How to tell if baby is lactose intolerant formula
Lactose Intolerance Symptoms in Babies: What to Know
Cow’s milk can do a number on the tummy — in adults and children. While that doesn’t always stop us from eating a bowl of ice cream, we may pay for it later with that familiar stomach gurgling.
Usually, it’s the lactose in milk that’s the culprit of tummy troubles. If you’re lactose intolerant, your body can’t digest lactose — the sugar in dairy products. And as a result, drinking milk or eating dairy products like cheese or yogurt can cause symptoms ranging from stomach cramps to diarrhea.
Many adults live with a lactose intolerance. In fact, it’s estimated to affect as many as 30 to 50 million American adults. But more rarely, babies can have it as well.
Here’s what you need to know about lactose intolerance in babies, as well as how an intolerance affects breastfeeding and formula feeding.
Of course, if your baby appears to have trouble digesting dairy, this doesn’t necessarily mean that they’re lactose intolerant. Their symptoms could be caused by something else. (Nothing about parenthood is ever simple, is it?)
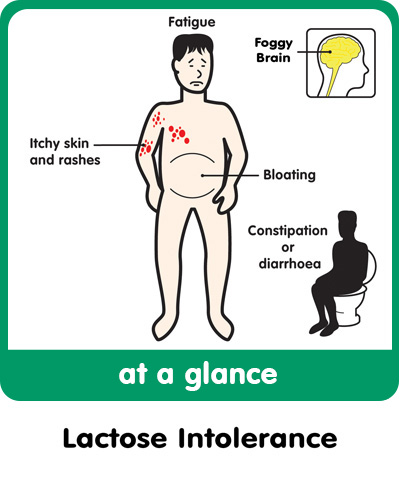
But typically, symptoms of a lactose intolerance in babies include:
- diarrhea (check out our guide to lactose intolerant baby poop)
- stomach cramping
- bloating
- gas
Since babies can’t talk, they can’t explain what’s bothering them. So it’s not always easy to tell when they’re having stomach issues.
Signs of stomach pain might include:
- clenching their fists
- arching their backs
- kicking or lifting their legs
- crying while passing gas
A bloated stomach may look slightly larger than normal and feel hard to the touch.
Another sign of lactose intolerance is symptoms starting shortly after feedings — within 30 minutes to 2 hours of consuming breast milk, milk-based formula, or solid foods containing dairy.
Keep in mind, too, that your baby might not have a problem with lactose, but rather a milk allergy.
Milk allergy symptoms are similar to symptoms of a lactose intolerance, but these conditions aren’t the same.
A milk allergy is a type of food allergy that occurs when the immune system overreacts to dairy. If your baby has a milk allergy, they may have an upset stomach and diarrhea. But they’ll also have symptoms that don’t occur with an intolerance:
- wheezing
- coughing
- swelling
- itching
- watery eyes
- vomiting
If you suspect a milk allergy — even a mild allergy — see your doctor. A milk allergy can advance and cause severe symptoms like a drop in blood pressure, trouble breathing, and anaphylaxis. According to Food Allergy Research and Education, milk allergies affect about 2.5 percent of children under 3 years old.
Most people with a lactose intolerance don’t develop symptoms until later in life when their body’s natural production of lactase — the enzyme that helps the body digest lactose — declines.
This decline doesn’t usually take place until later in childhood, during the teenage years, or in adulthood.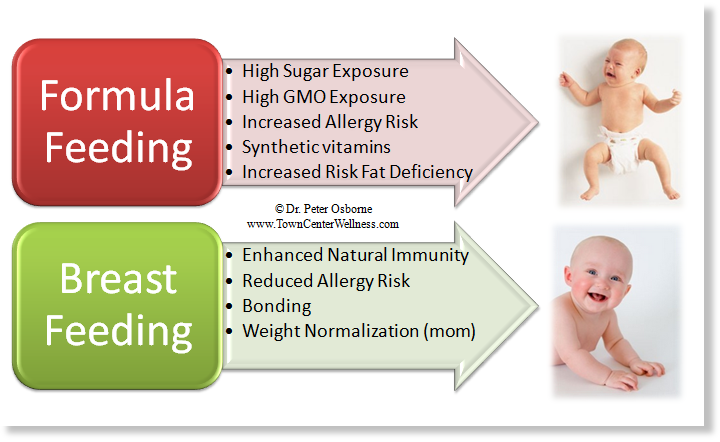 So lactose intolerance in babies under age 1 is pretty rare — but it’s not impossible.
So lactose intolerance in babies under age 1 is pretty rare — but it’s not impossible.
Congenital lactase deficiency
Some babies have a lactose intolerance because they’re born without any lactase enzymes to begin with. This is known as congenital lactase deficiency, and if your baby has this deficiency, you’ll know it almost immediately after birth. They’ll have symptoms after drinking breast milk — which also contains lactose — or formula based in cow’s milk.
It’s unknown how many babies are born with this condition worldwide. Interesting fact: It seems to be most common in Finland, where about 1 in 60,000 newborns can’t digest lactose. (Note that this is still pretty rare!)
The cause of this deficiency is a mutation of the LCT gene, which essentially instructs the body to produce the enzyme needed to digest lactose. This is an inherited condition, so babies inherit this gene mutation from both of their parents.
Developmental lactase deficiency
Some premature infants are born with a developmental lactase deficiency.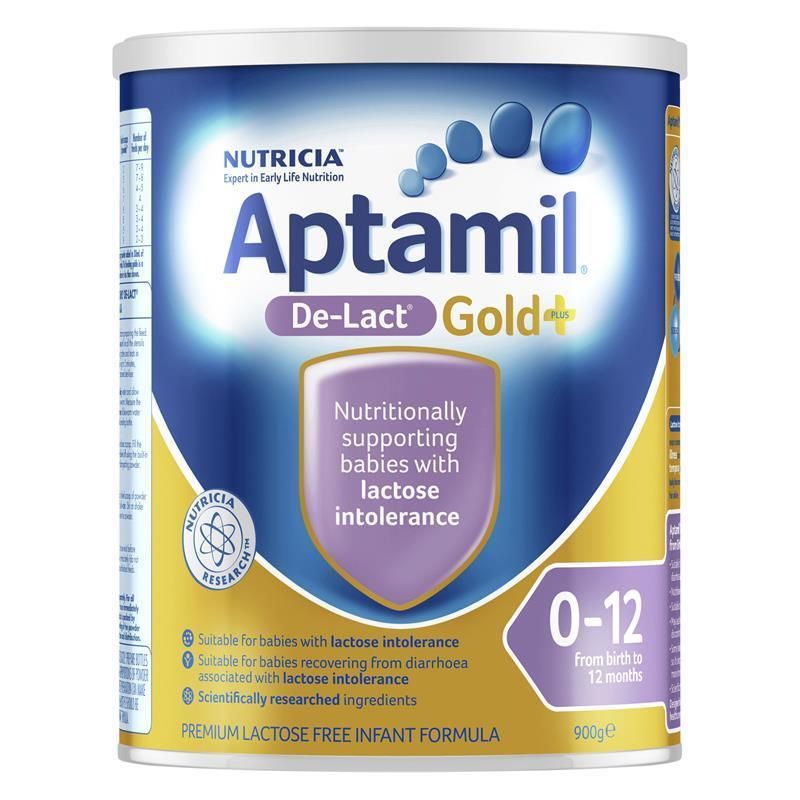 This is a temporary intolerance that occurs in infants born before their small intestines are fully developed (generally, before 34 weeks gestation).
This is a temporary intolerance that occurs in infants born before their small intestines are fully developed (generally, before 34 weeks gestation).
Also, some babies develop a temporary lactose intolerance after a viral illness, like gastroenteritis.
If your baby has signs of a lactose intolerance, don’t diagnose the condition yourself. Talk to your pediatrician. They’ll have more experience distinguishing between a lactose intolerance and a milk allergy.
Since a lactose intolerance is uncommon in infants, your doctor may refer you to an allergist to rule out a dairy allergy after also ruling out other common digestive issues.
The allergist may expose your baby’s skin to a small amount of milk protein, and then monitor their skin for an allergic reaction.
If your baby doesn’t have a milk allergy, your doctor may take a stool sample to check the acidity of their poop. Low acidity can be a sign of lactose malabsorption, and traces of glucose is evidence of undigested lactose.
Your doctor may also suggest removing lactose from their diet for 1 to 2 weeks to see if their digestive symptoms improve.
If diagnostic testing confirms a lactose intolerance, don’t immediately panic and stop breastfeeding. Whether you’re able to continue breastfeeding depends on the type of lactase deficiency.
For example, if your baby develops a lactose intolerance after a viral illness, the general recommendation is to continue breastfeeding. Breast milk can give their immune system a boost and help heal their gut.
If your infant has developmental lactase deficiency due to a premature birth, this condition only lasts a few weeks or months. So your baby may eventually drink milk-based formula or breast milk with no problem, although you’ll need to use lactose-free infant formula in the meantime.
But breastfeeding isn’t an option if your baby has a congenital lactase deficiency. The lactose in your breast milk can cause severe diarrhea and lead to dehydration and electrolyte loss. You’ll need to feed your baby with lactose-free infant formula.
You’ll need to feed your baby with lactose-free infant formula.
Lactose intolerance following a viral illness or a premature birth is usually temporary — hooray! — and your baby’s body may eventually produce normal levels of the lactase enzyme to digest the sugar in milk.
But a congenital lactase deficiency is a lifelong condition, and you’ll need to modify your little one’s diet to avoid symptoms.
The good news is that lactose-free infant formulas contain nutrients — like calcium, vitamin D, and vitamin A — that babies receive from drinking lactose-based products. (And there’s never been a better time to grow up with lactose intolerance, as so many people are going dairy-free by choice.)
Foods to avoid
When you buy food for your baby, read labels and don’t purchase items containing lactose (whey, milk by-products, nonfat dry milk powder, dry milk solids, and curds).
Popular baby-friendly foods that may contain lactose include:
- yogurt
- prepared oatmeal
- formula
- instant mashed potatoes
- pancakes
- biscuits (including teething biscuits)
- cookies
- pudding
- sherbet
- ice cream
- cheese
Q: If my baby’s lactose intolerant and I’m breastfeeding, will it help if I quit eating lactose or will I still have to switch to a dairy-free formula?
A: Taking dairy or lactose out of your diet will not reduce the lactose in your breast milk. Breast milk naturally contains lactose.
Breast milk naturally contains lactose.
Depending on the type of lactose intolerance your baby has, you may have to switch to a lactose-free formula. Some lactose intolerance is a short-term situation and will resolve over time. Congenital lactose intolerance will not go away and your child will have to remain lactose free for their whole life.
Please make all changes to your baby’s diet with the assistance of your healthcare provider.
— Carissa Stephens, RN
Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
An inability to digest the sugar in milk can be uncomfortable for a baby, but diarrhea, gas, and stomach pain don’t always mean lactose intolerance. These symptoms could indicate a milk allergy, general digestive problems common in the first 3 months of life, or something else.
If you believe that your baby has trouble digesting milk, see your pediatrician for a diagnosis.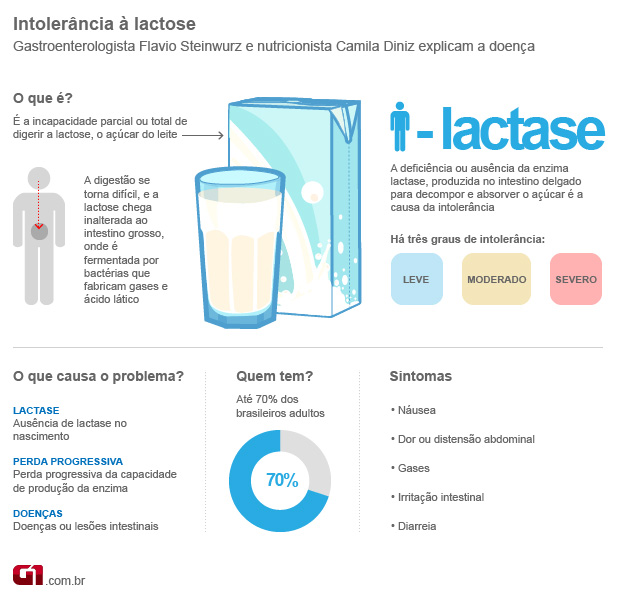 And take heart — while a diagnosis may seem daunting at first, it’ll put you well on your way to having a happier, less fussy baby.
And take heart — while a diagnosis may seem daunting at first, it’ll put you well on your way to having a happier, less fussy baby.
Lactose Intolerance Symptoms in Babies: What to Know
Cow’s milk can do a number on the tummy — in adults and children. While that doesn’t always stop us from eating a bowl of ice cream, we may pay for it later with that familiar stomach gurgling.
Usually, it’s the lactose in milk that’s the culprit of tummy troubles. If you’re lactose intolerant, your body can’t digest lactose — the sugar in dairy products. And as a result, drinking milk or eating dairy products like cheese or yogurt can cause symptoms ranging from stomach cramps to diarrhea.
Many adults live with a lactose intolerance. In fact, it’s estimated to affect as many as 30 to 50 million American adults. But more rarely, babies can have it as well.
Here’s what you need to know about lactose intolerance in babies, as well as how an intolerance affects breastfeeding and formula feeding.
Of course, if your baby appears to have trouble digesting dairy, this doesn’t necessarily mean that they’re lactose intolerant. Their symptoms could be caused by something else. (Nothing about parenthood is ever simple, is it?)
But typically, symptoms of a lactose intolerance in babies include:
- diarrhea (check out our guide to lactose intolerant baby poop)
- stomach cramping
- bloating
- gas
Since babies can’t talk, they can’t explain what’s bothering them. So it’s not always easy to tell when they’re having stomach issues.
Signs of stomach pain might include:
- clenching their fists
- arching their backs
- kicking or lifting their legs
- crying while passing gas
A bloated stomach may look slightly larger than normal and feel hard to the touch.
Another sign of lactose intolerance is symptoms starting shortly after feedings — within 30 minutes to 2 hours of consuming breast milk, milk-based formula, or solid foods containing dairy.
Keep in mind, too, that your baby might not have a problem with lactose, but rather a milk allergy.
Milk allergy symptoms are similar to symptoms of a lactose intolerance, but these conditions aren’t the same.
A milk allergy is a type of food allergy that occurs when the immune system overreacts to dairy. If your baby has a milk allergy, they may have an upset stomach and diarrhea. But they’ll also have symptoms that don’t occur with an intolerance:
- wheezing
- coughing
- swelling
- itching
- watery eyes
- vomiting
If you suspect a milk allergy — even a mild allergy — see your doctor. A milk allergy can advance and cause severe symptoms like a drop in blood pressure, trouble breathing, and anaphylaxis. According to Food Allergy Research and Education, milk allergies affect about 2.5 percent of children under 3 years old.
Most people with a lactose intolerance don’t develop symptoms until later in life when their body’s natural production of lactase — the enzyme that helps the body digest lactose — declines.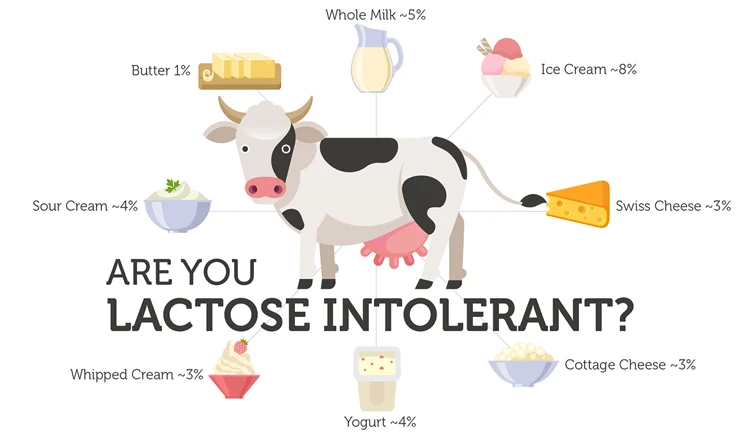
This decline doesn’t usually take place until later in childhood, during the teenage years, or in adulthood. So lactose intolerance in babies under age 1 is pretty rare — but it’s not impossible.
Congenital lactase deficiency
Some babies have a lactose intolerance because they’re born without any lactase enzymes to begin with. This is known as congenital lactase deficiency, and if your baby has this deficiency, you’ll know it almost immediately after birth. They’ll have symptoms after drinking breast milk — which also contains lactose — or formula based in cow’s milk.
It’s unknown how many babies are born with this condition worldwide. Interesting fact: It seems to be most common in Finland, where about 1 in 60,000 newborns can’t digest lactose. (Note that this is still pretty rare!)
The cause of this deficiency is a mutation of the LCT gene, which essentially instructs the body to produce the enzyme needed to digest lactose. This is an inherited condition, so babies inherit this gene mutation from both of their parents.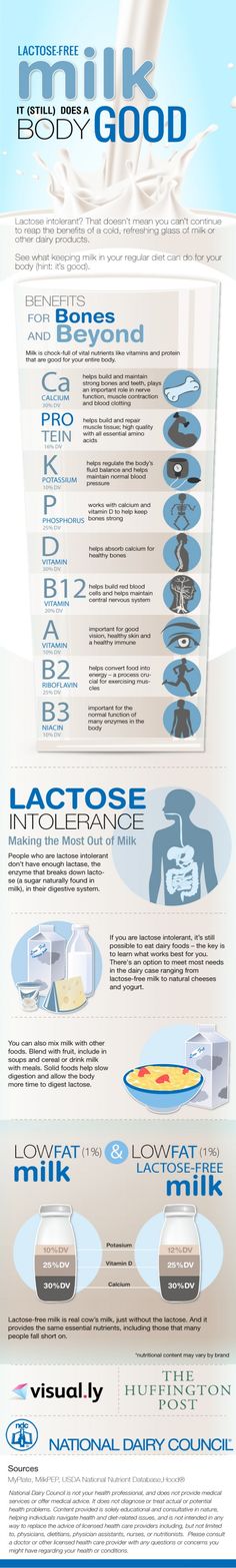
Developmental lactase deficiency
Some premature infants are born with a developmental lactase deficiency. This is a temporary intolerance that occurs in infants born before their small intestines are fully developed (generally, before 34 weeks gestation).
Also, some babies develop a temporary lactose intolerance after a viral illness, like gastroenteritis.
If your baby has signs of a lactose intolerance, don’t diagnose the condition yourself. Talk to your pediatrician. They’ll have more experience distinguishing between a lactose intolerance and a milk allergy.
Since a lactose intolerance is uncommon in infants, your doctor may refer you to an allergist to rule out a dairy allergy after also ruling out other common digestive issues.
The allergist may expose your baby’s skin to a small amount of milk protein, and then monitor their skin for an allergic reaction.
If your baby doesn’t have a milk allergy, your doctor may take a stool sample to check the acidity of their poop. Low acidity can be a sign of lactose malabsorption, and traces of glucose is evidence of undigested lactose.
Low acidity can be a sign of lactose malabsorption, and traces of glucose is evidence of undigested lactose.
Your doctor may also suggest removing lactose from their diet for 1 to 2 weeks to see if their digestive symptoms improve.
If diagnostic testing confirms a lactose intolerance, don’t immediately panic and stop breastfeeding. Whether you’re able to continue breastfeeding depends on the type of lactase deficiency.
For example, if your baby develops a lactose intolerance after a viral illness, the general recommendation is to continue breastfeeding. Breast milk can give their immune system a boost and help heal their gut.
If your infant has developmental lactase deficiency due to a premature birth, this condition only lasts a few weeks or months. So your baby may eventually drink milk-based formula or breast milk with no problem, although you’ll need to use lactose-free infant formula in the meantime.
But breastfeeding isn’t an option if your baby has a congenital lactase deficiency. The lactose in your breast milk can cause severe diarrhea and lead to dehydration and electrolyte loss. You’ll need to feed your baby with lactose-free infant formula.
The lactose in your breast milk can cause severe diarrhea and lead to dehydration and electrolyte loss. You’ll need to feed your baby with lactose-free infant formula.
Lactose intolerance following a viral illness or a premature birth is usually temporary — hooray! — and your baby’s body may eventually produce normal levels of the lactase enzyme to digest the sugar in milk.
But a congenital lactase deficiency is a lifelong condition, and you’ll need to modify your little one’s diet to avoid symptoms.
The good news is that lactose-free infant formulas contain nutrients — like calcium, vitamin D, and vitamin A — that babies receive from drinking lactose-based products. (And there’s never been a better time to grow up with lactose intolerance, as so many people are going dairy-free by choice.)
Foods to avoid
When you buy food for your baby, read labels and don’t purchase items containing lactose (whey, milk by-products, nonfat dry milk powder, dry milk solids, and curds).
Popular baby-friendly foods that may contain lactose include:
- yogurt
- prepared oatmeal
- formula
- instant mashed potatoes
- pancakes
- biscuits (including teething biscuits)
- cookies
- pudding
- sherbet
- ice cream
- cheese
Q: If my baby’s lactose intolerant and I’m breastfeeding, will it help if I quit eating lactose or will I still have to switch to a dairy-free formula?
A: Taking dairy or lactose out of your diet will not reduce the lactose in your breast milk. Breast milk naturally contains lactose.
Depending on the type of lactose intolerance your baby has, you may have to switch to a lactose-free formula. Some lactose intolerance is a short-term situation and will resolve over time. Congenital lactose intolerance will not go away and your child will have to remain lactose free for their whole life.
Please make all changes to your baby’s diet with the assistance of your healthcare provider.
— Carissa Stephens, RN
Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
An inability to digest the sugar in milk can be uncomfortable for a baby, but diarrhea, gas, and stomach pain don’t always mean lactose intolerance. These symptoms could indicate a milk allergy, general digestive problems common in the first 3 months of life, or something else.
If you believe that your baby has trouble digesting milk, see your pediatrician for a diagnosis. And take heart — while a diagnosis may seem daunting at first, it’ll put you well on your way to having a happier, less fussy baby.
Lactase deficiency in infants: symptoms and diagnosis
Signs of lactase deficiency in infants should be known to parents, because this will allow them to suspect this condition in a timely manner, identify its cause and improve the condition of the baby.
Signs of lactose intolerance
Signs of lactase deficiency in a child are diverse.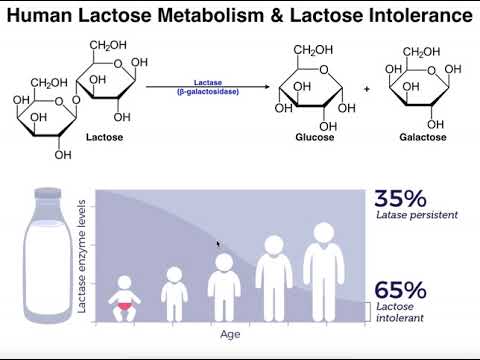 This is a stool with a large water spot and a sour smell, bloating, rumbling, abdominal pain (colic). One of the most common symptoms that worries parents is frequent loose stools in a baby. It is watery, frothy and has a sour smell. It should be remembered that the younger the child, the more frequent his stool, and this is completely normal. So if the baby is developing well and feels good, and his feces are normal, you should not think that these are signs of lactose intolerance in newborns.
This is a stool with a large water spot and a sour smell, bloating, rumbling, abdominal pain (colic). One of the most common symptoms that worries parents is frequent loose stools in a baby. It is watery, frothy and has a sour smell. It should be remembered that the younger the child, the more frequent his stool, and this is completely normal. So if the baby is developing well and feels good, and his feces are normal, you should not think that these are signs of lactose intolerance in newborns.
Sometimes lactase deficiency in newborns is accompanied by poor weight gain and growth. This is due to the fact that the carbohydrates necessary for the child do not enter the body, and the baby may lack nutrients.
If the baby quickly grew out of the recently purchased sliders and sleepsuits, and his cheeks and handles are round and plump, you should not suspect lactase deficiency in the child.
Intestinal colic may be present in children with lactose intolerance. After eating, the child will experience bloating, anxiety, crying.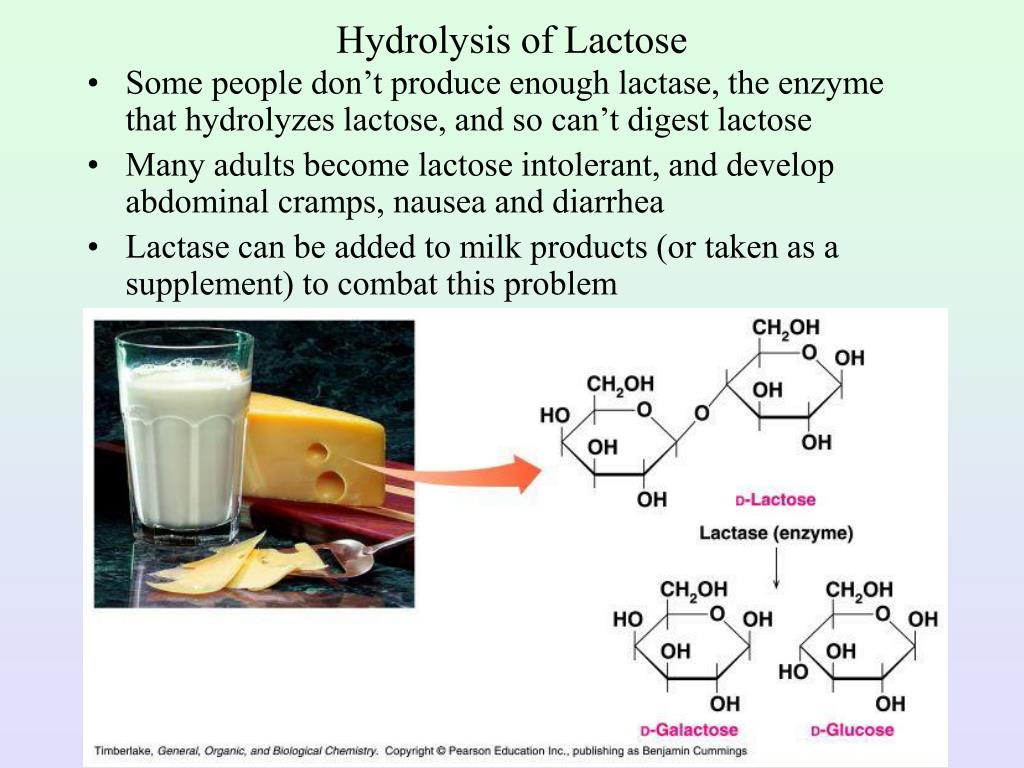 These signs usually appear on the 3-6th week of a baby's life. This is probably due to an increase in milk consumption by an older baby.
These signs usually appear on the 3-6th week of a baby's life. This is probably due to an increase in milk consumption by an older baby.
The mechanism of such manifestations of lactose intolerance as intestinal colic, bloating and rumbling is as follows. Carbohydrates that are not digested due to the absence or lack of the lactase enzyme continue their movement through the intestines. In the colon, they are exposed to intestinal microflora, resulting in the formation of an excess of gases (hydrogen, methane, carbon dioxide). Gas stretches the walls of the intestines, causing bloating, pain and increased intestinal peristalsis. Violation of the normal chemical composition of intestinal contents can lead to disturbances in the composition of the intestinal microflora.
When should you not think about lactase deficiency?
Quite often in recent years, when there are problems with digestion, children are diagnosed with lactose intolerance. However, this is not always true. As mentioned above, the frequency of stool in infants is individual. Frequent or rare stools are not in themselves a sign of lactase deficiency in a child. The symptoms of this pathology are multiple.
As mentioned above, the frequency of stool in infants is individual. Frequent or rare stools are not in themselves a sign of lactase deficiency in a child. The symptoms of this pathology are multiple.
Important!
Sometimes regurgitation is taken as a sign of lactose intolerance by parents. But even if regurgitation is frequent and plentiful, it is unlikely that this is lactase deficiency - the symptoms in children with this pathology are associated with the work of the intestines, and not the esophagus or stomach.
How to identify lactose intolerance
The diagnosis of lactose intolerance usually begins with an organoleptic evaluation of feces. Unformed, watery, frothy yellow or green feces with a sour smell testify in favor of this pathology. In a chemical study, the reaction of feces is acidic (pH less than 5.5).
Another test method is to determine the content of carbohydrates in feces. Exceeding their value by 0.25% is typical for lactase deficiency.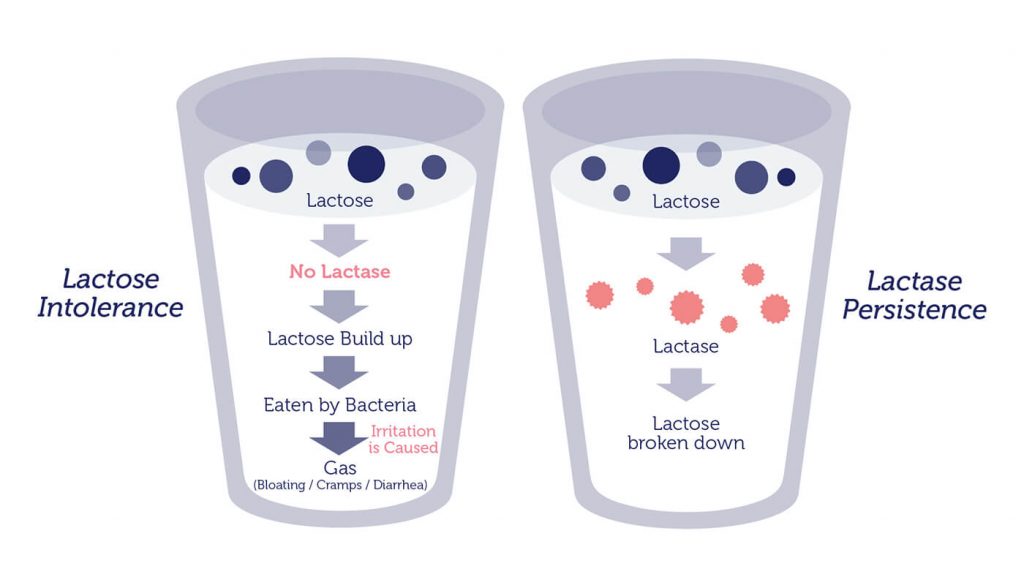 Despite the widespread use, this method is not the most accurate, since it does not allow you to determine which carbohydrates are present in the feces.
Despite the widespread use, this method is not the most accurate, since it does not allow you to determine which carbohydrates are present in the feces.
Important!
Whenever lactose intolerance is suspected, a specialist should be consulted. He will prescribe examinations that will allow you to say if the child has lactose intolerance, or if the symptoms are not associated with this condition.
Other methods are used in difficult cases. For example, a specific breath test based on determining the concentration of hydrogen in exhaled air after a load of lactose. The advantage of this method is its simplicity, the disadvantage is the possibility of false positive results and the impossibility of determining the degree of lactase deficiency.
Lactose curve is another test for lactose intolerance. Normally, lactose, under the action of the lactase enzyme, breaks down into simpler sugars, in particular, glucose. Subsequently, glucose is absorbed through the intestinal wall and enters the bloodstream.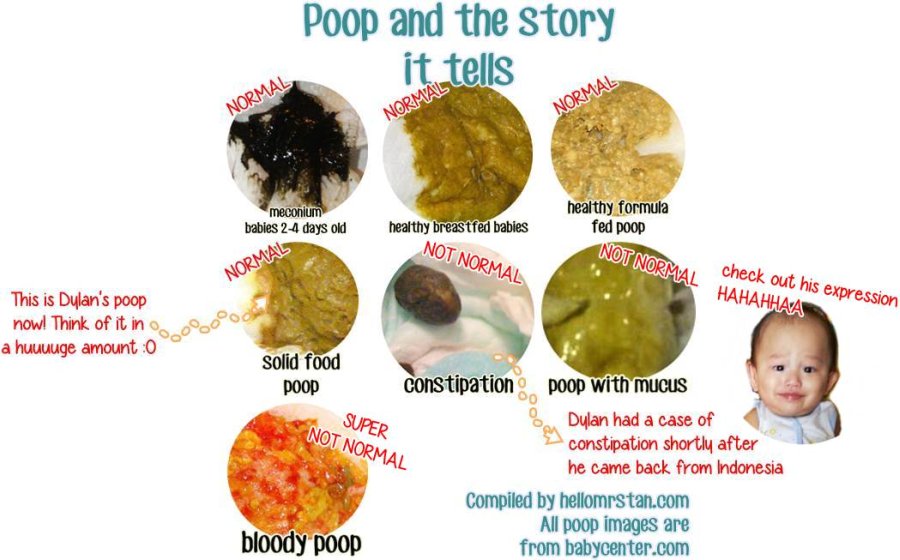 Accordingly, the determination of the level of glucose in the blood on an empty stomach and after taking lactose makes it possible to judge the breakdown of the latter under the influence of the lactase enzyme. If the rise in blood glucose levels after a lactose load is less than 20%, one should think about the insufficiency of this enzyme.
Accordingly, the determination of the level of glucose in the blood on an empty stomach and after taking lactose makes it possible to judge the breakdown of the latter under the influence of the lactase enzyme. If the rise in blood glucose levels after a lactose load is less than 20%, one should think about the insufficiency of this enzyme.
Reliable but rarely used methods for detecting lactose intolerance include intestinal biopsy and genetic testing.
A biopsy is an examination of cells in the lining of the small intestine. Intestinal tissue is taken during endoscopic examination. In the tissues obtained, the activity of intestinal digestion and absorption using enzymes is determined. This analysis for lactase deficiency is a reference. However, it is difficult to perform, invasive and expensive, so it is used quite rarely.
Diagnosis of lactase deficiency also includes a number of genetic tests to determine the defect in the genes responsible for the production of lactase.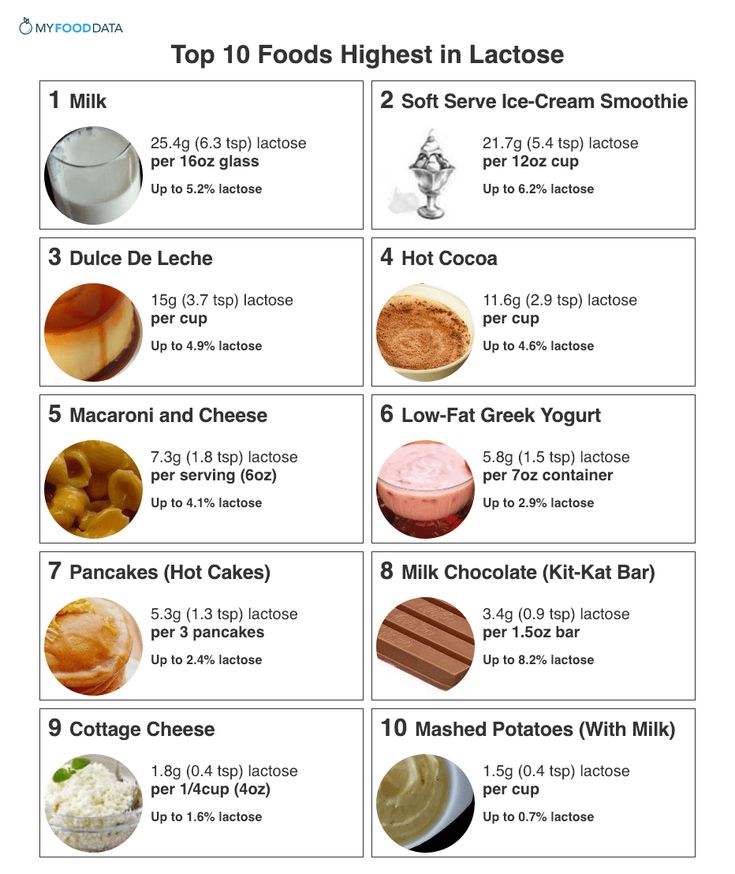
Parents' attention to the health of the crumbs, knowledge of how lactase deficiency manifests itself, timely access to a specialist, effective diagnosis and strict adherence to recommendations will effectively cope with lactase deficiency and improve the health of the child.
causes and solutions
When should you see a doctor?, Symptoms and treatment
Many people do not tolerate one or another food, and sometimes even several. One of the most common types of these nutritional problems is lactose intolerance in children. This pathology occurs as a result of the fact that lactose (milk sugar) is not able to break down. Meanwhile, this nutrient is very important for babies under 3 years old. It is necessary for the absorption of trace elements and provides energy needs. In addition, it has a depressing effect on the development of pathogenic microorganisms, is a life-giving environment for the vital activity of lacto- and bifidobacteria.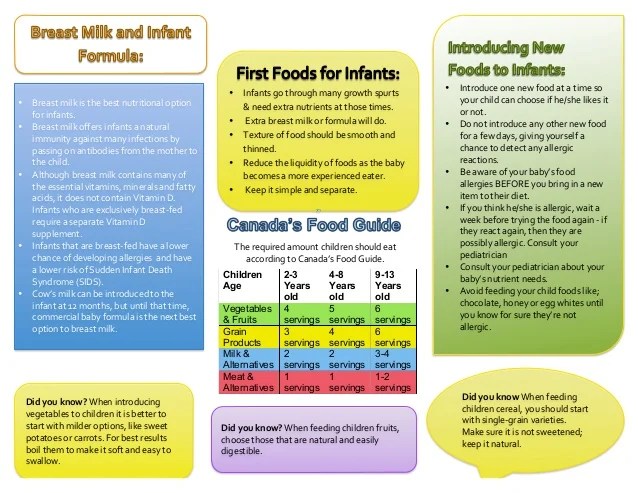
Author : Ph.D. Zoryana Tomkiv
Lactose intolerance (lactase deficiency) is a pathological process in which dairy products are no longer digested. The problem arises in the first months of life, since the main product that the baby eats at this time is breast milk. With an increase in its consumed amount, the severity of clinical manifestations increases. This problem also occurs in adults.
Speaking about the inability to digest dairy products, it should be noted that the body may not tolerate cow's milk protein. However, in this case, we are no longer talking about lactose intolerance, but about an allergy to cow's milk protein.
Why babies develop lactose intolerance
Our ability to metabolize milk sugar is directly dependent on the activity of the enzyme involved in this process, ¾ lactase. It is he who breaks down lactose (milk sugar) in our small intestine into simpler carbohydrates, which are then absorbed into the bloodstream and used by the body.
Lactase first begins to form in the baby's body at 3-4 months of fetal development, and from 6 months it begins to become more active. Before childbirth, the activity of this enzyme increases dramatically, and its level at the birth of a baby becomes higher than in adults. Lactase remains highly active during the entire period of breastfeeding. A gradual decrease in its activity is observed already when the child switches to adult food, on average, at the age of 3-5 years and is a natural consequence of a change in the baby's diet.
If a baby is diagnosed with lactase deficiency, then it can be of two types: primary or secondary.
In turn, primary lactose intolerance, depending on the mechanisms of development, can be:
- congenital;
- constitutional;
- temporary (transient).
Congenital alactasia (lack of lactase) is characterized by the fact that there is no enzyme that breaks down lactose in the body at all, but such cases are very rare and have a genetic nature.
In constitutional lactase deficiency, a sufficient amount of lactase is secreted in the intestine, but a decrease in its activity is observed. As a rule, the activity of the enzyme begins to decrease after complementary foods are introduced, that is, it directly depends on the type of nutrition characteristic of the child during life. This type of lactose intolerance is common in older children as well as adults. It is associated with genetic predisposition and belonging to a particular ethnic group.
Insufficiently mature newborns, as well as in babies born prematurely, transient or temporary lactase deficiency may occur. The reason for this phenomenon is that lactase has not yet become active enough by the time of birth to break down all the milk sugar that enters the baby's body with food.
Secondary lactose intolerance in a child occurs against the background of some other pathology in which enterocytes (epithelial cells of the small intestine) are damaged.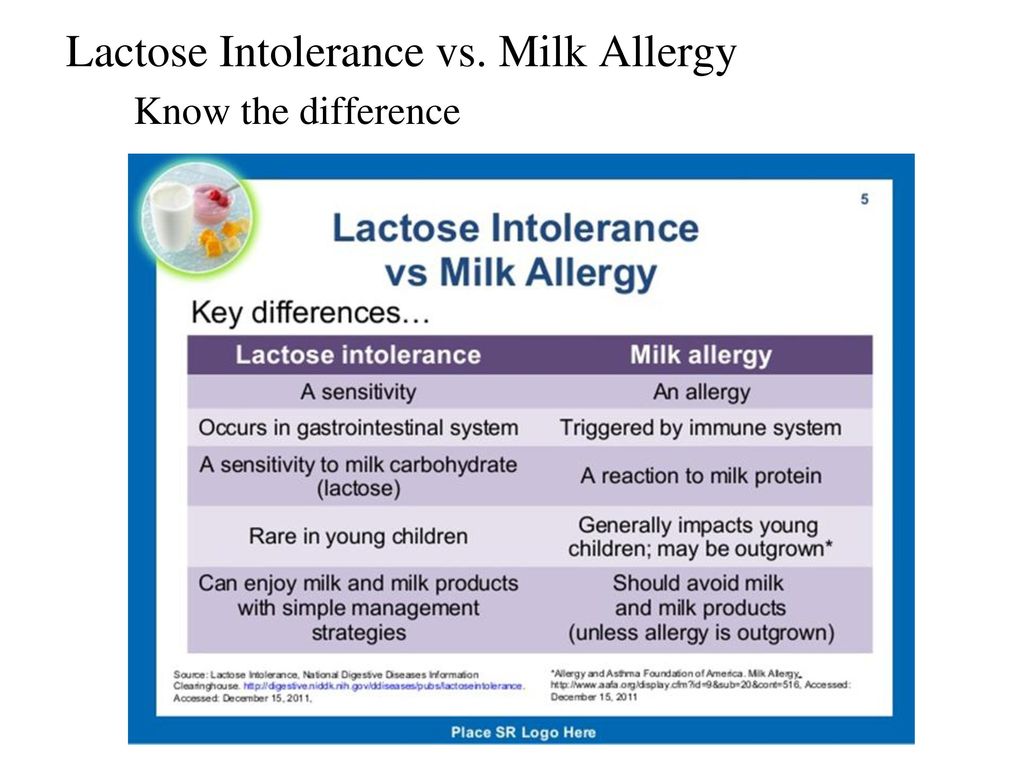 Often the functioning of these cells is disturbed by intestinal infections, allergies and other inflammatory diseases, as well as pathological processes in which atrophic changes occur in the small intestine. In this case, the secretion of lactase is disturbed, which provokes the development of insufficiency.
Often the functioning of these cells is disturbed by intestinal infections, allergies and other inflammatory diseases, as well as pathological processes in which atrophic changes occur in the small intestine. In this case, the secretion of lactase is disturbed, which provokes the development of insufficiency.
In any case, both with insufficient production of the lactase enzyme and with its low activity, undigested lactose from the small intestine passes into the large intestine, where it plays the role of a nutrient medium for intestinal flora microorganisms. The result of this is increased fermentation, gas formation and acidification of the intestinal contents.
Symptoms
In order to understand that an infant is lactose intolerant, one must first pay attention to the specific manifestations of the disease.
Symptoms of lactase deficiency in infants are as follows:
- Stools are thin, frothy, yellow. The chair can be frequent (8-10 times a day) and rare.
 Feces have a sour smell and look like yeast dough. When settling in a glass container, after some time it separates into 2 fractions - dense and liquid. This is important to consider when using diapers: the liquid part is absorbed, so you can miss this violation.
Feces have a sour smell and look like yeast dough. When settling in a glass container, after some time it separates into 2 fractions - dense and liquid. This is important to consider when using diapers: the liquid part is absorbed, so you can miss this violation. - Intestinal motility is enhanced.
- Baby is restless during and after feeding.
- There is bloating, intestinal colic, flatulence.
- Regurgitation occurs, vomiting is possible.
- The baby is not gaining weight well and may even lose it.
A child with this pathology does not suffer from appetite. Often he sucks greedily, but after a while he pulls his legs up to his stomach, starts crying and throws his breast. In the first weeks of life, the disease may be asymptomatic. Its manifestations intensify with an increase in the consumption of milk.
Older children - often after 5 years - the signs of lactose intolerance are less pronounced, since milk is no longer the dominant product in their diet. The intestinal microflora of the child gradually adapts to the intake of lactose, due to which the symptoms also decrease and can only appear after taking a large amount of milk.
The intestinal microflora of the child gradually adapts to the intake of lactose, due to which the symptoms also decrease and can only appear after taking a large amount of milk.
How does lactose intolerance manifest itself in an infant if it has developed a secondary type? Clinical manifestations are supplemented by regurgitation, the presence of greens in the feces, mucus in large quantities, undigested lumps of food, and expressed anxiety. After feeding, rumbling is felt along the intestines.
Diagnosis of lactase deficiency in the newborn
The diagnosis of lactase deficiency is made after examination and observation of clinical signs in the infant and is confirmed by additional tests, which may include: The presence of carbohydrates in the stool is determined, as well as the pH of the feces (as a rule, with this pathology it is less than 5.5). The test is carried out without delay on a fresh portion of stool with sufficient lactose intake.
 It can be argued whether the child has lactase deficiency, according to the curve reflecting the amount of glucose in the blood, as well as the clinical manifestations of the baby. Usually the study is carried out on an empty stomach, with an interval of 15, 30 and 60 minutes after the child is given lactose. Before carrying out, it is recommended to conduct a standard glucose tolerance test for the baby.
It can be argued whether the child has lactase deficiency, according to the curve reflecting the amount of glucose in the blood, as well as the clinical manifestations of the baby. Usually the study is carried out on an empty stomach, with an interval of 15, 30 and 60 minutes after the child is given lactose. Before carrying out, it is recommended to conduct a standard glucose tolerance test for the baby. In certain cases, additional tests may be ordered to make a correct diagnosis.
In addition, the so-called elimination diet effect is important in diagnosing lactase deficiency in infants: that is, if the child is transferred to a lactose-free diet, the symptoms of the disease will decrease, and eventually disappear altogether.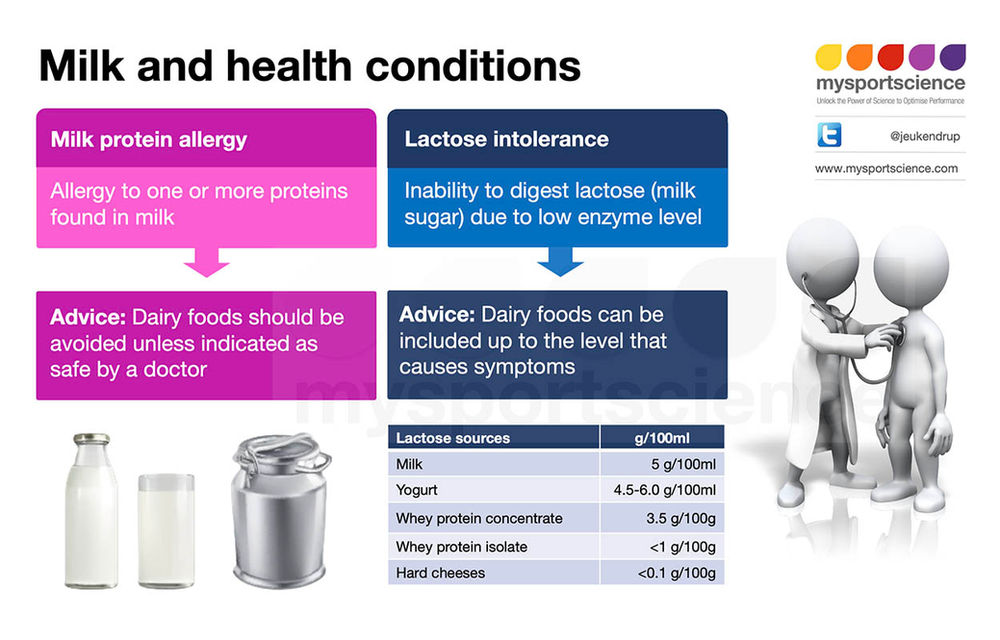
Treatment of lactose intolerance in children
Lactose intolerance is tested before treatment is started in infants. With its positive result, the amount of lactose in the diet is reduced or, if possible, eliminated altogether. At the same time, other symptoms are corrected. This tactic works with primary lactase deficiency.
If secondary lactose intolerance is diagnosed in children, the underlying disease must first be treated. The amount of lactose consumed is temporarily reduced. During the period of treatment of the primary disease, the damaged intestinal mucosa is restored, and the secretion of lactase is getting better.
The treatment of lactase deficiency is difficult in that the most effective method is the elimination of milk from the diet. As soon as this product is not in the diet, the condition returns to normal. This is a good option for older children, but not for babies who need it, because proper feeding helps the baby develop normally. When we talk about lactose intolerance, proper nutrition of the child is, literally, the key to successful treatment.
When we talk about lactose intolerance, proper nutrition of the child is, literally, the key to successful treatment.
For those babies who are fed mother's milk, reducing its amount is undesirable, so the missing enzyme is added directly to it. To do this, the doctor individually calculates the dose of lactase, before feeding it is pre-diluted in expressed breast milk, left for the fermentation process for 5-10 minutes and then given to drink to the baby. After that, feeding is carried out according to age needs. Sometimes a problem can arise if a baby who is used to breastfeeding refuses to take the bottle.
If lactase deficiency occurs in an infant who is bottle-fed, the problem is solved by using low-lactose and lactose-free mixtures. The attending physician will help you choose an infant formula with the maximum amount of lactose that does not cause negative symptoms in the newborn. If the signs of the disease are severe, the baby is transferred to a lactose-free mixture, which does not contain lactose at all.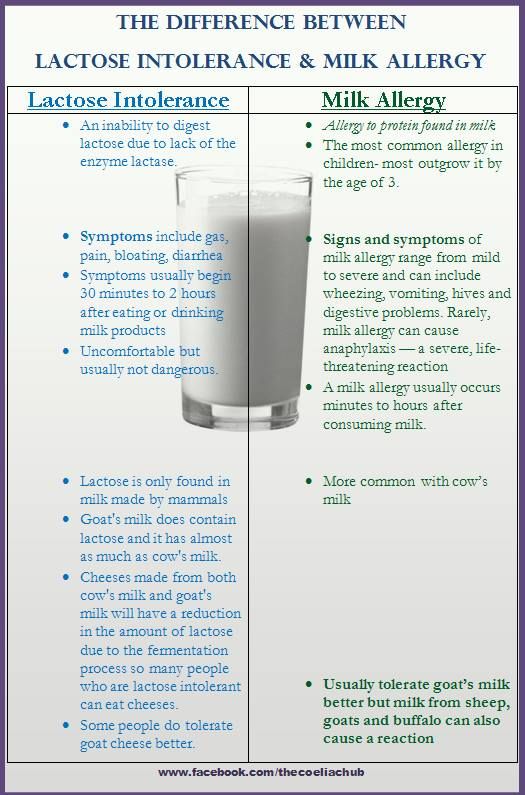
For secondary lactose intolerance due to a food allergy, food intolerance, or malabsorption, your doctor may prescribe formulas based on total protein hydrolysis to combat the underlying disorder. After that, the diet is gradually expanded by adding lactose to the diet of the baby.
Symptomatic therapy may also be needed, in which multivitamin complexes, pancreatic enzymes, drugs for the correction of dysbacteriosis and water and electrolyte balance are prescribed.
A special analysis will help to control the correctness of therapy, in which the level of carbohydrates in the feces is determined. With any form of lactose intolerance, such control is carried out regularly, and in accordance with its results, the baby's diet is adjusted.
With the right choice of treatment, the child's ability to absorb lactose from food gradually increases. Therefore, most infants with temporary lactase deficiency can return to milk nutrition by 3-4 months.
Diet for lactose intolerance
Lactose intolerance in a child requires a special lactose-free or low-lactose diet.