Is it possible to get mastitis while pregnant
Infections in Pregnancy: Mastitis | Healthline
Infections in Pregnancy: Mastitis | HealthlineMedically reviewed by Janine Kelbach, RNC-OB — By the Healthline Medical Network on March 15, 2012
What Is Mastitis?
Mastitis is a breast infection. It commonly develops in breast-feeding women during the first few weeks after delivery. Occasionally, this infection occurs in breast-feeding women several months after the baby is born.
Mastitis develops when bacteria (usually staphylococci or streptococci) from the baby’s mouth enter into the breast through the mother’s nipple. This causes an infection and inflammation in and around the milk-producing glands. Typically, a woman with mastitis develops a fever and notices pain and redness in one area of the breast. She is likely to develop flu-like body aches and fatigue as well.
How Is Mastitis Diagnosed?
Mastitis is often easy to diagnose. Reporting the symptoms to your doctor should be enough for them to identify the problem and prescribe treatment. In fact, laboratory tests are seldom needed.
What Are the Complications of Mastitis?
If not recognized or treated, simple mastitis may progress into a collection of pus called an abscess. Your doctor will suspect an abscess if they find a lump beneath the area of redness on your skin.
The formation of an abscess is rare. Most women see their doctor when they experience breast pain and fever. However, it’s important to identify an abscess because it requires different treatment than mastitis.
What Are the Usual Treatments for Mastitis?
Mastitis typically responds to antibiotic treatment within 24 hours. Your doctor may prescribe the antibiotic dicloxacillin. If you’re allergic to penicillin, alternatives include erythromycin (Ery-Tab) or clindamycin (Cleocin). Also, you can clear the infection faster with continued breast-feeding or pumping. This will help remove milk from your breast.
If your mastitis doesn’t improve within 48 to 72 hours, you may develop an abscess. In these cases, treatment is more aggressive. A surgeon must lance (by incision) and drain the abscess. This may require a trip to the emergency or operating room. You may also need antibiotics. Depending on the severity of your infection, you may be given the antibiotics intravenously rather than orally.
In these cases, treatment is more aggressive. A surgeon must lance (by incision) and drain the abscess. This may require a trip to the emergency or operating room. You may also need antibiotics. Depending on the severity of your infection, you may be given the antibiotics intravenously rather than orally.
After the abscess is lanced, a sample of your breast tissue is sent to the laboratory. This will help doctors identify the bacteria that caused the infection. Doctors may also examine the sample to make sure cancer isn’t present. However, cancer is unusual in young women with mastitis.
What is the Outlook for Mastitis?
Antibiotics are usually effective when treating mastitis. However, in some cases antibiotic-resistant infections can be difficult to treat. In these cases, several antibiotics or probiotics may be prescribed.
Start a medication plan as soon as possible to reduce your risk of forming an abscess. If you follow treatment directions carefully, your case of mastitis will likely clear up within several days.
How Can You Prevent Mastitis?
Many new mothers find it helpful to speak with a lactation consultant before starting breast-feeding. A lactation consultant can give you information on how to properly breast-feed your baby and avoid breast-feeding problems such as mastitis.
Here are some other tips for reducing your risk of getting mastitis:
- Make sure you fully drain the milk from your breasts while breast-feeding
- Allow your baby to completely empty one breast before switching to another
- Change your breast-feeding position each time
- Check that your baby latches on properly during feedings
Q:
Can mastitis become a recurring problem during breast-feeding?
Anonymous patient
A:
Mastitis may reoccur for several reasons. Some of the factors include:
- – sore nipples or plugged ducts
- – a history of breast surgery or lumps
- – stress or fatigue
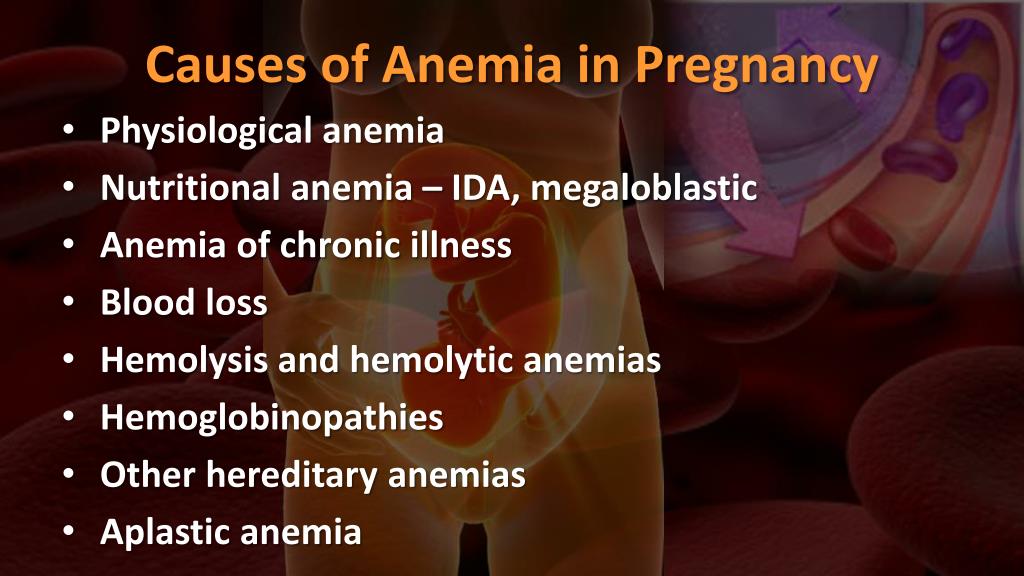
- – low iron (anemia)
- – breasts that aren’t fully drained (engorgement)
- – tight clothing (slows the flow of milk)
- – cigarette smoking (prevents the breast from emptying completely)
- – sleep position (may put too much pressure on the breast)
- – not finishing antibiotics from the original infection
Janine Kelbach RNC-OB Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
All content is strictly informational and should not be considered medical advice.
Last medically reviewed on February 18, 2016
- Parenthood
- Health & Well-being
4 sourcescollapsed
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Arroyo, R., Martín, V., Maldonado, A., Jiménez, E., Fernández, L., & Rodríguez, J. M. (2010). Treatment of infectious mastitis during lactation: Antibiotics versus oral administration of lactobacilli isolated from breast milk. Clinical Infectious Diseases, 50(12), 1551-1558. Retrieved from
cid.oxfordjournals.org/content/50/12/1551.full - Mayo Clinic Staff. (2015, June 12). Mastitis. (2015, June 12)
mayoclinic. org/diseases-conditions/mastitis/basics/definition/con-20026633
org/diseases-conditions/mastitis/basics/definition/con-20026633 - Scott, J. A., Robertson, M., Fitzpatrick, J., Knight, C., & Mulholland, S. (2008). Occurrence of lactational mastitis and medical management: A prospective cohort study in Glasgow. International Breastfeeding Journal, 3, 21.
doi.org/10.1186/1746-4358-3-21 - What can I do about my repeated cases of mastitis? (2016, January 9)
llli.org/faq/repeatmastitis.html
FEEDBACK:
Medically reviewed by Janine Kelbach, RNC-OB — By the Healthline Medical Network on March 15, 2012
Read this next
Mastitis
Medically reviewed by Michael Weber, MD
Mastitis is an inflammation of the breast tissue usually caused by infection. It occurs almost always in breast-feeding women. Find out about symptoms…
READ MORE
What Causes Lumps in Breasts of Breastfeeding Women?
Medically reviewed by Karen Gill, M.
 D.
D.Lumps in the breasts of breastfeeding women are common. We explore seven possible causes for lumps and discuss home remedies and other treatment…
READ MORE
All About Breast Lymphoma: A Rare Form of Non-Hodgkin’s Lymphoma
Breast lymphoma is not breast cancer. It’s a rare type of non-Hodgkin's lymphoma, a cancer of the lymphatic system. Learn more.
READ MORE
Breast Self-Exam
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
A breast self-exam is a screening technique you can do at home to check for breast lumps. This exam can screen for tumors, cysts, or other…
READ MORE
When to Worry About Breast Pain
Most women will experience breast pain at some point in their lives, but only a few will be diagnosed with cancer.
 Learn the causes and when to visit…
Learn the causes and when to visit…READ MORE
What Can Cause Large Areolas and Is This Normal?
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
The areola is the colored area around your nipple. Like breasts themselves, areolas come in all shapes, sizes, and colors. Many women worry that their…
READ MORE
Lipomas in the Breast: What You Need to Know
Medically reviewed by Meredith Goodwin, MD, FAAFP
Lipomas are common fatty tumors of the breast. They are generally harmless, but doctors will perform an exam to be sure the lump is a lipoma.
READ MORE
Why Are My Nipples Itchy?
Medically reviewed by Alana Biggers, M.D., MPH
Find out all you need to know about what causes an itchy breast or nipple, what treatments are available, and when you should seek medical help.

READ MORE
Infections in Pregnancy: Mastitis | Healthline
Infections in Pregnancy: Mastitis | HealthlineMedically reviewed by Janine Kelbach, RNC-OB — By the Healthline Medical Network on March 15, 2012
What Is Mastitis?
Mastitis is a breast infection. It commonly develops in breast-feeding women during the first few weeks after delivery. Occasionally, this infection occurs in breast-feeding women several months after the baby is born.
Mastitis develops when bacteria (usually staphylococci or streptococci) from the baby’s mouth enter into the breast through the mother’s nipple. This causes an infection and inflammation in and around the milk-producing glands. Typically, a woman with mastitis develops a fever and notices pain and redness in one area of the breast. She is likely to develop flu-like body aches and fatigue as well.
How Is Mastitis Diagnosed?
Mastitis is often easy to diagnose. Reporting the symptoms to your doctor should be enough for them to identify the problem and prescribe treatment. In fact, laboratory tests are seldom needed.
Reporting the symptoms to your doctor should be enough for them to identify the problem and prescribe treatment. In fact, laboratory tests are seldom needed.
What Are the Complications of Mastitis?
If not recognized or treated, simple mastitis may progress into a collection of pus called an abscess. Your doctor will suspect an abscess if they find a lump beneath the area of redness on your skin.
The formation of an abscess is rare. Most women see their doctor when they experience breast pain and fever. However, it’s important to identify an abscess because it requires different treatment than mastitis.
What Are the Usual Treatments for Mastitis?
Mastitis typically responds to antibiotic treatment within 24 hours. Your doctor may prescribe the antibiotic dicloxacillin. If you’re allergic to penicillin, alternatives include erythromycin (Ery-Tab) or clindamycin (Cleocin). Also, you can clear the infection faster with continued breast-feeding or pumping. This will help remove milk from your breast.
This will help remove milk from your breast.
If your mastitis doesn’t improve within 48 to 72 hours, you may develop an abscess. In these cases, treatment is more aggressive. A surgeon must lance (by incision) and drain the abscess. This may require a trip to the emergency or operating room. You may also need antibiotics. Depending on the severity of your infection, you may be given the antibiotics intravenously rather than orally.
After the abscess is lanced, a sample of your breast tissue is sent to the laboratory. This will help doctors identify the bacteria that caused the infection. Doctors may also examine the sample to make sure cancer isn’t present. However, cancer is unusual in young women with mastitis.
What is the Outlook for Mastitis?
Antibiotics are usually effective when treating mastitis. However, in some cases antibiotic-resistant infections can be difficult to treat. In these cases, several antibiotics or probiotics may be prescribed.
Start a medication plan as soon as possible to reduce your risk of forming an abscess. If you follow treatment directions carefully, your case of mastitis will likely clear up within several days.
If you follow treatment directions carefully, your case of mastitis will likely clear up within several days.
How Can You Prevent Mastitis?
Many new mothers find it helpful to speak with a lactation consultant before starting breast-feeding. A lactation consultant can give you information on how to properly breast-feed your baby and avoid breast-feeding problems such as mastitis.
Here are some other tips for reducing your risk of getting mastitis:
- Make sure you fully drain the milk from your breasts while breast-feeding
- Allow your baby to completely empty one breast before switching to another
- Change your breast-feeding position each time
- Check that your baby latches on properly during feedings
Q:
Can mastitis become a recurring problem during breast-feeding?
Anonymous patient
A:
Mastitis may reoccur for several reasons. Some of the factors include:
- – sore nipples or plugged ducts
- – a history of breast surgery or lumps
- – stress or fatigue
- – low iron (anemia)
- – breasts that aren’t fully drained (engorgement)
- – tight clothing (slows the flow of milk)
- – cigarette smoking (prevents the breast from emptying completely)
- – sleep position (may put too much pressure on the breast)
- – not finishing antibiotics from the original infection
Janine Kelbach RNC-OB Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
All content is strictly informational and should not be considered medical advice.
Last medically reviewed on February 18, 2016
- Parenthood
- Health & Well-being
4 sourcescollapsed
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Arroyo, R., Martín, V., Maldonado, A., Jiménez, E., Fernández, L., & Rodríguez, J. M. (2010). Treatment of infectious mastitis during lactation: Antibiotics versus oral administration of lactobacilli isolated from breast milk. Clinical Infectious Diseases, 50(12), 1551-1558. Retrieved from
cid.oxfordjournals.org/content/50/12/1551.full - Mayo Clinic Staff. (2015, June 12). Mastitis. (2015, June 12)
mayoclinic. org/diseases-conditions/mastitis/basics/definition/con-20026633
org/diseases-conditions/mastitis/basics/definition/con-20026633 - Scott, J. A., Robertson, M., Fitzpatrick, J., Knight, C., & Mulholland, S. (2008). Occurrence of lactational mastitis and medical management: A prospective cohort study in Glasgow. International Breastfeeding Journal, 3, 21.
doi.org/10.1186/1746-4358-3-21 - What can I do about my repeated cases of mastitis? (2016, January 9)
llli.org/faq/repeatmastitis.html
FEEDBACK:
Medically reviewed by Janine Kelbach, RNC-OB — By the Healthline Medical Network on March 15, 2012
Read this next
Mastitis
Medically reviewed by Michael Weber, MD
Mastitis is an inflammation of the breast tissue usually caused by infection. It occurs almost always in breast-feeding women. Find out about symptoms…
READ MORE
What Causes Lumps in Breasts of Breastfeeding Women?
Medically reviewed by Karen Gill, M.
D.
Lumps in the breasts of breastfeeding women are common. We explore seven possible causes for lumps and discuss home remedies and other treatment…
READ MORE
All About Breast Lymphoma: A Rare Form of Non-Hodgkin’s Lymphoma
Breast lymphoma is not breast cancer. It’s a rare type of non-Hodgkin's lymphoma, a cancer of the lymphatic system. Learn more.
READ MORE
Breast Self-Exam
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
A breast self-exam is a screening technique you can do at home to check for breast lumps. This exam can screen for tumors, cysts, or other…
READ MORE
When to Worry About Breast Pain
Most women will experience breast pain at some point in their lives, but only a few will be diagnosed with cancer.
 Learn the causes and when to visit…
Learn the causes and when to visit…READ MORE
What Can Cause Large Areolas and Is This Normal?
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
The areola is the colored area around your nipple. Like breasts themselves, areolas come in all shapes, sizes, and colors. Many women worry that their…
READ MORE
Lipomas in the Breast: What You Need to Know
Medically reviewed by Meredith Goodwin, MD, FAAFP
Lipomas are common fatty tumors of the breast. They are generally harmless, but doctors will perform an exam to be sure the lump is a lipoma.
READ MORE
Why Are My Nipples Itchy?
Medically reviewed by Alana Biggers, M.D., MPH
Find out all you need to know about what causes an itchy breast or nipple, what treatments are available, and when you should seek medical help.
READ MORE
Mastitis – Medscan
blog articleWhat is mastitis? What are the symptoms of the disease? How to recognize the pathology and take measures to prevent its occurrence? Questions that do not lose their relevance. Mastitis is an inflammation of the mammary glands that may or may not be accompanied by an infection. In most cases, the disease is directly related to the process of lactation in a woman, therefore, in medical practice, another name for the pathology is lactational mastitis. In the absence of timely treatment and the development of complications, mastitis can lead to death, which is why it is so important to consult a doctor when the first signs and symptoms of inflammation are detected.
According to studies, mastitis in most cases develops during the first 2-3 weeks after the birth of a child. However, the disease can also occur at other stages of lactation. About 10-15% of the disease occurs in non-nursing women and 0. 5-1% in pregnant women. Mastitis usually affects one breast, but the inflammatory process can also affect the second mammary gland (bilateral mastitis).
5-1% in pregnant women. Mastitis usually affects one breast, but the inflammatory process can also affect the second mammary gland (bilateral mastitis).
Causes of mastitis
To date, experts identify two main factors that contribute to the development of the disease:
- milk stasis;
- infection.
If we talk about lactational mastitis, then the root cause of the pathology is milk stagnation, which occurs due to improper attachment of the newborn to the breast, minimal emptying of the mammary glands, blockage of the ducts. Other conditions that contribute to the development of mastitis are also recognized as excessive milk secretion and breastfeeding of multiple twin babies.
Infectious mastitis, as the name implies, occurs due to excessive colonization of pathological microorganisms. In most cases, the causative agent of this disease is Staphylococcus aureus, which can penetrate the tissues of the breast through cracks in the nipples when breastfeeding or expressing milk.
Increase the risk of developing mastitis and other factors, which can be ranked:
- concomitant diseases causing a weakening of the woman's immunity;
- difficult delivery and late attachment of the baby to the breast;
- postpartum complications;
- mastopathy;
- gross cicatricial changes in tissues after surgery, for example, to remove benign neoplasms;
- improper care of the mammary glands.
Symptoms of the disease
The symptoms of mastitis are as follows:
- Gland engorgement - the woman experiences chest discomfort and pain. It looks swollen, the skin acquires a characteristic luster. There may be hyperemia (reddening of the skin), which has blurry edges. The nipple stretches, becomes flat, which makes it difficult for the baby to suckle the breast due to the impossibility of grabbing. There is a fever that goes away within 24 hours.
- Obstruction of the milk ducts manifests itself in the form of the formation of painful nodes, the skin over which acquires a characteristic red hue.
 In some cases, a white spot forms on the nipple, which causes a characteristic severe pain when sucking.
In some cases, a white spot forms on the nipple, which causes a characteristic severe pain when sucking. - An increase in the venous network due to a violation of the outflow of milk and the accumulation of tissue fluid.
Symptoms of mastitis also directly depend on the stage of progress of the disease. With a serous form of mastitis, a woman may experience pain in one of the mammary glands; palpation may reveal a dense formation that has clear boundaries and good mobility. The outflow of milk is free, therefore, when the breast is empty, lactostasis can pass without medical help within 1-2 days. But despite this, doctors recommend that patients in the event of such signs of mastitis seek help from specialists. Only timely assistance will help to avoid complications and the transition of the disease to an infiltrative or destructive form, which require inpatient treatment, often surgically.
Diagnosis of mastitis
In most cases, diagnosing mastitis is not difficult for a doctor. To do this, it is enough to know the patient's complaints and conduct a visual examination. To clarify the clinical diagnosis, laboratory tests may be prescribed:
To do this, it is enough to know the patient's complaints and conduct a visual examination. To clarify the clinical diagnosis, laboratory tests may be prescribed:
- UAC and OAM;
- bacteriological analysis of milk from two mammary glands;
- cytological analysis of milk;
- test for reductase activity and determination of the pH level of breast milk.
Of the functional examination methods, an ultrasound examination of the mammary gland can be performed if the symptoms of mastitis indicate a destructive form. Mammography may be recommended to clarify the diagnosis and for the differential diagnosis of cancer.
Treatment of the disease
If we talk about the treatment of this pathology, then both a conservative method and a radical one, which involves the opening of abscesses, can be applied. Conservative treatment of mastitis is indicated in cases where:
- the patient feels well;
- breast inflammation lasts less than 3 days;
- the temperature did not rise above 37.
 5 degrees;
5 degrees; - no symptoms suggestive of a purulent abscess;
- moderate soreness;
- UAC indicators are within the normal range.
If other symptoms of mastitis join, and treatment does not help, then an urgent surgical operation is necessary.
Preventive measures
Is there a cure for mastitis? Undoubtedly. A woman should pay special attention to the condition of the mammary glands and, at the first signs of milk stasis, take measures to prevent stagnation. The correct technique of applying the baby to the breast is also important, since in the absence of cracks and other damage to the nipples, the risk of infection penetrating into the mammary gland tissues is minimal.
When the first symptoms of mastitis appear, you should seek help from a specialist. The diagnostic centers of Medscan.rf are equipped with modern premium-class equipment, thanks to which it is possible to make a clinical diagnosis in a matter of hours, which is the key to the health and successful motherhood of every woman.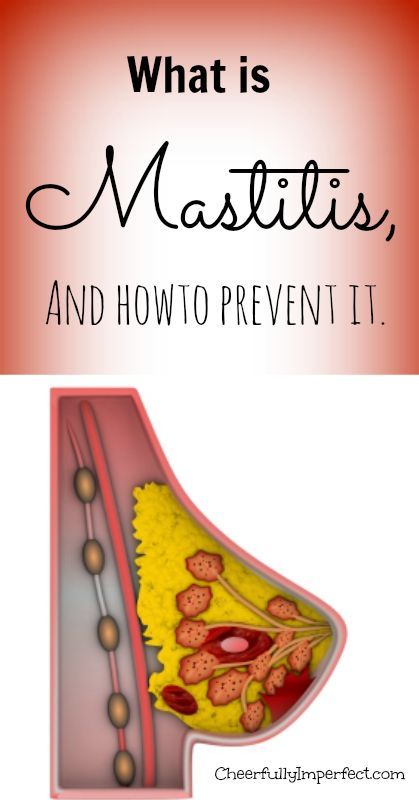
22920
Author: Medscan
Might be interesting...
Skin neoplasms
Tumors and tumor-like skin lesions are the most common human neoplasms.
Read more
Lymphedema of the extremities
Lymphedema of the extremities is a pathological condition that is accompanied by swelling of the soft tissues in the affected area. The lower extremities are most commonly affected.
Read more
Craniopharyngioma
Craniopharyngioma is a rare type of brain tumor. It is localized in the pituitary gland.
Read more
No referral for research?
Still have questions?
Make an appointment with a doctor or ask
for the necessary information by phone.
Make an appointment with a doctor
Return to the list
Non-lactational mastitis
« Back
Non-lactational mastitis 08/01/2019 18:47
This disease is in no way associated with breastfeeding, therefore it can develop in patients of absolutely any age
. Unlike lactational mastitis, it has nothing to do with breastfeeding. That is why this pathology can develop in patients of absolutely any age.
The main cause of its occurrence are all the same pathogens. More often Staphylococcus aureus and Streptococcus aureus. They live in the body of everyone, but under certain conditions their number increases, and the inflammatory process begins.
The most common causes of non-lactational mastitis:
- Reduced immunity.
Yes, banal hypothermia can affect not only the respiratory or urinary organs, but also the mammary gland.
- Surgery, especially plastic surgery.
This factor is often associated with non-compliance with the rules of asepsis and antisepsis during the surgical intervention itself, as well as in the early postoperative period.
- Hormonal disorders.
Non-lactational mastitis is very often a concomitant manifestation of the three main stressful periods for the female body - adolescence 14-18 years (ovaries synthesize a lot of estrogen, and immunity decreases due to active restructuring of the body), reproductive 19-35 years (active proliferation of connective tissue and glandular hypertrophy) and premenopause (estrogen concentration and immunity decrease, sensitivity to microbes and bacteria increases.).
- The presence of foci of chronic infection in the body.
The mammary gland, like any other organ, has a connection through the lymphatic and circulatory system with the entire body. Thus, it costs nothing for the pathogen to get with the blood flow from the source of infection to the mammary gland, especially when the defense mechanisms are reduced.
Thus, it costs nothing for the pathogen to get with the blood flow from the source of infection to the mammary gland, especially when the defense mechanisms are reduced.
- Breast injuries, including nipple piercing.
Often, mastitis in a non-nursing woman begins due to the penetration of an infectious agent into the breast tissue through a nipple puncture, that is, during piercing.
- Wearing the wrong bra.
An incorrectly sized and shaped bra can lead to stagnant processes in the mammary glands, and hence the concentration of pathogenic bacteria.
Symptoms of mastitis
Symptoms of non-lactational mastitis in non-lactating women can vary greatly depending on whether the disease is acute or chronic.
In the first case, the patient develops severe pain in the mammary gland, which has no clear localization. The breast itself may turn red and become swollen. As the disease progresses, the pain moves to the axillary region. In this case, an increase in the size of the lymph nodes is often observed. Body temperature in acute mastitis often increases to 39degrees, the patient complains of chills, weakness, dizziness, nausea and general malaise. Acute non-lactational mastitis requires an urgent referral to a mammologist and surgeon.
As the disease progresses, the pain moves to the axillary region. In this case, an increase in the size of the lymph nodes is often observed. Body temperature in acute mastitis often increases to 39degrees, the patient complains of chills, weakness, dizziness, nausea and general malaise. Acute non-lactational mastitis requires an urgent referral to a mammologist and surgeon.
Symptoms of mastitis in a non-nursing woman, if the disease is chronic, are much less pronounced. The general condition in this case will be satisfactory. In the area of inflammation, there may be retraction of the skin, under which there is a dense infiltrate.
Mastitis diagnosis:
- complete blood and urine test
- Ultrasound of the mammary glands and regional lymph nodes
- biopsy
- inoculation of purulent discharge from the nipple or fistula on nutrient media
Treatment
The key tasks of a doctor are to suppress the growth and reproduction of pathological microorganisms, restore immunity, remove intoxication, prevent possible complications of therapy and (if necessary) sanitize the focus of infection.