How to treat cold sores while pregnant
Cold sores in pregnancy | Pregnancy Birth and Baby
Cold sores in pregnancy | Pregnancy Birth and Baby beginning of content6-minute read
Listen
What is HSV?
If you or your partner has the virus that causes cold sores or genital herpes, you might be worried about what could happen when you're pregnant or have a new baby. Here's what you need to know about herpes simplex virus (HSV), and how to protect your baby from infection.
The herpes simplex virus is a very common virus carried by most people. Sometimes it causes cold sores or genital herpes.
Cold sores are blisters that form on the lips, around the mouth and nose. Genital herpes is blisters or sores around the genitals or anus. The blisters may form a crust after about 3 days. The sores go away by themselves within 2 weeks.
There are two main types of HSV:
- HSV-1 causes mostly cold sores on the face and lips, and sometimes on the genitals
- HSV-2 causes mostly genital herpes
Both viruses are transferred though contact of the skin, saliva or genitals, and the viruses stay in the body for life. The viruses do not always cause symptoms, so you can carry the virus without knowing it.
HSV-1 is very common, with about 8 in 10 Australians carrying it in their bloodstream. But only 1 in 3 people with the virus has ever had a cold sore. HSV-2 is less common.
It is common for women who have had cold sores in the past to experience an outbreak while pregnant.
What happens if I get cold sores or genital herpes during pregnancy?
Having the HSV virus does not affect your chance of becoming pregnant.
It is quite common for women to have a cold sore during their pregnancy, even if they haven’t had one for a long time. Cold sores should not affect your unborn baby. But they are infectious, so it’s a good idea to treat them.
But they are infectious, so it’s a good idea to treat them.
Genital herpes should not affect the baby if you have your first outbreak or it comes back in the first 34 weeks. But it can be transferred to your baby during the birth, especially if it’s your first outbreak.
If you've ever had a cold sore or genital herpes and you become pregnant, or you develop these conditions during pregnancy, it's important to tell your doctor or midwife about it. Together you can make a plan for managing herpes during pregnancy and birth.
How is HSV treated during pregnancy or breastfeeding?
You can treat cold sores and genital herpes with:
- aciclovir cream, available from a pharmacist without prescription
- aciclovir or valaciclovir tablets, for which you need a prescription
These 'antiviral' drugs are known to be safe for pregnant and breastfeeding women and are effective most of the time.
Famciclovir tablets are not recommended to take during pregnancy. Speak to your doctor if the cold sore is severe.
Speak to your doctor if the cold sore is severe.
How is genital herpes treated during pregnancy?
You should take acyclovir or valaciclovir tablets, as above.
If it's your first outbreak of genital herpes, your baby may be more at risk because you haven't had time to develop immune protection against the virus, which also helps protect the baby.
Some women experiencing an outbreak of genital herpes might be advised to have a caesarean. This would prevent the herpes virus passing from mother to baby during a vaginal birth. But most women in Australia with genital herpes do give birth safely to healthy babies vaginally.
It's often recommended that women who have ever had genital herpes take antiviral tablets prior to the birth, even if the herpes isn't active at the time.
Talk to your doctor or midwife about the best course of action for your situation.
How do I protect my baby from herpes?
Herpes can cause serious problems in a baby, such as infections to the eyes and throat, brain damage and even death.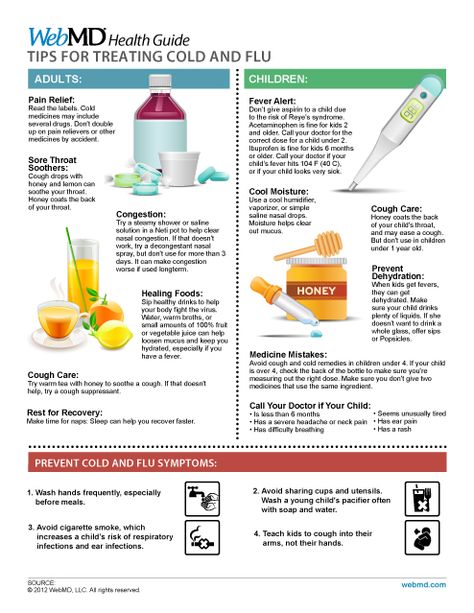
A newborn baby can catch HSV-1 and HSV-2 from being kissed or touched by someone with cold sores, or during childbirth.
Fortunately, most babies born to women who carry the virus are not affected. But if you or your partner has a cold sore or genital herpes, talk to your doctor about keeping it under control during the pregnancy and after the birth. It is also important to treat these conditions aggressively while you are breastfeeding.
It's important to maintain strict hygiene habits when caring for a new baby if you, or anyone in close contact with the baby, have cold sores.
If you have cold sores, you should:
- cover cold sores when you're around the baby
- avoid kissing your baby until the sores are completely healed
- avoid touching the cold sores then touching your baby
- wash your hands thoroughly before touching your baby
What if I have a cold sore while breastfeeding?
If you have cold sores, it is safe to breastfeed your baby as long as the cold sores are not on the breast or nipple.
If they are, it may be wise to breastfeed from the unaffected nipple only until the lesions have cleared up. You would express and dispose of breastmilk from the affected nipple. Breastmilk itself doesn't contain the herpes virus but it can be contaminated through the skin lesions.
Talk to your doctor or midwife as soon as you notice any cold sores on your breast or nipple.
What happens if my baby gets herpes?
It is very important that herpes in a newborn is recognised and treated by a doctor in hospital immediately. Signs of herpes in a newborn include:
- blisters on the skin
- fever
- irritability
- tiredness
- lack of appetite
If you think your baby might have the herpes virus, don't wait to see if they get better — seek medical help. Tell medical staff if you or your partner carry the herpes virus.
Resource and Support
If you are worried about your baby, see a doctor or midwife, or take them to the hospital.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
If you're not sure what to do or want more information, you call Pregnancy Birth Baby on 1800 882 436 to speak with a maternal child nurse.
Sources:
Family Planning NSW (Genital herpes), The Royal Woman’s Hospital (Genital herpes), Mothersafe (Cold sores in pregnancy and breastfeeding), Queensland Government Health (Genital Herpes and Pregnancy), SA Health (Cold sores (herpes simplex type 1) - including symptoms, treatment and prevention), Safer Care Victoria (Herpes simplex virus in neonates)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Need more information?
Genital Herpes (HSV) | Body Talk
Genital herpes is a common STI caused by the Herpes Simplex Virus (HSV). Find out all the facts about Genital Herpes here.
Find out all the facts about Genital Herpes here.
Read more on Body Talk website
Cold sores - Better Health Channel
Cold sores are blisters around the mouth and nose, caused by the herpes simplex virus.
Read more on Better Health Channel website
Cold sores overview - MyDr.com.au
A cold sore is a skin infection that is caused by the herpes simplex virus (HSV). Cold sores usually occur on or around the lips or nose and are very common. They have nothing to do with colds.
Read more on myDr website
Cold sores: self-care - MyDr.com.au
Cold sores are caused by the herpes simplex type 1 virus. Most people carry this virus in their bodies. Find out what products are available for cold sores.
Find out what products are available for cold sores.
Read more on myDr website
Cold sores | SA Health
Herpes simplex virus type 1 (HSV1) causes cold sores on the face or lips - it is spread by skin or mucous membrane contact with infected saliva
Read more on SA Health website
Cold sore infections - MyDr.com.au
Find the answers to common questions about cold sores, irritating blisters which are caused by the herpes simplex type 1 virus and can be triggered by stress, fatigue or exposure to sunlight.
Read more on myDr website
Cold sores: children & teens | Raising Children Network
Cold sores are quite common in older children and teenagers. Cold sores usually clear up by themselves, but see your GP if you’re concerned.
Cold sores usually clear up by themselves, but see your GP if you’re concerned.
Read more on raisingchildren.net.au website
Genital Herpes and Pregnancy
If you are pregnant and you get genital herpes, it is important to tell your midwife or obstetrician.
Read more on Queensland Health website
Genital herpes
Genital herpes is a sexually transmitted infection (STI) which shows as blisters or sores on the genitals. This is caused by the herpes simplex virus (HSV).
Read more on WA Health website
Genital herpes: what is it? - MyDr.com.au
Genital herpes is a viral infection characterised by outbreaks of blisters and sores around your genital area.
Read more on myDr website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Affect on Baby and Safe Treatments
If you’ve ever had cold sores — those annoying, painful, tiny, fluid-filled blisters that usually form around your mouth and on your lips — you know how inconvenient they can be.
But also if you’ve ever had cold sores (and therefore already have the virus that causes them), did you know they can recur, especially when you’re under stress or are undergoing hormonal fluctuations?
Stress and hormonal changes. That sounds an awful lot like pregnancy.
That sounds an awful lot like pregnancy.
Cold sores in pregnancy aren’t unheard of, and they don’t usually have any impact on your growing baby. So first, let out a deep sigh of relief. Next, read on — because there are still important things to know about cold sores if you’re expecting.
Cold sores are caused by a virus — the herpes simplex virus (HSV). Of the two types of HSV, cold sores are generally caused by HSV-1, whereas genital herpes is usually a result of exposure to HSV-2. There have been a few instances where HSV-1 sores have been found in the genitals and vice versa.
Once you’ve had a cold sore (oral herpes), the virus remains in your system for life — it’s just not active unless you have a current outbreak.
But when we say that stress and hormones can cause the virus to reactivate, it’s important to know that stress and hormones don’t cause the virus in the first place.
If you’ve never had HSV, you can only get it through contact with someone who has. When it comes to a first-time cold sore infection, this can happen via activities like:
When it comes to a first-time cold sore infection, this can happen via activities like:
- kissing
- sharing food or utensils
- using someone else’s ChapStick or lip gloss
- oral sex
Here’s the really good news: If you already have the virus that causes cold sores, and you have an outbreak of oral herpes during pregnancy, it’s most likely not going to have any impact on your growing baby.
Cold sores are a localized infection, usually around the mouth area. They don’t typically cross the placenta and reach your baby.
The highest risk scenario is if you get HSV for the first time during your third trimester of pregnancy.
When you get the virus for the first time, your body hasn’t developed any protective antibodies to it yet. And while HSV-1 is usually associated with oral herpes, it can cause a genital herpes outbreak, which can be dangerous to your baby — especially as they pass through the birth canal.
Birth-acquired herpes is serious. However, it’s a concern with genital rather than oral herpes. That being said, because the same virus can cause both, it’s important to talk to your OB about any cold sores during pregnancy.
However, it’s a concern with genital rather than oral herpes. That being said, because the same virus can cause both, it’s important to talk to your OB about any cold sores during pregnancy.
The most common treatment for cold sores is docosanol (Abreva), an over-the-counter topical cream. But the Food and Drug Administration hasn’t evaluated it for safety in pregnancy.
While some research has determined that it’s “likely safe” during pregnancy, at least one pharmaceutical company that manufactures the drug warns against using it unless it’s definitely needed — which really means you need to check with your doctor. There may be other treatments you should try first.
If you’ve had herpes in the past, your doctor may recommend antivirals — like acyclovir or valacyclovir — starting at week 36 and continuing until delivery of your baby, even if you don’t have a current outbreak of lesions around the genital area. This helps prevent reactivation and spread of the virus to the genital area.
This precaution is because you shouldn’t expose your baby to herpes in the vaginal area during delivery.
Alternatively, your doctor may suggest a cesarean delivery, which avoids the birth canal altogether — something that’s especially important if you have a current outbreak of genital herpes.
Cold sores are highly contagious, despite the fact that they won’t affect your baby in the womb. If you have them after your baby is born, avoid kissing those adorable little cheeks or touching any sores and then touching your newborn without first washing your hands with soap.
In the extremely rare event that you have cold sores on either breast, avoid breastfeeding from that breast while you’re still contagious.
Your cold sores are contagious until they crust over, at which point they’ll start to heal.
If you do pass a cold sore infection on to your newborn, it’s known as neonatal herpes. While not as serious as the birth-acquired version, it can still cause serious complications in a baby who hasn’t yet developed a robust immune system.
The cold sore on your mouth is likely to be more of an annoyance to you than a serious risk to your developing baby, particularly in your first two trimesters of pregnancy and especially if you’ve had one before. But you should still let your OB know about it.
The virus that causes cold sores — usually HSV-1 — can also cause genital herpes, which is more of a risk to your pregnancy and growing little one.
If you have an outbreak in your third trimester — or if you acquire the virus for the first time in your third trimester — your doctor may want you to follow certain treatment or precautionary guidelines, like antivirals or a cesarean delivery.
Herpes during pregnancy - consequences of lichen for pregnant women
Herpes viruses are many-sided and very dangerous for humans. Of particular concern is the infection in a woman expecting a baby.
Doctor's consultation
You can get the consultation of the necessary specialist online in the Doctis application
Laboratory
You can undergo a comprehensive examination of all major body systems nine0005
- Genital herpes in early pregnancy
- Genital herpes in late pregnancy
- Pregnancy herpes test
- Chicken pox and herpes zoster during pregnancy
- Prevention of infection of the newborn with chickenpox
- Treatment and prevention of exacerbations of herpes
There is an opinion that if a pregnant woman is infected with the herpes simplex virus, then the unborn danger! But everything is not so scary if the disease does not manifest itself (is in stable remission) or a pregnant woman with an active form of the disease is observed by an infectious disease specialist. Today approaches to maintaining patients with genital herpes changed
Today approaches to maintaining patients with genital herpes changed
Why is herpes dangerous during pregnancy
I am pregnant, short term, and I have genital herpes. Does this mean that I need to terminate the pregnancy?
No way! Genital herpes is not an indication for abortion. Virus crosses the placenta extremely rarely. But for a child, herpes is dangerous if it first appeared a month before birth. or repeated a few days before the birth, since there is a risk of infection of the baby at the time of his passage through the infected birth canal. If infected, the infant will develop severe the disease is neonatal herpes, often occurring with damage to the central nervous system. nine0005
Although during pregnancy the risk of transmission of herpes virus from mother to fetus minimal, tolerate the manifestations of genital herpes and not take antiviral drugs, being afraid the consequences of treatment for the unborn child are not worth it.
After 14 weeks of pregnancy, if genital herpes occurs, treatment with an antiviral drug is possible acyclovir. After 22 weeks, therapy with valaciclovir is possible.
In the vast majority of cases, the herpes simplex virus is transmitted from the mother child during childbirth, so the closer to the end of pregnancy there is a recurrence of genital herpes, the higher the risk of infection of the child and the more relevant the treatment of the disease. nine0037If primary genital herpes or recurrence occurs at or after 36 weeks of gestation, clinicians do not limit treatment to 5-10 days, but continue the entire period until the moment of delivery. As in the case very frequent recurrences of genital herpes during pregnancy (one outbreak in 1-2 months) - at week 36, proactive treatment with acyclovir or its analogues begins and continues until the moment childbirth. The goal of proactive treatment is to prevent recurrence shortly before delivery and to reduce the likelihood of asymptomatic carriage.
nine0005
It must be remembered that it is the asymptomatic shedding of the virus from the urogenital tract that can often be cause of infection of the child during childbirth.
Even when there seems to be no cause for concern, since the manifestations genital herpes are absent in the last months of pregnancy, still at 32-34 weeks pregnancy, it is necessary to conduct a smear (scraping) examination from the cervical canal for the presence of DNA herpes simplex virus types 1 and 2 by PCR. nine0037This analysis is necessary for primary genital herpes or its recurrence in the 1st and / or 2nd trimester, relapses genital herpes before pregnancy, relapses of genital herpes in a sexual partner, lesions urogenital tract of unknown cause, antibodies to herpes simplex virus type 1 and type 2 IgM class, detected during a routine examination during pregnancy.
For rashes or virus shedding on Wednesday within 7 days before delivery, especially in the presence of genital herpes by the beginning of childbirth, a caesarean section is performed to reduce the risk of transmission virus from mother to child.nine0037
I'm just planning a pregnancy. And I want to get rid of herpes recurrences that have been haunting me for a long time me. How do you feel about the treatment of genital herpes with interferon inducers and immunomodulators?
Widespread use of immunomodulators and interferon preparations in Russian medical centers (viferon, polyoxidonium, isoprinosine, etc.) for the treatment of herpesvirus infections is completely unreasonable. The so-called "ozone therapy" will not help the patient either. You will not find these methods in international protocols, recommendations for the treatment of viral infections in children and adults, including pregnant women women. Neither in Russia nor abroad have studies been conducted proving the effectiveness of these drugs in accordance with all international regulations. nine0005
An infectious disease specialist, a professional in his field, will never turn to immunomodulators and inducers interferon, but will look for the cause of the disease and prescribe therapy that acts on the pathogen itself - drugs acyclovir, valaciclovir or famaciclovir.With primary genital herpes for 10 days, with relapses diseases - in appropriate doses for 5 days.
Therapy should be started as early as possible at the very first signs of an exacerbation. Application possible antiherpetic drugs as a preventive treatment - 2-3 days before the expected relapse, if the patient is aware of the factors that provoke it, and for the entire period of the risk factor. If genital herpes disturbs a person more than 6 times a year and / or relapses reduce the quality of life of the patient and bring him not only physical, but also serious psychological discomfort, should be discussed with the patient long-term (at least 12 months) daily suppressive antiviral therapy (for example, valaciclovir). The effectiveness of such treatment tactics for the prevention of recurrence of herpes infection has been proven. all international rules. nine0005
Sequelae of chickenpox during pregnancy
How dangerous are chicken pox and shingles for a pregnant woman?
These diseases are caused by the varicella-zoster virus (VZV), which also belongs to the herpesvirus family.
infect women are most often children who easily tolerate the disease. At the same time, chickenpox in an adult can be severe and dangerous to his health.
Infection is transmitted by airborne droplets from person to person already 48 hours before the onset of the rash, during the entire period of the rash and for a week after appearance of the last bubbles. nine0037Expectant mothers who catch chickenpox may develop severe herpes pneumonia. Therefore, when sick chickenpox during pregnancy should be observed by an infectious disease specialist and in most cases of antiviral therapy.
In maternal varicella at 8 to 20 weeks of gestation infection fetus with the varicella-zoster virus can lead to fetal chickenpox with the development of a "syndrome congenital chicken pox" with severe malformations - damage to the brain, eyes, skeletal defects. Therefore, if a woman falls ill with chicken pox in the 1-3rd month of pregnancy, the doctor the woman should be informed about all possible risks of the disease for the fetus and discussed with her the question of a possible termination of pregnancy.
nine0005
Second and third trimesters infectious disease doctor monitors the state of the future mothers. If the infection is severe or the infection occurred in the last month of pregnancy, prescribe antiviral treatment with acyclovir or its analogues. If ultrasound does not detect fetal pathology, pregnancy is not interrupted.
Within 96 hours (preferably within the first 48 hours) after contact a pregnant woman with chickenpox in the absence of IgG class antibodies to VVZ it is possible to introduce a specific VVZ-immunoglobulin as a measure to prevent the development of the disease. Immunity persists for 3-4 weeks, may be re-introduced after 21 days. nine0037If the mother-to-be becomes ill with chicken pox in the last month of pregnancy , then the child may be born with skin rashes. If a woman falls ill in the last few days of pregnancy or in the first days after childbirth in a newborn infected during childbirth, the symptoms of chickenpox appear in the first 11 days of life.
Chickenpox is most severe in infants whose mothers fell ill 5 days before or 2-3 days after delivery. In case of chickenpox in mothers, newborn children are given a specific immunoglobulin to prevent the development of the disease. In case of its severe course - appoint acyclovir for intravenous administration. nine0005
Infection of a child with VVV a few days after birth may manifest as postnatal varicella in the period of 12-28 day of his life. This form of the disease is less severe, it is possible to introduce a specific immunoglobulin with the risk of the disease and the appointment of intravenous acyclovir for destructive skin lesions.
Vaccination against the varicella-zoster virus is not given to pregnant women because this is a live vaccine. Therefore, if a young woman does not have IgG antibodies to VVZ before planning pregnancy, it is advisable to vaccinate against chicken pox. nine0037Herpes zoster ("secondary" VVZ infection) in a pregnant woman is not dangerous for a child.
Contact seronegative pregnant woman with herpes zoster is not desirable, although the threat of her infection There is practically no VVZ.
I'm just planning a pregnancy. And I want to get rid of herpes recurrences that have been haunting me for a long time me. How do you feel about the treatment of genital herpes with interferon inducers and immunomodulators?
nine0002 Widespread use of immunomodulators and interferon preparations in Russian medical centers (viferon, polyoxidonium, isoprinosine, etc.) for the treatment of herpesvirus infections is completely unreasonable. The so-called "ozone therapy" will not help the patient either. You will not find these methods in international protocols, recommendations for the treatment of viral infections in children and adults, including pregnant women women. Neither in Russia nor abroad have studies been conducted proving the effectiveness of these drugs in accordance with all international regulations.nine0005
Infectionist, a professional in his field will never turn to immunomodulators and interferon inducers, but will look for the cause of the disease and prescribe an effective pathogen therapy - drugs acyclovir, valaciclovir or famaciclovir. With primary genital herpes for 10 days, with relapses of the disease - in appropriate doses for 5 days.Therapy should be started as early as possible at the very first signs of an exacerbation. Application possible antiherpetic drugs as a preventive treatment - 2-3 days before the expected relapse, if the patient is aware of the factors that provoke it, and for the entire period of the risk factor. If genital herpes disturbs a person more than 6 times a year and / or relapses reduce the quality of life of the patient and bring him not only physical, but also serious psychological discomfort, should be discussed with the patient long-term (at least 12 months) daily suppressive antiviral therapy (for example, valaciclovir).
The effectiveness of such treatment tactics for the prevention of recurrence of herpes infection has been proven. all international rules. nine0005
If you have any questions, you can ask your doctor obstetrician-gynecologist or infectious disease specialist online at Doctis app.
The author of the article: Vasily Iosifovich Shakhgildyan
Herpes, cytomegalovirus, Epstein-Barr virus in pregnant women
Expecting a baby is always stressful for the female body, which has to work hard for nine months. And during pregnancy, the expectant mother has a lot of reasons for unrest. Infection with any infectious disease causes serious consequences that negatively affect both the condition of the pregnant woman and the child. Let's consider these diseases in more detail. nine0005
Herpes
The concept of "herpes during pregnancy" is too broad and often becomes a cause for unreasonable panic among pregnant women who do not know what and in what cases a threat to their unborn child may appear.
It is important for a pregnant woman to have information about all the features of this disease at different stages of pregnancy in order to contact a gynecologist in time and understand when there is really a danger to the fetus when a cold appears on the lips. nine0005
If a woman in an interesting position has a recurrent form of the virus, that is, she has already encountered it before pregnancy, almost any manifestation of herpes is not dangerous for the mother and child. A simple herpes virus can only be a threat during pregnancy if it is a primary infection, especially in the early stages, when all the internal organs of the baby are laid and, most dangerously, the neural tube. Only in the case of primary infection in the early stages of pregnancy, up to the second trimester, the virus poses a threat, as it can lead to missed pregnancy, miscarriage, and developmental abnormalities. However, this clinical situation is more likely to be an exception to the rule, because most women repeatedly experience herpes before pregnancy.
nine0005
Cytomegalovirus
For a pregnant woman, the virus is dangerous during the primary infection during the expectation of a child. Infection from a sick person with an acute cytomegalovirus infection is the worst option for a pregnant woman, because due to the lack of antibodies in the blood, the virus easily crosses the placenta and has a negative effect on the fetus. According to statistics, infection of the fetus occurs in 40-50% of cases. The degree of adverse effect of the virus on the fetus depends on the duration of pregnancy. If the fetus is infected in early pregnancy, there is a high probability of spontaneous miscarriage or anomalies in the development of the child. If the infection happened at a later date, no fetal malformations are observed, but quite often polyhydramnios occurs during pregnancy, premature birth and the so-called "congenital cytomegaly" of the newborn are noted. Such children may have jaundice, enlarged liver and spleen, and anemia. nine0005
Eppstein-Barr virus
The Epstein-Barr virus predisposes to premature termination of pregnancy, fetal malnutrition, in newborn children causes damage to the nervous system, organs of vision, recurrent chroniosepsis, hepatopathy and respiratory distress syndrome.
![]()
Learn more