Is it safe to use abreva while pregnant
Affect on Baby and Safe Treatments
If you’ve ever had cold sores — those annoying, painful, tiny, fluid-filled blisters that usually form around your mouth and on your lips — you know how inconvenient they can be.
But also if you’ve ever had cold sores (and therefore already have the virus that causes them), did you know they can recur, especially when you’re under stress or are undergoing hormonal fluctuations?
Stress and hormonal changes. That sounds an awful lot like pregnancy.
Cold sores in pregnancy aren’t unheard of, and they don’t usually have any impact on your growing baby. So first, let out a deep sigh of relief. Next, read on — because there are still important things to know about cold sores if you’re expecting.
Cold sores are caused by a virus — the herpes simplex virus (HSV). Of the two types of HSV, cold sores are generally caused by HSV-1, whereas genital herpes is usually a result of exposure to HSV-2. There have been a few instances where HSV-1 sores have been found in the genitals and vice versa.
Once you’ve had a cold sore (oral herpes), the virus remains in your system for life — it’s just not active unless you have a current outbreak.
But when we say that stress and hormones can cause the virus to reactivate, it’s important to know that stress and hormones don’t cause the virus in the first place.
If you’ve never had HSV, you can only get it through contact with someone who has. When it comes to a first-time cold sore infection, this can happen via activities like:
- kissing
- sharing food or utensils
- using someone else’s ChapStick or lip gloss
- oral sex
Here’s the really good news: If you already have the virus that causes cold sores, and you have an outbreak of oral herpes during pregnancy, it’s most likely not going to have any impact on your growing baby.
Cold sores are a localized infection, usually around the mouth area. They don’t typically cross the placenta and reach your baby.
The highest risk scenario is if you get HSV for the first time during your third trimester of pregnancy.
When you get the virus for the first time, your body hasn’t developed any protective antibodies to it yet. And while HSV-1 is usually associated with oral herpes, it can cause a genital herpes outbreak, which can be dangerous to your baby — especially as they pass through the birth canal.
Birth-acquired herpes is serious. However, it’s a concern with genital rather than oral herpes. That being said, because the same virus can cause both, it’s important to talk to your OB about any cold sores during pregnancy.
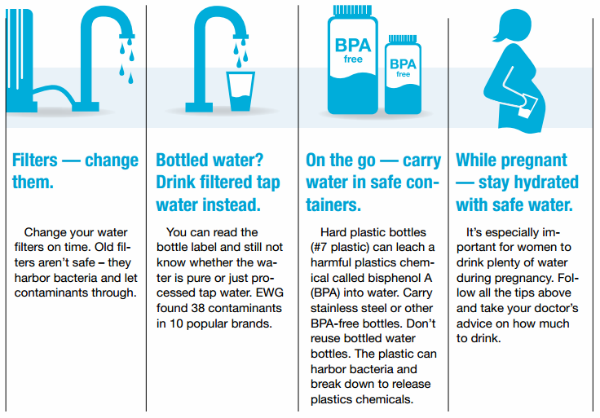
The most common treatment for cold sores is docosanol (Abreva), an over-the-counter topical cream. But the Food and Drug Administration hasn’t evaluated it for safety in pregnancy.
While some research has determined that it’s “likely safe” during pregnancy, at least one pharmaceutical company that manufactures the drug warns against using it unless it’s definitely needed — which really means you need to check with your doctor. There may be other treatments you should try first.
If you’ve had herpes in the past, your doctor may recommend antivirals — like acyclovir or valacyclovir — starting at week 36 and continuing until delivery of your baby, even if you don’t have a current outbreak of lesions around the genital area. This helps prevent reactivation and spread of the virus to the genital area.
This precaution is because you shouldn’t expose your baby to herpes in the vaginal area during delivery.
Alternatively, your doctor may suggest a cesarean delivery, which avoids the birth canal altogether — something that’s especially important if you have a current outbreak of genital herpes.
Cold sores are highly contagious, despite the fact that they won’t affect your baby in the womb. If you have them after your baby is born, avoid kissing those adorable little cheeks or touching any sores and then touching your newborn without first washing your hands with soap.
In the extremely rare event that you have cold sores on either breast, avoid breastfeeding from that breast while you’re still contagious.
Your cold sores are contagious until they crust over, at which point they’ll start to heal.
If you do pass a cold sore infection on to your newborn, it’s known as neonatal herpes. While not as serious as the birth-acquired version, it can still cause serious complications in a baby who hasn’t yet developed a robust immune system.
The cold sore on your mouth is likely to be more of an annoyance to you than a serious risk to your developing baby, particularly in your first two trimesters of pregnancy and especially if you’ve had one before. But you should still let your OB know about it.
The virus that causes cold sores — usually HSV-1 — can also cause genital herpes, which is more of a risk to your pregnancy and growing little one.
If you have an outbreak in your third trimester — or if you acquire the virus for the first time in your third trimester — your doctor may want you to follow certain treatment or precautionary guidelines, like antivirals or a cesarean delivery.
Affect on Baby and Safe Treatments
If you’ve ever had cold sores — those annoying, painful, tiny, fluid-filled blisters that usually form around your mouth and on your lips — you know how inconvenient they can be.
But also if you’ve ever had cold sores (and therefore already have the virus that causes them), did you know they can recur, especially when you’re under stress or are undergoing hormonal fluctuations?
Stress and hormonal changes. That sounds an awful lot like pregnancy.
Cold sores in pregnancy aren’t unheard of, and they don’t usually have any impact on your growing baby. So first, let out a deep sigh of relief. Next, read on — because there are still important things to know about cold sores if you’re expecting.
Cold sores are caused by a virus — the herpes simplex virus (HSV). Of the two types of HSV, cold sores are generally caused by HSV-1, whereas genital herpes is usually a result of exposure to HSV-2. There have been a few instances where HSV-1 sores have been found in the genitals and vice versa.
Once you’ve had a cold sore (oral herpes), the virus remains in your system for life — it’s just not active unless you have a current outbreak.
But when we say that stress and hormones can cause the virus to reactivate, it’s important to know that stress and hormones don’t cause the virus in the first place.
If you’ve never had HSV, you can only get it through contact with someone who has. When it comes to a first-time cold sore infection, this can happen via activities like:
- kissing
- sharing food or utensils
- using someone else’s ChapStick or lip gloss
- oral sex
Here’s the really good news: If you already have the virus that causes cold sores, and you have an outbreak of oral herpes during pregnancy, it’s most likely not going to have any impact on your growing baby.
Cold sores are a localized infection, usually around the mouth area. They don’t typically cross the placenta and reach your baby.
The highest risk scenario is if you get HSV for the first time during your third trimester of pregnancy.
When you get the virus for the first time, your body hasn’t developed any protective antibodies to it yet. And while HSV-1 is usually associated with oral herpes, it can cause a genital herpes outbreak, which can be dangerous to your baby — especially as they pass through the birth canal.
Birth-acquired herpes is serious. However, it’s a concern with genital rather than oral herpes. That being said, because the same virus can cause both, it’s important to talk to your OB about any cold sores during pregnancy.
The most common treatment for cold sores is docosanol (Abreva), an over-the-counter topical cream. But the Food and Drug Administration hasn’t evaluated it for safety in pregnancy.
While some research has determined that it’s “likely safe” during pregnancy, at least one pharmaceutical company that manufactures the drug warns against using it unless it’s definitely needed — which really means you need to check with your doctor. There may be other treatments you should try first.
If you’ve had herpes in the past, your doctor may recommend antivirals — like acyclovir or valacyclovir — starting at week 36 and continuing until delivery of your baby, even if you don’t have a current outbreak of lesions around the genital area. This helps prevent reactivation and spread of the virus to the genital area.
This precaution is because you shouldn’t expose your baby to herpes in the vaginal area during delivery.
Alternatively, your doctor may suggest a cesarean delivery, which avoids the birth canal altogether — something that’s especially important if you have a current outbreak of genital herpes.
Cold sores are highly contagious, despite the fact that they won’t affect your baby in the womb. If you have them after your baby is born, avoid kissing those adorable little cheeks or touching any sores and then touching your newborn without first washing your hands with soap.
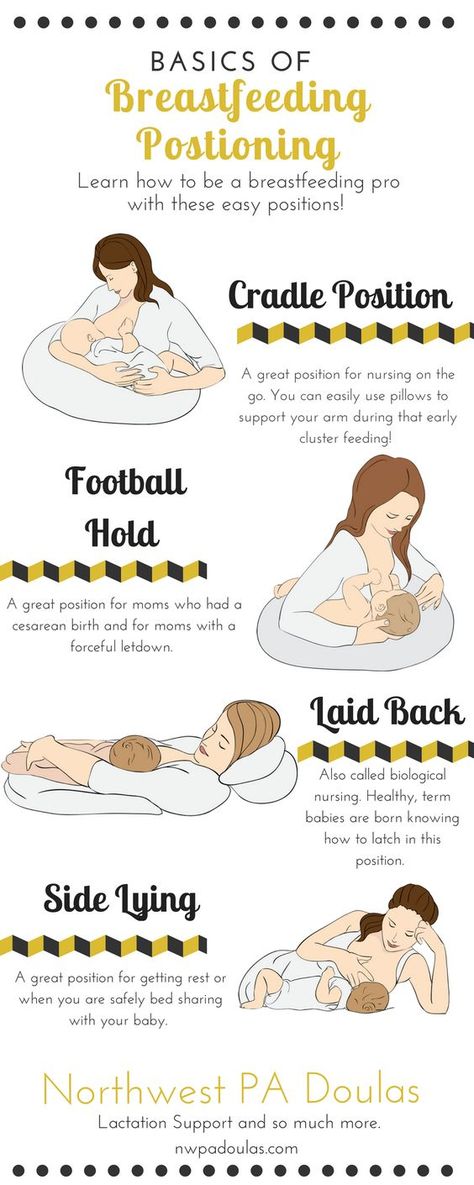
In the extremely rare event that you have cold sores on either breast, avoid breastfeeding from that breast while you’re still contagious.
Your cold sores are contagious until they crust over, at which point they’ll start to heal.
If you do pass a cold sore infection on to your newborn, it’s known as neonatal herpes. While not as serious as the birth-acquired version, it can still cause serious complications in a baby who hasn’t yet developed a robust immune system.
The cold sore on your mouth is likely to be more of an annoyance to you than a serious risk to your developing baby, particularly in your first two trimesters of pregnancy and especially if you’ve had one before. But you should still let your OB know about it.
The virus that causes cold sores — usually HSV-1 — can also cause genital herpes, which is more of a risk to your pregnancy and growing little one.
If you have an outbreak in your third trimester — or if you acquire the virus for the first time in your third trimester — your doctor may want you to follow certain treatment or precautionary guidelines, like antivirals or a cesarean delivery.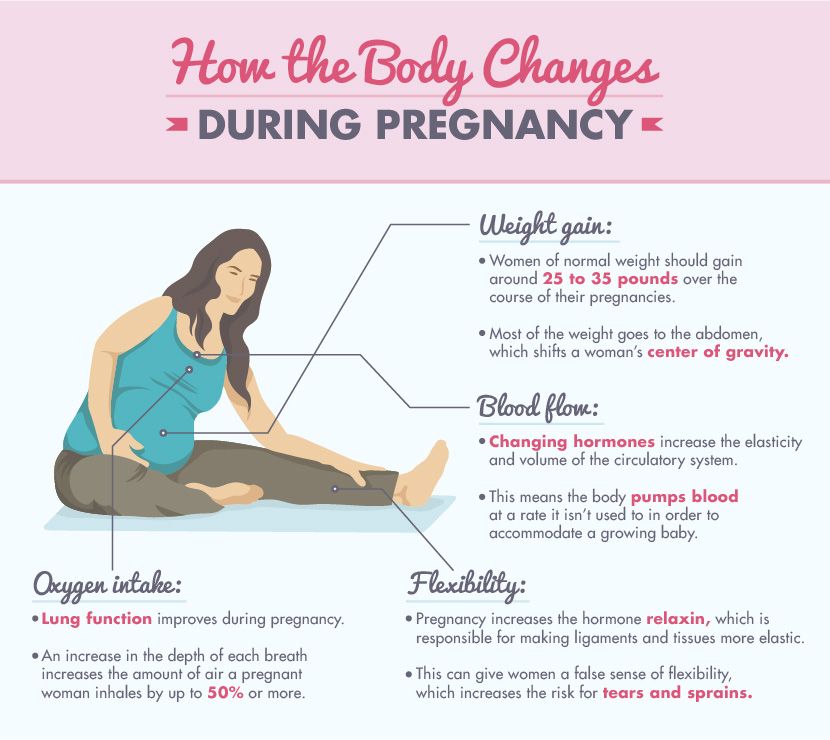
Pregnancy and medicines / Obstetrics and gynecology, reproductive medicine / Articles about health / Articles and encyclopedia / madez.ru
We have been actively planning for a baby for a long time, but we never think about the dangers of drugs during pregnancy!
Gynecologist, gynecologist endocrinologist Popova Natalya Vladimirovna will tell you what medicines can be taken during pregnancy, and which ones are categorically not recommended.
One of the most important periods in a woman's life is the period of bearing a child. And in these few months, the expectant mother must do everything in her power to give birth to a healthy baby. But pregnancy lasts nine calendar months - it is very difficult during this time to never feel any ailments or health problems.
If it is necessary to use any drug during pregnancy, the mother-to-be should remember:
- Any drug during pregnancy (at any stage) can be used only in accordance with the indications and only as prescribed by the attending physician;
- When choosing a medicinal product, preference should be given only to those medicinal products that have proven efficacy;
- Prefer monotherapy, i.
 e. treatment with only one drug if possible; combined treatment during this period is undesirable;
e. treatment with only one drug if possible; combined treatment during this period is undesirable; - Topical treatment is more desirable than systemic (oral, intravenous, intramuscular) administration of the drug.
- A pregnant woman should remember that completely safe and absolutely harmless drugs do not exist.
The most dangerous period for the use of any drugs, both of chemical and natural origin, is considered the first trimester of pregnancy (the first 12 gestational weeks), when all organs and systems are laid in the fetus, which in the future will only develop and form the placenta. It is at this time that the fetus is considered the most vulnerable to any chemical and medicinal substances.
Pronounced mutagenic hazard:
1. in industry - asbestos, acetaldehyde, vinyl chloride, dimethyl sulfate; factors of metallurgical and rubber industries;
Metals: copper, nickel, lead, zinc, cadmium, mercury, chromium, arsenic, styrene, formaldehyde, chloroprene, epichlorohydrin, ethylene oxide.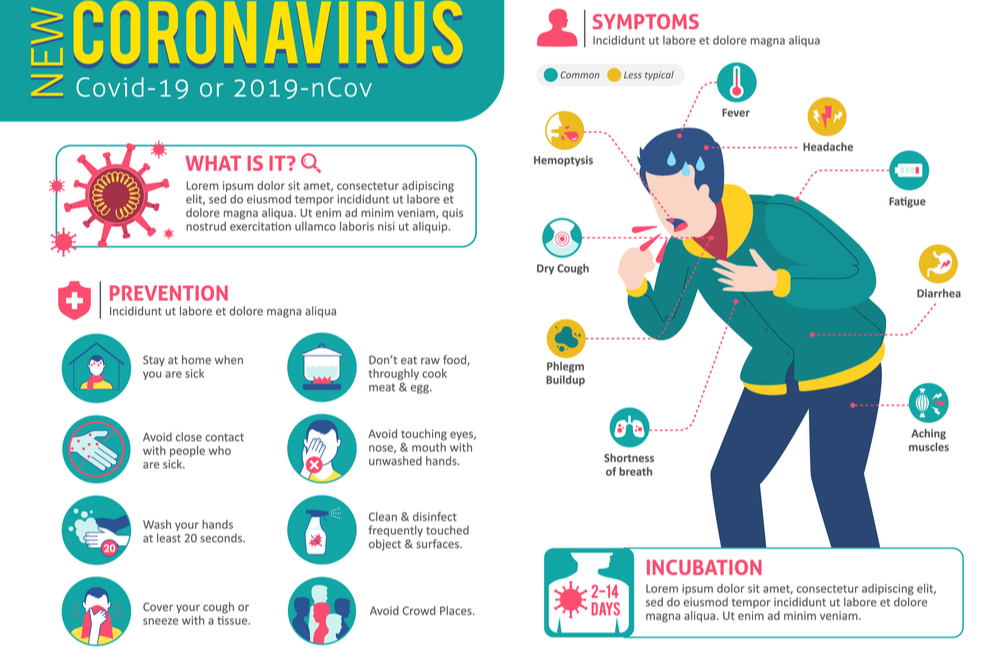
2. agriculture - a mixture of defoliants, pesticides, insectiosides, repellents, fungicides, pesticides, methylpartion, phthalaphos, chlorophos, gardona, DDT, contan.
If you work in a hazardous industry and come into contact with these chemicals, from early pregnancy, switch to "light work".
Global trends in early pregnancy from the point of view of evidence-based medicine are unambiguous: the need for rational diet therapy , intake of folic acid at least 400 mcg/day and potassium iodide 200 mg/day.
After 12-14 weeks of pregnancy, with an inadequate diet, the use of vitamin preparations during pregnancy and lactation is recommended as a way to improve the health of the mother and fetus . Vitamin complexes intended for other groups of the population (including children) are contraindicated for pregnant women!
Medicines during pregnancy
In existing classifications, it is customary to subdivide drugs during pregnancy into groups - safe, relatively safe, relatively unsafe and dangerous.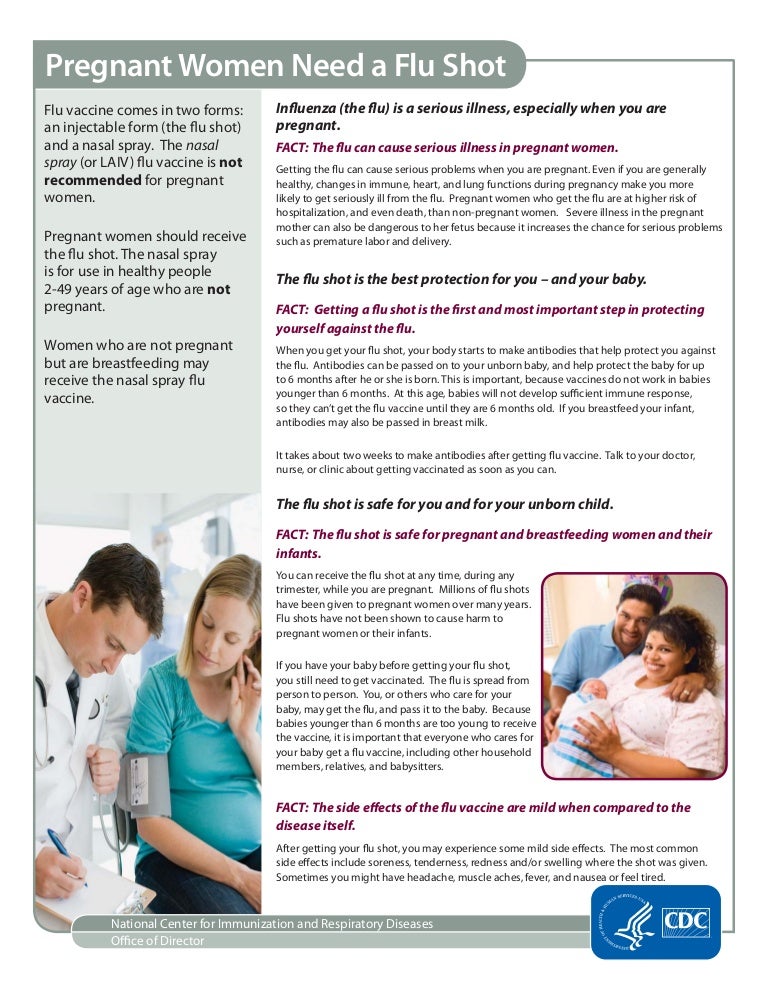 Moreover, the list of drugs is periodically updated.
Moreover, the list of drugs is periodically updated.
- Category A - safe drugs. Controlled trials have shown no risk to the fetus for the first 12 weeks of pregnancy. Regarding them, there is no evidence of a harmful effect on the fetus in late pregnancy. These are folic acid, levothyroxine sodium, paracetamol, magnesium sulfate.
- Category B - relatively safe drugs. Experimental studies have generally not shown their teratogenic effects in animals and children whose mothers took such drugs. These are amoxicillin, heparin, insulin, aspirin, metronidazole (except for the first trimester)
- Category C - relatively unsafe drugs. When testing these drugs on animals, their teratogenic or embryotoxic effects were revealed. Controlled trials have not been conducted or the effect of the drug has not been studied (isoniazid, fluoroquinolones, gentamicin, antidepressants, antiparkinsonian drugs).
 These drugs should only be used if the potential benefit outweighs the potential risk.
These drugs should only be used if the potential benefit outweighs the potential risk. - Caregory D - dangerous drugs. The use of drugs in this group is associated with a certain risk to the fetus, but despite this, it is possible to use the drug for health reasons (anticonvulsants, doxycycline, kanamycin, diclofenac).
- Category X - dangerous drugs that are contraindicated for use.
The teratogenic effect of drugs in this group has been proven, their use is contraindicated during pregnancy, as well as when planning a pregnancy.
Although almost 1000 chemicals are known to be teratogenic in animals, only a few chemicals have been proven to be permanently teratogenic in humans. These include a number of narcotic analgesics, chemotherapeutic drugs (antimetabolites, alkylating agents), anticonvulsants (trimethadione, valproic acid, fenithione, carbamazepine), androgens, warfarin, danazol, lithium, retinoids, thalidomide.
The safest drugs
(Larimore W.L., Petrie K.A., 2000)
| Drug groups | The safest drugs |
| Analgesics | Paracetamol, narcotic analgesics (short courses), NSAIDs (except due date) |
| Antibiotics | Aminopenicillins, macrolides (Vilprafen), azithromycin, cephalosporins, clindamycin, erythromycin, metronidazole (except 1st trimester), penicillins, trimethoprim (except 1st trimester) |
| Antidepressants | Venlafaxine, fluoxetine, trazodone |
| Antidiarrheals | Loperamide |
| Antiemetics | Andacids, doxylamine, prochlorperazine, promethazine, vitamin B |
| Antihypertensives | B-blockers, hydralazine, methyldopa, prazosin |
| Antiparasitics | Permethrin |
| Antituberculous drugs | Ethambutol, isoniazid |
| Antivirals | Amantadine, acyclovir |
| Antihistamines | Cetirizine, loratadine |
| Anti-asthma/anti-allergy products | Epinephrine, inhaled bronchodilators, theophylline |
| Cardiovascular medicines | B-blockers, calcium channel blockers, digoxin, nitroglycerin |
| Constipation products | Bisacodyl, methylcellulose |
| Antidiabetics | Insulin |
| Gastrointestinal drugs | Sucralfate, metoclopramide |
| Thyroid hormones | Levothyroxine, liothyronine |
Terminals
It is very important that every pregnant woman remember that any drug during pregnancy can bring not only benefits, but also considerable harm, therefore, any self-administration during this period is not permissible, since their consequences are unpredictable and in many cases can cause irreparable harm to the developing fetus.
Key words
Anesthesia in a gentle beriod
Answers questions
Sergeev Viktor Mikhailovich
dentist of the network of dental clinics "Smile"
Pregnancy is a long-awaited, and as doctors say, a completely normal physiological state of the female body. However, it is fundamentally different from the usual state of the female body, primarily by changing the hormonal background. The best motto that every woman should be guided by in anticipation of a child is better to prevent than to cure.
What to do if you have a toothache during pregnancy?
Unfortunately, there is no “magic pill” or “guaranteed remedy” for caries. Dental caries is a multifactorial, infectious disease.
The normal growth and development of the fetus during pregnancy depends on the health of the teeth of the expectant mother. The threat posed by untreated caries should not be underestimated.
It is important to visit a dentist when planning a pregnancy, to cure foci of infection.
And during pregnancy, pay more attention to oral hygiene and good nutrition of the expectant mother.
If you still have a toothache during pregnancy, you should contact your dentist as soon as possible.
Therefore, in order for dental treatment in pregnant women to be limited to regular check-ups at the dentist, it is necessary to carefully maintain oral hygiene.
Unified reference telephone
+7 384 234-44-19
Painkillers for pregnant women
Let's say right away that the safest drugs are Paracetamol and Ibuprofen . Here it should only be noted that Ibuprofen is contraindicated in pregnant women in the 3rd trimester (in the 1st and 2nd trimesters it is approved for use). Pain tablets for pregnancy see Table #1 below.
Taking medications, dosages, duration of administration - you need to coordinate with your doctor. Because there may be certain conditions and chronic diseases in the mother's body that can make these drugs less safe than they are, for example, for a healthy pregnant woman.
Because there may be certain conditions and chronic diseases in the mother's body that can make these drugs less safe than they are, for example, for a healthy pregnant woman.
Prenatal antibiotics
Can pregnant women drink an antibiotic, and which antibiotics can pregnant women take?
In the treatment of pregnant women, the drugs of choice are beta-lactam antibiotics, for example, a group of penicillins. In Table No. 1 you will see a list of the safest antibiotics (safety category "B").
Antibiotics of the following groups are prohibited for use: tetracyclines and fluoroquinolones. With caution (undesirable, but in some cases necessary) - sulfonamides and some representatives of aminoglycosides.
IMPORTANT: It is best to discuss this with your attending OB/GYN before starting antibiotics.
Anesthesia during lactation
Medicines and breastfeeding
When deciding on the appointment of the drug
to a nursing woman, the doctor takes into account:
- Drug toxicity index
- Dose and duration of administration of the drug
- Breastfeeding age
- Amount of milk consumed
- Effect of the drug on lactation
Ways to reduce the amount of drug
passing through mother's milk to the baby
- Suspension of breastfeeding
- Refusal to feed the child during peak plasma concentrations of the drug
- Taking the drug during the longest sleep of the child
What antibiotics can be used for pregnant and lactating women, as well as painkillers and injections for dental treatment - are listed in Table No.1 .
Table 1.
Medicines used in dentistry during pregnancy and lactation.
| Medicine | Pregnancy risk category * | Risk category for lactation * |
|---|---|---|
| Local anesthetics (injections for dental treatment) | ||
| Lidocaine | In (maybe) | Safe |
| mepivacaine | C (unwanted) | Safe |
| Analgesics | ||
| Paracetamol | In (maybe) | Safe |
| Ibuprofen (1st and 2nd trimesters) | In (maybe) | Safe |
| Ibuprofen (3rd trimester) | D (absolutely impossible) | Safe |
| Antibiotics | ||
| Penicillins | In (maybe) | Safe |
| Cephalosporins | In (maybe) | Safe |
| Clindamycin | In (maybe) | Safe |
| Metronisazole | In (maybe) | Safe |
* - in accordance with the classification of the Food and Drug Administration (FDA, USA). Description of risk categories "B", "C", "D" is given below Description of risk categories "B", "C", "D" is given below | ||
What are drug safety categories?
Today, the safety of drugs for the fetus is classified according to the recommendations of the experts of the Food and Drug Administration.
This classification was developed in the USA and is generally followed by physicians in all countries. You can see the drugs of choice for emergency dental interventions in pregnant and lactating women in Table No. 1 .
The level of drug safety is determined by the risk categories, which are denoted by Latin letters A, B, C, D:
-
Category B drugs - Considered to be very safe.
-
Category C drugs - not recommended.
-
Category D drugs - dangerous to use (use only if the possible benefit outweighs the possible harm, and if there is no safer similar drug).
Anesthesia for high and low blood pressure
If the patient has high blood pressure or cardiac dysfunction (heart disease, heart rhythm disturbances, heart failure, etc.