Yeast infection at 36 weeks pregnant
Yeast Infections During Pregnancy
During pregnancy, a woman is at an increased risk of contracting several different types of infections, including urinary tract infections (UTI) and bacterial vaginosis (BV).
A yeast infection is another condition that is very common for expecting mothers, especially during their second and third trimesters. You already may be well aware of yeast infections. An estimated 75% of all women have a yeast infection in their lifetime.
While a yeast infection can be quite annoying and uncomfortable (particularly during the third trimester of pregnancy), it is generally harmless and can be easily treated with antifungal medication. Still, it's important to treat this condition as early as possible. Because you want to avoid transferring the infection to the baby during labor and delivery.
Read below to find out more about this condition, the causes, available treatments, and how to prevent one in the future.
What Is a Yeast Infection?
A vaginal yeast infection (vaginal candidasis) is a fungal infection that causes irritation and discharge of the vagina. Under normal circumstances, the vagina keeps a healthy balance of its pH (acid level) and the amount of yeast inside of it. This balance acts as a type of protection and helps kill off bad bacteria. When a yeast infection occurs, the levels of acid and yeast in the vagina become unbalanced and allow the yeast to overgrow, which causes uncomfortable symptoms.
A yeast infection is not a sexually transmitted infection (STI), but women often develop the condition after they first become regularly sexually active. It may also be linked to mouth-to-genital contact (oral-genital sex). This infection affects up to 3 out of 4 women, making it extremely common. Fortunately, yeast infections are not considered serious and can be cured within two weeks with appropriate treatment.
Why Are Yeast Infections Common During Pregnancy?
Yeast infections are much more common in pregnant women because of the hormonal changes happening in their bodies. They are notoriously difficult to treat during pregnancy.
They are notoriously difficult to treat during pregnancy.
Pregnancy increases the release of the hormone estrogen, which is known to upset the vagina's chemical balance. Pregnant women also have a higher amount of sugar in their vaginal secretions, making it easier for the yeast to grow. These factors will also increase the risk of contracting a yeast infection:
- Hormonal changes that come with pregnancy or before your period
- Taking hormone medication
- Taking antibiotics
- Taking steroids
- Having high blood sugar or diabetes
- Vaginal intercourse
- Douching
- The vagina comes into contact with blood or semen
- An impaired immune system
What Are the Symptoms of a Yeast Infection?
The symptoms of a yeast infection during pregnancy can vary by how far the infection has progressed. It generally includes one or more of the following:
- An increased amount of discharge
- Watery vaginal discharge
- Discharge that looks white/tan in color, or possibly green/yellow
- Discharge that looks similar to cottage cheese (odorless)
- Discharge smells like yeast/bread
- Itching or irritation in the vagina and vulva
- Redness or swelling of the vulva
- Burning sensation during urination or intercourse
Pregnant women are more likely to have what's called a "complicated yeast infection.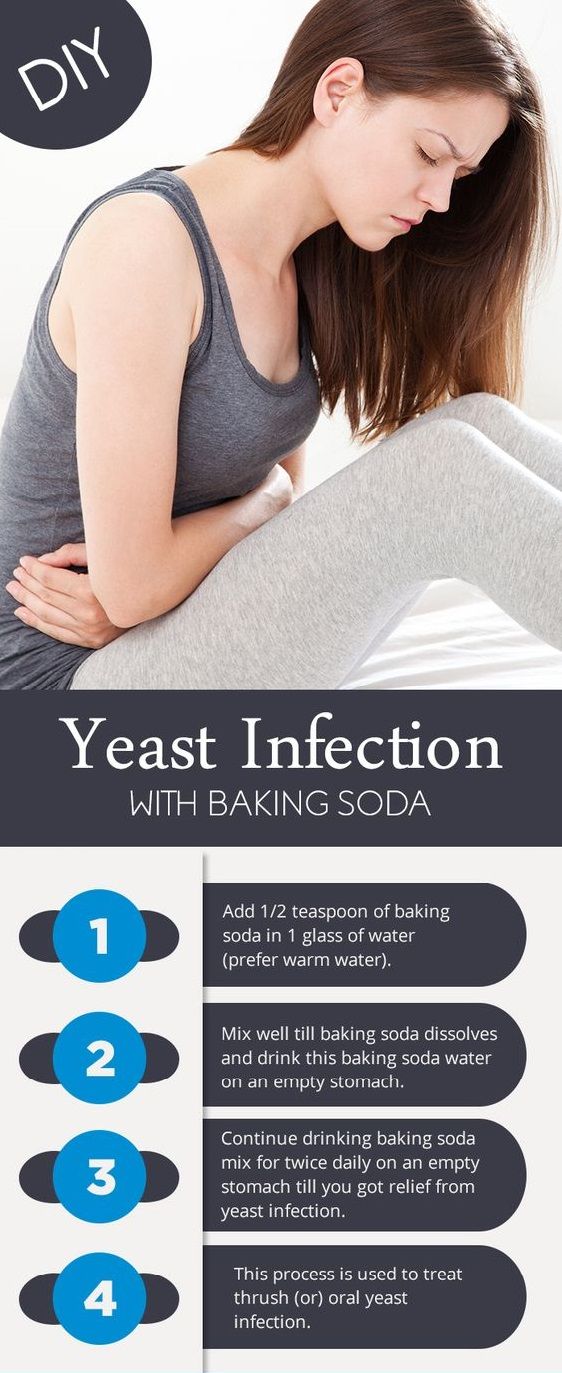 " This simply means that you may experience multiple yeast infections throughout your pregnancy, which can create chronic symptoms that take longer to resolve. This is considered normal and is not a cause for concern, especially if you are in your second or third trimester.
" This simply means that you may experience multiple yeast infections throughout your pregnancy, which can create chronic symptoms that take longer to resolve. This is considered normal and is not a cause for concern, especially if you are in your second or third trimester.
How Is a Yeast Infection Diagnosed?
If you suspect that you might have a yeast infection, make an appointment with your doctor right away. Treating yeast infections early can save you from experiencing more uncomfortable symptoms of a yeast infection during pregnancy.
At the doctor's office, your doctor will provide a pelvic exam and use a small tool to painlessly swab your discharge or vaginal secretions. The sample is put under a microscope, where a physician can identify and diagnose an infection.
How Is a Yeast Infection Treated?
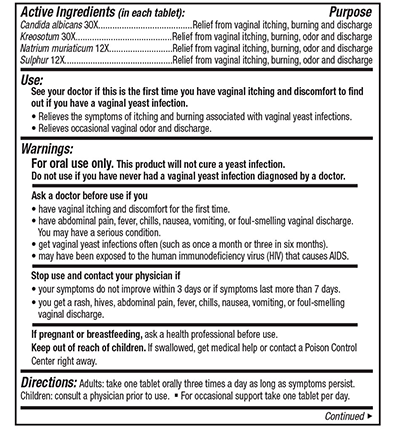
In normal circumstances, doctors usually prescribe a single-dose oral medication called Diflucan that can clear up an infection within a few days. However, this medication has not been proven to be safe to take during pregnancy and should be avoided if possible.
However, this medication has not been proven to be safe to take during pregnancy and should be avoided if possible.
Instead of an oral pill, doctors will recommend you take vaginal creams and suppositories to cure the infection. These are anti-fungal medications that fight off overgrown yeast and restore the vaginal balance. Only certain creams and suppositories are safe to use during pregnancy. Treatments like Terazol or Monistat are generally considered safe for pregnant women, but make sure to consult with your doctor to get their professional opinion.
It may take up to two weeks to fully get rid of a yeast infection, but the uncomfortable symptoms may subside within the first few days. After the infection has cleared, it may be beneficial to use a starch-free drying powder to prevent another infection.
Can a Yeast Infection Harm My Baby?
Yeast infections rarely cause any complications for you or your baby. These common infections, particularly during the second and third trimesters, are easy to treat and tend to stay localized in one area.
These common infections, particularly during the second and third trimesters, are easy to treat and tend to stay localized in one area.
But an untreated yeast infection has the possibility of passing to your baby's mouth during labor and delivery. This condition is called "thrush.", You want to avoid thrush. Still, it can be treated with the Nystatin, another anti-fungal medication. So pregnant women need to visit their doctor as soon as they start experiencing symptoms.
That said, if a persistent yeast infection during pregnancy gains steam and travels through the vagina or blood, there is a risk, albeit low, of complications. It can in rare cases cause chorioamnionitis, prematurity, endometriosis, and neonatal sepsis.
How Can I Prevent a Yeast Infection?
You do not need to be dealing with an untreated yeast infection during the third trimester of your pregnancy. You have enough to worry about. So an untreated yeast infection during pregnancy is a complication you want to avoid. There are several different steps you can take to prevent a yeast infection from occurring or recurring:
So an untreated yeast infection during pregnancy is a complication you want to avoid. There are several different steps you can take to prevent a yeast infection from occurring or recurring:
- Wear loose, breathable cotton underwear.
- After showering, use your blow dryer on a low, cool setting to help dry the outside of your genital area.
- Always wipe from front to back when using the restroom.
- Avoid wearing damp, wet clothes. Change your clothes immediately after swimming or working out.
- Include yogurt with the bacteria "lactobacillus acidophilus" in your diet.
- Limit your sugar intake, as sugar promotes the growth of yeast.
Avoid using these:
- Tight-fitting pants or pantyhose
- Douching
- Feminine hygiene sprays
- Sanitary pads and tampons that contain deodorant or scents
- Taking a bubble bath or sitting in a hot tub
- Using scented soaps
- Using colored or perfumed toilet paper
Dealing with a Yeast Infection During Pregnancy
Overall, yeast infections are more of a nuisance than a concern during pregnancy. But there are enough rare occasions with tragic outcomes not to not only keep an eye on your yeast infection but to also consult with your doctor to make sure it is under control.
But there are enough rare occasions with tragic outcomes not to not only keep an eye on your yeast infection but to also consult with your doctor to make sure it is under control.
But the good news is as awful as yeast infections can be, they are usually easy to treat and only rarely present long-term complications.
If your symptoms are particularly hard to manage, talk to your doctor about other over-the-counter medications that specifically treat burning sensations, itchiness, and swelling. Remember to completely finish the entire course of medication to get rid of the infection completely and prevent it from coming back.
Sources and Additional Literature
Elkady, A., Sinha, P., & Hassan, S. A. Z. (Eds.). (2019). Infections in Pregnancy: An Evidence-Based Approach. Cambridge University Press.
Vieira-Baptista, P., & Bornstein, J. (2019). Candidiasis, Bacterial Vaginosis, Trichomoniasis, and Other Vaginal Conditions Affecting the Vulva. Vulvar Disease (pp. 167-205). Springer, Cham.
Vulvar Disease (pp. 167-205). Springer, Cham.
Jeanmonod, R., et al. (2019). Vaginal Candidiasis (Vulvovaginal Candidiasis). StatPearls.
Presterl, E., et al. (2019). Medical Mycology: Fungal Infections. Basic Microbiology and Infection Control for Midwives (pp. 155-159). Springer, Cham.
Chatzivasileiou, P., & Vyzantiadis, T. A. (2019). Vaginal yeast colonisation: From a potential harmless condition to clinical implications and management approaches-A literature review. Mycoses: Diagnosis, Therapy, and Prophylaxis of Fungal Diseases.
Infections in pregnancy and how they affect the baby
During pregnancy, people may worry more about contracting infections and how they might affect the developing baby.
Vaginal infections, including yeast infections, are common during pregnancy and are usually not a cause for concern. Uterine infections may produce more complications, however.
This article looks at common infections during pregnancy, how they might affect the baby, and how to prevent them from developing.
Someone who is pregnant might be more vulnerable to certain infections and may develop more severe complications if the infections are left untreated. Anyone who has even a minor infection during pregnancy should talk to a doctor or midwife.
Typical vaginal infections during pregnancy include:
Vaginal yeast infections
Vaginal yeast infections are caused by a fungus called Candida. These infections tend to occur during pregnancy because of changes in the immune system, increased production of glycogen, and higher estrogen levels.
According to a 2015 report, about 20 percent of all women have Candida, which rises to 30 percent during pregnancy. It appears to be more common during the second and third trimesters.
The most common symptoms of a vaginal yeast infection include:
- itchiness around the vagina or vulva
- a thick, white, cottage cheese-like vaginal discharge
- an odor of bread or beer coming from the vagina
- pain or burning in or around the vagina
- pain or burning during sexual intercourse
People can use prescription or over-the-counter medications to treat a vaginal yeast infection. However, anyone who is pregnant should not use these drugs without first talking to a doctor or midwife.
However, anyone who is pregnant should not use these drugs without first talking to a doctor or midwife.
It is essential to get a diagnosis before beginning treatment as other infections, such as bacterial vaginosis and chlamydia, can be confused with yeast infections.
Bacterial vaginosis
Bacterial vaginosis (BV) is an easily treated bacterial infection in the vagina. Symptoms include:
- itching, burning, or pain in the vagina or vulva
- a fishy odor coming from the vagina
- a bad smell that gets worse after sexual intercourse
- a large amount of thin, grey colored discharge
If BV is left untreated during pregnancy, it might cause preterm labor, premature birth, and lower birth weight babies.
Group B Streptococcus (GBS)
Group B streptococcus (GBS) is a group of bacteria that come and go in the body but often frequent the vagina and rectum. They do not typically cause symptoms or even an infection. However, women who have GBS in their bodies when they give birth may pass it to their babies.
Mothers who have GBS will pass it on to their babies in 1 to 2 percent of cases. Although uncommon, GBS in a newborn can be fatal.
Testing between the beginning of week 36 and the end of week 37 of pregnancy can detect GBS and is a standard part of most prenatal care.
Treatment with antibiotics through a needle in a vein (IV antibiotics) can significantly reduce the risk of a GBS infection passing to the baby.
An infection in the uterus can be dangerous for a variety of reasons. The infection may affect the placenta, harm the developing baby, cause premature labor, or lead to birth abnormalities.
Uterine infections can also make labor more dangerous and difficult. Some individuals experience organ failure and other life-threatening complications.
Uterine infections often develop when bacteria from the vagina travels to the uterus, so an untreated vaginal infection is a risk factor for uterine infections. A person is more susceptible to uterine infections if their membranes rupture during an extended labor.
Treatment includes antibiotics and may require hospitalization. If a fever develops during labor, a doctor or midwife will monitor the fetus. If the symptoms are severe, the doctor may recommend a cesarean delivery.
Pregnancy causes many changes in the body, making people more susceptible to complications from many infections.
For example, hormone-related skin changes during pregnancy can cause conditions such as eczema or severely dry skin. If the skin cracks open and bleeds, a serious skin infection, such as cellulitis, can develop. A rare skin disorder called Sweet’s syndrome is also more common during pregnancy than at other times.
Some other infections that may be more serious during pregnancy include:
- the flu
- hepatitis E, which is a typically mild viral form of hepatitis
- herpes, including herpes simplex virus (HSV) and varicella zoster virus (VZV)
- Listeria, which can cause food poisoning
- measles
- HIV
The increased risk of these infections during pregnancy is not well understood but may be due to hormone and other changes that alter the number of blood cells in the body. For example, late in pregnancy, T cells that help fight infection decrease in number.
For example, late in pregnancy, T cells that help fight infection decrease in number.
Pregnancy also causes increased blood circulation and demands on the heart. These demands can also worsen complications. For example, if a pregnant person develops pneumonia from the flu, they may have more difficulty breathing because of the increased demands the fetus places on the heart and lungs.
Some medications that can effectively treat common infections may be less safe during pregnancy. So it is essential that pregnant people who have an infection talk to their doctor or midwife to weigh up the benefits and risks of various treatment options.
Numerous infections can affect the developing baby. However, it is difficult for doctors to tell whether and to what extent a fetus will be affected.
Infections can affect a developing baby in one of three ways:
- They may harm the mother, making her body less able to nurture the baby or requiring the use of drugs that may harm a fetus.

- They can directly harm the baby by causing changes that lead to birth abnormalities.
- They can trigger premature labor or a miscarriage.
According to the National Institutes of Health (NIH), infections that are known to harm the developing baby include, but are not exclusive to:
- bacterial vaginosis, which might cause preterm labor
- contagious diseases, such as hepatitis, syphilis, herpes, and HIV, which can infect the fetus
- chlamydia, which can cause eye infections and pneumonia
- gonorrhea, which can contaminate the amniotic fluid, cause preterm labor, and lead to eye infections and possible blindness
- fifth disease, which can trigger a miscarriage or cause fetal anemia
- group B streptococcus, which can cause severe complications in newborns, and in rare cases can be fatal
- toxoplasmosis, which can cause birth abnormalities and intellectual disabilities
- Listeria, which can cause miscarriage, stillbirth, and birth abnormalities
- cytomegalovirus, which is often harmless but can also cause birth abnormalities and intellectual disabilities
- Zika, which is usually mild, can cause pregnancy loss or birth abnormalities in an infant
Zika infection, which is a disease carried by mosquitoes, may cause birth abnormalities and increase the risk for stillbirths and miscarriages in those who have the virus. However, it is unclear why some fetuses are affected, and others are not.
However, it is unclear why some fetuses are affected, and others are not.
Other infections may also harm a developing baby, depending on the overall health of the pregnant person, when the infection developed, and whether the person has received treatment.
The Centers for Disease Control and Prevention (CDC) provide some strategies to reduce the risk of developing an infection during pregnancy, including:
- avoiding travel to areas where Zika is prevalent, and using bug spray to prevent mosquito bites
- using a condom and asking a partner to be tested for sexually transmitted infections (STIs)
- washing hands carefully and diligently
- avoiding people who have contagious infections
- getting a flu shot
- avoiding unpasteurized foods
- asking someone else to change the cat litter
- testing for STDs and group B strep
Most people who experience an infection during pregnancy will not experience complications. Prompt treatment increases the likelihood of a healthy birth.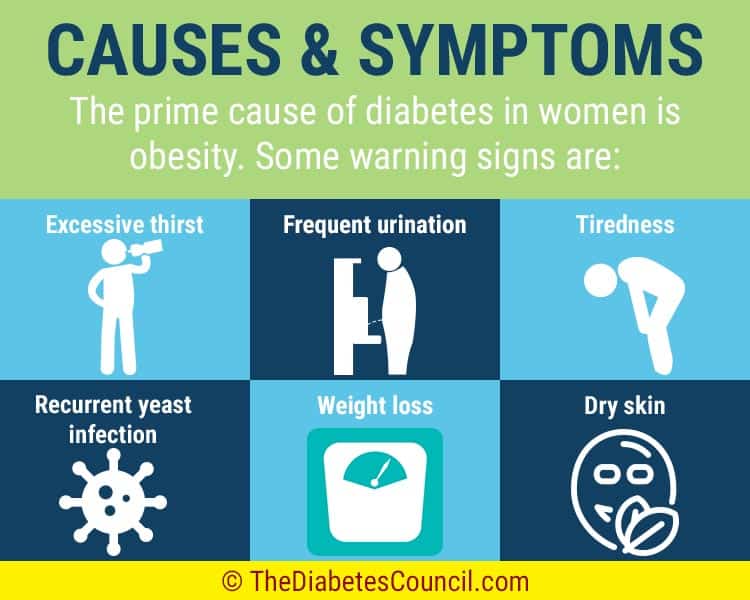
Anyone who experiences any unusual symptoms during their pregnancy should talk to their doctor or midwife. Prenatal care is also crucial since it can detect certain infections even before they cause symptoms.
symptoms, treatment (1st, 2nd, 3rd trimesters)
Did you know that every third woman in the world suffers from candidiasis? At the same time, thrush occurs three times more often in pregnant women. Let's take a look at the causes of thrush together, and also talk about the main symptoms and methods of treating thrush at different stages of pregnancy.
Lyudmila Starichenko
doctor of the highest qualification category,
head doctor of the Clinic of Innovative Technologies
work experience 41 years
learn more on the website
Causes of thrush
Signs and symptoms of thrush in pregnant women
Treatment of thrush in pregnant women
What to avoid when treating thrush?
Why is thrush dangerous during pregnancy?
What if it doesn't go away?
Prevention
Causes of thrush
Thrush or vulvovaginal candidiasis is a common disease of the vaginal mucosa. The main reason for its appearance is a fungal infection.
The main reason for its appearance is a fungal infection.
Pregnant women are at particular risk. After all, in this position, the patient has a natural decrease in immunity, which can even lead to a decrease in local immunity. As a result, the inevitable growth of opportunistic microorganisms occurs. Among them are yeast-like fungi that cause candidiasis. Changes in the hormonal background, namely, an increase in the level of female sex hormones, can also affect the increased growth of yeast-like fungi. This is especially true for patients who have pregnancy complications.
Read more about the causes of candidiasis in our material.
learn more
Signs and symptoms of thrush in pregnancy
The signs and symptoms of thrush in pregnancy are no different from the usual symptoms of thrush. They differ only in what particular organ is affected by thrush.
So, for example, with urogenital candidiasis, the most characteristic symptoms are discharge from the genital tract, itching, burning in the genital area and its intensification during sleep and water procedures.
Treatment of thrush in pregnant women
All medications during pregnancy must be selected by a doctor. Self-treatment is out of the question here, because by wrong actions a woman can harm not only herself, but also her child!
As a rule, only local therapy is prescribed during pregnancy at any time.
First trimester
In the first trimester, use Natamycin 100 mg intravaginally for 6 days. The drug refuses fungicidal and antifungal action.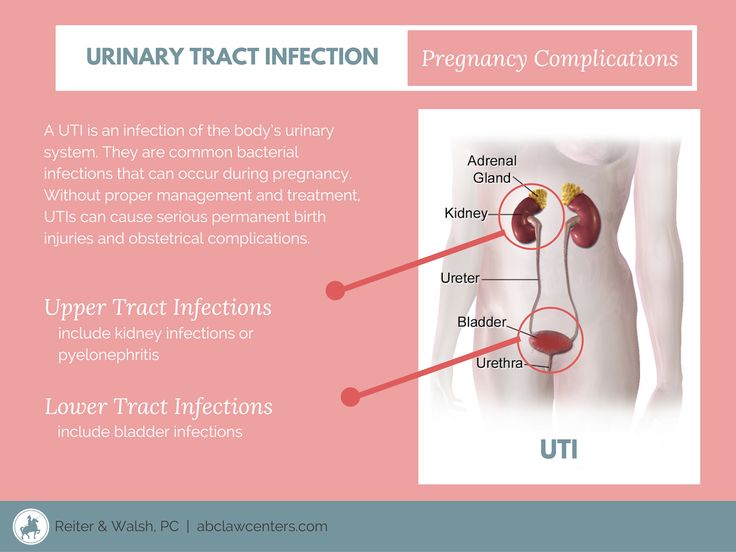 Thanks to the active substance, it binds to the sterols of the cell membrane of the fungus and disrupts its permeability. This leads to the destruction of the fungal cell as a result of damage or rupture of the membrane.
Thanks to the active substance, it binds to the sterols of the cell membrane of the fungus and disrupts its permeability. This leads to the destruction of the fungal cell as a result of damage or rupture of the membrane.
Natamycin is active against most yeast-like fungi, and especially against fungi of the genus Candida. The advantage of this drug is that it does not have a systemic effect and is not absorbed into the gastrointestinal tract, acting only locally on the damaged mucous membrane. Of the possible side effects with topical application - only irritation and burning sensation at the site of application.
Second and third trimesters
In the II and III trimester, Sertoconazole 300 mg is used intravaginally once. This drug has a powerful antifungal effect by increasing the permeability of the cell membrane, which leads to the destruction of the cells of the opportunistic fungus. Side effects do not differ from the previous drug. Of the side effects at the site of application of Sertoconazole, itching and burning may occur, which will pass on their own.
Side effects do not differ from the previous drug. Of the side effects at the site of application of Sertoconazole, itching and burning may occur, which will pass on their own.
Followed by Econazole 150 mg intravaginally for 3 days. The drug has a local antifungal and antibacterial effect. It stops the biosynthesis of ergosterol and other sterols that regulate the permeability of the fungal cell wall. With intravaginal administration, patients did not experience pregnancy complications or other undesirable effects of therapy on reproduction. Local reactions are possible: rash, burning irritation, itching, redness and dryness of the skin.
The last stage of treatment is Clotrimazole 100 mg intravaginally for 6-10 days. The drug belongs to a broad spectrum antifungal agent. It is applied topically only by the intravaginal method. Clotrimazole inhibits the growth and division of microorganisms.
The mechanism of action of the drug is associated with a change in the permeability of cell membranes. It inhibits the synthesis of proteins, fats, damages nucleic acids in fungal cells and accelerates the excretion of potassium. Very rarely, but sometimes there are yeast-like fungi that may be immune to the drug. In general, reviews of the drug are extremely positive, however, some patients may experience side effects that Clotrimazole has in abundance.
It inhibits the synthesis of proteins, fats, damages nucleic acids in fungal cells and accelerates the excretion of potassium. Very rarely, but sometimes there are yeast-like fungi that may be immune to the drug. In general, reviews of the drug are extremely positive, however, some patients may experience side effects that Clotrimazole has in abundance.
In addition, when treating candidiasis, it is recommended to follow a diet. About what foods can be consumed, and which are better not worth it, read our material.
Folk methods
It should be said that the doctor with whom we consulted does not advise the use of folk remedies for thrush, as they are simply not able to help with this disease. But on the Internet, some means are indicated. Among them: douching and tar soap, soda and chamomile, potassium permanganate and sea buckthorn oil.
For more information on how to use these folk remedies, look in our material.
However, we want to remind you once again that none of the folk remedies is a panacea for thrush. Alternative recipes can reduce the intensity of unpleasant symptoms, but can not cure candidiasis. Therefore, we recommend that you seek professional medical help without fail and do not self-medicate.
find out how to get diagnosed
What to avoid when treating thrush?
First of all, do not self-medicate. This advice is especially relevant during pregnancy. Not all drugs are compatible with pregnancy, and which of them can or cannot be taken - only the attending physician can decide!
As we said above, during pregnancy, only local therapy is prescribed. Ignorance of these features can adversely affect the fetus.
Ignorance of these features can adversely affect the fetus.
Why is thrush dangerous during pregnancy?
Thrush is dangerous during pregnancy. At this time, the development of an ascending infection with intrauterine infection of the fetus and a newborn with the development of intrauterine infection is possible.
Do not start this disease. This is fraught not only with unpleasant symptoms, but also with consequences for the body. Candidiasis carries the following complications: systemic damage to the pelvic organs, a significant decrease in the quality of life, constant discomfort, dysbiotic disorders of the microflora of the intestinal tract. During pregnancy, the effects may intensify.
What to do if it doesn't go away?
Unfortunately, thrush can easily develop from an active to a chronic form.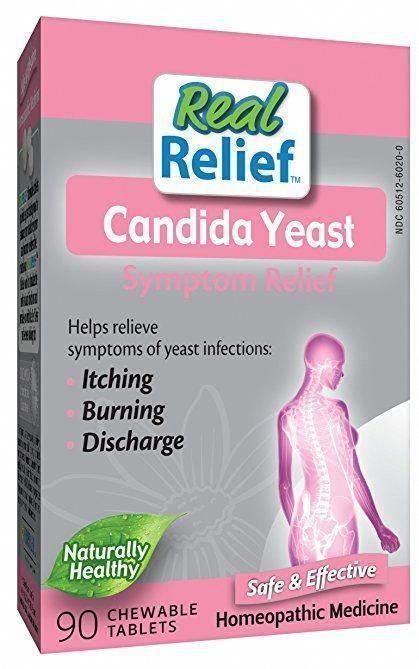 This happens for a number of reasons. For example, hormonal disruptions and other health-related causes, which abound during pregnancy, can lead to the reappearance of candidiasis. In addition, a decrease in immunity, fatigue, and even climate change can provoke a relapse.
This happens for a number of reasons. For example, hormonal disruptions and other health-related causes, which abound during pregnancy, can lead to the reappearance of candidiasis. In addition, a decrease in immunity, fatigue, and even climate change can provoke a relapse.
If candidiasis does not go away during pregnancy or returns, you should not fight it yourself according to the prepared scheme from the last time. The patient needs to contact the attending physician again to select the most effective drugs.
This is especially true for pregnant women. Drugs used outside of pregnancy can not only not help, but also harm.
Prevention
How to avoid the unpleasant symptoms and consequences of thrush? It is not so difficult to do this if you strictly follow the basic rules of prevention and hygiene. Among them - the selection of comfortable underwear, personal hygiene, the rejection of scented pads and, of course, maintaining the immune system. The last point is, in principle, relevant for pregnant women.
Among them - the selection of comfortable underwear, personal hygiene, the rejection of scented pads and, of course, maintaining the immune system. The last point is, in principle, relevant for pregnant women.
Conclusion
During pregnancy, a woman has a natural decrease in immunity, which may, unfortunately, lead to thrush. And if you do not start a fight with it in time, then the disease can be transmitted to the child. However, with timely treatment and elimination of the factors that cause the disease, it is possible to forget about this disease once and for all. The main thing is not to start thrush to a chronic form. Only a medical specialist will be able to individually select for you a treatment that will cope with the disease.
If you still have questions, you can ask them to the specialists of the Innovative Technology Clinic.
Website: https://3dkit.ru/
Phone: +7 (963) 380-10-31 +7 (865) 257-76-05
. Dovatortsev, 53 B
Author: Ekaterina Vlasova
Photo: Anastasia Ryazhskaya
Thrush during pregnancy. Alternative treatments - Mama Lara - professionally about the birth of a child | Pregnancy | Childbirth
You probably know that thrush during pregnancy is quite common. In this article, I will talk in detail about this problem, as well as what treatment for thrush during pregnancy will be most effective.
Symptoms of thrush during pregnancy
During pregnancy, thrush, or vaginal candidiasis, as this disease is called in another way, sometimes brings real suffering for a woman, although some pregnant women find out that something is wrong only according to the results of the analyses.
Symptoms of thrush are white or whitish-yellow, homogeneous or cheesy discharge with a specific sour or “fishy” smell, as well as itching and burning in the vagina. Such discharge may appear in early pregnancy or later, in the second or even third trimester. It is because of the nature of the discharge that this disease is usually called thrush.
Why is thrush so common during pregnancy?
Cause of thrush during pregnancy is the rapid multiplication of Candida fungi on the vaginal mucosa. In fact, these fungi in small quantities can be found on the vaginal mucosa of any healthy woman. This means that they are elements of our healthy microbiota (the term microflora is erroneous, since flora in translation into Russian means a plant).
However, during pregnancy fungi begin to germinate from spores and multiply rapidly. This happens because during pregnancy, as a result of hormonal changes (the amount of progesterone in the woman's body increases), the acidity of the vagina changes, and the immune activity of the body decreases. And for fungi, such conditions are the best. As a result, a large number of fungi causes an inflammatory process, accompanied by itching, burning and discharge.
And for fungi, such conditions are the best. As a result, a large number of fungi causes an inflammatory process, accompanied by itching, burning and discharge.
These unpleasant sensations intensify in the evening and at night, during intimacy, shortly after hygiene procedures. The trouble is, if before the onset of pregnancy a woman underwent a course of antibiotic therapy, since antibiotics, while suppressing the growth of other bacteria, have no effect on fungi. As a result, the rapid growth of fungi, due not only to the fact that the environment in the vagina has become more acidic, but also to the fact that fungi have no competitors left.
Of course, it is even worse if antibiotics have to be used already during pregnancy. Consider that in this case, thrush during pregnancy is practically guaranteed to you.
Treatment of thrush during pregnancy
- The first thing to do is to make sure that you really have thrush, because discharge and itching in the vagina during pregnancy are symptoms not only of candidiasis, but also of other infections of the genitourinary system.
 It also happens that there are no symptoms at all, and the pregnant woman learns about the disease at a doctor's appointment. Whether to treat the asymptomatic course of thrush during pregnancy is up to you (you rarely want to treat something that does not hurt). However, immediately before the birth, I would still advise a course of treatment.
It also happens that there are no symptoms at all, and the pregnant woman learns about the disease at a doctor's appointment. Whether to treat the asymptomatic course of thrush during pregnancy is up to you (you rarely want to treat something that does not hurt). However, immediately before the birth, I would still advise a course of treatment. - Second - pay attention to whether you have symptoms of intestinal dysbacteriosis. Very often, disturbances in the composition of the microbiota are observed simultaneously in the intestine and in the vagina. If so, then I strongly advise you to drink a long course (at least a month) of Linex or Hilak Forte in parallel with the treatment of thrush.
- The third thing to take care of is your diet. Fungi love sweets, so it is necessary to exclude all confectionery, sweet pastries (you can leave homemade pastries with the addition of a lot of fruit), sweets, cookies. In addition, I advise eliminating kefir fermented with kefir fungus from the diet, it can also support the growth of pathogenic fungus.
 Therefore, when choosing fermented milk products, give preference to those prepared using bifidobacteria and acidophilus bacillus.
Therefore, when choosing fermented milk products, give preference to those prepared using bifidobacteria and acidophilus bacillus. - Fourth, if you choose to treat thrush with medication, remember that most antifungal drugs are contraindicated during pregnancy. As a rule, at this time, doctors prefer the use of local methods of treatment (suppositories, creams), rather than general ones, since one should not forget that all drugs that enter the blood of the expectant mother in large quantities eventually end up in the child's body. In any case, the right medicine, its dose and duration of use should be prescribed only by your doctor.
- Fifth, if you prefer folk or non-standard methods of treatment, I can offer several to choose from. These methods have been tested by me for many years of working with pregnant women. In my experience, I know that they are much more effective than medication in treating thrush during pregnancy.
Treatment of thrush during pregnancy with homeopathic medicines
To get detailed information about the treatment of thrush during pregnancy with homeopathic medicines, use our Telegram assistant bot.
To use the Telegram bot, just type @mamalarabot in the search box of the messenger and click the Start button.
Treatment of thrush during pregnancy with cold
This method of treating thrush may seem quite wild, and yet it is extremely effective. The fact is that mushrooms are very fond of heat, while low temperatures kill them. Everyone knows that mushrooms do not grow in the forest in winter! So in the human body, they live and reproduce only because they like the temperature of our body. So, if you are not afraid to insert a piece of ice into your vagina, then this method will suit you treatment of thrush during pregnancy .
To make ice, you will need three clean oval-shaped plastic containers (if you don't have anything suitable, you can use the ones that contain small toys inside Kinder Surprise chocolate eggs). Ice frozen in special containers or edible ice bags has sharp edges and is therefore unsuitable. You need to fill these containers by submerging them underwater. It can be ordinary clean or boiled water, or you can use Malavit's solution (1:30 with water). This drug has antifungal activity.
It can be ordinary clean or boiled water, or you can use Malavit's solution (1:30 with water). This drug has antifungal activity.
It is necessary to carry out the procedure lying on your back, bending and slightly spreading your legs. Place a disposable waterproof diaper under you so as not to wet the bed. In order to make it easier to get the ice out of the containers, and also in order to reduce the size of the ice egg if necessary (if this size of ice seems too large for you to insert into the vagina), prepare a container of hot water next to you.
So, relax and gently insert the ice into the vagina as deeply as possible, lie down for 5 minutes, and then take a squatting position near the bed and “pull out” the ice (ie ice water) that has melted during this time. Rest 5-10 minutes, repeat the introduction of ice. Do the same for the third time. The duration of the course is 5-7 days.
Such a short exposure to cold will not cause any harm to the pelvic organs, however, if you have chronic cystitis, I advise you to choose another method of treating thrush.
Treatment of thrush during pregnancy with honey.
Yes, yes! Honey is the most powerful naturopathic antifungal medicine and is great for treating thrush during pregnancy. Only it should be really natural, unadulterated honey. And it's getting harder and harder to buy these days. However, if you know a beekeeper or have good reviews about one of the sellers, buy honey and use it safely.
Honey is inserted into the vagina on a tampon, while you can make a tampon yourself from cotton wool and a bandage, or you can use the hygienic one of the smallest size. After inserting a tampon, it is better to lie down so that the honey is distributed throughout the vagina, and does not leak out. After two hours, the swab should be removed. The duration of the course is 7-10 days.
Treatment of thrush during pregnancy with tea tree oil
One of the most active antifungal agents is tea tree essential oil. It is also well suited for the treatment of thrush during pregnancy.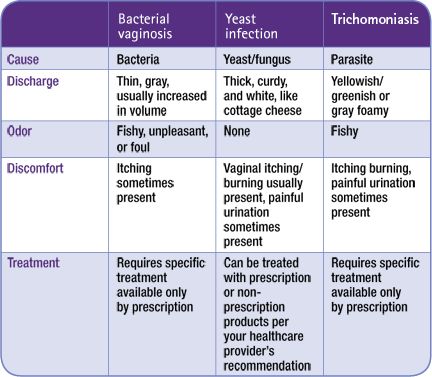 When buying, it is important to pay attention to the quality of the product. Give preference to branded oils, for example, the Austrian company Stix. As a base, you can take any vegetable oil (peach, almond, grape seed, olive and regular sunflower). In 20 ml of base, add 3-5 drops of tea tree oil. Introduce oil into the vagina on a swab or simply dip your clean finger into the oil and lubricate the walls of the vagina with it.
When buying, it is important to pay attention to the quality of the product. Give preference to branded oils, for example, the Austrian company Stix. As a base, you can take any vegetable oil (peach, almond, grape seed, olive and regular sunflower). In 20 ml of base, add 3-5 drops of tea tree oil. Introduce oil into the vagina on a swab or simply dip your clean finger into the oil and lubricate the walls of the vagina with it.
Other non-drug treatments for thrush during pregnancy include topical baking soda and borax in glycerin. Borax in glycerin can be bought at a pharmacy, it is called sodium tetraborate.
In conclusion, I want to say that the non-drug methods I have listed are effective not only in the treatment of thrush during pregnancy . In the same way, any candidiasis of the genitourinary sphere of a woman can be treated. And honey helps well in the treatment of thrush in the mouth in infants (natural honey, contrary to popular belief, does not cause allergies).