How long is colostrum good for after pumping
Pumped Colostrum and How to Store It
Now reading: Liquid Gold: Pumped Colostrum and How to Store It
PrevNextThe birth of a baby is an exciting time, but it can also be overwhelming for new mothers. You’re faced with incredible physical and emotional demands, and the new chapter is only beginning. You’re now ready to take your first step along your breastfeeding journey.
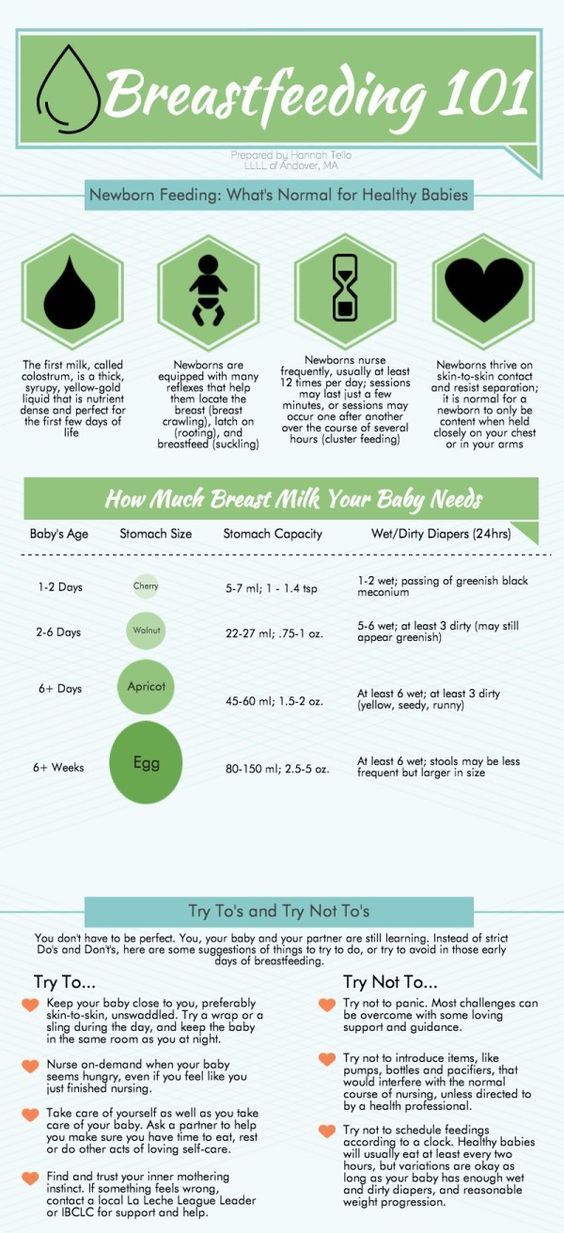
It’s common for new mothers to struggle with nursing. In fact, 92% of new mothers struggle with breastfeeding in the first three days post-partum. Breastfeeding isn’t always successful on the first try. Babies often have difficulty latching on, and sometimes a mother’s milk supply isn’t abundant. Luckily, pumping is an effective way to express milk for the baby and helps produce and maintain milk supply for mom.
The earliest supply of milk – colostrum – has some of the most important nutrients mothers can supply their newborns. Colostrum is essential to babies in the first few days after birth. To set yourself up for success, it’s helpful to know what to do with pumped colostrum and how to store it.
Until full milk production begins two to three days after birth, new moms produce small amounts of colostrum. Also called “liquid gold,” this thick, yellowish milk is rich in nutrients and carbohydrates. In addition to providing essential nutrition to the baby, colostrum helps with digestion and bowel movements in newborns. This is important in ridding the baby’s body of toxins that can cause jaundice.
Colostrum is also high in white blood cells and antibodies that develop the baby’s immune system. It builds a protective coating in their digestive system that helps prevent the growth of disease-causing germs. It’s a baby super-food and is an invaluable asset to their health and well-being.
What to Do with Pumped ColostrumA baby only consumes small amounts of colostrum in its first days. Regardless, studies show that expressing these low quantities within the first hour of birth can prevent delays in milk production. If a newborn doesn’t nurse within six hours after birth, it’s a good idea for mom to begin pumping. Make sure your hands are clean and that any collection tools are sterilized for the baby’s safety. Once you’re ready to pump colostrum, you’ll want to follow these next steps.
If a newborn doesn’t nurse within six hours after birth, it’s a good idea for mom to begin pumping. Make sure your hands are clean and that any collection tools are sterilized for the baby’s safety. Once you’re ready to pump colostrum, you’ll want to follow these next steps.
Many new moms prefer to use a syringe or Hegen’s revolutionary press-to-close, twist-to-open airtight storage bottles to collect colostrum. As you pump the breast, you’ll notice beads of liquid forming. Gather this in one of the containers and, once complete, put the syringe in a sealable baggie or close the bottle tightly. Then, write the date on the container so you can keep track of your stored supply.
2. Feed It to Your BabyOnce you’ve collected colostrum, it’s ready for consumption. You can administer it via a syringe or small bottle (remember, quantities will be relatively low). You can also feed drops of it to your baby on a clean finger. Every bit is packed with nutrients to help your baby’s development.
Every bit is packed with nutrients to help your baby’s development.
If your colostrum production is going well and you’re building up a steady supply, you can store it for future use. In fact, some women begin collecting their colostrum before the baby actually arrives. In a typical healthy pregnancy, there’s no need to express colostrum before giving birth. However, in some instances, it’s beneficial to collect colostrum toward the end of the pregnancy. Harvesting colostrum this early may be recommended if:
- You’re having twins – birth weight tends to be low for multiples.
- You have health concerns – gestational diabetes can affect the baby’s glucose levels at birth.
- Your baby has a cleft lip or palate – this can make breastfeeding difficult.
Whatever the case, pumped colostrum can be collected and saved for when the time is right.
4. Bring It to the Hospital
Bring It to the Hospital If you do decide to pump and store your colostrum before giving birth, be sure to include this in your hospital bag list to take along with you when you head to the hospital for delivery. Carry it in an insulated bag with ice packs and ask the nurse to store it in the maternity ward’s refrigerator until you’re ready to use it. This colostrum will be safe for use for up to 48 hours.
4 Tips for Storing ColostrumBreastfeeding mothers can ensure the safety and quality of expressed breast milk by following proper storing techniques. Consider these four tips for storing colostrum safely.
Properly Seal the ContainerTo maintain freshness and quality, be sure your storage container is completely sealed. Never use disposable bags or liners to store pumped colostrum. These aren’t designed to protect against bacteria and germ growth.
Consider Shelf LifeColostrum can be stored at room temperature for up to four hours. It can remain in a refrigerator for up to four days. You can store pumped colostrum in the freezer for up to six months (for best quality) or 12 months, at most. If you’re uncertain about how long your colostrum has been stored, it’s best to dispose of it. Better safe than sorry!
It can remain in a refrigerator for up to four days. You can store pumped colostrum in the freezer for up to six months (for best quality) or 12 months, at most. If you’re uncertain about how long your colostrum has been stored, it’s best to dispose of it. Better safe than sorry!
When storing expressed colostrum in the refrigerator or freezer, set the container at the back of the shelf where temperatures are coolest. Avoid storing it in the door compartment, as opening and closing the fridge will expose stored colostrum to frequent temperature changes that can negatively impact its quality and freshness.
Store It On-the-GoWith careful planning, it’s possible to travel safely with stored colostrum. Pack the container in an insulated bag and surround the colostrum with ice packs. It can remain safe for consumption this way for up to 24 hours. When your journey is over, use it right away or store it in the fridge or freezer.
Additional Colostrum Questions
We've received quite a few questions from moms who have reached out to us.
We will continually add to this post as we receive new questions and want to thank those who have helped to provide us with great questions that will eventually help so many other new moms!
Is Frozen Colostrum good for a sick baby?Yes, frozen colostrum does help a sick baby. Research studies have proven that sick or preterm infants who take colostrum from mothers have “significantly better health outcomes”. Colostrum is made up of immune factors, protein, sugar, and facts. Therefore, every drop counts!
How Long Does Colostrum Last in the Freezer?
Colostrum can last 2 to 6 months with a separate door freezer (5 degrees Fahrenheit or -15 degrees Celsius) with proper storage.
What Should I Do with Frozen Colostrum That's Been Stored For More than 6 Months?
If the colostrum has been stored with a deep chest freezer (-4 Fahrenheit or -20 Celsius) is fine!
How Do I Pump Colostrum After Birth?
Colostrum is thick, sticky, concentrated milk. The best way to collect the colostrum is by hand expressing. Remember the best pump is still the baby. If your baby suckles well, you can just concentrate on latching for the first few days. Unless a baby is separating from his/her mother due to medical reasons, you, as a mother, need to start pumping 8 to 12 times a day.
The best way to collect the colostrum is by hand expressing. Remember the best pump is still the baby. If your baby suckles well, you can just concentrate on latching for the first few days. Unless a baby is separating from his/her mother due to medical reasons, you, as a mother, need to start pumping 8 to 12 times a day.
What is the Best Way to Reheat Colostrum (if any) or Best Methods For Thawing Colostrum For the Baby?
Place the frozen container in the refrigerator the night before you intend to use it. Then warm the milk by placing it in a bowl of warm water or by simply using an electric warmer.
Are There Any Negatives to Giving Colostrum to a Toddler?
Colostrum will not negatively affect toddlers because of the amazing antibodies in the breast milk!
Is Colostrum Considered Better Than Breast Milk?
It is important to note that breast milk changes from colostrum, transitional milk to to mature milk to meet your baby’s nutritional needs at the different stages.
Tips For Hand Expressing Colostrum
Starting by massaging the breast with clean hands to help milk flow. Then by placing your thumb and the rest of your fingers on either side of the areola, about an inch away, gently push your fingers back & towards your chest wall, then compress the milk ducts of the breast, and roll the tissue forward & towards the nipple. Be sure not to squeeze the nipple or slide fingers along your skin.
When is the Best Time to Start Expressing Colostrum?
From 36 weeks of gestational age onwards, mothers are encouraged to harvest colostrum with a proper technique. You can start 2 or 3 times a day and each time for about 3 to 5 minutes, but you'll need to stop if you experience cramps or early contractions to avoid premature delivery.
How Long Do You Produce Colostrum For After Birth?
Colostrum is usually produced for the first few days (usually 3 days ) after the baby’s birth. However, some mothers might not see colostrum until day 5 after giving birth due to various factors.
Can you collect some Colostrum and then pump some more later and add to the original bag?
If the colostrum was stored inside the freezer or fridge and you need to add more to it later, you need to ensure the colostrum is the same temperature. We would suggest to first store the second round of colostrum in a different container and keep it inside the fridge for at least 1 hour. This allows the milk to cool to the same temperature as the initial container which makes it safe to combine.
You can also opt to align their temperatures by keeping it out. Please make sure it remains under 77°F (under room temperature). At this temperature, it can last for approximately 4 hours. This allows for ample time to combine the two containers together but do kindly ensure proper hygiene to minimize contamination.
Hegen Helps New Moms Pump and Store Their Colostrum
Today’s women are juggling their passions, careers, and responsibilities with the full-time job of motherhood. While it’s a wonderful adventure, being a mom brings numerous challenges. Breastfeeding shouldn’t be one of them. At Hegen, we want to make breastfeeding easier, rewarding, and empowering. From state-of-the-art breastmilk storage supplies to educational resources, we cover all the bases for you as you transition to your new role.
While it’s a wonderful adventure, being a mom brings numerous challenges. Breastfeeding shouldn’t be one of them. At Hegen, we want to make breastfeeding easier, rewarding, and empowering. From state-of-the-art breastmilk storage supplies to educational resources, we cover all the bases for you as you transition to your new role.
You are free to browse our storage containers as well as our 2 oz bottles (which double as colostrum collectors) which can help you on your breastfeeding journey!
What Is It, Benefits & What To Expect
Overview
What is colostrum?
Colostrum (kuh-loss-trum) is the first milk your body produces during pregnancy. It forms in your mammary glands (breasts) and plays an important role in building your baby's immune system. If you plan on breastfeeding (nursing or chestfeeding), it's the first milk your baby will get from your breasts. If you don't want to breastfeed or if your baby is struggling to breastfeed, you can hand express colostrum.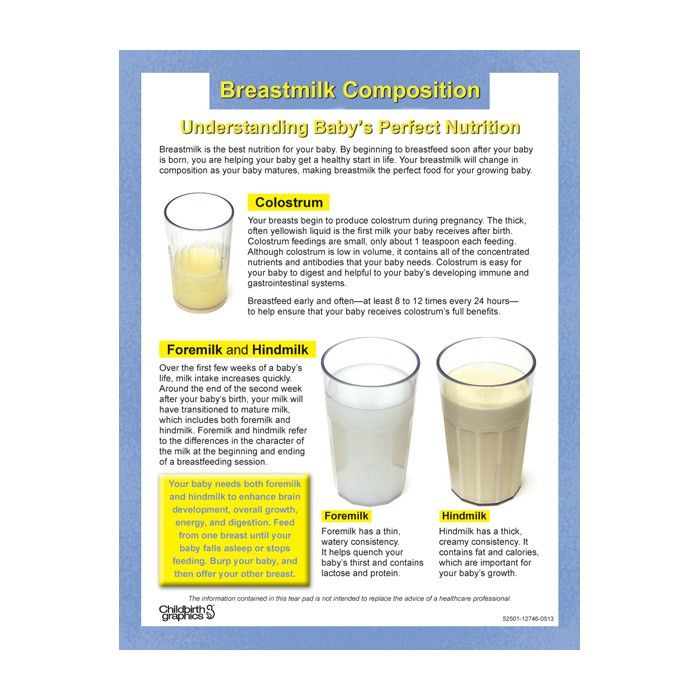 It's high in protein, vitamins, minerals and immunoglobulins (antibodies) that help build your baby's immune system. It's often called "liquid gold" because of its rich, golden color and valuable benefits.
It's high in protein, vitamins, minerals and immunoglobulins (antibodies) that help build your baby's immune system. It's often called "liquid gold" because of its rich, golden color and valuable benefits.
What is colostrum made of?
Colostrum is high in protein and low in fat and sugar. It's filled with white blood cells that produce antibodies. These antibodies strengthen your baby's immune system, protecting him or her from infection. Colostrum is highly concentrated and nutrient-dense even in tiny doses, so your baby's tummy doesn't need a lot to reap its benefits.
What kind of nutrients are in colostrum?
Colostrum is rich in nutrients that protect and nourish your baby unlike anything else. It's made up of things like:
- Immunoglobulin A (an antibody).
- Lactoferrin (a protein that helps prevent infection).
- Leukocytes (white blood cells).
- Epidermal growth factor (a protein that stimulates cell growth).
It gets its color from carotenoids (an antioxidant) and vitamin A. Vitamin A plays a vital role in your baby's vision, skin and immune system. Colostrum is rich in magnesium, which supports your baby’s heart and bones, and copper and zinc, which also support immunity.
Vitamin A plays a vital role in your baby's vision, skin and immune system. Colostrum is rich in magnesium, which supports your baby’s heart and bones, and copper and zinc, which also support immunity.
What's the difference between colostrum and breast milk?
Colostrum is a nutrient-rich first milk produced by your breasts during pregnancy. It changes to transitional breast milk a few days after your baby is born. However, small amounts of colostrum remain in your breast milk for several weeks.
There are distinct differences between colostrum and breast milk:
- Colostrum is filled with immunoglobins to boost your baby's immune system and protect it from illness.
- Colostrum has two times as much protein.
- Colostrum has four times as much zinc.
- Colostrum is lower in fat and sugar so it's easier to digest.
- Colostrum is thicker and more yellow.
What are the stages of breast milk?
There are three different stages of breast milk: colostrum, transitional milk and mature milk.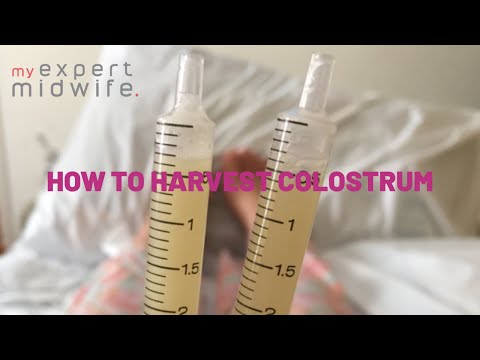
- Colostrum: Your first milk that lasts between two and four days after birth.
- Transitional milk: Begins approximately four days after birth and lasts about two weeks.
- Mature milk: Milk that lasts from approximately 14 days after birth until you are done producing milk.
When does colostrum turn to milk?
After approximately three or four days, colostrum will turn to transitional milk. This is often referred to as someone's milk "coming in." Your breasts will feel firm, tender and full. It means your milk supply has ramped up. By this time your baby's stomach has expanded and they can drink more milk each feeding. Once your milk supply is established and your body has stabilized, transitional milk changes to mature milk.
What makes colostrum turn to breast milk?
The pregnancy hormones created by the placenta help you create colostrum. The hormone progesterone drops significantly when the placenta separates from your uterus (after your baby is born). This drop in progesterone triggers your breasts to create milk.
This drop in progesterone triggers your breasts to create milk.
Function
What is the purpose of colostrum?
The function of your breasts, or mammary glands, is to produce milk to feed your baby. Colostrum is more than the first milk your baby consumes after birth. It's highly concentrated with nutrients and antibodies to fight infection and protect your baby. It provides a powerful, unique immunity that only it can provide. Because your baby only needs a little bit of colostrum, it also helps them learn to suck, swallow and breathe during feeding.
What are the benefits of colostrum?
Colostrum builds your baby's immune system and provides concentrated nutrition. Some of the benefits of colostrum are:
- Helps strengthen your baby's immune system.
- Helps to establish a healthy gut by coating the intestines. This helps keep harmful bacteria from being absorbed.
- Offers ideal nutrition for a newborn.
- Has a laxative effect that helps your baby clear meconium (your baby's first poop) and lessens the chance of jaundice.

- Easy to digest.
- Helps prevent low blood sugar in full-term babies.
Why is colostrum good for newborns?
Colostrum has all the nutrients your baby needs in the first few days of life. It's also packed with nutrients and vitamins to strengthen your baby's immune system.
The flow of colostrum from your nipples is slow so your baby can learn to breastfeed (nurse). Learning how to breastfeed takes practice and requires your newborn to not only learn to suck and swallow but breathe at the same time.
Does leaking colostrum mean labor is close?
Colostrum leaking from your breasts doesn't mean labor is coming. Leaking colostrum is normal and some people notice it as early as the second trimester. Some don't notice any signs of leaking colostrum while others will see dried colostrum on their nipples. If you are leaking colostrum, you can wear disposable or washable breast pads.
Can you express colostrum if you're pregnant?
Colostrum can be expressed by about week 37 in pregnancy and is beneficial for some people. Using your hands to compress your breasts in a rhythmic pattern so that milk comes out is called hand expressing. Expressing colostrum before your baby is born carries some risks like contractions or premature labor. It can be beneficial to those at risk for premature birth, low milk supply or when certain health conditions present.
Using your hands to compress your breasts in a rhythmic pattern so that milk comes out is called hand expressing. Expressing colostrum before your baby is born carries some risks like contractions or premature labor. It can be beneficial to those at risk for premature birth, low milk supply or when certain health conditions present.
Speak with your healthcare provider before you remove colostrum from your breasts. If you are leaking colostrum, it may be safe to collect and store it for when your baby is born.
Can you pump colostrum?
It's difficult to pump colostrum with a breast pump because of its thick consistency. Most people recommend and prefer using their hands to express colostrum. Hand expressing colostrum usually produces more colostrum than a pump.
Anatomy
What does colostrum look like?
Colostrum is often a deep, rich yellow or orange color, almost like the yolk of an egg. This is because it contains high levels of beta carotene. It can sometimes appear white, clear or creamy. It's a thicker consistency than breast milk (or cow's milk), but the thickness varies from person to person. Colostrum is often sticky and can contain faint traces of blood (this is normal).
It's a thicker consistency than breast milk (or cow's milk), but the thickness varies from person to person. Colostrum is often sticky and can contain faint traces of blood (this is normal).
How do I know I am making colostrum?
Your body begins producing colostrum between 12 and 18 weeks in pregnancy. Most people will produce anywhere from a tablespoon to an ounce of colostrum within the first 24 hours of delivery. This slowly increases until transitional milk comes in around the third or fourth day. In most cases, you will not know if you are making colostrum, however, it's very rare to be unable to produce colostrum. You will know if your baby is getting colostrum if he or she is maintaining their weight and wetting diapers.
How long do you have colostrum?
Your body produces colostrum for up to about five days after your baby is born. It changes to transitional milk around this time, then changes again to mature milk after about 14 days. Traces of colostrum are present in your breast milk for up to six weeks.
Conditions and Disorders
What happens if you don't produce colostrum?
Most people will produce some colostrum — not producing it is rare. It's normal to feel like nothing is coming out of your breasts and worry that your baby isn't getting enough. Your baby only needs a few teaspoons of colostrum to fill their tiny stomach.
Care
How do you store pumped colostrum?
If you and your healthcare provider decide it's safe to express and store colostrum, there are a few rules to follow. First, you should ensure the colostrum is stored in a sterile container or syringe. It can be kept in your refrigerator for about two or three days. It must be moved to a freezer after three days. Colostrum can be kept in a freezer for at least three months.
Frequently Asked Questions
How much colostrum does a newborn need?
Your newborn's tummy is about the size of a marble. They only need about an ounce of colostrum per day. This equals about a teaspoon each feeding (you can expect to feed your newborn eight to 10 times the first few days). The amount of colostrum (and then transitional milk) your baby needs increases slowly each day as their stomach expands. As your body transitions to producing regular breast milk, your milk production will increase to meet their needs.
The amount of colostrum (and then transitional milk) your baby needs increases slowly each day as their stomach expands. As your body transitions to producing regular breast milk, your milk production will increase to meet their needs.
Do I need to supplement?
No, you shouldn't need to supplement. A tiny bit of colostrum goes a long way in filling up your baby. Check with your healthcare provider to make sure your baby is gaining weight. If your baby is wetting diapers and seems pretty happy, supplementing is usually not necessary.
Is it okay to squeeze out colostrum?
Yes, it's usually OK to squeeze out colostrum once you reach full-term pregnancy (37 weeks). Check with your healthcare provider if you wish to do this prior to your baby being born. If you want to hand express colostrum for your newborn, follow these steps:
- Cup your breasts with your hand in a "C" shape. Four fingers should be under your breast and your thumb should be above your nipple.

- Use your thumb and index finger to gently squeeze your areola and nipple.
- Repeat several times and in a pattern. Apply firm pressure but do not slide your fingers. If colostrum doesn't come out, try moving your fingers to another spot.
- Colostrum should slowly flow out within minutes. It's thick and comes out in drops.
- You can repeat this a few times per day.
Please note that expressing colostrum before your baby is born carries risks. Some people can go into premature labor or begin having contractions. Talk to your healthcare provider before you express colostrum.
A note from Cleveland Clinic
Colostrum is the first milk produced by your breasts. It's rich in nutrients and high in antibodies and antioxidants. Getting started with breastfeeding can be difficult and usually requires assistance, so don't be ashamed to ask your healthcare provider for help. Breastfeeding early and often is the best way to make sure your baby gets the many benefits from colostrum. Hand expressing colostrum and feeding your baby with a syringe is also an option. Ask your healthcare team for help if feeding your baby colostrum is something you wish to do.
Hand expressing colostrum and feeding your baby with a syringe is also an option. Ask your healthcare team for help if feeding your baby colostrum is something you wish to do.
Colostrum during pregnancy | Medela
Colostrum is sometimes called liquid gold, and not only because of its color. We will tell you why this first food is so important for a newborn baby.
Share this information
Colostrum, the first milk produced at the start of breastfeeding, is the ideal nutrition for a newborn. It is very concentrated and rich in proteins and nutrients, so even in small quantities it saturates the tiny tummy of a newborn for a long time. Colostrum is low in fat and easy to digest, yet provides the baby with all the essential ingredients for an optimal developmental start. And perhaps most importantly, it plays a decisive role in the formation of the baby's immune system.
Colostrum looks thicker and yellower than mature milk. Its composition also differs in accordance with the special needs of the newborn.
Its composition also differs in accordance with the special needs of the newborn.
Colostrum fights infections
Almost two-thirds of the cells in colostrum are white blood cells, which not only protect the baby's body from infections, but also teach them to fight them themselves. 1 “White blood cells are very important for the development of immunity. They provide protection and counteract pathogenic microbes,” says Professor Peter Hartmann of the University of Western Australia, a leading lactation expert.
After giving birth, your body no longer protects the baby, and he must confront the new dangers of the world on his own. The white blood cells found in colostrum produce antibodies that can neutralize bacteria and viruses. These antibodies are especially good at dealing with indigestion and diarrhea, which is very important for very young children, whose intestines are not yet fully developed.
Colostrum supports the child's immune system and intestinal function
Colostrum is especially rich in secretory immunoglobulin A -
is the most important antibody that protects the child from diseases, but not through the circulatory system, but as a protective coating of the mucous membrane of the gastrointestinal tract. 2 “The molecules that provide the mother's immune defenses enter the mother's bloodstream into the breast, where they combine to form secretory immunoglobulin A, which is then transferred to the baby along with colostrum,” explains Professor Hartmann. “Secretory immunoglobulin A accumulates on the mucous membranes of the intestines and respiratory system of the child and protects him from diseases that the mother has already had.”
2 “The molecules that provide the mother's immune defenses enter the mother's bloodstream into the breast, where they combine to form secretory immunoglobulin A, which is then transferred to the baby along with colostrum,” explains Professor Hartmann. “Secretory immunoglobulin A accumulates on the mucous membranes of the intestines and respiratory system of the child and protects him from diseases that the mother has already had.”
Colostrum also contains many other immunological components and growth factors that stimulate the development of protective mucous membranes in the intestines of the child, and the prebiotics contained in it contribute to the formation of beneficial microflora. 3
Colostrum prevents jaundice
Colostrum not only protects against indigestion, but also has a laxative effect. This helps newborns to empty the intestines frequently, removing from it everything that was digested there in the prenatal state, in the form of meconium - dark and viscous feces.
Frequent stools in newborns also reduce the risk of jaundice. A baby is born with a high level of red blood cells that absorb oxygen from the air. As these cells break down, the liver helps to process them, producing a by-product called bilirubin. If the child's liver is not yet sufficiently formed to process it, bilirubin begins to be deposited in the body, causing jaundice. 4 The laxative properties of colostrum help the baby to remove bilirubin from the body along with the stool.
Colostrum contains vitamins and minerals
Carotenoids and vitamin A give colostrum its characteristic yellow color. . 7 Babies are usually born with a low supply of vitamin A, 8 and colostrum helps to replenish it.
"The first three days are especially important for establishing breastfeeding"
In addition, colostrum is rich in minerals, such as magnesium, which is good for the baby's heart and bones, and copper and zinc, which are involved in the development of the immune system. 9.10 Zinc also contributes to the development of the brain, and there is almost four times more zinc in colostrum than in mature milk, 10 because the brain of a newborn must develop rapidly.
9.10 Zinc also contributes to the development of the brain, and there is almost four times more zinc in colostrum than in mature milk, 10 because the brain of a newborn must develop rapidly.
Colostrum helps your baby grow and develop
Colostrum contains many other ingredients that help your baby grow and develop. The role of some of them is still unknown to scientists.
“Colostrum retains its composition for about 30 hours after the baby is born,” says Prof. Hartmann. - It contains quite a lot of proteins, because all the antibodies in its composition are essentially proteins. It is relatively low in lactose [milk sugar] and has a different fat composition than mature milk.”
In addition, colostrum is close in composition to the amniotic fluid that your baby swallowed and excreted while in the womb, making it ideal for adapting to the outside world. 11
Transition from colostrum to mature milk
Breast milk usually begins to arrive two to four days after birth. The breasts become firmer and fuller, and instead of colostrum, transitional milk is excreted, which is whiter in color and creamier in consistency.
The breasts become firmer and fuller, and instead of colostrum, transitional milk is excreted, which is whiter in color and creamier in consistency.
“The first three days are especially important for establishing breastfeeding,” says Prof. Hartmann. “If everything is done correctly during this period, lactation is likely to be good, and the baby will be able to grow normally.”
It seems unbelievable now, but in just one year your baby will be able to walk and maybe even talk. Colostrum is produced for only a few days, but makes an invaluable contribution to the development of the baby during the first 12 months, and the resulting benefits remain with him for life.
Want to know more? Read our free e-book Surprising Breast Milk Facts and article What is Transitional Milk?.
Literature
1 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology. 2 Pribylova J et al. Colostrum of healthy mothers contains broad spectrum of secretory IgA autoantibodies. J Clin Immunol. 2012;32(6):1372-1380. - Pribylova J. et al., "Healthy mother's colostrum contains a broad spectrum of secretory autoimmune antibodies to immunoglobulin A". W Clean Immunol. 2012;32(6):1372-1380. 3 Bode L. Human milk oligosaccharides: every baby needs a sugar mama. Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby." Glycobiology (Glycobiology). 2012;22(9):1147-1162. 4 Mitra S, Rennie J. Neonatal jaundice: aetiology, diagnosis and treatment. 5 Patton S et al. Carotenoids of human colostrum. Lipids. 1990;25(3):159-165. - Patton S. et al., Carotenoids in Maternal Colostrum Lipidz. 1990;25(3):159-165. 6 Gilbert C , Foster Childhood blindness in the context of VISION 2020--the right to sight. Bull World Health Organ. 2001;79(3):227-232. - Gilbert S., Foster A., "Childhood Blindness in Context VISION 2020 - the right to see". Bull World Health Organ. 2001;79(3):227-232. 7 Bates CJ. Vitamin A. Lancet. 1995;345(8941):31-35. — Bates S.J., "Vitamin A". Lancet (Lancet) 1995;345(8941):31-35. 8 World Health Organization. e-Library of Evidence for Nutrition Actions (eLENA) [Internet]. Geneva , Switzerland : WHO ; 2018 [ Accessed : 05/14/2018]. Available from Evidence-based electronic library on WHO nutrition activities ( eLENA ) [Internet]. Geneva, Switzerland: WHO; 2018 [visited 14 May 2018] Article at: [ www.who.int/elena/titles/vitamina_infants/en/ ] 9 Kulski JK, Hartmann PE. Changes in human milk composition during the initiation of lactation. AUST J EXP Biol  2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.  Br J Hosp Med (Lond). 20172;78(12):699-704. - Mitra S, Rennie J, Neonatal Jaundice: Etiology, Diagnosis, Treatment. Br J Hosp Med (Lond). 20172;78(12):699-704.
Br J Hosp Med (Lond). 20172;78(12):699-704. - Mitra S, Rennie J, Neonatal Jaundice: Etiology, Diagnosis, Treatment. Br J Hosp Med (Lond). 20172;78(12):699-704. 

10 Casey CE Studies in human lactation: zinc, copper, manganese and chromium in human milk in the first month of lactation. Am J Clin Nutr 1985;41(6):1193-1200. - Casey S.I. et al., Female Lactation Study: Zinc, Copper, Magnesium, and Chromium in Breast Milk in the Early Months of Lactation. Am J Clean Nutr. 1985;41(6):1193-1200.
11 Marlier L et al. Neonatal responsiveness to the odor of amniotic and lacteal fluids: a test of perinatal chemosensory continuity. Child Dev . 1998;69(3):611-623. - Marlier L. et al., "Newborn responses to amniotic and milk odors: testing perinatal chemosensory continuity. Child Dev. 1998;69(3):611-623.
Article "Pumping - when and how?"
There are times in the life of mother and baby when breastfeeding is either impossible or difficult for some reason. For example, a child has to be left without a mother for several hours - which means that a supply of milk is needed for him. Or in the case when the baby sucks badly at the breast, but eats well from the bottle, and pumping is the only way to feed him.
For example, a child has to be left without a mother for several hours - which means that a supply of milk is needed for him. Or in the case when the baby sucks badly at the breast, but eats well from the bottle, and pumping is the only way to feed him.
This can happen if the baby is born prematurely, and the very process of sucking the mother's breast turns out to be hard physical work for him - such an infant can also be offered expressed milk.
The same applies to the situation when the baby is ill and feeling unwell prevents him from fully sucking, as he is too weak to make the efforts necessary to "extract" breast milk. In this case, it should be expressed for 2 reasons: firstly, to provide the child with complete and optimal nutrition for him, and secondly, to maintain lactation.
Situations are different, so it is important to understand why pumping is necessary, how to do it correctly and what are the conditions for storing breast milk.
When and why to express?
Pumping is the process by which a nursing mother manually or with the help of a breast pump extracts milk from her breast.
This is not a mandatory procedure for everyone, and it does not need to be carried out after each feeding, since the milk in the female breast is formed exactly as much as is needed to saturate the baby at a certain age. Those. how much milk the baby ate in one feeding - so much will appear in the breast by the next.
But if, after applying, you also express the rest of the milk, then by the upcoming feeding it will be produced more than the child can eat - and this often leads to stagnation of milk (lactostasis).
Milk should be expressed when:
-
Having to bottle feed or supplement a baby for one reason or another. If at the same time the pediatrician did not forbid the baby to eat breast milk, then the mother needs to feed the baby expressed.
-
The baby is left without a mother for a long time. There are times when a woman needs to go away, and she cannot take the child with her. In this case, you can leave a supply of milk for several hours, after decanting it.

-
Mom is sick. It happens that during lactation a woman becomes seriously ill and is forced to take medications that penetrate into breast milk, which is strictly forbidden to give to a child. Medicines contained in milk, once in the child's body, can have an adverse effect on it. To prevent this from happening, the pediatrician will help you choose the milk formula that you need to feed the baby during the mother’s illness. Pumping in such a situation will help a woman maintain lactation until recovery.
-
Mom goes to work. A mother's return to work before the end of lactation can put her before a choice: transfer the baby to formula milk or feed it with expressed milk. Recently, more and more parents are choosing the latter option, since breast milk is much healthier than artificial nutrition.
-
Injured nipples. With improper care and attachment of the child to the breast, cracks may appear on the nipples. Feeding in this condition of the nipples becomes very painful for the mother, and then the baby should be briefly transferred to expressed milk from a bottle.
 This is useful because the nipples are less likely to get irritated when they are expressed than when they are sucked by an infant. In a few days, the nipples will heal, and it will be possible to resume feeding the crumbs directly from the breast.
This is useful because the nipples are less likely to get irritated when they are expressed than when they are sucked by an infant. In a few days, the nipples will heal, and it will be possible to resume feeding the crumbs directly from the breast. -
There is a risk of lactostasis. A child, especially in the first days after birth, is not always able to suck out all the milk. To avoid lactostasis, mom needs to express excess milk. If this is not done in a timely manner, stagnation of milk can lead to inflammation of the mammary gland - mastitis. However, you must follow all the rules of pumping and do not resort to it after each feeding: this will only increase the flow of milk.
-
Not enough milk is produced. Pumping will help normalize lactation, as it leads to an increase in the production of milk in the breast, which can be useful during a lactation crisis.
5 pumping inhibitions
In order not to harm herself and not leave the baby without breast milk, the mother must know and be sure to follow the basic rules of pumping:
-
Do not express more than 3 times a day if pumping is combined with breastfeeding because this will lead to excess milk production.
 If the mother is sick and the baby is not applied to the breast, it is necessary to express with a frequency approximately equal to the number of feedings (on average, once every 3 hours - 8 times a day).
If the mother is sick and the baby is not applied to the breast, it is necessary to express with a frequency approximately equal to the number of feedings (on average, once every 3 hours - 8 times a day). -
Do not express immediately after feeding, as this may lead to hyperlactation, ie. increased milk production.
-
Do not express "to the last drop". The main indicator by the end of pumping should be a feeling of relief in the chest. The female body regards the emptying of the breast without a trace as an increased need for milk by the child - and begins to produce more milk, which the baby cannot eat, therefore, there will be a threat of milk stagnation.
-
Do not express during the night, as this may also lead to the formation of excess milk. The main hormone responsible for milk production - prolactin - has a daily rhythm of formation, most of all it is produced at night, in response to the baby sucking or pumping.
-
Do not express on the first day after the arrival of milk.
 Usually, when lactation begins, more milk is produced than the newborn needs, and it is necessary to get rid of its excess. Therefore, just at the time of the arrival of milk, you can not express everything without a trace. If the breast is very dense, then it is recommended to express only a small amount of milk so that it becomes softer and the baby can fully capture and eat it.
Usually, when lactation begins, more milk is produced than the newborn needs, and it is necessary to get rid of its excess. Therefore, just at the time of the arrival of milk, you can not express everything without a trace. If the breast is very dense, then it is recommended to express only a small amount of milk so that it becomes softer and the baby can fully capture and eat it.
Substances that signal that milk is being produced in excess appear in the filled breast after about 1 day. If you express all the milk accumulated in the chest earlier than in a day, then it will be produced in the same amount.
Hand Expression Technique
There are two ways to express - manually and with a breast pump. Usually, each mother chooses the most convenient option for her. It is better to do it manually at home, when a woman has enough time, since the whole process will take some time. Breast pumps will help a working mother, which greatly facilitate the pumping process.
Rules for hand pumping
It is best to express milk 10-15 minutes after the end of feeding the baby. Wash your hands thoroughly beforehand. If you use any breast cream, wipe the skin and nipples with a cotton swab or pad soaked in breast milk. Prepare a wide-mouth milk container by first washing it under running water and then sterilizing it (by boiling, in a steam sterilizer or in a dishwasher).
Sit comfortably, keeping your back straight, because pumping can take some time, and an uncomfortable position can cause back pain.
Gently grasp the chest: the little finger is under the chest at the ribs, the remaining fingers are positioned so as to support the chest from below. The thumb lies on top, about 3-4 cm from the nipple. In this case, the thumb and forefinger are located opposite each other, forming the letter "C".
Use your thumb and forefinger to gently press down on your chest and hold this position for a few seconds. In no case do not bring your fingers together, they should remain in the same position, the letter "C".
In no case do not bring your fingers together, they should remain in the same position, the letter "C".
Repeat pressing, moving the palm in a circle - this way you will use all the ducts of the mammary gland.
Be patient, milk may not come out immediately, but only after a while. If you are pumping for the first time, check with your doctor or lactation consultant beforehand to show you how to proceed.
Manual pumping errors
Do not squeeze the nipple: this way you will only hurt yourself and injure the breast, and you will not express milk fully.
Do not press the palm too tightly against the skin, moving the hand across the chest so that there is no irritation and microtrauma.
Do not give up at the first unsuccessful attempts, be patient.
Breast pumps
Breast pumps make pumping much easier, as they are designed to fit all the anatomical features of the female breast.
Which one to choose? Breast pumps are divided into mechanical and electrical. In the first case, the pumping process is carried out manually: by squeezing the “pear”, the woman starts the suction mechanism. Electric models are good because they work independently: from the mains or from batteries (batteries, accumulators) and do not require additional effort on the part of the woman.
In the first case, the pumping process is carried out manually: by squeezing the “pear”, the woman starts the suction mechanism. Electric models are good because they work independently: from the mains or from batteries (batteries, accumulators) and do not require additional effort on the part of the woman.
Mom usually chooses a breast pump model according to her taste and financial capabilities. It should be borne in mind that devices powered by batteries lose power faster than devices powered by the mains.
Many women are confused by the fact that electric breast pumps are loud enough. To date, there are a large number of silent devices, which is recommended to pay attention to when buying. The most effective are electric breast pumps that express both breasts at the same time and have the option of adjusting the thrust force and suction speed.
When choosing a breast pump, pay attention to the presence of the “boil and sterilize” marking. There must be the possibility of such heat treatment of parts of the apparatus. If the model cannot be boiled and sterilized, it is better to refuse to purchase it and look for another one.
If the model cannot be boiled and sterilized, it is better to refuse to purchase it and look for another one.
Rules for expressing with a breast pump
Before pumping for the first time, carefully read the instructions for the device. Check that it is properly assembled.
Sterilize the funnel and sump (boil or use a sterilizer).
Position the funnel so that the nipple is in the center of the funnel.
The draw should be the lowest, especially at first, until the breast is accustomed to expressing with a breast pump. Each breast must be pumped until a feeling of relief, add 2 minutes to this time. On average, the process will take about 15 minutes.
Pumping, like manual pumping, should be carried out some time after feeding.
Basic mistakes when expressing with a breast pump
Incorrect position of the funnel of the breast pump can cause pain to the woman. Remember: the nipple should be located strictly in the center of the funnel of the device.
Very long pumping. Do not exceed the time required to collect milk, this can lead to hyperlactation (production of excess milk).
Very strong traction. If your breast pump has a selectable thrust function, you should use the smallest one so as not to hurt your breasts.
Care of the breast pump. A breast pump, like any machine, needs proper care. It must not be clogged so as not to contaminate the milk.
Each model has a care instruction, which you should definitely read before using the device.
When washing, always disassemble the pump completely, removing even the smallest parts. This will prevent stagnation of milk residues in them.
Before each use, sterilize all parts of the machine that come into contact with milk. This can be done with a sterilizer.
Milk defrosting
Never thaw or heat breast milk in a microwave oven. When heated in the microwave, the milk warms up unevenly, while feeding the baby can burn.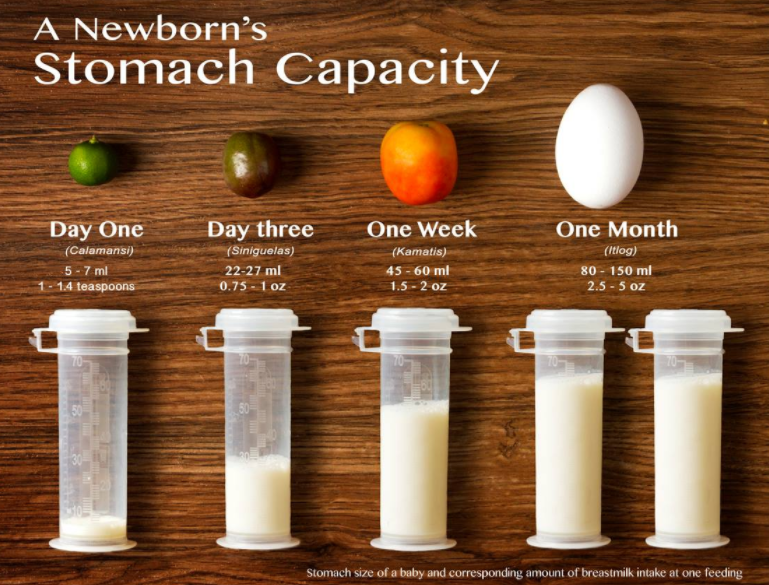 Also, due to the rapid heating of frozen milk when using a microwave, most of the useful properties of this invaluable product are lost.
Also, due to the rapid heating of frozen milk when using a microwave, most of the useful properties of this invaluable product are lost.
To defrost breast milk, place it on the refrigerator shelf, and when it becomes liquid, heat it up. To do this, lower the milk bottle into hot water or put it under hot water. Also, special heaters can be used to warm milk.
If you have questions or don't know how to express, it's worth talking to a specialist. The doctor will not only tell, but also show how to do it correctly, give recommendations on the pumping schedule and advise which method is better to choose.
Remember that milk is undoubtedly a valuable food for the baby, but feeding with expressed milk should be used in exceptional cases.
At the School of Moms, our doctors talk in detail not only about how and when to express milk correctly, but also about how to properly attach a baby to the breast, how to avoid common problems with breastfeeding, such as lactostasis, as well as about the rules of self-examination mammary glands.