35 weeks pregnant cramps and pressure
Pregnancy at week 35 | Pregnancy Birth and Baby
Pregnancy at week 35 | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Your baby
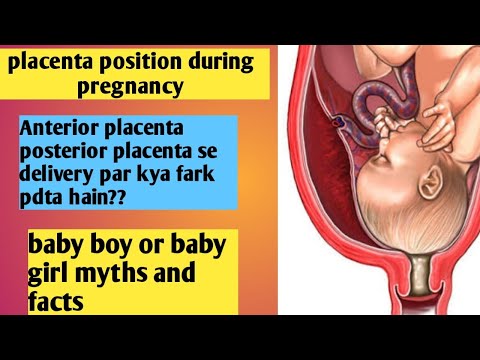
Your baby now weighs more than 2.3kg and measures about 32cm from head to bottom. They are quite cramped and their legs are bent up into their chest, but they can still change position and kick you. They can swallow about a litre of amniotic fluid every day, which is passed as urine.
Don’t worry if your baby is still in the breech position (head up, feet down) – most babies will gradually turn into the head-down position during the last month. If your baby is still in the breech position during the next week or two, your doctor or midwife may try to turn them using a procedure known as External Cephalic Version (ECV).
Your baby at 35 weeks
| Length: | 32cm (head to bottom) |
| Weight: | 2.3kg |
Your body
You may be having a lot of Braxton Hicks contractions by now. They feel like a tightening or cramping in your tummy, and they can happen as often as every 10 to 20 minutes in late pregnancy. They are your body’s way of preparing for the birth and are nothing to be worried about. You can tell if they’re Braxton Hicks and not real contractions because they normally go away if you move position.
They may be real contractions if:
- they get stronger or closer together
- they last longer as time goes by
- they are stronger when you walk
- you feel pain or pressure in your pelvis, abdomen or lower back
If you went into labour now it would be considered premature labour and you would need medical attention straight away. If you’re in doubt, contact your doctor or midwife.
If you’re in doubt, contact your doctor or midwife.
Things to remember
If your pregnancy is high risk, your doctor or midwife will probably want to see you more often from now on.
One serious complication that can develop in late pregnancy is pre-eclampsia. This is usually diagnosed if your doctor notices you have high blood pressure or protein in your urine.
See your doctor straight away if you develop:
- a bad headache
- pain in the tummy
- blurry vision
- sudden swelling of your hands or feet
Read next
Your pregnancy at 36 weeks
Learn about your pregnancy journey and what is happening to you and your baby.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Raising Children Network (Pregnancy week-by-week), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Breech Presentation at the End of your Pregnancy), NHS (You and your baby at 35 weeks pregnant), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2020
Back To Top
Need more information?
Pregnancy at week 34
As at the start of your pregnancy, you’re probably feeling tired and emotional. The baby doesn't have much room to move, but you might feel them kick and roll.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 39
Your baby's weight gain should slow down since they are now ready to be born. You might soon start to notice the early signs of labour.
Read more on Pregnancy, Birth & Baby website
Pregnancy and travel - Better Health Channel
Travelling to developing nations is not encouraged during pregnancy, due to the risk of disease and the standard of medical facilities.
Read more on Better Health Channel website
Multiple birth - triplets or more
If you are pregnant with triplets or more, the birth will need careful planning. The main risk is that your babies will be born prematurely. Find out more here.
Read more on Pregnancy, Birth & Baby website
Episiotomy
An episiotomy is a procedure performed during labour to assist with the delivery of your baby.
Read more on Pregnancy, Birth & Baby website
The role of exercise in improving fertility, quality of life and emotional wellbeing
Being in the healthy weight range reduces the risk of infertility and improves the chance of conceiving spontaneously and with assisted reproductive technology (ART).
Read more on Your Fertility website
Undescended testicles - Better Health Channel
Undescended testicles means that one or both testicles are missing from the scrotum.
Read more on Better Health Channel website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Baby, Symptoms & Cramping • Kopa Birth®
Welcome to week 35 pregnancy! You are likely busy getting ready for your little one’s arrival, and it’s finally right around the corner. Let’s talk about your baby, your pregnancy symptoms, and discuss cramping you may experience late in pregnancy and when you should take it seriously.
Estimated reading time: 7 minutes
Updated August, 24, 2021
Table of contents
- Week 35 Pregnancy: Baby
- Variation in Baby’s Size
- Week 35 Pregnancy: Symptoms
- Leg and Foot Swelling
- When is Swelling a Problem?
- Numbness
- Snoring
- Pelvic Pain or Pressure
- Leg and Foot Swelling
- Week 35 Pregnancy: Cramping
- Preterm Labor Cramps
- When to Call Your Doctor
- Preterm Labor Cramps
Week 35 Pregnancy: Baby
Your baby is getting so big! At 33 weeks from conception, he or she now weighs over 5 1/4 pounds, and is about 13 1/4 inches from crown to rump or 18 1/4 inches in total length (1).
In other week 35 baby news:
- The lungs are getting close to maturity
- The circulatory system is complete
- The musculoskeletal system is complete (2)
You continue to grow right along with baby! You have probably gained between 24 to 29 pounds, and your uterus now reaches 6 inches above your belly button.
Variation in Baby’s Size
As we’ve talked about baby’s size through your pregnancy, we’ve used general numbers that approximate baby’s size at each stage. These are more accurate in the beginning, as babies all begin development on the same schedule.
Later in pregnancy, though, there is more variation. Your baby’s genetics are a factor — if all members of your family are tall, your baby may be longer than average length already. Weight also varies, and your baby may especially be heavier if you gained more weight than average or if you have untreated gestational diabetes. Baby’s size is almost never a problem for a natural delivery, but if your doctor has any concern, he or she may use ultrasound to get a general idea of baby’s weight. But please note, estimates of baby’s weight performed late in pregnancy are often inaccurate and can lead to unnecessary labor inductions or cesarean sections.
Read more: Natural Childbirth, Large Baby: Worried? Read This.
Week 35 Pregnancy: Symptoms
Leg and Foot Swelling
Most pregnant women experience swelling in their legs and feet during pregnancy. By week 35 of your pregnancy, it’s probably a symptom that you’re quite familiar with. You may feel like you don’t have ankles anymore or that your feet look like swollen sausages. Your skin may feel tight and uncomfortable.
To relieve the swelling, stay off of your feet as much as possible, and when you do sit or lie down, prop your legs up (2). This is the time to opt for comfortable shoes. Slip-ons may be easier than shoes you need to tie as it becomes harder for you to bend and reach your feet. You also want to make sure that your shoes have enough room to accommodate your feet by the end of the day when they may be swollen and larger than in the morning.
When is Swelling a Problem?
Sudden, severe swelling can be a symptom of preeclampsia, a serious problem. Call your doctor or midwife right away if you notice sudden swelling, swelling in your face, or swelling that’s accompanied by pain, a headache that won’t go away, or blurry vision.
Numbness
You may notice numbness or tingling in your hands, fingers, or toes. It’s a strange feeling, but not worrisome. It’s a result of your body’s tissues swelling due to extra the extra fluids of pregnancy, and then pressing on your nerves (2). Some women even develop carpal tunnel syndrome, which is caused by the compression of a nerve within the carpal tunnel in the wrist. (We discuss carpal tunnel syndrome in our Week 30 Pregnancy article.) These feelings of numbness, tingling, and pain usually go away after your baby is born and your tissues return to normal.
Snoring
More than a third of women snore during pregnancy (1). Snoring is caused by your upper airway relaxing and closing partway during sleep, making it harder to get air in and out. Pregnancy adds the extra factor of swollen nasal passages, which exacerbates the problem. You may find that it helps to sleep partly upright, like in a recliner, which makes gravity work for you instead of against you. If you have concerns about your snoring or feel like you’re struggling to breathe properly, talk to your healthcare provider.
If you have concerns about your snoring or feel like you’re struggling to breathe properly, talk to your healthcare provider.
Pelvic Pain or Pressure
You may be feeling an increase in pressure or even pain in your pelvis. A couple of things may be happening that could cause these sensations. First, as you get into the final stretch of pregnancy, the joints throughout your body loosen even more. This loosening will help your baby fit through the birth canal, so it’s beneficial to you. However, it also means that you may feel increased aches and pains throughout your body, especially in your pelvis and lower back. (The increasingly loose joints paired with the ever-growing bump may also make you feel like your walk has turned into a waddle.)
In the last month or so of pregnancy, baby may also settle lower in your pelvis, which is called lightening or the baby dropping. For some women, this doesn’t occur until labor, but for others, it happens weeks before baby is born. You may see a distinct difference in the shape of your baby bump. And you may feel a difference in your ability to take a deep breath or eat a meal without discomfort (thanks to baby moving lower and therefore not pushing up into your lungs and stomach.) Unfortunately, the downside is that around 20% of women have pelvic pain (4) as baby’s large, bony head sits lower the your pelvis, putting pressure on both bones and nerves. You may find it helpful to rest with your feet up, lie down when you have the chance, and wear a pregnancy support belt.
You may see a distinct difference in the shape of your baby bump. And you may feel a difference in your ability to take a deep breath or eat a meal without discomfort (thanks to baby moving lower and therefore not pushing up into your lungs and stomach.) Unfortunately, the downside is that around 20% of women have pelvic pain (4) as baby’s large, bony head sits lower the your pelvis, putting pressure on both bones and nerves. You may find it helpful to rest with your feet up, lie down when you have the chance, and wear a pregnancy support belt.
Week 35 Pregnancy: Cramping
This late in pregnancy, moms often scrutinize every cramp carefully, wondering if it may be the beginning of labor. Although cramping most often isn’t always related to labor contractions, it’s a good idea to pay attention to your body’s signals as you approach the last few weeks of pregnancy.
Preterm Labor Cramps
Preterm labor is one that begins before week 37 of pregnancy. At 35 weeks, baby may still be immature and underdeveloped, so it’s often best to halt labor contractions at this point in the pregnancy.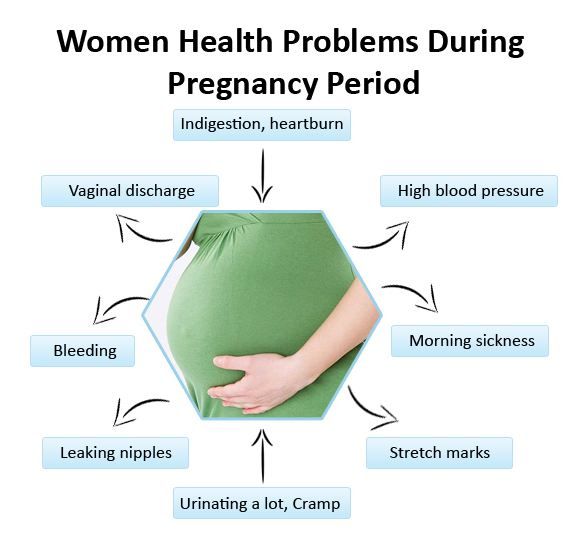
Preterm labor cramps can be difficult to distinguish. You might experience mild to moderate abdominal cramping, similar to menstrual cramps. This may or may not be accompanied by discomfort in your thighs (3). This feeling may come and go. It may eventually progress into distinct contractions, or it may stop altogether.
When to Call Your Doctor
When it comes to preterm labor, it’s best to err on the side of caution. Call your doctor or midwife if you’re experiencing any 2 of the following symptoms:
- At least 6 contractions in an hour
- Menstrual-like cramps that are continuous or come and go, and are accompanied by a feeling of pressure
- A dull lower back ache that won’t go away
- Intestinal cramping without any diarrhea
- A noticeable change in vaginal discharge (blood-tinged, lots of mucus, etc.)
Also, pick up the phone if cramping is severe, comes with a fever or dizziness, or is accompanied by bleeding.
Check back in soon to learn all about week 36 of your pregnancy!
Kopa Birth’s online birthing classes allow you to prepare for a natural hospital birth from the comfort of your own home, 24/7.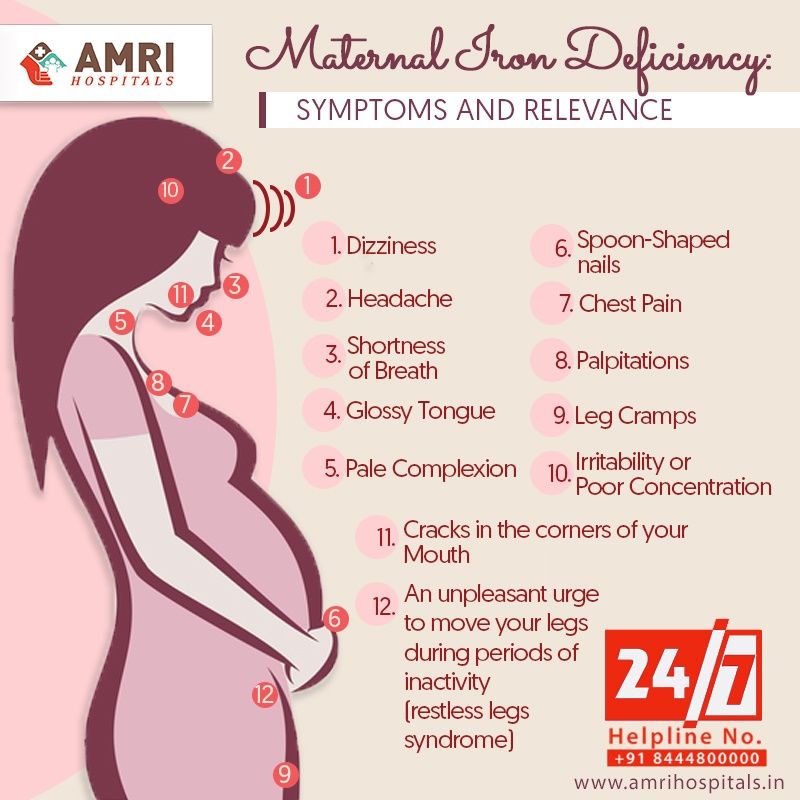 Enroll today in our free online childbirth class and start preparing for your natural birth!
Enroll today in our free online childbirth class and start preparing for your natural birth!
References:
- Glade, B.C., Schuler, J. (2011). Your Pregnancy Week by Week, 7th edition. First Da Capo Press
- The American College of Obstetricians and Gynecologists. (2010). Your Pregnancy and Childbirth Month to Month, 5th edition
- Simkin, P. (2010). Pregnancy, Childbirth and the Newborn, 4th edition. Meadowbrook Press
- Pennick V, Liddle SD. Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database of Systematic Reviews 2013, Issue 8. Art. No.: CD001139. DOI: 10.1002/14651858.CD001139.pub3.
Here are some other birth articles and stories we know you’ll love.
Hypertension in pregnancy
High blood pressure during pregnancy
Changes in blood pressure (BP) in women during pregnancy are observed quite often, which can adversely affect the mother and fetus. Blood pressure is one of the most important indicators of the functioning of the circulatory system in the body. During pregnancy, all organs and systems of the mother work with increased stress, especially the cardiovascular system. Therefore, it is necessary to regularly measure blood pressure to prevent the development of severe complications. At the beginning of pregnancy, blood pressure, as a rule, decreases slightly, which is associated with the action of hormones. In later pregnancy, as the fetus grows and blood flow increases to feed it, blood pressure may increase relative to pre-pregnancy physiological values. Hypertension is said to occur when a pregnant woman's blood pressure exceeds 140/9.0 mmHg However, in women with low blood pressure before pregnancy, arterial hypertension may be at blood pressure levels that are usually considered normal. Therefore, it is important to know your normal blood pressure.
Blood pressure is one of the most important indicators of the functioning of the circulatory system in the body. During pregnancy, all organs and systems of the mother work with increased stress, especially the cardiovascular system. Therefore, it is necessary to regularly measure blood pressure to prevent the development of severe complications. At the beginning of pregnancy, blood pressure, as a rule, decreases slightly, which is associated with the action of hormones. In later pregnancy, as the fetus grows and blood flow increases to feed it, blood pressure may increase relative to pre-pregnancy physiological values. Hypertension is said to occur when a pregnant woman's blood pressure exceeds 140/9.0 mmHg However, in women with low blood pressure before pregnancy, arterial hypertension may be at blood pressure levels that are usually considered normal. Therefore, it is important to know your normal blood pressure.
Why is high blood pressure dangerous during pregnancy?
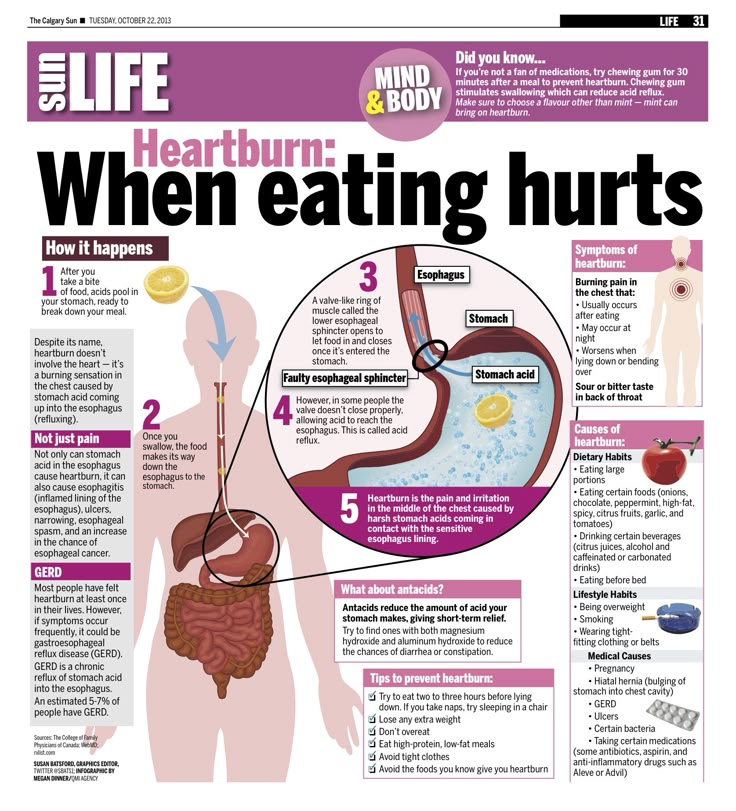
High blood pressure during pregnancy poses a great danger to the mother and fetus. Against this background, vasoconstriction occurs and the blood supply to all vital organs, including the placenta, is disturbed. Due to the lack of essential nutrients and oxygen, the process of growth and development of the fetus slows down. There is a serious danger of placental abruption, which is accompanied by bleeding and threatens the life of the mother and fetus. High blood pressure during pregnancy can lead to the development of a dangerous pregnancy complication - preeclampsia. Edema, large weight gain, and the presence of protein in the urine can also be a manifestation of preeclampsia. Very dangerous symptoms of preeclampsia are: headache, blurred vision ("flies", "veil" before the eyes), pain in the upper abdomen. Deterioration of the general condition may be accompanied by dizziness, tinnitus, nausea, vomiting. Pre-eclampsia can provoke a formidable complication - eclampsia. In this condition, the pregnant woman loses consciousness and convulsions occur. nine0005
Against this background, vasoconstriction occurs and the blood supply to all vital organs, including the placenta, is disturbed. Due to the lack of essential nutrients and oxygen, the process of growth and development of the fetus slows down. There is a serious danger of placental abruption, which is accompanied by bleeding and threatens the life of the mother and fetus. High blood pressure during pregnancy can lead to the development of a dangerous pregnancy complication - preeclampsia. Edema, large weight gain, and the presence of protein in the urine can also be a manifestation of preeclampsia. Very dangerous symptoms of preeclampsia are: headache, blurred vision ("flies", "veil" before the eyes), pain in the upper abdomen. Deterioration of the general condition may be accompanied by dizziness, tinnitus, nausea, vomiting. Pre-eclampsia can provoke a formidable complication - eclampsia. In this condition, the pregnant woman loses consciousness and convulsions occur. nine0005
Register for pregnancy at the antenatal clinic as early as possible!
A very important feature of arterial hypertension during pregnancy is that often even with high blood pressure numbers, the patient feels normal. High blood pressure is detected by chance, at the next appearance in the antenatal clinic. The absence of clinical manifestations of elevated blood pressure does not exclude the development of dangerous complications.
High blood pressure is detected by chance, at the next appearance in the antenatal clinic. The absence of clinical manifestations of elevated blood pressure does not exclude the development of dangerous complications.
In order to detect unwanted deviations during pregnancy in time and prevent the development of complications in the mother and fetus, pregnant women need to regularly monitor their blood pressure. It is very important to register for pregnancy in a antenatal clinic in a timely manner. The doctor will promptly detect changes in blood pressure and prescribe the optimal therapy to maintain blood pressure in the normal range. If a woman had high blood pressure before pregnancy, and she is taking medications, it is necessary to adjust the treatment and individually select the drugs that can be taken during pregnancy. To prevent high blood pressure, a pregnant woman should eat a healthy and balanced diet, observe a drinking regimen, and monitor weight gain. The correct recommendations on these issues will also be given by the doctor of the antenatal clinic.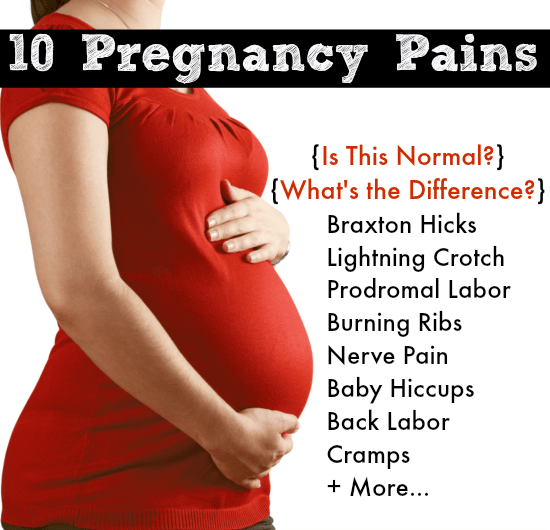 A pregnant woman must follow the recommendations and not violate the prescribed therapy. nine0005
A pregnant woman must follow the recommendations and not violate the prescribed therapy. nine0005
What to do if a pregnant woman has high blood pressure?
If a pregnant woman regularly monitors blood pressure on her own and notices even a slight increase with good health, she should visit the doctor of the antenatal clinic as soon as possible (before the scheduled next visit). Self-administration of drugs in this case is strictly prohibited. Before visiting a doctor, you can lower blood pressure by taking a mild sedative based on motherwort or valerian. nine0005
If necessary, you can consult with an obstetrician-gynecologist of the remote medical advisory panel of the Ambulance and Emergency Medical Care Station. A.S. Puchkov, Moscow by phone: (495) 620-42-44.
When is it necessary to call an ambulance?
If blood pressure rises suddenly, you feel unwell, urgent hospitalization is necessary, and it is advisable for the patient to immediately call an ambulance team. Such signs as: headache, feeling of flashing dots or "flies", a veil before the eyes, pain in the upper abdomen, nausea, vomiting, agitation or depression, along with this - an increase in blood pressure should alert. There may be a high convulsive readiness, which is manifested by twitching of the muscles of the face, neck, upper limbs, loss of consciousness, convulsions are possible. nine0005
Such signs as: headache, feeling of flashing dots or "flies", a veil before the eyes, pain in the upper abdomen, nausea, vomiting, agitation or depression, along with this - an increase in blood pressure should alert. There may be a high convulsive readiness, which is manifested by twitching of the muscles of the face, neck, upper limbs, loss of consciousness, convulsions are possible. nine0005
What to do before the ambulance arrives?
First of all, go to bed, if possible, eliminate all unwanted irritants (turn off all sources of noise, close the curtains), do not leave the pregnant woman alone, as convulsions may occur and help will be needed. Give it a position with a raised head end. It is possible to take pressure-lowering drugs prescribed by a doctor. If a woman has not previously taken antihypertensive drugs, then drugs should not be taken on the advice of others. nine0005
In the event of an attack of convulsions, the pregnant woman should be laid on a flat surface, turn her head to the side (to prevent aspiration of vomit), protect from damage (cover with a blanket), do not hold physically. After an attack, clean the oral cavity with a napkin from vomit, blood and mucus. Wait for the ambulance to arrive!
After an attack, clean the oral cavity with a napkin from vomit, blood and mucus. Wait for the ambulance to arrive!
The ambulance will arrive quickly and provide the necessary assistance. Hospitalization in this condition is mandatory. Only in a hospital is it possible to fully monitor the condition of the mother and child, complete therapy and determine the delivery plan. nine0005
We wish you health and happy motherhood!
Chief Specialist
in Obstetrics and Gynecology Arkhipova N.L.
Is it safer to induce labor immediately or wait if the mother has elevated but not persistently high blood pressure after 34 weeks of pregnancy?
What is the problem?
Women with high blood pressure (hypertension) during pregnancy or who develop preeclampsia (high blood pressure with protein in the urine or involvement of other organs or systems, or both) can develop serious complications. Possible maternal complications include worsening preeclampsia, seizures and eclampsia, HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet count), placental abruption, liver failure, kidney failure, and breathing problems due to fluid buildup in the lungs. . nine0005
. nine0005
Delivery usually prevents worsening of hypertension, but a premature baby has other health problems, such as respiratory problems due to lung immaturity. Inducing labor can lead to overstimulation of contractions and fetal distress. Another option is to wait for natural childbirth, carefully monitoring the condition of the mother and child.
Why is this important?
Because there are benefits and risks to both planned preterm birth and expectant management when the mother has high blood pressure towards the end of pregnancy, we wanted to know which was the safest strategy. We reviewed clinical trials that compared planned preterm delivery by induced labor versus caesarean section versus expectant management. nine0005
What evidence did we find?
We searched for evidence up to 12 January 2016 and found five randomized trials involving 1819 women. The two studies were large and of high quality and included 704 women with gestational hypertension, mild preeclampsia, or exacerbation of existing hypertension at 34–37 weeks, and 756 pregnant women with hypertension or mild preeclampsia at 36–41 weeks.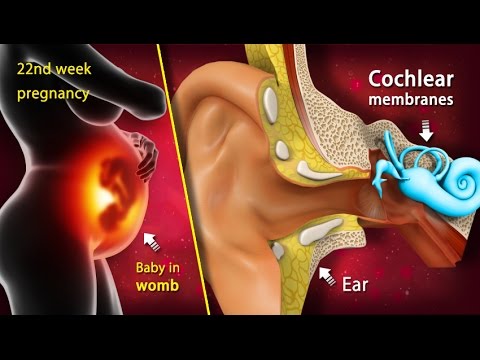 . Few women who had planned preterm births experienced serious adverse outcomes (1459women, high-quality evidence). There was insufficient information to draw any conclusions about the number of children born with poor health and there was a high level of variability between the two studies (1495 infants, low-quality evidence). No difference was found between early planned births and delayed births in terms of the number of caesarean sections (four studies, 1728 women, moderate quality of evidence), or the length of time mothers spent in hospital after delivery (two studies, 925 women, moderate quality of evidence) (or child (one study, 756 infants, moderate quality of evidence). Most preterm infants had respiratory problems (respiratory distress syndrome, three studies, 1511 infants) or were admitted to the neonatal unit (four studies, 1585 infants). A small number of women who gave birth prematurely developed HELLP syndrome (three studies, 1628 women) or serious kidney problems (one study, 100 women).
. Few women who had planned preterm births experienced serious adverse outcomes (1459women, high-quality evidence). There was insufficient information to draw any conclusions about the number of children born with poor health and there was a high level of variability between the two studies (1495 infants, low-quality evidence). No difference was found between early planned births and delayed births in terms of the number of caesarean sections (four studies, 1728 women, moderate quality of evidence), or the length of time mothers spent in hospital after delivery (two studies, 925 women, moderate quality of evidence) (or child (one study, 756 infants, moderate quality of evidence). Most preterm infants had respiratory problems (respiratory distress syndrome, three studies, 1511 infants) or were admitted to the neonatal unit (four studies, 1585 infants). A small number of women who gave birth prematurely developed HELLP syndrome (three studies, 1628 women) or serious kidney problems (one study, 100 women). nine0005
nine0005
Two studies compared women with preterm labor at 34 to 36 weeks and 34 to 37 weeks of gestation with a control group who followed up to 37 weeks when labor was induced if it did not start spontaneously. Three studies compared women in induced labor with a normal or near-normal duration of pregnancy at 37 completed weeks and between 36 and 41 weeks and women seen before 41 weeks when labor was induced if they didn't start spontaneously. Inclusion and exclusion criteria also differed across the five studies. nine0005
Information regarding which study group women belonged to was not withheld from both women and clinicians. Women and staff were made aware of this intervention, which could affect aspects of care and decision making. Most of the evidence was of moderate quality, so we can be relatively confident in the results.
What does this mean?
In general, if labor was induced immediately after 34 weeks of gestation, the risk of complications for the mother was lower and there was generally no apparent difference in the rate of complications for the baby, but information was limited.