Dairy allergy symptoms kids
What should I do if I think my baby is allergic or intolerant to cows' milk?
If you think your baby is having a reaction to cows' milk, see your GP or health visitor to discuss your concerns.
They will be able to assess if your baby's symptoms may be caused by a cows' milk allergy or something else. Make sure you get medical advice before taking cows' milk out of your child's diet as it contains important nutrients.
Cows' milk allergy in babies
Cows' milk allergy (CMA), also called cows' milk protein allergy, is one of the most common childhood food allergies. It is estimated to affect around 7% of babies under 1, though most children grow out of it.
CMA typically develops when cows' milk is first introduced into your baby's diet either in formula or when your baby starts eating solids.
More rarely, it can affect babies who are exclusively breastfed because of cows' milk from the mother's diet passing to the baby through breast milk.
There are 2 main types of CMA:
- immediate CMA – where symptoms typically begin within minutes of having cows' milk
- delayed CMA – where symptoms typically begin several hours, or even days, after having cows' milk
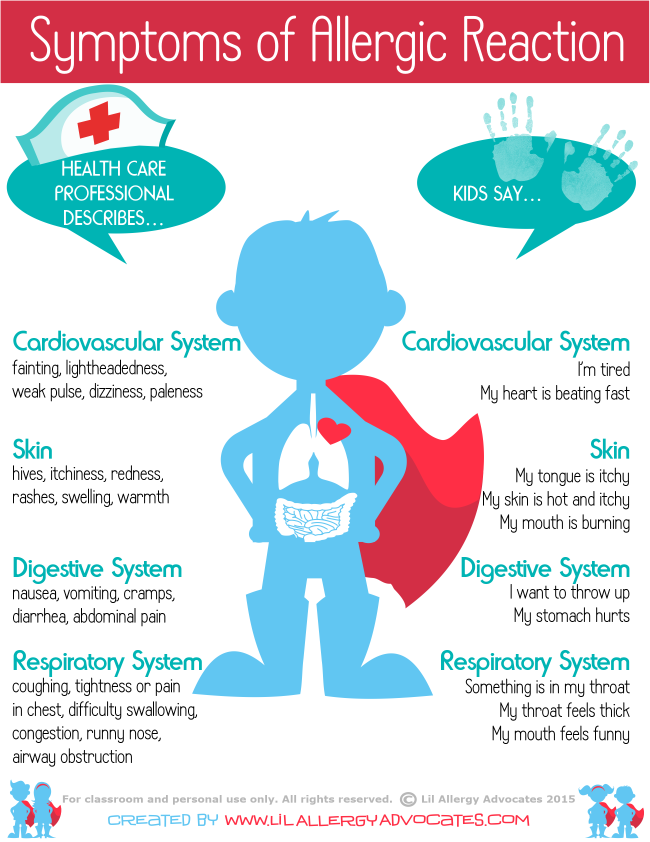
Symptoms of cows' milk allergy
Cows' milk allergy can cause a wide range of symptoms, including:
- skin reactions – such as an itchy rash or swelling of the lips, face and around the eyes
- digestive problems – such as stomach ache, vomiting, colic, diarrhoea or constipation
- hay fever-like symptoms – such as a runny or blocked nose
- eczema that does not improve with treatment
Occasionally CMA can cause severe allergic symptoms that come on suddenly, such as swelling in the mouth or throat, wheezing, cough, shortness of breath, and difficult, noisy breathing.
A severe allergic reaction (anaphylaxis) is a medical emergency. Call 999 for an ambulance immediately if you think your child has anaphylaxis (even if they start to feel better).
Treatment for CMA
If your baby is diagnosed with CMA, you'll be offered advice by your GP or an allergy specialist on how to manage their allergy. You may also be referred to a dietitian.
Treatment involves removing all cows' milk from your child's diet for a period of time.
If your baby is formula-fed, your GP can prescribe special infant formula.
Do not give your child any other type of milk without first getting medical advice.
If your baby is exclusively breastfed, the mother will be advised to avoid all cows' milk products.
Your child should be assessed around every 6 to 18 months to see if they have grown out of their allergy.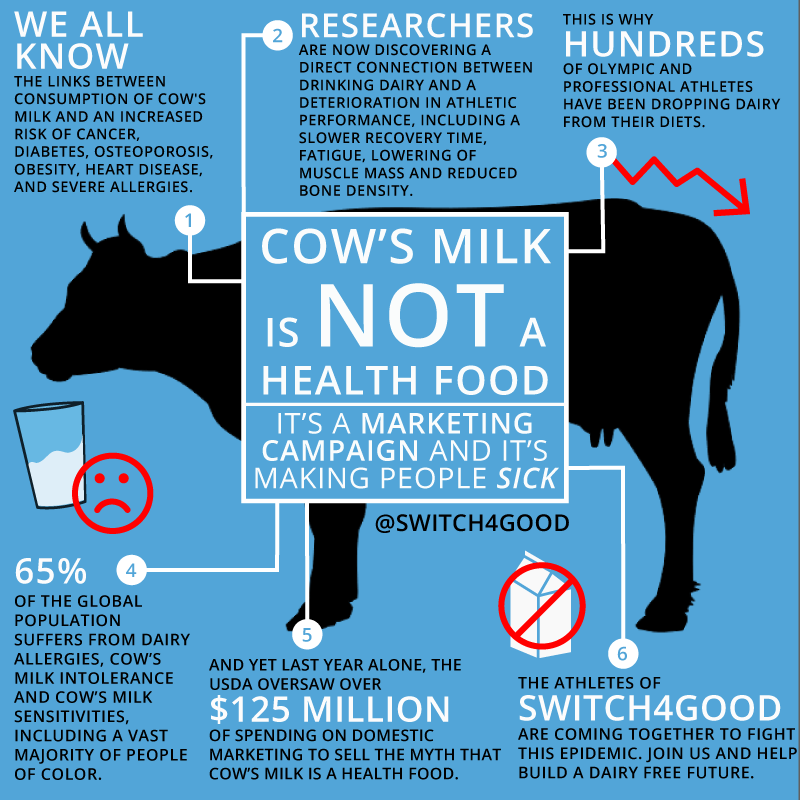
Read more about cows' milk allergy in children on National Institute for Health and Care Excellence (NICE).
Could it be lactose intolerance?
Lactose intolerance is another type of reaction to milk, when the body cannot digest lactose, a natural sugar found in milk. However, this is not an allergy.
Lactose intolerance can be temporary – for example, it can come on for a few days or weeks after a tummy bug.
Symptoms of lactose intolerance include:
- diarrhoea
- vomiting
- stomach rumbling and pains
- wind
Treatment for lactose intolerance
Treatment depends on the extent of your child's intolerance. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.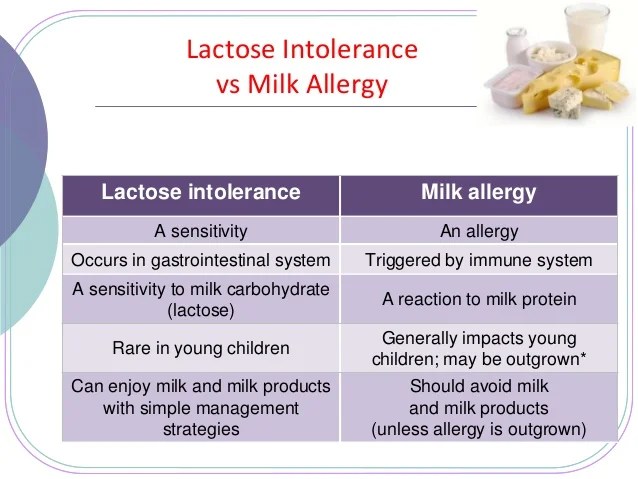
Your child may be referred to a dietitian for specialist advice.
Read more about treatment for lactose intolerance.
Further information:
- Colic
- Food allergies in babies and children
- Reflux in babies
- How can I tell if my baby is seriously ill?
- Your baby's first solid foods
- National Institute for Health and Care Excellence (NICE): food allergy in children
Page last reviewed: 28 November 2022
Next review due: 28 November 2025
Milk Allergy (for Parents) - Nemours KidsHealth
What Is Milk Allergy?
When someone has a milk allergy, the body's immune system, which normally fights infections, overreacts to proteins in milk. If the person drinks or eats a product that contains milk, the body thinks these proteins are harmful invaders. The immune system responds by working very hard to fight off the invader. This causes an allergic reaction.
The immune system responds by working very hard to fight off the invader. This causes an allergic reaction.
Milk is among the most common foods that cause allergic reactions. Some kids with a milk allergy outgrow it as they get older.
What Happens in a Milk Allergy?
People who are allergic to milk react to one or more of the proteins in it. Some people are allergic to casein (KAY-seen) protein and some are allergic to whey (WAY) protein. Some people are allergic to both casein and whey.
When a person with a milk allergy eats these proteins, the body releases chemicals like histamine. This can cause symptoms like:
- wheezing
- trouble breathing
- coughing
- hoarseness
- throat tightness
- belly pain
- vomiting
- diarrhea
- itchy, watery, or swollen eyes
- hives
- swelling
- a drop in blood pressure, causing lightheadedness or loss of consciousness
Allergic reactions to milk can vary. Sometimes the same person can react differently at different times. Some reactions to milk are mild and involve only one part of the body, like hives on the skin. But even when someone has had only a mild reaction in the past, the next reaction can be serious.
Sometimes the same person can react differently at different times. Some reactions to milk are mild and involve only one part of the body, like hives on the skin. But even when someone has had only a mild reaction in the past, the next reaction can be serious.
Milk allergies can cause a severe reaction called anaphylaxis. Anaphylaxis can begin with some of the same symptoms as a less severe reaction, but can quickly get worse. The person may have trouble breathing or pass out. More than one part of the body might be involved. Anaphylaxis that isn't treated can be life-threatening.
Milk allergy is often confused with lactose intolerance because it can cause some of the same symptoms, like belly pain or diarrhea. While lactose intolerance can upset someone’s digestive system, it can’t cause a life-threatening reaction the way that a milk allergy can.
How Is a Milk Allergy Diagnosed?
If your child might have a milk allergy, the doctor may want you to go to an allergist or allergy specialist for more testing.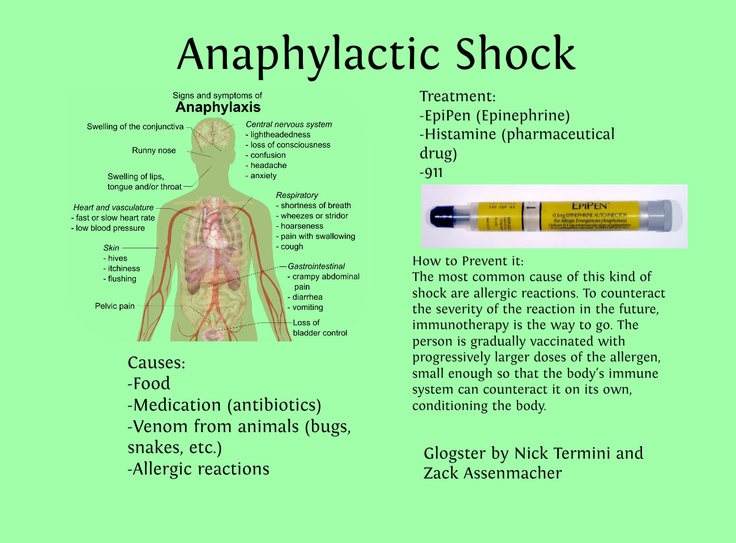 They will ask about how often the reaction happens, the time it takes between when your child eats a particular food and the start of the symptoms, and whether any family members have allergies or conditions like eczema and asthma.
They will ask about how often the reaction happens, the time it takes between when your child eats a particular food and the start of the symptoms, and whether any family members have allergies or conditions like eczema and asthma.
The allergy specialist may do a skin test. This involves placing tiny amounts of milk protein on your child’s forearm or back, making a small scratch or prick on the skin, and waiting to see if a reddish, raised spot forms. If so, it may indicate a milk allergy.
Your child may need to stop taking some medicines (such as over-the-counter antihistamines) 5 to 7 days before the skin test because they can affect the results. Check with the allergist's office if you’re not sure about what medicines to stop or for how long.
An allergist might do a blood test as well as skin testing. A small blood sample will go to a lab for testing. The lab checks the blood for IgE antibodies to specific foods. If your child’s blood has enough IgE antibodies to milk, a milk allergy is very likely.
If the results of the skin and blood tests are still unclear, though, an allergist might do something called a food challenge. During this test, your child will get slowly increasing amounts of milk while the doctor watches for symptoms.
How Is an Allergic Reaction to Milk Treated?
Kids with a milk allergy should always carry two epinephrine auto-injectors in case of a severe reaction. An epinephrine auto-injector is a prescription medicine that comes in a small, easy-to-carry container. It's easy to use. Your doctor will show you how. Always have two auto injectors with your child in case one doesn't work or they need a second dose.
The doctor can also give you an allergy action plan, which helps you prepare for, recognize, and treat an allergic reaction. Share the plan with anyone else who needs to know, such as other caregivers, babysitters, relatives, school officials, and coaches. Also consider having your child wear a medical alert bracelet.
Every second counts in an allergic reaction. If your child has serious allergic symptoms, like trouble breathing or throat tightness, use the epinephrine auto-injector right away. Also use it right away if your child’s symptoms involve two different parts of the body, like hives with vomiting. Then call 911 and have them take your child to the emergency room. This is because even if the worst seems to have passed, a second wave of serious symptoms can happen.
What Else Should I Know?
Kids with a milk allergy must not eat or drink any products that contain milk or milk proteins.
Be sure to read food labels carefully and teach your child to do the same. Milk and milk proteins can be in unexpected places, such as processed lunchmeats, salad dressings, baked goods, chocolate, and crackers. Even foods that say “non-dairy” still may contain milk protein.
One thing that might not show up on a label is cross-contamination risk. This can happen if a manufacturer uses the same equipment to grind lots of different foods, for example. Some companies put statements on their labels about the risk of cross-contamination, like: "May contain milk," "Processed in a facility that also processes milk," or "Manufactured on equipment also used for milk." Your child should avoid products that have these kinds of alerts.
Some companies put statements on their labels about the risk of cross-contamination, like: "May contain milk," "Processed in a facility that also processes milk," or "Manufactured on equipment also used for milk." Your child should avoid products that have these kinds of alerts.
But companies are not required to put cross-contamination alerts on a food label. So it's best to contact the company to see if a product might have come in contact with milk. You may be able to get this information from a company website. If not, contact the company and ask.
Reviewed by: Larissa Hirsch, MD
Date reviewed: January 2021
Allergy to cow's milk proteins (CMP)
- Nestlé Health Science
- health care
- The concept of "Allergy to cow's milk proteins (CMP)"
The concept of cow's milk protein allergy (CMP)
What is a food allergy?
Food allergies occur when the body's immune system (the body's own defense mechanism) reacts incorrectly to certain foods. Normally, the immune system helps the body fight harmful things, such as infectious agents. In a food allergy, the immune system misrecognizes certain food components as harmful, leading to unpleasant and sometimes life-threatening allergy-related signs and symptoms. nine0017 More than 120 foods are known to cause food allergies. Cow's milk protein allergy (CMP) is the most common type of food allergy in infants under one year of age.
Normally, the immune system helps the body fight harmful things, such as infectious agents. In a food allergy, the immune system misrecognizes certain food components as harmful, leading to unpleasant and sometimes life-threatening allergy-related signs and symptoms. nine0017 More than 120 foods are known to cause food allergies. Cow's milk protein allergy (CMP) is the most common type of food allergy in infants under one year of age.
Do not confuse CMPA with lactose intolerance
Sometimes CMPA is confused with lactose intolerance. Both diseases have some common signs and symptoms, but different causes and treatments.
CMPA usually develops at an early age, while lactose intolerance is extremely rare before the age of 5 years. nine0013
What is ABKM?
CMA is a type of food allergy in which the child's immune system reacts to proteins found in cow's milk. As a result, the child develops allergy symptoms: skin problems (rash, hives, dry, flaky or itchy skin), digestive system disorders (diarrhea, vomiting, constipation and reflux) and respiratory problems (noisy breathing, cough, runny nose). CMPA usually occurs before a child's first birthday. nine0013
CMPA usually occurs before a child's first birthday. nine0013
What is lactose intolerance?
Unlike CMPA, lactose intolerance does not depend on the immune system. This is actually lactase deficiency, the inability to digest the lactose sugar found in cow's milk, and is very rare in children under 5 years of age. Lactose is one of the most important carbohydrates (sugars) in breast milk and is very beneficial for babies. Lactose promotes healthy intestinal flora and calcium absorption. nine0013
Cow's milk protein allergy and lactose intolerance are different diseases
learn more about cow's milk protein allergy
All about CMPA
How common is CMPA?
Is CMPA hereditary?
Why does my child have CMPA?
Can CMPA be cured?
What is the difference between the AAA line and hypoallergenic formulas?
Your steps towards the diagnosis of CMPA
Allergy symptoms can be frightening, but CMPA can be easily managed with the right diet, so it's important to get the right diagnosis from your doctor and get treatment on time. If you notice any symptoms in your child that could be associated with CMPA, first of all, don't worry. Discuss the problems with the doctor, the doctor will take the necessary actions to make a final diagnosis. Follow the links below for information and guidance regarding the diagnosis of CMPA and the common signs and symptoms of CMPA. nine0013
If you notice any symptoms in your child that could be associated with CMPA, first of all, don't worry. Discuss the problems with the doctor, the doctor will take the necessary actions to make a final diagnosis. Follow the links below for information and guidance regarding the diagnosis of CMPA and the common signs and symptoms of CMPA. nine0013
SIGNS AND SYMPTOMS OF CMPA
CMPA is a food allergy, but symptoms can affect more than just the digestive system, they can also affect the respiratory system and skin.
Learn more about the signs and symptoms of CMPA
Symptom Analysis
Diagnosis
To make a diagnosis, the doctor will examine the child and ask about any symptoms you may notice. If an allergy to cow's milk proteins is suspected, a doctor may do certain tests. Once diagnosed, the symptoms of CMPA can be easily managed under the experienced guidance of a physician.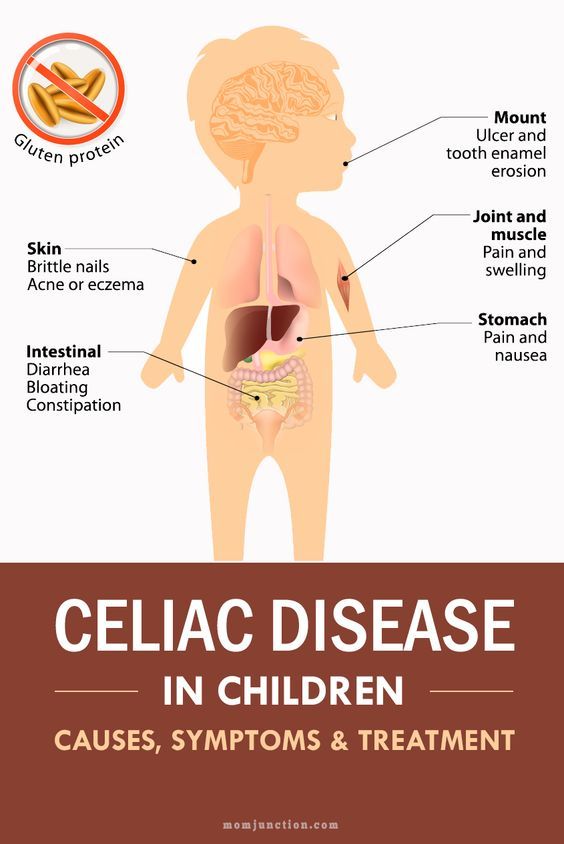 nine0013
nine0013
Find out more about the diagnosis of CMDD
Get ready for your doctor's visit
Would you like some help preparing for your doctor's visit? By printing and completing My Child's Symptom Diary, you can be sure that your doctor will have all the information you need to make an accurate diagnosis.
Symptom diary
IMPORTANT NOTE: Breastfeeding may continue if the infant is allergic to cow's milk protein. To do this, the mother needs a special diet with the exclusion of all sources of cow's milk protein. Only if these measures do not bring the desired effect, the doctor recommends the use of a special therapeutic mixture intended for children from 0 to 1 year old. It is important to follow the correct methods of preparing the mixture: using boiled water, sterilized bottles and following the rules for diluting the mixture. Medicinal mixtures intended for diet therapy of CMPA should be used under the supervision of a physician. nine0013
nine0013
Good to know about MILK ALLERGY (melk)
MILK ALLERGY
Useful information about milk allergy – Information sheet of the Norwegian Asthma and Allergy Association
What is milk allergy?
When allergic to cow's milk protein, a strong reaction of the body's immune system may be the production of antibodies (IgE), or the activation of inflammatory cells. With every meal containing milk proteins, an allergic reaction of the immune system is observed in the form of the production of mediators, such as histamine, or a T-cell inflammatory reaction. Histamine is produced in several places in the body and leads to symptoms such as diarrhea, nausea, abdominal pain, or skin lesions (urticaria, eczema). nine0013
Cow's milk contains over 25 different proteins that can cause a reaction in "milk" allergies. For most people, an allergic reaction can be caused by more than one type of protein. The milk of other artiodactyls such as goat, horse and buffalo contains many of the same proteins. Therefore, allergy sufferers should not consume artiodactyl milk at all.
Therefore, allergy sufferers should not consume artiodactyl milk at all.
If a breastfeeding mother consumes cow's milk herself, some proteins may be transferred with mother's milk to the baby's body and lead to negative consequences. Therefore, a breastfeeding mother should follow a dairy-free diet. nine0013
Cow's milk allergy is not the same as lactose intolerance. The latter occurs due to the reduced ability of the body to digest milk sugar (lactose). Lactose intolerance leads to stomach pain and diarrhea as a consequence of eating large amounts of dairy products with high levels of lactose (sweet milk, brown (goat) cheese, ice cream and cream).
Symptoms
The symptoms of a milk allergy are very individual. For some, they are minor and harmless, while for others, a severe allergic reaction can occur, even when drinking a small amount of milk. Gastrointestinal tract disorder is common. Not so often there is itching in the mouth and throat, swelling of the mucous membrane and breathing problems, which is especially true for young children. It is also common for them to develop eczema and hives on the skin. nine0013
It is also common for them to develop eczema and hives on the skin. nine0013
Who is affected?
Milk allergy is the most common type of allergy in young children, which is explained by the early introduction of cow's milk into the diet of infants (for example, in cereals or mother's milk substitute). About 2-5% of Norwegian babies (0-3 years old) suffer from this type of allergy.
Diagnosis
In order to determine the presence of milk allergy, the doctor must read the patient's medical history, as well as take a blood test for allergic antibodies and a Pirquet test. Not all milk allergy sufferers will show positive results from these tests. This is especially true for infants with symptoms such as vomiting, diarrhea, or blood in the stool. The only reliable way to find out if milk causes these symptoms is to eliminate milk from the diet for a period of time. When in doubt, reintroduce it back into the diet and see if symptoms return. For children who have not received milk for some time due to allergies, a control test using cow's milk should be performed to ensure that there is no allergic reaction. nine0013
nine0013
Predictions
Generally, cow's milk allergy has a fairly good prognosis. Most of the children get rid of it before reaching school age. Babies who have had negative test results are often allowed to resume milk intake after half a year or a year. It is not known how many adults suffer from milk allergy, but it is estimated that this number does not exceed one percent of the population.
Where is milk protein found?
Milk is found in many processed and prepared industrial foods. Therefore, when buying a product, it is important to familiarize yourself with the list of substances contained in it. The goods declaration must list all ingredients containing milk. A certain group of words used in such lists indicates the content of milk protein in the product: butter, yogurt, yogurt powder. nine0145
Cocoa butter, lactic acids and group E substances do not contain milk protein.
Diet
Milk is an important source of nutrients in the Norwegian diet. 25% of the protein given to children, 70% of the iodine and about 70% of the calcium are obtained from dairy products. That is why, in cases of exclusion of dairy products from the diet, these products should be replaced with others that will provide the intake of the above nutrients. Alternatively, specially formulated additives can be used. nine0013
25% of the protein given to children, 70% of the iodine and about 70% of the calcium are obtained from dairy products. That is why, in cases of exclusion of dairy products from the diet, these products should be replaced with others that will provide the intake of the above nutrients. Alternatively, specially formulated additives can be used. nine0013
How to replace milk?
- Drinks: For small children, a hypoallergenic milk substitute is recommended, available from a pharmacy. These products can be purchased at a pharmacy or obtained from a blue prescription (prescription prescription). Because older children can be difficult to accustom to these milk substitutes due to their taste, it is recommended to start using substitutes as early as possible, for example during breastfeeding. Youth and adults can consume milk substitutes such as rice milk, oat milk, etc. The amount of calcium contained in these products corresponds to the calcium content in cow's milk, however, these drinks often contain less protein and nutrients.