How to stop constant coughing in child
Causes, Treatments & When To See A Doctor
Coughing is your body’s way of getting rid of an irritant. Many things can cause a dry cough in kids, from a simple cold to an inhaled object.
Coughing is an important part of your body’s defense system, helping rid your body of potentially harmful microbes and irritants.
Coughs come in many types, including wet and dry. Wet coughs produce, or sound like they are producing, phlegm, or mucus. Dry coughs, on the other hand, don’t.
These are some common causes of cough in children:
Infections
Various viral or bacterial respiratory infections can lead to coughing due to irritation and inflammation in the airways.
The most familiar cause is the common cold, an infection in your upper respiratory tract with symptoms including sneezing, runny nose, and coughing. Rhinovirus is the most common cause of the common cold.
Another common cause is bronchitis, which can occur as a result of either the common cold or the flu. Bronchitis can be acute or chronic. Acute bronchitis is usually a result of an infection. Chronic bronchitis can happen due to smoking or being exposed to air pollution.
Other infections that can lead to dry cough in kids include:
- croup: a viral condition that causes swelling around the vocal cords. It is usually viral but may be bacterial less commonly.
- pneumonia: an infection that causes inflammation in the lungs. It can be viral or bacterial.
- bronchiolitis: a viral infection that causes inflammation in the bronchioles or smallest passages in your lungs.
- pertussis: known as whooping cough, it’s a bacterial respiratory infection that causes violent, uncontrollable coughing that can make it hard to breathe. Whooping cough can be prevented through vaccination.
- COVID-19: The coronavirus can present with dry cough in children.
Depending on the infection, the cough may sound hoarse or have more of a wheezing sound. It may also worsen at night due to mucus from the nose trickling down the throat, irritating.
It may also worsen at night due to mucus from the nose trickling down the throat, irritating.
Other signs that your child may have a viral infection include:
- fever
- runny or stuffy nose
- sneezing
- headache
- body aches and pains
Unlike bacterial infections, viral infections don’t respond to antibiotic treatment. Instead, treatment relies on getting plenty of rest and fluids.
If your child is over 6 months old, they can be given ibuprofen (Motrin, Advil) to help relieve fevers and body aches. Babies younger than 6 months can get acetaminophen (Tylenol). Avoid giving them aspirin, which can cause Reye’s syndrome in children.
Sometimes a cough can linger for several weeks after a viral respiratory infection. This is called post-viral cough. It likely occurs due to lingering inflammation or sensitivity in the airways following infection.
There’s no specific treatment for post-viral cough, but symptoms typically go away on their own after a few weeks.
Allergies
Allergies happen when the immune system mistakes something harmless for a foreign invader and overreacts.
The thing that causes an allergic reaction is called an allergen. There are many allergens, including pollen, animal dander, and specific foods or medications.
A substance called histamine is released during an allergic reaction and can cause respiratory symptoms.
Hoarse, dry coughing can be a symptom of allergies, particularly if it begins at a certain time of year or occurs after exposure to something specific like dust. For example, seasonal allergy or allergic rhinitis may develop in the spring when pollen is in the air.
Other allergy symptoms include:
- sneezing
- itchy, watery eyes
- runny nose
- rash
The best way to manage allergies is to avoid things that trigger your child’s symptoms. You can also try over-the-counter (OTC) allergy remedies, but follow the product instructions and ensure it’s appropriate for your child’s age and size.
If your child seems to experience allergies often, you may want to visit an allergy specialist. They can help you narrow potential allergens and recommend a long-term management plan.
Asthma
Allergies can also make asthma worse. This chronic disease causes inflammation and narrowing of the airways, making it hard to breathe. Symptoms of asthma can also be triggered by respiratory illness or exercise.
Frequent spells of coughing, which can be dry or productive, are one of the signs of asthma in kids. Coughing may be more frequent at night or while playing. You may also hear a whistling noise when your child breathes in or out.
In some cases, chronic coughing may be the only symptom of asthma. This is called cough-variant asthma.
Other symptoms of asthma that you may see can include:
- difficulty breathing or shortness of breath
- rapid breathing
- low energy levels
- chest tightness or pain
If your child is diagnosed with asthma, their healthcare professional will work with you to develop an asthma action plan. The plan will include your child’s asthma triggers and how and when they should take their medication.
The plan will include your child’s asthma triggers and how and when they should take their medication.
Asthma medication helps lower the inflammation in your child’s airways. Your child will likely have two types of medication — one for long-term asthma control and one for quick relief of asthma symptoms.
Environmental irritants
Exposure to various environmental irritants can cause throat inflammation, leading to a dry cough.
Common irritants that can cause a cough include:
- cigarette smoke
- car exhaust
- air pollution
- air that’s too cold or dry
The dry cough may become chronic if your child is frequently exposed to an irritant. Your child may be more susceptible to irritation if they also have allergies or asthma.
Coughs caused by exposure to irritants usually resolve once the irritant is removed.
Inhaled or swallowed foreign object
It’s not unusual for young children to put things in their mouths or noses, including buttons, beads, and other small objects. If they inhale too deeply, the object may get lodged in their airway. Or they might swallow the object, causing it to get stuck in their esophagus.
If they inhale too deeply, the object may get lodged in their airway. Or they might swallow the object, causing it to get stuck in their esophagus.
If your child has swallowed or inhaled something, their cough could be a sign that their body is trying to dislodge the object. You may also hear wheezing or choking noises.
If you believe your child has inhaled or swallowed a foreign object, seek immediate treatment.
A bronchoscopy may be needed to find and remove the object.
After removing the object, you’ll want to monitor them for signs of infection or further irritation.
GERD
Gastroesophageal reflux disease (GERD) is chronic acid reflux that can cause regurgitation, which is when the stomach’s content rises back up into the esophagus.
The burning sensation your child may feel is what we call heartburn. In some cases, however, some children with GERD can also experience persistent cough, hoarseness, or wheezing.
Different triggers for GERD in children may include exposure to secondhand smoking, obesity, and coexisting conditions that affect the lungs or the nervous system.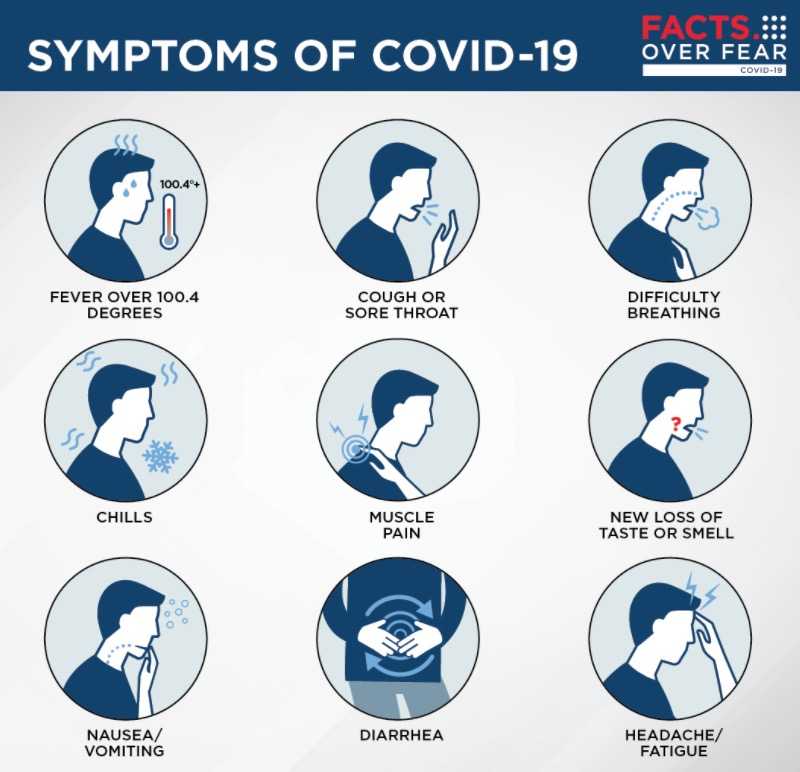
Somatic cough
A psychosomatic or somatic cough is a term that doctors use to refer to a cough that doesn’t have a clear cause and doesn’t respond to treatment. An underlying psychological issue or distress usually causes these coughs.
But these coughs are rarely diagnosed as there is more often a physical cause for the cough. If they occur, these coughs often last for more than 6 months and get in the way of day-to-day activities.
If your child’s healthcare professional has ruled out all the potential causes of their dry cough, they may diagnose it as a somatic cough. You’ll likely be referred to a child psychologist or psychiatrist.
It can take some time to figure out the cause of a dry cough in children. The main treatment will depend on the underlying cause.
These tips can help to provide some relief in the meantime:
- Inhale warm, moist air. Turn on the shower in your bathroom and close the door, allowing the room to steam up.
 Sit with your child for about 20 minutes as they inhale the warm mist.
Sit with your child for about 20 minutes as they inhale the warm mist. - Use a cool mist humidifier. If the air in your house is dry, it can also dry out your child’s airways. Try using a cool mist humidifier to add moisture to the air. Avoid heated humidifiers as these can cause burns.
- Drink warm fluids. Warm fluids can feel soothing if your child’s throat is sore from coughing. If your child is at least a year old, you can add some honey for added relief.
Coughing helps your body get rid of potentially harmful microbes and irritants. In children, dry coughs can be caused by many things, including viral or bacterial infections, asthma, allergies, and irritants.
OTC cough medications, inhaling steam from warm fluid, and using a cool-mist humidifier may help relieve cough symptoms. But you should discuss with your pediatrician which medication is appropriate for your child based on age and the right dosage.
Most coughs will resolve in 1 to 2 weeks, but contact a doctor if your child’s cough lasts longer than 2 to 3 weeks.
Here you will find answers to some common questions about dry cough in children:
What can I give my child for a dry cough?
In some cases, giving your child OTC cough medicines may be appropriate. But only give it to a child older than 6, and ensure to carefully follow the dosing directions on the packaging.
Children under age 6 shouldn’t take OTC cough medication unless it is recommended by their healthcare professional, especially decongestants, which can be associated with dangerous side effects.
If an OTC cough medication does not seem to help, there is no benefit to continuing to use it. These medicines do not cure a cough or help it go away faster.
Should I take my child to the doctor for a dry cough?
Most coughs will resolve in 1 to 2 weeks. If your child’s cough lasts longer than 2 to 3 weeks, contact a doctor.
When should I be concerned about my child’s cough?
Reasons for concern and seeking medical attention include:
- if you observed your child choking or think they may have swallowed an object
- if your child’s cough is increasingly frustrating
- if it persists longer than you think is reasonable
- if your child coughs up blood
- if the cough is affecting your child’s ability to participate in daily activities
- If your child is struggling to breathe or breathing fast
Coughing (for Parents) - Nemours KidsHealth
What Are Coughs?
Coughs are one of the most common symptoms of childhood illness. A cough can sound awful, but usually isn't a sign of a serious condition. In fact, coughing is a healthy and important reflex that helps protect the airways in the throat and chest.
A cough can sound awful, but usually isn't a sign of a serious condition. In fact, coughing is a healthy and important reflex that helps protect the airways in the throat and chest.
What Are the Different Types of Coughs?
Sometimes, though, a cough needs a doctor's care. Understanding the different types of cough can help you know when to handle them at home and when to call your doctor.
The most common types of coughs are:
- "barky" cough
- whooping cough
- cough with wheezing
- nighttime cough
- daytime cough
- cough with a fever
- cough with vomiting
- persistent cough
"Barky" Cough
Barky coughs are usually caused by swelling in the upper airway. Most of the time, a barky cough comes from croup, a swelling of the larynx (voice box) and trachea (windpipe). Younger children have smaller airways that, if swollen, can make it hard to breathe. Kids younger than 3 are most at risk for croup because their airways are so narrow.
A cough from croup can start suddenly, often in the middle of the night. Most kids with croup will also have stridor, which is a noisy, harsh breathing that happens when the child inhales (breathes in).
Whooping Cough
Whooping cough (pertussis) is an infection of the airways caused by the
bacteriaBordetella pertussis. Kids with pertussis will have spells of back-to-back coughs without breathing in between. At the end of the coughing, they'll take a deep breath in that makes a "whooping" sound. Other symptoms are a runny nose, sneezing, mild cough, and a low-grade fever.
Whooping cough can happen at any age, but is most severe in infants under 1 year old who did not get the pertussis vaccine, which is part of the DTaP vaccine (diphtheria, tetanus, acellular pertussis). It's very contagious, so all kids should get the pertussis shot at 2 months, 4 months, 6 months, 15 months, and 4–6 years of age.
Cough With Wheezing
If your child makes a wheezing (whistling) sound when breathing out (exhaling), this could mean that the lower airways in the lungs are swollen. This can happen with asthma or with the viral infection bronchiolitis. Wheezing also can happen if the lower airway is blocked by a foreign object. A child who starts to cough after inhaling something such as food or a small toy should see a doctor.
Nighttime Cough
Lots of coughs get worse at night. When your child has a cold, the mucus from the nose and sinuses can drain down the throat and trigger a cough during sleep. This is only a problem if the cough won't let your child sleep.
Asthma also can trigger nighttime coughs because the airways tend to be more sensitive and irritable at night.
Daytime Cough
Cold air or activity can make coughs worse during the daytime. Try to make sure that nothing in your house — like air freshener, pets, or smoke (especially tobacco smoke) — is making your child cough.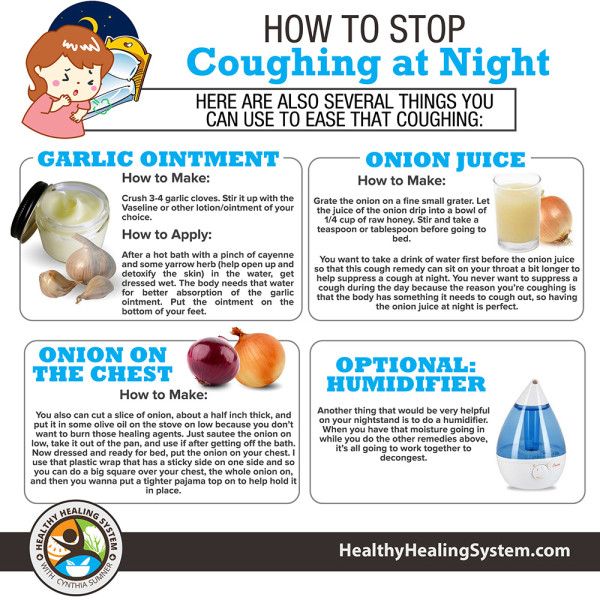
Cough With a Fever
A child who has a cough, mild fever, and runny nose probably has a common cold. But coughs with a fever of 102°F (39°C) or higher can sometimes be due to pneumonia, especially if a child is weak and breathing fast. In this case, call your doctor immediately.
Cough With Vomiting
Kids often cough so much that it triggers their gag reflex, making them throw up. Also, a child who has a cough with a cold or an asthma flare-up might vomit if lots of mucus drains into the stomach and causes nausea. Usually, this is not cause for alarm unless the vomiting doesn't stop.
Persistent Cough
Coughs caused by colds due to viruses can last weeks, especially if a child has one cold right after another. Asthma, allergies, or a chronic infection in the sinuses or airways also might cause lasting coughs. If your child still has a cough after 3 weeks, call your doctor.
How Are Types of Coughs Diagnosed?
If you're concerned about your child's cough, call your doctor. Depending on the type of cough, other symptoms, and how long it's lasting, the doctor might want to see your child.
Depending on the type of cough, other symptoms, and how long it's lasting, the doctor might want to see your child.
Many health care providers now offer telehealth visits, which can save parents a trip to the office (especially for a nighttime cough). "Video chatting" lets doctors see and hear a child cough, and often this is enough to make a diagnosis or rule out a serious problem. Hearing the cough will help the doctor decide whether (and how) to treat it.
How Are Coughs Treated?
Most coughs are caused by viruses and have to just run their course. Sometimes, this can take up to 2 weeks. Doctors usually don't prescribe antibiotics because these only work against bacteria.
Unless a cough won't let your child sleep, cough medicines are not needed. They might help a child stop coughing, but they don't treat the cause of the cough. If you do use an over-the-counter (OTC) cough medicine, call the doctor to be sure of the correct dose and to make sure it's safe for your child.
Do not use OTC combination medicines (like "Tylenol Cold") — they have more than one medicine in them, and kids can have more side effects than adults and are more likely to get an overdose of the medicine.
Cough medicines are not recommended for any children under 6 years old.
How Can I Help My Child Feel Better?
To help your coughing child feel better:
- For a "barky" or "croupy" cough, turn on the hot water in the shower in your bathroom and close the door so the room will steam up. Then, sit in the bathroom with your child for about 20 minutes. The steam should help your child breathe more easily. Try reading a book together to pass the time.
- A cool-mist humidifier in your child's bedroom might help with sleep.
- Sometimes, brief exposure to cool air outdoors can relieve the cough. Make sure to dress your child appropriately for the outdoor weather and try this for 10–15 minutes.
- Cool beverages like juice can be soothing and it is important to keep your child hydrated.
 But do not give soda or orange juice, as these can hurt a throat that is sore from coughing.
But do not give soda or orange juice, as these can hurt a throat that is sore from coughing. - You should not give your child (especially a baby or toddler) OTC cough medicine without first checking with your doctor.
- If your child has asthma, make sure you have an asthma action plan from your doctor. The plan should help you choose the right asthma medicines to give.
- Cough drops are OK for older kids, but kids younger than 3 years old can choke on them. It's better to avoid cough drops unless your doctor says that they're safe for your child.
When Should I Call the Doctor?
Always call your doctor if your child is coughing and:
- has trouble breathing or is working hard to breathe
- is breathing faster than usual
- has a blue or dusky color to the lips, face, or tongue
- has a high fever (especially if your child is coughing but does NOT have a runny or stuffy nose)
- has any fever and is younger than 3 months old
- is younger than 3 months old and has been coughing for more than a few hours
- makes a "whooping" sound when breathing in after coughing
- is coughing up blood
- has stridor (a noisy or musical sound) when breathing in
- has wheezing when breathing out (unless your doctor already gave you an asthma action plan)
- is weak, cranky, or irritable
- is dehydrated; signs include dizziness, drowsiness, a dry or sticky mouth, sunken eyes, crying with little or no tears, or peeing less often (or having fewer wet diapers)
Night cough keeps you awake.
 How to stop an attack?
How to stop an attack? Cough is an important helper in the fight against illness. This is a protective reflex that helps clear the airways of phlegm and germs. But nocturnal coughing attacks interfere with rest and exhaust the already weakened body.
Why does the cough get worse at night?
When a person is in a horizontal position, mucus accumulates in the nasopharynx, the airways are not cleared. With a runny nose, discharge from the nose and paranasal sinuses drain into the throat and cause a cough reflex, so coughing is tormenting in a dream, especially when we roll over from side to side, and in the morning when we get out of bed. nine0003
Dust and dry air can exacerbate coughing. This is especially true in apartments with central heating. Dry and hot air irritates the mucous membranes and provokes coughing fits. To alleviate your condition, regularly ventilate the bedroom and do wet cleaning. It will not be superfluous to buy a humidifier. But if you don’t have it, and you need to fight a cough right now, you can hang a damp towel on the battery or put a container of water next to the bed.
Dry and wet cough - is there a difference? nine0005
Yes. A wet cough associated with colds and flu is helpful in clearing the nasopharynx and airways. Phlegm protects the mucous membranes and prevents bacteria from entering the body.
A dry, throat-tearing cough, on the contrary, is quite dangerous for the body. With such a cough, sputum is not secreted, the bronchi are not cleared, and the nasopharynx dries up. A constant inflammatory process is maintained on the walls of the respiratory tract. A dry cough, unlike a wet cough, does not help to recover, but only exhausts and interferes with rest. To speed up the healing process, you need to try to translate a dry cough into a wet one. But this should be done under the supervision of a doctor. nine0003
Night cough in a child - is it dangerous?
No, unless the cough is a symptom of a serious illness (such as asthma or pneumonia). The most common cause of cough in children is a viral infection. Viruses infect the respiratory tract at different levels - from the nose to the bronchi, bronchioles and lungs. Sometimes the cough lasts for several weeks, because the child does not have time to recover from one infection and picks up another. About 10% of children continue to cough even after being treated with SARS. nine0003
Sometimes the cough lasts for several weeks, because the child does not have time to recover from one infection and picks up another. About 10% of children continue to cough even after being treated with SARS. nine0003
Some doctors are even suggesting a new term, "post-viral cough". Such long attacks scare parents, but most often they do not speak of serious pathologies.
But even if the disease is not dangerous or has completely disappeared, it is difficult for a child to endure sleepless nights, especially with a dry cough. Yes, and parents have a hard time if they don’t know how to help.
Important: if the child coughs frequently at night, this may be a sign of respiratory problems, allergies or whooping cough. Be sure to consult a doctor and do not treat the child yourself, so as not to worsen his condition. nine0028
What should I do if my child coughs and cannot sleep?
To quickly stop a night cough attack and help your child, you can:
- Place a high pillow under the back, turn the child from back to side to prevent a strong outflow of mucus swallowed and accumulated during the day.

- If the child does not have allergies, a spoonful of honey will help - it envelops and soothes the mucous membranes of the throat.
- Give your child warm tea or water to relieve cough and soothe the airways. It is better not to drink carbonated drinks or citrus juices - they can additionally irritate the already inflamed mucous membranes. nine0036
How to stop a night cough attack in an adult?
Try to find a comfortable position. Place a high pillow under your back. Drink warm tea or water to soothe your throat. This is especially important for dry coughs - the liquid will help soothe the irritation.
If you find it difficult to breathe, ventilate the bedroom and try humidifying the air. If you don't have a humidifier, hang a couple of wet towels on the radiator. You can arrange a small session of steam therapy: go to the bathroom, close the door, turn on the hot water and wait a few minutes. nine0003
What drugs will help get rid of a cough?
It is ineffective and dangerous to treat cough only with the help of folk remedies. If it does not go away within a few days and nights, be sure to consult a doctor. It is important to remember that cough is a symptom of the disease, and not an independent disease, therefore, complex treatment is required.
If it does not go away within a few days and nights, be sure to consult a doctor. It is important to remember that cough is a symptom of the disease, and not an independent disease, therefore, complex treatment is required.
Wet cough is treated with mucolytic and expectorant drugs. They improve the excretion of sputum and mucus. But with a dry cough, such medicines do not help, but only increase the attacks, because the body will try to remove sputum that is not there. Antitussive drugs that inhibit or suppress the cough reflex help to get rid of a dry cough. nine0003
Mucolytic drugs, which include, for example, ambroxol, will help to cope with a wet cough in bronchitis or pneumonia. SANTO manufactures Ambro® solution, which can be taken orally or inhaled. Ambro® has an anti-inflammatory effect, as well as antioxidant properties, stimulates local immunity, increases the concentration of antibiotics in sputum and bronchial secretions.
How to get rid of a nocturnal cough | How to soothe a wet cough at night
Author, editor and medical expert
Petrashevich Anna Aleksandrovna
Views: 861 922
Last update date: 26. 12.2022
12.2022
Content
cough?
How to relieve a night cough and relieve an attack?
Cough in itself is an unpleasant phenomenon that prevents you from doing your usual activities and significantly worsens your general well-being. But when this condition does not stop day or night, the consequences can be much more serious than just feeling tired due to lack of sleep. nine0003
WHAT IS A NIGHT COUGH DANGEROUS?
Coughing attacks that occur at night can cause many temporary and even permanent health problems. To understand how harmful this condition is to the body, only one of the complications can be cited. Will you like memory impairment, decreased visual acuity, and impaired smell? It would seem that what does a night cough have in common with the loss of such important functions as the ability to clearly see the world around, remember information and smell? The relationship is more obvious than it seems at first glance: oxygen starvation and lack of rest in the main organ of the human body - the brain. In the dark, the brain must rest and restore the resources spent during the day. These processes are possible only in the process of deep sleep, into which the body is simply not able to immerse itself - it is constantly awakened by a cough. You will survive several of these nights without consequences, but a prolonged dry or wet night cough will sooner or later lead to chronic brain fatigue with subsequent dysfunction of its various areas. What to do if a night cough interferes with normal life? nine0003
In the dark, the brain must rest and restore the resources spent during the day. These processes are possible only in the process of deep sleep, into which the body is simply not able to immerse itself - it is constantly awakened by a cough. You will survive several of these nights without consequences, but a prolonged dry or wet night cough will sooner or later lead to chronic brain fatigue with subsequent dysfunction of its various areas. What to do if a night cough interferes with normal life? nine0003
HOW TO ELIMINATE A NIGHT COUGH AND RELIEVE AN ATTACK?
Soothing a nocturnal cough in a child or adult is not an easy task, but it is quite doable. By following the recommendations listed below, you will significantly improve not only the quality of sleep, but also recovery from an illness accompanied by a cough.
-
Take care of full nasal breathing. A stuffy nose makes you breathe through your mouth, which leads to drying of the mucous membrane of the throat, itching and .
 .. a coughing fit is repeated again and again, as the body tries to moisten the airways in this way, pushing the mucus out of the bronchi. nine0003
.. a coughing fit is repeated again and again, as the body tries to moisten the airways in this way, pushing the mucus out of the bronchi. nine0003 -
Lower the room temperature. If your comfortable bedroom temperature is 22 degrees, lower it to 20. The lower the temperature, the higher the humidity and the easier it is for you to breathe. But do not get carried away: an excessive decrease in degrees will have the opposite effect, and the cough will begin already due to spasms when inhaling cold air. Do not forget: during colds, bronchitis and other ailments, the mucous membranes are very sensitive - use your own well-being as an indicator, and not just a thermometer. nine0003
-
Keep your feet warm. Feet and bronchi are far apart, but still within the same circulatory system. The warmer the legs, the greater the flow of blood to them and, as a result, its outflow from the upper respiratory tract.
 This will help calm the cough by relieving swelling of the mucous membranes and making it more efficient to clear mucus from the bronchi.
This will help calm the cough by relieving swelling of the mucous membranes and making it more efficient to clear mucus from the bronchi. -
Drink plenty of water. It is generally accepted that the consumption of a large amount of liquid makes sense only in viral diseases that are accompanied by an increase in body temperature. But with a wet night cough, drinking plenty of water helps no less: compotes and tea that you drink during the day reduce the viscosity of not only blood, but also other fluids, including mucus, which your bronchi try to push out during coughing fits. Make it easy for them: don't forget to drink more. nine0003
-
Do not eat at night. A full stomach is one of the night cough provocateurs even in a healthy person. Moreover, a late dinner can worsen the condition with bronchitis. Make sure that the last meal is no later than 2 hours before you take a horizontal position and the likelihood that a night cough will interfere with sleep will be much less.