How long does gastroenteritis last in child
Kids Health Information : Gastroenteritis (gastro)
This fact sheet is available in the following languages: Arabic, Assyrian, Burmese, Chinese (simplified), Chinese (traditional), English, Karen, Persian, Somali, Turkish and Vietnamese.
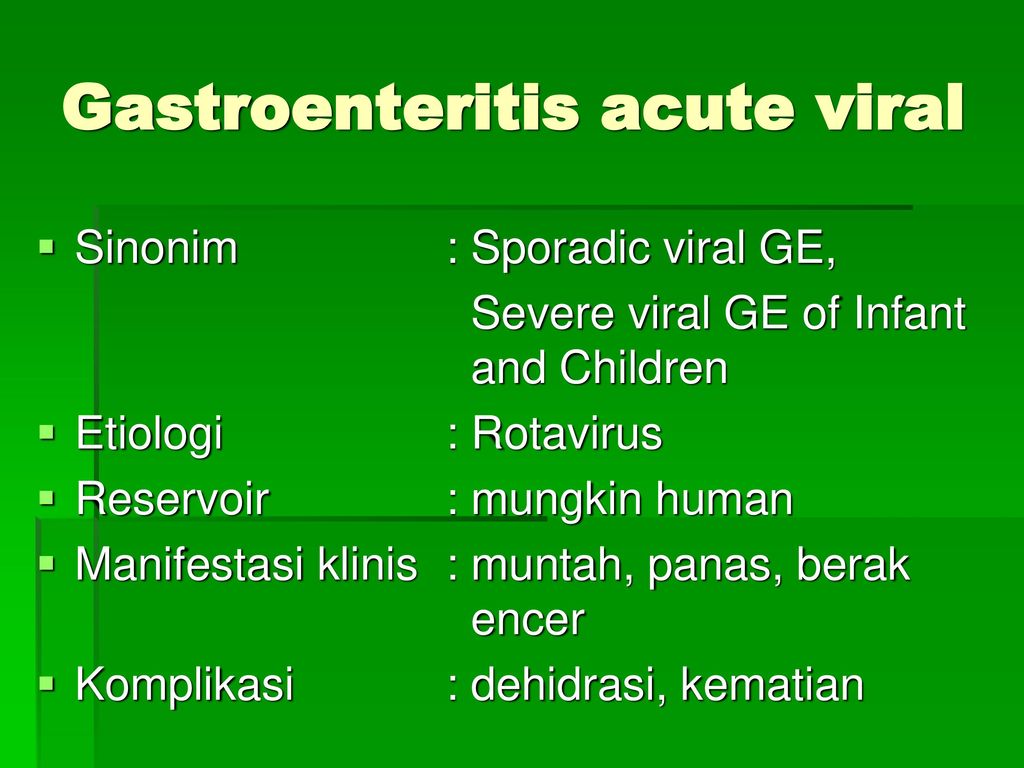
Gastroenteritis (gastro) is a bowel infection that causes diarrhoea (runny, watery poo) and sometimes vomiting. The vomiting may settle quickly, but the diarrhoea can last up to 10 days.
Gastro can be caused by many different germs, although the most common cause of gastro is a viral infection. Most children do not need to take any medicine for gastro; however, it is important that they drink plenty of water to avoid becoming dehydrated.
Gastro is spread easily, and is more common and severe in babies and young children. Babies under six months old can become dehydrated very easily and need to be checked by a GP if they have gastro.
Signs and symptoms of gastro
If your child has gastro, they may:
- feel unwell, and not want to eat or drink
- vomit in the first 24 to 48 hours (usually before diarrhoea begins)
- have diarrhoea, which can last up to 10 days
- have some stomach pain
- have a fever.
Care at home
The main treatment is to keep your child drinking fluids often such as water, oral rehydration solution, breastmilk or formula. It is very important to replace the fluids lost due to the vomiting and diarrhoea.
Gastrolyte, HYDRAlyte, Pedialyte and Repalyte are different types of oral rehydration fluid that can be used to replace fluids and body salts. These are the best option if your child is dehydrated. They are also available as icy poles, which children are often happy to have.
If your child refuses water or oral rehydration fluids, try diluted apple juice. Do not give drinks that are high in sugar (e.g. flat lemonade or sports drinks), because they can make dehydration worse. You can give your child their usual milk; however, some children may not feel like drinking milk if they have gastro.
You can give your child their usual milk; however, some children may not feel like drinking milk if they have gastro.
|
Infants |
|
If your baby is under six months old, they should always be seen by a doctor if they have gastro. For babies over six months:
|
|
Older children |
|
Do not give your child over-the-counter medicines that reduce vomiting and diarrhoea, as the medicines may be harmful for children.
Children with gastro are infectious, so wash your hands thoroughly after contact with your child, particularly before feeding and after nappy changes.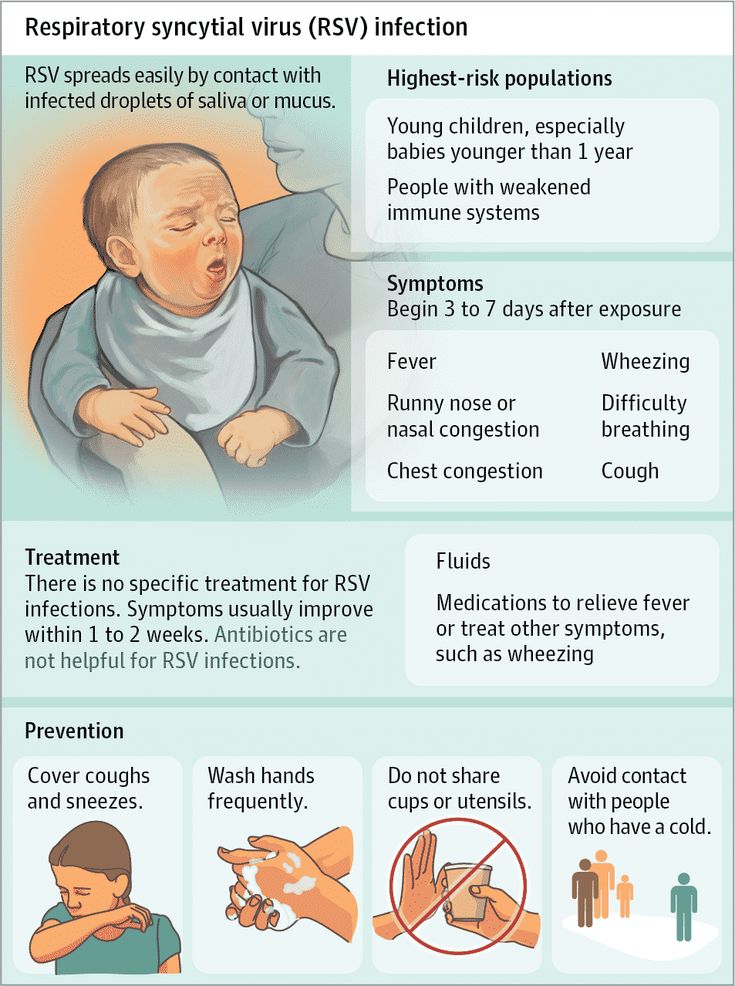 Keep your child away from other children as much as possible until the diarrhoea has stopped.
Keep your child away from other children as much as possible until the diarrhoea has stopped.
When to see a doctor
Babies under six months old should always be checked by a GP if they have gastro, because they are at higher risk of dehydration.
Any child with gastro should see a GP if they:
- are vomiting and have diarrhoea, and are not drinking
- have a lot of diarrhoea (eight to 10 watery poos, or two or three large poos per day) or if the diarrhoea is not improving after 10 days
- vomit frequently and seem unable to keep any fluids down
- show signs of dehydration e.g. fewer wet nappies or not going to the toilet much, dark yellow or brown wee, feel lightheaded or dizzy, have dry lips and mouth
- have a bad stomach pain
- have any blood in their poo
- have green vomit
- are making you worried for any other reason.
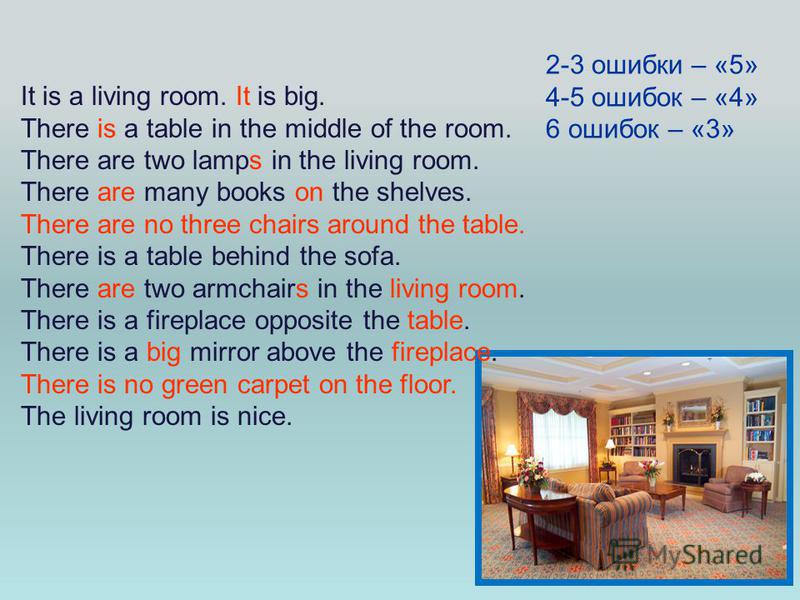
If your child is very dehydrated and cannot keep any fluids down, they may need to be admitted to hospital to have fluids by a tube through the nose into the stomach (a nasogastric tube) or directly into a vein through a drip (intravenous or IV therapy).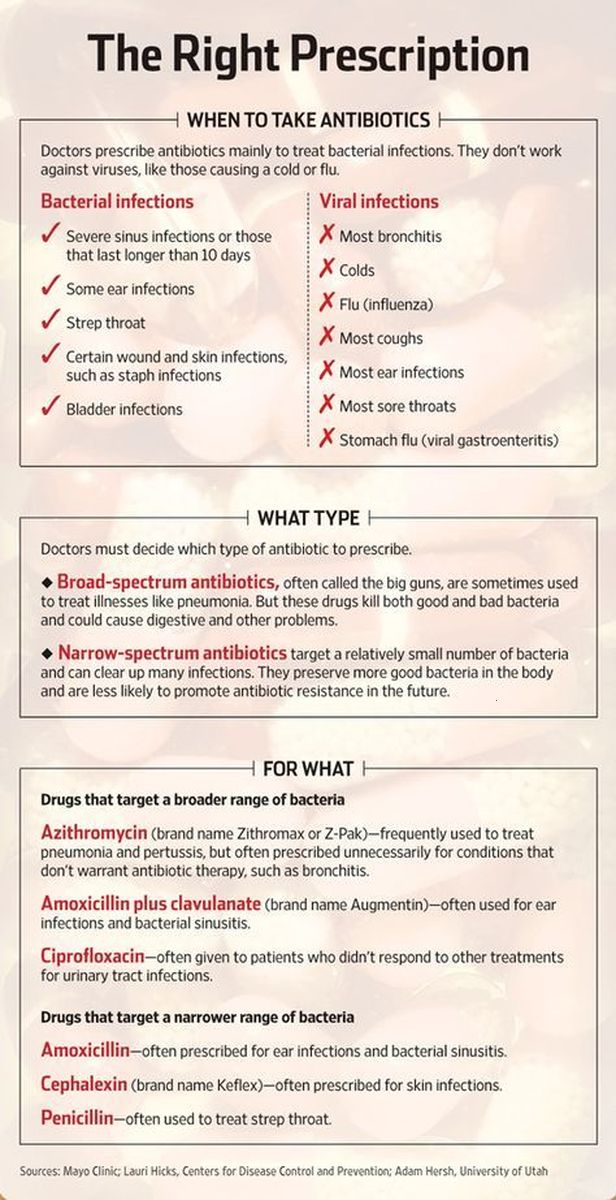
Key points to remember
- Babies under six months old with gastro can become dehydrated very easily and need to be checked by a GP.
- Offer babies a drink every time they vomit. Keep breastfeeding. If bottle feeding, give oral rehydration solution for the first 12 hours.
- Give children small amounts of fluid often.
- Your baby or child is infectious, so regularly wash your hands thoroughly, particularly before feeding and after nappy changes.
- Take your child to the doctor if they are becoming dehydrated, have bad stomach pain or you are worried.
For more information
- Better Health Channel: Gastroenteritis
- Raising Children Network: Gastroenteritis
- Kids Health Info fact sheet: Dehydration
- Kids Health Info fact sheet:
Stopping the spread of germs
Common questions our doctors are asked
I’m concerned the fluids I am giving my child is making the diarrhoea worse.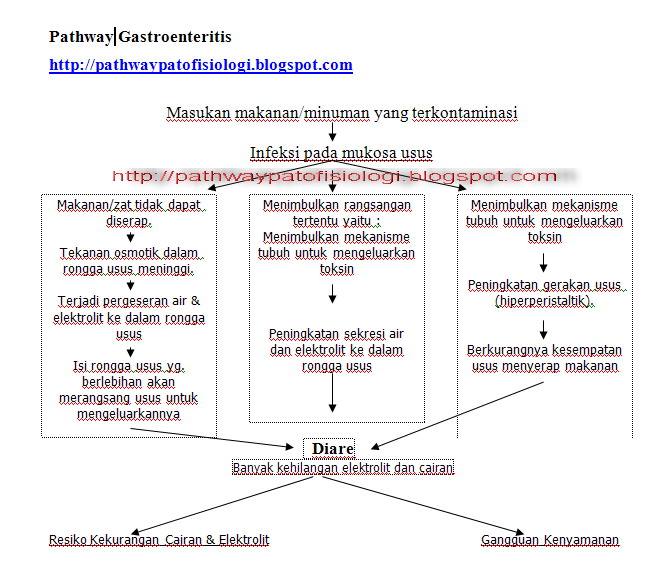 Should I give her less to drink?
Should I give her less to drink?
It is very important for fluids to be given, even if the diarrhoea seems to get worse. It is important to replace the fluids that are lost due to diarrhoea or vomiting to prevent dehydration.
Should I be worried that my child doesn’t want to eat when he has gastro?
When your child first gets gasto they may refuse food to start with. This is not a problem as long as they are drinking fluids. When your child becomes hungry again, give them the food they feel like eating.
Can my child have dairy after a bout of gastro?
Many children become sensitive to dairy following a bout of gastro. You can usually manage this by reducing their dairy intake for a period of three weeks following gastro. If the symptoms persist beyond this, take your child back to your GP.
Developed by The Royal Children's Hospital General Medicine, Emergency and Gastroenterology departments, and Centre for Community Child Health. We acknowledge the input of RCH consumers and carers.
We acknowledge the input of RCH consumers and carers.
Reviewed February 2018.
This information is awaiting routine review. Please always seek the most recent advice from a registered and practising clinician.
Kids Health Info is supported by The Royal Children’s Hospital Foundation. To donate, visit www.rchfoundation.org.au.
Gastroenteritis (Stomach Flu) (for Parents)
What Is Gastroenteritis?
Gastroenteritis, often called the stomach flu, is a common illness that causes nausea, vomiting, diarrhea, and belly cramps. It usually lasts a few days and isn't serious. Most kids get better at home by resting and drinking plenty of liquids.
What Causes Gastroenteritis?
Gastroenteritis (gass-troh-en-teh-RYE-tis) happens when germs (viruses, bacteria, or parasites) infect the stomach or intestines, causing inflammation.
In kids, viruses are the most common cause of gastroenteritis.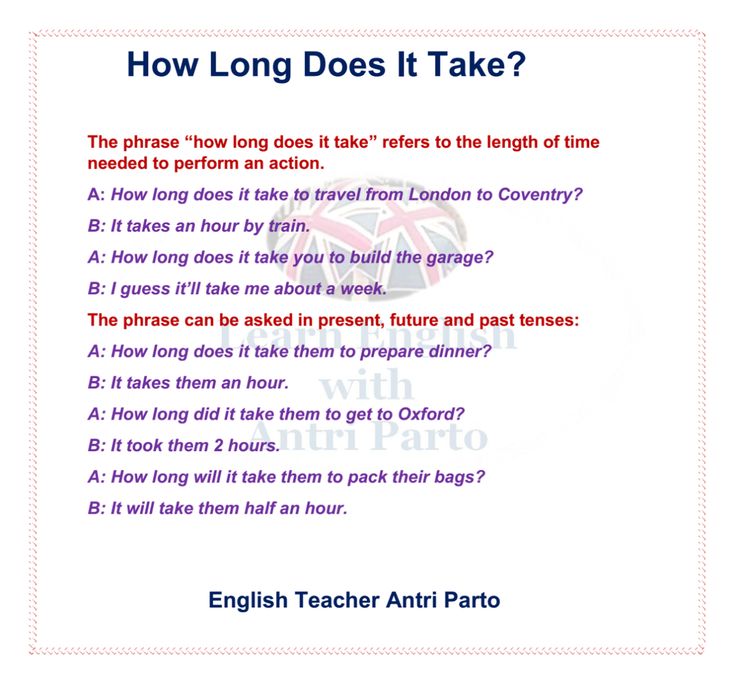 Rotavirus causes many cases of stomach flu in children, but the rotavirus vaccine can help prevent them.
Rotavirus causes many cases of stomach flu in children, but the rotavirus vaccine can help prevent them.
Many of the germs that cause gastroenteritis spread easily. So someone can get sick if they:
- Touch something contaminated and then touch food or their mouth.
- Share food or drinks with someone who is sick.
- Live with someone who’s infected, even if that person isn’t sick.
What Are the Signs & Symptoms of Gastroenteritis?
The most common signs of gastroenteritis are vomiting and diarrhea. Many children also have a fever.
When kids have diarrhea or vomiting, they lose lots of fluid in their poop or vomit. This can lead to dehydration (not having enough water in the body). If that happens, the body can have trouble working as it should.
How Is Gastroenteritis Diagnosed?
Doctors usually can tell if someone has stomach flu by hearing about the symptoms. Usually, no tests are needed. If a child is very sick or has blood or mucus in the poop, doctors might order a stool (poop) test, urine (pee) test, or blood test to check for dehydration and to see what’s causing it.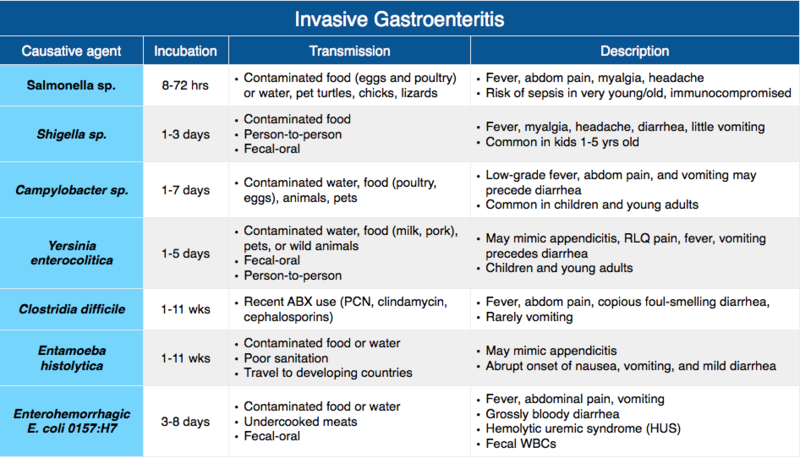
How Is Gastroenteritis Treated?
There is no specific treatment for gastroenteritis, and most kids can be treated at home. Keep your child hydrated by offering plenty of liquids. Kids with more severe dehydration may need treatment in the ER or hospital.
Mild dehydration is treated with oral (by mouth) rehydration. This usually includes giving oral rehydration solution (such as Pedialyte, Enfalyte, or a store brand). It has the right amounts of water, sugar, and salt to help with dehydration. You can buy it without a prescription at drugstores or supermarkets. If you can’t get oral rehydration solution, talk to your doctor.
If your child has mild dehydration and your doctor says it’s OK to start treatment at home:
- Give your child an oral electrolyte solution as often as possible. If your child throws up, start with small sips, about 1 or 2 teaspoons every few minutes.
- Babies can continue to breastfeed or take formula as long as they are not throwing up repeatedly.
- Don't give babies plain water instead of oral rehydration solution. It doesn't have the right nutrients for babies with dehydration.
- Older children can have frozen electrolyte popsicles.
- Do not give your child full-strength juice (undiluted), soda, or sports drinks. These have a lot of sugar, which can make diarrhea worse.
When your child stops vomiting, you can offer small amounts of solid foods, such as toast, crackers, rice, or mashed potatoes. Yogurt, fruits, vegetables, and lean meat, like chicken, are also OK.
A child who isn’t throwing up can eat a regular diet, if they feel up to it. It may take time for them to feel like eating. There's no need to avoid dairy unless it makes the vomiting or diarrhea worse. Avoid fatty foods, which can make diarrhea worse.
To help your child feel better, let your child rest as needed. You can give medicine for fever or pain, like acetaminophen or ibuprofen (do not give ibuprofen to babies under 6 months old), if your doctor says it’s OK. Follow the package directions for how much medicine to give and how often. Don't give aspirin to your child or teen. It's linked to a rare but serious illness called Reye syndrome.
Follow the package directions for how much medicine to give and how often. Don't give aspirin to your child or teen. It's linked to a rare but serious illness called Reye syndrome.
Don't give medicines for diarrhea or vomiting unless your doctor tells you to.
Keep your child out of school or childcare until 24 hours without vomiting or fever and diarrhea has improved. Your child also should stay out of swimming pools until all symptoms have stopped.
When Should I Call the Doctor?
Call the doctor if your child:
- can’t drink for several hours
- is peeing less often (more than 4–6 hours for babies and 6-8 hours for older children)
- has signs of dehydration, such as crying with few or no tears, having a dry mouth or cracked lips, feeling dizzy or lightheaded, acting very sleepy or less alert
- has a high fever
- has blood in their poop or vomit
- is vomiting for more than 24 hours or the diarrhea doesn’t get better after several days
Can Gastroenteritis Be Prevented?
Germs that cause gastroenteritis are contagious. The best way to avoid the illness is to keep the germs from spreading:
The best way to avoid the illness is to keep the germs from spreading:
- Teach all family members to wash their hands well and often. They should wash for at least 20 seconds with soap and water. This is especially important after using the bathroom and before preparing or eating food.
- Clean tabletops, doorknobs, and other surfaces that get touched a lot with a cleaner that kills viruses.
- Follow food safety guidelines to prevent bacteria and viruses from getting into food and drinks (food poisoning).
- Make sure your kids get all recommended immunizations on time.
Reviewed by: Mary L. Gavin, MD
Date reviewed: September 2021
What is gastroenteritis? - Outpatient medical facility
Wednesday, eleven December 2019
What is gastroenteritis?
Gastroenteritis is an infectious disease of the gastrointestinal tract, accompanied by vomiting and diarrhea.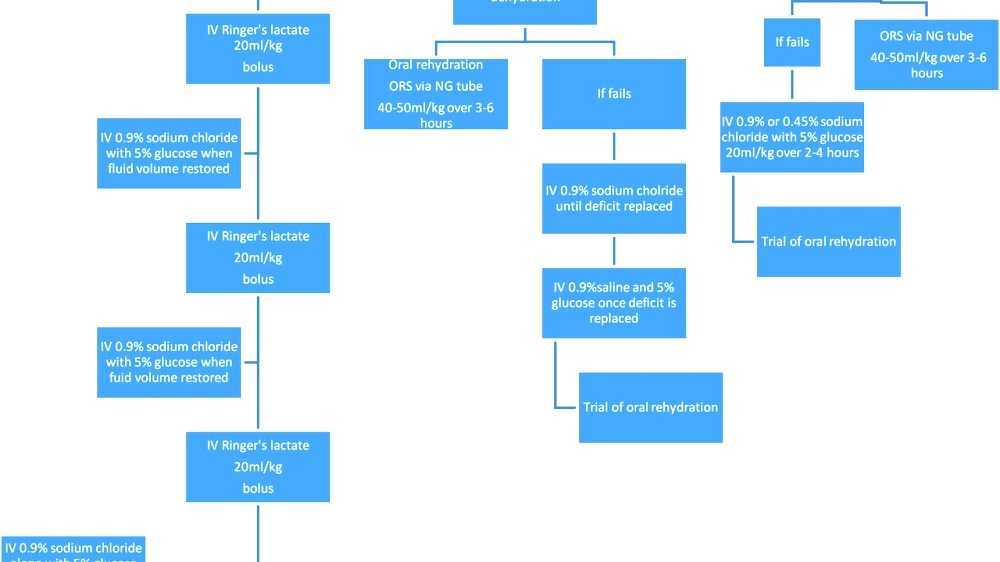 This is a very common disease in young children.
This is a very common disease in young children.
Symptoms of gastroenteritis include abdominal pain, nausea, vomiting, loose stools, and sometimes fever.
The incubation period lasts from several hours to several days. Gastroenteritis is caused by pathogenic bacteria or viruses. Since antibiotics do not work on viruses, they are not always prescribed. Drugs that stop diarrhea should be avoided: they prevent the rapid elimination of pathogens from the intestines.
The illness usually lasts 3-5 days. All this time the child should remain under supervision and receive plentiful drink.
Due to dehydration, the child feels very bad, he is overcome by weakness, drowsiness. Surround him with care and attention.
Gastroenteritis is a "disease of dirty hands". The causative agents of the disease enter the body with contaminated food, water, through dirty household items: nipples, spoons, toys, etc. One of the adult family members may be a carrier of the infection: without signs of illness, it releases pathogens into the environment if the sanitary and hygienic regime is not observed.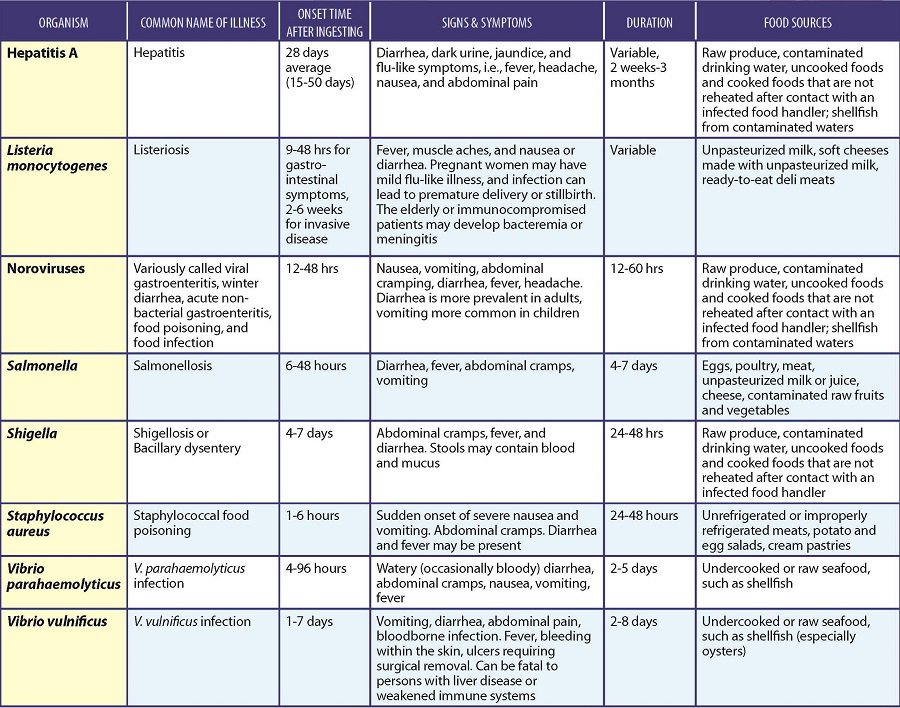
Bacteria can cause intestinal infections if food is not properly cooked and utensils and household items are not stored properly. The infection is also caused by salmonella, which is found in eggs, dairy products and raw poultry meat.
Protozoa: gastroenteritis can be caused, for example, by amoebas, giardia, which are easily contracted on foreign trips.
The main symptoms of gastroenteritis are repeated vomiting and frequent loose stools, but their severity may vary in each specific case. The stool is often watery, offensive, with flakes and greens. . Sometimes in children with gastroenteritis there is a significant increase in temperature, causing febrile convulsions in young children. . Bacterial and viral intestinal infections are often accompanied by crampy abdominal pain.
Call the doctor if the child continues to vomit for several hours, becomes lethargic and refuses to eat or drink.
If your child develops symptoms of dehydration, it is important to seek medical attention promptly.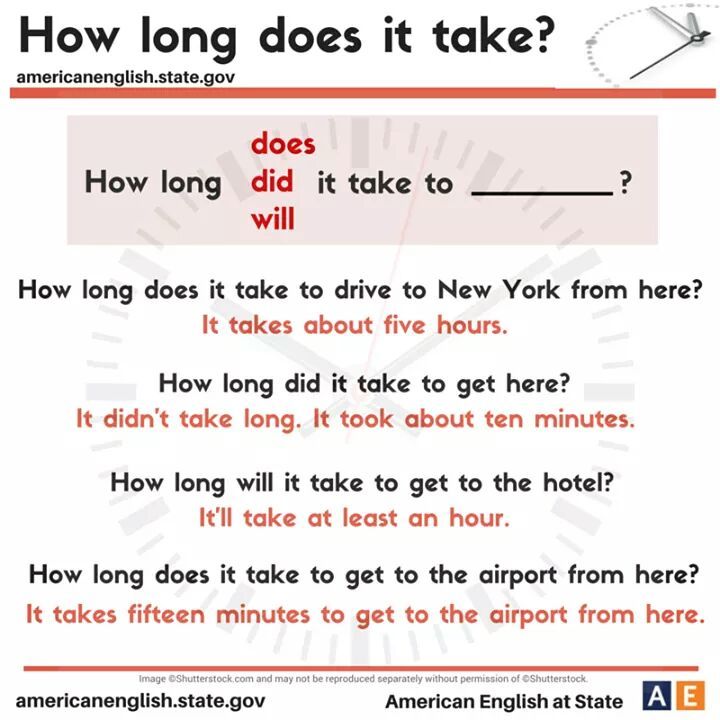 In most cases, dehydration can be eliminated fairly quickly by giving the child plenty of fluids.
In most cases, dehydration can be eliminated fairly quickly by giving the child plenty of fluids.
2-3 teaspoons every 2-3 minutes of any liquid helps to avoid the most serious complications.
Remember that your child is not well, so try to comfort him and make him as comfortable as possible. If the temperature starts to rise, remove the warm blanket, ventilate the room, turn on the fan. From constant diarrhea, the child may experience irritation in the anus. Gently wash the child with warm water, apply an emollient cream.
If the child drinks willingly and a lot, do not force him to eat. Nothing bad will happen if he refuses food for several days. It's important to stay hydrated.
Diarrhea may continue for several days after the fever subsides and vomiting stops.
If the child has a fever but is not vomiting, try to bring down the fever with a dose of a child's antipyretic. Keep in mind the following:
- Always thoroughly cook meat, wash even organic vegetables thoroughly.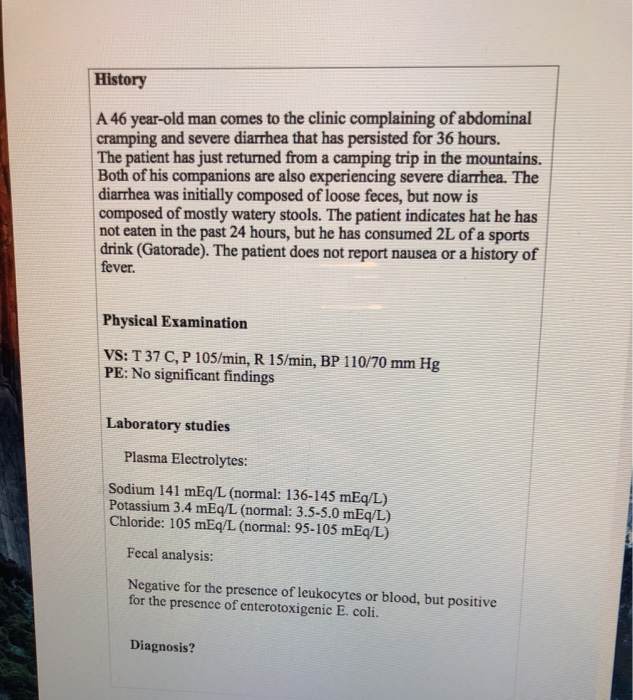
- When traveling with young children, drink only bottled water and eat at tourist restaurants. Do not eat food bought in bazaars and street stalls.
- Keep children away from people with gastroenteritis.
To prevent intestinal infection, be hygienic when preparing any food.
Gastroenteritis in children. What is gastroenteritis in children?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Gastroenteritis in children is an inflammation of the stomach and small intestine that occurs when infected with viruses, bacteria, or protozoa, under the influence of drugs, chemical toxins, or allergens. The clinical picture is represented by vomiting, repeated diarrhea with impurities of mucus and undigested food, cramping pains and cuttings in the abdominal cavity. Diagnosis of gastroenteritis includes mainly laboratory tests: coprogram, culture of feces and vomit, serological reactions. Less commonly, instrumental diagnostics (ultrasound, EFGDS) are performed. Treatment involves diet therapy, rehydration, etiopathogenetic and symptomatic medications.
Diagnosis of gastroenteritis includes mainly laboratory tests: coprogram, culture of feces and vomit, serological reactions. Less commonly, instrumental diagnostics (ultrasound, EFGDS) are performed. Treatment involves diet therapy, rehydration, etiopathogenetic and symptomatic medications.
ICD-10
A09.0 A09.9
- Causes
- Pathogenesis
- Symptoms of gastroenteritis in children
- Complications
- Diagnostics
- Treatment of gastroenteritis in children
- Diet therapy and rehydration
- Conservative therapy
- Prognosis and prevention
- Prices for treatment
General
Gastroenteritis, along with other disorders of the gastrointestinal tract, ranks second in the structure of morbidity after SARS. More than 3 billion cases are recorded annually in the world, more often among the child population of developing countries. Gastroenteritis is called "dirty hands disease", which indicates the main mechanism of infection. It poses the main danger for patients under 5 years of age, in whom dehydration rapidly increases, and in the absence of proper medical care, death. In the world, more than 10 thousand children die every year from the consequences of gastroenteritis.
Gastroenteritis is called "dirty hands disease", which indicates the main mechanism of infection. It poses the main danger for patients under 5 years of age, in whom dehydration rapidly increases, and in the absence of proper medical care, death. In the world, more than 10 thousand children die every year from the consequences of gastroenteritis.
Gastroenteritis in children
Causes
Gastroenteritis is often infectious in nature. They are caused by microorganisms that enter the mouth with food and water, when licking fingers, toys and foreign objects. Viral infections (rotavirus, norovirus, adenovirus) are considered the most common etiological factor. They tend to affect young children and preschoolers. There are other causes of pathology:
- Bacteria and parasites. Infants and younger children under three years of age are characterized by infection with pathogenic strains of E. coli, Staphylococcus aureus, and Salmonella.
 Regardless of the child's belonging to the age group, infection with Shigella, Yersinia, Campylobacter is possible. Among protozoan invasions, giardiasis and cryptosporidiosis occur.
Regardless of the child's belonging to the age group, infection with Shigella, Yersinia, Campylobacter is possible. Among protozoan invasions, giardiasis and cryptosporidiosis occur. - Allergens. When a prohibited product enters the gastrointestinal tract, an inflammatory process begins in the gastric and small intestine wall, manifested by typical symptoms of gastroenteritis. The most famous allergens for children are cow's milk, eggs, nuts. Less often, symptoms are provoked by the intake of fish, fruits and vegetables.
- Improper nutrition. In children of younger age groups, the digestive system is characterized by functional inferiority, therefore, gastrointestinal disorders in them are possible even with the use of high-quality products. Eating dry food, eating too much, or trying a new dish for the first time are all causes of gastroenteritis.
- Chemical toxins. Small children can accidentally swallow household chemicals and cosmetics, poisons for plants and insects.
 Toxic gastroenteritis also develops when poisoned by poisonous mushrooms, some types of exotic seafood that contain heavy metals.
Toxic gastroenteritis also develops when poisoned by poisonous mushrooms, some types of exotic seafood that contain heavy metals. - Medicines. At preschool age, it is not uncommon for a child to eat pills left unattended. Another reason for inflammation of the stomach and intestines is the long-term use of antibiotics or hormones as prescribed by a doctor, because of which the microflora of the gastrointestinal tract is disturbed in children, conditions are created for the reproduction of pathogens.
Pathogenesis
Unpleasant manifestations of gastroenteritis are associated with an inflammatory process affecting the gastric and intestinal wall. As a result of irritation of peripheral nerve receptors, signals arise that are sent to the centers of the medulla oblongata and provoke vomiting. Pain is caused by increased peristalsis, accumulation of pro-inflammatory substances, and their action on nerve endings.
Diarrhea in gastroenteritis in children develops by an osmotic or secretory mechanism. In the first case, the digestion of food components in the small intestine is disturbed, as a result of which its contents become hyperosmolar. In response to this, an increased amount of fluid enters the intestinal lumen from the vessels. Secretory diarrhea is characterized by a change in the transport systems of cells, the accumulation of sodium and chlorine ions in the gastrointestinal tract, which pull water along with them.
In the first case, the digestion of food components in the small intestine is disturbed, as a result of which its contents become hyperosmolar. In response to this, an increased amount of fluid enters the intestinal lumen from the vessels. Secretory diarrhea is characterized by a change in the transport systems of cells, the accumulation of sodium and chlorine ions in the gastrointestinal tract, which pull water along with them.
Symptoms of gastroenteritis in children
With infectious gastroenteritis, the incubation period ranges from 2-3 hours to several days. The disease begins suddenly and includes 3 main symptoms: severe pain and cramps in the abdomen, repeated vomiting, diarrhea. Older children complain of soreness in the upper abdomen and around the navel, and preschool patients usually cannot indicate the localization of discomfort.
Vomiting is repeated from 1-2 to 10 or more times per day. At first, vomit in children is abundant, they contain partially digested food. As the stomach empties, the child burps a meager amount of mucus mixed with bile. The frequency of stool varies from 5 to 20 times a day. The stools are liquid and fetid, contain a lot of mucus, food particles. Depending on the infection, the feces become bright yellow, orange, swamp green, etc.
As the stomach empties, the child burps a meager amount of mucus mixed with bile. The frequency of stool varies from 5 to 20 times a day. The stools are liquid and fetid, contain a lot of mucus, food particles. Depending on the infection, the feces become bright yellow, orange, swamp green, etc.
The disease is characterized by flatulence, rumbling and seething in the abdominal cavity, aggravated before the urge to defecate. The clinical picture of gastroenteritis in children is supplemented by an increase in body temperature to subfebrile or febrile numbers, lethargy and weakness, and a complete lack of appetite. In severe cases of the disease, dryness of the skin and mucous membranes, refusal of water is observed.
With chemical and medicinal gastroenteritis, the child's condition is more severe from the very beginning. There may be blood in the vomit and feces. The appearance of neurological or cardiovascular symptoms is characteristic, which indicates a total damage to the body by toxic substances. In infants, fontanelles sink, the skin becomes dry and cyanotic. Possible oppression of consciousness up to stupor and coma.
In infants, fontanelles sink, the skin becomes dry and cyanotic. Possible oppression of consciousness up to stupor and coma.
Complications
The most dangerous consequence of gastroenteritis in children is exsicosis (dehydration). With a mild degree, when fluid loss does not exceed 5% of body weight, thirst worries, diuresis slightly decreases, but the patient's general condition is satisfactory. With moderate dehydration, urination decreases sharply, the heart rate increases, and blood pressure decreases. Severe dehydration is characterized by collapse, confusion.
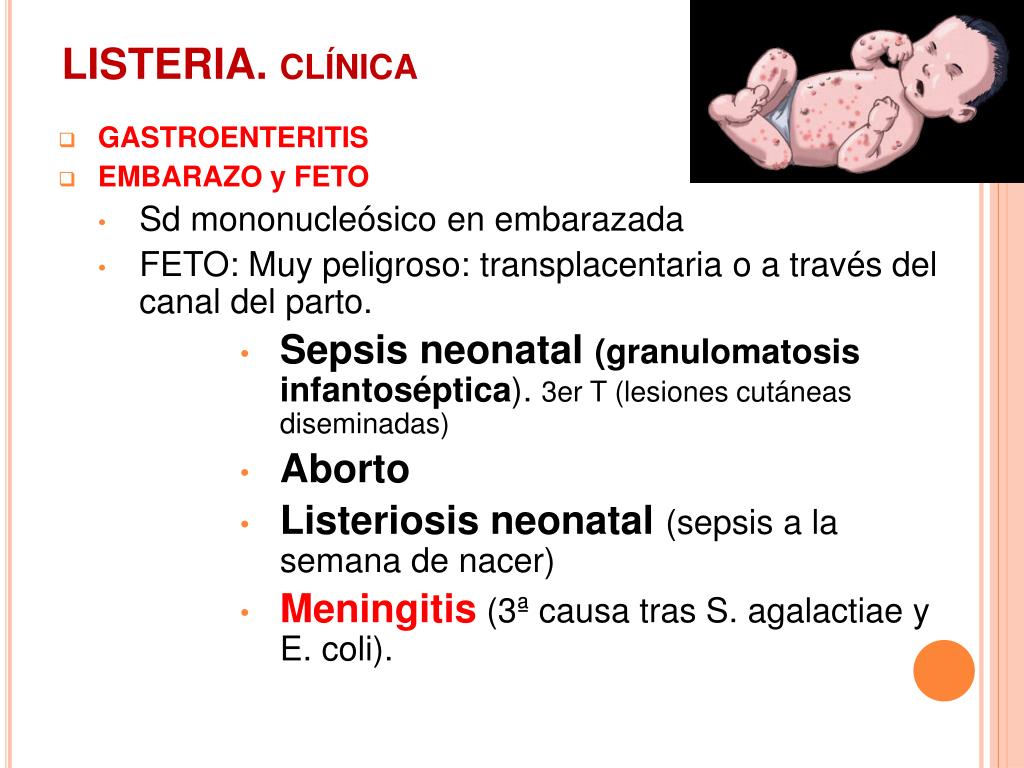
When infected with certain strains of Shigella and Escherichia, there is a risk of developing hemolytic uremic syndrome (HUS). It is manifested by the classical triad: hemolytic anemia with the presence of fragmented erythrocytes, acute renal failure, thrombocytopenia. It occurs mainly before the age of 3 with a frequency of 2-3 cases per 10,000 children with infectious gastroenteritis.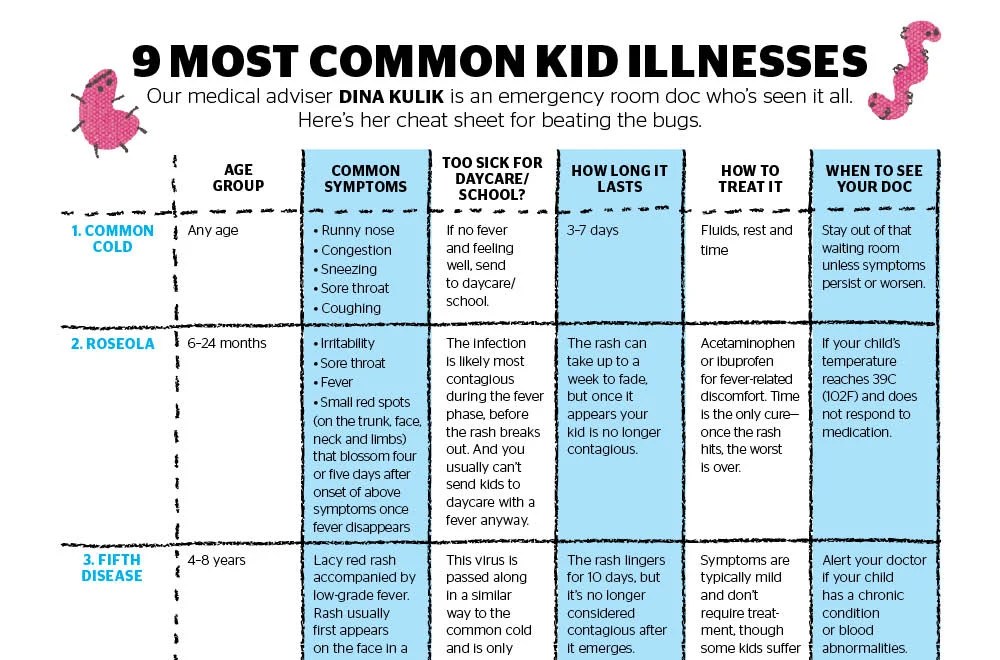
Diagnostics
When collecting complaints and anamnesis of the disease, conducting a physical examination, the pediatrician makes a topical diagnosis of "acute gastroenteritis". Further diagnostic search is aimed at identifying the etiological factors of the disease, which is necessary for the selection of differentiated treatment. The diagnostic plan includes:
- Coprogram. The main analysis, which demonstrates signs of an inflammatory process (leukocytes, mucus) and impaired digestion of food components (striated muscle fibers, starch grains). Additionally, they put the Gregersen reaction to occult blood to rule out colitis, an invasive type of diarrhea.
- Bakposev. For microbiological diagnostics, feces, vomit, gastric lavage are used. To establish the source of gastroenteritis in case of mass infection, examine the remains of food, drinking water. The material is sown on nutrient media, and ELISA and PCR of feces are also carried out for acute intestinal infections.
- Blood tests. A hemogram is ordered to assess the degree of dehydration (by hematocrit) and to look for signs of infectious inflammation. Additionally, a biochemical study and a coagulogram are recommended. For rapid diagnosis of gastroenteritis caused by protozoa and parasites, blood ELISA is performed.
- Instrumental methods. Research is used only for complicated course of gastroenteritis or for suspected chronic gastrointestinal disease in the acute stage. In pediatric gastroenterology, a non-invasive method of abdominal ultrasound is used; EFGDS and radiography are shown to clarify the diagnosis.
Treatment of gastroenteritis in children
Diet therapy and rehydration
Treatment of mild gastroenteritis is carried out on an outpatient basis, with moderate and severe course, especially in children under three years of age, emergency hospitalization is indicated. Medical tactics depend on the age of the patient, the degree of dehydration. Therapy begins with a diet: a decrease in the daily amount of food by 30-50% in the acute period, the use of mucous soups and cereals, vegetable purees. After the disappearance of vomiting and diarrhea, the menu is supplemented with familiar products.
Therapy begins with a diet: a decrease in the daily amount of food by 30-50% in the acute period, the use of mucous soups and cereals, vegetable purees. After the disappearance of vomiting and diarrhea, the menu is supplemented with familiar products.
The most important step in treatment is adequate rehydration. For patients who can drink water and do not suffer from uncontrollable vomiting, replenishment of fluid losses is carried out orally. To do this, use special solutions with a balanced content of electrolytes in order to prevent violations of homeostasis. During the first 6 hours, children are provided with enhanced rehydration, and then they move on to the maintenance stage.
In severe condition of the child, the method of choice for gastroenteritis is parenteral rehydration. The volume of infusion solutions is calculated taking into account the weight of the patient and the degree of exsicosis. In the first 4-8 hours, a massive water load is carried out in the hospital to correct pathological losses and normalize the child's condition. After you feel better and thirsty, you can switch to oral rehydration.
After you feel better and thirsty, you can switch to oral rehydration.
Conservative therapy
Antibacterial agents for the treatment of acute gastroenteritis in pediatrics are prescribed according to strict indications - in the presence of severe forms of the disease in infants up to six months, immunodeficiency states and hemolytic anemia in all age groups, the development of secondary bacterial complications. From antibiotics, cephalosporins, macrolides, nitrofuran derivatives are used. Pathogenetic therapy includes a number of drugs:
- Probiotics. Medicines normalize the intestinal microflora and increase natural immunity to the action of bacteria and viruses. They are taken in addition to antibiotics or as independent medicines. In practical gastroenterology, preparations with lacto- and bifidobacteria, saccharomycetes are used.
- Enterosorbents. Means fix pathogens of intestinal infections and their toxins on their surface, reduce the damaging effect on the intestinal wall, and prevent the generalization of the process.
 “White” sorbents are recognized as the best for children to take, which are safe, do not require taking a large number of tablets (as is the case with activated charcoal).
“White” sorbents are recognized as the best for children to take, which are safe, do not require taking a large number of tablets (as is the case with activated charcoal). - Immunomodulators. Recommended for severe viral gastroenteritis to speed up recovery if the child's body's own defenses are reduced. Recombinant interferons, interferon inducers, immunoglobulin preparations are used.
- Enzymes. Medications do not have a high level of evidence, but are occasionally prescribed for prolonged gastroenteritis, which are accompanied by impaired digestion of food. Means with pancreatic enzymes improve the breakdown of nutrients and prevent the development of protein-energy malnutrition in children.
Prognosis and prevention
In mild and moderate forms of the disease, recovery occurs after 1-2 weeks without unpleasant consequences. In cases of severe gastroenteritis, the prognosis in children is determined by the timeliness of seeking medical help and the volume of therapeutic measures. Early initiation of rehydration in combination with medical therapy significantly reduces the risk of complications.
Early initiation of rehydration in combination with medical therapy significantly reduces the risk of complications.
A modern measure for the prevention of rotavirus infection in children is vaccination, which is carried out at the age of 6 months to 3 years. To prevent other forms of gastroenteritis, you must follow the standard rules: teach your child to personal hygiene, thoroughly wash food and heat treat it, and do not use drinking water from unknown sources.
You can share your medical history, what helped you in the treatment of gastroenteritis in children.
Sources
- Rational prevention of complications of acute intestinal infections in pediatric practice / Т.А. Ruzhentsova, N.A. Meshkova // Attending physician. — 2019.
- Childhood diseases/ N.P. Shabalov. — 2017.
- Clinical guidelines of the Ministry of Health of the Russian Federation (treatment protocol) for the provision of medical care to children with rotavirus infection.
 Offer your baby a drink every time they vomit.
Offer your baby a drink every time they vomit.