Dull pain pelvis
Pelvic pain - NHS
Pelvic pain is felt in the lower part of your tummy. The type of pain varies, and it may be sudden and severe (acute pelvic pain) or last 6 months or longer (chronic pelvic pain).
Symptoms of pelvic pain
Pelvic pain varies. It may affect a small area around your pelvis (your lower tummy) or the whole area.
Types of pelvic pain include:
- a sharp, stabbing or burning pain that happens suddenly
- a pain that comes on slowly but does not go away
- a dull or heavy ache, or feeling of pressure
- a twisted or knotted feeling
- a cramping or throbbing pain, which may come and go
- pain only when you’re doing something, like exercising, having sex, or peeing
Common causes of pelvic pain
There are lots of causes of pelvic pain. It might be caused by an infection or a condition affecting one of the organs in the pelvic area, such as the bowel or bladder.
Common causes include:
- constipation or irritable bowel syndrome
- urinary tract infections (UTIs)
- sexually transmitted infections (STIs)
Most causes of pelvic pain are not serious. But there a few conditions that cause pelvic pain and need emergency treatment, such as appendicitis and peritonitis.
But do not self-diagnose – see a GP if you're worried.
Pelvic pain in women
Pelvic pain is more common in women and common causes include:
- period pain
- conditions affecting female reproductive organs, such as an ovarian cyst or endometriosis
- pelvic pain in pregnancy
Rarely it could be something more serious, like an ectopic pregnancy, womb cancer or ovarian cancer.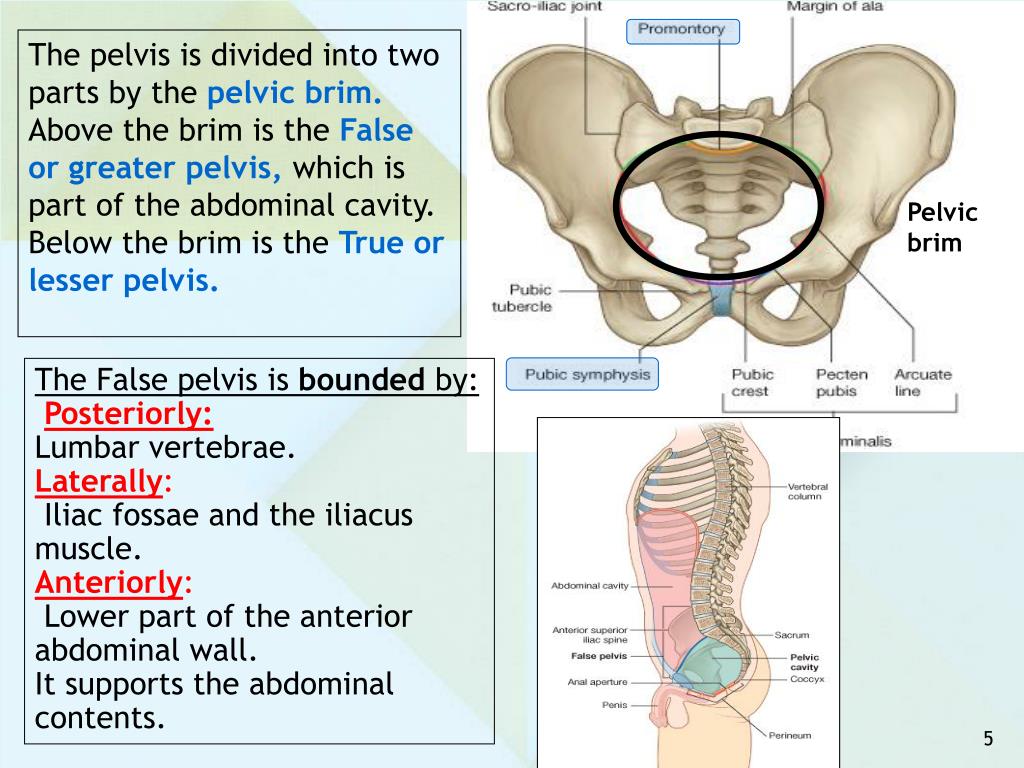
Pelvic pain in men
Pelvic pain can sometimes be caused by conditions affecting the prostate, such as prostatitis.
Non-urgent advice: See a GP if:
- pelvic pain does not go away
- you have been feeling bloated for a while (about 3 weeks)
- you're losing weight without trying to
- there's blood in your pee or poo, or an unusual discharge or bleeding from your vagina
- you have constipation or diarrhoea that does not go away
Urgent advice: Ask for an urgent GP appointment or get help from NHS 111 if:
You have pelvic pain and:
- it's severe, getting worse or hurts when you move or touch the area
- you find it difficult to pee or poo
- you have pain when peeing or need to pee more than usual
- you have a very high temperature (you feel hot and shivery)
- you are pregnant or may be pregnant
You can call 111 or get help from 111 online.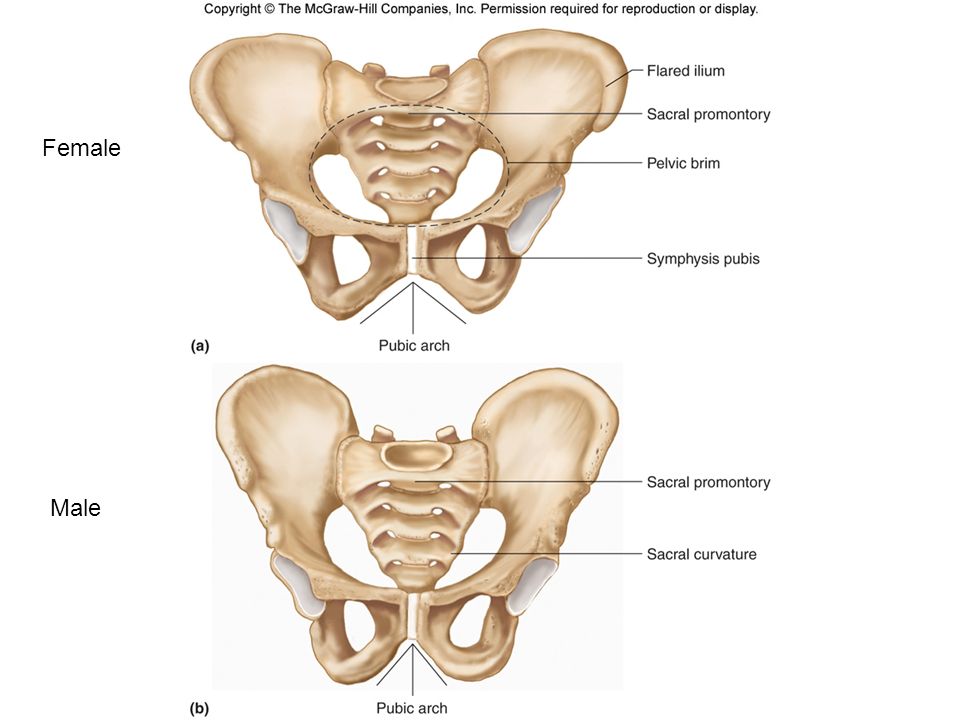
Treatments for pelvic pain
Any treatment for pelvic pain will depend on the cause.
A GP might suggest treatments such as:
- antibiotics
- painkillers
- physiotherapy, such as exercises for the pelvic floor muscles
- hormone treatments
They may refer you for tests or to a specialist if they do not know what is causing your pain.
Page last reviewed: 17 March 2022
Next review due: 17 March 2025
18 Possible Causes of Pelvic Pain in Women
If you have pain below your belly button and above your legs, it counts as pelvic pain. It can be caused by a lot of things. It may be a harmless sign that you’re fertile, a digestive disorder, or a red flag that you need to go to the hospital.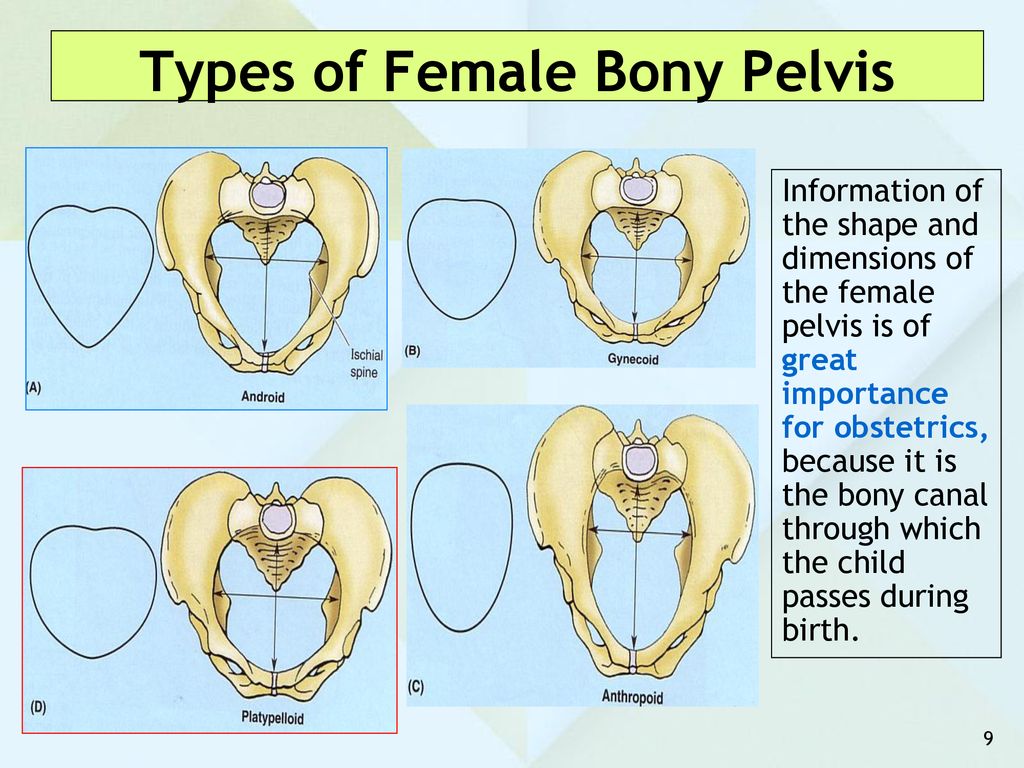
If you have a sharp pain in the lower right part of your belly, are vomiting, and have a fever, it could be appendicitis. If you have these symptoms, go to the ER. An infected appendix may need surgery. If it bursts, it can spread the infection inside your body. This can cause serious complications.
Do you have belly pain, cramps, bloating, and diarrhea or constipation that keeps coming back? Talk to your doctor to figure out the problem. It could be IBS, sometimes called spastic colon. Doctors aren’t sure what causes it. Diet changes, stress management, and medications may help.
Ever feel a painful twinge between periods? You may be feeling your body ovulate. When you do, the ovary releases an egg along with some fluid and blood. It can cause irritation. This feeling is called mittelschmerz -- German for "middle" and "pain." That’s because it happens midway through your monthly cycle. The pain may switch sides from month to month. It isn't harmful and usually goes away in a few hours.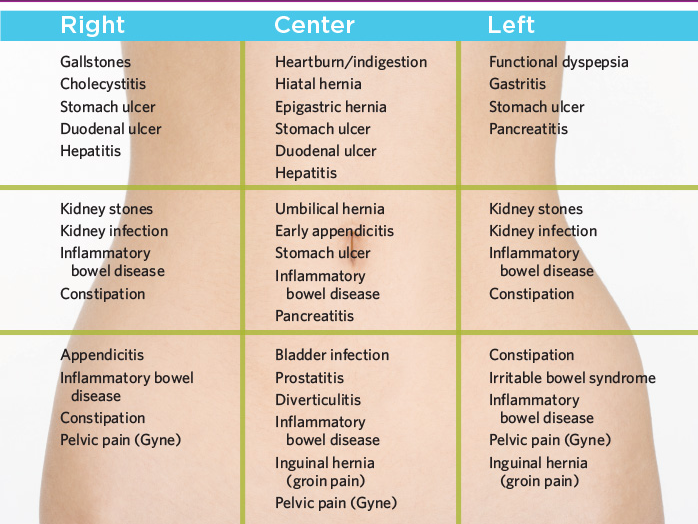
You can usually feel these cramps in your lower belly or back. They typically last 1 to 3 days. Why the pain? Every month, your uterus builds up a lining of tissue. That’s where an embryo can implant and grow. If you don't get pregnant, the lining breaks down and is shed during your period. When the uterus tightens to push it out, you get a cramp. Try a heating pad and over-the-counter pain relievers to ease pain. Exercise and de-stressing can help, too. You can also talk to your doctor about PMS pain. Certain birth control pills or antidepressants may help.
This happens when an embryo implants somewhere outside of the uterus and begins to grow. This usually happens in the fallopian tubes. Sharp pelvic pain or cramps (particularly on one side), vaginal bleeding, nausea, and dizziness are symptoms. Get medical help right away. This is a life-threatening emergency.
Pelvic pain is a warning sign of some STDs. Two of the most common are chlamydia and gonorrhea (shown here through a microscope). You often get both at the same time. They don't always cause symptoms. But when they do, you may have pain when you pee, bleeding between periods, and abnormal vaginal discharge. See your doctor. It’s also important to get partners checked and treated, too, so you don’t pass the infection back and forth.
You often get both at the same time. They don't always cause symptoms. But when they do, you may have pain when you pee, bleeding between periods, and abnormal vaginal discharge. See your doctor. It’s also important to get partners checked and treated, too, so you don’t pass the infection back and forth.
This is a complication of sexually transmitted diseases. It's the No. 1 preventable cause of infertility in women. It can cause permanent damage to the uterus, ovaries, and fallopian tubes. Belly pain, fever, abnormal vaginal discharge, and pain during sex or urination can be symptoms. Get it treated right away to avoid damage. It is treated with antibiotics. In severe cases, you may need to be hospitalized. Get your partner treated, too.
Ovaries release eggs when you ovulate. Sometimes a follicle doesn't open to release the egg. Or it recloses after it does and swells with fluid. This causes an ovarian cyst. They’re usually harmless and go away on their own. But they may cause pelvic pain, pressure, swelling, and bloating.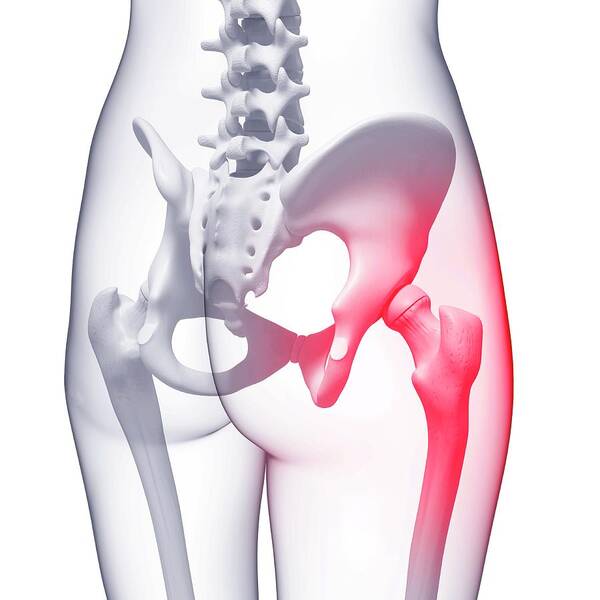 And if a cyst bursts or twists, it can cause sudden, severe pain, sending you to the emergency room. Doctors can spot them during a pelvic exam or ultrasound.
And if a cyst bursts or twists, it can cause sudden, severe pain, sending you to the emergency room. Doctors can spot them during a pelvic exam or ultrasound.
These grow on or in the wall of the uterus. While they’re sometimes called fibroid tumors, they are not cancerous. Fibroids are common in women in their 30s and 40s. They usually don’t cause problems. But some women may have pressure in the belly, low back pain, heavy periods, painful sex, or trouble getting pregnant. Talk with your doctor if you need treatments to shrink or remove them.
In some women, there is tissue growing outside the uterus that is similar to tissue that lines the uterus. It can happen on the ovaries, fallopian tubes, bladder, intestines, and other parts of the body. When it's time for your period, these clumps of tissue break down. But the tissue has no way to leave the body. While this is rarely dangerous, it can cause pain and form scar tissue that may make it tough to get pregnant. There are several treatment options.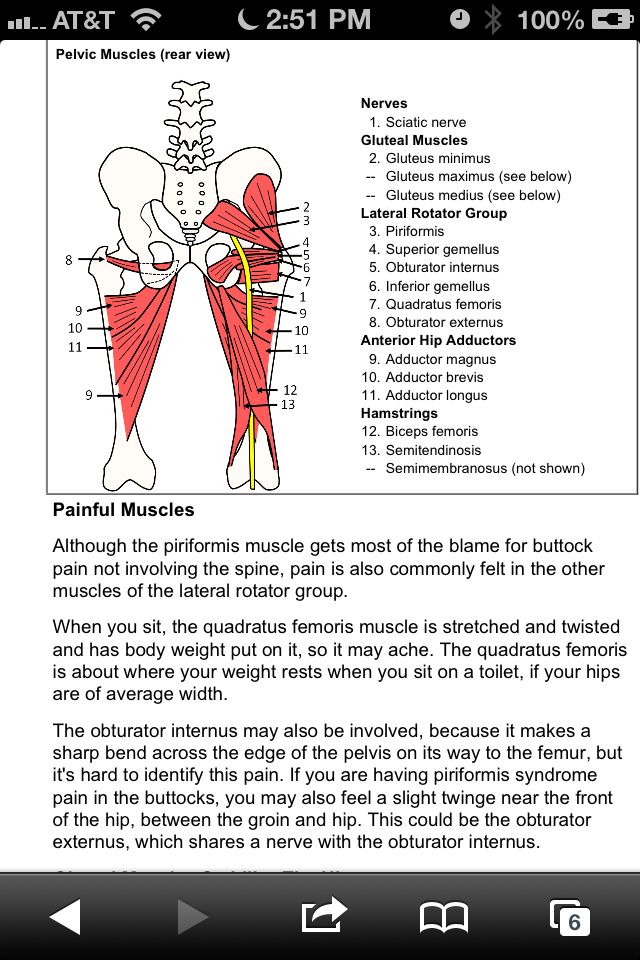 Pain medications, birth control pills, hormones to stop periods, surgery with small incisions, and even a hysterectomy (taking out your uterus) are options.
Pain medications, birth control pills, hormones to stop periods, surgery with small incisions, and even a hysterectomy (taking out your uterus) are options.
Do you have to pee often, or does it hurt when you do? Or do you feel like your bladder is full? It could be a UTI. This happens when germs get into your urinary tract. Treating it quickly can keep it from it getting serious. But if it spreads to the kidneys, it can cause serious damage. Signs of a kidney infection include fever, nausea, vomiting, and pain in one side of the lower back.
These are globs of salt and minerals that your body tries to get rid of in urine. They can be as tiny as a grain of sand or as large as a golf ball. And boy can they hurt! Your urine may turn pink or red from blood. See your doctor if you think you have a kidney stone. Most will pass out of your system on their own, but some need treatment. Even if they can pass on their own, your doctor can help with pain medication and will tell you to drink lots of water.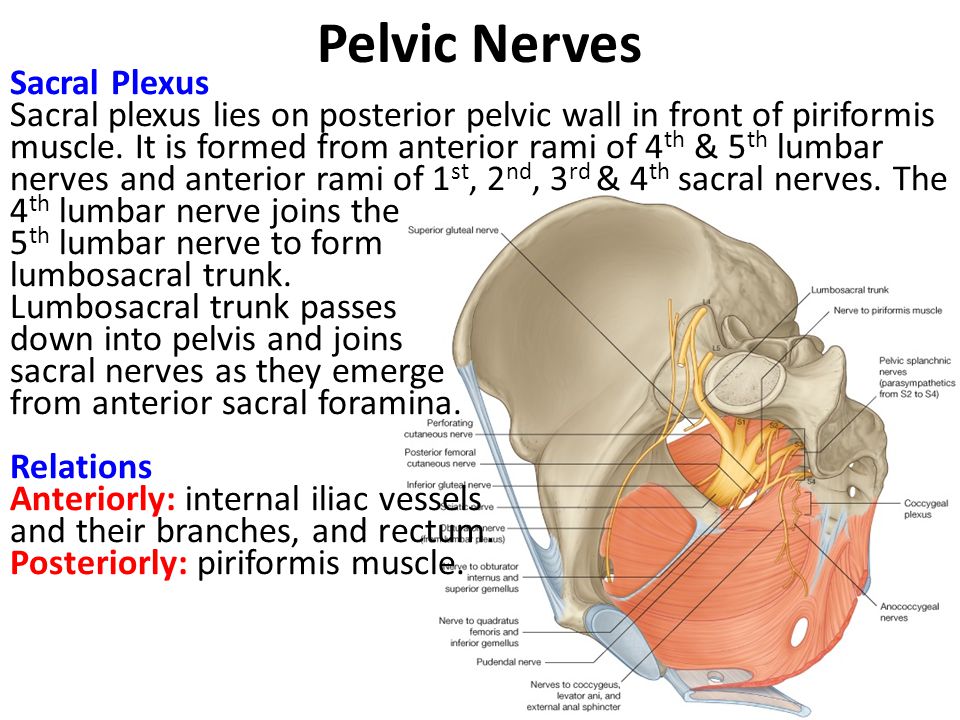
This condition causes ongoing pain and is related to inflammation of the bladder (illustrated here). It’s most common in women in their 30s and 40s. Doctors aren’t sure why it happens. People with severe IC may need to pee several times an hour. You might also feel pressure above the pubic area, pain when you urinate, and pain during sex. Although this can be a long-term condition, there are ways to ease the symptoms and avoid flares.
As you get older, this may happen. Your bladder or uterus drops into a lower position. It usually isn't a serious health problem, but it can be uncomfortable. You may feel pressure against the vaginal wall, or your lower belly may feel full. It may also give you an uncomfortable feeling in the groin or lower back and make sex hurt. Special exercises like Kegel’s or surgery may help.
We’ve all seen varicose veins in legs. (This is a picture of one in the upper thigh.) They can sometimes happen in the pelvis, too. When blood backs up in veins, they become swollen and painful.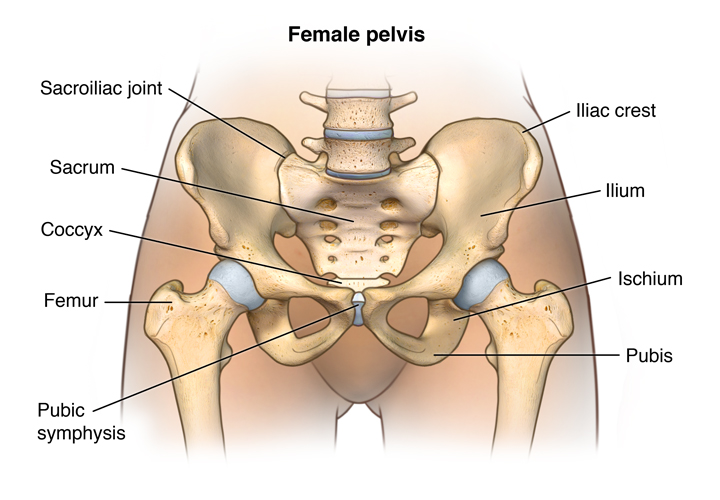 This is known as pelvic congestion syndrome. This is a condition that's difficult to diagnose and treat. It tends to hurt worse when you sit or stand. Lying down may feel better. But because the best treatment is still unclear, you need to work with your doctor to learn what the options are and to find what works well for you.
This is known as pelvic congestion syndrome. This is a condition that's difficult to diagnose and treat. It tends to hurt worse when you sit or stand. Lying down may feel better. But because the best treatment is still unclear, you need to work with your doctor to learn what the options are and to find what works well for you.
If you've had surgery or an infection, you could have ongoing pain from this. Adhesions are a type of scar tissue inside your body. They form between organs or structures that aren’t meant to be connected. Adhesions in your belly can cause pain and other problems, depending on where they are. In some cases, you may need a procedure or surgery to get rid of them.
Does it hurt when you ride a bike or have sex? If it burns, stings, or throbs around the opening of your vagina, it could be this. The feelings can be ongoing or come and go. Before you’re diagnosed with this, your doctor will rule out other causes. This isn’t caused by an infection. Treatment options range from medication to physical therapy.
This can be caused by many things. Most are treatable. It could be a vaginal infection, or you just may need more lubrication. The medical name is dyspareunia. Sometimes the pain gets better after sexual therapy. This type of talk therapy can focus on inner conflicts about sex or past abuse.
If you have pain that lasts at least 6 months, it’s considered chronic. It may be so bad it messes with your sleep, career, or relationships. See your doctor. Most of the conditions we've covered get better with treatment. Sometimes, even after a lot of testing, the cause of pelvic pain remains a mystery. But your doctor can still help you find ways to feel better.
Pain in the pelvic area - causes, examination and treatment | Symptoms
Menstrual cramps
Symptoms: Sharp or crampy pains that begin a few days before or during menstruation, are most intense within about 24 hours after the onset of menstruation and subside after 2 to 3 days, often accompanied by headache, nausea, constipation, diarrhea, or frequent urination. urination.
urination.
Endometriosis
Signs: Sharp or crampy pain that occurs before and during the first days of menstruation, often pain during intercourse and / or bowel movements. It can eventually lead to pain that is not related to the menstrual cycle.
Pain in the middle of the menstrual cycle
Signs: Severe, sharp pain that starts suddenly; can occur on either side, but only on one side each time, occurs at the same time during the menstrual cycle, usually in the middle of the cycle between periods (when the egg is released), most intense at the beginning, but then decreases over 1–2 days, there is often slight bleeding. nine0006
Pelvic inflammatory disease
Signs: Aching pain in the pelvic area, which can be felt on one or both sides. Usually a vaginal discharge that is sometimes foul-smelling and can become pus-like and yellow-green in color as the infection progresses. Sometimes pain during urination and/or intercourse, fever or chills, nausea or vomiting.
Rupture of an ovarian cyst
Signs: Pain that starts suddenly is initially limited to one area in the lower abdomen. Sometimes dizziness, fainting, slight vaginal bleeding, nausea, or vomiting occur.
Ectopic pregnancy
Signs: Persistent (not spasmodic) pain that starts suddenly, is initially limited to one area in the lower abdomen. Often slight vaginal bleeding, sometimes dizziness, fainting, fast heartbeat, or dangerously low blood pressure (shock) caused by severe internal bleeding. nine0006
Sudden degeneration fibromas in uterus
Symptoms: Sudden pain. It is most common during the first 12 weeks of pregnancy, after childbirth or abortion. Vaginal bleeding may occur.
Torsion (twisting) of the ovarian adnexa
Signs: Severe pain that starts suddenly, occurs on one side, grows rapidly. As well as intermittent pain that comes and goes (when the ovary twists and unwinds). Often occurs in pregnant women, after the use of drugs for the treatment of infertility or with an increase in the ovaries. nine0006
Often occurs in pregnant women, after the use of drugs for the treatment of infertility or with an increase in the ovaries. nine0006
Ovarian cancer / Endometrial cancer
Signs: Gradually increasing pain. Brown or bloody discharge from the vagina. Abnormal vaginal bleeding (bleeding after menopause or bleeding between periods), sometimes weight loss.
Spikes
Signs: Pain in the pelvic area, which gradually increases, often becomes chronic. As well as pain during intercourse. No vaginal bleeding or discharge. Sometimes nausea and vomiting (suggesting intestinal blockage). In women who have had abdominal surgery or in women with a pelvic infection. nine0006
Miscarriage
Signs: Spasmodic pain in the pelvis or back, accompanied by vaginal bleeding. Other signs of early pregnancy such as breast tenderness, nausea, and missed periods.
Appendicitis
Signs: Pain that usually occurs in the lower right side of the abdomen. Loss of appetite and usually nausea and vomiting. Often fever. nine0006
Loss of appetite and usually nausea and vomiting. Often fever. nine0006
Bladder infection
Signs: Pain just above the pubic bone. Sometimes an urgent need to urinate, more frequent urination, or burning when urinating.
Diverticulitis
Signs: Pain or tenderness in the left lower abdomen, fever.
Inflammatory bowel disease (including Crohn's disease and ulcerative colitis)
Signs: Cramping pain in the abdomen, diarrhea, in ulcerative colitis often with blood in the stool, loss of appetite and weight loss. nine0006
Stones in the urinary tract
Signs: Excruciating intermittent pain in the lower abdomen, side or lower back, depending on the location of the stone, nausea and vomiting, blood in the urine.
Gastrointestinal disorders (gastroenteritis, constipation, accumulation of pus; colon cancer)
Musculoskeletal disorders (pubic bone dehiscence after childbirth, fibromyalgia and abdominal muscle tension)
Psychological factors (stress and depression)
treatment, diagnosis, causes — 8(495)120-02-05
| Obstetrics and Gynecology | |
|---|---|
| Consultations of the Chief Physician | |
Primary obstetrician-gynecologist consultation (excellent student of health care, Khersonskaya E. B.) B.) | 8000.00 |
| Repeated consultation with an obstetrician-gynecologist (excellent worker in public health, Khersonskaya E.B.) | 7000.00 |
| Consultation of an obstetrician-gynecologist under the WB contract (excellent student of health care, Khersonskaya E.B.) 2022 | 6000.00 |
| Head physician remote consultation | 3000.00 |
| Chief physician's consultation on the correction of prescribed treatment | 4000.00 |
| Extended consultation of the head physician (more than 60 min.) | 9000.00 |
| CITO consultation (off-hours) | 10000.00 |
| Consulting | |
| Consultation of an obstetrician-gynecologist (Dr. Mezhlumova N.A.) | 3500.00 |
Primary obstetrician-gynecologist consultation (Dr. Fotina E.V.) Fotina E.V.) | 4500.00 |
| Obstetrician-gynecologist repeated consultation (Dr. Fotina E.V.) | 4000.00 |
| Consultation of an obstetrician-gynecologist under the WB contract (Fotina E.V.) 2022 | 3800.00 |
| Doctor's consultation on the correction of the prescribed treatment | 2000.00 |
| Obstetrician-gynecologist remote consultation | 3000.00 |
| Remote consultation of a doctor to correct the prescribed treatment | 1500.00 |
| Primary consultation with a gynecologist-reproductologist | 5000.00 |
| Repeated consultation with a gynecologist-reproductologist | 4500.00 |
| Consultation with a gynecologist-reproductologist and ultrasound to assess the ovarian reserve | 6500.00 |
| Extended consultation with a gynecologist-reproductologist and ultrasound to assess the ovarian reserve | 7000. 00 00 |
| Consultation of an obstetrician-gynecologist (Dr. Egorova A.A., Muravina E.L.) | 4000.00 |
| Consultation of an obstetrician-gynecologist (Dr. Kozlovskaya I.A.) | 4500.00 |
| Consultation of an obstetrician-gynecologist (Honored Doctor of the Russian Federation Ivanova N.V., professor Panina O.B.) | 8000.00 |
| Council of obstetricians-gynecologists (Honored Doctor of the Russian Federation Ivanova N.V. together with the chief physician Khersonskaya E.B.) | 4000.00 |
| Council of Obstetricians-Gynecologists (Chief Physician E.B. Khersonskaya together with Honored Doctor of the Russian Federation N.V. Ivanova) | 4000.00 |
| Obstetric invasions | |
| Amniotest (test for amniotic fluid leakage) | 800.00 |
| Amnisure Rapid Test | 4000. 00 00 |
| Pregnancy test | 1000.00 |
| Insertion of an unloading obstetric pessary (excluding the cost of the pessary) | 2500.00 |
| Removal of the unloading obstetric pessary (excluding the cost of the pessary) | 2500.00 |
| Gynecological procedures | |
| Gynecological smear collection (WB contract) | 500.00 |
| Collection of gynecological smear 1 category | 800.00 |
| Collection of gynecological smear 2 category | 1900.00 |
| Procedure in a gynecological room, category 1 | 1500.00 |
| Procedure in the gynecological room 2 category | 2700.00 |
| Colposcopy (video colposcopy) | 3000.00 |
| Colposcopy (video colposcopy) extended | 4500. 00 00 |
| Introduction of intrauterine contraceptives (excluding the cost of the spiral) | 2700.00 |
| Introduction of intrauterine contraceptives II degree of complexity (excluding the cost of the spiral) | 4500.00 |
| Removal of intrauterine devices (coils) | 1200.00 |
| Withdrawal of intrauterine contraceptives (spirals) II degree of difficulty | 1700.00 |
| Placement/removal of a contraceptive ring (without cost of the ring) | 800.00 |
| Placement/removal of a contraceptive ring (without the cost of the ring) II degree of complexity | 1100.00 |
| Removal of a foreign body from the vagina | 1000.00 |
| Removal of a foreign body from the vagina II degree of complexity | 1500.00 |
| Radio wave removal of single (up to 3 units) genital warts or papillomas | 2000. 00 00 |
| Radio wave removal of multiple (more than 3 units) genital warts or papillomas | 4000.00 |
| Treatment of cervical pathology by radio wave method (Surgitron device) I degree of complexity | 7000.00 |
| Treatment of cervical pathology by radio wave method (Surgitron device) II degree of complexity | 12000.00 |
| Treatment of cervical pathology by radio wave method (Surgitron device) III degree of complexity | 19000.00 |
| Cryogenic removal of single warts or papillomas of the female genital organs (up to 5 units) (nitrogen price included) | 2000.00 |
| Cryogenic removal of multiple warts or papillomas of the female genital organs (up to 10 units) (nitrogen price included) | 3000.00 |
| Chemical removal of single warts or papillomas of the female genital organs (up to 5 units) | 1000.00 |
| Chemical removal of multiple warts or papillomas of the female genital organs (up to 10 units) | 2000. 00 00 |
| Chemical destruction of cervical pathology (treatment of cervical diseases with Solkovagin) | 2500.00 |
| Opening of cervical cysts | 2000.00 |
| Opening of cervical cysts II degree of complexity | 3000.00 |
| Hysterosonography | 10000.00 |
| Hysterosonography II degree of complexity | 13000.00 |
| Uterine aspiration | 3200.00 |
| Aspiration of the contents of the uterus II degree of complexity | 4700.00 |
| Arabin obstetric pessary | 7500.00 |
| Endometrial aspiration biopsy (Pipel biopsy) | 3500.00 |
| Endometrial aspiration biopsy (Pipel biopsy) II degree of complexity | 4900.00 |
| Loop biopsy of the cervix (1 position) using the Surgitron apparatus | 2700.00 |
| Loop biopsy of the cervix (1 position) II degree of complexity using the apparatus Surgitron | 3300.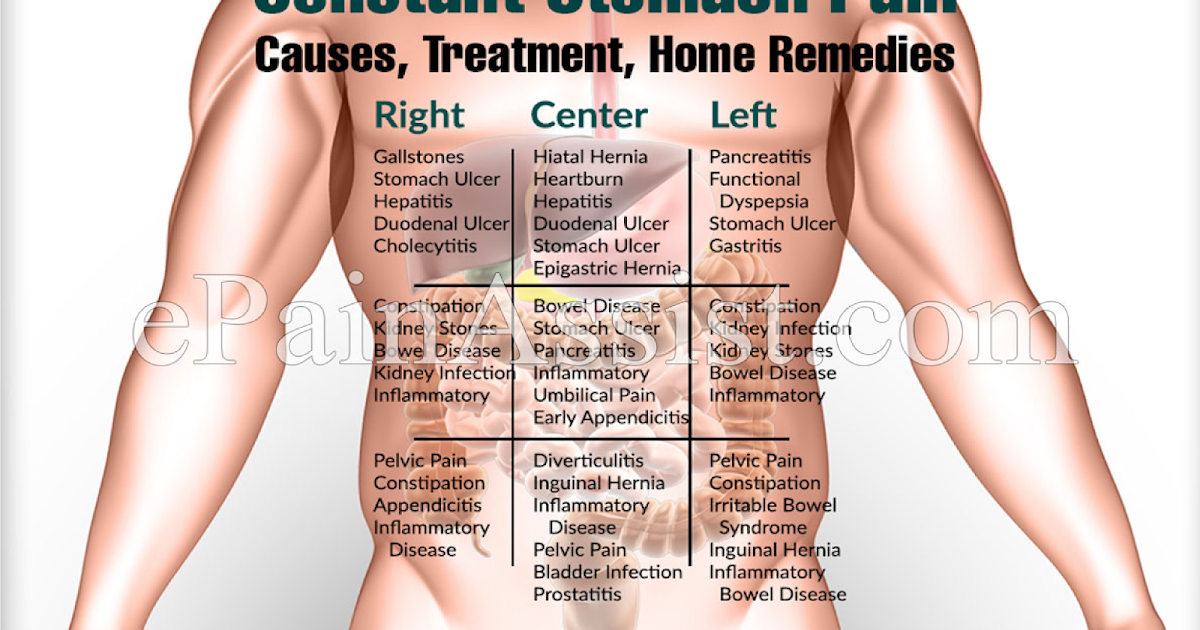 00 00 |
| Cervical scraping | 2200.00 |
| Curettage of the cervical canal II degree of difficulty | 3200.00 |
| Curettage of the cervical canal + loop biopsy of the cervix using the Surgitron device | 7000.00 |
| Curettage of the cervical canal + loop biopsy of the cervix using the Surgitron device II degree of complexity | 10000.00 |
| Curettage of the cervical canal + loop biopsy of the cervix using the Surgitron device III degree of complexity | 15000.00 |
| Hysteroscopy, separate diagnostic curettage | 16000.00 |
| Hysteroscopy, separate diagnostic curettage II degree of complexity | 19500.00 |
| Hysteroscopy, separate diagnostic curettage, IUD removal | 18000.00 |
| Hysteroscopy, separate diagnostic curettage, removal of the IUD II degree of complexity | 25500. 00 00 |
| Hysteroscopy, separate diagnostic curettage, cervical loop biopsy | 18000.00 |
| Hysteroscopy, separate diagnostic curettage, loop biopsy of the cervix II degree of complexity | 27000.00 |
| Hysteroscopy, separate diagnostic curettage, polypectomy | 20000.00 |
| Hysteroscopy, separate diagnostic curettage, polypectomy II degree of complexity | 27500.00 |
| Hysteroscopy, dissection of intrauterine synechiae | 25000.00 |
| Hysteroscopy, dissection of intrauterine synechia II degree of complexity | 37500.00 |
| Curettage of the cervical canal, removal of the polyp of the cervical canal | 10000.00 |
| Curettage of the cervical canal, removal of the polyp of the cervical canal II degree of complexity | 15000.00 |
| Instrumental IUD removal | 6000. 00 00 |
| Instrumental removal of the IUD II degree of complexity | 9000.00 |
| Cervical conization | 22000.00 |
| Conization of the cervix II degree of complexity | 25000.00 |
| Operations on the Bartholin's gland (Marsupialization, removal of the Bartholin's gland) | 15000.00 |
| Operations on Bartholin's gland (marsupialization, removal of Bartholin's gland) II degree of complexity | 22500.00 |
| Removal of stitches from the cervix | 3000.00 |
| Removal of stitches from the cervix II degree of complexity | 4500.00 |
| Removal of braces after caesarean section I category of complexity | 2500.00 |
| Removal of staples after caesarean section II category of complexity | 3500.00 |
| Removal of sutures of I category of complexity | 3000. 00 00 | nine0136
| Removal of sutures II category of complexity | 4500.00 |
| Cervicoscopy II degree of complexity | 12000.00 |
| Cervicoscopy+cervical curettage | 18000.00 |
| Cervicoscopy + curettage of the cervical canal II degree of complexity | 15000.00 |
| Polypectomy II degree of complexity | 9000.00 |
| Vaginal mass removal | 15000.00 |
| Removal of neoplasm of labia minora | 15000.00 |
| Removal of a neoplasm of the labia minora II category of complexity | 25000.00 |
| Contouring with hyaluronic acid fillers 3 ml | 40000.00 |
| Sling installation (without cost of the sling) | 55000 |
| Colporrhaphy, perineolevathoroplasty II level | |
| Colporrhaphy, perineolevathoroplasty level I | 70000 |
| Colporrhaphy II level | 70000 |
| Colporrhaphy level I | 50000 |
Hysteroresectoscopy + dissection of the uterine septum (Honored Doctor of Russia kmn Ivanova N.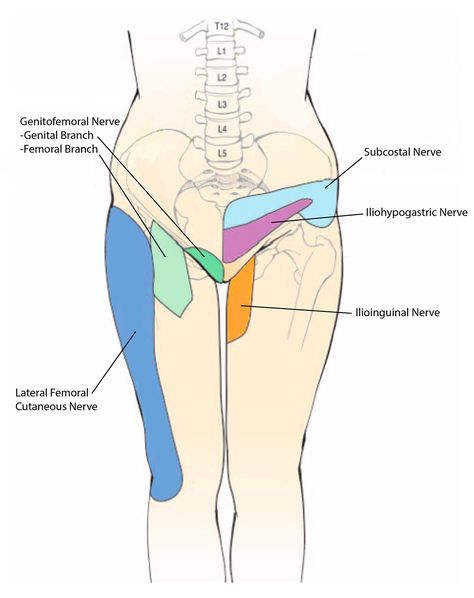 |