Incontinence early pregnancy sign
Causes, Management Tips, and More
Pregnancy Incontinence: Causes, Management Tips, and More- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Michael Weber, M. D. — By Ashley Marcin on February 22, 2017
What is pregnancy incontinence?
Frequent urination is one of the earliest signs of pregnancy. Leaking urine, or incontinence, is also a common symptom during and after pregnancy. About 54.3 percent of pregnant women report negative effects on their quality of life, including travel and emotional areas. Symptoms can increase as the baby grows and last a few weeks after birth.
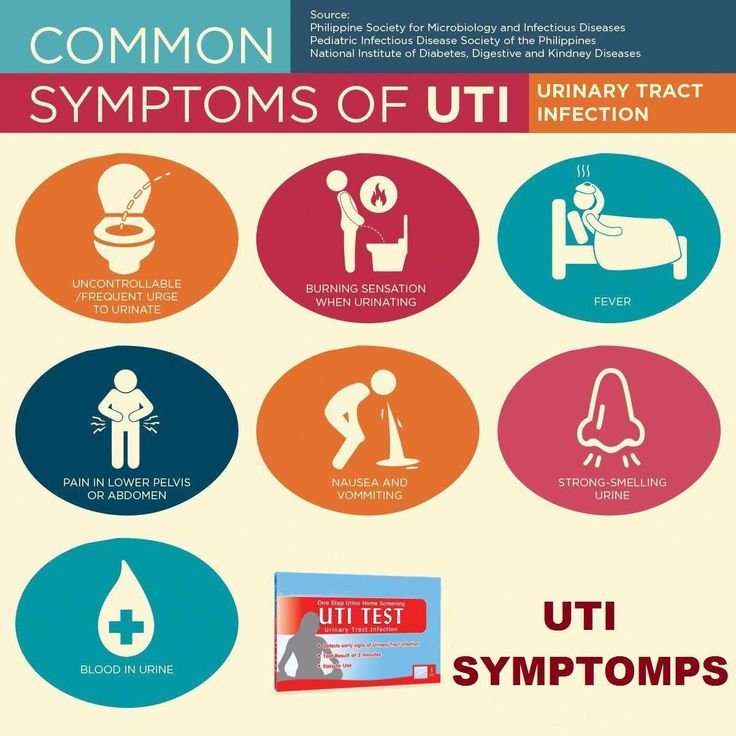
There are several types of urinary incontinence:
- stress incontinence: loss of urine due to physical pressure on the bladder
- urgency incontinence: loss of urine due to an urgent need to urinate, commonly caused by bladder contractions
- mixed incontinence: a combination of stress and urgency incontinence
- transient incontinence: temporary loss of urine due to a medication or a temporary condition, such as a urinary tract infection or constipation
Learn more about why you may have incontinence during or after pregnancy, what it means for you and baby, and how you can cope.
Is it urine or amniotic fluid?
Q:
How can I know if I’m leaking urine or amniotic fluid?
Anonymous patient
A:
Short of going to the hospital to test the fluid, you can check how the fluid leaks. If it’s appearing intermittently and in smaller amounts, it’s probably urine. Most of the time when amniotic fluid leaks, it comes in much larger amounts (often described as a “gush”) and persists continuously. The presence of a white waxy or dark green substance is also indicative of amniotic fluid.
Michael Weber, MD
Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
What causes pregnancy incontinence?
Your bladder sits right above your pelvic bones and is supported by your pelvic floor. It relaxes and fills with urine throughout the day while the sphincter keeps the organ closed until you can use the bathroom. During pregnancy and childbirth, your pelvic floor muscles are put to the test.
During pregnancy and childbirth, your pelvic floor muscles are put to the test.
Common causes of pregnancy incontinence include:
Pressure: You may leak when you cough, sneeze, exercise, or laugh. These physical movements put extra pressure on your bladder, which causes stress incontinence. Your baby also puts extra pressure on your bladder as they grow bigger.
Hormones: Changing hormones can affect the lining of your bladder and urethra.
Medical conditions: Some medical causes for incontinence include diabetes, multiple sclerosis, anxiety medications, or a stroke in the past.
Urinary tract infections (UTIs): Between 30 to 40 percent of women who didn’t treat their UTI completely will develop symptoms during pregnancy. Incontinence is a symptom of UTI.
What are the treatment options for pregnancy incontinence?
The first lines of treatment for pregnancy incontinence are lifestyle changes and bladder management. Here are some tips for managing your bladder:
Here are some tips for managing your bladder:
Do Kegels: Kegel exercises to strengthen your pelvic floor. They’re a safe and effective exercise before, during, and after pregnancy. To do a Kegel, focus on the muscles you use to hold in urine. Squeeze them for ten seconds before relaxing. Aim to do five sets of these exercises per day. Learning how to relax your pelvic floor may help during and after labor.
Create a bladder diary: Jot down when you notice the most leaks so you can plan your trips. This is also the first step to bladder retraining. Bladder retraining is about re-teaching your bladder to hold more urine by extending time between trips.
Avoid carbonated or caffeinated drinks: Avoid carbonated drinks, coffee, or tea. These beverages may make you feel like you need to use the bathroom more often. Try drinking more water or decaffeinated drinks.
Avoid drinking at night: Limit your beverages in the evening to avoid frequent trips to the bathroom and leaking at night.
Eat a high-fiber diet: Eat foods that are high in fiber to avoid constipation, which puts added stress on your pelvic floor.
Maintain a healthy weight: Extra weight, especially around your abdomen, increases pressure over your bladder. Losing weight after labor can also help with incontinence after pregnancy.
Read more: Natural remedies for an overactive bladder »
Discuss any big changes with your doctor to make sure you’re doing what’s best for yourself and your baby. While medication and surgery are also options for incontinence, you may want to wait until after your pregnancy.
Tips for preventing UTIs
Do
- drink plenty of water, up to eight glasses per day
- urinate before and after having sex
- wipe from front to back after urination
- wear cotton fabrics and loose fitting clothes when possible
- change your underwear each day
Contact your doctor if you think you have a UTI. An untreated UTI can lead to a kidney infection, which may also cause early labor and a low birth weight.
An untreated UTI can lead to a kidney infection, which may also cause early labor and a low birth weight.
Don’t
- engage in intercourse while you have a UTI
- drink beverages that irritate the bladder, like fruit juices, caffeine, alcohol, and sugar
- hold your urine for long periods of time
- use strong soaps, douches, sprays, or powders
- wear the same underwear for more than a day
Treatment for a UTI involves antibiotics for three to seven days. This treatment is safe for your baby. Call your doctor if you have side effects, such as a fever, chills, or cramps, after taking your medication.
Are some women more at risk for pregnancy incontinence?
Women who already have an overactive bladder or urgency incontinence will likely have symptoms that continue or worsen during pregnancy.
Other risk factors include:
- older age
- being overweight
- having previous vaginal delivery
- having previous pelvic surgery
- smoking, which leads to chronic coughing
Causes after childbirth
Giving birth can contribute to incontinence after pregnancy. During vaginal delivery, muscles and nerves may be injured. A long labor or prolonged pushing can increase the likelihood of damage to nerves as well. The American Congress of Obstetricians and Gynecologists recognizes that cesarean delivery reduces incontinence during the first year. However, the benefits go away two to five years after delivery.
During vaginal delivery, muscles and nerves may be injured. A long labor or prolonged pushing can increase the likelihood of damage to nerves as well. The American Congress of Obstetricians and Gynecologists recognizes that cesarean delivery reduces incontinence during the first year. However, the benefits go away two to five years after delivery.
How is pregnancy incontinence diagnosed?
Tell your doctor if you’re experiencing incontinence. In some cases, it may be a UTI and you may need antibiotics. If you’re near the end of your pregnancy, you may also confuse leaking urine with leaking amniotic fluid. It’s best to check with your doctor so you know the exact cause.
If signs of labor and infection are cleared, your doctor may perform other tests. A bladder scan using ultrasound can help see if your bladder is emptying the whole way. A bladder stress test allows your doctor to see if you have leaking when you cough or bend down.
If your doctor suspects you have a UTI, they will likely ask for a urine sample for lab testing.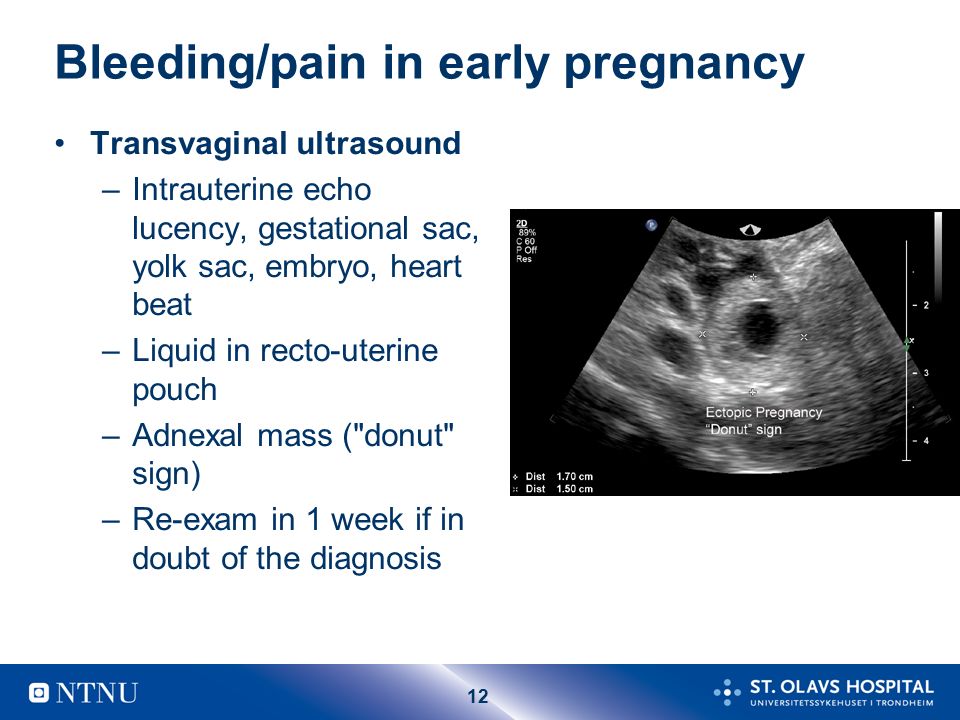 This may require you go to your hospital’s lab instead of your usual office. Your doctor may also perform special tests to check if the fluid you’re leaking is from your water breaking.
This may require you go to your hospital’s lab instead of your usual office. Your doctor may also perform special tests to check if the fluid you’re leaking is from your water breaking.
Does incontinence go away after the baby is born?
Some women’s incontinence symptoms go away in the days or weeks after their baby is born. For others, the leaking continues or may get worse. However, incontinence can be managed with first line treatments such as Kegels, bladder retraining, weight loss, and exercise.
Speak with your doctor about your concerns, especially if lifestyle changes don’t work or you’re still experiencing incontinence six or more weeks after delivery. You may want to consider other treatments such as medications and surgery after your pregnancy.
Read more: Female urinary stress incontinence treatments »
How can you prevent pregnancy incontinence?
Remember: Pregnancy incontinence is a common condition, especially as your belly grows or after your delivery. The good news is that the tips listed above are effective ways to manage incontinence.
The good news is that the tips listed above are effective ways to manage incontinence.
Keep reading: Prenatal care: Urinary frequency and urgency »
Last medically reviewed on February 22, 2017
- Parenthood
- Pregnancy
- Pregnancy Health
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Bladder control problems in women (Urinary incontinence). (2016, July)
niddk.nih.gov/health-information/urologic-diseases/bladder-control-problems-women - Committee opinion. (2015)
acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Cesarean-Delivery-on-Maternal-Request - Hooton, T.
 M. (2016, April 29). Urinary tract infections and asymptomatic bacteriuria in pregnancy
M. (2016, April 29). Urinary tract infections and asymptomatic bacteriuria in pregnancy
uptodate.com/contents/urinary-tract-infections-and-asymptomatic-bacteriuria-in-pregnancy - Mayo Clinic Staff. (2014, September 16). Stress incontinence: Risk factors
mayoclinic.org/diseases-conditions/stress-incontinence/basics/risk-factors/con-20027722 - Poise. (n.d.). How can I identify if I have pregnancy incontinence? Retrieved from
poise.com.au/facts-and-support/pregnancy-incontinence/how-can-i-identify-if-i-have-pregnancy-incontinence/ - Pregnancy, childbirth, & bladder control. (2016, February 2)
my.clevelandclinic.org/health/articles/pregnancy-childbirth-bladder-control - Sangsawang, B., & Sangsawang, N. (2013). Stress urinary incontinence in pregnant women: A review of prevalence, pathophysiology, and treatment. International Urogynecology Journal, 24(6), 901-912
ncbi.nlm.nih.gov/pmc/articles/PMC3671107/ - Urinary tract infection during pregnancy.
 (2015, August)
(2015, August)
americanpregnancy.org/pregnancy-complications/urinary-tract-infections-during-pregnancy/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Feb 22, 2017
Written By
Ashley Marcin
Edited By
Austin Anaya
Medically Reviewed By
Michael Weber, MD
Share this article
Medically reviewed by Michael Weber, M.D. — By Ashley Marcin on February 22, 2017
related stories
Overflow Incontinence: What Is It and How Is It Treated?
What You Need to Know About Urge Incontinence
What Causes Peeing While Coughing?
Stress Incontinence
Pregnancy Friendly Recipe: Creamy White Chicken Chili with Greek Yogurt
Read this next
Overflow Incontinence: What Is It and How Is It Treated?
Medically reviewed by Harshil Matta, DO
Overflow incontinence occurs when your bladder doesn't completely empty when you urinate.
 Learn why this happens and how it's managed.
Learn why this happens and how it's managed.READ MORE
What You Need to Know About Urge Incontinence
Medically reviewed by Stacy Sampson, D.O.
Urge incontinence occurs when you have a sudden urge to urinate and can’t hold the urine in. Discover causes, home remedies, and more here.
READ MORE
What Causes Peeing While Coughing?
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN
Having urine leak while you cough is a medical condition known as stress urinary incontinence. Learn more about what causes it.
READ MORE
Stress Incontinence
Medically reviewed by Graham Rogers, M.D.
Stress incontinence is the inability to control your urge to urinate. Read more on how to treat this serious and embarrassing disorder.
READ MORE
Pregnancy Friendly Recipe: Creamy White Chicken Chili with Greek Yogurt
This pregnancy-friendly spin on traditional chili is packed with the nutrients your body needs when you're expecting.
READ MORE
What You Should Know About Consuming Turmeric During Pregnancy
Consuming turmeric in pregnancy is a debated subject. We'll tell you if it's safe.
READ MORE
Pregnancy-Friendly Recipe: Herby Gruyère Frittata with Asparagus and Sweet Potatoes
Medically reviewed by Kathy W. Warwick, R.D., CDE
So easy and delicious. This frittata is high in protein and rich in essential nutrients your body needs to support a growing baby. Bonus: You can…
READ MORE
The Best Stretch Mark Creams and Belly Oils for Pregnancy in 2023
Stretch marks are easier to prevent than erase.
 If you're seeking a preventive, we've gathered a few of the best stretch mark creams for pregnancy.
If you're seeking a preventive, we've gathered a few of the best stretch mark creams for pregnancy.READ MORE
Why Twins Don’t Have Identical Fingerprints
Medically reviewed by Alana Biggers, M.D., MPH
Identical twins are the same in so many ways, but does that include having the same fingerprints? There's conflicting information out there so we look…
READ MORE
Doula vs. Midwife: What’s the Difference?
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
What is the difference between a doula and a midwife? Do I need to choose? Read on to learn more about the similarities and differences.
READ MORE
10 Early Pregnancy Symptoms - Lifeline Pregnancy Help Clinic
by Breanne Hunt
Interesting things happening in your body? Maybe you find yourself exhausted, nauseous, or more emotional than usual. And oh yeah, it’s been awhile since you’ve had a period. These clues start swimming around in your mind and you wonder, are these pregnancy symptoms??
And oh yeah, it’s been awhile since you’ve had a period. These clues start swimming around in your mind and you wonder, are these pregnancy symptoms??
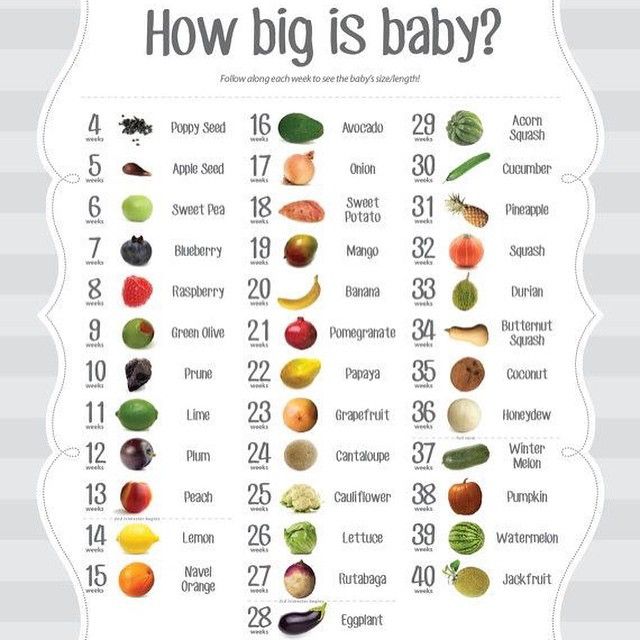
Now let’s be clear: the only way to be certain a woman is pregnant is through a pregnancy test. But if you are pregnant, you may experience a variety of bodily changes, even as early as a week after conception. Every woman is different. Your symptoms could be very different from your best friend’s or your sister’s or even from your own previous pregnancies. Just because you don’t have morning sickness or that famous pregnancy glow, doesn’t mean the possibility of pregnancy is out the window. You may not ever have these pregnancy symptoms, or they could crop up later on.
That being said, there are a variety of changes you are likely to undergo during the early stages of pregnancy.
10 Common Pregnancy Symptoms:
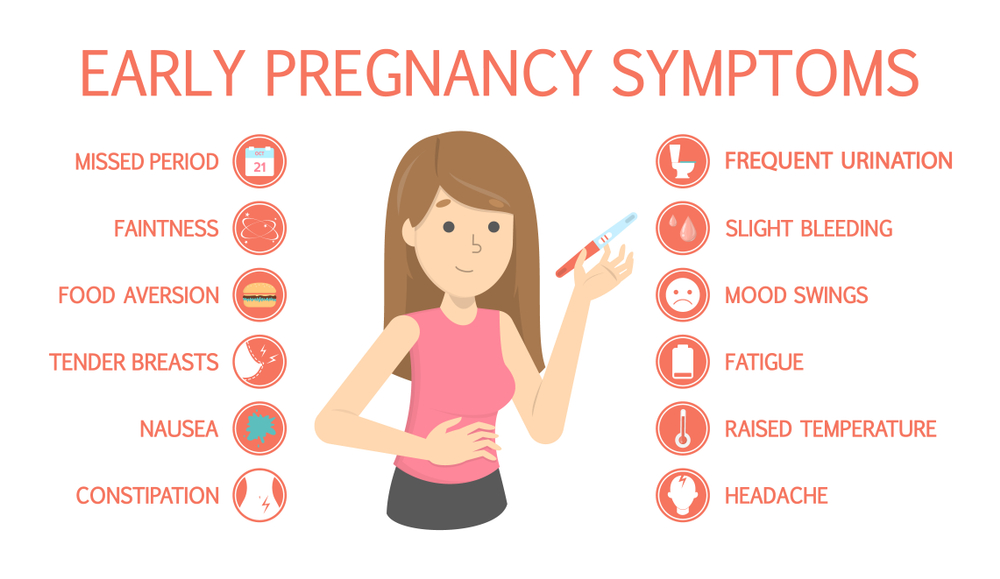
Spotting and cramping
After conception (when the sperm meets the egg), the fertilized egg implants into the wall of the uterus.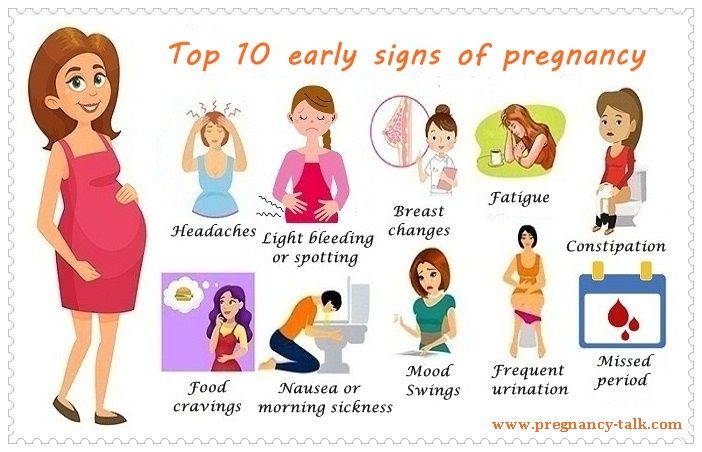 The uterus is where the baby grows and lives for nine months. When the egg attaches to the uterus, there could be some slight cramping or spotting, known as implantation bleeding. This happens 6-12 days after conception. If bleeding occurs it should be very light and could last a couple days. This bleeding should be lighter and shorter than a normal period.
The uterus is where the baby grows and lives for nine months. When the egg attaches to the uterus, there could be some slight cramping or spotting, known as implantation bleeding. This happens 6-12 days after conception. If bleeding occurs it should be very light and could last a couple days. This bleeding should be lighter and shorter than a normal period.
Missed Period
Once the fertilized egg implants, the body will begin releasing a hormone known HCG. HCG is what urine pregnancy tests are looking for. This hormone tells the ovaries to stop releasing eggs. HCG also tells the body to stop shedding the lining of the uterus (which means no periods). That lining instead turns into a cozy environment for a baby to develop.
Nausea (Morning Sickness)
According to the American Pregnancy Association, 25% of women report nausea as their earliest pregnancy symptom. Though commonly referred to as “morning sickness,” this can happen at any time of the day. Whatever causes this unpleasant symptom hasn’t been found, but it’s likely the body’s reaction to the change in hormones.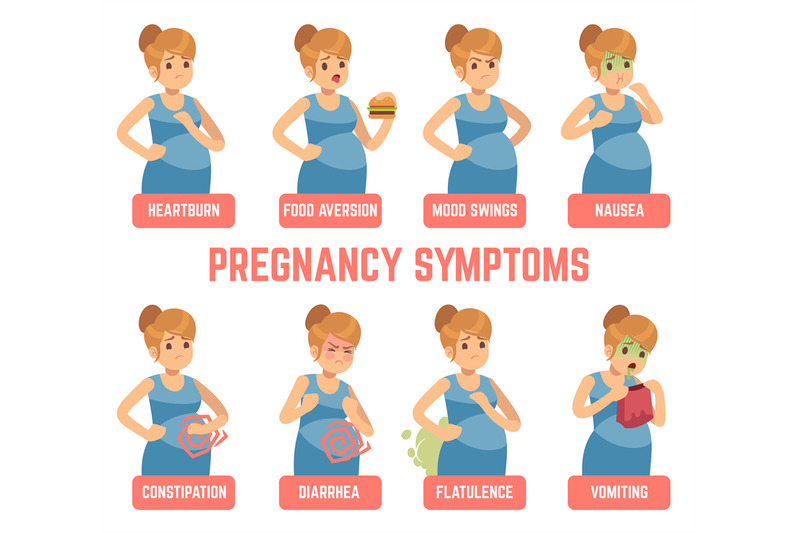
Breast Changes
Also as a result of rapid hormone changes, the breasts may feel swollen, sore, or tingly a couple weeks after conception. They may even feel fuller, and the area around the nipples (the areola) might darken.
Increased heart rate
The heart begins to pump faster during pregnancy due to the rise in hormones. Palpitations and changes in heart rhythm are common because of this. As always, talk to your doctor about what is normal during pregnancy and report any chest pain or other changes in your heart rate.
Fatigue
Because of the hormonal changes as well as a drop in blood sugar, blood pressure, and increased blood production, the body might feel more exhausted than normal. This can happen even as early as a week after conception.
Mood Swings
You may feel more emotional than usual during pregnancy. Those good ol’ hormonal changes could cause feelings of depression, anxiety, irritability, or intense excitement.
Skin changes
The pregnancy glow you hear about is caused by a combination of increased blood volume and higher hormone levels pushing more blood through the vessels.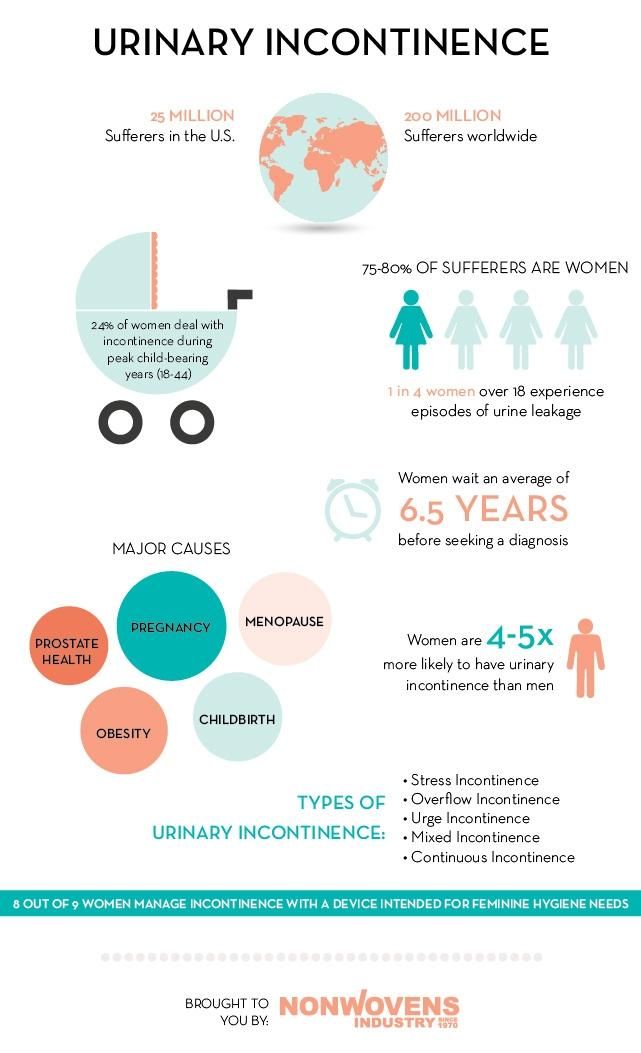 This causes the skin to produce more oil than usual, creating a natural gloss and blush. However, this increase in oil could also lead to more acne than you may typically experience.
This causes the skin to produce more oil than usual, creating a natural gloss and blush. However, this increase in oil could also lead to more acne than you may typically experience.
Frequent urination and incontinence
During pregnancy, the body boosts the amount of blood it pumps. This leads to the kidneys processing more fluid than usual, which in turn causes a fuller bladder.
Food cravings/aversions
Your developing baby needs lots of nutrients, some of which you may not normally eat. Your body will start to crave foods you don’t often find appealing so that you and baby will get all the right nutrients you both need. Some women report a new aversion to certain tastes or smells, which–you guessed it–is due to change in hormones. These aversions should go away around week 13 or 14.
How do I know for sure?
Remember, you could experience all of these pregnancy symptoms or only a couple. Always talk to your doctor about any symptoms that interfere with your everyday life. He or she can help you form a plan to ease these more uncomfortable changes.
Taking a pregnancy test is the first step in confirming a pregnancy. Lifeline Pregnancy Help Clinic offers confidential, no-cost pregnancy tests, as well as a variety of other resources to help you figure out your next steps if the test is positive. Pregnancy brings a lot of changes, physical and otherwise, but you don’t have to walk through it alone. Call Lifeline at 660-665-5688 or click here to request an appointment.
Make an Appointment
References:
WebMD http://www.webmd.com/baby/guide/pregnancy-am-i-pregnant#1
American Pregnancy Association http://americanpregnancy.org/getting-pregnant/early-pregnancy-symptoms/
What to Expect http://www.whattoexpect.com/pregnancy/pregnancy-health/early-symptoms-of-pregnancy
What causes urinary incontinence in pregnant women
One of the signs of pregnancy is frequent urination. In process of increase in term the phenomenon is expressed more often, especially at night. Unfortunately, this is often not the only change in the work of the expectant mother's urination organs. Against the background of metamorphoses occurring in the body of a woman, various disorders in the functioning of the kidneys and bladder appear. One of these troubles can be urinary incontinence in pregnant women. The condition causes discomfort but is not a serious health threat. The main symptoms are involuntary excretion of urine in small portions. This usually manifests itself at the moment of tension in the abdominal muscles. If a woman laughs, sneezes or coughs, the laundry suddenly becomes wet. There is no need to be afraid of this, in most cases the condition intensifies in the 2nd or 3rd trimester, but after childbirth the body returns to normal. However, to rule out the presence of serious problems, it is worth consulting with your doctor.
Types of urinary incontinence during pregnancy
Most often, 3 types of urinary incontinence in a pregnant woman appear, and in each case there are characteristic signs.
- Stress. It manifests itself with the tension of the abdominal muscles and fluctuations of the diaphragm. That is, it is enough to sneeze, cough or laugh so that a couple of drops of urine appear on the linen. The condition is typical for the first trimester.
- Urgent. Symptoms are sudden urge to urinate. They arise so unexpectedly that the expectant mother simply does not have enough time to run to the bathroom. One of the causes of the condition lies in the irritation of the urinary canal. You can also blame the failure of the nervous system and overstretching of the muscles in the pelvis. The condition is typical for the last trimester, but also occurs after childbirth.
- Full bladder syndrome. The symptom is the inability to completely empty the bladder. A woman often feels an acute urge to urinate, and after leaving the toilet it seems that urine remains in the ureter. The reason may be hidden in the stretched and therefore sluggish walls of the bladder.
Regardless of the cause of urinary incontinence in a pregnant woman, the condition causes discomfort and stress. This is not a reason to panic, in fact, the situation is not so critical - most often, not the entire volume of urine from the bladder is released, but only a small amount. To calm down in such a difficult period, it is enough to consult a doctor and get an appointment if necessary.
Main causes of urinary incontinence in pregnant women
Given that it is not difficult to find an explanation for urinary incontinence in a pregnant woman, it should not cause much concern. It is only necessary to identify the causes and make sure that this is due to physiology, and not diseases of the genitourinary system. The doctor who leads the pregnancy will help dispel fears.
The main cause is weakened muscles in the pelvic area. Excessive stretching of muscle tissue leads to loss of tone. As a result, the sphincter that holds urine, the walls of the bladder, and other muscles are weakened. This is due to hormonal changes, as well as changes in the size of internal organs. For example, the growing uterus during pregnancy compresses the bladder. As a result, its volume decreases, and urination occurs more often.
Another cause of urinary incontinence in a woman during pregnancy is the impact of a baby's foot on the bladder. This phenomenon does not happen to everyone. Doctors explain its severity by the position and size of the fetus, as well as the physical form of the expectant mother.
The number of previous pregnancies and births is also thought to increase the risk of urinary incontinence. Especially if the pregnancies go one after another, and the woman's muscles simply do not have time to recover.
Other factors associated with urinary incontinence during pregnancy are overweight and a sedentary lifestyle. A protracted birth process provokes a problem already in the postpartum period.
Healthy urinary retention occurs when the following conditions are met:
- when the bladder is in a normal position;
- immobility of the urethra;
- good work of the muscles surrounding the bladder and pelvic floor muscles;
- with the functional and anatomical integrity of the urethra and bladder closure apparatus.
What to do to deal with the problem
As mentioned above, urinary incontinence in women during pregnancy is most often associated with physiological changes, so no treatment is required. However, given the responsibility for the health of the baby during this period, you need to consult a doctor and, according to his appointment, take a urine test. This is necessary to exclude or identify urinary infections and diseases associated with them.
If the tests do not show deviations, it remains only to calm down and practice hygiene more often. The doctor will give recommendations on hygiene products - their choice and the frequency of changing underwear. But even without a specialist, we can say that the replacement of pads and panties is carried out as needed. Lingerie should fit the size, and it is better to choose a special cut for expectant mothers so that it does not press anywhere. Decorative details on underwear are not welcome, you should give preference to simple panties made of natural fabric.
If there is a problem, you will often have to wash yourself, go to the toilet on time. Doctors advise you to lean forward slightly when urinating. This will allow the urethra to open completely. At the end, you need to push slightly (without fanaticism) to completely empty the bladder.
Reducing the pressure on the diaphragm can help reduce the risk of urine leakage when sneezing and coughing. To do this, you need to open your mouth, normalizing the pressure.
Examination and treatment
Before dealing with incontinence, it is imperative to establish its cause by contacting a doctor. The doctor, in turn, will prescribe the necessary examination. It usually consists of several stages:
- Urodynamic examination. With the help of it, the work of the upper and lower urinary tract is evaluated.
- Clinical examination. It includes a routine urine test and urine culture for flora, as well as a study in a gynecological chair - during an external examination, the doctor can assess the mobility of the bladder neck during a cough test or straining, assess the condition of the vaginal mucosa and skin, and also identify a possible genital prolapse.
- Ultrasound examination. It is carried out to study the functioning of the renal system, the urethrovesical segment, the condition of the urethra in a pregnant woman with stress urinary incontinence, as well as to confirm the presence or absence of pathologies of the genitals.
In addition to tests and examinations, you will most likely be asked to keep a special diary in which for several days you will record several parameters of urination, such as the amount of urine released per urination, the number of urination per day, all cases of urinary incontinence, the number of used during the day pads and physical activity.
Only after the examination, conclusions are drawn about the methods of treatment, which are often necessary only in extreme cases. If no pathology or inflammatory processes are detected, then most likely no special treatment will be carried out, since after childbirth, incontinence most often goes away on its own or occurs less and less.
If incontinence is due to weakening of the pelvic floor muscles, then the situation can be significantly improved with the help of special exercises. Currently, there are a large number of complexes for intimate gymnastics. One of the most popular was developed by the American gynecologist and MD Arnold Kegel. The simplest and, perhaps, the most effective exercise that can be done several times a day is the repeated tension and relaxation of the "intimate muscles" (slow or intense, without delay).
It is important to know that if you have never strengthened intimate muscles before pregnancy, you need to do this with caution, in no case overdo it.
It is possible that the doctor will prescribe you some herbal preparation that supports the functioning of the bladder and has an antispasmodic, anti-inflammatory and antimicrobial effect.
Treatment with decoctions of herbs (rose hips, sage, dill, lingonberries) may also be recommended. They have not only preventive, but also curative properties.
Pelvic (intimate) muscle training
To reduce the risk of urinary incontinence in a pregnant woman at night and during the day, doctors recommend doing special exercises. These are Kegel exercises that are useful not only for expectant mothers, but for all women, without exception, regardless of age. The bottom line is to alternate tension and relaxation of intimate muscles. It is not difficult to determine the zone for training - during urination, you need to interrupt the process for a couple of minutes. At this moment, those muscles that are involved in gymnastics will just tighten. You need to do exercises before childbirth, during pregnancy and after the baby is born. A simple and understandable set of exercises will reduce the risk of any problems with the urinary system. You can read more about gymnastics in another article.
How to ensure your comfort and peace of mind
So that urinary incontinence in pregnant women in the early, and especially in the later stages (38-39 weeks), does not cause increased discomfort, manufacturers of hygiene products produce special pads. One of the options is German MoliMed urological pads. They are specifically designed to provide comfort during involuntary urination. Features of these pads:
- anatomically shaped to prevent urine from leaking out;
- absorbent layer that instantly absorbs liquids and odors;
- secure fit on underwear;
- small thickness so that the pad is not visible under clothing;
- safe even for sensitive skin;
- the ability to choose a product based on the amount of discharge.
If you need help choosing the right hygiene products, the PAUL HARTMANN Sp. z o.o. hotline will advise you.
How else can you help yourself
Go to the toilet as often as possible during the day. At the same time, you should not reduce your fluid intake. The expectant mother should drink as much as she wants. But you need to try not to drink large amounts of liquid an hour before bedtime.
Many women use disposable pads to avoid trouble. This should be done only when absolutely necessary, since the frequent use of sanitary pads can provoke colpitis, which, in turn, can lead to infection of the membranes, and as a result, a miscarriage or premature birth due to rupture of the membranes.
You can somewhat alleviate the condition with the help of a prenatal bandage. Its regular correct wearing allows you to somewhat ease the load on the bladder, respectively, reduce the number of urges to urinate.
MoliCare Articles
General Articles
Patient Care. Algorithm
Illnesses and disability lead to restriction in movement - a person is often bedridden. Prolonged bed rest can cause problems with the skin and lead to complications in the form of bedsores. This article describes in detail the algorithms for daily hygiene care.
Learn more
General articles
Absorbents and quality of life
Incontinence absorbents - the solution to hygiene problems. They allow people to remain socially active without fear of being embarrassed.
Learn more
General articles
Neurological aspects of urinary incontinence in the elderly
Urinary incontinence in the elderly is a serious medical and social problem. This is due to an increase in the number of elderly patients who suffer from diabetes mellitus (DM), Parkinson's disease, dementia (Alzheimer's disease, etc.), have suffered a stroke or have other diseases leading to urinary incontinence.
Learn more
Pressure ulcer risk assessment. Norton scale
The most important thing in the prevention of pressure ulcers is to identify the risk of developing this complication. For this purpose, many rating scales have been proposed.
Learn more
Curly Fiber technology in MoliCare® and MoliMed® incontinence hygiene products keeps skin comfortable and healthy
Learn more
How do I know when it's time to change MoliCare®?
To feel confident in everyday life, it is important to know when to change your incontinence medication.
Learn more
Absorbent hygiene products improve the quality of life for people with incontinence
Absorbent products successfully solve hygiene problems in urinary incontinence. Their use allows patients to remain socially active without fear of embarrassing situations.
Learn more
Intimacy and sexuality with urinary incontinence
Many incontinent people have great difficulty with sexuality and intimacy. Existing relationships deteriorate because of illness, and new ones end before they even start because of shame and fear. It shouldn't be like this, because urinary incontinence does not cancel a full-fledged sex life at all.
Learn more
MoliCare® Skin Care - Medical Incontinence Skin Care
MoliCare® Skin with Nutriskin Protection Complex offers three product lines close to the physiological pH of the skin to cleanse, protect and care for the skin patients experiencing constant stress due to the negative effects of urine breakdown products.
Learn more
Coping with mood swings in incontinent patients: advice for families
Incontinent people who need care often suffer from mood swings. Relatives who care for them must learn to understand and recognize such moments in order to help patients cope with difficulties. There is no insurance against this disease, so it is worth considering preventive measures. What? About a healthy lifestyle, sports and sex
Learn more
Overweight and urinary incontinence
Obesity puts extra stress on the body, causes and exacerbates various diseases. At the same time, it is known that losing extra pounds has a positive effect on health in general and on urinary incontinence in particular
Find out more
Caring for people with urinary incontinence or combined urinary and fecal incontinence during the coronavirus pandemic: what you need to know
The new coronavirus infection has made changes to the challenges facing healthcare. As you certainly know, especially many problems arise when caring for the sick. We've compiled the most important information for you on how to provide safe incontinence care during the coronavirus pandemic.
Learn more
7 life hacks. How to avoid burnout when caring for a sick relative?
Caring for a seriously ill person leads to consequences that, over time, affect health, relationships with other people and psychological state.
Learn more
Prevention of bedsores
One of the most serious problems in the care of bedridden patients is the risk of pressure ulcers, which aggravate the underlying disease and worsen the quality of life of patients, complicate care.
Find out more
How to beat incontinence
Incontinence is not life-threatening, but it significantly affects its quality. Most often, patients try to hide their condition, while modern medicine is ready to offer various methods of dealing with this problem.
Learn more
Men's urinary incontinence
Learn more
6 embarrassing questions about urinary incontinence in men
There is a misconception that urinary incontinence is a purely female problem. It's just that most men prefer to remain silent about it. What are the causes of incontinence in men and what to do about it?
Learn more than
On the problem of
Learn more than
Why is
Learn more than
Types of urinary incontinence
Learn more than
Learn more than
Treatment of urine
Learn more than
Expert opinion
Learn more
Urological pads for women: how to choose and where to buy?
Learn more
Kegel Exercises
Learn More
Strengthen Your Pelvic Floor Muscles
Learn More
MoliMed® Urological Pads vs Sanitary Pads: Find 6 Differences
Learn More
How to choose urological pads for women?
Learn more
Kegel exercises for men
Learn more
Why women get incontinent after childbirth and how to behave
Learn more
All about urinary incontinence in women
Learn more
What causes urinary incontinence in pregnant women
Learn more
What can cause regular bedwetting in women?
Find out more
What can cause regular urinary incontinence in women when coughing?
Learn more
What causes urinary incontinence in older women?
Learn more
All about urinary incontinence after prostate removal
Learn more
Main causes of bedwetting in men
Learn more
Kegel exercises for women and men with urinary incontinence
Learn more
What you need to know about stress urinary incontinence?
Learn more
Kegel exercises for uterine prolapse
Learn more
What is the most common cause of incontinence in women with cystitis?
Learn more
Kegel exercises for men during urine incontinence: Rules, benefits and contraindications
Learn more than
Stress incontinence of urine
Learn more than
Urbery in the elderly
Find out more than
Kegel exercises for men after removing the prostate
Learn more
Women's pelvic floor muscles
Learn more
Sleep enuresis in men
Learn more
Kegel exercises for prostatitis
Learn more
Reorganization of space. Home care for a bedridden patient
Anyone who has cared for a seriously ill relative knows how important it is to properly organize the space around the bed and the apartment as a whole. Let's take a look at what needs to be changed in the home when it comes to a patient with limited mobility.
Learn more
Bedridden care: advice for relatives
Caring for seriously ill relatives is a complex physical and psychological job that requires compassion and constant concentration. Unfortunately, people who find themselves in a similar situation often lack knowledge on how to make life easier for a loved one and their own.
Learn more
7 hacks for incontinent people
Learn more
Sanitary pads and urological pads - what's the difference?
Often women with urinary incontinence use sanitary napkins, while there are special urological ones that suit their needs.
Learn more
Male incontinence? No problem!
Men rarely experience urinary incontinence at a young age. If this happens, the cause is inflammation of the prostate gland or congenital anomalies of the reflexes responsible for emptying the bladder. Over the years, the percentage of men suffering from incontinence is increasing. This most often does not threaten life, but can significantly affect its quality.
Learn more
Prevention and rehabilitation schools
Learn more
New standards of care for sedentary patients
Learn more
10 factors in the development of pressure ulcers
Learn more
Clinical and economic analysis of the effectiveness of using MoliCare® Premium extra soft diapers for the prevention of dermatitis and pressure ulcers Learn more
General articles
Stroke care
Only 20% of stroke survivors return to work, and one third of all stroke survivors are of working age. Relatives of stroke patients often have a low level of knowledge about the care of seriously ill patients, so it is advisable to train them by medical professionals in special health schools.