If i have a cleft palate will my baby
Cleft lip and palate - NHS
A cleft is a gap or split in the upper lip and/or roof of the mouth (palate). It is present from birth.
The gap is there because parts of the baby's face did not join together properly during development in the womb.
A cleft lip and palate is the most common facial birth defect in the UK, affecting around 1 in every 700 babies.
What does a cleft lip and palate look like?
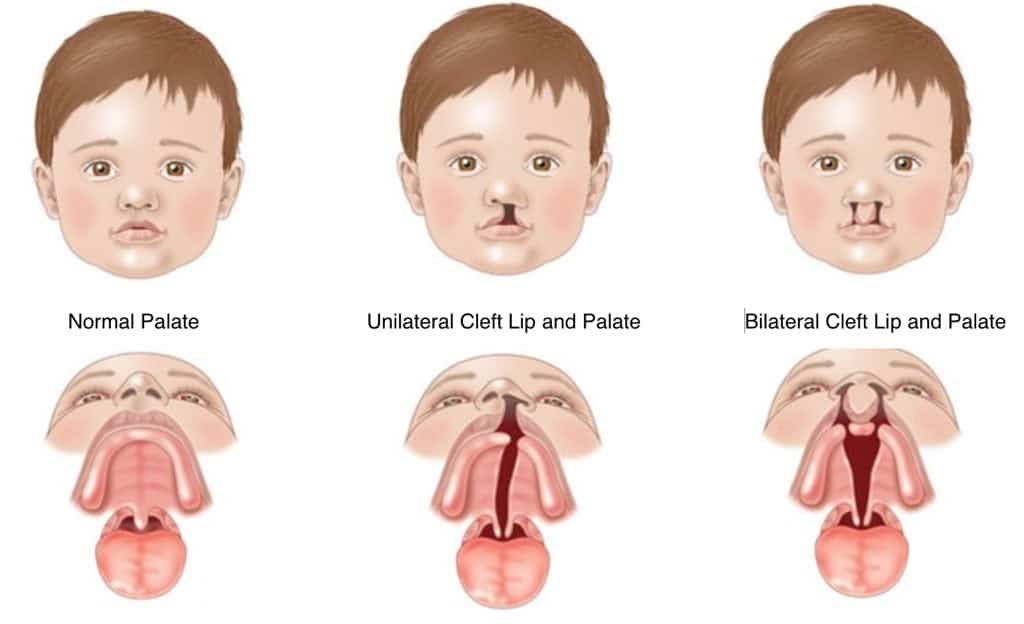
Babies can be born with a cleft lip, a cleft palate, or both.
A cleft lip may just affect one side of the lip or there may be 2 clefts.
Credit:
DR M.A. ANSARY/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/266603/view
It can range from a small notch to a wide gap that reaches the nose.
A cleft palate may just be an opening at the back of the mouth, or it may be a split in the palate that runs all the way to the front of the mouth.
Credit:
MORRIS HUBERLAND/SCIENCE PHOTO LIBRARY https://www.sciencephoto.com/media/95507/view
Sometimes it can be hidden by the lining of the roof of the mouth.
The Cleft Lip and Palate Association has a photo gallery with pictures of cleft lips and palates before and after surgery.
Problems related to cleft lip and palate
A cleft lip and cleft palate can cause a number of issues, particularly in the first few months after birth, before surgery is done.
Problems can include:
- difficulty feeding – a baby with a cleft lip and palate may be unable to breastfeed or feed from a normal bottle because they cannot form a good seal with their mouth
- hearing problems – some babies with a cleft palate are more vulnerable to ear infections and a build-up of fluid in their ears (glue ear), which may affect their hearing
- dental problems – a cleft lip and palate can mean a child's teeth do not develop correctly and they may be at a higher risk of tooth decay
- speech problems – if a cleft palate is not repaired, it can lead to speech problems such as unclear or nasal-sounding speech when a child is older
Most of these problems will improve after surgery and with treatments such as speech and language therapy.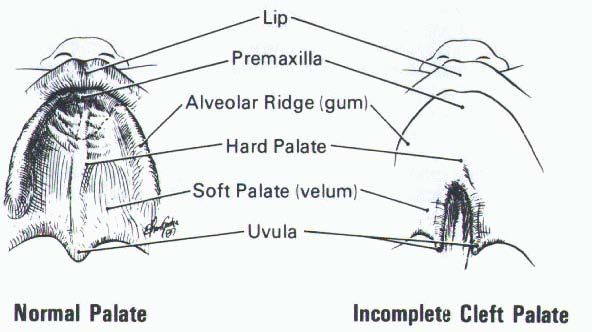
Causes of cleft lip and palate
A cleft lip or palate happens when the structures that form the upper lip or palate fail to join together when a baby is developing in the womb.
The exact reason why this happens to some babies is often unclear. It's very unlikely to have been caused by anything you did or did not do during pregnancy.
In a few cases, cleft lip and palate is associated with:
- the genes a child inherits from their parents (although most cases are a one-off)
- smoking during pregnancy or drinking alcohol during pregnancy
- obesity during pregnancy
- a lack of folic acid during pregnancy
- taking certain medicines in early pregnancy, such as some anti-seizure medications and steroid tablets
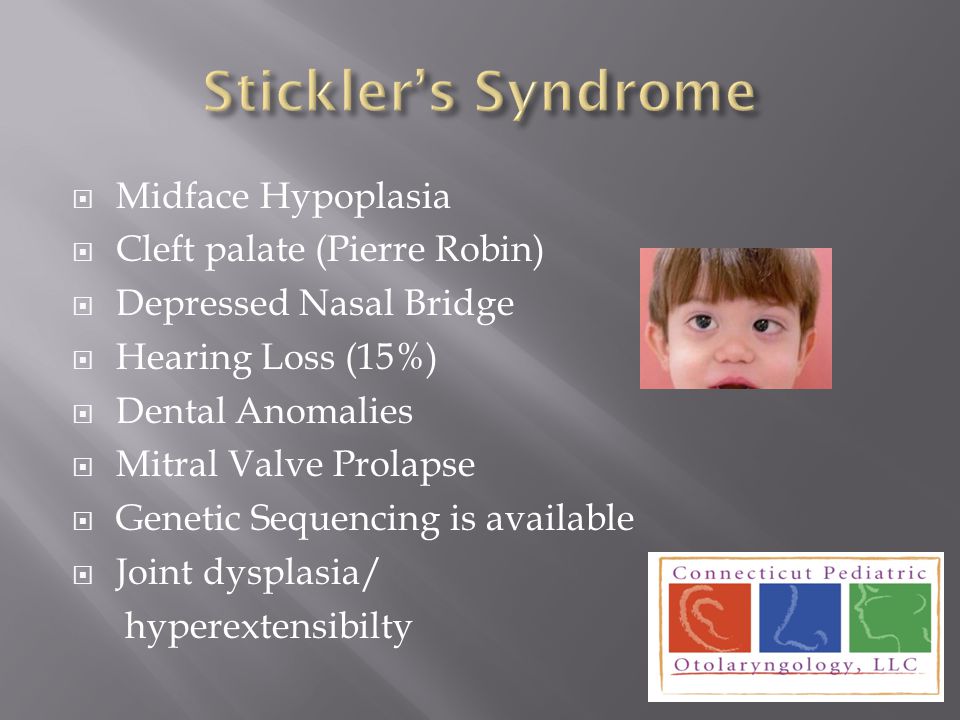
In some cases, a cleft lip or palate can occur as part of a condition that causes a wider range of birth defects, such as 22q11 deletion syndrome (sometimes called DiGeorge or velocardiofacial syndrome) and Pierre Robin sequence.
Diagnosing cleft lip and palate
A cleft lip is usually picked up during the mid-pregnancy anomaly scan done when you're between 18 and 21 weeks pregnant. Not all cleft lips will be obvious on this scan and it's very difficult to detect a cleft palate on an ultrasound scan.
If a cleft lip or palate does not show up on the scan, it's usually diagnosed immediately after birth or during the newborn physical examination done within 72 hours of birth.
When a cleft lip or palate is diagnosed, you'll be referred to a specialist NHS cleft team who will explain your child's condition, discuss the treatments they need and answer any questions you have.
You may also find it useful to contact a support group, such as the Cleft Lip and Palate Association, who can offer advice and put you in touch with parents in a similar situation.
Treatments for cleft lip and palate
Cleft lip and cleft palate are treated at specialist NHS cleft centres.
Your child will usually have a long-term care plan that outlines the treatments and assessments they'll need as they grow up.
The main treatments are:
- surgery – an operation to correct a cleft lip is usually done when your baby is 3 to 6 months and an operation to repair a cleft palate is usually done at 6 to 12 months
- feeding support – you may need advice about positioning your baby on your breast to help them feed, or you might need to feed them using a special type of bottle
- monitoring hearing – a baby born with cleft palate has a higher chance of glue ear, which may affect hearing. Close monitoring of their hearing is important and if glue ear affects their hearing significantly, a hearing aid may be fitted or small tubes called grommets may be placed in their ears to drain the fluid
- speech and language therapy – a speech and language therapist will monitor your child's speech and language development throughout their childhood and help with any speech and language problems
- good dental hygiene and orthodontic treatment – you'll be given advice about looking after your child's teeth, and they may need braces if their adult teeth don't come through properly
Read more about how cleft lip and palate is treated.
Outlook for cleft lip and palate
The majority of children treated for cleft lip or palate grow up to have completely normal lives.
Most affected children will not have any other serious medical problems and treatment can usually improve the appearance of the face and problems with feeding and speech.
Surgery to repair a cleft lip may leave a small pink scar above the lips. This will fade over time and become less noticeable as your child gets older.
Credit:
Maos / Thinkstock https://www.istockphoto.com/gb/photo/baby-with-cleft-before-and-after-surgery-gm520421636-90969427
Some adults who've had a cleft lip or palate repair may be self-conscious or unhappy about their appearance. Your GP may refer you back to an NHS cleft centre for further treatment and support if there are any ongoing issues.
Will a cleft lip and palate happen again?
Most cases of cleft lip or palate are a one-off and it's unlikely you'll have another child with the condition.
The risk of having a child with a cleft lip or palate is slightly increased if you've had a child with the condition before, but the chances of this happening are thought to be around 2 to 8%.
If either you or your partner were born with a cleft lip or palate, your chance of having a baby with a cleft is also around 2 to 8%.
The chances of another child being born with a cleft or of a parent passing the condition to their child can be higher in cases related to a genetic condition.
For example, a parent with 22q11 deletion syndrome (DiGeorge syndrome) has a 1 in 2 chance of passing the condition to their child.
Information about your child
If your child has a cleft lip or palate, your cleft team will pass information about them to the National Congenital Anomaly and Rare Diseases Registration Service (NCARDRS).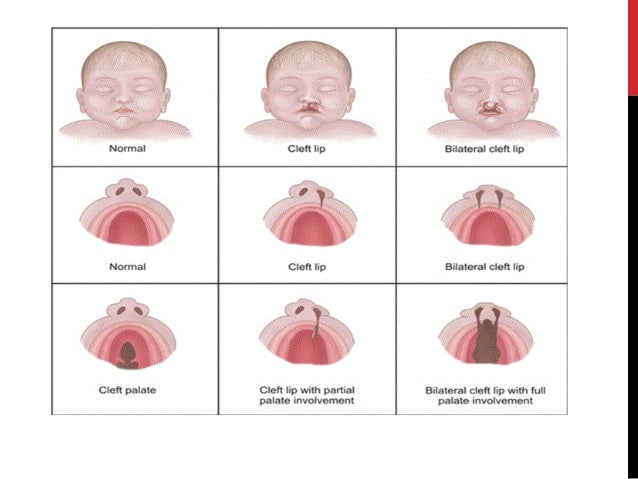
This helps scientists look for better ways to prevent and treat this condition. You can opt out of the register at any time.
Find out more about the register.
Page last reviewed: 13 August 2019
Next review due: 13 August 2022
Facts about Cleft Lip and Cleft Palate
Cleft lip and cleft palate are birth defects that occur when a baby’s lip or mouth do not form properly during pregnancy. Together, these birth defects commonly are called “orofacial clefts”.
Click here to view a larger image
Click here to view a larger image
What is Cleft Lip?
The lip forms between the fourth and seventh weeks of pregnancy. As a baby develops during pregnancy, body tissue and special cells from each side of the head grow toward the center of the face and join together to make the face. This joining of tissue forms the facial features, like the lips and mouth.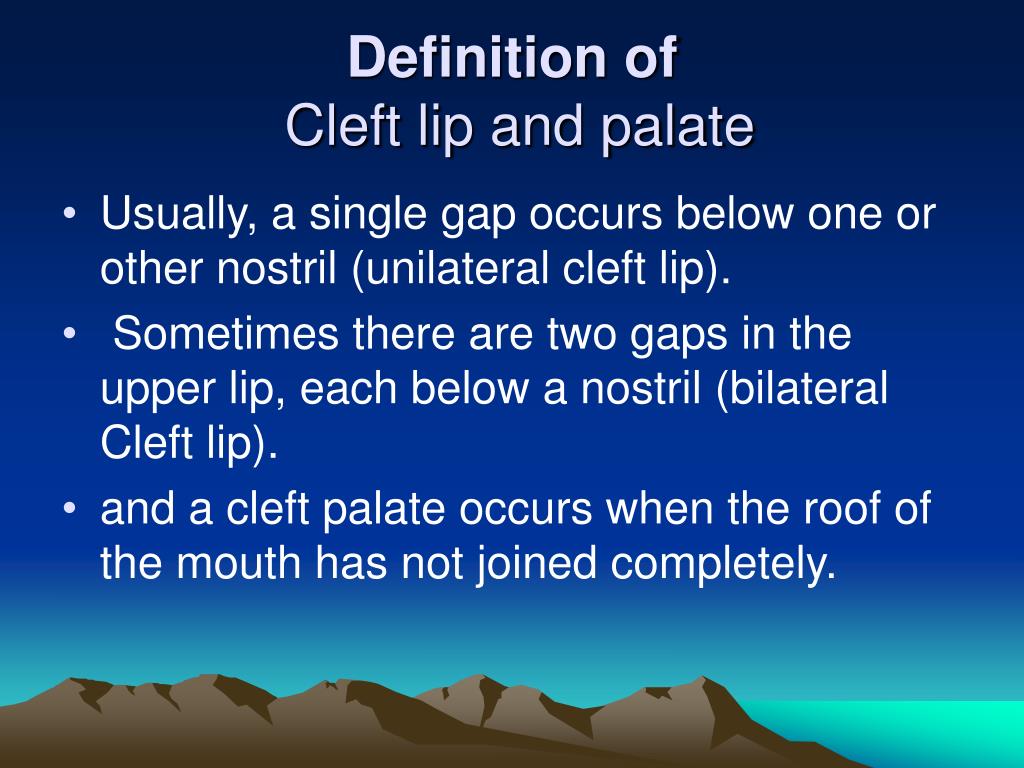 A cleft lip happens if the tissue that makes up the lip does not join completely before birth. This results in an opening in the upper lip. The opening in the lip can be a small slit or it can be a large opening that goes through the lip into the nose. A cleft lip can be on one or both sides of the lip or in the middle of the lip, which occurs very rarely. Children with a cleft lip also can have a cleft palate.
A cleft lip happens if the tissue that makes up the lip does not join completely before birth. This results in an opening in the upper lip. The opening in the lip can be a small slit or it can be a large opening that goes through the lip into the nose. A cleft lip can be on one or both sides of the lip or in the middle of the lip, which occurs very rarely. Children with a cleft lip also can have a cleft palate.
What is Cleft Palate?
The roof of the mouth (palate) is formed between the sixth and ninth weeks of pregnancy. A cleft palate happens if the tissue that makes up the roof of the mouth does not join together completely during pregnancy. For some babies, both the front and back parts of the palate are open. For other babies, only part of the palate is open.
Other Problems
Children with a cleft lip with or without a cleft palate or a cleft palate alone often have problems with feeding and speaking clearly and can have ear infections. They also might have hearing problems and problems with their teeth.
How Many Babies are Born with Cleft Lip/Cleft Palate?
- About 1 in every 1,600 babies is born with cleft lip with cleft palate in the United States.
- About 1 in every 2,800 babies is born with cleft lip without cleft palate in the United States.
- About 1 in every 1,700 babies is born with cleft palate in the United States.1
Causes and Risk Factors
The causes of orofacial clefts among most infants are unknown. Some children have a cleft lip or cleft palate because of changes in their genes. Cleft lip and cleft palate are thought to be caused by a combination of genes and other factors, such as things the mother comes in contact with in her environment, or what the mother eats or drinks, or certain medications she uses during pregnancy.
Like the many families of children with birth defects, CDC wants to find out what causes them. Understanding the factors that are more common among babies with a birth defect will help us learn more about the causes. CDC funds the Centers for Birth Defects Research and Prevention, which collaborate on large studies such as the National Birth Defects Prevention Study (NBDPS; births 1997-2011) and the Birth Defects Study To Evaluate Pregnancy exposureS (BD-STEPS; began with births in 2014), to understand the causes of and risks for birth defects, including orofacial clefts.
CDC funds the Centers for Birth Defects Research and Prevention, which collaborate on large studies such as the National Birth Defects Prevention Study (NBDPS; births 1997-2011) and the Birth Defects Study To Evaluate Pregnancy exposureS (BD-STEPS; began with births in 2014), to understand the causes of and risks for birth defects, including orofacial clefts.
Recently, CDC reported on important findings from research studies about some factors that increase the chance of having a baby with an orofacial cleft:
- Smoking―Women who smoke during pregnancy are more likely to have a baby with an orofacial cleft than women who do not smoke.2-3
- Diabetes―Women with diabetes diagnosed before pregnancy have an increased risk of having a child with a cleft lip with or without cleft palate, compared to women who did not have diabetes.5
- Use of certain medicines―Women who used certain medicines to treat epilepsy, such as topiramate or valproic acid, during the first trimester (the first 3 months) of pregnancy have an increased risk of having a baby with cleft lip with or without cleft palate, compared to women who didn’t take these medicines.
 6-7
6-7
CDC continues to study birth defects, such as cleft lip and cleft palate, and how to prevent them. If you are pregnant or thinking about becoming pregnant, talk with your doctor about ways to increase your chances of having a healthy baby.
Diagnosis
Orofacial clefts, especially cleft lip with or without cleft palate, can be diagnosed during pregnancy by a routine ultrasound. They can also be diagnosed after the baby is born, especially cleft palate. However, sometimes certain types of cleft palate (for example, submucous cleft palate and bifid uvula) might not be diagnosed until later in life.
Management and Treatment
Services and treatment for children with orofacial clefts can vary depending on the severity of the cleft; the child’s age and needs; and the presence of associated syndromes or other birth defects, or both.
Surgery to repair a cleft lip usually occurs in the first few months of life and is recommended within the first 12 months of life.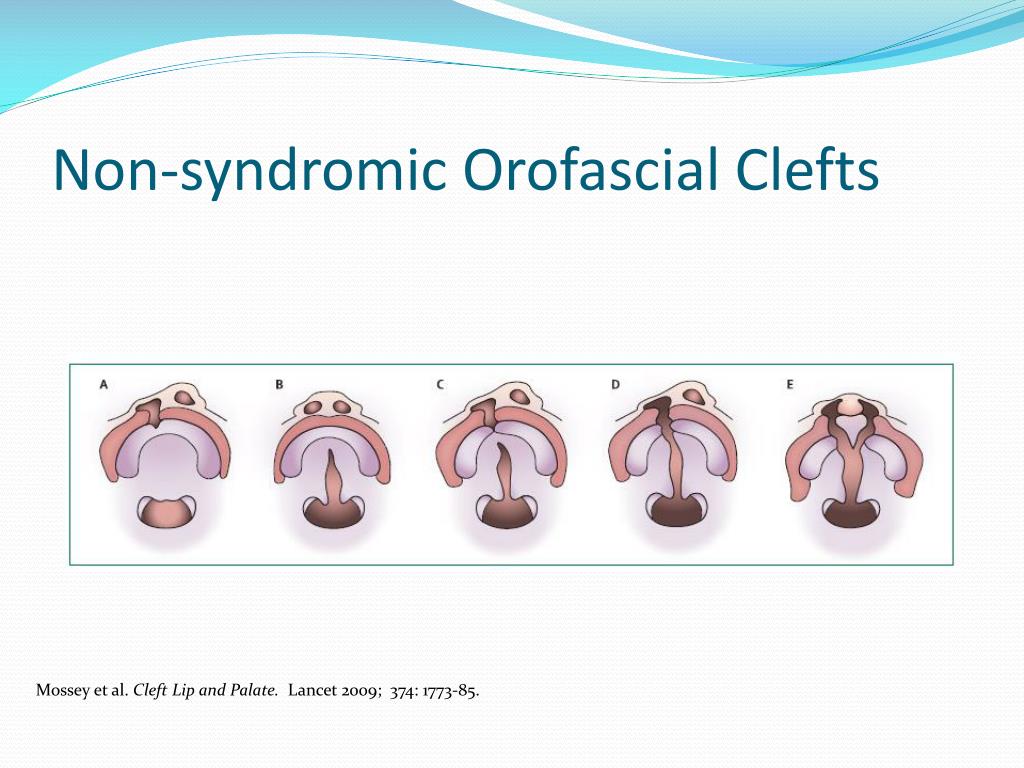 Surgery to repair a cleft palate is recommended within the first 18 months of life or earlier if possible.8 Many children will need additional surgical procedures as they get older. Surgical repair can improve the look and appearance of a child’s face and might also improve breathing, hearing, and speech and language development. Children born with orofacial clefts might need other types of treatments and services, such as special dental or orthodontic care or speech therapy.4,8
Surgery to repair a cleft palate is recommended within the first 18 months of life or earlier if possible.8 Many children will need additional surgical procedures as they get older. Surgical repair can improve the look and appearance of a child’s face and might also improve breathing, hearing, and speech and language development. Children born with orofacial clefts might need other types of treatments and services, such as special dental or orthodontic care or speech therapy.4,8
With treatment, most children with orofacial clefts do well and lead a healthy life. Some children with orofacial clefts may have issues with self-esteem if they are concerned with visible differences between themselves and other children. Parent-to-parent support groups can prove to be useful for families of babies with birth defects of the head and face, such as orofacial clefts.
References
- Mai CT, Isenburg JL, Canfield MA, Meyer RE, Correa A, Alverson CJ, Lupo PJ, Riehle‐Colarusso T, Cho SJ, Aggarwal D, Kirby RS.
 National population‐based estimates for major birth defects, 2010–2014. Birth Defects Research. 2019; 111(18): 1420-1435.
National population‐based estimates for major birth defects, 2010–2014. Birth Defects Research. 2019; 111(18): 1420-1435. - Little J, Cardy A, Munger RG. Tobacco smoking and oral clefts: a meta-analysis. Bull World Health Organ. 2004;82:213-18.
- Honein MA, Rasmussen SA, Reefhuis J, Romitti P, Lammer EJ, Sun L, Correa A. Maternal smoking, environmental tobacco smoke, and the risk of oral clefts. Epidemiology 2007;18:226–33.
- Yazdy MM, Autry AR, Honein MA, Frias JL. Use of special education services by children with orofacial clefts. Birth Defects Research (Part A): Clinical and Molecular Teratology 2008;82:147-54.
- Correa A, Gilboa SM, Besser LM, Botto LD, Moore CA, Hobbs CA, Cleves MA, Riehle-Colarusso TJ, Waller DK, Reece EA. Diabetes mellitus and birth defects. American Journal of Obstetrics and Gynecology 2008;199:237.e1-9.
- Margulis AV, Mitchell AA, Gilboa SM, Werler MM, Glynn RJ, Hernandez-Diaz S, National Birth Defects Prevention Study.
 Use of topiramate in pregnancy and risk of oral clefts. American Journal of Obstetrics and Gynecology 2012;207:405.e1-e7.
Use of topiramate in pregnancy and risk of oral clefts. American Journal of Obstetrics and Gynecology 2012;207:405.e1-e7. - Werler MM, Ahrens KA, Bosco JL, Michell AA, Anderka MT, Gilboa SM, Holmes LB, National Birth Defects Prevention Study. Use of antiepileptic medications in pregnancy in relation to risks of birth defects. Annals of Epidemiology 2011;21:842-50.
- American Cleft Palate-Craniofacial Association. Parameters for evaluation and treatment of patients with cleft lip/palate or other craniofacial anomalies. Revised edition, Nov 2009. Chapel Hill, NC. P. 1-34. https://acpa-cpf.org/wp-content/uploads/2017/06/Parameters_Rev_2009_9_.pdf
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.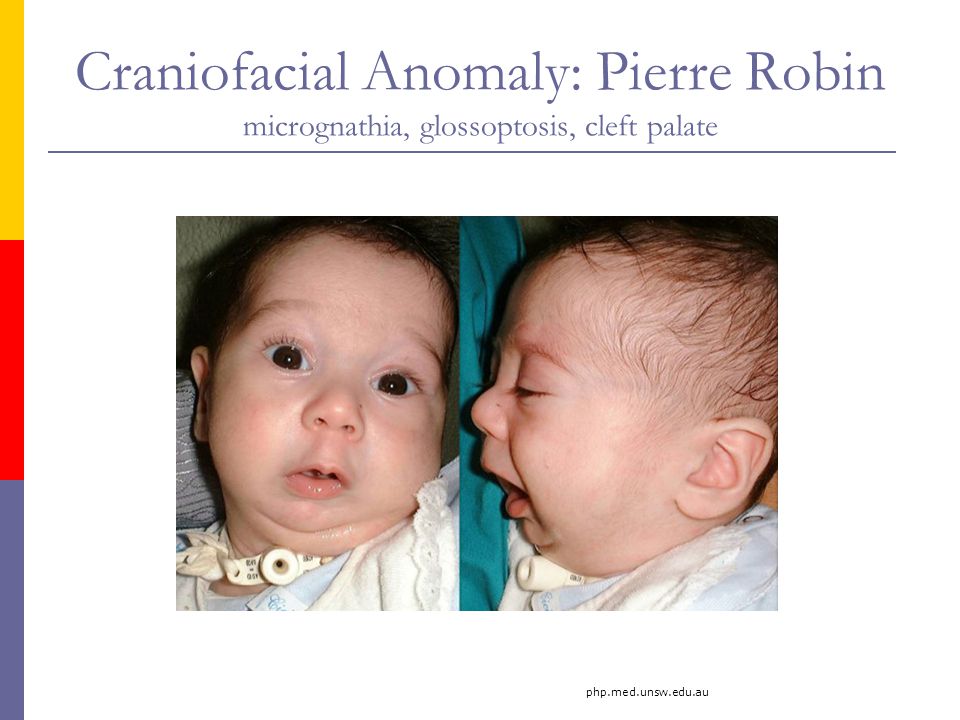
The images are in the public domain and thus free of any copyright restrictions. As a matter of courtesy we request that the content provider (Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities) be credited and notified in any public or private usage of this image.
The cleft palate in a child: photos, causes, symptoms, treatment
The cleft palate develops in the womb in the early stages of development. At the same time, the baby has a cleft in the sky, which is why there is a direct communication between the mouth and nose. In medicine, such a defect is called cheiloschisis.
Often the cleft palate occurs simultaneously with another defect - the cleft lip. The cause and mechanism of their occurrence is the same. A cleft of the bony structures of the palate can lead to splitting of soft tissues, including the lips and nose. If this happens, then the child has both pathologies - the cleft palate and the cleft lip.
While the cleft lip may be more of a cosmetic defect and interfere with speech, the cleft palate is much more serious. A cleft palate may go unnoticed if the soft tissues are not affected. Parents pay attention to the problem when the baby cannot suck normally, chokes, milk comes out of the nose. In maternity hospitals, babies are examined to exclude this ailment, but in the case of a home birth, it can be skipped.
The cleft palate is one of the ten most common congenital pathologies in children. Girls are more likely to have cleft palate without affecting the lip, and boys are more likely to have cleft lip without palate pathology.
What is the cleft palate
Initially, in the womb, the fetus does not have fused bones of the skull in the form in which it is customary to see in the end. This is part of development. By the 11th week of pregnancy, all the necessary parts of the bones of the skull and face of the embryo are normally fused. If in the early stages the fetus was adversely affected, some crevices do not overgrow, in this case the sky.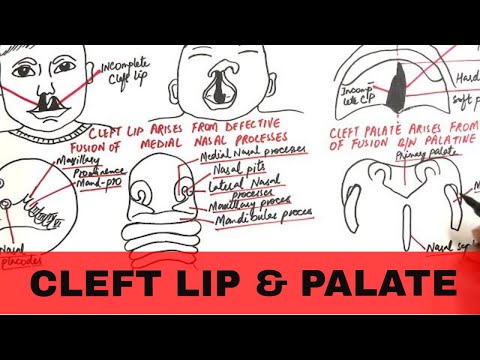
Such children cannot eat properly - the sucking process is disturbed, food enters the nasal cavity, causing inflammation. In the future, speech is also impaired, the pronunciation of sounds is difficult, the children “gundos”. Intellectually and emotionally, children with a cleft palate are absolutely normal, the problem is purely anatomical.
A cleft palate may not be the only defect. Sometimes it occurs as part of various syndromes.
Causes of the cleft palate in a child
According to scientists, only 10-15% of the defect is genetically determined. That is, even if one of the relatives had a wolf's mouth, the probability of the appearance of the same in a child increases by only 7%.
The main causes of pathology - the influence of external factors in the early stages of pregnancy. Often during this period, a woman does not know that she is carrying a child, and continues to take drugs prohibited during pregnancy, smoke or drink alcohol. This adversely affects the development of the fetus, the process of bone fusion is disrupted.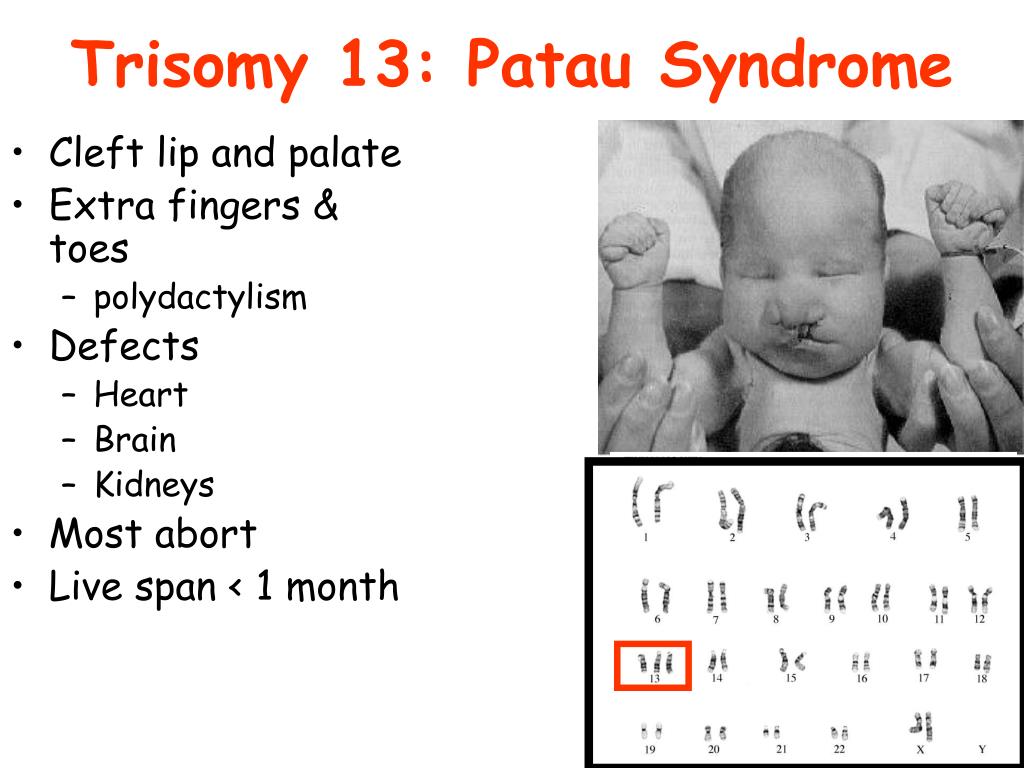
At the beginning of pregnancy, many women have reduced immunity, and infections picked up at this point are dangerous to the fetus.
Abdominal injuries, radiation, vitamin deficiency, early abortions, tumors and obesity are no less dangerous. Even the age of the mother and her mental state can affect the likelihood of having a child with a cleft palate.
Photo: pixabay.comSymptoms of the cleft palate in a child
The larger the cleft in the palate, the more noticeable the presence of pathology. With an incomplete cleft, the child chokes when sucking, eats poorly, milk can flow from the nose. If the cleft is through, complete, the baby has difficulty breathing, in principle he cannot suckle. Often, during natural childbirth, amniotic fluid enters the respiratory tract of such children, so they need emergency help.
Examination of the oral cavity and pharynx shows a hole in the place where the entire soft palate is normally located. If the splitting also affected the lip, then the division of the upper lip into two or more halves is outwardly noticeable.
Treatment of the cleft palate in a child
The cleft palate is dangerous with serious complications, so it must be treated. Unfortunately, the only solution to the problem is surgery. Treatment consists of several stages, and the first operation can be performed up to a year.
Many children with cleft palate wear an obturator before surgery, a prosthesis that closes the opening between the nasal and oral cavities. This helps the baby breathe normally, facilitates the process of nutrition and the formation of speech.
Even before surgery, the child is taught to feed with a special spoon, since sucking is difficult without additional devices. The skill of such a special diet will also come in handy after the operation, since the wound is quite painful and nutrition is impossible. In addition, there is a risk of large scars, and the healing itself will slow down.
After a series of operations, you need to carefully care for the oral cavity, treat wounds with antiseptics, and take antibiotics.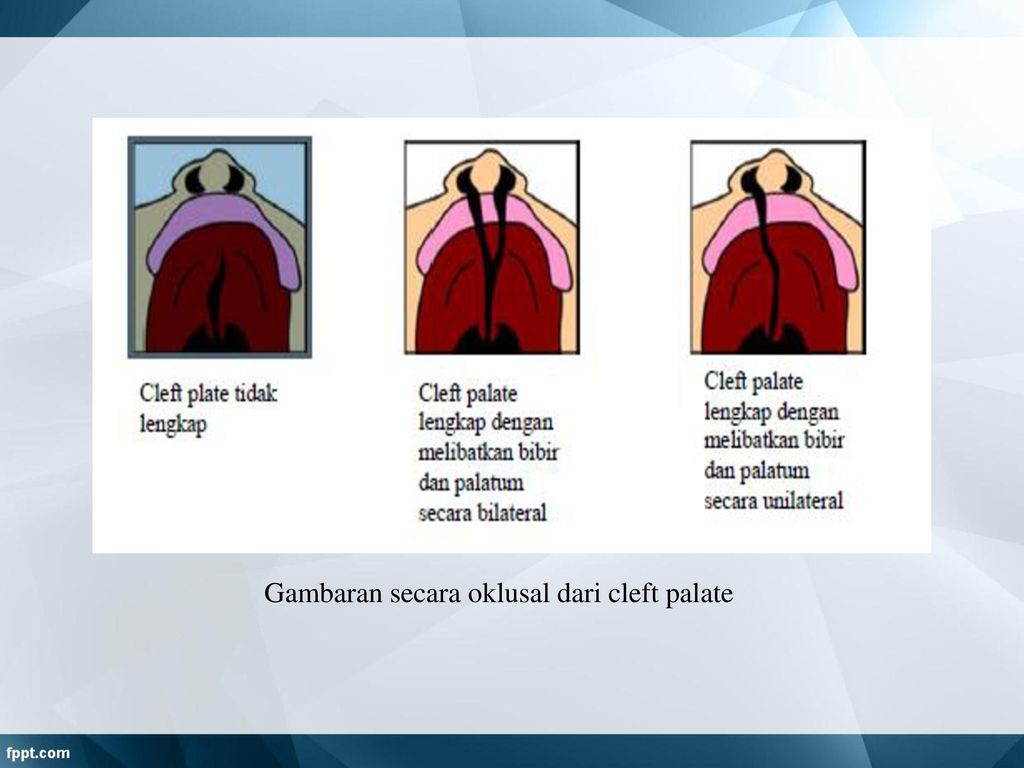 A special massage of the soft palate is also used, which improves blood circulation and dissolves scars. During the recovery period, you will need the help of a speech therapist, defectologist to establish normal speech. And the orthodontist will control the correct growth of teeth and jaw development. If something goes wrong, they will write out corrective plates, staples.
A special massage of the soft palate is also used, which improves blood circulation and dissolves scars. During the recovery period, you will need the help of a speech therapist, defectologist to establish normal speech. And the orthodontist will control the correct growth of teeth and jaw development. If something goes wrong, they will write out corrective plates, staples.
Treatment is complex and lengthy, but results in almost 95% of children with a cleft palate will forever forget about the problem.
Diagnosis
The defect is often assumed during pregnancy, during ultrasound. But it is possible to assess the degree of splitting of the sky only after the birth of the baby. During childbirth, there is a danger of amniotic fluid entering the respiratory tract through a cleft, so doctors should better know about the pathology in advance.
After the baby is born, the doctors examine it and the cleft can be seen with the naked eye. In addition, they check hearing, smell, take blood tests to rule out infections.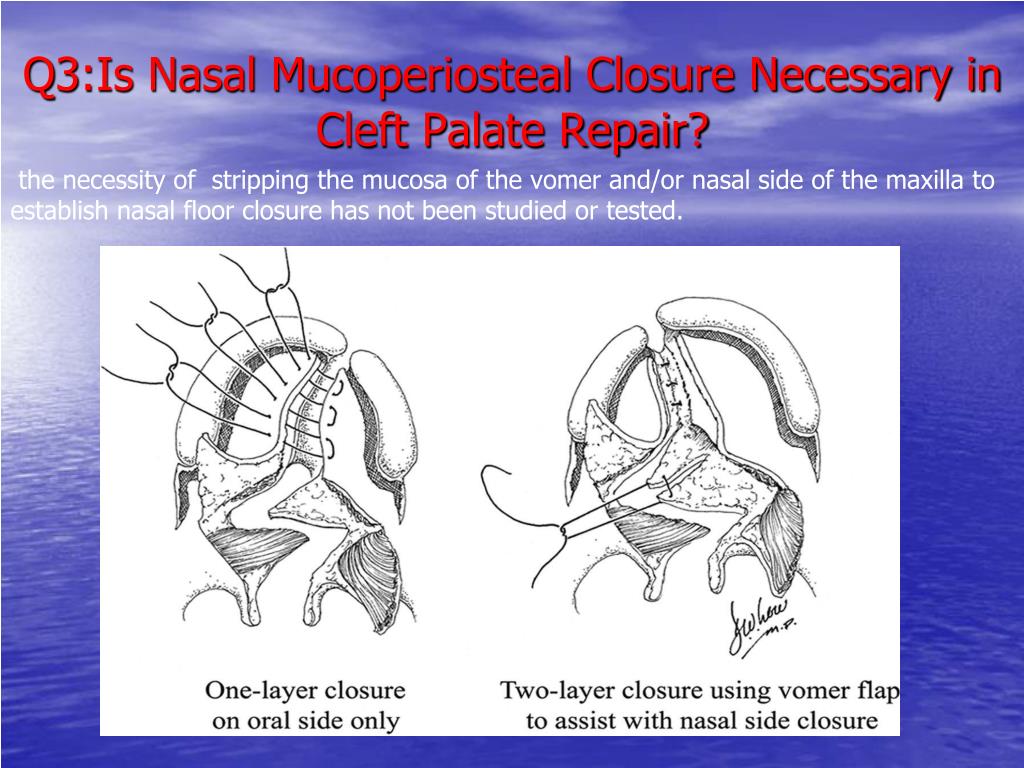
Modern methods of treatment
Before surgery, the baby is carefully examined and plans how exactly the problem will be solved. There are various methods, and they are selected individually for each little patient. During planning, they additionally consult a pediatrician, otolaryngologist, neurologist, maxillofacial surgeon, speech therapist, orthodontist.
Surgical repair of an incomplete cleft palate is called uranoplasty. It is carried out at about the age of 2 years. This technique will help if the shape of the jaw is not distorted, and the cleft is not too large. During the operation, the soft palate is lengthened for the baby, the muscles are connected. If there are not enough local tissues, additional ones are used from the cheeks and tongue.
If the jaw is narrowed and the teeth are misaligned, the child is first treated by an orthodontist. The operation will be much later, otherwise the development of the jaw may be impaired. Usually uranoplasty in this case is carried out at 4-6 years.
Prevention of the cleft palate in a child at home
It is advisable to plan a pregnancy. Then the woman will expect it and at the most important early stages she will avoid accidentally taking toxic medications, smoking, alcohol. This often happens if the woman is not yet aware of the pregnancy.
It is important to take vitamins prescribed by a gynecologist and have regular check-ups. Avoid crowds and dress warmly, because in the first weeks the mother's immunity is very vulnerable.
Popular Questions and Answers
Pediatrician - chief pediatrician - works on the solution of the problem of the cleft palate along with surgeons, orthodontists and other specialists. The pediatrician makes sure that the child eats normally, helps reduce the risk of infections, and gives advice on caring for the baby. Read more about the treatment of children with cleft palate will tell pediatrician Daria Schukina .
What are the complications of cleft palate?
Such a child cannot eat normally without throwing food into the nasal cavity, which provokes the development of chronic inflammation and infections of the ENT organs.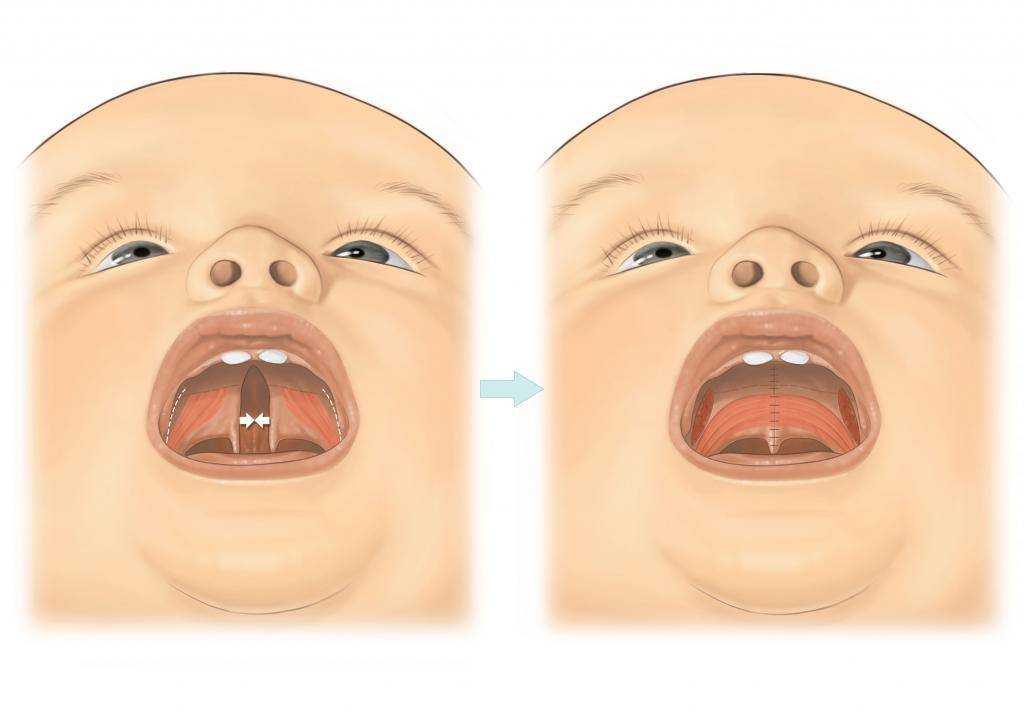 These defects lead to psychological trauma, speech development disorders. Children with cleft palate are more likely to get ARVI, may lag behind in growth and development. And they can also have combined malformations.
These defects lead to psychological trauma, speech development disorders. Children with cleft palate are more likely to get ARVI, may lag behind in growth and development. And they can also have combined malformations.
When to call a doctor at home for cleft palate?
Diagnosis and treatment of cleft palate is planned, a doctor's call to the house is not required. In case of respiratory failure in a child with a large cleft palate, signs of infection, high temperature, an ambulance is more likely to be needed. How early can a pathology be determined in a child? Can this be somehow influenced even in the womb? The first trimester of pregnancy is the most dangerous in terms of the development of defects. It is believed that a cleft lip and palate is formed as a result of a combination of hereditary traits and adverse environmental influences. The age of the mother over 35 is also a risk factor.
It is impossible to influence this when the fetus has already formed. Most often, pathology is detected already at the birth of a child. However, a pronounced defect can be seen on ultrasound. Fetoscopy and fetoamniotomy may also help. However, the diagnostic efficiency during pregnancy fluctuates around 30%.
However, a pronounced defect can be seen on ultrasound. Fetoscopy and fetoamniotomy may also help. However, the diagnostic efficiency during pregnancy fluctuates around 30%.
At what age should the operation be done so that it is not too late?
Severe malformations with cleft palate are corrected as early as possible in 2 stages by maxillofacial surgeons, the first of which falls on 8-14 months. However, with cleft palate, the growth of the child is taken into account, and the fact that plastic surgery can be temporary until the child outgrows it, and the bones stop growing for a permanent implant.
Cleft palate: Causes, Complications, Causes | doc.ua
Forms
The splitting of the palate may be complete or incomplete. With complete splitting of the palate, a cleft is formed in the soft and hard palate. Incomplete - only a hole is formed in the sky.
Often the defect is accompanied by a bifurcation of a process on the back of the upper palate - the so-called uvula.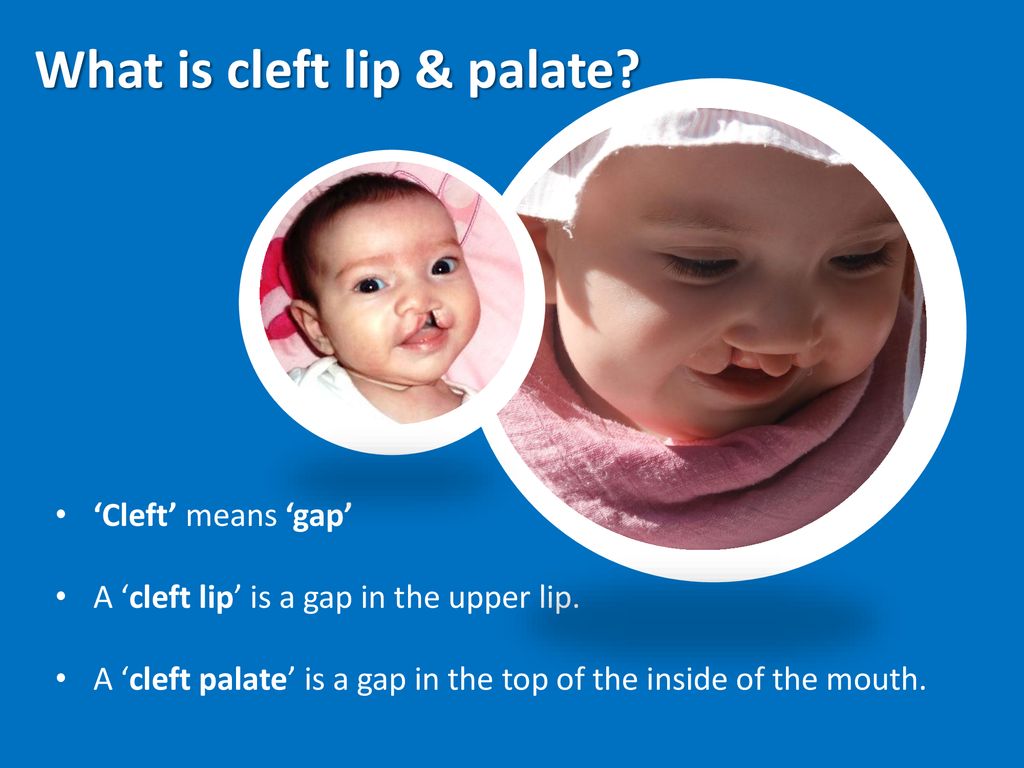 This is due to improper development of the connection of the nasal septum and the lateral, medial palatine processes.
This is due to improper development of the connection of the nasal septum and the lateral, medial palatine processes.
Causes
The cause of the cleft palate is called the genetic component. British scientists in 1991 discovered the TBX22 gene responsible for the development of the cleft palate - it is located on the X chromosome. The risk factor is teratogenic effects on the fetus. To date, the relationship between the development of such defects as cleft lip, cleft palate and the future mother's use of alcohol, drugs, and smoking has already been identified. The risk increases with a woman's obesity and lack of folic acid in her diet.
The bad ecology in the region where the pregnant woman lives, the toxicosis, mental and mechanical traumas, as well as acute infections she suffered while carrying a child, also plays a negative role. The first three months of pregnancy are especially dangerous - it is then that the maxillofacial apparatus is formed.
Non-occlusion of the palate occurs as an independent defect, and in combination with any maxillofacial pathology.
Complications
The problems associated with having a cleft palate start from the first moments of life. During childbirth, aspiration is likely - the ingress of amniotic fluid into the respiratory tract of the child.
Children with this defect are extremely sick. This is explained by the fact that the air that they inhale is not moistened or warmed, and the ingress of cold and dry air into the respiratory tract causes the development of inflammatory processes not only of the respiratory organs, but also of the inner ear.
Such a child is retarded because his breathing is difficult and sucking naturally is impossible. For feeding, a special tool is used - a spoon that is put on a bottle.
In addition to the upper respiratory tract, the digestive organs suffer, and there are serious hearing problems. Children with cleft palate have problems with speech: it is changed due to the incorrect process of forming sounds. Such speech is characterized by an open rhinolalia. Quite often there are otitis media and sinusitis. Inflammation occurs due to the fact that the consumed liquid and food through the cleft enters the sinuses and the Eustachian tubes. The bite and teeth are deformed, which is bad for the process of chewing food. For all of the above reasons, this birth defect must be corrected as early as possible.
Quite often there are otitis media and sinusitis. Inflammation occurs due to the fact that the consumed liquid and food through the cleft enters the sinuses and the Eustachian tubes. The bite and teeth are deformed, which is bad for the process of chewing food. For all of the above reasons, this birth defect must be corrected as early as possible.
Treatment
The treatment of the cleft palate is performed surgically. In order for it to be successful, it is necessary to combine the efforts of many doctors - a pediatrician, maxillofacial surgeon, orthodontist, as well as an otolaryngologist, neurologist, speech therapist.
To eliminate the effect, plastic surgery of the upper palate is performed, the integrity of the alveolar process and, if necessary, the upper lip is restored.
The first such operation was carried out two hundred years ago in France. Today, physicians are armed with several methods of treating a defect. The most successful are cheiloplasty (correction of a defect in the upper lip) and uranoplasty (elimination of a cleft palate).
Operations are carried out in several stages. In some cases, 2-3 procedures are enough, in others - 5-7 (it all depends on the severity of the pathology). But even experienced plastic surgeons will not be able to rid the child of a postoperative scar, but over time it becomes almost invisible.
Experts disagree on when to perform an operation to treat a disease of the cleft palate. Some believe that surgery is needed as early as possible - at 3-6 months, while others prefer to wait until the child grows up. However, both of them agree that it is necessary to complete the correction of the defect and rehabilitation by the age of 6. In part, such terms are called, since a child at this age should go to a school where healthy children study: the presence of a palatine cleft does not affect the intellectual development of the child, although until the defect is corrected, he is registered for disability.
The treatment of such defects is carried out in profiled clinics, where there are all the necessary specialists. They not only work on eliminating the physical handicap, but also help to overcome the mental trauma caused by external inferiority in order to fully integrate into society.
They not only work on eliminating the physical handicap, but also help to overcome the mental trauma caused by external inferiority in order to fully integrate into society.
Uranoplasty is one of the most effective methods for removing the cleft palate in children. It restores the anatomical structure of the hard and soft palate, middle sections of the pharynx.
The classic and basic version of this operation is Limberg uranoplasty. It is successful in 92-98% of cases.
The elimination of the cleft requires specialists to solve a whole range of tasks, including the restoration of each layer of the hard and soft palate, the elimination of the vicious attachment of the palatopharyngeal muscles, their correct connection, the elimination of the risk of damage to the nerves responsible for muscle contraction during surgery, etc. .
Radical uranoplasty is recommended for children aged 3-6 years. Patients with blind clefts are operated on at the age of 3–5 years, with penetrating unilateral and bilateral clefts – at the age of 5–6 years.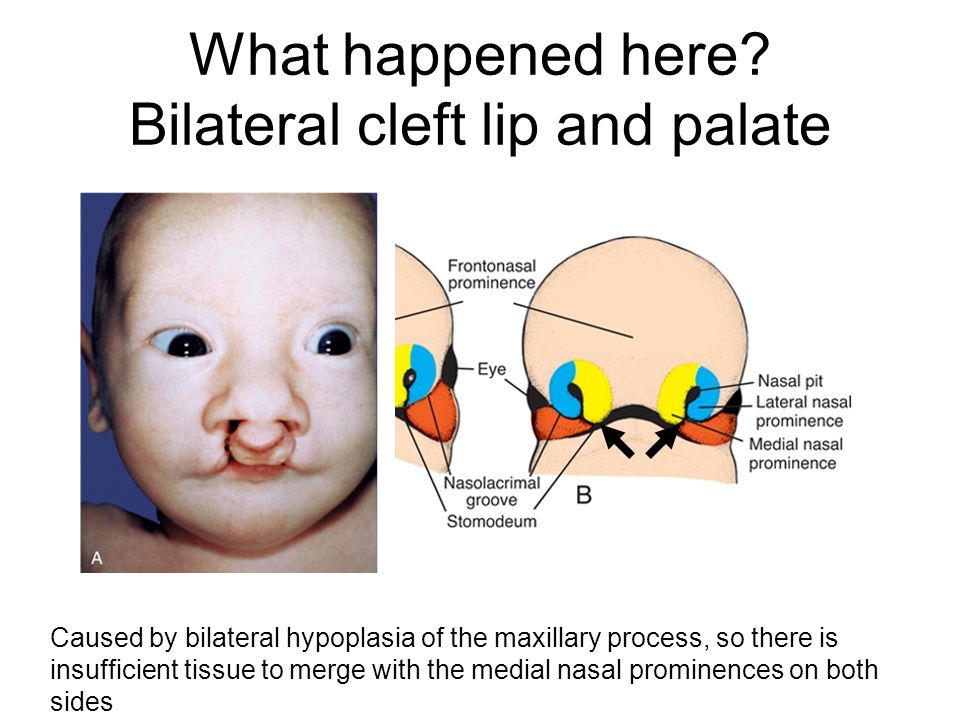
Radical uranoplasty is not recommended for children under 3 years of age. It is believed that it can lead to a delay in the development of the upper jaw. At the age of 2 years, sparing uranoplasty is possible.
Before surgery, the child is assigned to wear a "floating" obturator. It allows you to eat normally, breathe, develop correct speech. The device is removed two weeks before the operation.
After the operation, the child is given bed rest for 2-3 days. Only mashed food is allowed, plentiful alkaline drinking is recommended. Oral care should be especially thorough. Before and after meals, irrigation of the mouth with a weak solution of potassium permanganate (potassium permanganate) is necessary.
It is recommended to inflate balloons several times a day. Starting from the second week after the surgery, finger palate massage and special exercises are performed.
To prevent postoperative infection, antibiotics are prescribed, and painkillers if pain is present.