Itchy toes pregnancy
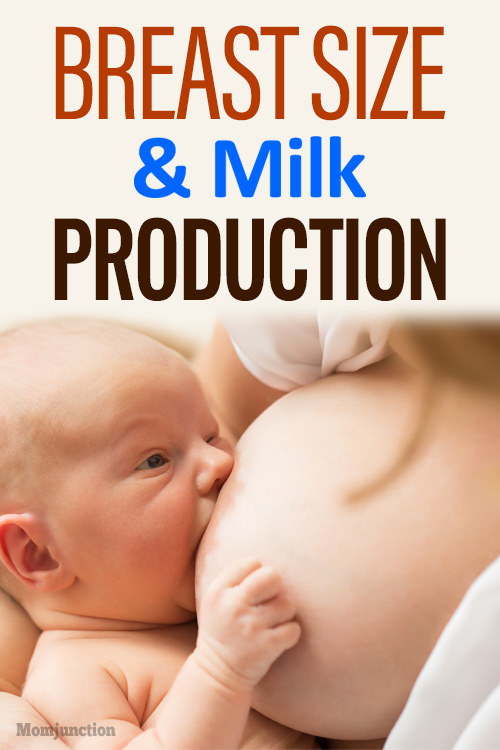
Why Itchy Feet Are a Thing During Pregnancy & How to Get Relief
While not the most talked-about pregnancy woe (swollen feet and back pain, anyone?) itching, also known as pruritus, is a very common complaint. Some women experience itching all over, while others feel it specifically on certain body parts such as their hands, feet, belly, or chest.
Most itching is just downright annoying, but severe itching can lead to loss of sleep or even be a sign of a very serious medical problem. We’ll talk about what could be causing your itchy feet, some treatments you can try, and when to call your doctor.
Hormonal skin changes
Your hormones are going crazy (as you’ve probably already noticed), and all that extra action from your endocrine system can cause your skin to get irritated.
Plus, your immune system works differently while you’re pregnant — it temporarily increases or suppresses certain functions so that your baby can grow in the best way possible.
The combination of hormones and immune system changes can lead to some pregnancy-specific skin conditions that may cause itchy feet.
You may notice:
- small, itchy bumps that resemble bug bites (prurigo)
- rash-like, itchy hives (PUPP)
- red, scaly, itchy patches (eczema or AEP)
The good news is that these skin conditions will not harm your baby and should go away after you deliver.
Nerve sensitivity
Again thanks to our good friends, the hormones, some pregnant women find that their nerves just seem more sensitive during pregnancy.
So seemingly “normal” things like sweating, being warm, wearing tight clothing, chafing, wearing the wrong shoes, or just lying in your bed can make your feet itchy.
Stretching
Not the kind of stretching you do in your prenatal yoga class — we’re talking about stretching of the skin. Your body goes through some amazing changes to house that rapidly growing baby, and stretching the skin, on your abdomen, thighs, buttocks, and breasts, is one of them.
Depending on your genes, hormones, and rate of weight gain you may be more or less prone to developing stretch marks (striae gravidarum).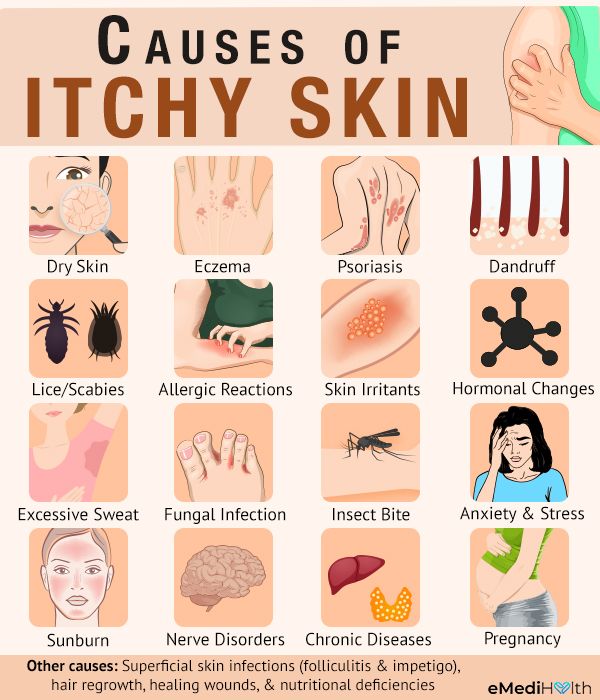 Stretch marks can be a source of itching.
Stretch marks can be a source of itching.
While your feet are unlikely to develop stretch marks, they do bear extra weight during pregnancy and the ligaments undergo some stretching of their own that can lead to an itching sensation.
Psoriasis
If you experienced psoriasis prior to pregnancy, you might get a welcome break from symptoms while you are pregnant. But, some women continue to experience painful, itchy plaques even during pregnancy, which can occur on your feet.
Cholestasis
Now for the rare, but serious, reason for itchy feet during pregnancy: intrahepatic cholestasis of pregnancy. This is a liver condition that, if it occurs, usually shows up during the third trimester.
Normally, your liver helps send bile to your digestive tract, where it aids in breaking down dietary fat.
Hormonal and digestive changes, as well as possible genetic predisposition, can cause the liver to not work like it should, which allows bile acids to build up in your body. This buildup of bile can cause some intense itching, particularly on your hands and feet.
This buildup of bile can cause some intense itching, particularly on your hands and feet.
Cholestasis can be dangerous for your baby. It can increase the risk of premature birth, fetal distress, and even stillbirth.
Call your doctor if you experience any of the following symptoms
- severe itching
- increase in itching
- itching that gets worse at night
- yellowish tinge to your skin or eyes (jaundice)
- dark urine
- pale or grey bowel movements
- right-sided upper abdominal pain
- nausea or upset stomach
For typical causes of itchy feet during pregnancy, there are several remedies you can try to get some relief and much-needed rest. These include:
- Soothing oatmeal baths. This natural and effective remedy is simple to try at home — and what pregnant mama doesn’t need a nice soak in the tub? Do check with your doctor before you add essential oils to your soak, as some are not safe for pregnancy or can further irritate your skin.

- Cold. Cool footbaths, cold washcloths, or even ice packs wrapped in towels can be applied to your feet to help soothe itchy skin. Don’t apply ice for more than 15 minutes.
- New socks. Loose-fitting socks made of natural, breathable fibers (such as cotton or even wool) can help keep feet from becoming sweaty and itchy.
- Massage. A foot massage — performed by you, your partner, or any willing pal — may help distract your nerves and decrease itchiness. Just be sure to stroke gently and avoid acupressure points on your feet and around your ankles, as some spots may stimulate uterine contractions. (Talk to your OB-GYN if you have any questions about this, especially if you’re far from your due date.)
- Moisturizers. A simple, unscented moisturizer such as cocoa butter, shea butter, or colloidal oatmeal can help soothe itchy feet. Check with your doctor before using any kind of topical medications, such as calamine lotion or lotion with diphenhydramine (Benadryl), as some may not be safe during pregnancy.

- Medications. If your itchy feet are caused by eczema or psoriasis, check with your doctor before using medications, even if they are over the counter. Many of these meds are not safe to use during pregnancy, and your doctor can help find safer alternatives. One preferred treatment for psoriasis during pregnancy is ultraviolet B phototherapy. If your itchy feet are keeping you from sleeping, in spite of trying at-home remedies, your doctor may be able to recommend a mild sleep aid to help you rest in spite of the discomfort.
If you think you have any symptoms of cholestasis, call your doctor right away. They may want to do blood tests to check your liver function, as well as an ultrasound called a biophysical profile to check on your baby’s movement, breathing, heartbeat, blood flow, and fluid levels.
If you do have cholestasis, your doctor will monitor you and your baby more frequently. Some possible treatments and tests include:
- nonstress test and biophysical profile
- blood work to check your liver function
- soaking itchy areas in cool or lukewarm water
- medication, such as ursodiol, to help decrease bile accumulation
- early delivery of your baby
While it may sound scary to deliver your baby earlier than you expected, your doctor will carefully weigh the risks of both early delivery and continuing your pregnancy with cholestasis.
The risks of cholestasis can be high, so it is often safer to deliver your baby, especially if you are at least 37 weeks pregnant. Babies delivered at this time typically do amazingly well, and you get to snuggle your bundle a little sooner!
Pregnancy is a wonderful, bumpy (pun intended) ride. In addition to all of the excitement and anticipation, there may be some less-than-glamorous side effects along the way. One of these may be itchy feet.
Itchy feet can be caused by a variety of hormonal and immunological changes that are normal during pregnancy. There are options to relieve your discomfort at home, such as oatmeal baths, cold packs, and moisturizers. If these aren’t effective, your doctor may be able to help.
In rare cases, itchy feet can be a sign of a serious medical problem. It’s important to call a doctor if you’re concerned about any of your symptoms so that they can help keep you and your baby safe. They will be able to monitor your baby, as well as recommend medication or delivery if needed.
Itching and intrahepatic cholestasis of pregnancy
Itching is common in pregnancy. Usually it's thought to be caused by raised levels of certain chemicals in the blood, such as hormones.
Later, as your bump grows, the skin of your tummy (abdomen) is stretched and this may also feel itchy.
However, itching can be a symptom of a liver condition called intrahepatic cholestasis of pregnancy (ICP), also known as obstetric cholestasis (OC).
ICP needs medical attention. It affects 1 in 140 pregnant women in the UK.
Symptoms of ICP
The main symptom is itching, usually without a rash. For many women with ICP, the itching is often:
- more noticeable on the hands and feet, but can be all over the body
- worse at night
Other symptoms can include:
- dark urine
- pale poo
- yellowing of the skin and whites of the eyes (jaundice), but this is less common
Symptoms of ICP typically start from around 30 weeks of pregnancy, but it's possible to develop the condition as early as 8 weeks.
Non-urgent advice: Call your midwife or GP if you have itching that's:
- mild or distressing, possibly worse at night
- anywhere on your body, but may be worse on the palms of your hands and soles of your feet
Feeling itchy like this can be a sign of ICP and needs to be checked.
Mild itching
Wearing loose clothes may help prevent itching, as your clothes are less likely to rub against your skin and cause irritation.
You may also want to avoid synthetic materials and opt for natural ones, such as cotton, instead. These are "breathable" and allow the air to circulate close to your skin.
You may find having a cool bath or applying lotion or moisturiser can help soothe the itching.
Some women find that products with strong perfumes can irritate their skin, so you could try using unperfumed lotion or soap.
Mild itching is not usually harmful to you or your baby, but it can sometimes be a sign of a more serious condition, particularly if you notice it more in the evenings or at night.
Let your midwife or doctor know if you are experiencing itching so they can decide whether you need to have any further investigations.
Intrahepatic cholestasis of pregnancy
Intrahepatic cholestasis of pregnancy (ICP) is a potentially serious liver disorder that can develop in pregnancy.
Normally, bile acids flow from your liver to your gut to help you digest food.
In ICP, the bile acids do not flow properly and build up in your body instead. There's no cure for ICP, but it should go once you've had your baby.
ICP seems to run in families, but it can happen even if there is no family history. It is more common in women of south Asian origin, affecting around 1 in 70 to 80 pregnancies.
It is more common in women of south Asian origin, affecting around 1 in 70 to 80 pregnancies.
If you have had ICP in a previous pregnancy, you have a high chance of developing it again in another pregnancy.
Some studies have found that babies whose mothers have ICP have a higher chance of being born prematurely or stillborn.
Because of the link with stillbirth, you may be offered induction of labour. This could be any time from 35 weeks, depending on the level of bile acids in your blood.
If you have ICP, you will probably be advised to give birth in hospital under a consultant-led maternity team.
Diagnosis and treatment of ICPICP is diagnosed by excluding other causes of the itch. Your doctor will probably talk to you about your medical and family history and order a variety of blood tests.
These will include tests to check your liver function (LFT) and measure your bile acid levels (BA).
If you are diagnosed with ICP, you will have regular liver function tests so your doctor can monitor your condition.
There is no agreed guideline on how often these tests should happen, but the Royal College of Obstetricians & Gynaecologists (RCOG) and the British Liver Trust advise weekly tests.
ICP Support, the UK's largest research group investigating ICP, also recommends weekly bile acid measurements. These readings help doctors recommend when your baby should be born.
If your LFTs and bile acids are normal and you continue to have severe itching, the blood tests should be repeated every week or 2, to keep an eye on them.
Creams and medicines for ICPCreams, such as aqueous cream with menthol, are safe to use in pregnancy and can provide some relief from itching.
There are some medicines, such as ursodeoxycholic acid (UDCA), that help reduce bile acids and ease itching.
UDCA is considered safe to take in pregnancy, although it is prescribed on what is known as an "informed consent" basis as it has not been properly tested in pregnancy.
You may also be offered a vitamin K supplement. This is because ICP can affect your absorption of vitamin K, which is important for healthy blood clotting.
Most experts on ICP only prescribe vitamin K if the mother-to-be reports pale stools, has a known blood clotting problem, or has very severe ICP from early in pregnancy.
If you are diagnosed with ICP, your midwife and doctor will discuss your health and your options with you.
Further information
The Royal College of Obstetricians & Gynaecologists (RCOG) has more information about obstetric cholestasis, including what it means for you and your baby, and the treatment that's available. You can also get information about ICP from the British Liver Trust.
You can also get information about ICP from the British Liver Trust.
The charity ICP Support provides information about ICP. You can also watch their video about ICP featuring mums and clinical experts.
Community content from HealthUnlockedWhy does the skin itch during pregnancy?
Skin itching during pregnancy is not a very common phenomenon. Most often, the skin begins to itch unbearably (as after mosquito bites) in the evening, closer to night, which can provoke insomnia and generally worsen a woman’s mood. Usually itching does not harm the baby and goes away after childbirth. However, it is still worth consulting with a gynecologist and dermatologist.
What does it come from?
The cause of itching during pregnancy in most cases is a violation of the liver: the production and outflow of bile, a general increase in the level of bilirubin in the blood. This is due to a hormonal failure in the body of the future mother - a violation of the synthesis of estrogens, as well as due to fetal pressure on the bile ducts. The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
The fatty acids produced in large quantities enter the woman's skin with the bloodstream and irritate the nerve endings, causing excruciating itching. Similar phenomena associated with stagnation of bile in the body can make themselves felt in the third trimester of pregnancy. Sometimes itching is accompanied by such dangerous diseases as diabetes mellitus.
Who is predisposed?
Itching during pregnancy is usually observed in women with chronic diseases of the biliary tract and with high levels of cholesterol in the blood. Such future mothers need to regularly (at least once a month) do a biochemical blood test to exclude toxic effects on liver cells.
How to fight?
A pregnant woman should tell her gynecologist about the discomfort associated with skin itching. In some cases, itching can be a sign of the development of such a dangerous disease as hepatitis. The doctor will conduct appropriate examinations. If, according to an objective examination, itching does not pose any danger, it is often possible to get rid of discomfort simply by following a diet aimed at lowering cholesterol levels, limiting the intake of fatty, spicy and salty foods that prevent the liver from coping with the function of bile secretion, as well as drinking plenty of water - it is necessary to eliminate dry skin. If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women.
If the diet does not help, the doctor may prescribe choleretic drugs suitable for pregnant women.
It is important to find the cause of the bothersome itching, eliminating a whole group of skin diseases that can occur during pregnancy.
Itching in the abdomen and chest
This itch is worth mentioning separately. As a rule, the skin on the abdomen or chest itches in the second and third trimesters due to its stretching, because it is these parts of the body that increase in volume during pregnancy. In this case, it is very important not to scratch the skin - this will lead to the appearance of stretch marks, which, unlike itching, will not go away after childbirth. Regularly use moisturizing creams, special products for stretch marks, do a light massage of the chest and abdomen with circular movements of your fingers and do not take hot showers.
You can get answers to any questions about pregnancy and childbirth from leading EMC experts in the classes of the School of Moms.
Subscribe to our Instagram. You will find useful information about pregnancy and childbirth from leading EMC obstetricians and gynecologists.
Dermatoses of pregnancy
Cost: from 1500 rubles
Sign up
Pregnancy is a wonderful time for any woman, especially when it is a planned and desired event in the life of a couple. Unfortunately, due to various circumstances, pregnancy does not always occur naturally - in such cases, modern medicine offers various procedures for assisted reproductive technologies. This makes the woman's attitude to such a natural process even more reverent. And here, often, our skin can present surprises. A number of skin conditions can worsen during pregnancy. However, traditionally prescribed drugs have limitations for use in such a situation. And here it is important that the specialist has experience in treating such situations.
Our Clinic is unique in some way, since not only the chief physician, who has been a consultant at the D. O. Ott, but also other specialists who are employees of the Department of Skin Diseases of the First Medical University. Academician I.P. Pavlov.
O. Ott, but also other specialists who are employees of the Department of Skin Diseases of the First Medical University. Academician I.P. Pavlov.
Now let's try to explain the causes and identify the most common skin diseases during pregnancy.
During pregnancy, the main cause of skin lesions is considered to be changes in the immune system of the pregnant woman. Pathological processes can be manifested by an exacerbation of chronic skin diseases or the appearance of specific pregnancy-associated dermatosis, the so-called "pregnancy dermatosis".
Changes on the skin are very diverse both in manifestations and in the mechanisms of development. Conventionally, they can be divided into 3 groups:
I. Pregnancy stigmas:
Chloasma is the most famous of them. As a development mechanism, various functional endocrine-metabolic changes during pregnancy are assumed. It appears as brownish spots of indefinite outlines, often symmetrical, on the skin of the cheeks, forehead, chin, neck without subjective sensations. Chloasma can occur at different gestational ages, intensifying as it develops and disappearing without a trace shortly after childbirth. But with subsequent pregnancies, chloasma occurs again. Exposure to sunlight enhances the severity of spots.
Chloasma can occur at different gestational ages, intensifying as it develops and disappearing without a trace shortly after childbirth. But with subsequent pregnancies, chloasma occurs again. Exposure to sunlight enhances the severity of spots.
Pregnancy melanosis - skin changes in the form of hyperpigmentation in the nipples, genitals, white line of the abdomen, also without subjective sensations or inflammation. After childbirth, these disorders disappear. Chloasma and melanosis usually do not require special treatment and spontaneously regress after delivery.
II. Skin diseases that are relatively often registered during pregnancy:
This group includes a variety of skin changes and diseases that often accompany pregnancy, as well as some common dermatoses, the course of which usually worsens during gestation. The main mechanism is a change in hormonal ratios in the body of a pregnant woman. This, in turn, affects the functionality of the immune and nervous systems, the state of the gastrointestinal tract, kidneys, cardiovascular activity, water-salt metabolism, etc.
This group includes: hyperhidrosis
- hypertrichosis
- palmoplantar telangiectasias
- erythema of the palms
- alopecia - hair loss
- onychodystrophy - changes in the nail plates
Most of these and other conditions, as a rule, disappear after childbirth. Their treatment, if necessary, is symptomatic.
The course and severity of symptoms of other skin diseases also change during pregnancy. These primarily include eczema, atopic dermatitis, psoriasis, lichen planus, acne, Dühring's herpetiformis. During pregnancy, they often worsen, and exacerbations are usually more pronounced, more severe than before gestation. Sometimes, on the contrary, during pregnancy, a remission occurs, which continues until childbirth, after which another exacerbation occurs. Correction of exacerbations of these dermatoses during pregnancy is very difficult. Many medicines used under normal conditions affect the development of the fetus. Therefore, external symptomatic therapy becomes the leading method.
Therefore, external symptomatic therapy becomes the leading method.
III. Actually dermatoses of pregnant women
The four skin diseases characteristic of pregnancy, gestational pemphigoid, polymorphic dermatosis of pregnancy, atopic dermatitis of pregnancy, and cholestasis of pregnancy can be distinguished by clinical presentation, histopathology, risk of fetal complications. Only gestational pemphigoid and intrahepatic cholestasis of pregnancy are associated with significant risk to the fetus. Because all of these dermatoses are characterized by pruritus, careful evaluation of any pruritic pregnancies is necessary.
Pregnancy pemphigoid , formerly known as herpes gestationis, is the rarest of the skin disorders of pregnancy and is an autoimmune disease. Clinically, it manifests itself in the form of papules and plaques, transforming into vesiculobullous elements, localized in the umbilical region with spread to the chest, back and limbs. Pemphigoid usually resolves spontaneously within a few months after delivery. As a rule, there is a recurrence of dermatosis during subsequent pregnancies with an earlier onset of dermatosis and greater severity compared to the previous pregnancy. Treatment should be aimed at reducing itching and blistering. In mild cases, topical corticosteroids and antihistamines are effective. In severe pemphigoid, it is advisable to use systemic corticosteroids.
Pemphigoid usually resolves spontaneously within a few months after delivery. As a rule, there is a recurrence of dermatosis during subsequent pregnancies with an earlier onset of dermatosis and greater severity compared to the previous pregnancy. Treatment should be aimed at reducing itching and blistering. In mild cases, topical corticosteroids and antihistamines are effective. In severe pemphigoid, it is advisable to use systemic corticosteroids.
Polymorphic dermatosis of pregnancy (PEP) is a benign, pruritic inflammatory disease. It usually occurs at the end of the third trimester or immediately after delivery in the first pregnancy. Urticarial papules and plaques appear first on the abdomen and, unlike gestational pemphigoid, do not affect the umbilical region. The rash usually spreads to the thighs and buttocks, and can rarely be widespread. Eruptions with clear boundaries regress spontaneously within 4-6 weeks without treatment. Treatment for PEP is based on symptomatic relief with topical corticosteroids and antihistamines. If the rash becomes generalized, a short course of systemic corticosteroids may be used.
If the rash becomes generalized, a short course of systemic corticosteroids may be used.
Atopic dermatitis of pregnancy (AEP) is the most common skin disorder in pregnancy. AEP is a benign disease characterized by an pruritic eczematous or papular rash. Two-thirds of AEP cases are characterized by eczematous skin changes localized to atopic areas of the body such as the neck and flexor surfaces of the extremities. The remaining cases are characterized by a papular rash in the abdomen and extremities. Lesions usually respond well to treatment and resolve spontaneously after delivery. However, AEP is more likely to recur in subsequent pregnancies. Dermatosis does not significantly affect the fetus, but there is an increased risk of developing atopic dermatitis in an infant.
Intrahepatic cholestasis of pregnancy (ICP) - characterized by itching with acute onset, which often begins on the palms and soles, and then generalizes. The skin has mostly secondary lesions such as excoriations but may also have papules. In 10%, jaundice develops due to concomitant extrahepatic cholestasis. After giving birth, itching goes away within a few weeks. There is a risk of recurrence in subsequent pregnancies. Diagnosis of ICP is important because there is a risk of complications for both mother and fetus.
The skin has mostly secondary lesions such as excoriations but may also have papules. In 10%, jaundice develops due to concomitant extrahepatic cholestasis. After giving birth, itching goes away within a few weeks. There is a risk of recurrence in subsequent pregnancies. Diagnosis of ICP is important because there is a risk of complications for both mother and fetus.
Treatment is aimed at normalizing the level of bile acids in the blood serum in order to reduce the risk to the fetus and to control symptoms in the mother. Treatment with ursodeoxycholic acid (UDCA) is recommended. Other drugs that reduce itching may be used, such as antihistamines, dexamethasone. Treatment of pregnant women with dermatoses is very difficult, especially in the first trimester of pregnancy. If dermatosis is detected in a pregnant woman, it is necessary to jointly manage it by a dermatologist, an obstetrician-gynecologist. Treatment of dermatoses in pregnant women requires a differentiated approach to therapy, taking into account the duration of pregnancy, exacerbation of the disease and the prevalence of the process.


-Step-1.jpg/aid1554278-v4-728px-Safely-Lose-Weight-(for-Teen-Girls)-Step-1.jpg)