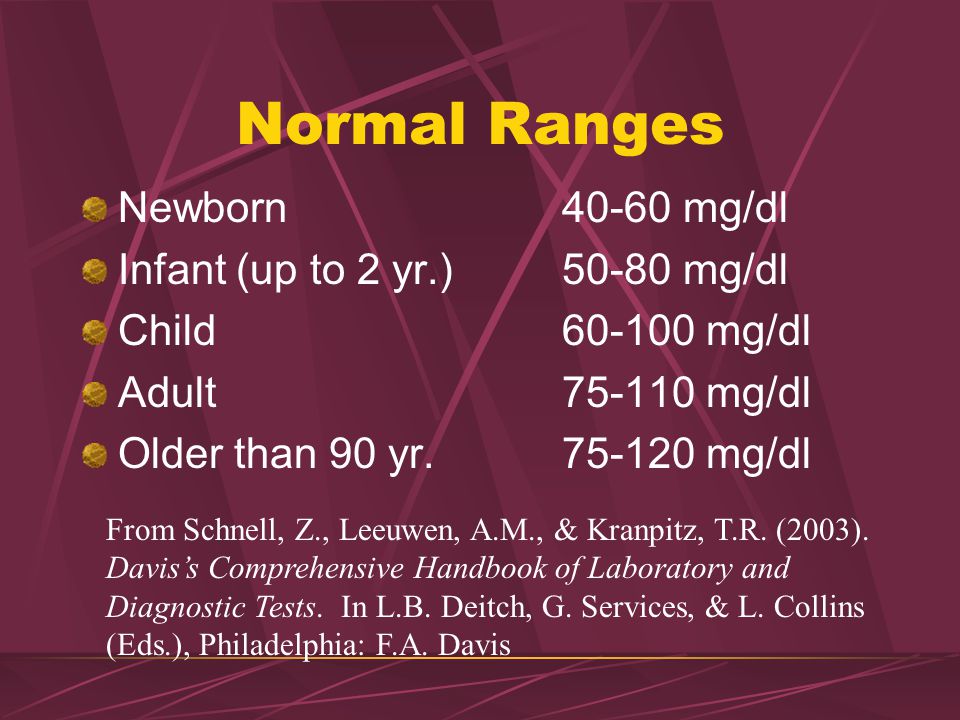
| Glucose | 0-1 month 1 month-adult |
40-99 65-99 |
mg/dL mg/dL |
| Iron | Birth-4 months 5-23 months 24-35 months 3-11 years 12 years+ |
110-270 30-70 20-124 53-119 Use adults ranges |
mcg/dL mcg/dL mcg/dL mcg/dL |
| N-terminal-pro-BNP | 0-30 days 1-11 months 12-35 months 3-6 years 7-14 years 15-18 years |
263-6500 37-1000 39-675 23-327 10-242 6-207 |
pg/mL pg/mL pg/mL pg/mL pg/mL pg/mL |
| Percent Saturation | Newborn 4-10 months 3-10 years |
65 25 30 |
% % % |
| Phosphorus | Newborn-11 months 12 months-15 years 16+ years |
4. 2-9.0 2-9.03.2-6.3 2.7-4.5 |
mg/dL mg/dL mg/dL |
| Potassium | <10 days >10 days |
3.5-6.0 3.5-5.0 |
mEq/L mEq/L |
| Sodium | Premature | 130-140 | mEq/L |
| Uric Acid | 0-2 years 2-12 years 12-14 years |
2.0-7.0 2.0-6.5 2.0-7.0 |
mg/dL mg/dL mg/dL |
Critical Care / Special Care Nurseries |
|||
| Test |
Age |
Range |
Units |
| Bilirubin | cord 24 hrs Preterm Term 48 hrs Preterm Term 3-5 days Preterm Term 1m-adult |
<1.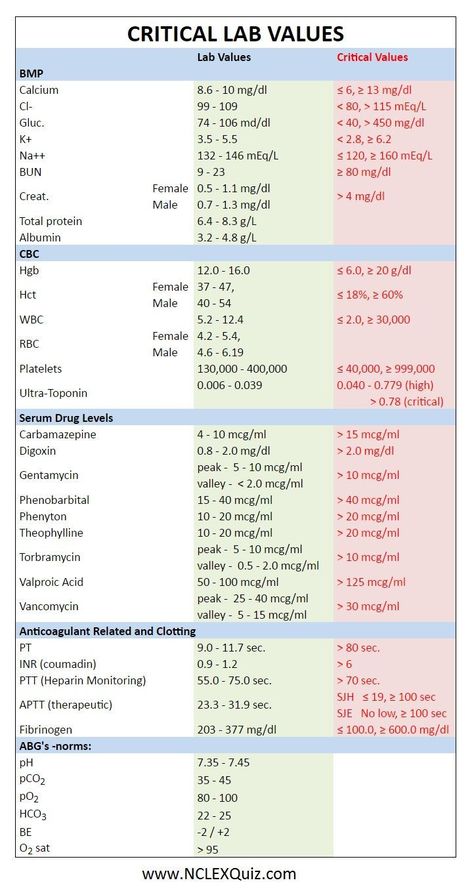 8 8< or = 6.0 < or = 6.0 < or = 8.0 < or =12.0 |
mg/dL mg/dL mg/dL mg/dL mg/dL |
| Calcium (ionized) | Neonatal | 4.2-5.9 | mg/dL |
| Glucose | 0-30 days > 1month Special Care Nursery: |
40-99 65-99 50-99 |
mg/dL |
| pCO2 (Arterial) | 0-18 years | 30-40 | mmHg |
| pCO2 (Venous/Capillary) | 0-18 years Boys: Girls: |
35-48 32-45 |
mmHg |
| pH (Arterial) | 0-1 month > 1 month |
7. 32-7.42 32-7.427.35-7.45 |
|
| pH (Venous) | 0-1 month > 1 month |
7.30-7.40 7.33-7.43 |
|
| pH (Capillary) | All ages | 7.30-7.40 | |
| pO2 (Arterial) | 0-1 month > 1month |
60-80 80-100 |
mmHg |
| pO2 (Venous/Capillary) | 0-18 years | 50-65 | mmHg |
| Potassium | 0-10 days > 10 days |
3. 5-6.0 5-6.03.5-5.0 |
mEq/L |
Hemoglobin and Hematocrit Ranges |
||||
|
Hemoglobin |
Hematocrit | |||
| Age | Male | Female | Male | Female |
| 0-31 days | 13.4-19.9 | 13.4-19.9 | 42-64% | 42-64% |
| 31 days-2 months | 10.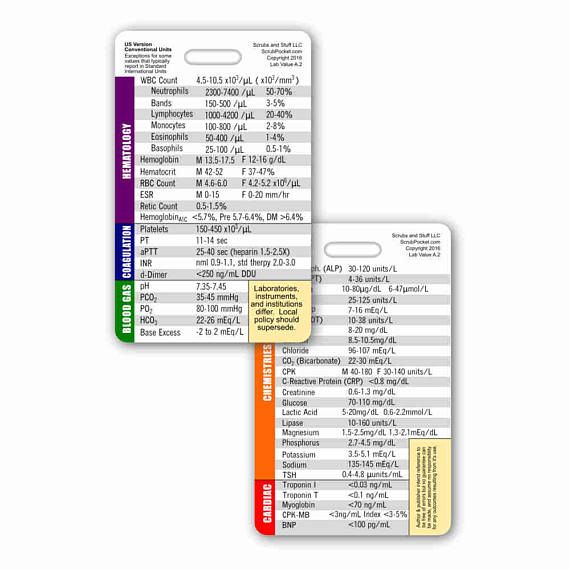 7-17.1 7-17.1 |
10.7-17.1 | 33-54% | 33-54% |
| 2-3 months | 9.0-14.1 | 9.0-14.1 | 28-41% | 28-41% |
| 3-6 months | 9.5-14.1 | 9.5-14.1 | 29-41% | 29-41% |
| 6 months-1 year | 11.3-14.1 | 11.3-14.1 | 31-41% | 31-41% |
| 1-5 years | 10.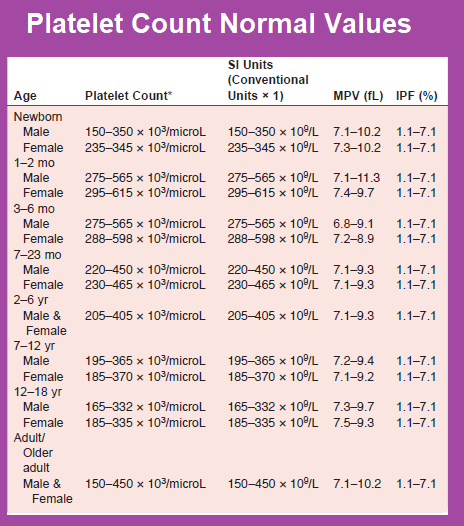 9-15.0 9-15.0 |
10.9-15.0 | 31-44% | 31-44% |
| 5-11 years | 11.9-15.0 | 11.9-15.0 | 35-44% | 35-44% |
| 11-18 years | 12.7-17.7 | 11.9-15.0 | 37-48% | 34-44% |
References:
*Neonatal reference values for ionized calcium; "Scand. J Lab Invest". 1987, 47: 111-117.
- Meites, S. Ed. "Pediatric Clinical Chemistry", 2nd edition.
- "The American Association for Clinical Chemistry", 1981; Tietz, NW.

- "The Textbook of Clinical Chemistry", 1984.
- Lundberg, GD, et al."JAMA", 1986, 255: 2329-39.
- Scully, RE, et al. "New England Journal of Medicine" 1986, 314:39-49.
- Diabetes Care 28 (Suppl 1) S41, 2005.
Laboratory indicators of hemostasis in healthy newborns
| Indicator | Days of life | ||||
| 1 | 3 | 8 | 14 | 30 | |
| Microcoagulant test (MKT), % | 60-80 (↓) | 30-55 (↓↓) | 55-75 (↓) | 75-85 (↓) | 75-90 (↓) |
| Prothrombin test (PT), % | 60-80 (↓) | 30-55 (↓↓) | 55-75 (↓) | 80-100 | 80-100 |
| Thrombin time (TV), sec | 19-20 (↑) | 15 - 16 | 14 - 16 | ||
| Fibrinogen, g/l | 2 - 4 | ||||
| Orthophenanthroline test (OFT), mcg/ml | 5 - 10 | 12 - 16 | 5 - 7 | 3. | |
↓ - some decrease in the indicator
↓↓ - significant decrease in the indicator
↑ - some increase in the indicator
Laboratory data for the most common hemorrhagic syndromes in newborns
| Indicators | The norm in full-term children | Hemorrhagic disease | Hemophilia | Thrombocytopenias | DIC (2nd phase) |
| Quantity platelets | 150 – 400x10 9 /l | Norm | Norm | Reduced | Reduced |
| Clotting time | 2-4min | Extended | Extended | Norm | Extended |
| Time bleeding | 3-4 min | Norm | Norm | Extended | Extended |
| PV | 13–16s | Extended | Norm | Norm | Extended |
| Thrombin time (TV) | 10-16s | Norm | Norm | Norm | Extended |
| Activated partial thromboplastic time (APTT) | 45–60s | Extended | Extended | Norm | Extended |
| Fibrinogen | 1. | Norm | Norm | Norm | Reduced |
| Products fibrin degradation | 0-7mg/ml | Norm | Norm | Norm | Upgraded |
BIOCHEMICAL BLOOD TEST VALUES,
RECOMMENDED MULTIPLICITY OF THEIR DEFINITION
IN NEWBORN FOR DIFFERENT GESTATIONAL AGES
Biochemical parameters of blood tests in children of different ages and adults
(Pediatric in-patient department of the MEP "Maternity Hospital No. 1" Omsk)
| Biochemical parameters | Units measurements | Norms in children | Norms in adults |
| Protein | g/l | Newborn - 46-68 Children under 1 year -50-73 | 65-85 |
| Bilirubin total | µmol/l | By Shabalov in cord blood up to 51 3-4 days full-term - up to 256; premature up to 171 hourly gain - less than 6. | 1.7-20.5 |
| Bilirubin direct | µmol/l | By Shabalov up to 10% of the total with TTH | 0-5 |
| Glucose | mmol/l | Newborn full term - 2.2-3.3 Up to 1 month - 2.8-4.4 max up to 6.5 Children under 1 year - 3.3-5.5 | 3.3-5.5 |
| Potassium | mmol/l | Newborn - 3.6-6.1 Children under 1 year - 3.5-5.8 | 3.5-5.1 |
| Sodium | mmol/l | Newborn - 132-147 Children under 1 year old 130-143 | 135-145 |
| Calcium total | mmol/l | Newborn - 1. Children - 2.0-2.6 | 2.0-2.6 |
| Calcium ionized | mmol/l | Makes up about 50% of the total | 1.0-1.23 |
| Phosphorus | mmol/l | Newborn-1.6-3.0 Children under 1 year old - 1.45-2.26 | 0.86-1.62 |
| Magnesium | mmol/l | Newborn - 0.7-1.0 Children under 1 year old-0.8-1.0 | 0.8-1.0 |
| Chlorides | mmol/l | Novorozhd-95-110 Children under 1 year old-93-112 | 95-110 |
| Iron | µmol/l | Newborn 17. | Zh-8,8-27 |
| Children-8.9-21.4 | M-9.5-30 | ||
| Total iron binding capacity (OJSS) | µmol/l | Up to 2 months-27-61 | Zh-49-89 |
| Children under 1 year - 52-78 | М-52-77 | ||
| Coefficient Fe saturation 2++ | % | 25-40% | 20-55% |
| Alanine aminotransferase (ALAT) | U/L | 6 days-6 months up to 60 7-12 months up to 57 | up to 42 |
| Aspartic aminotransferase (ASAT) | U/l | 6 days-6 months up to 84 7-12 months up to 89 | up to 37 |
| Gammaglutamine transferase (GGT) | U/l | 6 days-6 months - up to 204 7-12 months - up to 34 | up to 47 |
| Alkaline phosphatase (AP) | U/l | 6 days-6 months - up to 1076 7-12 months - up to 1107 | Up to 306 |
| Lactate dehydrogenase (LDH) | U/l | 6 days-6 months - up to 975 7-12 months - up to 1100 | Up to 450 |
| Alpha-amylase | U/l | In serum - up to 220 In urine - up to 1000 | up to 220 up to 1000 |
| Cholesterol total | mmol/l | Newborn - 1. Children under 1 year - 1.8-4.5 | 3.6-6.0 suspicious >5.2 |
| Triglycerides | mmol/l | Children 0.4-1.29 | 0.57-2.2 suspicious > 1.7 |
| Beta-lipoproteins | Unit | Up to 50 units | 35-55 units |
| Urea | mmol/l | Newborn - up to 7.0 Up to 6 months - up to 7.2 | 1.7-8.1 |
| Creatinine | µmol/l | Preterm newborn -up to 115 Up to 1 week - up to 88 2-4 weeks - up to 44 children under 1 year up to 62 | M. Women - 44-80 |
| Thymol test | unit | 0-5 units | 0-6 units, suspicious>5 |
Child health - infancy
Comprehensive laboratory examination, including the main indicators of the health of a child up to a year, including blood and urine tests, as well as an assessment of protein, carbohydrate and fat metabolism.
Russian synonyms
Laboratory examination of a child under one year old, preventive (screening) tests up to a year old.
English synonyms
Laboratory check-up, Infancy, Infant Health Check up.
What biomaterial can be used for research?
Venous, capillary blood, mid morning urine.
How to properly prepare for an examination?
General information about the study
Infancy is the period of life from birth to 1 year.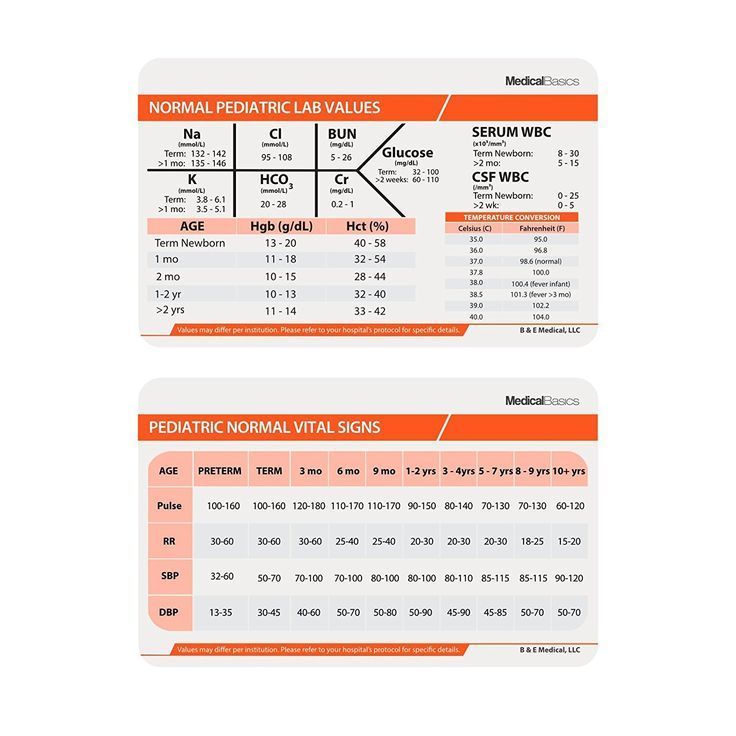 It is characterized by some features both during normal development and in the event of diseases in this period. Often, diseases of the infancy period manifest themselves in the form of such non-specific signs as poor appetite, anxiety, sleep disturbance, indomitable crying, reduced activity, hypotension, and fatigue. These signs can hide quite serious diseases, such as congenital heart defects. On the other hand, these same signs can be observed from time to time in healthy babies. Thus, a clinical examination does not always allow an accurate assessment of the child's health. In order to more accurately assess the health of a child in the period up to 1 year, additional laboratory tests are carried out - preventive (screening) tests. A comprehensive laboratory examination is especially convenient for the pediatrician and the patient, in which all the necessary tests are performed with a single biomaterial (blood and urine) sampling.
It is characterized by some features both during normal development and in the event of diseases in this period. Often, diseases of the infancy period manifest themselves in the form of such non-specific signs as poor appetite, anxiety, sleep disturbance, indomitable crying, reduced activity, hypotension, and fatigue. These signs can hide quite serious diseases, such as congenital heart defects. On the other hand, these same signs can be observed from time to time in healthy babies. Thus, a clinical examination does not always allow an accurate assessment of the child's health. In order to more accurately assess the health of a child in the period up to 1 year, additional laboratory tests are carried out - preventive (screening) tests. A comprehensive laboratory examination is especially convenient for the pediatrician and the patient, in which all the necessary tests are performed with a single biomaterial (blood and urine) sampling.
This comprehensive analysis includes key general clinical and biochemical parameters.
Complete blood count (CBC) allows you to get basic information about the function of the hematopoietic system of an infant, exclude congenital and acquired anemia and suspect signs of hypoxia in congenital diseases of the cardiovascular and respiratory systems. Using the analysis of the leukocyte formula, one can suspect congenital immunodeficiencies or identify torpid infections. An additional indicator that is used to identify the current infectious and inflammatory process is the erythrocyte sedimentation rate (ESR).
Urinalysis with sediment microscopy is the best initial test for diagnosing diseases of the urinary system. It includes a macroscopic assessment of urine (color, odor, transparency), its physicochemical properties (relative density, pH, presence of protein, glucose) and microscopic examination (presence of leukocytes, epithelium, erythrocytes, additional inclusions). Urinalysis can detect signs of infection and occult bleeding in both the lower and upper urinary tract.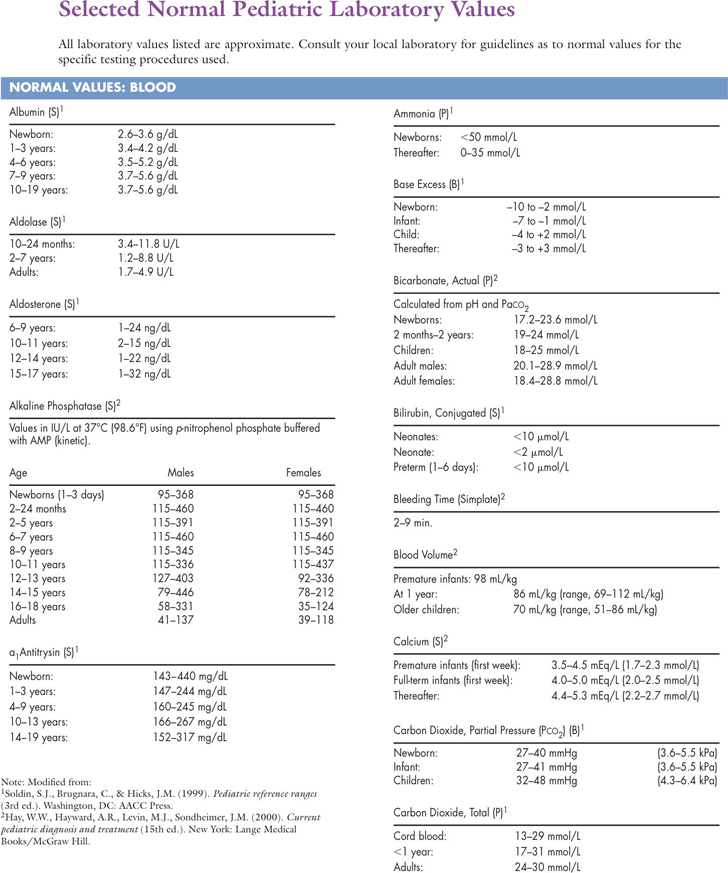 Diagnosis of congenital anomalies of the urinary system (for example, posterior urethral valve syndrome), although it requires a more thorough instrumental examination (ultrasound), also always begins with a urine test.
Diagnosis of congenital anomalies of the urinary system (for example, posterior urethral valve syndrome), although it requires a more thorough instrumental examination (ultrasound), also always begins with a urine test.
To assess the nutritional status of an infant, total protein, glucose, and cholesterol are examined. Total protein is an integral indicator of protein metabolism in the body. Of greater importance is the decrease in total protein, which in pediatric practice can be observed with malnutrition (the extreme option is kwashiorkor), long-term infections (including helminthiases and parasitosis), congenital malformations of the digestive tube (congenital pyloric stenosis, duodenal atresia). Glucose is an integral indicator of carbohydrate metabolism. Hypoglycemia may indicate malnutrition, the presence of diseases of the liver (glycogenoses) and adrenal glands (autoimmune polyendocrine syndrome). A special condition is hypoglycemia observed in newborn mothers suffering from diabetes mellitus. Hyperglycemia may accompany an ongoing infectious-inflammatory process (eg, sepsis) or indicate congenital disorders of carbohydrate metabolism (eg, congenital adrenal hyperplasia). Cholesterol (cholesterol) is an integral indicator of body fat metabolism. Cholesterol is the main component of cell membranes and is absolutely necessary for the normal growth and development of not only an infant, but also an adult. Low cholesterol levels are more likely to indicate malnutrition. The cholesterol levels of breastfed or formula-fed infants can vary greatly. Thus, by 6 months of age, exclusively breastfed infants have a total cholesterol level of about 200 mg/dL (which is about the same as adult cholesterol), while exclusively formula-fed infants have a cholesterol level of about 140 mg/mL. . Hypercholesterolemia in infancy often indicates congenital cholesterol metabolism diseases (eg, familial hypercholesterolemia).
Hyperglycemia may accompany an ongoing infectious-inflammatory process (eg, sepsis) or indicate congenital disorders of carbohydrate metabolism (eg, congenital adrenal hyperplasia). Cholesterol (cholesterol) is an integral indicator of body fat metabolism. Cholesterol is the main component of cell membranes and is absolutely necessary for the normal growth and development of not only an infant, but also an adult. Low cholesterol levels are more likely to indicate malnutrition. The cholesterol levels of breastfed or formula-fed infants can vary greatly. Thus, by 6 months of age, exclusively breastfed infants have a total cholesterol level of about 200 mg/dL (which is about the same as adult cholesterol), while exclusively formula-fed infants have a cholesterol level of about 140 mg/mL. . Hypercholesterolemia in infancy often indicates congenital cholesterol metabolism diseases (eg, familial hypercholesterolemia).
Bilirubin is a pigment produced by the breakdown of hemoglobin and some other heme-containing proteins in the liver, spleen and bone marrow. An increase in the level of bilirubin can be observed in many diseases of the hepatobiliary system (biliary atresia, hepatitis B), hemolytic anemia, as well as in many other conditions, including hypothyroidism, sepsis, galactosemia, Crigler-Najjar syndrome and others. To clarify the cause of hyperbilirubinemia, separate determination of direct and indirect bilirubin, as well as the study of the level of liver enzymes, gamma-HT and alkaline phosphatase may be required.
An increase in the level of bilirubin can be observed in many diseases of the hepatobiliary system (biliary atresia, hepatitis B), hemolytic anemia, as well as in many other conditions, including hypothyroidism, sepsis, galactosemia, Crigler-Najjar syndrome and others. To clarify the cause of hyperbilirubinemia, separate determination of direct and indirect bilirubin, as well as the study of the level of liver enzymes, gamma-HT and alkaline phosphatase may be required.
This comprehensive analysis excludes major diseases in infancy. Additional laboratory tests may be required to provide more information about the baby's health. Repeated analyzes are recommended to be performed using the same test systems, that is, in the same laboratory.
What is research used for?
- For a comprehensive assessment of the health status of a child under one year old;
- for the timely detection of major diseases of infancy.
When is the test scheduled?
- At a preventive examination of a child;
- if the baby has poor appetite, insufficient weight gain, hypotension, indomitable crying, poor sleep, rapid fatigue.
 5 - 4
5 - 4 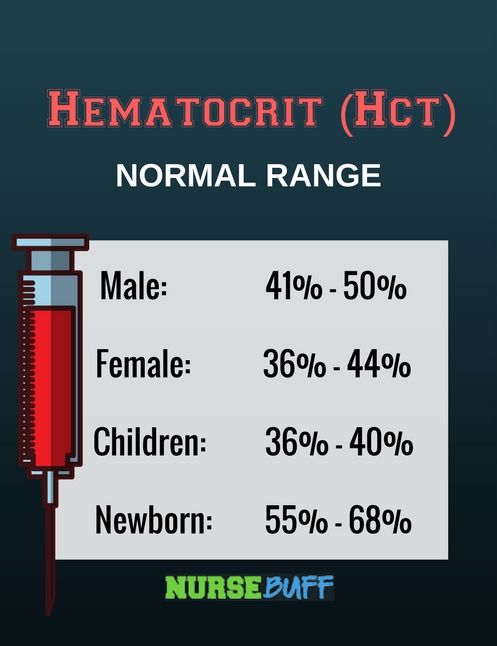 5–3.0 g/l
5–3.0 g/l  8
8  75-2.73
75-2.73  8-34
8-34  3-3.5
3-3.5 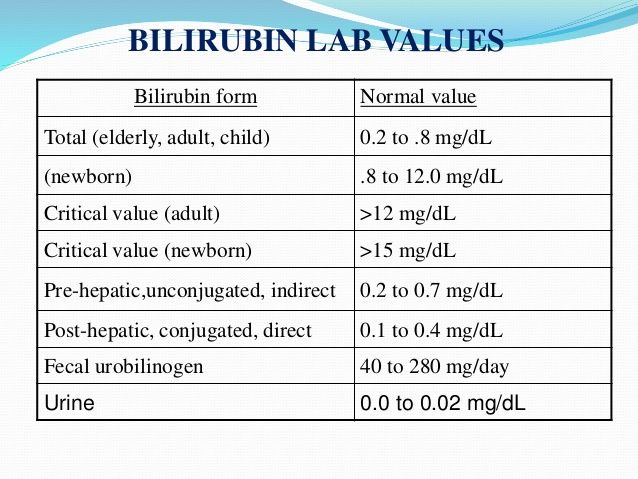 -53-97
-53-97