Can you increase milk supply at 2 months
Worried About Milk Supply? Read How to Increase Breast Milk Output – Nourisher
Increasing your milk supply to feed your breastfed baby properly is a top concern among new mothers. But the strategies used to boost output depend on the age of your child and the length of your breastfeeding journey. Find out what you can do to increase your milk supply at delivery, in the first two weeks of motherhood, in the first month as well as after three months.
Understand how diet and calories affect your breast milk output and learn what foods women have eaten for decades to try and positively impact their supply. Finally, learn who to turn to when you need an advocate or resource with help establishing your milk supply.
Breast Milk Supply at Each Stage of Your Child’s Life
Your milk supply changes dramatically in the first few months of your child's life. While it is easier to increase your milk production in the early days of breastfeeding, you can still boost your supply after establishing a routine.
Increasing Milk Production at Delivery
Your body has been preparing for this day since the beginning of your pregnancy. For months pregnancy hormones have stimulated the growth of mammary glands and milk ducts. At delivery, your breasts will leak a thicker, yellowish fluid called colostrum. Small drops of this nutrient-rich “liquid gold” are enough to feed your newborn until milk production kicks into high gear. Women should nurse their baby as soon as possible and continue feeding at 2-hour intervals.
After Delivery Use Skin-to-Skin to Increase Milk Production
Skin-to-Skin contact has proven to have positive long-term effects on a healthy breastfeeding relationship. Global health organizations such as UNICEF and the World Health Organization advocate for babies to be placed “skin-to-skin within minutes of birth, remaining for 60 minutes or longer, with all mothers encouraged to support the infant to breastfeed with their babies show signs of readiness.” Ask for skin-to-skin contact immediately after birth, and don't be dissuaded if you give birth via a cesarean.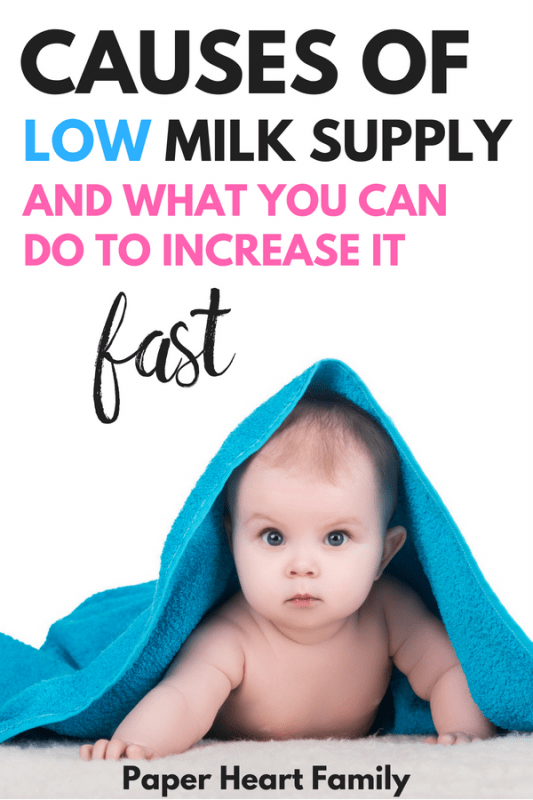 Skin-to-skin contact allows your body to relax, your heart rate to sync with your child and the release of the hormone oxytocin. All of these benefits contribute to a happier and smoother breastfeeding experience.
Skin-to-skin contact allows your body to relax, your heart rate to sync with your child and the release of the hormone oxytocin. All of these benefits contribute to a happier and smoother breastfeeding experience.
Related: Why All Breastfeeding Moms Should Advocate for Skin-to-Skin Contact
Increasing Milk Production in the First Two Weeks
What does it mean for your milk to come in and when does it happen? Milk “coming-in” refers to the time 2-5 days after birth when breasts feel firm, full and at times engorged. When you deliver the placenta after birth, the hormone progesterone drops and the hormone prolactin rises. This hormone shift alerts your body to start making milk.
In the first few days, hormones are the driving initiator of milk production. Your body has not yet learned how much breast milk is needed, so it goes into overdrive making milk before taking cues from your feeding patterns.
If you experience a forceful letdown, don’t waste any milk that might go into a nursing pad or your bra. Use a cup or a manual pump to catch those ounces coming from the letdown on the side you aren't nursing. Store this milk for future use and begin building your freezer stash!
Use a cup or a manual pump to catch those ounces coming from the letdown on the side you aren't nursing. Store this milk for future use and begin building your freezer stash!
Increasing Milk Production in the First Month
The first several weeks are a crucial time to show your body how much milk to produce. Some refer to this time as the “calibration window.” Your body produces milk on a demand and supply basis. The more demand for milk; the more supply you will have.
Here are tips for maintaining a stable supply in the first month:
- Nurse as frequently as possible. Pediatricians recommend nursing every two hours until baby is back to birth-weight. Once your child reaches this milestone, you should continue to nurse frequently without going more than four hours between feedings.
- Feed your baby from both breasts at each session. Why is this important? Frequency is more important than duration when establishing your milk supply.
 The more stimulation each breast receives the more milk it will produce.
The more stimulation each breast receives the more milk it will produce. - Alternate which breast you feed from first. Try this tip for remembering where to start! Put a bracelet or hair tie on the wrist of the side you nurse from first. (So feed from the left breast first, put a hair tie on your left wrist. At the next feeding session, start with the right breast and switch the hair tie to the right wrist.) Having a visual reminder of which breast to start on will allow you to easily alternate nursing sides without losing track.
- Ensure a proper latch. Babies incorrectly latched will have trouble emptying a breast of all of its milk. If this pattern continues, your body will assume that milk is not needed and incrementally start producing less.
Increasing Milk Production After 3 Months
Your breastfeeding routine should be more established around the third month of infancy. While there is no “normal,” a typical 3-month old child may eat 32 ounces of breast milk throughout five or so feedings a day.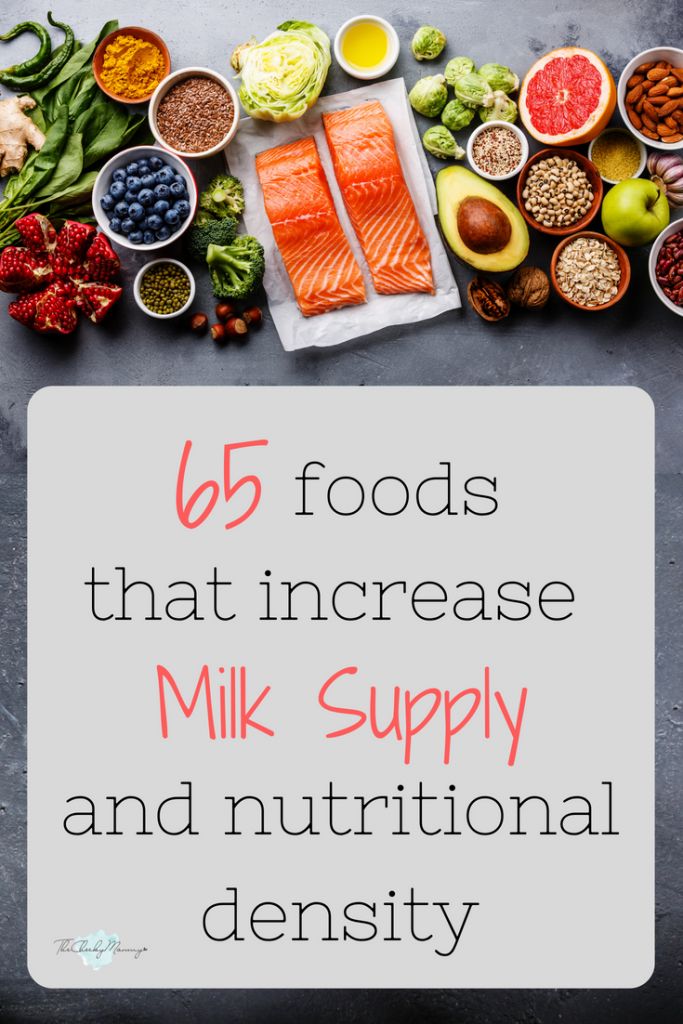
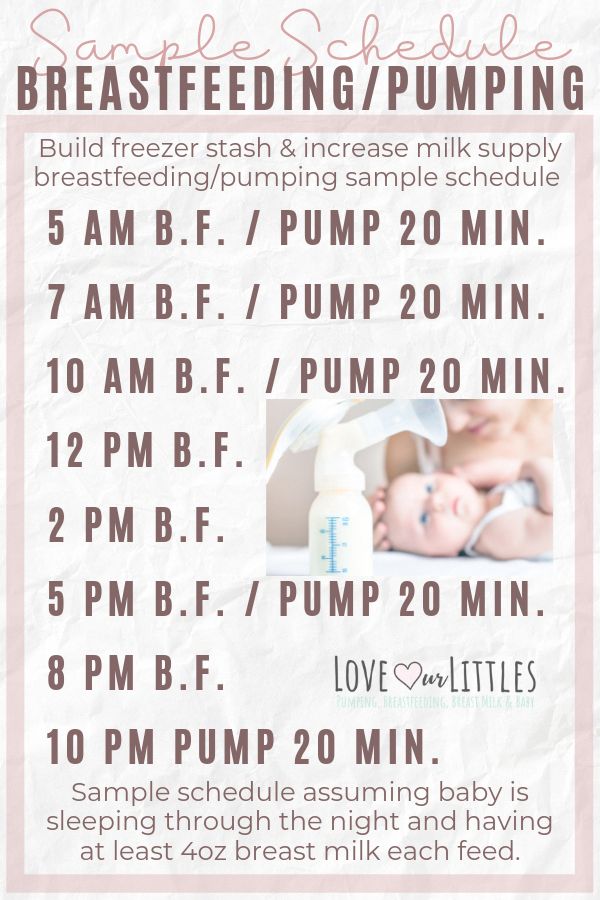
Women who want to increase their breast milk supply after the third month should continue to nurse frequently. Feed on demand and add in one additional pumping session a day to keep milk supply strong. Utilize the method of “power pumping” where you pump for 10 minutes, rest for 10 minutes, etc. for a total of 60 minutes to supercharge your supply.
Returning to Work When Breastfeeding
The 12-week mark also signifies a time when many women in the United States are transitioning back to work. A solid pumping routine and healthy freezer stash will allow your child to continue to receive the nourishment of breast milk for months to come.
Start building up your freezer stash before your maternity leave ends. Add in an extra pumping session in the morning and put those ounces in the freezer. Incorporate hand expression while pumping to get the most out of each session. Make small, circular movements starting from the outside of your breast and working in towards the pump. This massage helps your body release milk from each duct and drains your breast fully.
This massage helps your body release milk from each duct and drains your breast fully.
How Your Diet Can Increase Breast Milk Production
It is a myth that women need to eat specific types of foods to produce breast milk. After all, women are breastfeeding in California, Turkey, Argentina, Italy, South Africa – women breastfeed and eat differently in every country of the world!
A healthy diet with enough calories and a variety of nutrients is all that is needed to make breast milk. Focus on eating enough calories, drinking plenty of water and finding nutrient-rich foods to nourish your body.
Eat Enough Calories to Produce Breast Milk
Feeling hungry? Many women report feeling ravenous in the early days of breastfeeding. This hunger stems from mammary glands turning energy from your food (and your fat stores) into breast milk. Breastfeeding mothers need to add an extra 300-500 calories to their daily consumption.
Related: Breastfeeding Diet 101: What Your Body Needs to Produce Breast Milk
Avoid hitting your calorie quota with sugary, fattening snacks.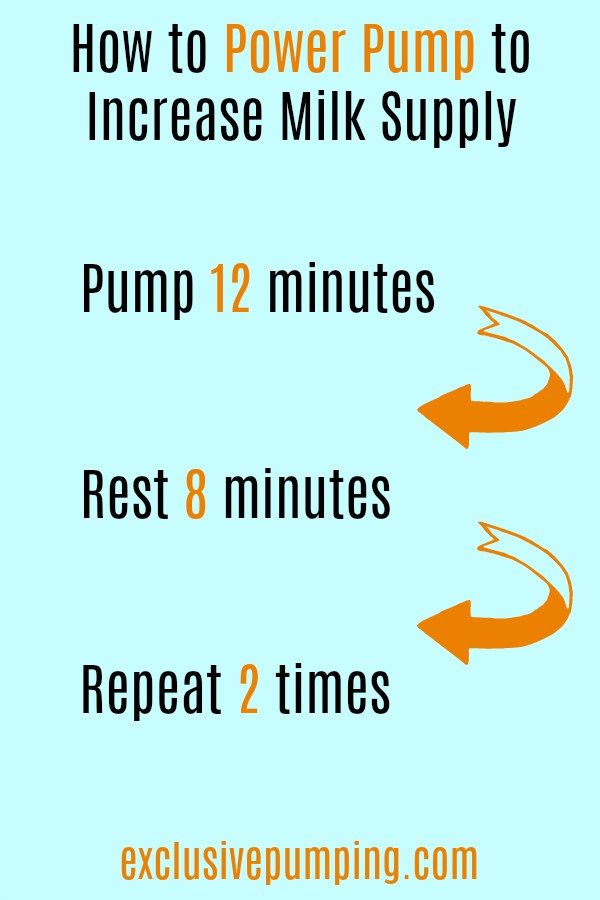 While two Snickers bars will meet the 500-calorie mark, they won’t fuel your body with healthy micronutrients found in vegetables or protein. Instead look for healthy lactation snacks that will replenish lost micronutrients and curb your hunger.
While two Snickers bars will meet the 500-calorie mark, they won’t fuel your body with healthy micronutrients found in vegetables or protein. Instead look for healthy lactation snacks that will replenish lost micronutrients and curb your hunger.
Do Specific Foods Boost Breast Milk Supply?
Brewer’s yeast, fenugreek, flax seeds, and nuts are commonly recommended foods to boost breast milk supply. High amounts of fiber, calcium, Vitamin B and magnesium qualify these foods as nutrient-rich choices for mothers who have depleted their micronutrient stores in pregnancy and childbirth.
Foods, supplements or beverages consumed to increase breast milk are called galactagogues. Women have eaten galactagogues for decades to increase breast milk output. The effectiveness of galactagogues varies among women. Some see an immediate boost in breast milk after eating brewer’s yeast or oats while others don’t notice a change in their supply. How can you tell which category you will fall into? Try eating lactation bars loaded with healthy ingredients! Nourisher provides a money-back guarantee on their 6-bar Milkful Nursing packs if they don’t work to increase your milk supply.
Remember to combine galactagogues with healthy breastfeeding habits if you want to see a positive change in your milk supply. Women who are looking to boost their supply should not expect diet or supplementation to overcome poor routines or latch issues.
Who Can You Talk to If You Suspect Milk Supply Issues?
These healthcare professionals are trained and ready to help remedy breastfeeding concerns for mothers.
Lactation Consultants - IBCLCs
Mothers looking to connect with healthcare professionals trained in breastfeeding support should connect with a Lactation Consultant. International Board Certified Lactation Consultants (IBCLC) are qualified to diagnose latch issues, assist a mother with a Supplemental Nursing System, coach a breastfeeding moms on pumping or nursing schedules and deal with individual concerns or questions.
Obstetricians and Gynecologists - OB/GYNs
Don’t overlook your OB/GYN as a resource for breastfeeding support.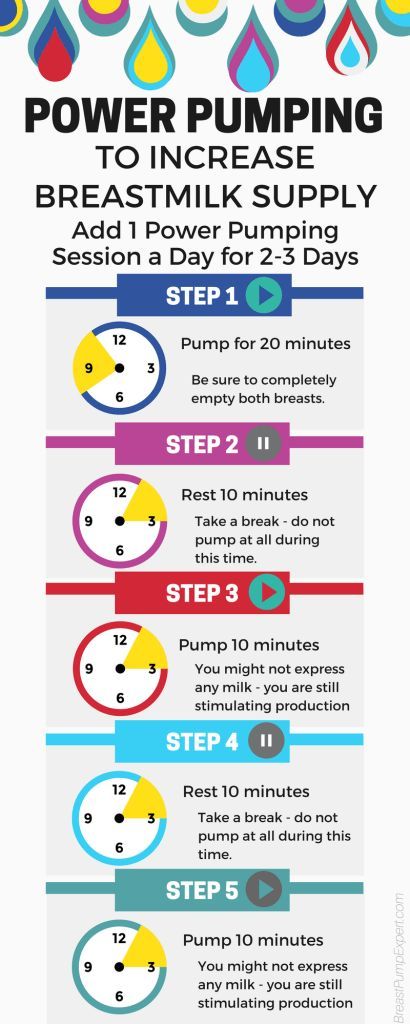 Unlike a Lactation Consultant, an OB/GYN has a complete view of your medical history. As a physician, they are also better equipped to answer questions about medications and breastfeeding, contraceptive options for breastfeeding women and breast pain that may cause disruptions to sustained breastfeeding.
Unlike a Lactation Consultant, an OB/GYN has a complete view of your medical history. As a physician, they are also better equipped to answer questions about medications and breastfeeding, contraceptive options for breastfeeding women and breast pain that may cause disruptions to sustained breastfeeding.
Your Child’s Pediatrician
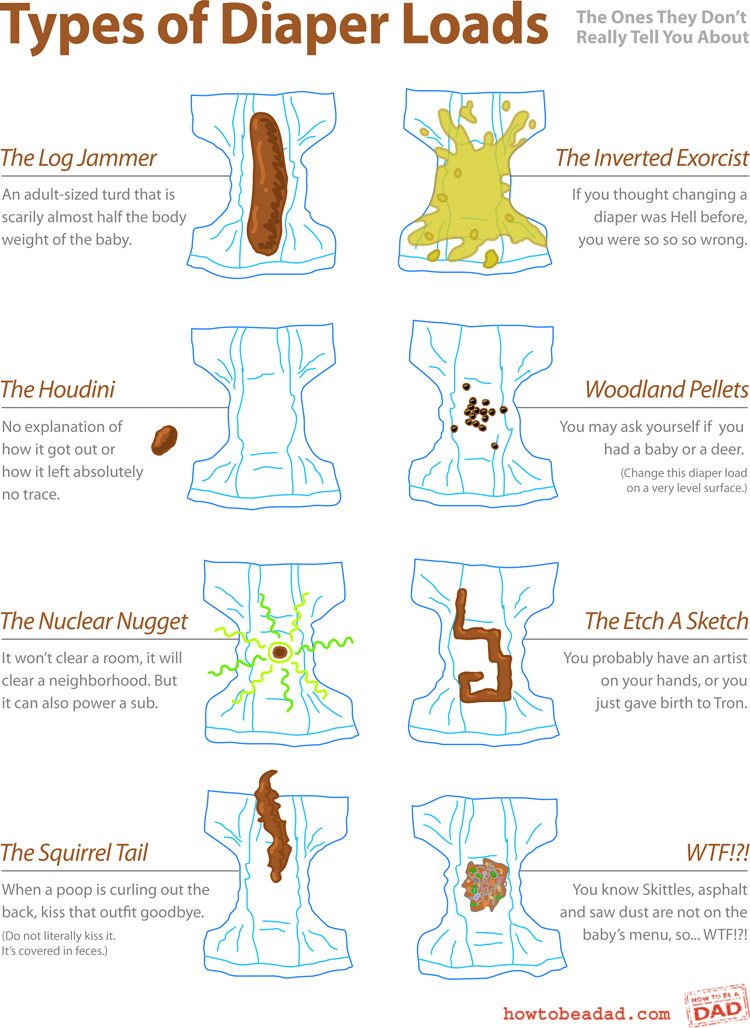
It’s not uncommon for mothers to question whether or not their baby is getting enough milk. Rather than focusing on the ounces you produce, focus on how your baby is progressing. Your child’s pediatrician can answer whether or not your baby is gaining enough weight, creating a healthy amount of wet and dirty diapers and meeting developmental milestones. Talk to your child’s pediatrician for confirmation on whether or not you need to increase your milk supply based on your child’s progress.
Keep Reading Preparing for Daycare When Breastfeeding ›
Disclaimer: Some portions of this site may provide you with health-related information or information about Nourisher products based upon information that you provide. However, that information and other content provided through the site (collectively, “Content”) are presented in a summary fashion and intended to be used for educational purposes only. The Content is not intended to be and should not be interpreted as a recommendation for a specific treatment plan or course of action. Your use of this site or the Content does not create a doctor/patient relationship. This site does not offer medical advice and nothing provided through this site, including any content, is intended to constitute professional advice for medical diagnosis or treatment. You should not use this site or any Content to diagnose a health or fitness problem or disease. Use of this site or any Content does not replace medical consultations with a qualified health or medical professional to meet the health and medical needs of you or any other party. Do not disregard the medical advice of a physician or health professional, or delay in seeking such advice, because of any information you obtain from the Site.
However, that information and other content provided through the site (collectively, “Content”) are presented in a summary fashion and intended to be used for educational purposes only. The Content is not intended to be and should not be interpreted as a recommendation for a specific treatment plan or course of action. Your use of this site or the Content does not create a doctor/patient relationship. This site does not offer medical advice and nothing provided through this site, including any content, is intended to constitute professional advice for medical diagnosis or treatment. You should not use this site or any Content to diagnose a health or fitness problem or disease. Use of this site or any Content does not replace medical consultations with a qualified health or medical professional to meet the health and medical needs of you or any other party. Do not disregard the medical advice of a physician or health professional, or delay in seeking such advice, because of any information you obtain from the Site.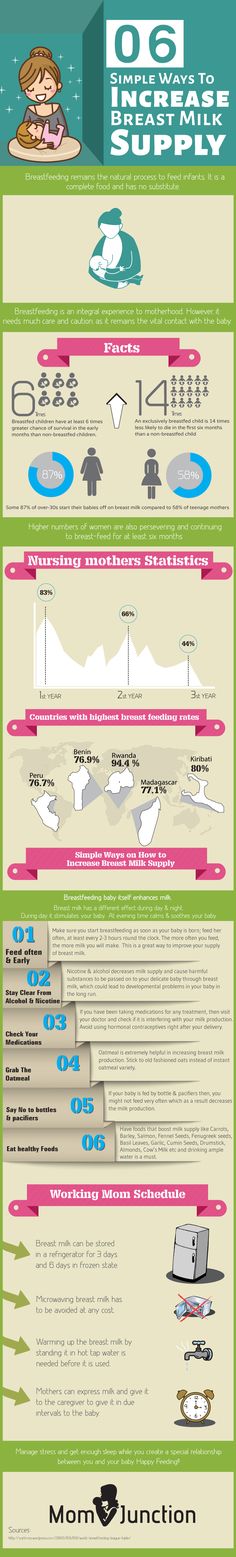
How to increase breast milk supply
How to increase breast milk supply | Pregnancy Birth and Baby beginning of content6-minute read
Listen
The best way to establish a healthy supply of breast milk is to start early, breastfeed frequently and make sure your baby is latching on correctly.
Some women have low supply, particularly during the early weeks of breastfeeding. This is the main reason some mothers start weaning or move to formula feeding. However, it's rare for a mother to produce less milk than her baby needs.
What are some reasons for a low supply?
There are many different reasons why some women have low supply including:
- delays in breastfeeding after delivery or separations of mother and baby such as if the baby needs to be admitted to the special care nursery or if the mother is unwell after delivery
- poor attachment to the breast, which can be caused by flat or inverted nipples, a tongue or lip tie, a sleepy baby because of jaundice, or a difficult or prolonged delivery
- if the mother is unwell due to problems like mastitis, retained placental tissue or large blood loss after the baby is born
- scheduled or timed feeding, rather than feeding baby on demand
- taking an oral contraceptive pill that contains oestrogen
- formula feeding as well as breastfeeding
- skipping breast feeds and offering a supplement formula feed but not expressing breast milk at that time to ensure that supply continues to meet baby's demand
- long-term use of dummies or nipple shields
- smoking
Breast milk supply can be low if the woman has medical problems such as polycystic ovarian syndrome, hypothyroidism, diabetes and pre-diabetes, or takes some blood pressure medications and cold and flu preparations, or has taken the contraceptive pill or has been infertile.
In some women, breast or nipple surgery makes breastfeeding difficult. In a few women, the breasts did not change during puberty and early pregnancy in a way that makes breastfeeding easier.
Typical baby behaviour
Some health professionals and mothers have an unrealistic expectation of how the baby will behave and might be concerned that what is normal baby behaviour could indicate low supply.
If your baby is having a good number of wet nappies each day, low supply is not a likely cause.
Some issues with breastfeeding include:
- wanting to be fed often — breast milk is digested in about 1.5 to 2 hours, whereas formula takes longer to digest
- being more fussy in the evening; you might produce less milk at this time and your baby will request fewer feeds or will 'cluster feed' (feed frequently at certain times of the day)
- liking to suck even if they have had a good breastfeed — sucking comforts them
- wanting lots of cuddles and skin to skin contact — this makes them feel secure and ensures that baby's needs are being met
- wanting to feed more frequently, which will happen when a baby is having a growth spurt — increased feeding will increase your supply
- reduced amount of sucking time at the breast — this often happens after 2 or 3 months as your baby becomes more efficient at the breast
What is normal for mum?
Although breastfeeding is different for every woman, the following do not mean that you have a low supply:
- your breasts suddenly seem softer — this is normal as your milk supply adjusts to your baby's needs
- your breasts do not leak milk, stop leaking or only leak a little
- you don’t feel a 'let-down' when milk pushes out of the breast
- you are unable to pump very much with an electric pump — remember the baby is much more efficient and will always get more than a pump
- how much you pump decreases over time
How do I know that baby is getting enough milk?
Always look at the whole picture to ensure that baby's growth and development is with normal limits. The baby is getting enough milk if they:
The baby is getting enough milk if they:
- go through 6 to 8 wet nappies in a 24-hour period including at least a few dirty nappies
- wake for feeds by themselves and feed vigorously at the breast
- have 8 to 12 breastfeeds in 24 hours
- pass a soft yellow stool
- settle and sleep fairly well after most feeds
- is back to birth weight in about 2 weeks
- gain on average 150g or more every week for the first 3 months
If your supply is low
Milk supply is considered to be low if you are not producing enough milk to meet your baby's normal growth and development needs.
Low milk supply is usually a temporary situation that will improve with appropriate breastfeeding support and management. Making more milk is all about supply and demand — the more milk is removed from the breast, the more milk is made. The less milk removed, the less made.
How to increase your supply
The following may help increase your breastmilk supply:
- ensure that baby is attaching well and removing milk efficiently from the breast
- be prepared to feed your baby more frequently — breastfeed on demand every 2-3 hours at least 8 times in 24 hours
- switch your baby from one breast to the other; offer each breast twice
- ensure your breasts are emptied well at each feed or pumping session; you can express after breastfeeds to make sure
- do not go longer than 5 hours without milk removal — your baby at the breast sucking is the most effective way to do this, but otherwise use a hand or electric pump
- when your baby is feeding, compress your breast to aid milk flow as this will also encourage more effective sucking
- make sure you are drinking a lot of water, eating a healthy balanced diet and not missing any meals
- also ensure you are resting as much as possible between feeds
Other options that can help with a low supply include:
- a supplemental nursing system or 'supply line'
- herbal and pharmacological remedies that are known to increase milk supply (galactogogues)
Some cultures use food or herbs to increase breast milk supply but many of these have not been formally studied. Domperidone is a prescription medicine that can increase the hormone prolactin, which can help stimulate breast milk production. Your doctor may discuss if this medicine is right for you. The main way to increase breast milk supply is through breastfeeding or expressing milk more than you currently do.
Domperidone is a prescription medicine that can increase the hormone prolactin, which can help stimulate breast milk production. Your doctor may discuss if this medicine is right for you. The main way to increase breast milk supply is through breastfeeding or expressing milk more than you currently do.
If you think you have low milk supply, talk to your doctor, lactation consultant, breastfeeding counsellor or child health nurse. You can call Pregnancy Birth and Baby on 1800 882 436 for advice and support.
Sources:
Australian Breastfeeding Association (Increasing supply), Karitane (Breastfeeding), Royal Women's Hospital (Low milk supply)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2021
Back To Top
Related pages
- Sore, cracked or bleeding nipples
- Breastfeeding your baby
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
How to increase the amount of milk for a nursing mother? - an article in the blog of the medical center Health for Children in Moscow
Breastfeeding is the key to good health and mental peace of the child for years to come. But besides this, breastfeeding solves most of the mother's issues: from financial issues to the convenience of building your day and bonding with your baby. Galina Vladimirovna Loseva, our most sought-after pediatrician with more than 20 years of experience, tells how to increase the amount of milk for good nutrition of a child
Galina Vladimirovna Loseva, our most sought-after pediatrician with more than 20 years of experience, tells how to increase the amount of milk for good nutrition of a child
The problem of lack of milk can occur both in the early neonatal period, when lactation is becoming established, and later, for example, during lactation crises, which can occur at certain periods of time (3-6 weeks, 3-4 months, 6 months), as well as after temporary weaning during the mother’s illness or the need to take certain medications that are incompatible with breastfeeding.
Ways to increase lactation:
- Feeding on demand , especially during early lactation. Frequent feedings in the first weeks of life are essential for maximizing the number of prolactin receptors to ensure sufficient milk production in the long term. Without these receptors, lactation will be at risk by 2-3 months of age. It is advisable to attach the baby to the breast as soon as possible after childbirth.
 If possible, do not use bottle supplements without a good reason. Night feedings are obligatory, the need for them usually lasts up to about 6 months.
If possible, do not use bottle supplements without a good reason. Night feedings are obligatory, the need for them usually lasts up to about 6 months. - Proper breastfeeding. The baby must include both the nipple and areola. His mouth should be wide open with his lower lip turned outward
- You can use post-feeding pumping to increase milk production. And at the same time, freeze milk to create a reserve in case the mother leaves or a case of illness in which it is necessary to interrupt breastfeeding.
- Rational nutrition for breastfeeding women. The menu should contain cereals, vegetables, fish, meat, eggs, fruits, dairy products are better than sour-milk, a small amount of nuts is acceptable. The use of strict hypoallergenic diets in a woman without an allergic history is unacceptable. Spicy dishes, spices, fried foods are excluded, this can affect the taste and smell of milk.
- Drinking enough liquid - water, green tea, compotes, fruit drinks.
 Drinks should preferably be warm or hot. It is recommended to take liquid 20-40 minutes before feeding.
Drinks should preferably be warm or hot. It is recommended to take liquid 20-40 minutes before feeding. - Eliminate alcohol, nicotine, including passive smoking.
- Compliance with the rest regimen , psycho-emotional peace, positive attitude. This is largely determined by the attitude of close people who can help a nursing mother in household chores, caring for other children, etc.
- Warm shower, light breast massage just before feeding.
- If you still need supplementary feeding, then it is better to give it with a pipette, spoon, syringe without a needle.
- Pharmacy products: Laktogon, Femilak. From herbs, galega, cumin, anise are considered safe. However, relying only on these funds is not worth it if the above points are not observed. They can be used as ancillary, as an addition to the diet of a nursing mother, which may be insufficient for certain reasons.
The material was provided by a pediatrician with more than 20 years of experience Galina Vladimirovna Loseva.
All recommendations should be applied after full-time consultation with a specialist doctor.
Lack of milk | How to increase milk supply
American Academy of Pediatrics and The American College of Obstetricians and Gynecologists. Breastfeeding Handbook for Physicians 2006). - American Academy of Pediatrics and American College of Obstetrics and Gynecology. The Doctor's Guide to Breastfeeding, 2006.
Donovan, T.J. & Buchanan, K. Medications for increasing milk supply in mothers expressing breastmilk for their preterm hospitalized infants. Cochrane . Database . Syst . Rev 3, CD 005544 (2012). - Donovan T.J. and Buchanan K., "Medicines for increasing the amount of milk in the impressive mothers of premature babies during the hospitalization period", Cochrane Database SYST ReV . 3 CD 005544(2012).
3 CD 005544(2012).
Hill, P.D., Aldag, J.C., Chatterton RT. Initiation and frequency of pumping and milk production in mothers of non-nursing preterm infants. J Hum Lact . 2001;17(1):9–13 - Hill P.D., Aldag J.S. and Chatterton, R.T., "Onset and frequency of expression and milk production in mothers who have given birth to premature babies and have not breastfed them." J Hum Lakt (Journal of the International Association of Lactation Consultants). 2001;17(1):9–13
Hill, P.D., Aldag J.C., Chatterton RT, Zinaman M. Comparison of Milk Output Between Mothers of Preterm and Term Infants: The First 6 Weeks After Birth. J Hum Lact . 2005 February 1, 2005; 21(1):22–30. - Hill P.D., Aldag J.S., Chatterton R.T., Zinaman M., "Comparison of the amount of milk in mothers of full-term and premature babies in the first 6 weeks after birth. " J Hum Lakt (Journal of the International Association of Lactation Consultants) 2005, 21(1): 22-30.
" J Hum Lakt (Journal of the International Association of Lactation Consultants) 2005, 21(1): 22-30.
Kent, J.C. et al. Importance of vacuum for breastmilk expression. Breastfeed Med 3, 11-19 (2008). - Kent J.S. et al., "The Importance of Vacuum in Expression of Breast Milk". Brestfeed Med 3 (Breastfeeding Medicine). 3.11-19 (2008).
Kent, J.C. et al. Longitudinal changes in breastfeeding patterns from 1 to 6 months of lactation. Breastfeed Med 8, 401–407 (2013). - Kent J.S. et al., Longitudinal changes in breastfeeding patterns from 1 to 6 months of lactation. Brestfeed Med (Breastfeeding Medicine) 8, 401-407 (2013).
Kent, J.C., Hepworth, A.R., Langton, D.B. & Hartmann, P.E. Impact of Measuring Milk Production by Test Weighing on Breastfeeding Confidence in Mothers of Term Infants. Breastfeed Med (2015). - "Measuring the amount of milk by weighing the baby and the impact of this process on the confidence of mothers of full-term babies.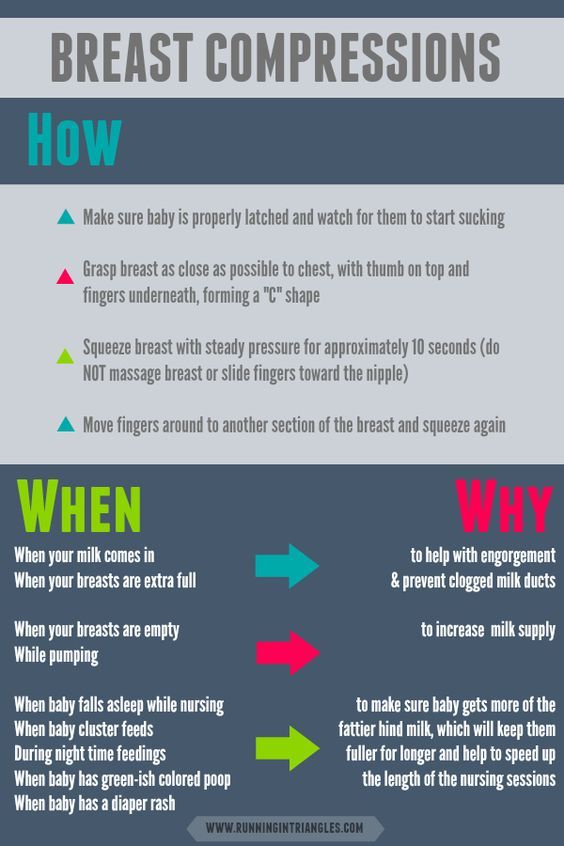 " Brestfeed Med (Breastfeeding Medicine) 2015.
" Brestfeed Med (Breastfeeding Medicine) 2015.
Morton, J., Hall, J.Y., Wong, R.J., Benitz, W.E. & Rhine, W.D. Combining hand techniques with electric pumping increases milk production in mothers of preterm infants. J Perinatol 29, 757–764 (2009). — Morton J., Hall J.I., Wong R.J., Benitz W.I. and Rhine, W.D., "Manual pumping combined with an electric breast pump increases breast milk production in mothers of preterm infants." J Perinatol (Journal of Perinatology) 29, 757-764 (2009)
Parker, L.A., Sullivan, S., Krueger, C. & Mueller, M. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants. Breastfeed Med (2015). - Parker L.A., Sullivan C., Krueger S. and Muller M., "Association of the time of onset of expression with the amount of milk and the timing of the onset of the second stage of lactogenesis in mothers of children who had extremely low birth weight.