Nuchal screening test
Nuchal translucency test Information | Mount Sinai
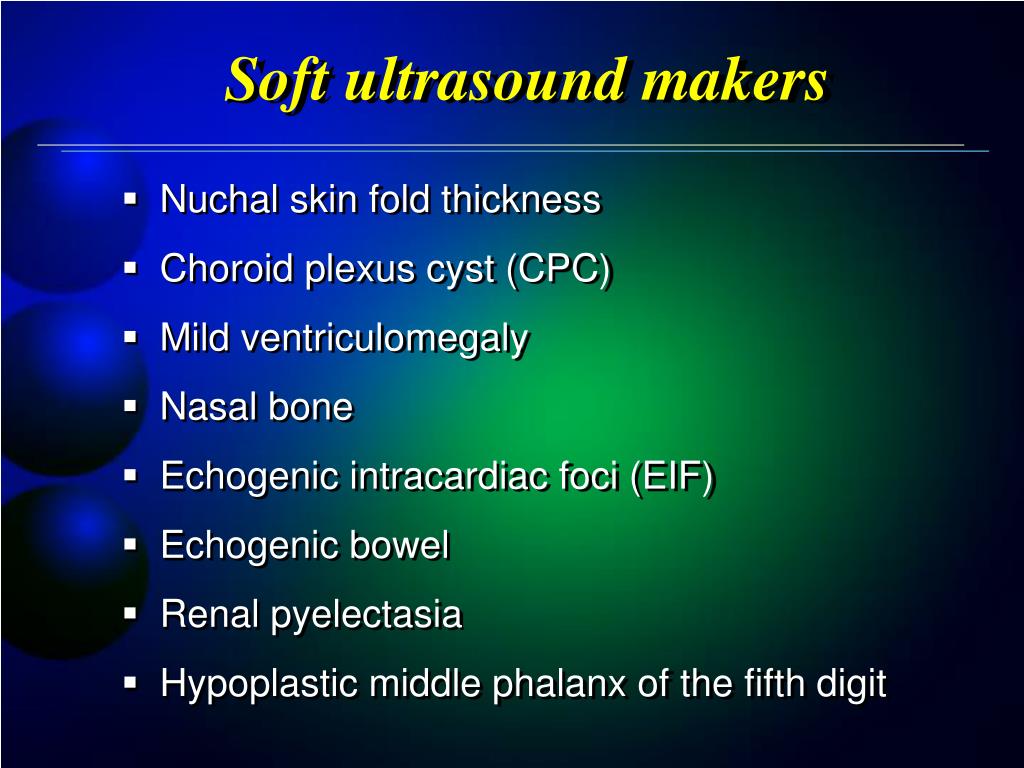
Nuchal translucency screening; NT; Nuchal fold test; Nuchal fold scan; Prenatal genetic screening; Down syndrome - nuchal translucency
The nuchal translucency test measures the nuchal fold thickness. This is an area of tissue at the back of an unborn baby's neck. Measuring this thickness helps assess the risk for Down syndrome and other genetic problems in the baby.
How the Test is Performed
Your health care provider uses abdominal ultrasound (not vaginal) to measure the nuchal fold. All unborn babies have some fluid at the back of their neck. In a baby with Down syndrome or other genetic disorders, there is more fluid than normal. This makes the space look thicker.
A blood test of the mother is also done. Together, these two tests will tell if the baby could have Down syndrome or another genetic disorder.
How to Prepare for the Test
Having a full bladder will give the best ultrasound picture. You may be asked to drink 2 to 3 glasses of liquid an hour before the test. DO NOT urinate before your ultrasound.
How the Test will Feel
You may have some discomfort from pressure on your bladder during the ultrasound. The gel used during the test may feel slightly cold and wet. You will not feel the ultrasound waves.
The gel used during the test may feel slightly cold and wet. You will not feel the ultrasound waves.
Why the Test is Performed
Your provider may advise this test to screen your baby for Down syndrome. Many pregnant women decide to have this test.
Nuchal translucency is usually done between the 11th and 14th week of pregnancy. It can be done earlier in pregnancy than amniocentesis. This is another test that checks for birth defects.
Normal Results
A normal amount of fluid in the back of the neck during ultrasound means it is very unlikely your baby has Down syndrome or another genetic disorder.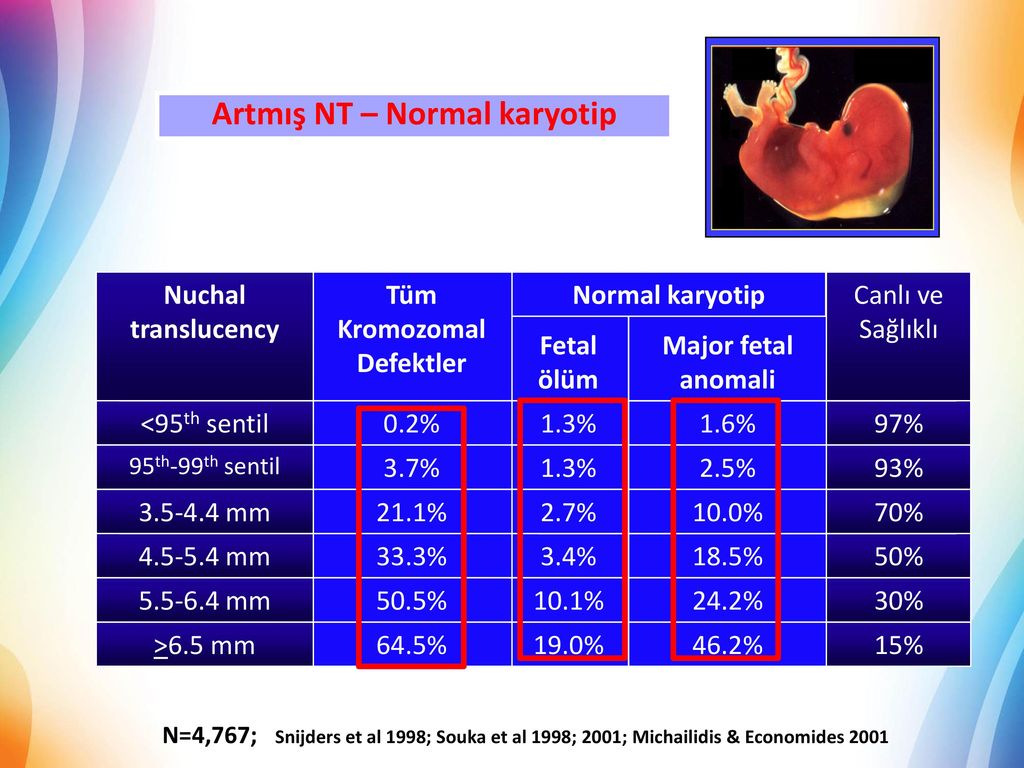
Nuchal translucency measurement increases with gestational age. This is the period between conception and birth. The higher the measurement compared to babies the same gestational age, the higher the risk is for certain genetic disorders.
The measurements below are considered low risk for genetic disorders:
- At 11 weeks -- up to 2 mm
- At 13 weeks, 6 days -- up to 2.8 mm
What Abnormal Results Mean
More fluid than normal in the back of the neck means there is a higher risk for Down syndrome, trisomy 18, trisomy 13, Turner syndrome, or congenital heart disease. But it does not tell for certain that the baby has Down syndrome or another genetic disorder.
If the result is abnormal, other tests can be done. Most of the time, the other test done is amniocentesis.
Risks
There are no known risks from ultrasound.
Driscoll DA, Simpson JL. Genetic screening and diagnosis. In: Landon MB, Galan HL, Jauniaux ERM, et al, eds. Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Philadelphia, PA: Elsevier; 2021:chap 10.
Walsh JM, D'Alton ME. Nuchal translucency. In: Copel JA, D'Alton ME, Feltovich H, et al, eds. Obstetric Imaging: Fetal Diagnosis and Care. 2nd ed. Philadelphia, PA: Elsevier; 2018:chap 45.
2nd ed. Philadelphia, PA: Elsevier; 2018:chap 45.
Last reviewed on: 3/31/2020
Reviewed by: John D. Jacobson, MD, Professor of Obstetrics and Gynecology, Loma Linda University School of Medicine, Loma Linda Center for Fertility, Loma Linda, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
First trimester screening - Mayo Clinic
Overview
Nuchal translucency measurement
Nuchal translucency measurement
First trimester screening includes an ultrasound exam to measure the size of the clear space in the tissue at the back of a baby's neck (nuchal translucency). In Down syndrome, the nuchal translucency measurement is abnormally large — as shown on the left in the ultrasound image of an 11-week fetus. For comparison, the ultrasound image on the right shows an 11-week fetus with a normal nuchal translucency measurement.
First trimester screening is a prenatal test that offers early information about a baby's risk of certain chromosomal conditions, specifically, Down syndrome (trisomy 21) and extra sequences of chromosome 18 (trisomy 18).
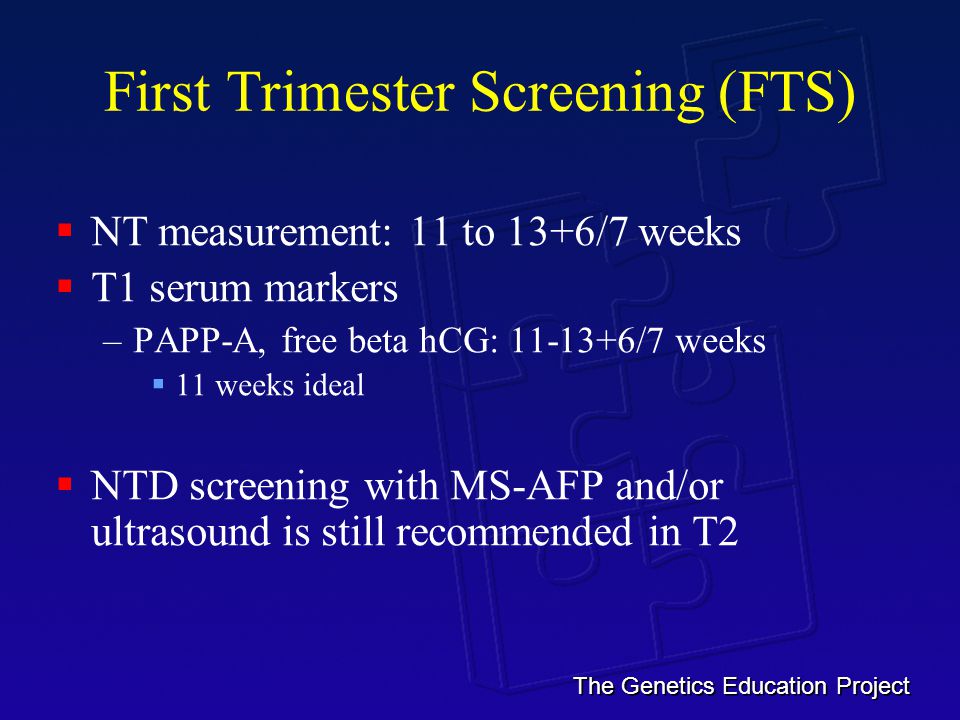
First trimester screening, also called the first trimester combined test, has two steps:
- A blood test to measure levels of two pregnancy-specific substances in the mother's blood — pregnancy-associated plasma protein-A (PAPP-A) and human chorionic gonadotropin (HCG)
- An ultrasound exam to measure the size of the clear space in the tissue at the back of the baby's neck (nuchal translucency)
Typically, first trimester screening is done between weeks 11 and 14 of pregnancy.
Using your age and the results of the blood test and the ultrasound, your health care provider can gauge your risk of carrying a baby with Down syndrome or trisomy 18.
If results show that your risk level is moderate or high, you might choose to follow first trimester screening with another test that's more definitive.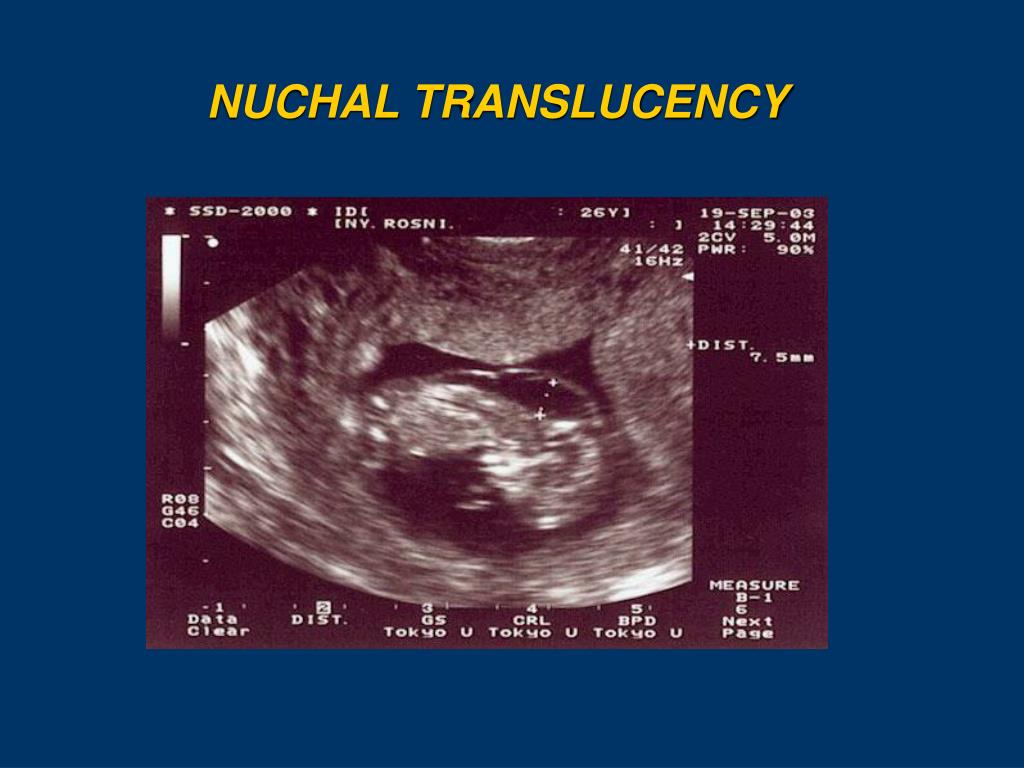
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Obstetricks
Why it's done
First trimester screening is done to evaluate your risk of carrying a baby with Down syndrome. The test also provides information about the risk of trisomy 18.
Down syndrome causes lifelong impairments in mental and social development, as well as various physical concerns. Trisomy 18 causes more severe delays and is often fatal by age 1.
First trimester screening doesn't evaluate the risk of neural tube defects, such as spina bifida.
Because first trimester screening can be done earlier than most other prenatal screening tests, you'll have the results early in your pregnancy. This will give you more time to make decisions about further diagnostic tests, the course of the pregnancy, medical treatment and management during and after delivery. If your baby has a higher risk of Down syndrome, you'll also have more time to prepare for the possibility of caring for a child who has special needs.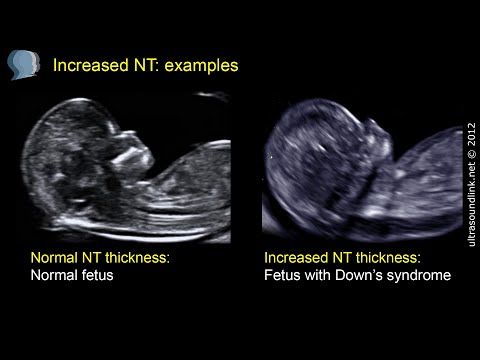
Other screening tests can be done later in pregnancy. An example is the quad screen, a blood test that's typically done between weeks 15 and 20 of pregnancy. The quad screen can evaluate your risk of carrying a baby with Down syndrome or trisomy 18, as well as neural tube defects, such as spina bifida. Some health care providers choose to combine the results of first trimester screening with the quad screen. This is called integrated screening. This can improve the detection rate of Down syndrome.
First trimester screening is optional. Test results indicate only whether you have an increased risk of carrying a baby with Down syndrome or trisomy 18, not whether your baby actually has one of these conditions.
Before the screening, think about what the results will mean to you. Consider whether the screening will be worth any anxiety it might cause, or whether you'll manage your pregnancy differently depending on the results. You might also consider what level of risk would be enough for you to choose a more invasive follow-up test.
More Information
- Prenatal testing: Quick guide to common tests
Request an Appointment at Mayo Clinic
Risks
First trimester screening is a routine prenatal screening test. The screening poses no risk of miscarriage or other pregnancy complications.
How you prepare
You don't need to do anything special to prepare for first trimester screening. You can eat and drink normally before both the blood test and the ultrasound exam.
What you can expect
First trimester screening includes a blood draw and an ultrasound exam.
During the blood test, a member of your health care team takes a sample of blood by inserting a needle into a vein in your arm. The blood sample is sent to a lab for analysis. You can return to your usual activities immediately.
For the ultrasound exam, you'll lie on your back on an exam table. Your health care provider or an ultrasound technician will place a transducer — a small plastic device that sends and receives sound waves — over your abdomen. The reflected sound waves will be digitally converted into images on a monitor. Your health care provider or the technician will use these images to measure the size of the clear space in the tissue at the back of your baby's neck.
The reflected sound waves will be digitally converted into images on a monitor. Your health care provider or the technician will use these images to measure the size of the clear space in the tissue at the back of your baby's neck.
The ultrasound doesn't hurt, and you can return to your usual activities immediately.
Results
Your health care provider will use your age and the results of the blood test and ultrasound exam to gauge your risk of carrying a baby with Down syndrome or trisomy 18. Other factors — such as a prior Down syndrome pregnancy — also might affect your risk.
First trimester screening results are given as positive or negative and also as a probability, such as a 1 in 250 risk of carrying a baby with Down syndrome.
First trimester screening correctly identifies about 85 percent of women who are carrying a baby with Down syndrome. About 5 percent of women have a false-positive result, meaning that the test result is positive but the baby doesn't actually have Down syndrome.
When you consider your test results, remember that first trimester screening indicates only your overall risk of carrying a baby with Down syndrome or trisomy 18. A low-risk result doesn't guarantee that your baby won't have one of these conditions. Likewise, a high-risk result doesn't guarantee that your baby will be born with one of these conditions.
If you have a positive test result, your health care provider and a genetics professional will discuss your options, including additional testing. For example:
- Prenatal cell-free DNA (cfDNA) screening. This is a sophisticated blood test that examines fetal DNA in the maternal bloodstream to determine whether your baby is at risk of Down syndrome, extra sequences of chromosome 13 (trisomy 13) or extra sequences of chromosome 18 (trisomy 18). Some forms of cfDNA screening also screen for other chromosome problems and provide information about fetal sex. A normal result might eliminate the need for a more invasive prenatal diagnostic test.

- Chorionic villus sampling (CVS). CVS can be used to diagnose chromosomal conditions, such as Down syndrome. During CVS, which is usually done during the first trimester, a sample of tissue from the placenta is removed for testing. CVS poses a small risk of miscarriage.
- Amniocentesis. Amniocentesis can be used to diagnose both chromosomal conditions, such as Down syndrome, and neural tube defects, such as spina bifida. During amniocentesis, which is usually done during the second trimester, a sample of amniotic fluid is removed from the uterus for testing. Like CVS, amniocentesis poses a small risk of miscarriage.
Your health care provider or a genetic counselor will help you understand your test results and what the results mean for your pregnancy.
By Mayo Clinic Staff
Related
Products & Services
what is it, why, when and how is the second pregnancy screening done
June 3, 2020
240722
0
share
Contents
What is 3rd Trimester Screening
Indications for 3rd Trimester Ultrasound Screening
What Your Doctor Will See at a 3rd Trimester Screening
Timing of 3rd trimester ultrasound
Explanation of results
Why 3rd trimester ultrasound is needed
Screening ultrasounds are the key to the favorable development of the fetus in the womb of the expectant mother. In total, within nine months, the patient is assigned three studies, which, in addition to ultrasound scanning, also include blood tests for biochemistry and specific hormones. It is a mistake to assume that any of the three screenings is optional. At each stage of pregnancy, it is necessary to prevent possible complications and carefully monitor the condition of the patient and the child. Ultrasound at 30 weeks of pregnancy is a mandatory third trimester screening.
It is a mistake to assume that any of the three screenings is optional. At each stage of pregnancy, it is necessary to prevent possible complications and carefully monitor the condition of the patient and the child. Ultrasound at 30 weeks of pregnancy is a mandatory third trimester screening.
Ultrasound of the 3rd trimester allows the obstetrician-gynecologist to make sure that there are no pregnancy pathologies, to determine the size of the head and the position of the fetus on the eve of childbirth. The full composition of the 3rd screening includes not only ultrasound, but also other studies: cardiotocography, Doppler, biochemistry and blood tests for the hCG hormone, free estriol, and alpha-fetoprotein.
Indications for 3rd trimester ultrasound screening
Three timed ultrasound scans are recommended by WHO for all pregnant women without exception. However, there is a risk group whose patients should be screened without fail.
This group includes the following categories of expectant mothers:
- Living in ecologically disadvantaged regions
- Over 35 years of age
- Previously diagnosed with miscarriage
- Having children in the family with genetically determined diseases (syndromes, triploidy, etc.
 )
) - Survivors of infectious diseases in the first trimester
- Treated with antibiotics during pregnancy
- Undergoing high-dose radiation training a few months before conception
- Having a close relative as the father of the child
What the doctor will see at the screening of the third trimester
Diagnosis in the last trimester of pregnancy is important in preparation for childbirth. In the process of scanning with an abdominal sensor, the obstetrician-gynecologist receives a lot of valuable information about the placenta, amniotic fluid and the patient's readiness for childbirth in general. 3rd trimester ultrasound provides data on:
- Amount of amniotic fluid (oligohydramnios, normal, polyhydramnios)
- Maturity of the placenta and the condition of the vessels in it
- The state of the internal organs of the fetus (heart, lungs, liver, kidneys, etc.)
- Fetal parameters: chest diameter, abdominal diameter and circumference, spine parameters, limb length (femur and humerus
Also, ultrasound at 33 weeks can set the exact date of birth.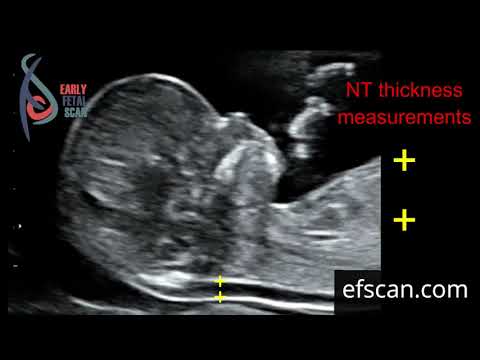 In addition to ultrasound, the doctor may prescribe such standard studies for pregnant women as dopplerography and cardiotocography. These diagnostic procedures are designed to identify the rate and nature of blood flow in the placenta and assess the state of the fetal cardiovascular system.
In addition to ultrasound, the doctor may prescribe such standard studies for pregnant women as dopplerography and cardiotocography. These diagnostic procedures are designed to identify the rate and nature of blood flow in the placenta and assess the state of the fetal cardiovascular system.
Timing of the 3rd trimester ultrasound
The pre-delivery third screening is performed between the 31st and 33rd weeks of pregnancy. This period is due to the fact that at this time the obstetrician-gynecologist can finally verify the health of the fetus and determine its position in the womb. Ultrasound at 32 weeks also allows you to determine the degree of maturation of the placenta. The results will help the doctor navigate the method of the upcoming delivery and recommend either natural childbirth or caesarean section.
Interpretation of third trimester screening results
Ultrasound examination parameters correlate with the patient's period by week. So, the values for 32 weeks of pregnancy will differ from the same indicators at 34 weeks.
So, the values for 32 weeks of pregnancy will differ from the same indicators at 34 weeks.
Normal parameters for screening at 32 weeks are:
- placenta: thickness 25.3 to 41.6 mm
- amniotic fluid: 81 to 278 mm
- placental maturity in degrees: first/second
- cervical dimensions (length): from 30 mm
Parameters of the fetal skeleton at the screening of 32-34 weeks of pregnancy:
- biparietal size: 85 to 89 cm;
- weight: from 1790 to 2390 grams - length (height): from 43 to 47 cm;
- head circumference: from 309 to 323 mm;
- fronto-occipital head size: from 102 to 107 mm;
- forearm (length): 46 to 55 mm;
- shoulder (length): from 55 to 59 mm;
- lower leg (length): from 52 to 57 mm;
- thigh (length): 62 to 66 mm;
- abdominal circumference: 266 to 285 mm
Why 3rd trimester ultrasound is needed
Many patients often wonder if screening is necessary at the last stage of bearing a baby.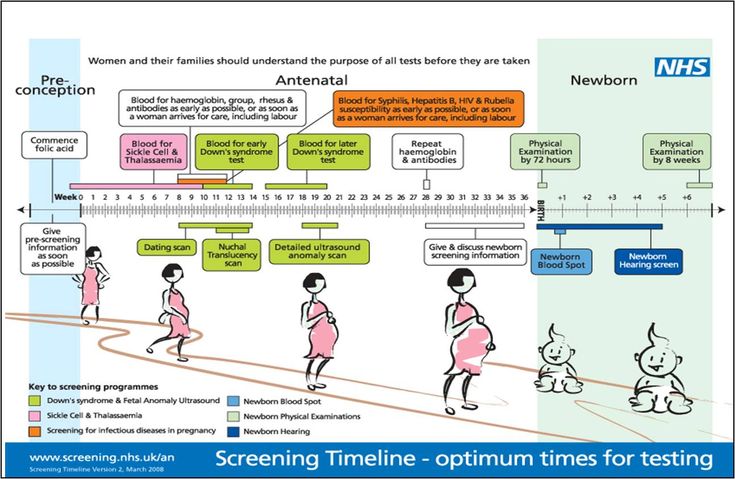 Doctors around the world are unanimous in their opinion: all pregnant women should be examined without exception. This is due to the importance of the scan results for the upcoming birth. Even the most favorable pregnancy can have hidden pathologies. Diagnosis will reveal problems with the placenta, blood flow in the umbilical cord (if any), and the position of the baby in the uterus.
Doctors around the world are unanimous in their opinion: all pregnant women should be examined without exception. This is due to the importance of the scan results for the upcoming birth. Even the most favorable pregnancy can have hidden pathologies. Diagnosis will reveal problems with the placenta, blood flow in the umbilical cord (if any), and the position of the baby in the uterus.
Ultrasound of the third trimester of pregnancy is the last routine examination for a woman.
The third ultrasound screening allows the attending obstetrician-gynecologist to bring the patient to the final line of pregnancy fully prepared.
(36 ratings, average 4.39 out of 5)
See also
Pregnancy
How to choose a gynecologist for pregnancy management?
Pregnancy
First trimester screening
Pregnancy
Pregnancy ultrasound
3 prenatal screening during pregnancy
Screening examinations conducted at different stages of pregnancy are the most accessible and at the same time comprehensive way to monitor intrauterine development of the fetus, as well as the course of the pregnancy itself. Laboratory data and ultrasound examination, carried out at certain periods of bearing a child, complement each other in terms of information. They allow specialists to make fairly accurate predictions about the risks of developing anomalies in the fetus or violations of the normal course of pregnancy.
Laboratory data and ultrasound examination, carried out at certain periods of bearing a child, complement each other in terms of information. They allow specialists to make fairly accurate predictions about the risks of developing anomalies in the fetus or violations of the normal course of pregnancy.
Here are just the main positive aspects of traditional screening:
- Low cost of screening;
- Possibility of mass carrying out with almost 100% coverage of pregnant women;
- Ease of performing the necessary manipulations;
- No risk to mother or fetus;
- For specialists - ease of interpretation of the results;
- Possibility of objective risk assessment.
With such advantages, there is one serious drawback, namely, the insufficient reliability of the data obtained. The accuracy in assessing the risks of fetal anomalies is about 85%.
Screening data that is very different from normal values is an indication for invasive diagnostics.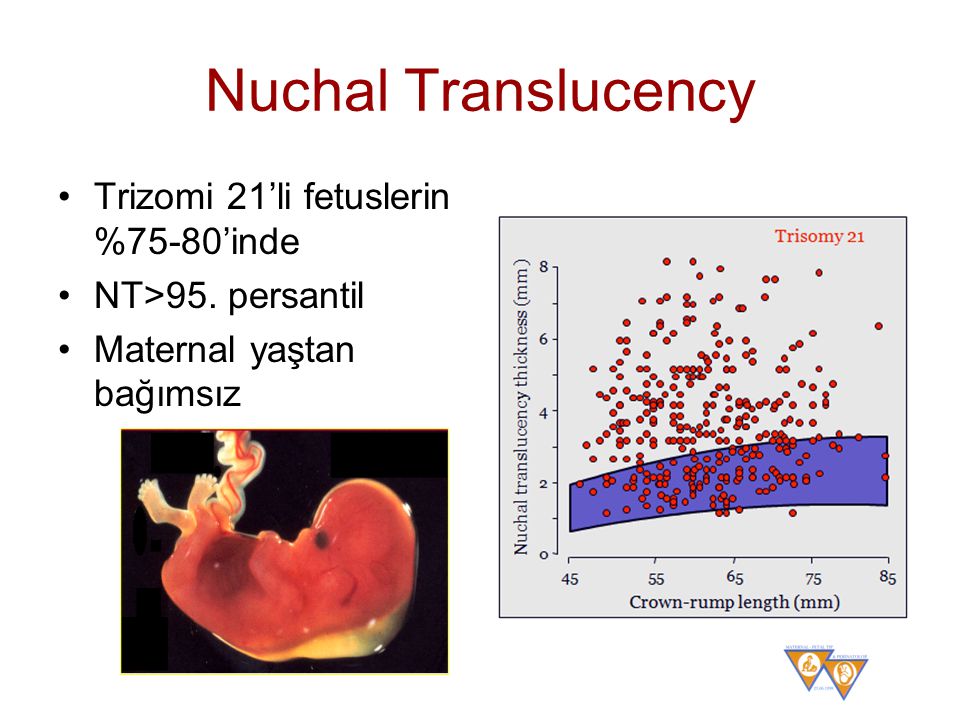 By the third trimester of pregnancy, these issues are usually resolved in one way or another, and the ultrasound performed at this time makes it possible to clarify the structural features of the fetal skeleton, extraembryonic structures, as well as the characteristics of the course of pregnancy.
By the third trimester of pregnancy, these issues are usually resolved in one way or another, and the ultrasound performed at this time makes it possible to clarify the structural features of the fetal skeleton, extraembryonic structures, as well as the characteristics of the course of pregnancy.
In its essence, it is final and often important decisions are made on the tactics of obstetric care based on its results.
The principle of comparing the obtained results with the "reference" values remains the same with the third screening. Naturally, the evaluation of the results obtained and the interpretation of the data should be carried out exclusively by a specialist. The main indicators of 3 screening during pregnancy are shown in the table below.
| Screening by week of pregnancy | |||||
| 30 week | 31 weeks | 32 week | 33 week | 34 week | |
| Embryonic indicators | |||||
| (DKG) Leg bones length, mm | 42-55 | 43-56 | 45-58 | 47-60 | 48-61 |
| (DBK) Length of the femur, mm | 47-63 | 50-66 | 52-68 | 54-69 | 57-71 |
| (BPR) Biparental head size, mm | 67-83 | 69-85 | 72-87 | 74-89 | 76-91 |
| (LZR) Fronto-occipital size, mm | 88-108 | 90-110 | 93-113 | 96-115 | 99-117 |
| (DPC) Humerus length, mm | 44-56 | 46-58 | 47-60 | 49-61 | 51-63 |
| (DKP) Forearm bone length, mm | 42-50 | 44-52 | 45-53 | 46-54 | 48-56 |
| (OG) Head circumference, mm | 265-305 | 273-315 | 283-325 | 289-333 | 295-339 |
| (OJ) Abdominal circumference, mm | 238-290 | 247-301 | 258-314 | 267-325 | 276-336 |
| Fetal heart rate, bpm | 130-170 with an average of 150 | ||||
| Extraembryonic structures* | |||||
| Placenta | Localization of attachment, structural features, maturity normally corresponds to grade I | ||||
| (PT) Placental thickness, mm | 23. | 24.6-40.6 | 25.3-41.6 | 26-42.7 | 26.8-43.8 |
| Amniotic fluid, calculated index, mm | 82-258 | 79-263 | 77-269 | 74-274 | 72-278 |
| Uterus, cervix | Describes all features of | ||||
The main difference between the third screening during pregnancy is that it does not assess the levels of serum markers, but the ultrasound data is already divided into those associated with the fetus and its development, and those associated with the mother's body and the readiness of her reproductive system for future delivery.

 9-39.5
9-39.5