What does iol mean in pregnancy
Induction of labour (IOL) | CUH
Induction of labour workshop
The Rosie Hospital now offers a virtual workshop for anyone who has an induction of labour booked with us.
Book your place
Introduction
This leaflet aims to give you information about induction of labour (IOL), the main reasons for induction, methods by which labour can be induced and to help you understand your choices so that you can be involved in decision making about you and your baby. It includes information about:
- Why induction of labour may be offered.
- How we induce labour.
- What to expect if being induced.
- What to expect if not being induced.
How your body changes before and during labour
During the pregnancy, your baby is surrounded by a fluid filled membrane, which offers protection whilst he or she is developing in the uterus (womb). The fluid inside the membrane is called amniotic fluid. In preparation for labour the cervix (neck of the womb) softens and shortens. This is sometimes referred to as ‘ripening of the cervix’. Before, or during labour, the membranes rupture (break) releasing the fluid. This is often referred to as ‘your waters breaking’. During labour, the cervix dilates (widens) and the uterus contracts to push your baby out.
The exact mechanism of the start of labour is uncertain but is thought to involve a complex interaction of factors between mother and baby.
In most pregnancies labour starts naturally between 37 and 42 weeks; this is called ‘spontaneous’ labour. However, sometimes pregnancy is prolonged, or the pregnancy is not completely straight forward and induction of labour may be offered.
Membrane Sweep
Membrane sweeping involves you having a vaginal examination and your midwife or an obstetrician placing a finger inside your cervix and, by making a circular movement, gently sweeping the membranes away from the cervix. This procedure can be done either in your own home or in hospital.
This procedure can be done either in your own home or in hospital.
This is usually offered when you are 40 - 41 weeks pregnant and it aims to stimulate the natural production of prostaglandins which might speed up the opening of the cervix and in time trigger active labour. You may find the internal examination uncomfortable, and you may experience some bleeding similar to a ‘show’ following the procedure. This is because the internal examination involves stretching your cervix. This is normal and will not cause any harm to your baby. There is no evidence to suggest that labour triggered by this method is any more painful than a labour that starts naturally.
What is IOL?
Induction of labour is the process used to encourage labour to start artificially.
When is IOL recommended?
There are two main reasons why induction of labour is offered:
- When you have progressed 10 - 14 days past your estimated due date.
 The aim is to commence the induction process by 42 weeks. If your pregnancy lasts longer than 42 weeks, your baby’s health could be at greater risk because your placenta may not work as well.
The aim is to commence the induction process by 42 weeks. If your pregnancy lasts longer than 42 weeks, your baby’s health could be at greater risk because your placenta may not work as well. - If the obstetrician looking after you feels that either you or your baby’s health would benefit from earlier delivery. Common worries are diabetes in pregnancy, high blood pressure, concerns for your baby’s growth or problems that have been identified on your baby’s scans.
How is labour induced (started)?
There are three methods of inducing labour; you may have one or a combination of the following depending on your individual circumstances:
Prostaglandins
Prostaglandins are hormone-like substances that help to induce labour by encouraging the cervix to ripen, soften and shorten. Prostaglandins are inserted into the vagina, either in a tablet form called Prostin®, or as a pessary (medicated vaginal suppository) called Propess®.
Prostin®
This is a tablet form of prostaglandin and is inserted high into the vagina behind the cervix. One or more doses of Prostin® may be required depending on how ‘ready for labour’ the cervix feels during the vaginal examinations and according to your sensitivity to the prostaglandin. A repeat dose can be given after a six-hour interval but no more than two doses are usually given in any 24 hour period. This is most likely to be used if you have had babies before.
Propess®
This prostaglandin comes in the form of a pessary which is also is inserted vaginally and sits high in the vagina behind the cervix. It is soft and looks like a small tampon and has a string attached to allow for removal. Once the Propess® is inserted it will swell to keep it in place. The Propess® pessary usually remains in place for a maximum of 24 hours. However, it can be removed earlier if there are signs that labour has started. This is most likely to be used if you are having your first baby.
This is most likely to be used if you are having your first baby.
After a period of initial monitoring, you can walk around, shower, eat and drink normally. If the string from the Propess® moves to the outside of your vagina you must be careful not to pull or drag on it, as this may cause it to come out. Please take special care when:
- wiping yourself after going to the toilet
- washing yourself
- getting on and off the bed
In the unlikely event that the pessary should come out, please inform your midwife as soon as possible. If it has come out because your cervix is opening and you are in labour then the pessary will not be re-inserted, however if you are not in labour then the pessary will need to be reinserted during a vaginal examination.
Occasionally prostaglandins can make your womb contract too much and this could affect the pattern of your baby’s heartbeat. Therefore, before and after prostaglandins are given, your baby’s heartbeat will be monitored using a cardiotocograph (CTG) machine.
Therefore, before and after prostaglandins are given, your baby’s heartbeat will be monitored using a cardiotocograph (CTG) machine.
Breaking the waters - Artificial rupture of the membranes (ARM)
Artificial rupture of membranes may be performed when the cervix has ripened and opened. This is performed by a midwife or an obstetrician on Delivery Unit. During a vaginal examination a slim hook is introduced, and a small hole is made in the membranes/sac around the baby to release the amniotic fluid. Breaking the waters releases natural prostaglandins and encourages the baby’s head to make close contact with the cervix; this further stimulates the release of natural prostaglandins. The stimulation effects may be enough to encourage contractions to start, particularly if you are having your second or subsequent baby.
After your waters have been broken and your baby´s heart rate monitored for a period of time, you will be encouraged to mobilise for a few hours in order to help labour to start. If labour does not start an oxytocin drip will be offered to stimulate contractions; this is often necessary for women having their first baby.
If labour does not start an oxytocin drip will be offered to stimulate contractions; this is often necessary for women having their first baby.
Oxytocin drip (Syntocinon®)
If your contractions have not started or they are not sufficient to open the cervix despite breaking your waters, a drip in your arm containing Syntocinon® will be offered. Syntocinon® is an artificial form of the hormone oxytocin which starts contractions. When the Syntocinon® drip is started, contractions do come on more suddenly than they might do if you went into labour spontaneously, particularly if you have not been prepared by the early/pre-labour contractions. The contractions are not necessarily more painful, just that they started more quickly. The drip is started slowly and increased gradually until your contractions become regular. The frequency, strength and length of contractions, as well as your baby's heartbeat, will all need to be monitored while you receive Syntocinon®.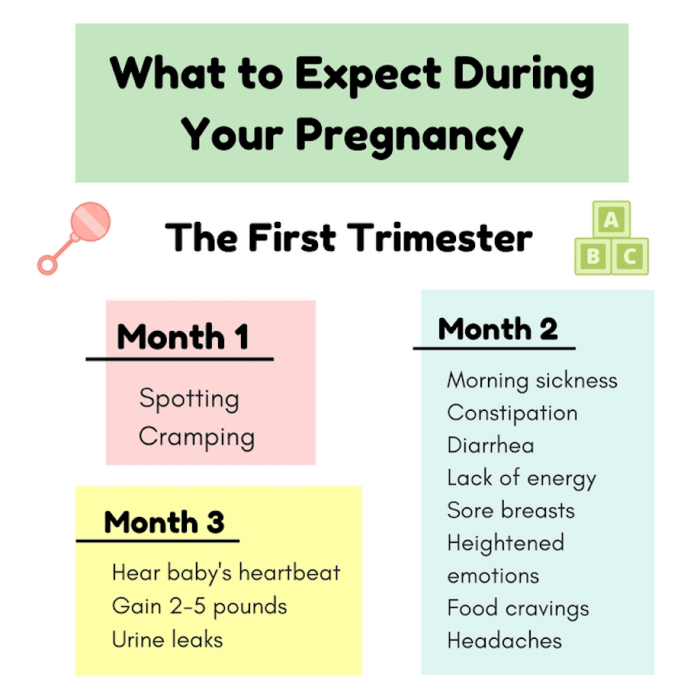
Arrangements for induction
Most inductions are commenced on the antenatal ward (Sara ward), however induction of labour for some women needs to be commenced on the delivery unit. Speak to your midwife or obstetrician if you have any questions about the area where you are going to be induced. You will be asked to call Sara ward or the delivery unit, depending on your clinical circumstances, at 09:30 on the planned day of your induction to find out what time to come in.
Sara ward direct dial: 01223 217671
There is no time restriction for one birthing partner to stay with you on Sara ward during the whole process of induction. The resting facilities for partners wishing to stay overnight are comfortable chairs next to your hospital bed.
If you wish to have two birth partners, your second partner may attend the ward between 17.00 and 19.30 during visiting hours (maximum of 2 visitors).
Delivery Unit direct dial: 01223 217648
If you wish to have two birth partners, both can be present on the Delivery Unit, but when you return to the postnatal ward after the birth, again only one partner may stay with you.
If your pregnancy is considered low risk and you are suitable to have an Outpatient Induction of Labour, you will be offered to attend Clinic 23 at 08:00 am in the morning for your induction to be commenced. If everything remains normal after the induction is commenced, you will be able to go back home. Your midwife will speak to you about this option.
Place of birth
As IOL usually means you need to have drugs (prostaglandins and/or Syntocinon®) it is important that you and your baby can be monitored during the induction and labour process, therefore you are advised to deliver your baby in hospital.
In the absence of any risk factors, and if you have had a previous vaginal birth before, you will be offered to go to the Rosie birth centre if you go into labour following prostaglandin administration only. If there are risk factors, you need to have your waters broken or you need to have the oxytocin drip, you will be transferred to the delivery unit.
If there are risk factors, you need to have your waters broken or you need to have the oxytocin drip, you will be transferred to the delivery unit.
How long will it take?
Every woman is different and starting labour can take different periods of time. In some cases, it can take a couple of days for labour to establish. The average length of stay on the Sara ward before going to Delivery Unit is between 24 - 72 hours.
Due to the nature of maternity care, there are occasions when your induction of labour must be delayed or postponed, or there may be some delay in transferring you to the Delivery Unit. This is because it is not possible to predict the number of women who will go into labour at any one time, or when emergency admissions occur. If this happens, we will keep you informed as much as possible and try to commence or continue with your induction as soon as we safely can. Occasionally we may offer monitoring of your baby while you are waiting to be admitted for induction.
We therefore advise that you prepare and make childcare arrangements if relevant, not just for the day of your induction but for several days afterwards.
Staying mobile and comfort measures
Women who can remain as mobile and upright as possible and to adopt optimal positions for labour, tend to cope better with the pain and have quicker labours than those who do not. Sometimes during IOL doing these things can feel awkward especially when you are being monitored and/or have a drip. Your midwife will encourage and help you remain mobile and try good positions. You should feel free to ask for help if you need it.
Birthing balls are available on Sara ward and delivery unit. If you wish to use them please ask a member of staff for one to borrow, they are a very helpful way of keeping upright and adopting comfortable positions during the induction and early labour process.
As you may be admitted for a couple of days before you go into labour it may be beneficial to bring in any small comforts from home that my help i. e., your own pillow. However, space and storage on the wards is limited, therefore we advise that you only bring the essentials whilst staying with us. If you are on any regular medication or are undertaking blood sugar monitoring, please bring these with you when you come for your induction.
e., your own pillow. However, space and storage on the wards is limited, therefore we advise that you only bring the essentials whilst staying with us. If you are on any regular medication or are undertaking blood sugar monitoring, please bring these with you when you come for your induction.
There are showers on the wards that you are welcome to use, and simple pain relief drugs are available if required. If you are thinking of using a TENS (transcutaneous electrical nerve stimulation) machine for pain relief we recommend you bring in your own machine from home, however TENS machines can be ordered on your request.
Eating and drinking
Throughout your stay on Sara ward, you will be encouraged to eat and drink as normal. It may be beneficial for you to bring in some snacks from home, which may be stored in the ward fridge if required. Isotonic or sports drinks may be more beneficial than water and are a good way of boosting energy levels especially during the early stages of labour and beyond. You may bring these with you if you wish.
You may bring these with you if you wish.
Unsuccessful induction of labour
Induction aims to tip the balance in favour of labour starting, but occasionally this does not work, and we say that the induction has been unsuccessful or “failed”. In these rare cases you may be offered a caesarean section to deliver your baby.
What to expect if you choose not to have induction of labour for prolonged pregnancy
If you choose not to be induced at 10 - 14 days past your estimated due date and the pregnancy is prolonged, after this time you will be offered a consultant appointment to discuss ‘expectant’ management which may include:
- An ultrasound scan to check your baby’s growth and amount of fluid (waters) around the baby.
- A check of your baby’s heartbeat using a CTG machine.
These are used to assess your baby’s health status at that particular time; however, these checks cannot always predict how your placenta will continue to function or how your baby will cope once labour begins.
Further information
If you have any queries at any time, please discuss these with your doctor or midwife.
More information is also available from:
- National Institute for Clinical Excellence - NICE The National Institute for Health and Care Excellence
- Royal College of Obstetricians and Gynaecologists - RCOG Royal College of Obstetricians and Gynaecologists
Privacy & dignity
Same sex bays and bathrooms are offered in all wards except critical care and theatre recovery areas where the use of high-tech equipment and/or specialist one to one care is required.
We are smoke-free
Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0800 169 0 169.
Other formats
Help accessing this information in other formats is available. To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
To find out more about the services we provide, please visit our patient information help page (see link below) or telephone 01223 256998. www.cuh.nhs.uk/contact-us/accessible-information/
Contact us
Cambridge University Hospitals
NHS Foundation Trust
Hills Road, Cambridge
CB2 0QQ
Telephone +44 (0)1223 245151
https://www.cuh.nhs.uk/contact-us/contact-enquiries/
What Does IOL Stand For In Pregnancy?
When you’re pregnant, you find yourself in a whole new world of terminology, jargon and acronyms.
It can be so confusing trying to work out what it all means, and sometimes you can’t help but feel like a newbie at it all.
Amongst all the incomprehensible doctor shorthand, you may notice the letters IOL on your medical records.
So what does IOL stand for in pregnancy?
If you see the letters IOL, it simply means induction of labour.
Perhaps you’ve had an IOL for a previous pregnancy, or perhaps you’ve been scheduled for one in your current pregnancy.
Your hospital may offer several forms of IOL, including:
#1: Cervical Ripening Gels, Tablets and Pessaries
If a woman’s cervix is closed and not ready for labour, it can be ripened with synthetic hormone (prostaglandin) first.
Prostaglandins can be administered via a gel, pessary or tablet, and just one dose is given to try and start labour. The dose may be repeated if nothing progresses after so many hours.
Gels and pessaries are inserted into the vagina, and tablets can be taken orally. Some hospitals allow women to go home after the application of prostaglandins, then return when labour is established.
#2: Synthetic Oxytocin
The most common method of induction is via an IV drip containing a synthetic version of the labour hormone, oxytocin. The drug is commonly known as Syntocinon in Australia, and Pitocin in the US.
To begin the induction, the pregnant woman is admitted to hospital, then hooked up to the IV. She will then be monitored as the contractions begin, as her labour is now classed as high risk. Unfortunately the monitors can restrict movement and further interventions are common.
She will then be monitored as the contractions begin, as her labour is now classed as high risk. Unfortunately the monitors can restrict movement and further interventions are common.
Read more about the risks of induction of labour.
#3: Artificial Rupture Of Membranes (AROM)
If a woman’s cervix is partially open, her doctor can rupture the membranes (also called an amniotomy).
Using an amnihook (which looks like a long crochet hook) inside the vagina, the doctor will break the bag of waters surroundingthe baby, in the hope it triggers labour.
#4: Foley Balloon Catheter
The Foley balloon catheter was originally designed to empty a patient’s bladder. It can be slowly inflated and manually dilates the cervix.
It’s a safer, recommended option for women who’ve had a previous c-section, and can be used on anyone who has a partially open cervix. Because it doesn’t involve medication, it’s has fewer risks for both mothers and babies.
…
While inductions of labour are a very common procedure, they do come with risks, especially if medications are used. Some of these risks are serious, others not so much. However, many inductions do result in further interventions, including emergency c-sections. In Australia and the US, one in three babies are born by c-section, which is double the recommended level from the World Health Organization. Reducing the number of inductions of labour will highly likely reduce the number of c-sections performed.
It’s important to make sure you’re aware of all the risks as well as the benefits, so you can make a decision which will offer the best outcome for you and your baby.
Recommended Reading
- The Risks Of Induction Of Labour
- 4 Methods Of Induction Of Labour (in much more detail than this article)
- How To Bring On Labour Naturally
Artificial eye lens
Answers to popular questions.
Intraocular lenses (IOLs) are artificial lenses (usually made of acrylic, silicone, or plexiglass) that are implanted to replace a cataract clouded lens.
IOL - what is it?
Intraocular lenses (IOLs) are artificial lenses (usually made of acrylic, silicone, or plexiglass) that are implanted to replace a cataract-clouded lens. nineThe 0003 IOL has also been successfully used in the treatment of patients with presbyopia, in which the lens causes trouble focusing at close range due to loss of elasticity.
The intraocular lens successfully performs the functions of a healthy lens, refracting the light flux to the retina. In this case, the optical part of the IOL in diameter is only 5-6 mm.
What types of IOLs are there?
IOLs are either monofocal or multifocal. nine0012
Monofocal lenses. They improve overall visual acuity after surgery and provide good vision at a certain focal length from the eye - either near or clear vision at a distance, which is useful when driving or watching movies. However, when implanting this type of lens, in order for the patient to see clearly at a different distance from the eyes, periodic use of reading or distance glasses is required.
Multifocal lenses, , in turn, allow you to see both close and distant objects equally well, i.e. do not require glasses.
There are also toric lenses , which compensate for the patient's astigmatism and achieve better vision. There are both monofocal toric lenses and multifocal toric lenses.
The decision to choose one or another type of lens is made by an ophthalmologist, based on the condition of the patient's eyes and the presence of indications and contraindications. nine0005
How is the IOL implantation performed?
Typically, the operation, during which the cataract is removed and an intraocular lens is implanted, takes 30 minutes.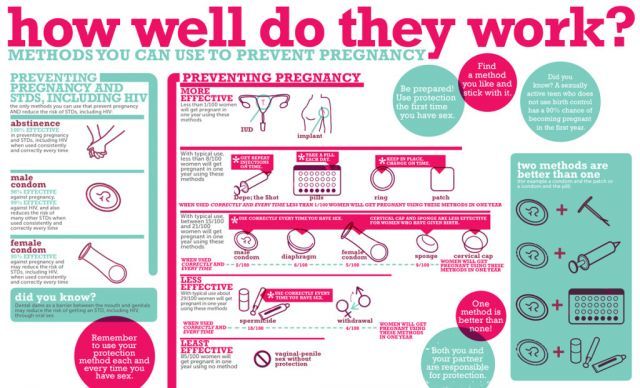 Local anesthesia is mainly used, less often general anesthesia.
Local anesthesia is mainly used, less often general anesthesia.
Special drops are instilled into the patient's eye to dilate the pupil. Next, the area around the eyes is processed and covered with a special sterile napkin. After that, the ophthalmic surgeon makes microscopic punctures for the introduction of special instruments. nine0012
Under the action of ultrasound, the lens is emulsified and removed, and an intraocular lens is introduced into its capsule.
When can I return to work?
If there are no complications, then the patient can leave the clinic almost immediately. However, it is recommended that an assistant be present for the first time, as vision will be blurry on the day of the operation.
It takes several days to resume normal activities, but there may be increased sensitivity to bright light or touch, as well as a feeling of discomfort in the form of a feeling of a foreign body or sand. nine0012
Initially, it is important to refrain from excessive exertion (including heavy lifting). It is unacceptable to get moisture or mechanical impact on the operated eye until it is completely healed.
It is unacceptable to get moisture or mechanical impact on the operated eye until it is completely healed.
Are IOLs dangerous?
Extensive studies conducted in Asia, Europe and the USA prove that intraocular lenses are completely safe for patients.
The first operation of this type was carried out in 1949. Every year, more than 1,000,000 cataract operations are performed worldwide, followed by IOL implantation. nine0012
Of course, any type of surgery carries the risk of complications, but it should be borne in mind that cataract removal is one of the most common operations, and the surgeons of the SPECTR Ophthalmological Clinic are highly qualified specialists.
Do I need to wear glasses after IOL implantation?
The operation helps restore vision in 98% of cases, but its severity depends on how the patient saw before the operation, on concomitant eye diseases, and also on the type of implanted lens. nine0012
A variety of existing IOLs allows you to choose a lens that maximizes the patient's vision. However, monofocal lenses require you to wear specialized glasses for near or far distances, while multifocals do not.
However, monofocal lenses require you to wear specialized glasses for near or far distances, while multifocals do not.
Is cataract surgery necessary after IOL implantation?
No. Recurrence of the removed cataract is impossible, since the disease affects the lens, which is replaced with an IOL.
Some patients may experience clouding of the posterior lens capsule, which holds the implanted lens in place. This problem is called a secondary cataract, but it is only a decrease in the transparency of the capsular bag that contains the IOL, and not a recurrence of the disease. Turbidity is removed with a laser, it is painless, and the risks are minimal. nine0012
Does an IOL help with astigmatism?
Most often, surgery to remove the affected lens (and replace it with an IOL) corrects most visual dysfunctions, including astigmatism. An IOL that helps correct this problem is called a toric IOL.
Who can have an IOL implanted?
An intraocular lens can be implanted in most cataract/presbyopia patients, provided there are no contraindications. Lens implantation is allowed in the treatment of children and adolescents (for example, with congenital cataracts), but they may subsequently need additional vision correction. nine0012
Lens implantation is allowed in the treatment of children and adolescents (for example, with congenital cataracts), but they may subsequently need additional vision correction. nine0012
Consultation on the presence of contraindications can be obtained from an ophthalmic surgeon.
Eyedoctor - Pregnancy and vision
PREGNANCY AND VISION
Pregnancy is a very important and certainly exciting period in a woman's life.
Over the entire period, I have repeatedly had to undergo scheduled examinations by various specialists, and one should not neglect the examination by an ophthalmologist. This applies to women, including those with good eyesight. nine0012
So, how does the bearing of a child sometimes affect vision?
Sign up
1. Mild transient myopia may occur in a healthy woman. The reason for such changes is an increase in the curvature and thickness of the cornea, and sometimes the lens, due to the delay or redistribution of fluid in them under the influence of progesterone. As a rule, these changes disappear after childbirth and the end of lactation. That is why pregnancy and lactation are the wrong time for laser vision correction surgery , because such fluctuations in refraction (“minus / plus”) will not allow accurate calculations and guarantee a stable result and one hundred percent vision.
As a rule, these changes disappear after childbirth and the end of lactation. That is why pregnancy and lactation are the wrong time for laser vision correction surgery , because such fluctuations in refraction (“minus / plus”) will not allow accurate calculations and guarantee a stable result and one hundred percent vision.
2. Against the background of hormonal changes - the appearance of Dry Eye Syndrome. Often pregnant patients note that during this period it became very uncomfortable for them to wear contact lenses. But there is also good news! Moisturizing Drops are completely safe for you and your baby and can relieve unpleasant symptoms. nine0012
3. During pregnancy, the sensitivity of the cornea decreases, so it becomes easier to injure and infect it.
Be careful when applying make-up, if possible, refrain from eyelash extensions, eyelid tattoos, etc. during this period.
4. Increased intraocular pressure, deterioration in patients with glaucoma, the appearance of flies before the eyes in healthy women.
5. Deterioration of blood supply to the retina, as a result - deterioration in color vision, blurred vision, etc. nine0012
Most of the above symptoms are temporary and vision returns to normal after childbirth, especially in healthy women. But patients suffering from severe myopia or glaucoma may find that the negative changes can persist after pregnancy.
It is also worth taking seriously such complaints as blurred vision, flashes, sparks in the eyes (photopsies), loss of part of the field of vision (scotomas), doubling can be a sign of high blood pressure. They may indicate the development of severe pregnancy complications such as preeclampsia and eclampsia. nine0012
As you can see, pregnancy can be accompanied by various visual disorders. Some of them are physiological and do not require treatment. Others, on the contrary, may be a signal of serious illness. Fortunately, the latter are much rarer.
In order to prevent pathology in a timely manner, mandatory diagnostics of vision in pregnant women is carried out. If there are no complaints, and the woman feels well, then the examination should be carried out twice during pregnancy. At 10–14 weeks, diagnosis of visual acuity and examination of the fundus with a dilated pupil. The same studies are repeated at 30–32 weeks to ensure that the delivery is safe for the woman and she retains her vision. During the examination, refraction is determined, the condition of the fundus is assessed; if necessary, women undergo perimetry, intraocular pressure is measured, the extreme periphery of the fundus with a goniolens is examined - this procedure is called CYCLOSCOPY.
If there are no complaints, and the woman feels well, then the examination should be carried out twice during pregnancy. At 10–14 weeks, diagnosis of visual acuity and examination of the fundus with a dilated pupil. The same studies are repeated at 30–32 weeks to ensure that the delivery is safe for the woman and she retains her vision. During the examination, refraction is determined, the condition of the fundus is assessed; if necessary, women undergo perimetry, intraocular pressure is measured, the extreme periphery of the fundus with a goniolens is examined - this procedure is called CYCLOSCOPY.
Cycloscopy allows an ophthalmologist to thoroughly examine the state of the peripheral region of the retina, ciliary muscle, choroid with a special lens of a special design, which has three mirror planes. These mirrors at certain angles reflect different areas inside the eyeball. and help diagnose retinal dystrophy, ruptures, changes in retinal vessels, assess the condition of the optic nerve. The collected and analyzed data will help the ophthalmologist to give a conclusion to exclude the straining period during childbirth or to refer to physiological childbirth.
The collected and analyzed data will help the ophthalmologist to give a conclusion to exclude the straining period during childbirth or to refer to physiological childbirth.
There is an opinion that is not entirely correct, which enrolls the owners of only a diagnosis of high myopia for delivery by Caesarean section. If, after examination by a doctor, he does not find pathological changes in the retina, then most likely he will give permission for natural childbirth. nine0012
But it also happens that an ophthalmologist discovers the so-called peripheral degenerative foci. Some require simple observation, and some require a preventive procedure called Retinal Laser Coagulation. The essence of the method is to use a special laser to delimit dystrophy zones by applying laser coagulates (microburns), which solder the retina to the underlying layers, thereby preventing the development of retinal detachment. She's running, at any stage of pregnancy preferably up to 32 weeks, is not dangerous for the health of the mother and child and in most cases is not accompanied by pain.