How to vaccinate a child
Your Child's Immunizations (for Parents)
Reviewed by: Elana Pearl Ben-Joseph, MD
en español Las vacunas de su hijo
Babies are born with protection against some diseases because their mothers pass antibodies (proteins made by the body to fight disease) to them before birth. Breastfed babies continue to get more antibodies in breast milk. But in both cases, the protection is temporary.
Immunization (vaccination) is a way to create immunity to (protection from) some diseases. Sometimes this is done by using small amounts of a killed or weakened germ that causes the disease. Other times the vaccine is simply a small piece of the germ, such as a protein or a piece of its genetic material.
Germs can be viruses (such as the measles virus) or bacteria (such as pneumococcus). Vaccines stimulate the immune system to react as if there were a real infection. It fends off the "infection" and remembers the germ. Then, it can fight the germ if it enters the body later.
What Are the Types of Vaccines?
There are a few different types of vaccines:
- Attenuated (weakened) live germs: These are used in some vaccines such as in the measles, mumps, and rubella (MMR) and chickenpox vaccines.
- Killed (inactivated) germs: These are used in some vaccines, such as in the flu shot or the inactivated poliovirus vaccine.
- Toxoid vaccines: These contain an inactivated toxin (harmful chemical) made by the germ. For example, the diphtheria and tetanus vaccines are toxoid vaccines.
- Conjugate vaccines: These contain small pieces of the germ combined with proteins that help trigger a strong immune response. Many commonly used vaccines are made this way, including those that protect against hepatitis B, HPV, whooping cough, and meningitis.
- mRNA (messenger RNA) vaccines: These use a piece of the germ’s RNA, which is part of its genetic material.
 Some of the COVID-19 vaccines are this type.
Some of the COVID-19 vaccines are this type.
The American Academy of Pediatrics (AAP) recommends that kids get combination vaccines (rather than single vaccines) whenever possible. Many vaccines are offered in combination to help lower the number of shots a child gets. This has been shown to be very safe. From the day a baby is born, their immune system is exposed to countless germs every day. A few more in a combination vaccine is very easy for the immune system to handle.
What Vaccines Do Kids Need?
The following vaccinations and schedules are recommended by the AAP. Some variations are normal, and recommendations change as new vaccines are developed. Your doctor will talk to you about the right vaccinations and schedule for your child.
Recommended vaccinations:
- Chickenpox (varicella) vaccine
- Diphtheria, tetanus, and pertussis (DTaP) vaccine
- Hepatitis A (HepA) vaccine
- Haemophilus influenzae type b (Hib) vaccine
- Hepatitis B (HepB) vaccine
- Human papillomavirus (HPV) vaccine
- Influenza (flu) vaccine
- Measles, mumps, and rubella (MMR) vaccine
- Meningococcal (MenACWY, MenB) vaccines
- Pneumococcal (PCV13, PPSV23) vaccines
- Polio (IPV) vaccine
- Rotavirus (RV) vaccine
- COVID-19 vaccine
- Dengue vaccine
Vaccine Concerns
Some parents may hesitate to have their kids vaccinated. They have questions or worry that a child might have a serious reaction or get the illness the vaccine prevents. But the components of vaccines are weakened or killed. In some cases, only parts of the germ are used. So they're unlikely to cause any serious illness.
They have questions or worry that a child might have a serious reaction or get the illness the vaccine prevents. But the components of vaccines are weakened or killed. In some cases, only parts of the germ are used. So they're unlikely to cause any serious illness.
Some vaccines may cause mild reactions, such as soreness where the shot was given or a fever. But serious reactions are rare. The risks of vaccinations are small compared with the health risks of the diseases they're intended to prevent.
Immunizations are one of the best ways to protect your family from contagious diseases.
Reviewed by: Elana Pearl Ben-Joseph, MD
Date reviewed: February 2022
Preparing for a positive experience
Vaccines can cause some pain and anxiety for children of all ages. This pain may cause your child to develop a fear of needles or other medical procedures. Fortunately, there are many strategies that can be used before and during the immunization appointment to help reduce pain and anxiety. Use these tips for a more positive immunization experience for you and your child.
Use these tips for a more positive immunization experience for you and your child.
Tip #1: Prepare your child before the visit
Children are very aware of the emotions of their caregivers. Although immunizations may be stressful for you, try to be calm during the appointment and when talking about immunization with your child. Use a matter-of-fact, supportive approach.
Toddlers and young children:
In general, toddlers and young children over 2 years of age should be informed about the vaccine shortly before the clinic visit or appointment. When you are discussing the vaccine with your child:
DO:
- Try to be calm even though you may be nervous about your child's immunizations. Your child is very sensitive to your emotions.
- Speak in an even, soft tone of voice.
- Answer questions honestly and choose words that lessen anxiety - for example, "you may feel pressure, squeezing, or poking", instead of words like "pain, hurt, or sting.
 "
" - You can say, "You need the vaccine to stay healthy. The medicine will be put in your arm with a needle. You will feel a quick poke."
DO NOT:
- Use words that focus the child's attention on the needle, such as "It will be over soon, and you will be okay."
- Give false reassurance, such as "It won't hurt." See "do" section above for suggested answers to the question, "Will it hurt?"
- Apologize - for example, "I am really sorry you have to go through this."
Why it works:
Your child is sensitive to your language and tone. If you speak positively about vaccines, your child is more likely to feel positive about it as well.
Consider using numbing creams and patches:
-
These products ease the feeling of pain by blocking pain receptors in the skin and should be applied about one hour before the appointment. These can be purchased without a prescription from most pharmacies.

-
Supervise your child after you apply the product so that they don't accidentally eat the cream or patch.
- For specific information on where to apply numbing creams or patches, ask your health care provider. You can find more information about numbing creams and patches here.
Tip #2: Comfort your child at the appointment
Use these tips to comfort your child at the appointment.
Children of all ages:
Comforting restraint:
Cuddle your baby or child firmly in your lap in a seated position.
Why it works:
Being held close to you calms your child and helps keep legs and arms still so vaccines can be given safely. Sitting upright helps children feel more secure and in control. Ask the health care provider for examples of upright positioning.
Distraction:
Use bubbles, a pinwheel or a squeaky, light-up or musical toy to distract your child immediately before and during the vaccination. Ask older children questions about something they are excited about. Older children can also use books, listen to music, or play video games to distract themselves.
Ask older children questions about something they are excited about. Older children can also use books, listen to music, or play video games to distract themselves.
Why it works:
Research shows that the part of the brain that processes pain is less active when children are distracted during immunizations.
Babies:
Breastfed babies:
Nurse your baby before, during, and after the immunization to provide comfort and distract them from the injection. Research shows that this is safe and will not cause the baby to associate breastfeeding with pain.
Why it works:
Breastfeeding comforts your baby with your presence. Sucking and the sweet taste of breast milk distract your baby. Breast milk also contains natural calming substances.
Breastfeed to minimize vaccination pain
Formula-fed babies:
A sucrose solution can be given immediately before the immunization for babies up to and including 12 months of age, to minimize pain and discomfort. Babies receiving the oral rotavirus vaccine (given at 2 and 4 months of age) do not need the sucrose solution because the vaccine contains sucrose and has the same effect as the sucrose solution.
Babies receiving the oral rotavirus vaccine (given at 2 and 4 months of age) do not need the sucrose solution because the vaccine contains sucrose and has the same effect as the sucrose solution.
You can prepare a sucrose solution at home and bring it with you to your child's immunization appointment. Health Canada recommends that all water given to infants be sterilized.
To prepare the sucrose solution:
- Bring cold tap water to a rolling boil for at least 2 minutes.
- Dissolve 1 teaspoon of sugar in 10 ml (2 teaspoons) of the boiled water in a sterile sealable container.
- Store the sucrose solution in the refrigerator prior to your child's appointment. The solution should be used within 24 hours.
At the appointment, give 2 ml of the sucrose solution to your baby with a cup, spoon, or syringe 1-2 minutes before the immunization and discard the unused portion.
Do not use sugar at home to calm upset or crying babies.
Why it works:
Research shows that this sweet tasting solution, given 1-2 minutes before a medical procedure, causes the release of natural pain-reducing chemicals in the brain.
Children 3 years of age and older:
Deep breathing:
Have your child focus on blowing out during the vaccine injection. Ask your child to:
- Blow bubbles
- Blow out a pretend candle
- Blow a pinwheel or party blower
Why it works:
Deep breathing triggers the body to relax its stress response. It also serves as a distraction.
Date last reviewed:
Tuesday, Mar 24, 2020
Vaccination of children with chronic diseases and pathological conditions
At present, among children there are a significant number of people with various deviations in health status, which causes apparent difficulties in administering preventive vaccinations to them. These difficulties, in particular, are associated with the belief of many medical professionals and parents that only healthy people should be vaccinated, believing that vaccination can cause exacerbation of diseases or post-vaccination complications and thus harm the health of children. However, in recent years, domestic and foreign pediatricians have conducted a number of studies that have proven the safety and effectiveness of vaccination of unhealthy children.
These difficulties, in particular, are associated with the belief of many medical professionals and parents that only healthy people should be vaccinated, believing that vaccination can cause exacerbation of diseases or post-vaccination complications and thus harm the health of children. However, in recent years, domestic and foreign pediatricians have conducted a number of studies that have proven the safety and effectiveness of vaccination of unhealthy children.
It is the weakened and unhealthy children, as most pediatricians in the world believe, that should be protected from infections in the first place, since they are the ones who get the most severe infections, give complications and deaths. However, vaccination of such children requires careful selection and application of individual vaccination tactics.
Vaccination should be started after studying the anamnesis of life and illness, characteristics of the perinatal period, psychophysical development, past diseases. If the child is under the supervision of a specialist and receives a course of treatment, it is necessary to familiarize yourself with his medical documents and decide on an individual vaccination schedule. If a child is in a state of acute illness, then he is exempted from vaccinations for the period of illness. With a variety of chronic diseases, children are vaccinated in remission. In such cases, the doctor determines the opportunity to start vaccination after examining the child, familiarizing himself with the data of his examination, treatment, consulting with relevant specialists: a neurologist, allergist, otolaryngologist, etc.
If the child is under the supervision of a specialist and receives a course of treatment, it is necessary to familiarize yourself with his medical documents and decide on an individual vaccination schedule. If a child is in a state of acute illness, then he is exempted from vaccinations for the period of illness. With a variety of chronic diseases, children are vaccinated in remission. In such cases, the doctor determines the opportunity to start vaccination after examining the child, familiarizing himself with the data of his examination, treatment, consulting with relevant specialists: a neurologist, allergist, otolaryngologist, etc.
Children with lesions of the nervous system, in which the disease proceeds without pronounced negative dynamics, are vaccinated against the background of the therapy received. Children with a history of convulsions, as well as with hypertension-hydrocephalic syndrome, are prescribed appropriate anticonvulsant and dehydration therapy for the duration of the vaccination process. Vaccinations can be carried out as early as a month after seizures. Children with Down's disease, phenylketonuria, infantile cerebral palsy are immunized according to the general schedule, observing the timing of the start of vaccination and the necessary intervals.
Vaccinations can be carried out as early as a month after seizures. Children with Down's disease, phenylketonuria, infantile cerebral palsy are immunized according to the general schedule, observing the timing of the start of vaccination and the necessary intervals.
For children suffering from food allergies with its various manifestations - skin, gastrointestinal, respiratory - it is very important to adhere to the diet and the undesirability of introducing new foods a week before and after vaccination. Parents should be given explanations about this even before the start of vaccination.
Children with a history of skin manifestations of allergies can be prescribed biologics and enzymes for the period of vaccination, since in most of them allergies are associated with dysbacteriosis or fermentopathies. Antimediator drugs (antihistamines, antiserotonin, etc.) before and after vaccination can be prescribed if the child is already receiving therapy with these drugs. It should not be changed (increased doses) for vaccination. Children with bronchial asthma are vaccinated against the background of basic therapy (including inhaled hormonal preparations, with a stable dose of the drug not less than 2–3 months before vaccination), but not earlier than one month after the last attack.
Children with bronchial asthma are vaccinated against the background of basic therapy (including inhaled hormonal preparations, with a stable dose of the drug not less than 2–3 months before vaccination), but not earlier than one month after the last attack.
Children with a tendency to immediate allergic reactions (urticaria, Quincke's edema, anaphylactic reactions in anamnesis) 30 minutes before the injection of the vaccine are administered a parenteral antihistamine drug in an age dose (if there was a history of shock, then 30 minutes before the vaccination, prednisolone may be administered at the rate of 1 mg/kg of the child's weight).
A large group consists of children who often suffer from acute respiratory viral diseases. Before vaccination, it is advisable for such children to prescribe a course of recreational activities. You can use vitamin therapy (for example, combined multivitamins with micronutrients or vitamin A, ascorbic acid alone), adaptogens, immunotropic drugs (cycloferon, thymogen, IRS-19, ribomunil). Ribomunil has a pronounced preventive effect and prevents the development of acute infections. Exacerbation of chronic diseases reduces the possibility of allergic reactions in the post-vaccination period. Can be used in children from 6 months of age.
Ribomunil has a pronounced preventive effect and prevents the development of acute infections. Exacerbation of chronic diseases reduces the possibility of allergic reactions in the post-vaccination period. Can be used in children from 6 months of age.
Children with endocrine pathology, diseases of the blood system, kidneys, congenital malformations of organs, rheumatoid diseases are vaccinated under the condition of stable remission using anti-relapse treatment or drugs that the child receives as the main therapy. Such patients need a minimum laboratory examination before and after vaccination to assess the safety of immunization and the sufficiency of the therapy.
Patients with a history of cancer can be vaccinated with all vaccines in the vaccination schedule, but not earlier than 6 months after the end of cytostatic therapy.
Children with primary immunodeficiency conditions can only be vaccinated with inactivated vaccines. HIV-infected children, without clinical manifestations of the disease and the absence of immunodeficiency, are vaccinated with all vaccines of the vaccination schedule.
All children with chronic diseases, including oncological diseases, as well as those with immunodeficiency conditions, should receive additional immunizations in addition to routine vaccinations and be vaccinated against influenza annually.
Vaccinations: to be or not to be?
The question of whether to vaccinate a child worries many parents. This topic is associated with many fears, myths and doubts. We asked the most exciting questions to the pediatrician of EuroMed Clinic Elena Sergeevna Kochetkova.
- Elena Sergeevna, can there be two opinions on the question of whether to vaccinate a child?
- Definitely not! Vaccination is the only way to protect your child from many dangerous (and sometimes deadly) infections. Many parents are afraid of complications after vaccinations, but I assure you, the risk of complications from past infections is many times higher. If we talk about complications after vaccinations, then first we need to distinguish between unwanted side effects and really real complications. Side effects are usually easily tolerated by the child and pass quickly. As for serious complications after vaccinations, I can say that in my more than 30 years of practice, I have only twice encountered really unpredictable and serious complications in children. And even then it cannot be said that they were completely criminal.
Side effects are usually easily tolerated by the child and pass quickly. As for serious complications after vaccinations, I can say that in my more than 30 years of practice, I have only twice encountered really unpredictable and serious complications in children. And even then it cannot be said that they were completely criminal.
Usually, complications can be avoided by preparing the child for vaccination, taking into account his history, diseases, and allergies he has.
- In what cases is the vaccine not given for medical reasons?
- Most of our medical exemptions are purely Russian reinsurance, a concession to anxious parents. Abroad, for example, a high temperature will be considered the basis for a temporary refusal to vaccinate, and we even have a runny nose, which was three days ago for many, is a reason to postpone vaccination. In most cases, vaccination does not affect recovery, just as recovery does not affect vaccination. But we have accepted everything that happens to the child for a long time after the introduction of the vaccine, to write off the vaccination. We forget the golden rule: “after” does not mean “due to”.
We forget the golden rule: “after” does not mean “due to”.
Of course, there are cases when it is better to postpone vaccination. This is an acute condition in case of allergies (during the remission period, vaccination for allergy sufferers is not only possible, but must be done), high fever, acute respiratory viral infections, and some neurological diseases. A separate case when vaccination is recommended to be postponed is the presence of benign neutropenia in a child under one year old. This condition is associated with the adaptation of the child to our urban conditions, modern loads; It is manifested by the fact that an insufficient number of neutrophils is observed in the blood test. Moreover, this amount does not fit either into the norm or into the state of illness, but is in the average value. In such a situation, it is better not to burden the body additionally, its immune forces are now already weakened, and all forces are aimed at adapting to the environment.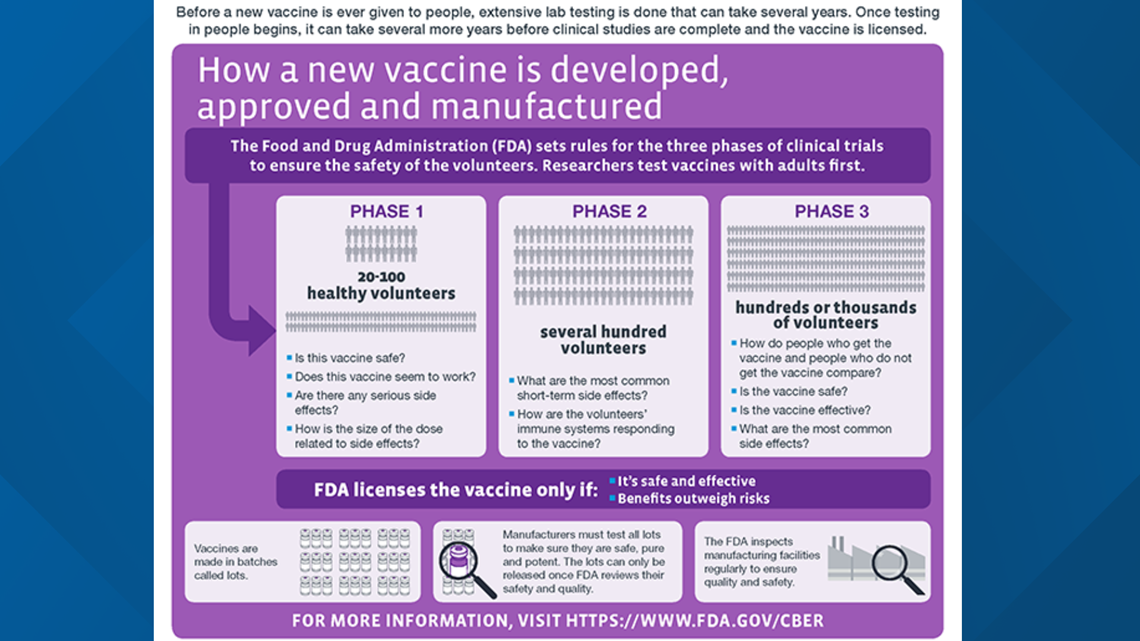
- Is it possible to vaccinate children prone to allergies, often ill?
- First of all! Of course, in an acute condition, vaccinations are not given. But in a state of remission, it is necessary to be vaccinated. Judge for yourself, if a child who is often ill, weakened, becomes infected with some serious infection, how will he get sick? With a high degree of probability - very difficult, most likely with complications. As for allergy sufferers, an additional problem will arise with them - how to treat them, how they will react to the disease, to medications. Again, there is a high risk that the disease will be severe.
Therefore, allergy sufferers, often ill children, patients with heart disease need to be vaccinated.
- There is an opinion that vaccination can provoke the development of allergies in a child. This is true?
- There is no direct connection here, of course. But if the child has a predisposition to allergies, the introduction of a vaccine can serve as an impetus for the development of the disease. In this situation, it is difficult to assume which is more dangerous, because the infection itself or medications can also provoke the development of allergies.
In this situation, it is difficult to assume which is more dangerous, because the infection itself or medications can also provoke the development of allergies.
- Many parents wonder whether it is worth vaccinating against hepatitis B and tuberculosis right away in the maternity hospital - after all, the newborn baby is still so weak. Perhaps it would be wiser to give him time to adapt, and give these vaccinations later - say, at 3-6 months?
- A child immediately after birth (and even while still in the womb!) Faces hundreds of microorganisms, and successfully processes them. So the additional couple of antigens that he will be injected with during vaccination do not play a special role against this background.
The immune response to BCG (vaccination against tuberculosis) develops within 2-3 months. Given that tuberculosis occurs in absolutely all social strata, including among very prosperous and wealthy people, then when should a child be vaccinated in order to provide him with reliable protection?
Hepatitis B is a disease that does not have the concept of “recovery” in childhood. If an adult becomes ill with hepatitis B, then he has a chance to control it - with the help of an appropriate lifestyle and medications. For children, this is not possible. They grow and therefore their hepatitis can only actively progress.
If an adult becomes ill with hepatitis B, then he has a chance to control it - with the help of an appropriate lifestyle and medications. For children, this is not possible. They grow and therefore their hepatitis can only actively progress.
In childhood, the main route of infection with hepatitis B is during medical procedures. And no one can know when a child will need medical attention: an emergency operation, a blood transfusion after an injury, an accident. Girls now have their ears pierced very early - and this is also a risk of contracting hepatitis.
It is no coincidence that hepatitis B vaccination is given on the first day after birth - precisely because no one is immune from urgent medical intervention.
- What other vaccinations, in addition to those listed in the vaccination calendar, can be recommended for a child?
- Vaccination against rotavirus infection. Rotavirus is very dangerous in the first years of a child's life. More than 90% of children with rotavirus infection are hospitalized in an infectious diseases hospital. In general, according to statistics, more than half of the hospitalizations of children with acute intestinal diseases are associated with rotavirus infection. The disease is accompanied by high fever, severe vomiting and diarrhea (diarrhea), which leads to dehydration, and for young children this can be very dangerous. In addition, children can get sick with this infection repeatedly, since it has a lot of varieties. The vaccine protects against rotavirus and greatly facilitates the course of the disease with related viruses (norovirus, astrovirus, etc.).
In general, according to statistics, more than half of the hospitalizations of children with acute intestinal diseases are associated with rotavirus infection. The disease is accompanied by high fever, severe vomiting and diarrhea (diarrhea), which leads to dehydration, and for young children this can be very dangerous. In addition, children can get sick with this infection repeatedly, since it has a lot of varieties. The vaccine protects against rotavirus and greatly facilitates the course of the disease with related viruses (norovirus, astrovirus, etc.).
The vaccination course includes three vaccinations with an interval of 4-10 weeks, the vaccine is administered orally (that is, drops in the mouth). The first vaccination is given at the age of 6 to 12 weeks (not later!), the last vaccination must be given no later than 8 months. After a full course of vaccination, the child develops immunity to rotavirus infection, which lasts up to 5 years. Revaccination is not required.
Chickenpox vaccination. This vaccination is not included in the Russian vaccination calendar, unlike many foreign countries, but I recommend doing it. You can get vaccinated against chickenpox from the age of the child.
Many parents ask themselves: why is it needed, because if a child gets chickenpox in childhood, then he will have immunity for life anyway? Everything is so simple. In childhood, chicken pox is usually quite easily tolerated, especially if the child's mother is immune to this infection, and, accordingly, the mother's antibodies still remain in the small child. In older adults, chickenpox, most often, proceeds quite severely and with a large number of complications.
Many years of experience allows us to make the following observations: now chickenpox mutates quite strongly. Even 15 years ago, most doctors treated chickenpox quite calmly, arguing in the same way: they had been ill with fairly predictable consequences, and immunity was formed.Now the virus is becoming more aggressive, deaths and serious complications are recorded every year! Rashes appear not only on the skin, but also on the mucous membranes, on the internal organs: the surface of the intestines, bronchi, and this can lead to the development of severe complications.
In addition, it is important to consider that chickenpox is caused by a generalized herpes infection. And after that, herpes does not leave the body. Often, after 40 years, the virus wakes up and manifests itself in the form of a neurological reaction: shingles in the intercostal spaces. This is usually associated with stress, with a decrease in immunity.
Thus, the relevance of vaccination against chickenpox is no longer in doubt.
Vaccination against HPV. Human papillomavirus (HPV) is the main cause of cervical cancer. Accordingly, timely vaccination of girls against HPV is a reliable protection against the development of cancer. HPV immunization is recommended for girls and young women who are not yet infected with HPV. It is advisable to vaccinate before the onset of sexual activity, it is usually recommended for teenage girls at 12 years of age. The standard vaccination course consists of 3 doses and is carried out according to the scheme (0-2-6 months): the second dose - 2 months after the first; the third dose - 6 months after the first.
It is advisable to vaccinate before the onset of sexual activity, it is usually recommended for teenage girls at 12 years of age. The standard vaccination course consists of 3 doses and is carried out according to the scheme (0-2-6 months): the second dose - 2 months after the first; the third dose - 6 months after the first.
This vaccine can be recommended for all girls. But if there is a family history (oncology in one of the close relatives, especially cancer of the cervix, vulva, vagina), then this vaccine is especially needed!
Boys are also recommended to be vaccinated. Firstly, in order to protect their future beloved women, since boys can be carriers of HPV. Secondly, HPV can be one of the factors in the development of oncology of the reproductive system in men, although this is much less common.
Thus, we repeat once again: only vaccination is a reliable protection against many serious infections. Let's not experiment on our children, testing their resistance to infections and playing Russian roulette: they will easily get sick or get severe complications from a disease from which we could easily protect them just by vaccinating.
- Vaccination
- is the most effective way to protect your child from infectious diseases. With the help of vaccinations, they successfully fight measles, rubella, mumps (mumps), chicken pox, polio, hepatitis B, rotavirus infection and bacteria that cause tuberculosis, diphtheria, whooping cough, tetanus, hemophilic infection.
The essence of vaccination lies in the fact that a child is vaccinated with a weakened or killed pathogen (or artificially synthesized, similar to the present one) in order to stimulate the body to produce antibodies to it.
- Immunization calendar
- is a list of vaccines and a scheme for their administration, approved by the Ministry of Health of the Russian Federation. The vaccination schedule regulates scheduled vaccinations and vaccinations that are given according to epidemiological indications.
Scheduled vaccinations are given against mass infections that are severe, have a high probability of adverse consequences or death.
They are carried out, starting from the birth of a child, according to a special schedule. In addition to the vaccinations approved in the calendar, you can separately vaccinate against certain serious infections if you wish: chicken pox, human papillomavirus, rotavirus infection, etc.
Vaccinations according to epidemic indications are given in case of outbreaks of certain infections; people living or visiting epidemiologically disadvantaged areas; workers of certain specialties (medical workers, teachers, etc.). For example, all residents of the Novosibirsk region are recommended to be vaccinated against tick-borne encephalitis, a dangerous infection that can be contracted by a tick bite.
| Categories and age of citizens subject to preventive vaccinations | Name of vaccination | Notes |
|---|---|---|
| Newborns in the first 24 hours of life | First vaccination against viral hepatitis B | |
| Newborns on 3-7 days of life | Tuberculosis vaccination | |
| Children at 1 month | Second vaccination against viral hepatitis B | |
| Children at 2 months | Third vaccination against viral hepatitis B | According to indications, only if the child is at risk. |
| First vaccination against pneumococcal infection (provides protection against pneumonia, bronchitis, otitis and moderate SARS) | ||
| Children at 3 months | First vaccination against diphtheria, whooping cough, tetanus | |
| First vaccination against Haemophilus influenzae (purulent otitis media, meningitis) | The course of vaccination against hemophilic infection for children aged 3 to 6 months consists of 3 injections of 0.5 ml with an interval of 1-1.5 months. | |
| First polio vaccination | ||
| Children at 4, 5 months | Second vaccination against diphtheria, whooping cough, tetanus | It is carried out for children who received the first vaccination at 3 months |
| Second vaccination against Haemophilus influenzae | It is carried out for children who received the first vaccination at 3 months | |
| Second polio vaccination | It is carried out for children who received the first vaccination at 3 months | |
| Children at 6 months | Third vaccination against diphtheria, whooping cough, tetanus | It is carried out for children who received the first and second vaccinations at 3 and 4. 5 months, respectively. 5 months, respectively. |
| Third vaccination against viral hepatitis B | It is carried out for children who do not belong to risk groups who received the first and second vaccinations at 0 and 1 months, respectively. | |
| Third vaccination against Haemophilus influenzae | It is carried out for children who received the first and second vaccinations at 3 and 4.5 months, respectively. | |
| Third polio vaccination | ||
| Children at 12 months | Vaccination against measles, rubella, mumps | |
| Fourth hepatitis B vaccination | Conducted for children at risk | |
| Children at 18 months | First revaccination against diphtheria, whooping cough, tetanus | |
| First revaccination against polio | ||
| Revaccination against Haemophilus influenzae | Revaccinations are carried out once for children vaccinated in the first year of life. |