Infants urinary tract infection
Urinary Tract Infections In Babies
AddictionAllergies & AsthmaAmbulatoryAudiologyAutismAwardsBC4TeensBehavioral HealthBehind the ScenesBurn CenterCancerCardiologyCenter for Healthy Weight and NutritionCenter for Injury Research and PolicyChild BehaviorChild DevelopmentColorectal and Pelvic ReconstructionCommunity EducationCommunity ResourcesCoronavirusDentistryDermatologyDiseases & ConditionsDiversity and InclusionEndocrinologyENTEpilepsyEverything MattersFertility and Reproductive Health ProgramFundraising EventsGastroenterologyGeneticsGynecologyHematologyHomecareHospiceHospital NewsInfants & NewbornsInfectious DiseaseKids & TeensLaboratory ServicesMake Safe HappenMarathonNeonatologyNephrologyNeurologyNeurosurgeryNew HospitalNICUNutrition & FitnessOccupational TherapyOphthalmologyOrthopedicsOur PatientsOur staffPalliative CareParentingPediatric NewsPharmacyPhysical Therapy - Sports and OrthopedicPlastic SurgeryPopulation HealthPregnancyPrimary CarePsychologyPulmonaryRadiologyReach Out and ReadRehabilitationResearchRheumatologySafety & PreventionSports MedicineSurgical ServicesThe Center for Family Safety and HealingTherapeutic RecreationTherapyTHRIVE ProgramToddlers & PreschoolersUrgent CareUrology
Aaron Barber, AT, ATC, PESAbbie Roth, MWCAbby Orkis, MSW, LSWAdam Ostendorf, MDAdriane Baylis, PhD, CCC-SLPAdrienne M. Flood, CPNP-ACAdvanced Healthcare Provider CouncilAila Co, MDAkua A. Amponsah Chrappah, MDAlaina White, AT, ATCAlana Milton, MDAlana Milton, MDAlecia Jayne, AuDAlena SchuckmannAlessandra Gasior, DOAlex Kemper, MDAlexandra Funk, PharmD, DABATAlexandra Sankovic, MDAlexis Klenke, RD, LDAlice Bass, CPNP-PCAlison PeggAllie DePoyAllison Rowland, AT, ATCAllison Strouse, MS, AT, ATCAmanda E. Graf, MDAmanda GoetzAmanda Smith, RN, BSN, CPNAmanda Sonk, LMTAmanda Whitaker, MDAmber Patterson, MDAmberle Prater, PhD, LPCCAmit Lahoti, MDAmy Brown Schlegel, MDAmy Coleman, LISWAmy Dunn, MDAmy E. Valasek, MD, MScAmy Fanning, PT, DPTAmy Garee, CPNP-PCAmy Hahn, PhDAmy HessAmy Leber, PhDAmy LeRoy, CCLSAmy Moffett, CPNP-PCAmy Randall-McSorley, MMC, EdD CandidateAmy Thomas, BSN, RN, IBCLCAmy Wahl, APNAnastasia Fischer, MD, FACSMAndala HardyAndrea Brun, CPNP-PCAndrea M. Boerger, MEd, CCC-SLPAndrea Sattler, MDAndrea ShellowAndrew AxelsonAndrew Kroger, MD, MPHAndrew SchwadererAndria Haynes, RNAngela AbenaimAngela Billingslea, LISW-SAnn Pakalnis, MDAnna Lillis, MD, PhDAnnette Haban-BartzAnnie Drapeau, MDAnnie Temple, MS, CCC-SLP, CLCAnnie Truelove, MPHAnthony Audino, MDAnup D.
 Patel, MDAri Rabkin, PhDAriana Hoet, PhDArielle Sheftall, PhDArleen KarczewskiAshlee HallAshleigh Kussman, MDAshley Debeljack, PsyDAshley Ebersole, MDAshley EcksteinAshley Kroon Van DiestAshley M. Davidson, AT, ATC, MSAshley Minnick, MSAH, AT, ATCAshley Overall, FNPAshley Parikh, CPNP-PCAshley Parker MSW, LISW-SAshley Parker, LISW-SAshley Tuisku, CTRSAsuncion Mejias, MD, PhDAurelia Wood, MDBailey Young, DOBecky Corbitt, RNBelinda Mills, MDBenjamin Fields, PhD, MEdBenjamin Kopp, MDBernadette Burke, AT, ATC, MSBeth Martin, RNBeth Villanueva, OTD, OTR/LBethany Uhl, MDBethany Walker, PhDBhuvana Setty, MDBill Kulju, MS, ATBlake SkinnerBonnie Gourley, MSW, LSWBrad Childers, RRT, BSBrandi Cogdill, RN, BSN, CFRN, EMT-PBrandon MorganBreanne L. Bowers, PT, DPT, CHT, CFSTBrendan Boyle, MD, MPHBrian Boe, MDBrian K. Kaspar, PhDBrian Kellogg, MDBriana Crowe, PT, DPT, OCSBrigid Pargeon, MS, MT-BCBrittany Mikuluk, M.Ed., CCLSBrittney Hardin, MOT, OTR/LBrooke Sims, LPCC, ATRCagri Toruner, MDCaitlin Bauer, RD, LDCaitlin TullyCaleb MosleyCallista DammannCallista PoppCami Winkelspecht, PhDCamille Wilson, PhDCanice Crerand, PhDCara Inglis, PsyDCarl H.
Patel, MDAri Rabkin, PhDAriana Hoet, PhDArielle Sheftall, PhDArleen KarczewskiAshlee HallAshleigh Kussman, MDAshley Debeljack, PsyDAshley Ebersole, MDAshley EcksteinAshley Kroon Van DiestAshley M. Davidson, AT, ATC, MSAshley Minnick, MSAH, AT, ATCAshley Overall, FNPAshley Parikh, CPNP-PCAshley Parker MSW, LISW-SAshley Parker, LISW-SAshley Tuisku, CTRSAsuncion Mejias, MD, PhDAurelia Wood, MDBailey Young, DOBecky Corbitt, RNBelinda Mills, MDBenjamin Fields, PhD, MEdBenjamin Kopp, MDBernadette Burke, AT, ATC, MSBeth Martin, RNBeth Villanueva, OTD, OTR/LBethany Uhl, MDBethany Walker, PhDBhuvana Setty, MDBill Kulju, MS, ATBlake SkinnerBonnie Gourley, MSW, LSWBrad Childers, RRT, BSBrandi Cogdill, RN, BSN, CFRN, EMT-PBrandon MorganBreanne L. Bowers, PT, DPT, CHT, CFSTBrendan Boyle, MD, MPHBrian Boe, MDBrian K. Kaspar, PhDBrian Kellogg, MDBriana Crowe, PT, DPT, OCSBrigid Pargeon, MS, MT-BCBrittany Mikuluk, M.Ed., CCLSBrittney Hardin, MOT, OTR/LBrooke Sims, LPCC, ATRCagri Toruner, MDCaitlin Bauer, RD, LDCaitlin TullyCaleb MosleyCallista DammannCallista PoppCami Winkelspecht, PhDCamille Wilson, PhDCanice Crerand, PhDCara Inglis, PsyDCarl H.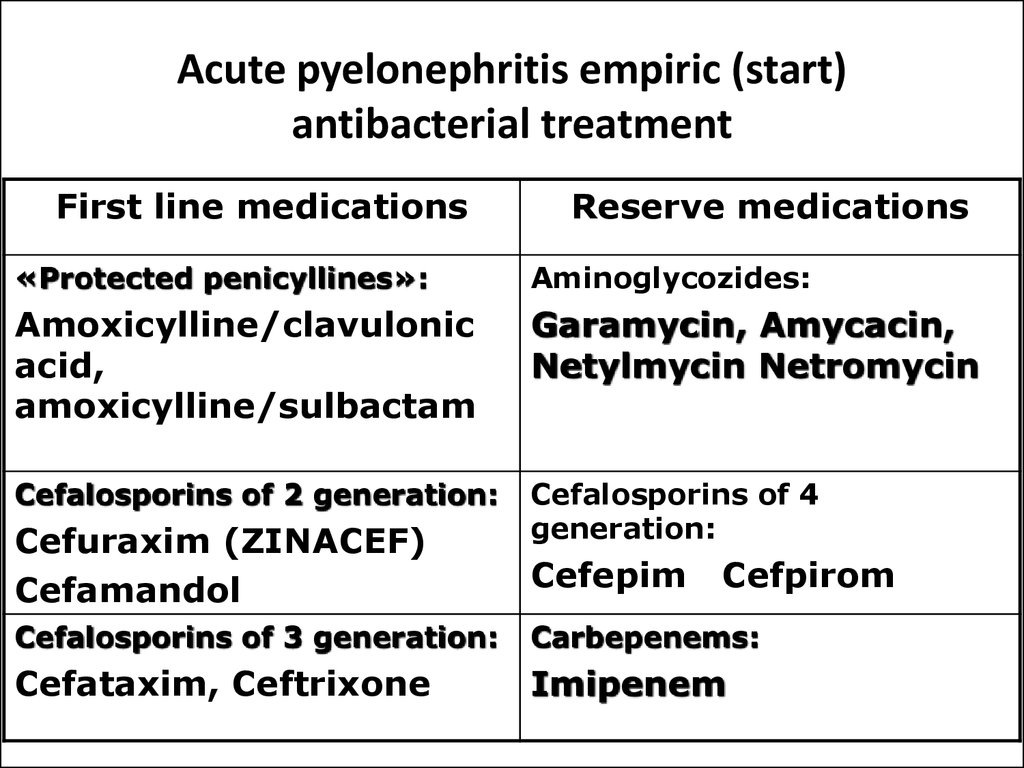 Backes, MDCarlo Di Lorenzo, MDCarly FawcettCarneshia EdwardsCarol Baumhardt, LMTCarolyn FigiCarrie Rhodes, CPST-I, MTSA, CHESCasey Cottrill, MD, MPHCasey TrimbleCassandra McNabb, RN-BSNCatherine Earlenbaugh, RNCatherine Jordan, MDCatherine Sinclair, MDCatherine Trimble, FNPCatrina Litzenburg, PhDCharae Keys, MSW, LISW-SCharles Elmaraghy, MDChelsea Britton, MS, RD, LD, CLC Chelsea Kebodeaux, MDChelsie Doster, BSCheryl Boop, MS, OTR/LCheryl G. Baxter, CPNPCheryl Gariepy, MDChet Kaczor, PharmD, MBAChris MarreroChris Smith, RNChris Westgarth-Taylor, MDChristina Ching, MDChristina DayChristine Johnson, MA, CCC-SLPChristine Koterba, PhDChristine Mansfield, PT, DPT, OCS, ATCChristine PrusaChristopher Goettee, PT, DPT, OCSChristopher Iobst, MDChristopher Ouellette, MDChristy Lumpkins, LISW-SCindy IskeClaire Kopko PT, DPT, OCS, NASM-PESCody Hostutler, PhDConnor McDanel, MSW, LSWCorey Rood, MDCorinne Syfers, CCLSCourtney Bishop. PA-CCourtney Brown, MDCourtney Hall, CPNP-PCCourtney Porter, RN, MSCristina Tomatis Souverbielle, MDCrystal MilnerCurt Daniels, MDCynthia Holland-Hall, MD, MPHDana Lenobel, FNPDana Noffsinger, CPNP-ACDane Snyder, MDDaniel Coury, MDDaniel DaJusta, MDDanielle Peifer, PT, DPTDavid A Wessells, PT, MHADavid Axelson, MDDavid Stukus, MDDean Lee, MD, PhDDebbie Terry, NPDeborah Hill, LSWDeborah Zerkle, LMTDeena Chisolm, PhDDeipanjan Nandi, MD MScDenis King, MDDenise EllDennis Cunningham, MDDennis McTigue, DDSDiane LangDominique R.
Backes, MDCarlo Di Lorenzo, MDCarly FawcettCarneshia EdwardsCarol Baumhardt, LMTCarolyn FigiCarrie Rhodes, CPST-I, MTSA, CHESCasey Cottrill, MD, MPHCasey TrimbleCassandra McNabb, RN-BSNCatherine Earlenbaugh, RNCatherine Jordan, MDCatherine Sinclair, MDCatherine Trimble, FNPCatrina Litzenburg, PhDCharae Keys, MSW, LISW-SCharles Elmaraghy, MDChelsea Britton, MS, RD, LD, CLC Chelsea Kebodeaux, MDChelsie Doster, BSCheryl Boop, MS, OTR/LCheryl G. Baxter, CPNPCheryl Gariepy, MDChet Kaczor, PharmD, MBAChris MarreroChris Smith, RNChris Westgarth-Taylor, MDChristina Ching, MDChristina DayChristine Johnson, MA, CCC-SLPChristine Koterba, PhDChristine Mansfield, PT, DPT, OCS, ATCChristine PrusaChristopher Goettee, PT, DPT, OCSChristopher Iobst, MDChristopher Ouellette, MDChristy Lumpkins, LISW-SCindy IskeClaire Kopko PT, DPT, OCS, NASM-PESCody Hostutler, PhDConnor McDanel, MSW, LSWCorey Rood, MDCorinne Syfers, CCLSCourtney Bishop. PA-CCourtney Brown, MDCourtney Hall, CPNP-PCCourtney Porter, RN, MSCristina Tomatis Souverbielle, MDCrystal MilnerCurt Daniels, MDCynthia Holland-Hall, MD, MPHDana Lenobel, FNPDana Noffsinger, CPNP-ACDane Snyder, MDDaniel Coury, MDDaniel DaJusta, MDDanielle Peifer, PT, DPTDavid A Wessells, PT, MHADavid Axelson, MDDavid Stukus, MDDean Lee, MD, PhDDebbie Terry, NPDeborah Hill, LSWDeborah Zerkle, LMTDeena Chisolm, PhDDeipanjan Nandi, MD MScDenis King, MDDenise EllDennis Cunningham, MDDennis McTigue, DDSDiane LangDominique R.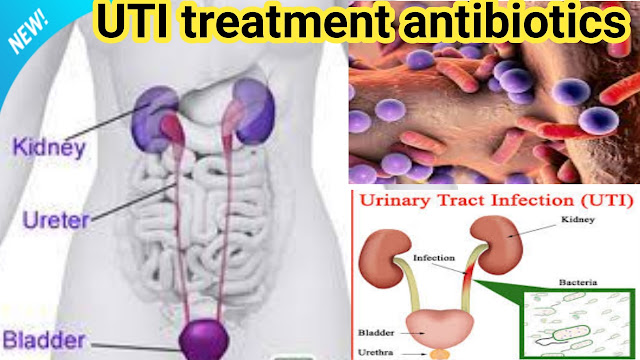 Williams, MD, MPH, FAAP, Dipl ABOMDonna M. Trentel, MSA, CCLSDonna Ruch, PhDDonna TeachDoug WolfDouglas McLaughlin, MDDrew Duerson, MDEd MinerEdward Oberle, MD, RhMSUSEdward Shepherd, MDEileen Chaves, PhDElena CamachoElise Berlan, MDElise DawkinsElizabeth A. Cannon, LPCCElizabeth Cipollone, LPCC-SElizabeth Murray, MDElizabeth Zmuda, DOEllyn Hamm, MM, MT-BCEmily A. Stuart, MDEmily Decker, MDEmily GetschmanEmma Wysocki, PharmD, RDNEric Butter, PhDEric Leighton, AT, ATCEric Sribnick, MD, PhDErica Domrose, RD, LDEricca L Lovegrove, RD, LDErika RobertsErin Gates, PT, DPTErin Johnson, M.Ed., C.S.C.S.Erin McKnight, MD, MPHErin Shann, BSN, RNErin TebbenFarah W. Brink, MDFatimah MasoodFrances Fei, MDGail Bagwell, DNP, APRN, CNSGail Besner, MDGail Swisher, ATGarey Noritz, MDGary A. Smith, MD, DrPHGeri Hewitt, MDGina Hounam, PhDGina McDowellGina MinotGrace Paul, MDGregory D. Pearson, MDGriffin Stout, MDGuliz Erdem, MDHailey Blosser, MA, CCC-SLPHanna MathessHannah Barton, PhDHeather Battles, MDHeather ClarkHeather L.
Williams, MD, MPH, FAAP, Dipl ABOMDonna M. Trentel, MSA, CCLSDonna Ruch, PhDDonna TeachDoug WolfDouglas McLaughlin, MDDrew Duerson, MDEd MinerEdward Oberle, MD, RhMSUSEdward Shepherd, MDEileen Chaves, PhDElena CamachoElise Berlan, MDElise DawkinsElizabeth A. Cannon, LPCCElizabeth Cipollone, LPCC-SElizabeth Murray, MDElizabeth Zmuda, DOEllyn Hamm, MM, MT-BCEmily A. Stuart, MDEmily Decker, MDEmily GetschmanEmma Wysocki, PharmD, RDNEric Butter, PhDEric Leighton, AT, ATCEric Sribnick, MD, PhDErica Domrose, RD, LDEricca L Lovegrove, RD, LDErika RobertsErin Gates, PT, DPTErin Johnson, M.Ed., C.S.C.S.Erin McKnight, MD, MPHErin Shann, BSN, RNErin TebbenFarah W. Brink, MDFatimah MasoodFrances Fei, MDGail Bagwell, DNP, APRN, CNSGail Besner, MDGail Swisher, ATGarey Noritz, MDGary A. Smith, MD, DrPHGeri Hewitt, MDGina Hounam, PhDGina McDowellGina MinotGrace Paul, MDGregory D. Pearson, MDGriffin Stout, MDGuliz Erdem, MDHailey Blosser, MA, CCC-SLPHanna MathessHannah Barton, PhDHeather Battles, MDHeather ClarkHeather L.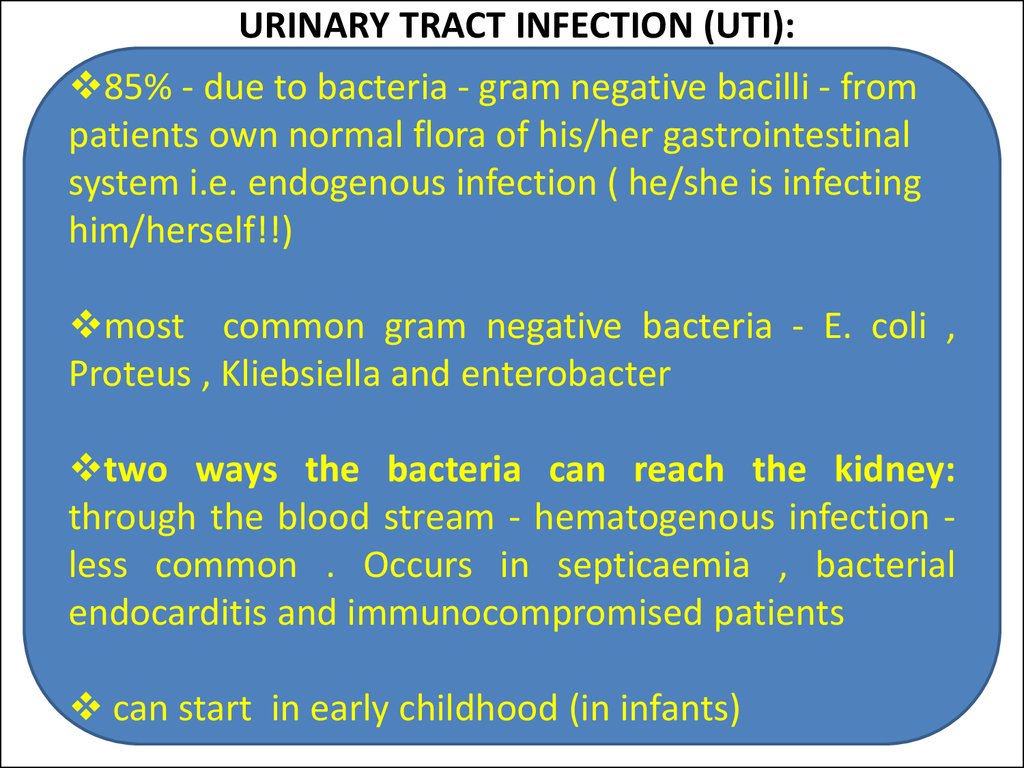 Terry, MSN, RN, FNP-C, CUNPHeather Yardley, PhDHenry SpillerHenry Xiang, MD, MPH, PhDHerman Hundley, MS, AT, ATC, CSCSHersh Varma, MDHilary Michel, MDHiren Patel, MDHolly Deckling, MSSW, LISWHoma Amini, DDS, MPH, MSHoward Jacobs, MDHunter Wernick, DOIbrahim Khansa, MDIhuoma Eneli, MDIlana Moss, PhDIlene Crabtree, PTIrene Mikhail, MDIrina Buhimschi, MDIvor Hill, MDJackie Cronau, RN, CWOCNJacqueline Wynn, PhD, BCBA-DJacquelyn Doxie King, PhDJaime-Dawn Twanow, MDJaimie D. Nathan, MD, FACSJames Murakami, MDJames Popp, MDJames Ruda, MDJameson Mattingly, MDJamie Macklin, MDJamie ReedyJane AbelJanelle Huefner, MA, CCC-SLPJanice M. Moreland, CPNP-PC, DNPJanice Townsend, DDS, MSJared SylvesterJason JacksonJason P. Garee, PhDJaysson EicholtzJean Hruschak, MA, CCC/SLPJeff Sydes, CSCSJeffery Auletta, MDJeffrey Bennett, MD, PhDJeffrey Hoffman, MDJeffrey Leonard, MDJen Campbell, PT, MSPTJena HeckJenn Gonya, PhDJennie Aldrink, MDJennifer Borda, PT, DPTJennifer HofherrJennifer LockerJennifer PrinzJennifer Reese, PsyDJennifer Smith, MS, RD, CSP, LD, LMTJennifer Walton, MD, MPH, FAAPJenny Worthington, PT, DPTJerry R.
Terry, MSN, RN, FNP-C, CUNPHeather Yardley, PhDHenry SpillerHenry Xiang, MD, MPH, PhDHerman Hundley, MS, AT, ATC, CSCSHersh Varma, MDHilary Michel, MDHiren Patel, MDHolly Deckling, MSSW, LISWHoma Amini, DDS, MPH, MSHoward Jacobs, MDHunter Wernick, DOIbrahim Khansa, MDIhuoma Eneli, MDIlana Moss, PhDIlene Crabtree, PTIrene Mikhail, MDIrina Buhimschi, MDIvor Hill, MDJackie Cronau, RN, CWOCNJacqueline Wynn, PhD, BCBA-DJacquelyn Doxie King, PhDJaime-Dawn Twanow, MDJaimie D. Nathan, MD, FACSJames Murakami, MDJames Popp, MDJames Ruda, MDJameson Mattingly, MDJamie Macklin, MDJamie ReedyJane AbelJanelle Huefner, MA, CCC-SLPJanice M. Moreland, CPNP-PC, DNPJanice Townsend, DDS, MSJared SylvesterJason JacksonJason P. Garee, PhDJaysson EicholtzJean Hruschak, MA, CCC/SLPJeff Sydes, CSCSJeffery Auletta, MDJeffrey Bennett, MD, PhDJeffrey Hoffman, MDJeffrey Leonard, MDJen Campbell, PT, MSPTJena HeckJenn Gonya, PhDJennie Aldrink, MDJennifer Borda, PT, DPTJennifer HofherrJennifer LockerJennifer PrinzJennifer Reese, PsyDJennifer Smith, MS, RD, CSP, LD, LMTJennifer Walton, MD, MPH, FAAPJenny Worthington, PT, DPTJerry R.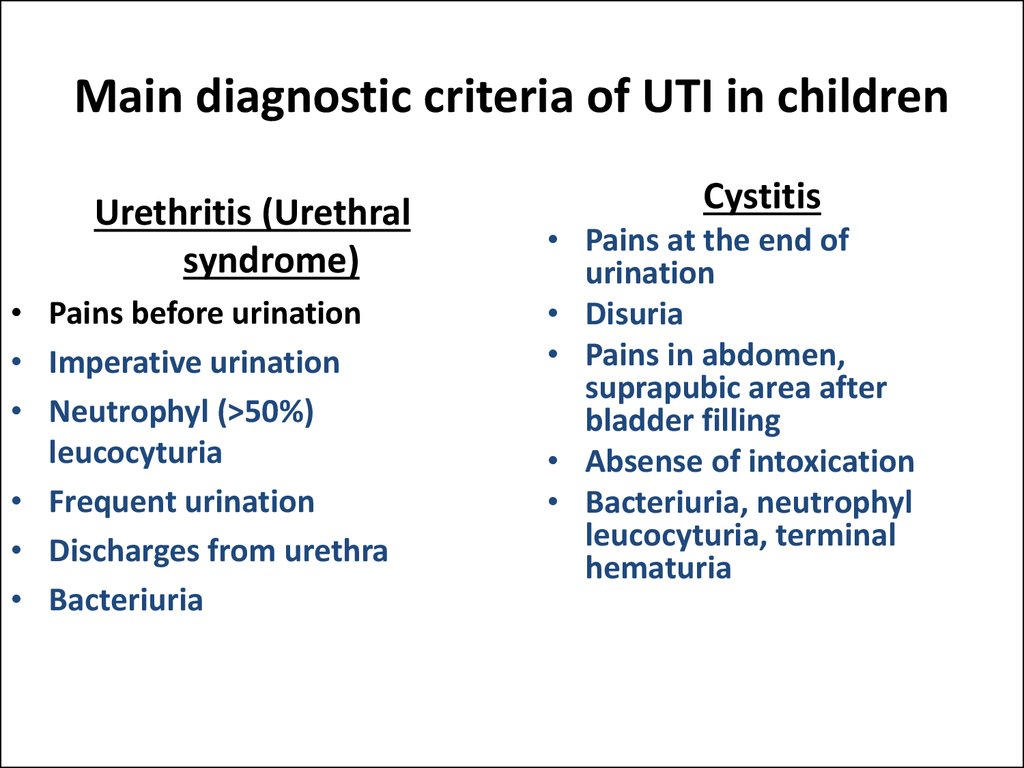 Mendell, MDJessalyn Mayer, MSOT, OTR/LJessica Bailey, PsyDJessica Bogacik, MS, MT-BCJessica Bowman, MDJessica BrockJessica Bullock, MA/CCC-SLPJessica Buschmann, RDJessica Scherr, PhDJim O’Shea OT, MOT, CHTJoan Fraser, MSW, LISW-SJohn Ackerman, PhDJohn Caballero, PT, DPT, CSCSJohn Kovalchin, MDJonathan D. Thackeray, MDJonathan Finlay, MB, ChB, FRCPJonathan M. Grischkan, MDJonathan Napolitano, MDJoshua Prudent, MDJoshua Watson, MDJulee Eing, CRA, RT(R)Julia Colman, MOT, OTR/LJulie ApthorpeJulie Lange, MDJulie Leonard, MD, MPHJulie Racine, PhDJulie Samora, MDJun Yasuhara, MDJustin Indyk, MD, PhDKady LacyKaitrin Kramer, DDS, MS, PhDKaleigh Hague, MA, MT-BCKaleigh MatesickKamilah Twymon, LPCC-SKara Malone, MDKara Miller, OTR/LKaren A. Diefenbach, MDKaren Allen, MDKaren Days, MBAKaren Rachuba, RD, LD, CLCKari A. Meeks, OTKari Cardiff, ODKari Dubro, MS, RD, LD, CWWSKari Phang, MDKarla Vaz, MDKaryn L. Kassis, MD, MPHKasey Strothman, MDKatelyn Krivchenia, MDKatherine Deans, MDKatherine McCracken, MD FACOGKatherine ReddenKathleen (Katie) RoushKathleen Nicol, MDKathryn Blocher, CPNP-PCKathryn J.
Mendell, MDJessalyn Mayer, MSOT, OTR/LJessica Bailey, PsyDJessica Bogacik, MS, MT-BCJessica Bowman, MDJessica BrockJessica Bullock, MA/CCC-SLPJessica Buschmann, RDJessica Scherr, PhDJim O’Shea OT, MOT, CHTJoan Fraser, MSW, LISW-SJohn Ackerman, PhDJohn Caballero, PT, DPT, CSCSJohn Kovalchin, MDJonathan D. Thackeray, MDJonathan Finlay, MB, ChB, FRCPJonathan M. Grischkan, MDJonathan Napolitano, MDJoshua Prudent, MDJoshua Watson, MDJulee Eing, CRA, RT(R)Julia Colman, MOT, OTR/LJulie ApthorpeJulie Lange, MDJulie Leonard, MD, MPHJulie Racine, PhDJulie Samora, MDJun Yasuhara, MDJustin Indyk, MD, PhDKady LacyKaitrin Kramer, DDS, MS, PhDKaleigh Hague, MA, MT-BCKaleigh MatesickKamilah Twymon, LPCC-SKara Malone, MDKara Miller, OTR/LKaren A. Diefenbach, MDKaren Allen, MDKaren Days, MBAKaren Rachuba, RD, LD, CLCKari A. Meeks, OTKari Cardiff, ODKari Dubro, MS, RD, LD, CWWSKari Phang, MDKarla Vaz, MDKaryn L. Kassis, MD, MPHKasey Strothman, MDKatelyn Krivchenia, MDKatherine Deans, MDKatherine McCracken, MD FACOGKatherine ReddenKathleen (Katie) RoushKathleen Nicol, MDKathryn Blocher, CPNP-PCKathryn J.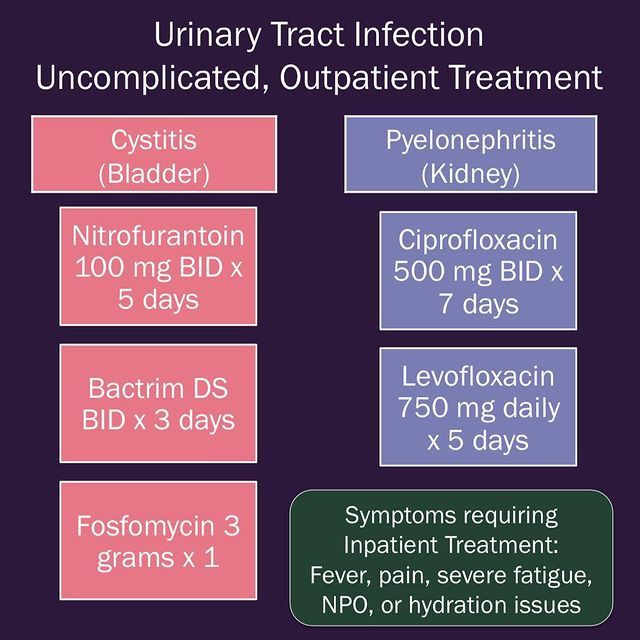 Junge, RN, BSNKathryn Obrynba, MDKatia Camille Halabi, MDKatie Brind'Amour, MSKatie DonovanKatie Thomas, APRKatrina Hall, MA, CCLSKatrina Ruege, LPCC-SKatya Harfmann, MDKayla Zimpfer, PCCKaylan Guzman Schauer, LPCC-SKeli YoungKelley SwopeKelli Dilver, PT, DPTKelly AbramsKelly BooneKelly HustonKelly J. Kelleher, MDKelly McNally, PhDKelly N. Day, CPNP-PCKelly Pack, LISW-SKelly Tanner,PhD, OTR/L, BCPKelly Wesolowski, PsyDKelly Wise, PharmDKent Williams, MDKevin Bosse, PhDKevin Klingele, MDKim Bjorklund, MDKim Hammersmith, DDS, MPH, MSKimberly Bates, MDKimberly Jones, PharmDKimberly Sisto, PT, DPT, SCSKimberly Van Camp, PT, DPT, SCSKirk SabalkaKris Jatana, MD, FAAPKrista Winner, AuD, CCC-AKristen Armbrust, LISW-SKristen Cannon, MDKristen E. Beck, MDKristen Martin, OTR/LKristi Roberts, MS MPHKristina Booth, MSN, CFNPKristina Reber, MDKristol Das, MDKyle DavisLance Governale, MDLara McKenzie, PhD, MALaura Brubaker, BSN, RNLaura Dattner, MALaura Martin, MDLaurel Biever, LPCLauren Durinka, AuDLauren Garbacz, PhDLauren Justice, OTR/L, MOTLauren Madhoun, MS, CCC-SLPLauryn Rozum, MS, CCLSLeah Middelberg, MDLee Hlad, DPMLeena Nahata, MDLelia Emery, MT-BCLeslie Appiah, MDLinda Stoverock, DNP, RN NEA-BCLindsay Kneen, MDLindsay Pietruszewski, PT, DPTLindsay SchwartzLindsey Vater, PsyDLisa GoldenLisa Halloran, CNPLisa M.
Junge, RN, BSNKathryn Obrynba, MDKatia Camille Halabi, MDKatie Brind'Amour, MSKatie DonovanKatie Thomas, APRKatrina Hall, MA, CCLSKatrina Ruege, LPCC-SKatya Harfmann, MDKayla Zimpfer, PCCKaylan Guzman Schauer, LPCC-SKeli YoungKelley SwopeKelli Dilver, PT, DPTKelly AbramsKelly BooneKelly HustonKelly J. Kelleher, MDKelly McNally, PhDKelly N. Day, CPNP-PCKelly Pack, LISW-SKelly Tanner,PhD, OTR/L, BCPKelly Wesolowski, PsyDKelly Wise, PharmDKent Williams, MDKevin Bosse, PhDKevin Klingele, MDKim Bjorklund, MDKim Hammersmith, DDS, MPH, MSKimberly Bates, MDKimberly Jones, PharmDKimberly Sisto, PT, DPT, SCSKimberly Van Camp, PT, DPT, SCSKirk SabalkaKris Jatana, MD, FAAPKrista Winner, AuD, CCC-AKristen Armbrust, LISW-SKristen Cannon, MDKristen E. Beck, MDKristen Martin, OTR/LKristi Roberts, MS MPHKristina Booth, MSN, CFNPKristina Reber, MDKristol Das, MDKyle DavisLance Governale, MDLara McKenzie, PhD, MALaura Brubaker, BSN, RNLaura Dattner, MALaura Martin, MDLaurel Biever, LPCLauren Durinka, AuDLauren Garbacz, PhDLauren Justice, OTR/L, MOTLauren Madhoun, MS, CCC-SLPLauryn Rozum, MS, CCLSLeah Middelberg, MDLee Hlad, DPMLeena Nahata, MDLelia Emery, MT-BCLeslie Appiah, MDLinda Stoverock, DNP, RN NEA-BCLindsay Kneen, MDLindsay Pietruszewski, PT, DPTLindsay SchwartzLindsey Vater, PsyDLisa GoldenLisa Halloran, CNPLisa M.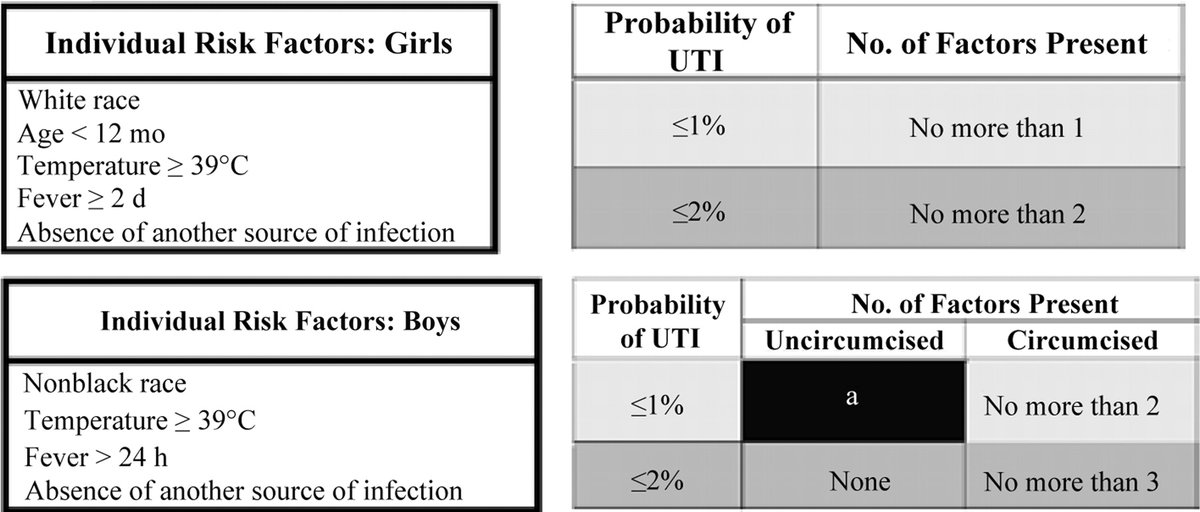 Humphrey, MDLogan Blankemeyer, MA, CCC-SLPLori Grisez PT, DPTLorraine Kelley-QuonLouis Bezold, MDLourdes Hill, LPCC-S Lubna Mazin, PharmDLuke Tipple, MS, CSCSLynda Wolfe, PhDLyndsey MillerLynn RosenthalLynne Ruess, MDMaggy Rule, MS, AT, ATCMahmoud Kallash, MDManmohan K Kamboj, MDMarc DutroMarc P. Michalsky, MDMarcel J. Casavant, MDMarci Johnson, LISW-SMarcie RehmarMarco Corridore, MDMargaret Bassi, OTR/LMaria HaghnazariMaria Vegh, MSN, RN, CPNMarissa Condon, BSN, RNMarissa E. Larouere, MBA, BSN, RNMark E. Galantowicz, MDMark Smith, MS RT R (MR), ABMP PhysicistMarnie Wagner, MDMary Ann Abrams, MD, MPHMary Fristad, PhD, ABPPMary Kay SharrettMary Shull, MDMatthew Washam, MD, MPHMeagan Horn, MAMegan Brundrett, MDMegan Dominik, OTR/LMegan FrancisMegan Letson, MD, M.EdMeghan Cass, PT, DPTMeghan Fisher, BSN, RNMeika Eby, MDMelanie Fluellen, LPCCMelanie Luken, LISW-SMelissa and Mikael McLarenMelissa McMillen, CTRSMelissa Winterhalter, MDMeredith Merz Lind, MDMichael Flores, PhDMichael T. Brady, MDMichelle Ross, MHA, RD, LD, ALCMike Patrick, MDMindy Deno, PT, DPTMitch Ellinger, CPNP-PCMolly Dienhart, MDMolly Fuchs, MDMolly Gardner, PhDMonica Ardura, DOMonica EllisMonique Goldschmidt, MDMotao Zhu, MD, MS, PhDMurugu Manickam, MDNancy AuerNancy Cunningham, PsyDNancy Wright, BS, RRT, RCP, AE-C Naomi Kertesz, MDNatalie DeBaccoNatalie I.
Humphrey, MDLogan Blankemeyer, MA, CCC-SLPLori Grisez PT, DPTLorraine Kelley-QuonLouis Bezold, MDLourdes Hill, LPCC-S Lubna Mazin, PharmDLuke Tipple, MS, CSCSLynda Wolfe, PhDLyndsey MillerLynn RosenthalLynne Ruess, MDMaggy Rule, MS, AT, ATCMahmoud Kallash, MDManmohan K Kamboj, MDMarc DutroMarc P. Michalsky, MDMarcel J. Casavant, MDMarci Johnson, LISW-SMarcie RehmarMarco Corridore, MDMargaret Bassi, OTR/LMaria HaghnazariMaria Vegh, MSN, RN, CPNMarissa Condon, BSN, RNMarissa E. Larouere, MBA, BSN, RNMark E. Galantowicz, MDMark Smith, MS RT R (MR), ABMP PhysicistMarnie Wagner, MDMary Ann Abrams, MD, MPHMary Fristad, PhD, ABPPMary Kay SharrettMary Shull, MDMatthew Washam, MD, MPHMeagan Horn, MAMegan Brundrett, MDMegan Dominik, OTR/LMegan FrancisMegan Letson, MD, M.EdMeghan Cass, PT, DPTMeghan Fisher, BSN, RNMeika Eby, MDMelanie Fluellen, LPCCMelanie Luken, LISW-SMelissa and Mikael McLarenMelissa McMillen, CTRSMelissa Winterhalter, MDMeredith Merz Lind, MDMichael Flores, PhDMichael T. Brady, MDMichelle Ross, MHA, RD, LD, ALCMike Patrick, MDMindy Deno, PT, DPTMitch Ellinger, CPNP-PCMolly Dienhart, MDMolly Fuchs, MDMolly Gardner, PhDMonica Ardura, DOMonica EllisMonique Goldschmidt, MDMotao Zhu, MD, MS, PhDMurugu Manickam, MDNancy AuerNancy Cunningham, PsyDNancy Wright, BS, RRT, RCP, AE-C Naomi Kertesz, MDNatalie DeBaccoNatalie I.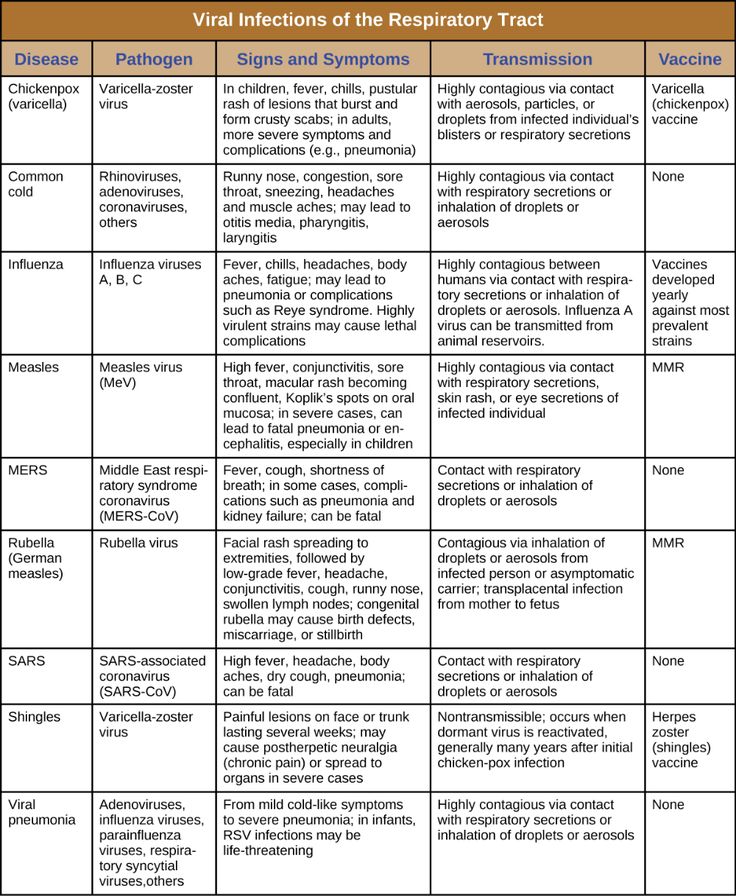 Rine, PharmD, BCPS, BCCCPNatalie Powell, LPCC-S, LICDC-CSNatalie Rose, BSN, RNNathalie Maitre, MD, PhDNationwide Children's HospitalNationwide Children's Hospital Behavioral Health ExpertsNeetu Bali, MD, MPHNehal Parikh, DO, MSNichole Mayer, OTR/L, MOTNicole Caldwell, MDNicole Dempster, PhDNicole Greenwood, MDNicole Parente, LSWNicole Powell, PsyD, BCBA-DNina WestNkeiruka Orajiaka, MBBSOctavio Ramilo, MDOliver Adunka, MD, FACSOlivia Silvera, CPNP-PCOlivia Stranges, CPNP-PCOlivia Thomas, MDOmar Khalid, MD, FAAP, FACCOnnalisa Nash, CPNP-PCOula KhouryPaige Duly, CTRSParker Huston, PhDPatrick C. Walz, MDPatrick Queen, BSN, RNPedro Weisleder, MDPeter Minneci, MDPeter White, PhDPitty JenningsPreeti Jaggi, MDPriyal Patel, DORachael Morocco-Zanotti, DORachel D’Amico, MDRachel Schrader, CPNP-PCRachel Tyson, LSWRajan Thakkar, MDRaymond Troy, MDRebecca Fisher, PTRebecca Hicks, CCLSRebecca Lewis, AuD, CCC-ARebecca M. Romero, RD, LD, CLC Reggie Ash Jr.Reilly Harrington, CCC-SLPReno Ravindran, MDRichard Kirschner, MDRichard Wood, MDRobert A.
Rine, PharmD, BCPS, BCCCPNatalie Powell, LPCC-S, LICDC-CSNatalie Rose, BSN, RNNathalie Maitre, MD, PhDNationwide Children's HospitalNationwide Children's Hospital Behavioral Health ExpertsNeetu Bali, MD, MPHNehal Parikh, DO, MSNichole Mayer, OTR/L, MOTNicole Caldwell, MDNicole Dempster, PhDNicole Greenwood, MDNicole Parente, LSWNicole Powell, PsyD, BCBA-DNina WestNkeiruka Orajiaka, MBBSOctavio Ramilo, MDOliver Adunka, MD, FACSOlivia Silvera, CPNP-PCOlivia Stranges, CPNP-PCOlivia Thomas, MDOmar Khalid, MD, FAAP, FACCOnnalisa Nash, CPNP-PCOula KhouryPaige Duly, CTRSParker Huston, PhDPatrick C. Walz, MDPatrick Queen, BSN, RNPedro Weisleder, MDPeter Minneci, MDPeter White, PhDPitty JenningsPreeti Jaggi, MDPriyal Patel, DORachael Morocco-Zanotti, DORachel D’Amico, MDRachel Schrader, CPNP-PCRachel Tyson, LSWRajan Thakkar, MDRaymond Troy, MDRebecca Fisher, PTRebecca Hicks, CCLSRebecca Lewis, AuD, CCC-ARebecca M. Romero, RD, LD, CLC Reggie Ash Jr.Reilly Harrington, CCC-SLPReno Ravindran, MDRichard Kirschner, MDRichard Wood, MDRobert A. Kowatch, MD, Ph.D.Robert Hoffman, MDRochelle Krouse, CTRSRohan Henry, MD, MSRose Ayoob, MDRose Schroedl, PhDRosemary Martoma, MDRoss Maltz, MDRustin Morse, MDRyan Ingley AT, ATCSamanta Boddapati, PhDSamantha MaloneSammy CygnorSandra C. Kim, MDSara Bentley, MT-BCSara Bode, MDSara Breidigan, MS, AT, ATCSara N. Smith, MSN, APRNSara O'Rourke, MOT, OTR/L, Clinical LeadSara Schroder, MDSarah A. Denny, MDSarah Cline, CRA, RT(R)Sarah Driesbach, CPN, APNSarah GreenbergSarah Hastie, BSN, RNC-NIC Sarah Keim, PhDSarah MyersSarah O'Brien, MDSarah SaxbeSarah Schmidt, LISW-SSarah ScottSarah TraceySarah VerLee, PhDSasigarn Bowden, MDSatya Gedela, MD, MRCP(UK)Scott Coven, DO, MPHScott Hickey, MDSean EingSean Rose, MDSeth Alpert, MDShalini C. Reshmi, PhD, FACMGShana Moore, MA, CCC-AShannon Reinhart, LISW-SShari UncapherSharon Wrona, DNP, PNP, PMHSShaun Coffman PT, DPT, OCSShawn Pitcher, BS, RD, USAWShawNaye Scott-MillerShea SmoskeSheena PaceSheila GilesShelly BrackmanSimon Lee, MDSini James, MDStacy Ardoin, MDStacy Whiteside APRN, MS, CPNP-AC/PC, CPONStefanie Bester, MDStefanie Hirota, OTR/LStephanie Burkhardt, MPH, CCRCStephanie CannonStephanie Santoro, MDStephanie TownsendStephanie Vyrostek BSN, RNStephen Hersey, MDSteve Allen, MDSteven C.
Kowatch, MD, Ph.D.Robert Hoffman, MDRochelle Krouse, CTRSRohan Henry, MD, MSRose Ayoob, MDRose Schroedl, PhDRosemary Martoma, MDRoss Maltz, MDRustin Morse, MDRyan Ingley AT, ATCSamanta Boddapati, PhDSamantha MaloneSammy CygnorSandra C. Kim, MDSara Bentley, MT-BCSara Bode, MDSara Breidigan, MS, AT, ATCSara N. Smith, MSN, APRNSara O'Rourke, MOT, OTR/L, Clinical LeadSara Schroder, MDSarah A. Denny, MDSarah Cline, CRA, RT(R)Sarah Driesbach, CPN, APNSarah GreenbergSarah Hastie, BSN, RNC-NIC Sarah Keim, PhDSarah MyersSarah O'Brien, MDSarah SaxbeSarah Schmidt, LISW-SSarah ScottSarah TraceySarah VerLee, PhDSasigarn Bowden, MDSatya Gedela, MD, MRCP(UK)Scott Coven, DO, MPHScott Hickey, MDSean EingSean Rose, MDSeth Alpert, MDShalini C. Reshmi, PhD, FACMGShana Moore, MA, CCC-AShannon Reinhart, LISW-SShari UncapherSharon Wrona, DNP, PNP, PMHSShaun Coffman PT, DPT, OCSShawn Pitcher, BS, RD, USAWShawNaye Scott-MillerShea SmoskeSheena PaceSheila GilesShelly BrackmanSimon Lee, MDSini James, MDStacy Ardoin, MDStacy Whiteside APRN, MS, CPNP-AC/PC, CPONStefanie Bester, MDStefanie Hirota, OTR/LStephanie Burkhardt, MPH, CCRCStephanie CannonStephanie Santoro, MDStephanie TownsendStephanie Vyrostek BSN, RNStephen Hersey, MDSteve Allen, MDSteven C. Matson, MDSteven Ciciora, MDSteven CuffSuellen Sharp, OTR/L, MOTSurlina AsamoaSusan Colace, MDSusan Creary, MDSwaroop Pinto, MDTabatha BallardTabbetha GrecoTabi Evans, PsyDTabitha Jones-McKnight, DOTahagod Mohamed, MDTamara MappTammi Young-Saleme, PhDTaylor Hartlaub, MD, MPHTenelle JonesTerry Barber, MDTerry Bravender, MD, MPHTerry Laurila, MS, RPhTheresa Miller, BA, RRT, RCP, AE-C, CPFTThomas Pommering, DOTiasha Letostak, PhDTiffanie Ryan, BCBA Tim RobinsonTim Smith, MDTimothy Cripe, MD, PhDTimothy Landers PhD RN APRN-CNP CIC FAANTracey L. Sisk, RN, BSN, MHATracie Steinke RD, LD, CDETracy Mehan, MATravis Gallagher, ATTrevor MillerTria Shadeed, NNPTyanna Snider, PsyDTyler Congrove, ATValencia Walker, MD, MPH, FAAPVanessa Shanks, MD, FAAPVenkata Rama Jayanthi, MDVidu Garg, MDVidya Raman, MDVidya Sivaraman, MDW. Garrett Hunt, MDWalter Samora, MDWarren D. Lo, MDWendy Anderson, MDWendy Cleveland, MA, LPCC-SWhitney McCormick, CTRSWhitney Raglin Bignall, PhDWilliam Cotton, MDWilliam J. Barson, MDWilliam Ray, PhDWilliam W.
Matson, MDSteven Ciciora, MDSteven CuffSuellen Sharp, OTR/L, MOTSurlina AsamoaSusan Colace, MDSusan Creary, MDSwaroop Pinto, MDTabatha BallardTabbetha GrecoTabi Evans, PsyDTabitha Jones-McKnight, DOTahagod Mohamed, MDTamara MappTammi Young-Saleme, PhDTaylor Hartlaub, MD, MPHTenelle JonesTerry Barber, MDTerry Bravender, MD, MPHTerry Laurila, MS, RPhTheresa Miller, BA, RRT, RCP, AE-C, CPFTThomas Pommering, DOTiasha Letostak, PhDTiffanie Ryan, BCBA Tim RobinsonTim Smith, MDTimothy Cripe, MD, PhDTimothy Landers PhD RN APRN-CNP CIC FAANTracey L. Sisk, RN, BSN, MHATracie Steinke RD, LD, CDETracy Mehan, MATravis Gallagher, ATTrevor MillerTria Shadeed, NNPTyanna Snider, PsyDTyler Congrove, ATValencia Walker, MD, MPH, FAAPVanessa Shanks, MD, FAAPVenkata Rama Jayanthi, MDVidu Garg, MDVidya Raman, MDVidya Sivaraman, MDW. Garrett Hunt, MDWalter Samora, MDWarren D. Lo, MDWendy Anderson, MDWendy Cleveland, MA, LPCC-SWhitney McCormick, CTRSWhitney Raglin Bignall, PhDWilliam Cotton, MDWilliam J. Barson, MDWilliam Ray, PhDWilliam W. Long, MD
Long, MD
Urinary Tract Infections in the Infant
1. Shaikh N, Morone NE, Bost JE, et al. Prevalence of urinary tract infection in childhood: a meta-analysis. Pediatr Infect Dis J. 2008;27:302–8. [PubMed] [Google Scholar]
2. Ismaili K, Lolin K, Damry N, et al. Febrile urinary tract infections in 0- to 3-month-old infants: a prospective follow-up study. J Pediatr. 2011;158:91–4. [PubMed] [Google Scholar]
3. Zorc JJ, Levine DA, Platt SL, et al. Clinical and demographic factors associated with urinary tract infection in young febrile infants. Pediatrics. 2005;116:644–8. [PubMed] [Google Scholar]
4. Lin DS, Huang SH, Lin CC, et al. Urinary tract infection in febrile infants younger than eight weeks of Age. Pediatrics. 2000;105:E20. [PubMed] [Google Scholar]
5. Bonadio W, Maida G. Urinary tract infection in outpatient febrile infants younger than 30 days of age: a 10-year evaluation. Pediatr Infect Dis J. 2014;33:342–4.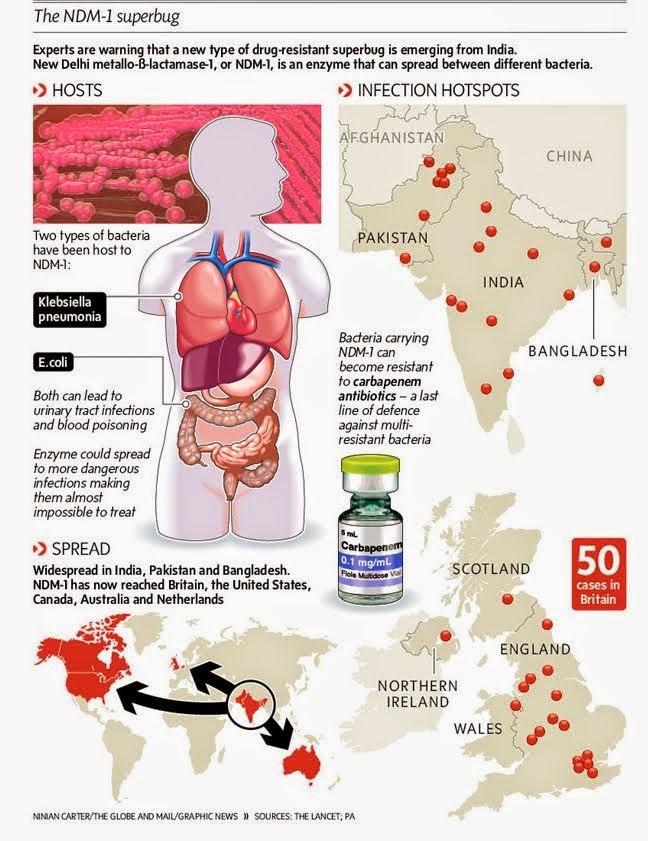 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
6. Morley EJ, Lapoint JM, Roy LW, et al. Rates of positive blood, urine, and cerebrospinal fluid cultures in children younger than 60 days during the vaccination era. Pediatr Emerg Care. 2012;28:125–30. [PubMed] [Google Scholar]
7. Visser VE, Hall RT. Urine culture in the evaluation of suspected neonatal sepsis. J Pediatr. 1979;94:635–8. [PubMed] [Google Scholar]
8. Tamim MM, Alesseh H, Aziz H. Analysis of the efficacy of urine culture as part of sepsis evaluation in the premature infant. Pediatr Infect Dis J. 2003;22:805–8. [PubMed] [Google Scholar]
9. Riskin A, Toropine A, Bader D, et al. Is it justified to include urine cultures in early (<72 hours) neonatal sepsis evaluations of term and late preterm infants? Am J Perinatol. 2013;30:499–504. [PubMed] [Google Scholar]
10. Samayam P, Ravi Chander B. Study of urinary tract infection and bacteriuria in neonatal sepsis. Indian J Pediatr. 2012;79:1033–6. [PubMed] [Google Scholar]
11. Wang SF, Huang FY, Chiu NC, et al. Urinary tract infection in infants less than 2 months of age. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1994;35:294–300. [PubMed] [Google Scholar]
Wang SF, Huang FY, Chiu NC, et al. Urinary tract infection in infants less than 2 months of age. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1994;35:294–300. [PubMed] [Google Scholar]
12. Kanellopoulos TA, Salakos C, Spiliopoulou I, et al. First urinary tract infection in neonates, infants and young children: a comparative study. Pediatr Nephrol. 2006;21:1131–7. [PubMed] [Google Scholar]
13. Didier C, Streicher MP, Chognot D, et al. Late-onset neonatal infections: incidences and pathogens in the era of antenatal antibiotics. Eur J Pediatr. 2012;171:681–7. [PubMed] [Google Scholar]
14. Watt K, Waddle E, Jhaveri R. Changing epidemiology of serious bacterial infections in febrile infants without localizing signs. PLoS One. 2010;5:e12448. [PMC free article] [PubMed] [Google Scholar]
15. Lo DS, Shieh HH, Ragazzi SL, et al. Community-acquired urinary tract infection: age and gender-dependent etiology. J Bras Nefrol. 2013;35:93–8. [PubMed] [Google Scholar]
16. Bitsori M, Maraki S, Raissaki M, et al. Community-acquired enterococcal urinary tract infections. Pediatr Nephrol. 2005;20:1583–6. [PubMed] [Google Scholar]
Bitsori M, Maraki S, Raissaki M, et al. Community-acquired enterococcal urinary tract infections. Pediatr Nephrol. 2005;20:1583–6. [PubMed] [Google Scholar]
17. Zurina Z, Rohani A, Neela V, et al. Late onset group b beta-hemolytic streptococcus infection in a neonate manifesting as a urinary tract infection: a rare clinical presentation. Southeast Asian J Trop Med Public Health. 2012;43:1470–3. [PubMed] [Google Scholar]
18. Hassoun A, Stankovic C, Rogers A, et al. Listeria and enterococcal infections in neonates 28 days of age and younger: is empiric parenteral ampicillin still indicated? Pediatr Emerg Care. 2014;30:240–3. [PubMed] [Google Scholar]
19. Downey LC, Benjamin DK, Jr, Clark RH, et al. Urinary tract infection concordance with positive blood and cerebrospinal fluid cultures in the neonatal intensive care unit. J Perinatol. 2013;33:302–6. [PMC free article] [PubMed] [Google Scholar]
20. Jean-Baptiste N, Benjamin DK, Jr, Cohen-Wolkowiez M, et al. Coagulase-negative staphylococcal infections in the neonatal intensive care unit. Infect Control Hosp Epidemiol. 2011;32:679–86. [PMC free article] [PubMed] [Google Scholar]
Coagulase-negative staphylococcal infections in the neonatal intensive care unit. Infect Control Hosp Epidemiol. 2011;32:679–86. [PMC free article] [PubMed] [Google Scholar]
21. Phillips JR, Karlowicz MG. Prevalence of Candida species in hospital-acquired urinary tract infections in a neonatal intensive care unit. Pediatr Infect Dis J. 1997;16:190–4. [PubMed] [Google Scholar]
22. Airede AI. Urinary-tract infections in African neonates. J Infect. 1992;25:55. [PubMed] [Google Scholar]
23. Eliakim A, Dolfin T, Korzets Z, et al. Urinary tract infection in premature infants: the role of imaging studies and prophylactic therapy. J Perinatol. 1997;17:304. [PubMed] [Google Scholar]
24. Shim YH, Lee JW, Lee SJ. The risk factors of recurrent urinary tract infection in infants with normal urinary systems. Pediatr Nephrol. 2009;24:309–12. [PubMed] [Google Scholar]
25. Laway MA, Wani ML, Patnaik R, et al. Does circumcision alter the periurethral uropathogenic bacterial flora. Afr J Paediatr Surg. 2012;9:109–12. [PubMed] [Google Scholar]
Afr J Paediatr Surg. 2012;9:109–12. [PubMed] [Google Scholar]
26. Cleper R, Krause I, Eisenstein B, et al. Prevalence of vesicoureteral reflux in neonatal urinary tract infection. Clin Pediatr (Phila) 2004;43:619–25. [PubMed] [Google Scholar]
27. Jantunen ME, Siitonen A, Ala-Houhala M, et al. Predictive factors associated with significant urinary tract abnormalities in infants with pyelonephritis. Pediatr Infect Dis J. 2001;20:597–601. [PubMed] [Google Scholar]
28. Goldman M, Lahat E, Strauss S, et al. Imaging after urinary tract infection in male neonates. Pediatrics. 2000;105:1232–5. [PubMed] [Google Scholar]
29. Sastre JB, Aparicio AR, Cotallo GD, et al. Urinary tract infection in the newborn: clinical and radio imaging studies. Pediatr Nephrol. 2007;22:1735–41. [PubMed] [Google Scholar]
30. Khalesi N, Khosravi N, Jalali A, et al. Evaluation of maternal urinary tract infection as a potential risk factor for neonatal urinary tract infection. J Family Reprod Health.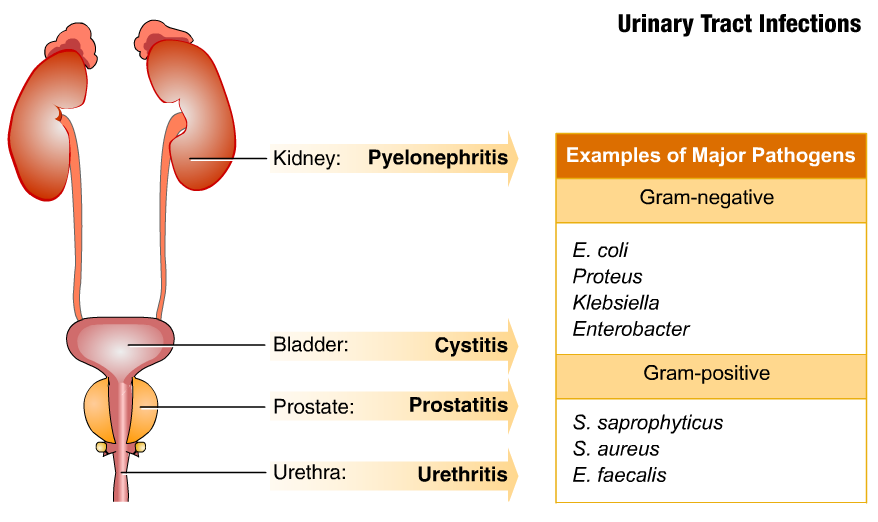 2014;8:59–62. [PMC free article] [PubMed] [Google Scholar]
2014;8:59–62. [PMC free article] [PubMed] [Google Scholar]
31. Milas V, Puseljić S, Stimac M, et al. Urinary tract infection (UTI) in newborns: risk factors, identification and prevention of consequences. Coll Antropol. 2013;37:871–6. [PubMed] [Google Scholar]
32. Littlewood JM. 66 infants with urinary tract infection in first month of life. Arch Dis Child. 1972;47:218–26. [PMC free article] [PubMed] [Google Scholar]
33. Levy I, Comarsca J, Davidovits M, et al. Urinary tract infection in preterm infants: the protective role of breastfeeding. Pediatr Nephrol. 2009;24:527–31. [PubMed] [Google Scholar]
34. Levine DA, Platt SL, Dayan PS, et al. Risk of serious bacterial infection in young febrile infants with respiratory syncytial virus infections. Pediatrics. 2004;113:1728–34. [PubMed] [Google Scholar]
35. Shahian M, Rashtian P, Kalani M. Unexplained neonatal jaundice as an early diagnostic sign of urinary tract infection. Int J Infect Dis. 2012;16:e487–90. [PubMed] [Google Scholar]
36. Pashapour N, Nikibahksh AA, Golmohammadlou S. Urinary tract infection in term neonates with prolonged jaundice. Urol J. 2007;4:91–4. [PubMed] [Google Scholar]
Pashapour N, Nikibahksh AA, Golmohammadlou S. Urinary tract infection in term neonates with prolonged jaundice. Urol J. 2007;4:91–4. [PubMed] [Google Scholar]
37. Garcia FJ, Nager AL. Jaundice as an early diagnostic sign of urinary tract infection in infancy. Pediatrics. 2002;109:846–51. [PubMed] [Google Scholar]
38. Mutlu M, Cayir Y, Asian Y. Urinary tract infections in neonates with jaundice in their first two weeks of life. World J Pediatr. 2014;10:164–7. [PubMed] [Google Scholar]
39. Xinias I, Demertzidou V, Mavroudi A, et al. Bilirubin levels predict renal cortical changes in jaundiced neonates with urinary tract infection. World J Pediatr. 2009;5:42–5. [PubMed] [Google Scholar]
40. American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297–316. [PubMed] [Google Scholar]
41. Fang SB, Lee HC, Yeung CY, et al. Urinary tract infections in young infants with prolonged jaundice. Acta Paediatr Taiwan. 2005;46:356–60. [PubMed] [Google Scholar]
Acta Paediatr Taiwan. 2005;46:356–60. [PubMed] [Google Scholar]
42. Chen HT, Jeng MJ, Soong WJ, et al. Hyperbilirubinemia with urinary tract infection in infants younger than eight weeks old. J Chin Med Assoc. 2011;74:159–63. [PubMed] [Google Scholar]
43. Tebruegge M, Pantazidou A, Clifford V, et al. The age-related risk of co-existing meningitis in children with urinary tract infection. PLoS One. 2011;6:e26576. [PMC free article] [PubMed] [Google Scholar]
44. Foglia EE, Lorch SA. Clinical predictors of urinary tract infection in the neonatal intensive care unit. J Neonatal Perinatal Med. 2012;5:327–33. [PMC free article] [PubMed] [Google Scholar]
45. Karacan C, Erkek N, Senel S, et al. Evaluation of urine collection methods for the diagnosis of urinary tract infection in children. Med Princ Pract. 2010;19:188–91. [PubMed] [Google Scholar]
46. Tosif S, Baker A, Oakley E, et al. Contamination rates of different urine collection methods for the diagnosis of urinary tract infections in young children: an observational cohort study. J Paediatr Child Health. 2012;48:659–64. [PubMed] [Google Scholar]
J Paediatr Child Health. 2012;48:659–64. [PubMed] [Google Scholar]
47. Hoberman A, Wald ER. Urinary tract infections in young febrile children. Pediatr Infect Dis J. 1997;16:11–7. [PubMed] [Google Scholar]
48. Crain EF, Gershel JC. Urinary tract infections in febrile infants younger than 8 weeks of age. Pediatrics. 1990;86:363–7. [PubMed] [Google Scholar]
49. Dukes C. The examination of urine for pus. Br Med J. 1928;1:391–3. [PMC free article] [PubMed] [Google Scholar]
50. Hoberman A, Wald ER, Reynolds EA, et al. Pyuria and bacteriuria in urine specimens obtained by catheter from young children with fever. J Pediatr. 1994;124:513–9. [PubMed] [Google Scholar]
51. Shah AP, Cobb BT, Lower DR, et al. Enhanced versus automated urinalysis for screening of urinary tract infections in children in the emergency department. Pediatr Infect Dis J. 2014;33:272–5. [PubMed] [Google Scholar]
52. Mori R, Yonemoto N, Fitzgerald A, et al. Diagnostic performance of urine dipstick testing in children with suspected UTI: a systematic review of relationship with age and comparison with microscopy. Acta Paediatr. 2010;99:581–4. [PubMed] [Google Scholar]
Acta Paediatr. 2010;99:581–4. [PubMed] [Google Scholar]
53. Glissmeyer EW, Korgenski EK, Wilkes J, et al. Dipstick screening for urinary tract infection in febrile infants. Pediatrics. 2014;133(5):e1121–7. [PMC free article] [PubMed] [Google Scholar]
54. Hasvold J, Bradford L, Nelson C, et al. Gentamicin resistance among Escherichia coli strains isolated in neonatal sepsis. J Neonatal Perinatal Med. 2013;6:173–7. [PubMed] [Google Scholar]
55. Shakir SM, Goldbeck JM, Robison D, et al. Genotypic and Phenotypic Characterization of Invasive Neonatal Escherichia coli Clinical Isolates. Am J Perinatol. 2014;31:975–82. [PubMed] [Google Scholar]
56. Taheri PA, Navabi B, Shariat M. Neonatal urinary tract infection: clinical response to empirical therapy versus in vitro susceptibility at Bahrami Children's Hospital-Neonatal Ward: 2001–2010. Acta Med Iran. 2012;50:348–52. [PubMed] [Google Scholar]
57. Williamson JC, Craft DW, Butts JD, et al. In vitro assessment of urinary isolates of ampicillin-resistant enterococci. Ann Pharmacother. 2002;36:246–50. [PubMed] [Google Scholar]
Ann Pharmacother. 2002;36:246–50. [PubMed] [Google Scholar]
58. Laugel V, Kuhn R, Beladdale J, et al. Effects of antenatal antibiotics on the incidence and bacteriological profile of early-onset neonatal sepsis. A retrospective study over five years Biol Neonate. 2003;84:24–30. [PubMed] [Google Scholar]
59. Kuhn P, Dheu C, Bolender C, et al. Incidence and distribution of pathogens in early-onset neonatal sepsis in the era of antenatal antibiotics. Paediatr Perinat Epidemiol. 2010;24:479–87. [PubMed] [Google Scholar]
60. Glasgow TS, Young PC, Wallin J, et al. Association of intrapartum antibiotic exposure and late-onset serious bacterial infections in infants. Pediatrics. 2005;116:696–702. [PubMed] [Google Scholar]
61. Benador D, Neuhaus TJ, Papazyan JP, et al. Randomised controlled trial of three day versus 10 day intravenous antibiotics in acute pyelonephritis: effect on renal scarring. Arch Dis Child. 2001;84:241–6. [PMC free article] [PubMed] [Google Scholar]
62. Cherry J, Demmler-Harrison GJ, Kaplan SL, et al. Feigin and Cherry's textbook of pediatric infectious diseases. Philadelphia: Elsevier Saunders; 2013. [Google Scholar]
Cherry J, Demmler-Harrison GJ, Kaplan SL, et al. Feigin and Cherry's textbook of pediatric infectious diseases. Philadelphia: Elsevier Saunders; 2013. [Google Scholar]
63. Nowell L, Moran C, Smith PB, et al. Prevalence of renal anomalies after urinary tract infections in hospitalized infants less than 2 months of age. J Perinatol. 2010;30:281–5. [PMC free article] [PubMed] [Google Scholar]
64. Siomou E, Giapros V, Fotopoulos A, et al. Implications of 99mTc-DMSA scintigraphy performed during urinary tract infection in neonates. Pediatrics. 2009;124:881–7. [PubMed] [Google Scholar]
65. Biyikli NK, Alpay H, Ozek E, et al. Neonatal urinary tract infections: analysis of the patients and recurrences. Pediatr Int. 2004;46:21–5. [PubMed] [Google Scholar]
66. Garin EH, Olavarria F, Garcia Nieto V, et al. Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled study. Pediatrics.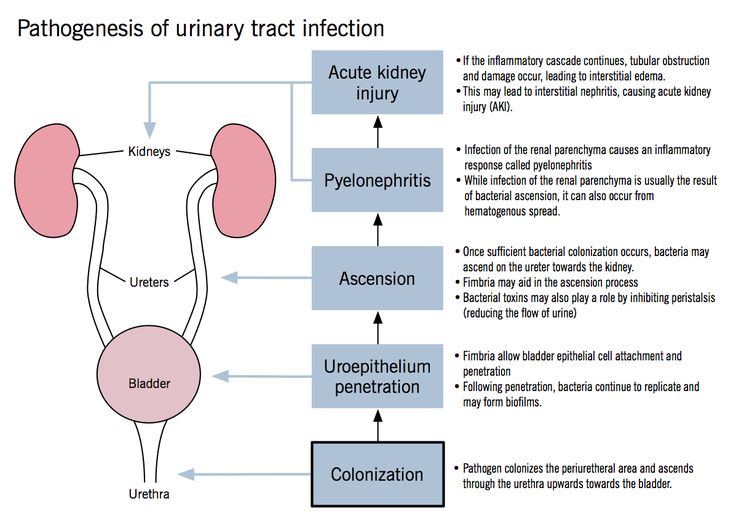 2006;117:626–32. [PubMed] [Google Scholar]
2006;117:626–32. [PubMed] [Google Scholar]
67. Hayashi Y, Kojima Y, Kamisawa H, et al. Is antibiotic prophylaxis effective in preventing urinary tract infections in patients with vesicoureteral reflux? Expert Rev Anti Infect Ther. 2010;8:51–8. [PubMed] [Google Scholar]
68. Williams GJ, Wei L, Lee A, et al. Long-term antibiotics for preventing recurrent urinary tract infection in children. Cochrane Database Syst Rev. 2006;(19) CD001534. [PubMed] [Google Scholar]
69. RIVUR Trial Investigators. Hoberman A, Greenfield SP, et al. Antimicrobial prophylaxis for children with vesicoureteral reflux. N Engl J Med. 2014;370:2367–76. [PMC free article] [PubMed] [Google Scholar]
70. Harris MC, Deuber C, Polin RA, et al. Investigation of apparent false-positive urine latex particle agglutination tests for the detection of group B streptococcus antigen. J Clin Microbiol. 1989;27:2214–7. [PMC free article] [PubMed] [Google Scholar]
71. Benjamin DK, Jr, Stoll BJ, Gantz MG, et al.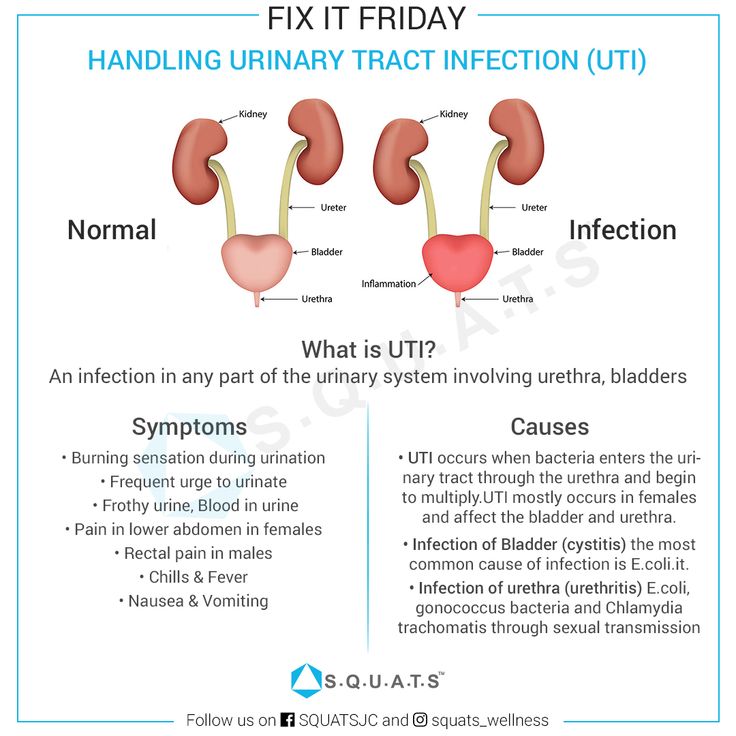 Neonatal candidiasis: epidemiology, risk factors, and clinical judgment. Pediatrics. 2010;26:e865–73. [PMC free article] [PubMed] [Google Scholar]
Neonatal candidiasis: epidemiology, risk factors, and clinical judgment. Pediatrics. 2010;26:e865–73. [PMC free article] [PubMed] [Google Scholar]
72. Cantey JB, Wozniak PS, Sánchez PJ. Prospective surveillance of antibiotic use in the neonatal intensive care unit: results from the SCOUT study. Pediatr Infect Dis J. 2014 [Epub ahead of print] [PubMed] [Google Scholar]
Urinary tract infection in newborns.
Urinary tract infection in young children is no less common than viral respiratory infections. Vomiting and nausea, cramps in the abdomen are often attributed by parents to colic, malnutrition or intestinal infections. However, with such symptoms, it is recommended to consult a doctor. If this is a urinary tract infection, then its untimely diagnosis and treatment will lead to unpleasant consequences for the baby.
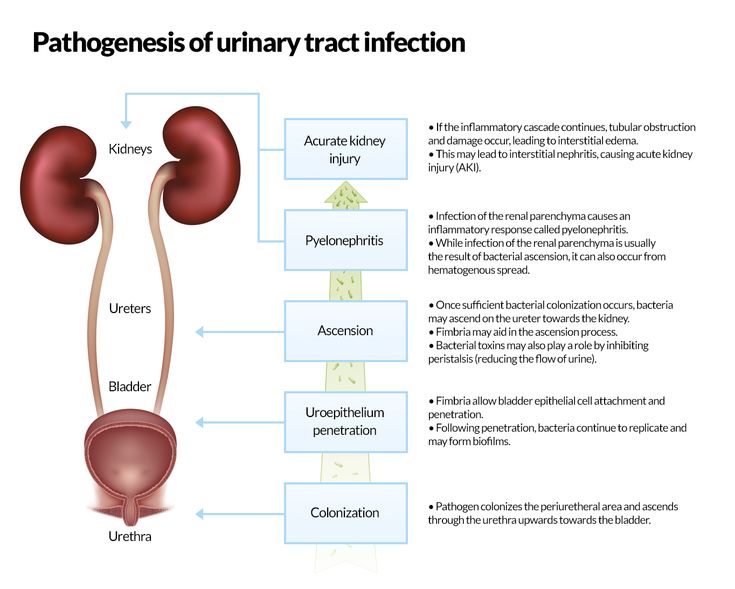
A urinary tract infection occurs when bacteria in the child's body begin to multiply rapidly in the urinary tract.
Most often this pathology is caused by microbes such as:
- Escherichia coli,
- Staphylococcus aureus,
- Pseudomonas aeruginosa,
- Klebsiella
These include:
- vesicoureteral reflux;
- narrowing of the ureters;
- malposition of the organs of the urinary system;
- horseshoe kidney and others
Another cause of infection is the presence of a microbial focus in the body.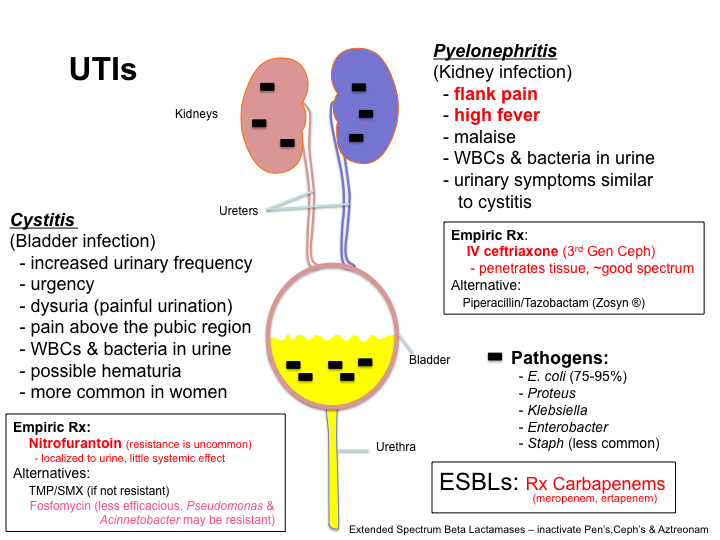 With an infectious-inflammatory pathology of other organs, the bacterial flora can enter the kidneys and urinary tract, causing inflammation there. Also, the bacterium can enter the baby's body from the mother during breastfeeding.
With an infectious-inflammatory pathology of other organs, the bacterial flora can enter the kidneys and urinary tract, causing inflammation there. Also, the bacterium can enter the baby's body from the mother during breastfeeding.
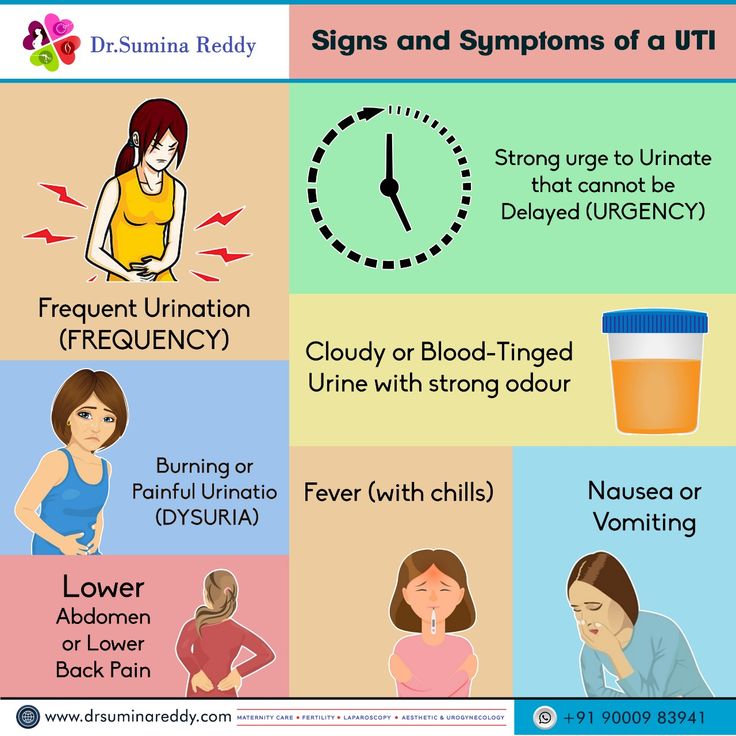
Genitourinary infection in infants presents with the same symptoms as in adults. The problem is that a newborn baby cannot complain.
Parents should keep a close eye on their child to detect symptoms of illness.
Initial symptoms include tearfulness, restlessness, poor sleep and loss of appetite.
In children under one year old, a urinary tract infection may be manifested by a decrease or increase from the age norm of urine excreted, a change in the color and saturation of urine (the child's urine may become bright yellow (with an increase in the concentration of urine, which is usually accompanied by a decrease in its quantity), red or brown (admixture of blood.) When bacteria appear, the urine does not change its color, but becomes cloudy and loses its transparency.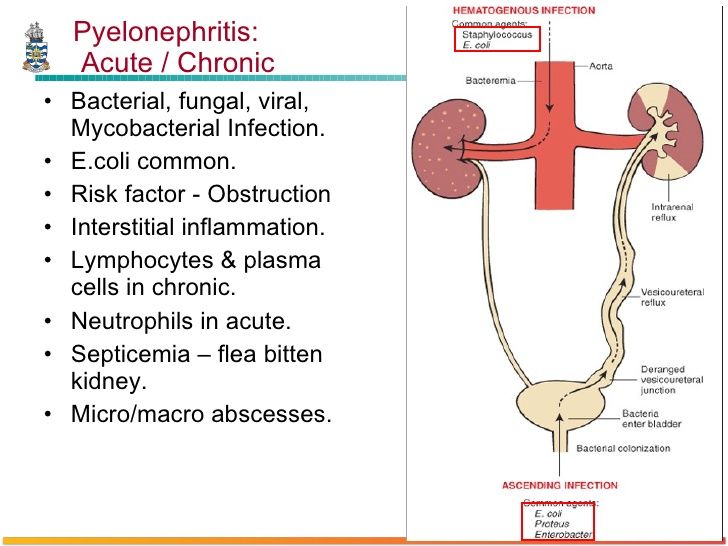 0003
0003
Edema may appear due to the characteristics of the baby's body, the appearance of an unpleasant smell from the diaper.
The appearance of restlessness and crying when urinating, which indicates the presence of pain and cramps in the baby. Often, mothers note that the child strains when urinating. In this case, an intermittent stream of urine is recorded.
The rise in temperature to high numbers, if it does not go away after taking antipyretics and persists for several days, this is a reason to suspect an infection.
Infection of the genitourinary system in infants is detected by laboratory analysis of urine, urine culture, blood test, b / x blood test.
In case of inflammation, blood and urine tests show an increase in the number of leukocytes. With bakposev, it is possible to identify which bacterium caused the infection, and determine the individual sensitivity of the microbe to the antibiotic.
As noted above, the cause of infection in infants may be a congenital malformation of the genitourinary organs.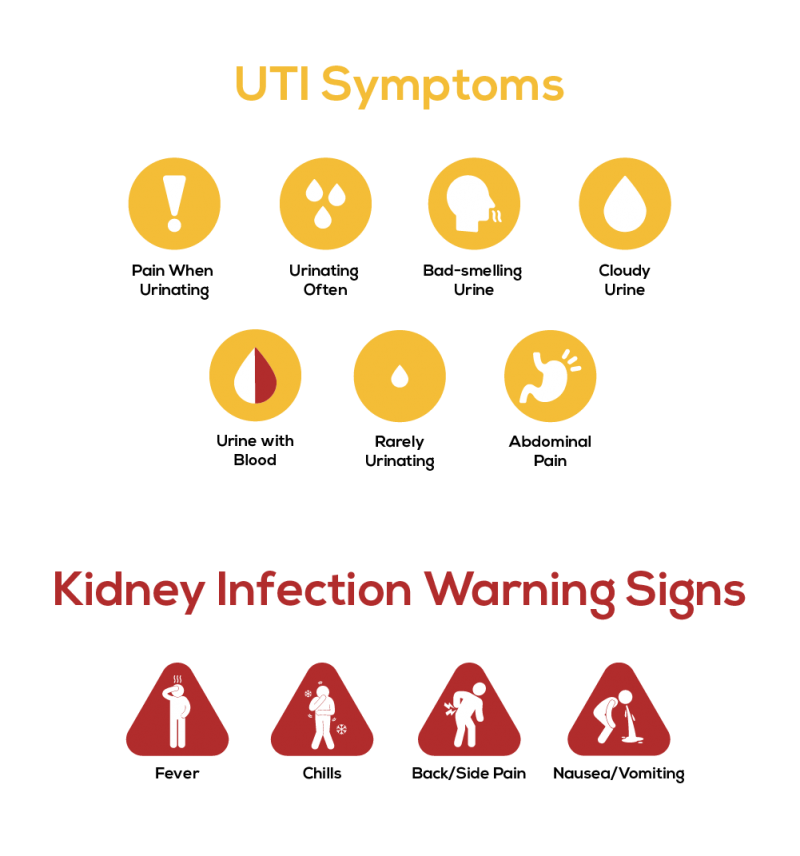
If this pathology is suspected, the following examinations should be performed:
- ultrasound examination of the urinary system organs;
- voiding cystography;
- retrograde radiography of the kidneys;
- CT or MRI of the kidneys.
The basis for the treatment of urinary tract infection is antibiotic therapy. A broad-spectrum antibiotic or a drug based on sensitivity is prescribed. The antibiotic is taken orally or injected intravenously.
It is important that if an infection is detected, the infant must be hospitalized for the duration of treatment.
In addition to antibiotics, anti-inflammatory drugs and antipyretics are used. Moreover, many medicines are produced in a convenient form of application, for example, in candles.
Herbal uroseptics are often prescribed, which do not have a toxic effect and contribute to the recovery of the child. In no case should you start treatment on your own or cancel medications without a doctor's prescription.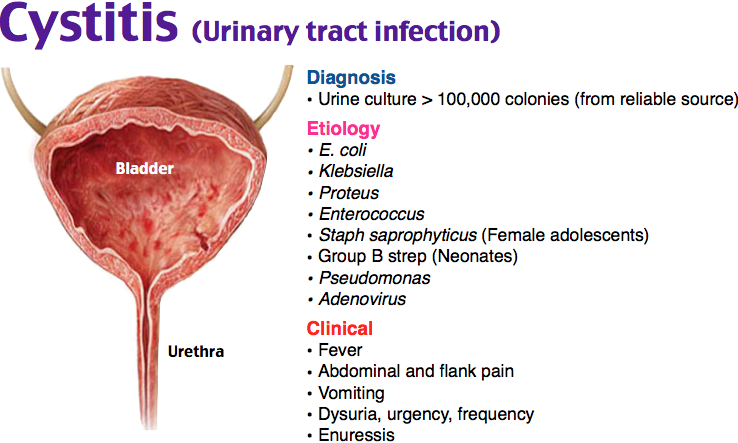 This will lead to the fact that the disease will go into a latent stage and will periodically worsen, again and again causing unpleasant symptoms. In addition, many drugs are contraindicated for children and their uncontrolled use will bring irreparable harm to the child.
This will lead to the fact that the disease will go into a latent stage and will periodically worsen, again and again causing unpleasant symptoms. In addition, many drugs are contraindicated for children and their uncontrolled use will bring irreparable harm to the child.
Infection in infants with malformations will constantly recur despite good treatment. Therefore, the only way out is to carry out an operational correction of the defect. It should be noted that the operation is possible only after the acute inflammatory process is eliminated.
Prevention of urinary tract infections in infants.
In order to rule out an illness in a child, the following points should be followed:
- Carefully monitor the hygiene of the child's urinary organs.
- avoid hypothermia of the baby;
- monitor the rationality of nutrition.
Every year about 1400 children are treated in the Department of Prematurity and Pathology of Newborns. Of these, with urinary tract infection 65-70, with various congenital malformations of the kidneys and urinary system 28-30 children. All children undergo a complex of examinations and treatment according to the developed standards. All children are discharged with improvement and recovery and are subsequently observed by nephrologists and urologists in the regional children's clinic.
All children undergo a complex of examinations and treatment according to the developed standards. All children are discharged with improvement and recovery and are subsequently observed by nephrologists and urologists in the regional children's clinic.
Infection of the genitourinary system is not such a terrible diagnosis. With a complete examination and high-quality, adequately selected therapy, the child will recover without any residual effects.
Urinary tract infection in children. What is urinary tract infection in children?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
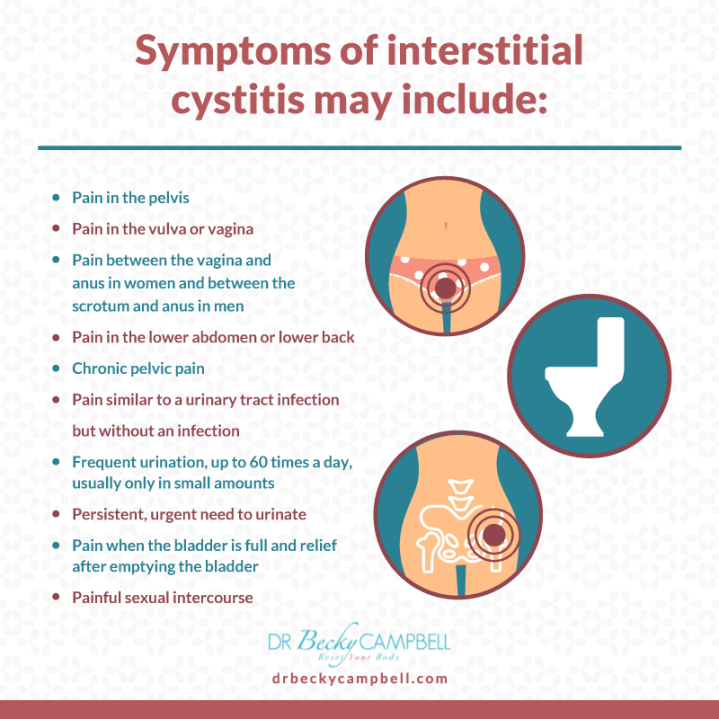
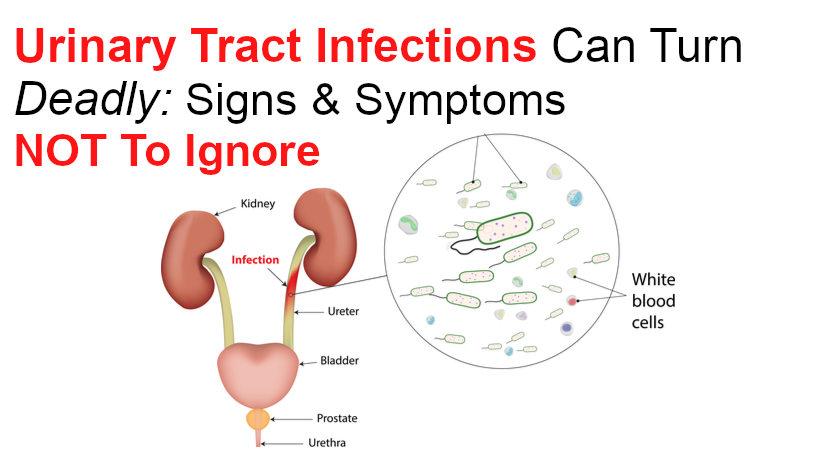
Urinary tract infection in children is a group of microbial-inflammatory diseases of the urinary system organs: kidneys, ureters, bladder, urethra.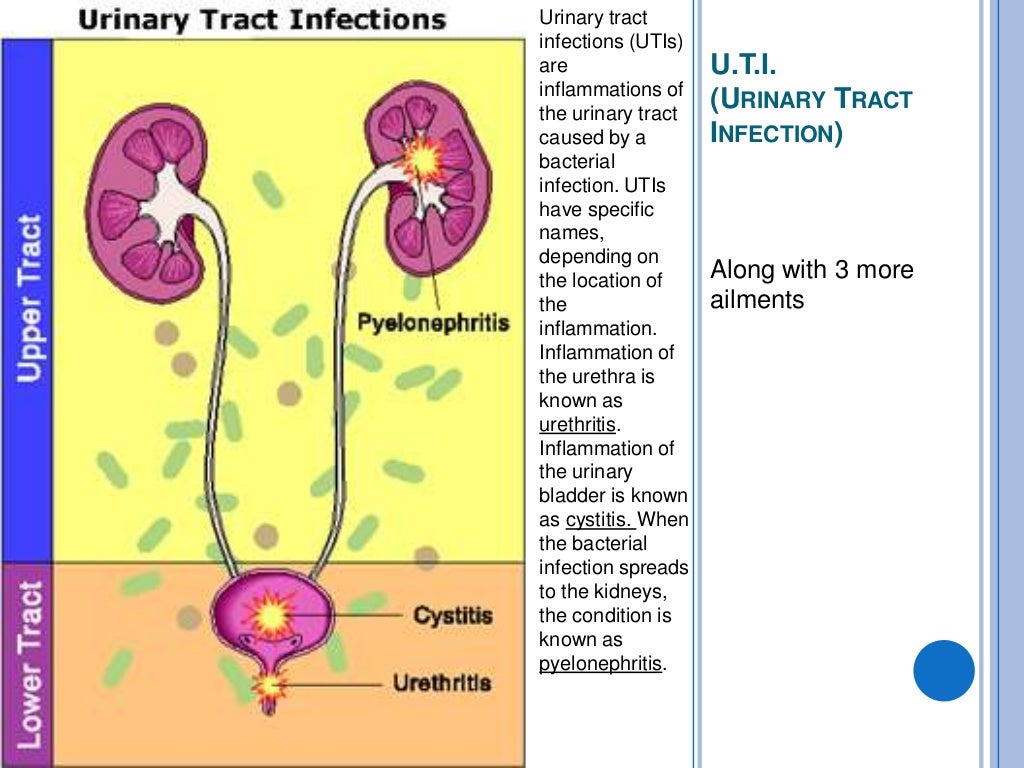 Depending on the location of the inflammation, urinary tract infection in children can be manifested by dysuric disorders, pain in the bladder or lower back, leukocyturia and bacteriuria, and temperature reaction. Examination of children with suspected urinary tract infection includes urinalysis (general, bacterial culture), ultrasound of the urinary system, cystoureterography, excretory urography, cystoscopy. The basis for the treatment of urinary tract infections in children is the appointment of antimicrobial drugs, uroantiseptics.
Depending on the location of the inflammation, urinary tract infection in children can be manifested by dysuric disorders, pain in the bladder or lower back, leukocyturia and bacteriuria, and temperature reaction. Examination of children with suspected urinary tract infection includes urinalysis (general, bacterial culture), ultrasound of the urinary system, cystoureterography, excretory urography, cystoscopy. The basis for the treatment of urinary tract infections in children is the appointment of antimicrobial drugs, uroantiseptics.
- Causes of urinary tract infection in children
- Classification
- Symptoms in children
- Diagnostics
- Treatment of urinary tract infection in children
- Prognosis and prevention
- Prices for treatment
General
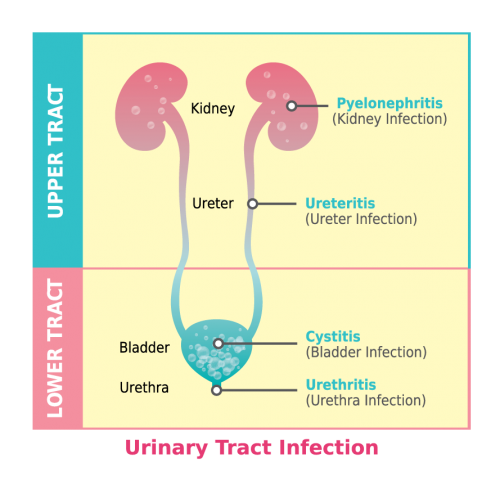
Urinary tract infection in children is a general concept that refers to inflammatory processes in various parts of the urinary tract: infections of the upper urinary tract (pyelitis, pyelonephritis, ureteritis) and lower urinary tract (cystitis, urethritis).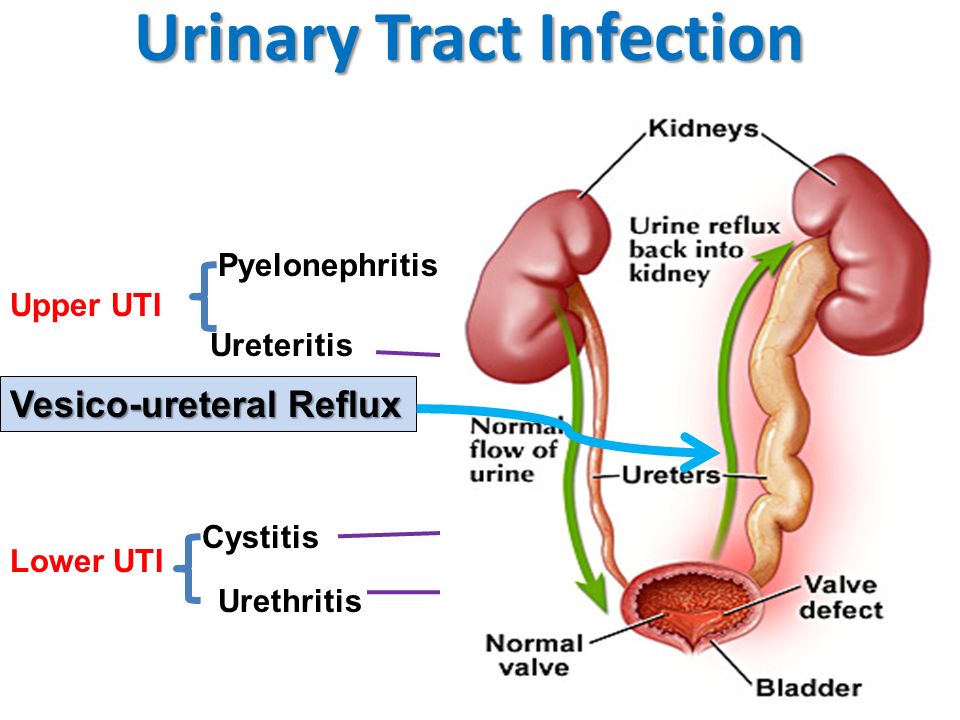 Urinary tract infections are extremely common in childhood - by age 5, 1-2% of boys and 8% of girls have had at least one episode of the disease. The prevalence of urinary tract infections depends on age and gender: for example, among newborns and infants, boys are more likely to get sick, and girls between the ages of 2 and 15 years. Most often in the practice of pediatric urology and pediatrics one has to deal with cystitis, pyelonephritis and asymptomatic bacteriuria.
Urinary tract infections are extremely common in childhood - by age 5, 1-2% of boys and 8% of girls have had at least one episode of the disease. The prevalence of urinary tract infections depends on age and gender: for example, among newborns and infants, boys are more likely to get sick, and girls between the ages of 2 and 15 years. Most often in the practice of pediatric urology and pediatrics one has to deal with cystitis, pyelonephritis and asymptomatic bacteriuria.
urinary tract infection in children
Causes of urinary tract infection in children
The spectrum of microbial flora that causes urinary tract infections in children depends on the sex and age of the child, the conditions of infection, the state of intestinal microbiocenosis and general immunity. In general, among bacterial pathogens, enterobacteria are in the lead, primarily E. coli (50-90%). In other cases, Klebsiella, Proteus, Enterococci, Pseudomonas aeruginosa, Staphylococci, Streptococci, etc.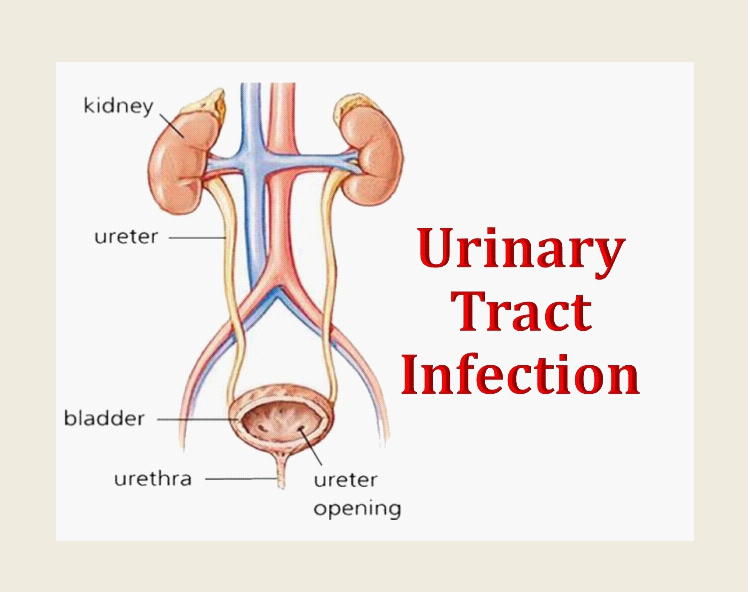 are sown. Acute urinary tract infections in children are usually caused by one type of microorganism, however, with frequent relapses and malformations of the urinary system, microbial associations are often detected.
are sown. Acute urinary tract infections in children are usually caused by one type of microorganism, however, with frequent relapses and malformations of the urinary system, microbial associations are often detected.
Urinary tract infections in children can be associated with urogenital chlamydia, mycoplasmosis and ureaplasmosis and combined with vulvitis, vulvovaginitis, balanoposthitis. Fungal infections of the urinary tract often occur in debilitated children: premature, suffering from malnutrition, immunodeficiency states, anemia. There is an assumption that a viral infection (infection with Coxsackie, influenza, adenoviruses, herpes simplex virus types I and II, cytomegalovirus) is a factor contributing to the layering of a bacterial infection.
Conditions accompanied by impaired urodynamics predispose to the development of urinary tract infection in children: neurogenic bladder, urolithiasis, bladder diverticula, vesicoureteral reflux, pyelectasis, hydronephrosis, polycystic kidney disease, kidney dystopia, ureterocele, phimosis in boys, synechia of the labia in girls.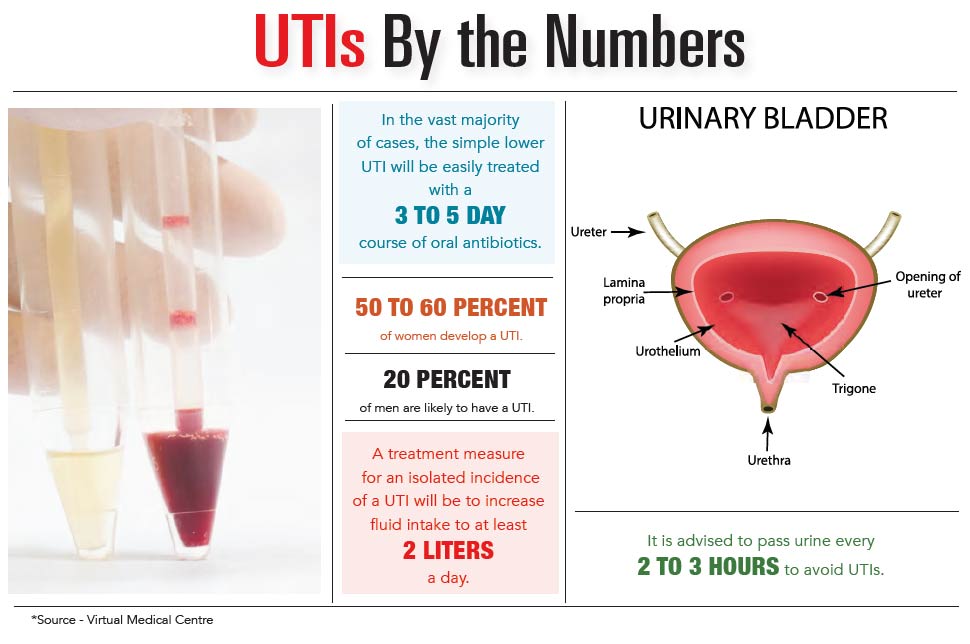 Often, urinary tract infections in children develop against the background of gastrointestinal diseases - dysbacteriosis, constipation, colitis, intestinal infections, etc. Metabolic disorders (dysmetabolic nephropathy in children, glucosuria, etc.) can be a risk factor.
Often, urinary tract infections in children develop against the background of gastrointestinal diseases - dysbacteriosis, constipation, colitis, intestinal infections, etc. Metabolic disorders (dysmetabolic nephropathy in children, glucosuria, etc.) can be a risk factor.
The introduction of infection into the urinary tract can occur with insufficient hygiene of the external genitalia, improper washing technique of the child, lymphogenous and hematogenous routes, during medical manipulations (bladder catheterization). Boys who have undergone circumcision suffer from urinary tract infections 4-10 times less often than uncircumcised boys.
Classification
According to the localization of the inflammatory process, infections of the upper urinary tract are distinguished - the kidneys (pyelonephritis, pyelitis), ureters (ureteritis) and the lower sections - the bladder (cystitis) and urethra (urethritis).
According to the period of the disease, urinary tract infections in children are divided into the first episode (debut) and relapse.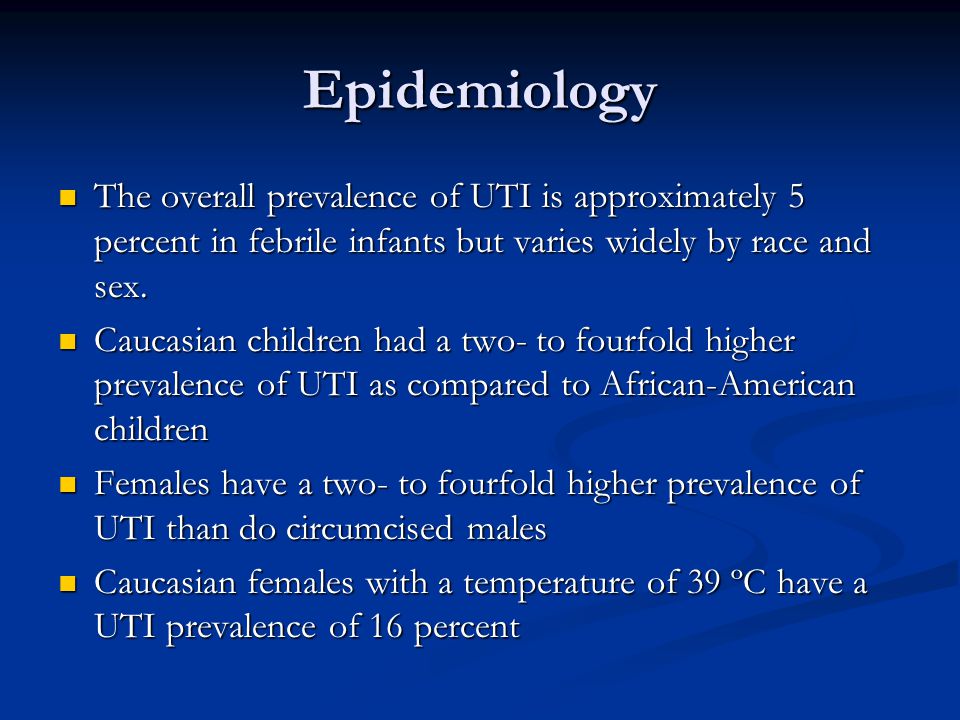 The course of recurrent urinary tract infection in children may be maintained by unresolved infection, persistence of the pathogen, or reinfection.
The course of recurrent urinary tract infection in children may be maintained by unresolved infection, persistence of the pathogen, or reinfection.
According to the severity of clinical symptoms, mild and severe urinary tract infections in children are distinguished. In a mild course, the temperature reaction is moderate, dehydration is insignificant, the child complies with the treatment regimen. Severe urinary tract infection in children is accompanied by high fever, persistent vomiting, severe dehydration, sepsis.
Symptoms in children
Clinical manifestations of urinary tract infection in a child depend on the localization of the microbial-inflammatory process, the period and severity of the disease. Consider the signs of the most common urinary tract infections in children - pyelonephritis, cystitis and asymptomatic bacteriuria.
Pyelonephritis in children occurs with febrile temperature (38-38.5 ° C), chills, symptoms of intoxication (lethargy, pallor of the skin, loss of appetite, headache).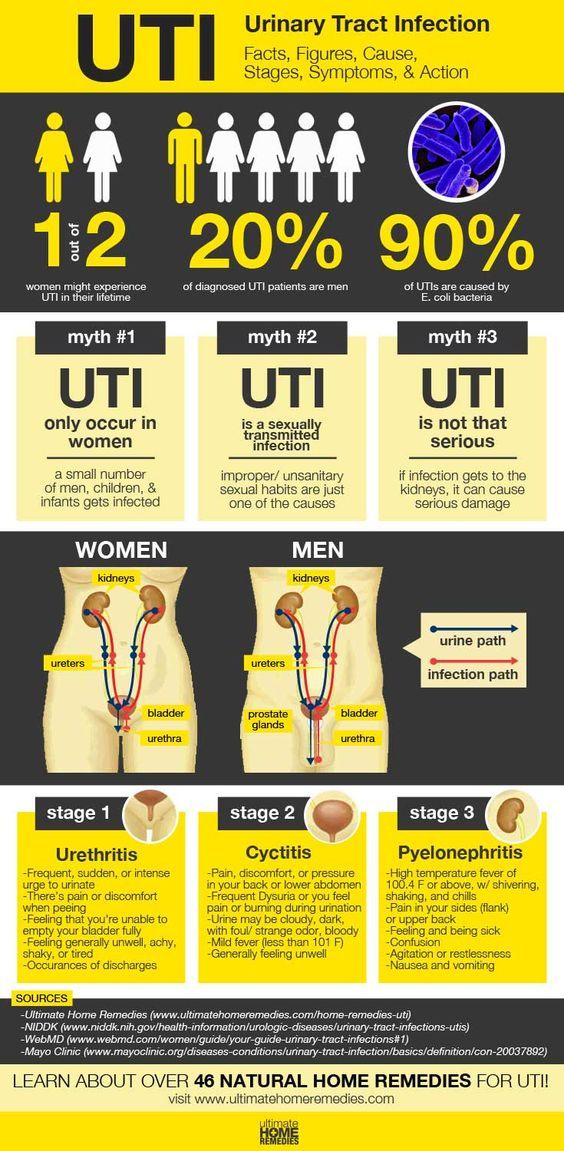 At the height of intoxication, frequent regurgitation, vomiting, diarrhea, neurotoxicosis, and meningeal symptoms may develop. The child is concerned about pain in the lumbar region or abdomen; effervescence symptom is positive. At an early age, infections of the upper urinary tract in children can be hidden under the guise of pylorospasm, dyspeptic disorders, acute abdomen, intestinal syndrome, etc.; in older children - flu-like syndrome.
At the height of intoxication, frequent regurgitation, vomiting, diarrhea, neurotoxicosis, and meningeal symptoms may develop. The child is concerned about pain in the lumbar region or abdomen; effervescence symptom is positive. At an early age, infections of the upper urinary tract in children can be hidden under the guise of pylorospasm, dyspeptic disorders, acute abdomen, intestinal syndrome, etc.; in older children - flu-like syndrome.
Cystitis in children is manifested primarily by dysuric disorders - frequent and painful urination in small portions. In this case, complete simultaneous emptying of the bladder is not achieved, episodes of urinary incontinence are possible. In infants, cystitis is often accompanied by stranguria (urinary retention). The presence of dysuria in children of the first year of life can be indicated by anxiety or crying associated with urination, intermittent and weak urine stream. Cystitis is characterized by pain and tension in the suprapubic region; the temperature in cystitis is normal or subfebrile.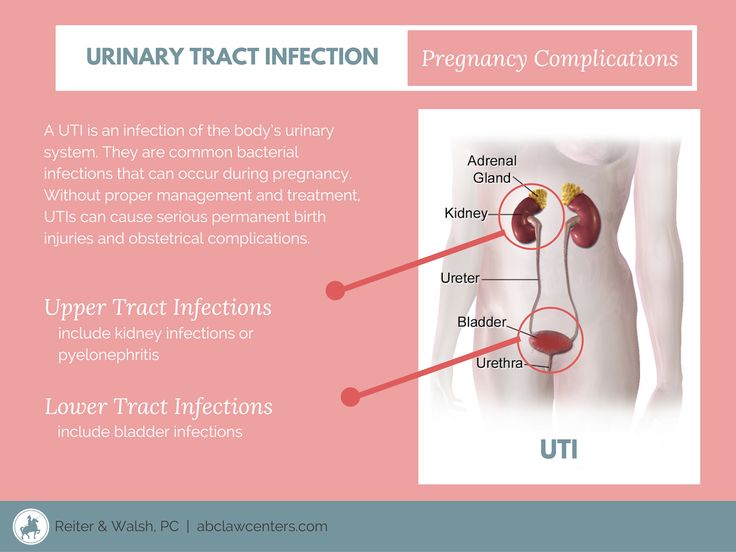
Asymptomatic bacteriuria is more common in girls. This form of urinary tract infection in children is not accompanied by any subjective clinical signs, but is detected only during laboratory examination. Sometimes parents pay attention to the turbidity of the child's urine and the bad smell emanating from it.
Diagnosis
Assessment of the severity of urinary tract infections in children requires an integrated approach and the participation of a number of specialists - a pediatrician, pediatric urologist, pediatric nephrologist, pediatric gynecologist.
Urinary tract infections in children may be suspected if leukocyturia, bacteriuria, proteinuria, and sometimes hematuria are detected in a general urine test. For a more detailed diagnosis, a urine test according to Nechiporenko, Zimnitsky's test is shown. Blood changes are characterized by neutrophilic leukocytosis, elevated ESR; with pyelonephritis - a high level of acute phase proteins (CRP, alpha globulins).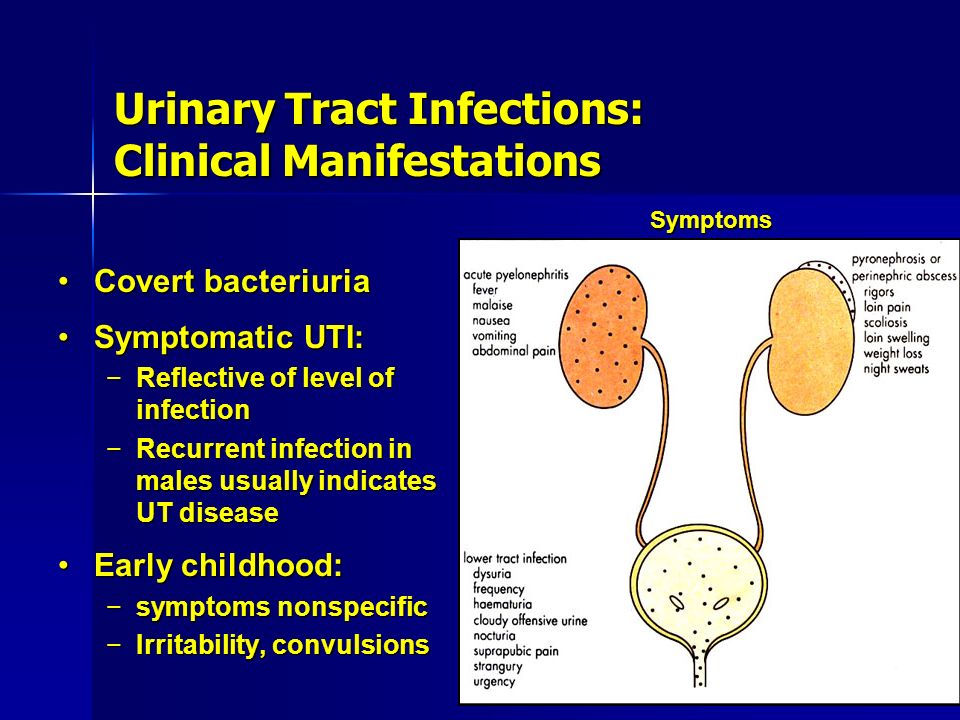
The basis for the diagnosis of urinary tract infections in children is a bacteriological culture of urine with the release of the pathogen, an assessment of the degree of bacteriuria and sensitivity to antibiotics. In some cases, a urine test for chlamydia, ureaplasma, mycoplasma is required by cultural, cytological, serological (ELISA) methods, PCR.
Children with a urinary tract infection must undergo an ultrasound examination of the urinary system (ultrasound of the kidneys, ultrasound of the vessels of the kidneys, ultrasound of the bladder). X-ray contrast studies of the urinary tract (excretory urography, voiding cystography, urethrography) are indicated only for repeated episodes of urinary tract infections in children and only in the remission phase. To study the state of the renal parenchyma, static or dynamic scintigraphy of the kidneys is performed.
Endoscopy methods in children (ureteroscopy, cystoscopy) are used to detect urethritis, cystitis, anomalies of the urethra and bladder.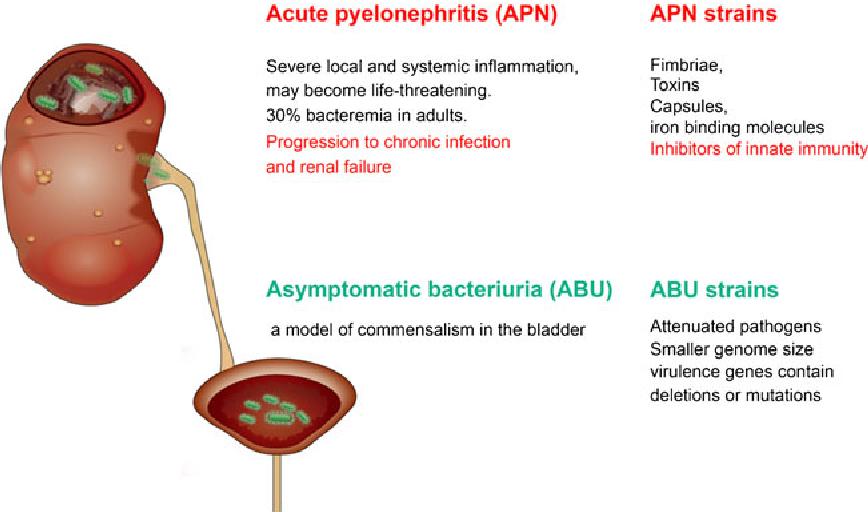 In order to study urodynamics, uroflowmetry and cystometry are performed.
In order to study urodynamics, uroflowmetry and cystometry are performed.
Treatment of urinary tract infection in children
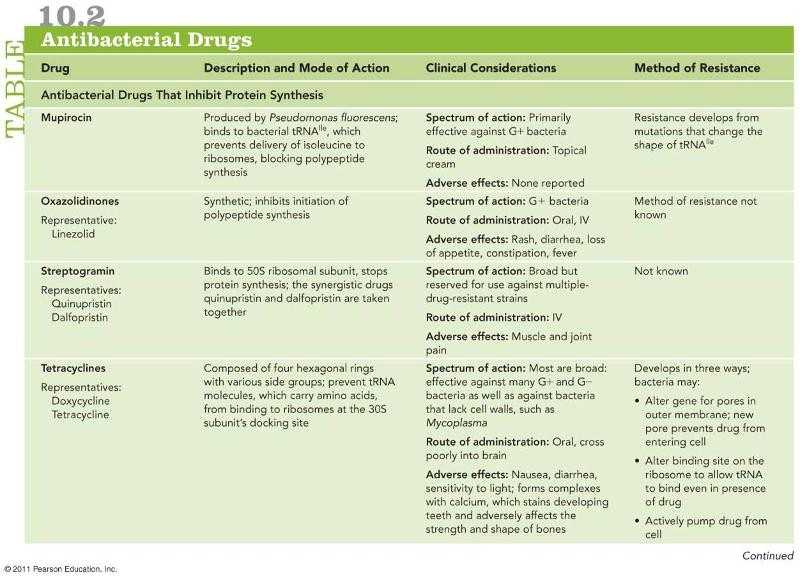
The main place in the treatment of urinary tract infections in children belongs to antibiotic therapy. Until a bacteriological diagnosis is established, initial antibiotic therapy is given on an empirical basis. Currently, in the treatment of urinary tract infections in children, preference is given to inhibitor-protected penicillins (amoxicillin), aminoglycosides (amikacin), cephalosporins (cefotaxime, ceftriaxone), carbapenems (meropenem, imipenem), uroantiseptics (nitrofurantoin, furazidin). The duration of the course of antimicrobial therapy should be 7-14 days. After completion of the course of treatment, a repeated laboratory examination of the child is carried out.
It is recommended to take NSAIDs (ibuprofen), desensitizing agents (clemastine, loratadine), antioxidants (vitamin E, etc.), herbal medicine.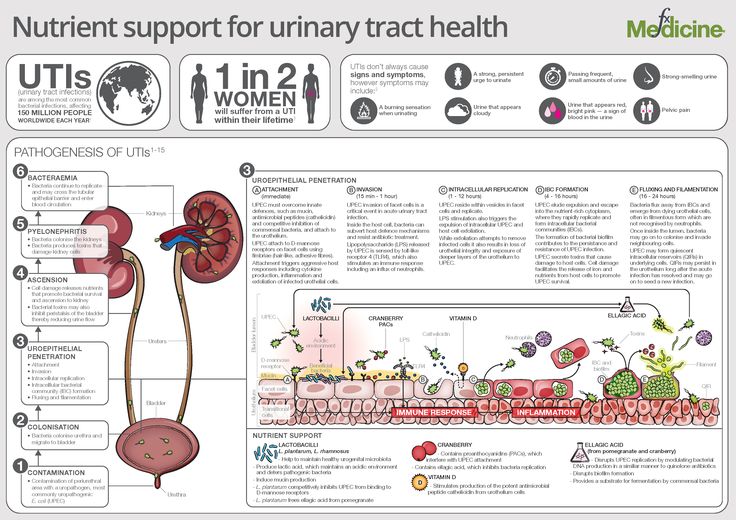 Asymptomatic bacteriuria usually does not require treatment; sometimes uroseptics are prescribed in these cases.
Asymptomatic bacteriuria usually does not require treatment; sometimes uroseptics are prescribed in these cases.
When an acute urinary tract infection subsides, children are shown physiotherapy: microwave, UHF, electrophoresis, paraffin and ozocerite applications, mud therapy, pine baths.
Prognosis and prevention
Advanced urinary tract infections in children can lead to irreversible damage to the renal parenchyma, kidney shrinkage, hypertension, and sepsis. Recurrences of urinary tract infections occur in 15-30% of cases, so children at risk are given anti-relapse prophylaxis with antibiotics or uroantiseptics. The child should be under the supervision of a pediatrician and a nephrologist. Vaccination of children is carried out during periods of clinical and laboratory remission.
Primary prevention of urinary tract infection in children should include the inculcation of proper hygiene skills, the rehabilitation of chronic foci of infection, and the elimination of risk factors.