Retained of placenta
Retained placenta | Pregnancy Birth and Baby
Retained placenta | Pregnancy Birth and Baby beginning of content6-minute read
Listen
It’s important to contact your doctor or medical team as soon as possible if you have any heavy bleeding from your vagina and/or pain in the days or weeks following birth.
If the bleeding and/or pain become significantly worse, call an ambulance on triple zero (000). Or go to your nearest hospital emergency department.
What is retained placenta?
Retained placenta is when the placenta doesn’t completely come out of the uterus after the baby is born.
Sometimes, a piece of the placenta is left behind in the uterus (womb). It’s not common, but it can be serious. It can cause problems days or weeks after the birth.
Retained placenta can lead to severe infection or life-threatening blood loss for the mother.
How is the placenta delivered after birth?
After your baby is born, the placenta also needs to be delivered. This is called the third stage of labour.
You may choose to ‘actively manage’ this stage of labour. Meaning that you will receive an injection of Syntocinon (a synthetic version of the hormone oxytocin) to help your uterus contact and birth the placenta. Actively managing your 3rd stage of labour can take up to 30 minutes. This also helps reduce the risk of heavy bleeding from the vagina (called postpartum haemorrhage).
Some women choose not to have the oxytocin injection. This is called ‘expectant management’ or ‘physiological management of the third stage’. It means waiting for the placenta to be born naturally, usually with gravity and some contractions. This may take up to one hour.
It’s important to make an informed decision by discussing the options with your midwife or doctor.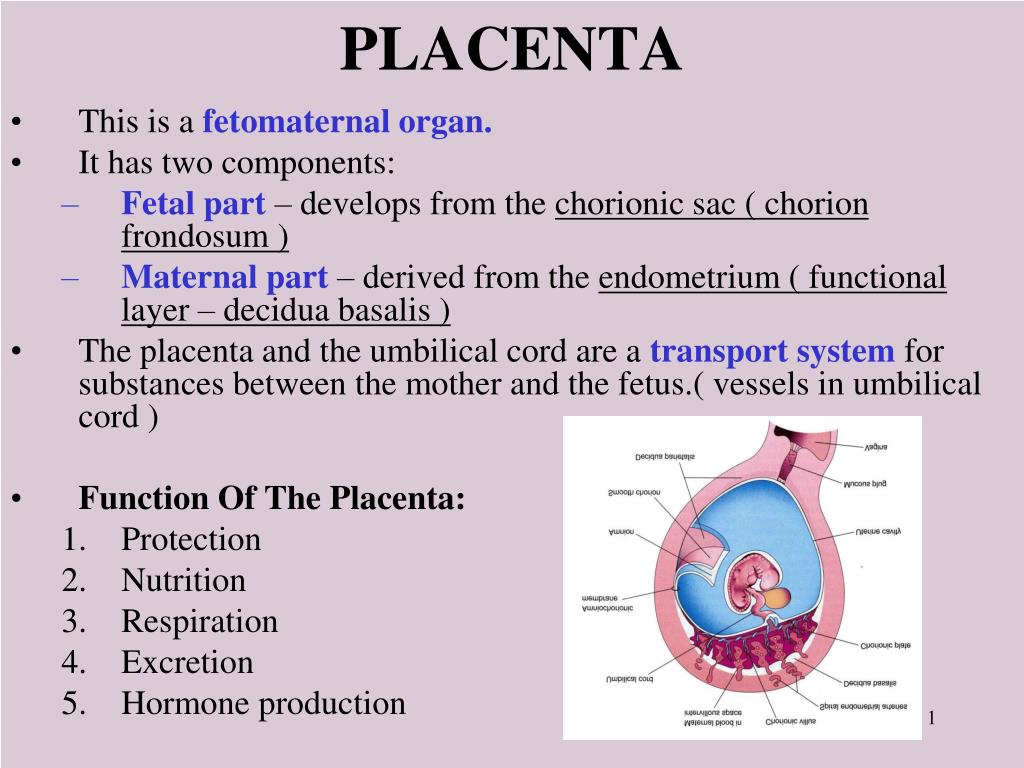 You may choose to write your preferences in a birth plan.
You may choose to write your preferences in a birth plan.
What causes retained placenta?
Sometimes the placenta takes longer than expected to be delivered. The placenta can be retained after your baby is born if:
- your contractions aren’t strong enough to expel it
- the placenta is unusually strongly attached to the wall of the uterus
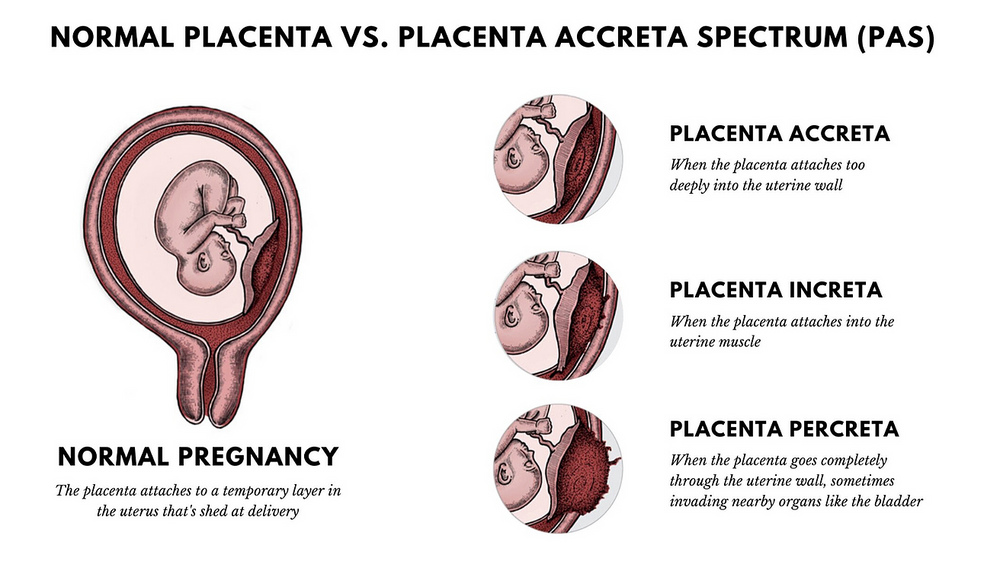
- you have placenta accreta (when the placenta implants too deeply into the wall of the uterus)
- the cervix closes and traps the placenta inside your uterus
What are the signs and symptoms of retained placenta?
Retained placenta is when the placenta doesn’t completely come out of the uterus after the baby is born.
Sometimes a piece of placenta is left behind in the uterus. If this happens, you may develop symptoms days or weeks after the birth. These may include:
- fever
- a bad smelling discharge from the vagina
- heavy bleeding
- large pieces of tissue coming out of the vagina
- pain
It’s important to contact your doctor or medical team as soon as possible if you have any heavy bleeding from your vagina and/or pain in the days or weeks following birth.
If the bleeding and/or pain become significantly worse, call an ambulance on triple zero (000). Or go to your nearest hospital emergency department.
How is retained placenta diagnosed?
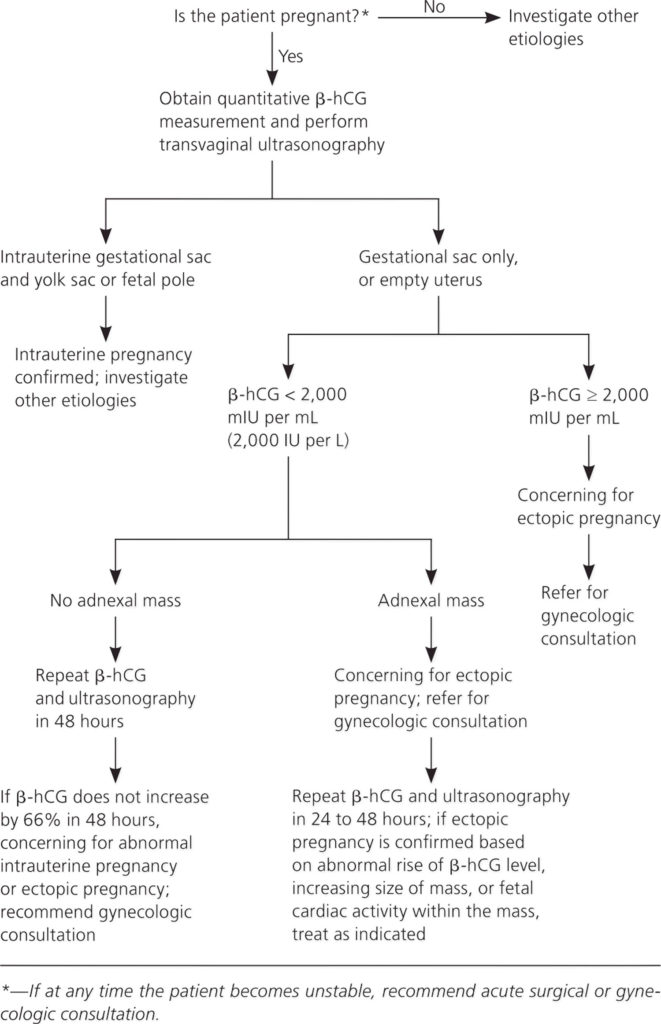
Your doctor or midwife will diagnose retained placenta if the placenta hasn’t completely come out of the uterus within 30 minutes - if you are actively manage or 1 hour - if you choose physiological management, after a vaginal birth.
At every birth, the midwife or doctor checks the placenta once it’s delivered. This is to check that none has been left in the uterus. But it is not always obvious if a small amount of tissue has been left behind.
If you have symptoms of retained placenta in the days or weeks after birth, your doctor may suspect that a piece of the placenta has been left behind. They may recommend an ultrasound scan. This is to check whether you have any retained placenta.
What is the treatment for retained placenta?
If you have just given birth, retained placenta might be treated by:
- emptying your bladder
- your doctor or midwife gently pulling on the umbilical cord.
If that doesn’t work, you will need a procedure to remove the placenta. You will be taken into surgery after the birth and given an epidural or anaesthetic so you don’t feel anything.
While you’re waiting for surgery, the medical team will keep a close eye on you to check you're not bleeding heavily (postpartum haemorrhage). The procedure itself is quick, but you will need to be monitored for several hours afterwards to make sure you are not bleeding.
It’s not always obvious after the placenta has been delivered that some placenta tissue may have been left behind. If you are bleeding heavily in the days or weeks after birth, you may need imaging tests or surgery to investigate the cause.
If you have an infection, you will need treatment with antibiotics.
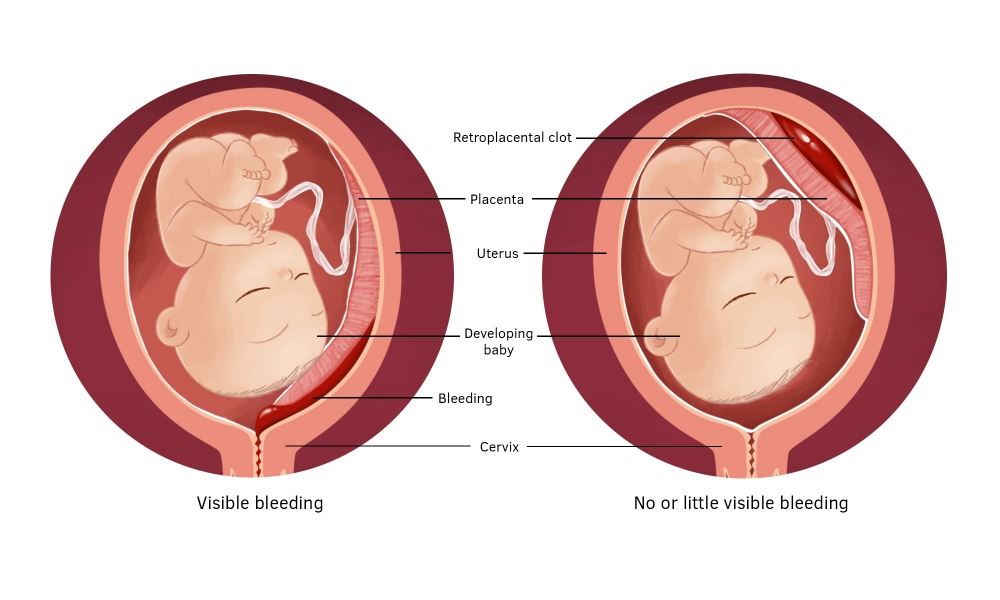
What are the complications of a retained placenta?
Retained placenta can be serious. In rare cases, it can lead to life-threatening infection or blood loss (postpartum haemorrhage).
While there is usually some normal blood loss with birth, blood loss associated with retained placenta can be very severe.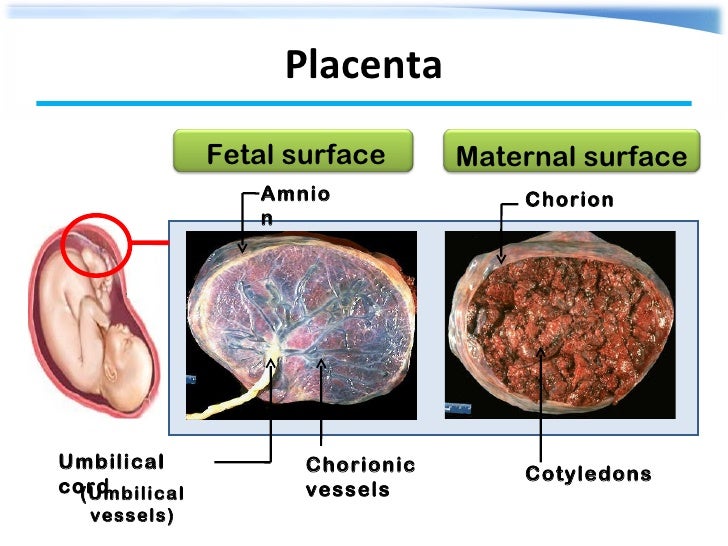 This is because the area in the uterus where the placenta is still attached can continue to bleed.
This is because the area in the uterus where the placenta is still attached can continue to bleed.
Postpartum haemorrhage can be divided into:
- primary postpartum haemorrhage – this happens within the first 24 hours after delivery
- secondary postpartum haemorrhage – this happens in the days and weeks following birth (between 24 hrs and 6 weeks after birth)
Diagnosing and managing retained placenta early helps prevent complications such as severe blood loss and infection.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
The Royal Women’s Hospital (Postpartum Haemorrhage), Government of Western Australia NMHS Health (Labour: Third Stage), International Journal of Women's Health (Retained placenta after vaginal delivery: risk factors and management), Cochrane Database of Systematic Reviews (Active versus expectant management for women in the third stage of labour), RANZCOG (Management of Postpartum Haemorrhage PPH)Learn more here about the development and quality assurance of healthdirect content.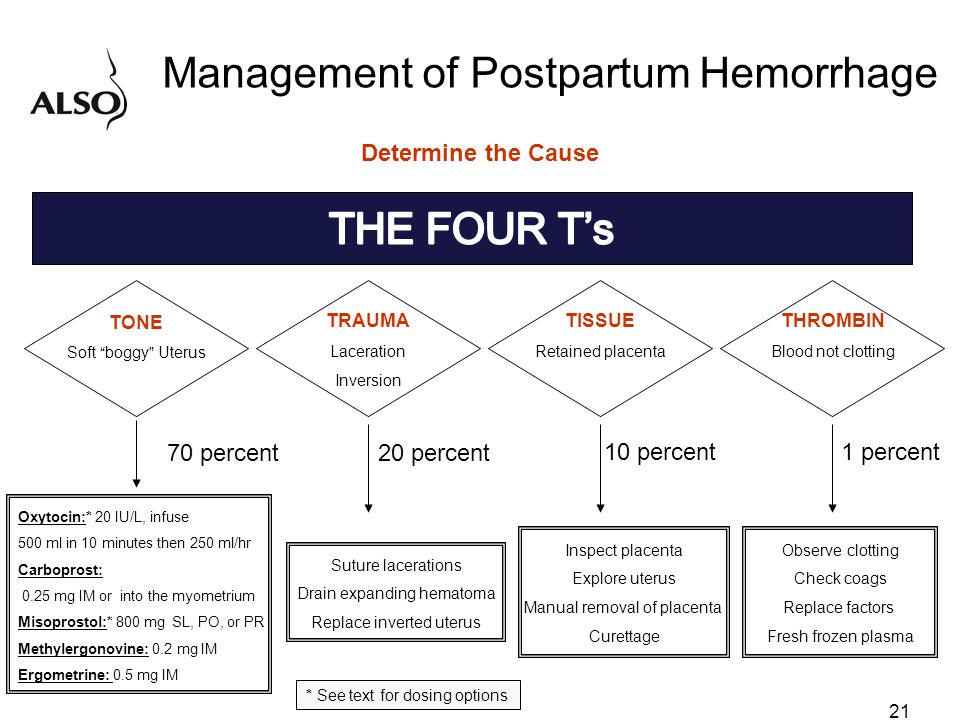
Last reviewed: July 2022
Back To Top
Related pages
- About the placenta
Need more information?
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Read more on Pregnancy, Birth & Baby website
Asherman Syndrome
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Why do some mums stop breastfeeding before 6 months?
Most new parents know 'breast is best', but while more than 9 out of 10 babies are breastfed at birth, few mums are breastfeeding exclusively 5 months later.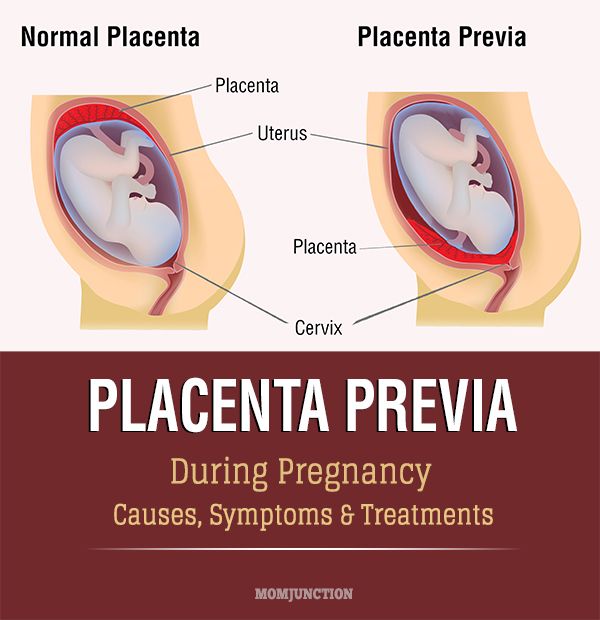
Read more on Pregnancy, Birth & Baby website
What is freebirth?
Freebirth is when a woman chooses to birth her baby without medical or midwifery assistance, but this greater independence comes with some risks.
Read more on Pregnancy, Birth & Baby website
About the placenta
The placenta develops inside the uterus (womb) during pregnancy. It gives your baby nutrients and oxygen. Find out more about the placenta here.
Read more on Pregnancy, Birth & Baby website
Postpartum haemorrhage
Postpartum haemorrhage is when you bleed more than normal after giving birth. It can be very serious and requires medical attention right away.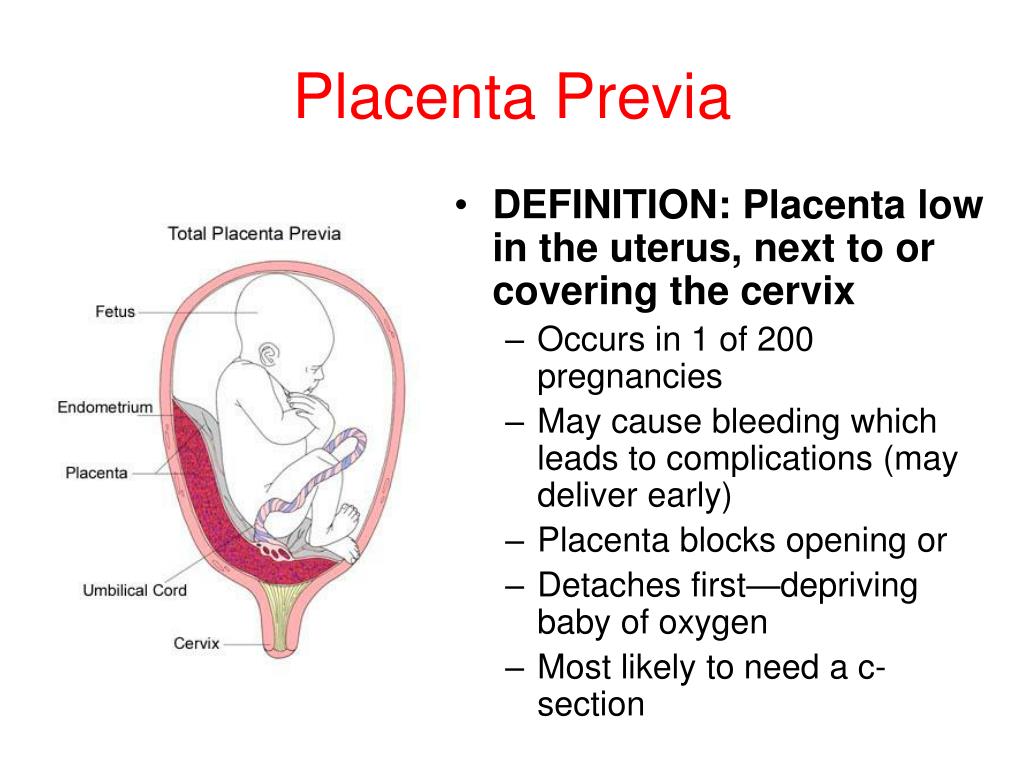
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.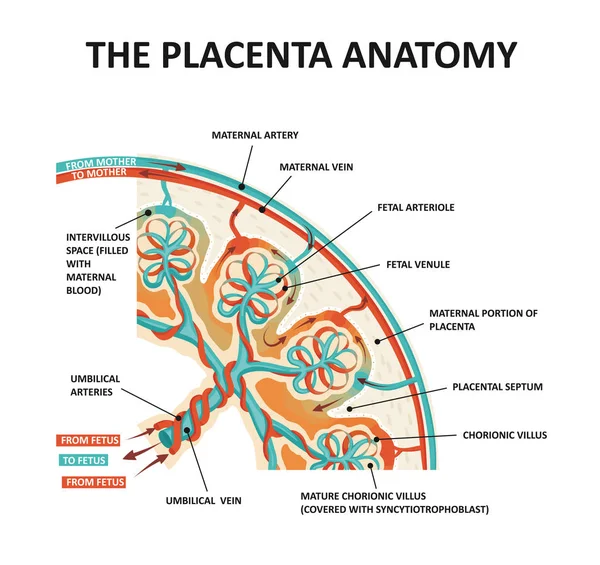
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care.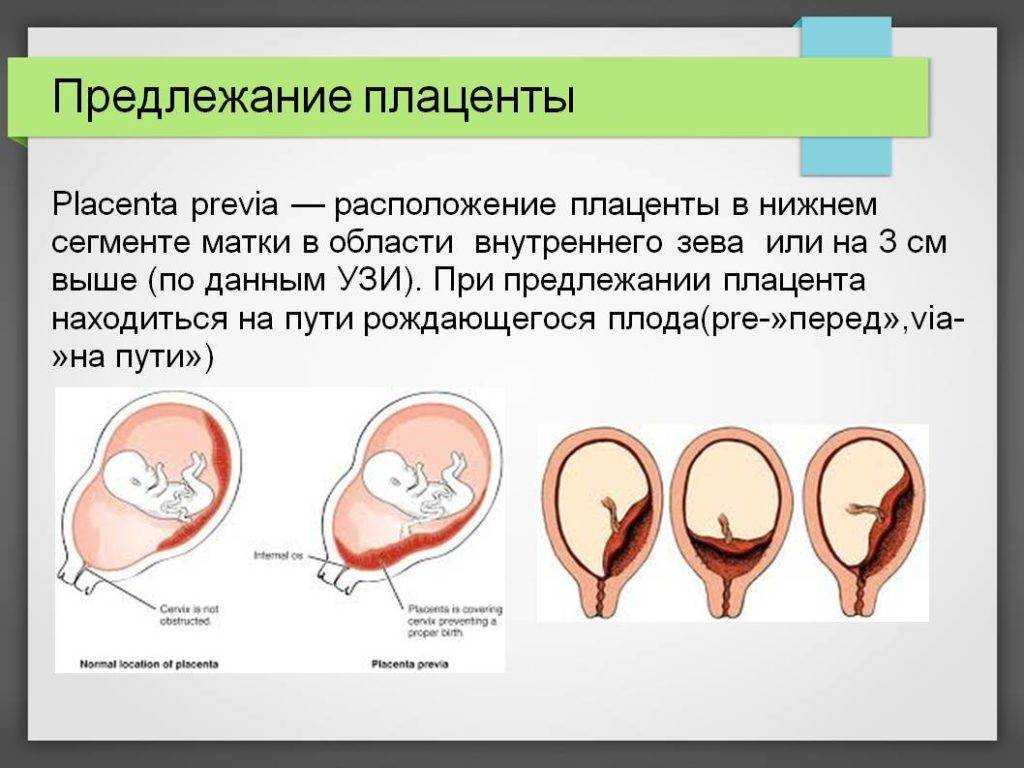 If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What You Should Know About a Retained Placenta
Written by WebMD Editorial Contributors
In this Article
- Causes of a Retained Placenta
- Symptoms of a Retained Placenta
- Risks of a Retained Placenta
- Treatment for Retained Placenta
The placenta is a temporary organ that grows during pregnancy to filter oxygen, blood, and nutrients to your baby.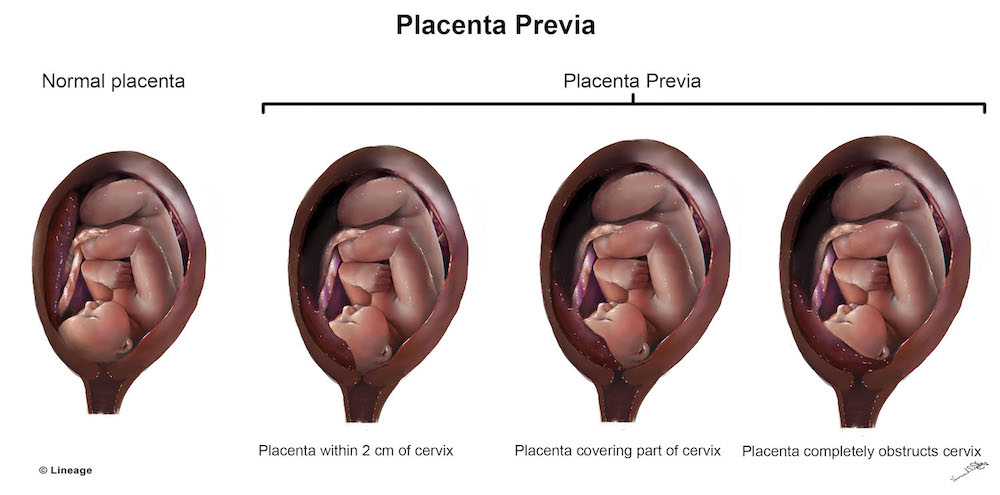 After you give birth, you will also deliver your placenta shortly after.
After you give birth, you will also deliver your placenta shortly after.
Sometimes all or part of the placenta stays in the womb. This is called a retained placenta and it can have serious side effects.
Causes of a Retained Placenta
After your baby is born, you will usually deliver your placenta within 18 to 60 minutes. Your uterus contracts, which pulls the placenta away from the wall of your uterus and pushes it out. Sometimes this doesn’t happen and can be caused by different things, including:
- Not enough contractions
- The placenta grows into the uterus wall
- The cervix closes
- Early delivery
- Giving birth many times
- Previous surgery in the uterus
- Conceiving by in vitro fertilization
- Having a retained placenta in another pregnancy
- Being born with uterus deformities
- Having oxytocin medication for too long
The most common reason for a retained placenta is not enough contractions in the uterus. Contractions can slow down or the uterus can have trouble contracting for different reasons. These include:
Contractions can slow down or the uterus can have trouble contracting for different reasons. These include:
- Having large babies
- Giving birth many times
- Too much oxytocin medication
- A long labor
- A fast labor
- Fibroids
- Having twins or multiples
- Magnesium sulfate infusions
Symptoms of a Retained Placenta
The most obvious sign of a retained placenta is that you don’t deliver it. The most common symptom of a retained placenta after birth is sudden blood loss and life-threatening bleeding.
At times you might push out most of it, however, some pieces of the placenta can be stuck inside. This can cause symptoms that take a while to show up such as:
- Delayed and heavy bleeding
- Blood clots
- Fever
- Chills
- Feeling sick or flu-like
- Foul-smelling vaginal discharge
If you have heavy bleeding and blood clots at home, make sure to keep your pads and show them to your doctor right away.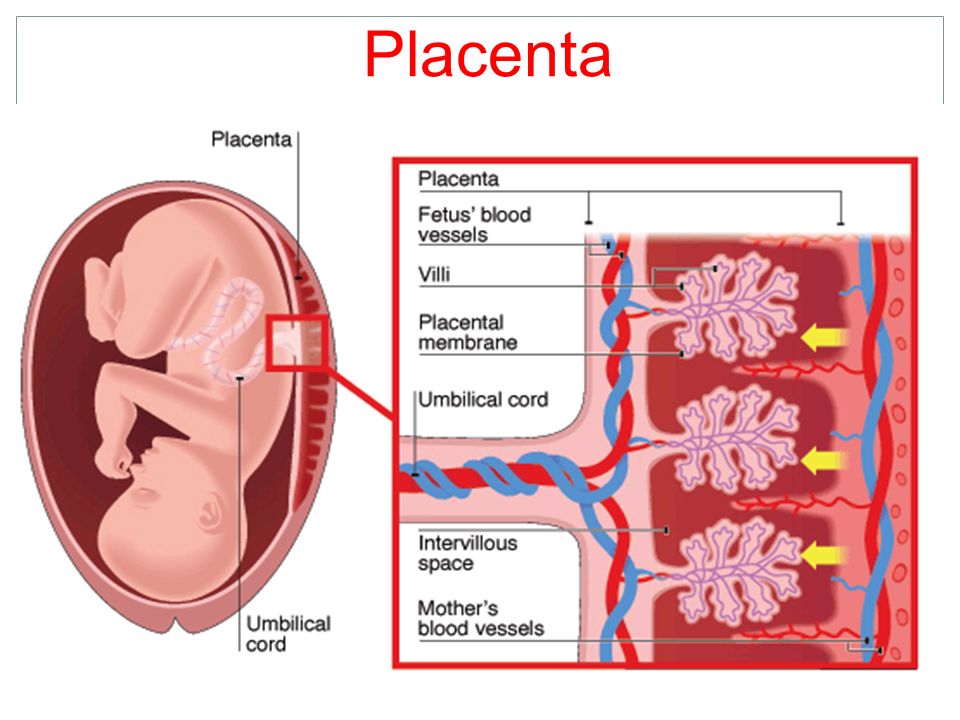 They may want to check for placenta tissue.
They may want to check for placenta tissue.
Risks of a Retained Placenta
Most women safely deliver the placenta after having a baby, but sometimes it can stay inside the womb. This can cause serious side effects.
Life-threatening bleeding. If your placenta is not delivered, it can cause life-threatening bleeding called hemorrhaging.
Infection. If the placenta, or pieces of the placenta, stay inside your uterus, you can develop an infection.
A retained placenta or membrane has to be removed and you will need to see your doctor right away. If you have major bleeding, this is a medical emergency and you should go to your nearest hospital immediately.
Treatment for Retained Placenta
Some conditions can make it more likely that your uterus won’t contract properly. This can lead to a retained placenta. Your doctor will carefully check your medical history and consider how many births you’ve had and what kind of births.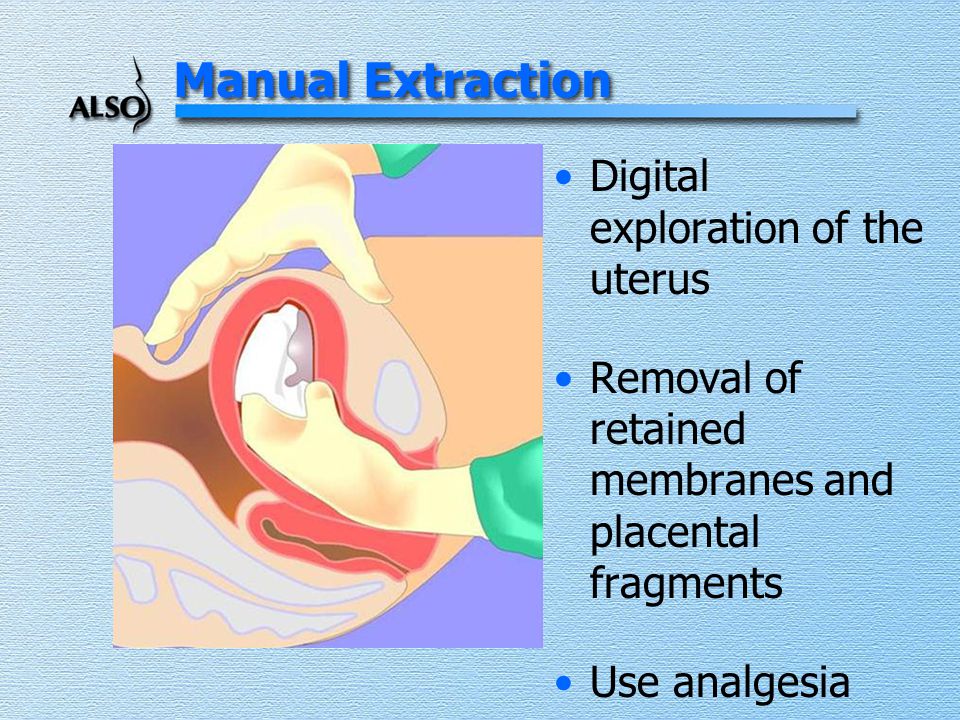 They might make plans during your pregnancy that can help ensure you won't have a retained placenta or prepare for retained placenta treatment.
They might make plans during your pregnancy that can help ensure you won't have a retained placenta or prepare for retained placenta treatment.
Your doctor or midwife will also usually ask you to do a few things right after giving birth that can help prevent a retained placenta.
Breastfeeding. Your doctor, midwife, or nurse will likely ask you to start breastfeeding your baby as soon as possible after you give birth. This is because breastfeeding makes your uterus contract and is a natural process that will help prevent a retained placenta.
Changing positions. Your doctor might ask you to roll to the side or to squat. Changing positions can help your uterus contract and push out your placenta.
Massage. After delivery, your doctor might massage your abdomen to help it contract. This can feel uncomfortable but can be helpful. Abdominal massage is often used after your second birth. This is because your uterus might not contract very well if you’ve had several births.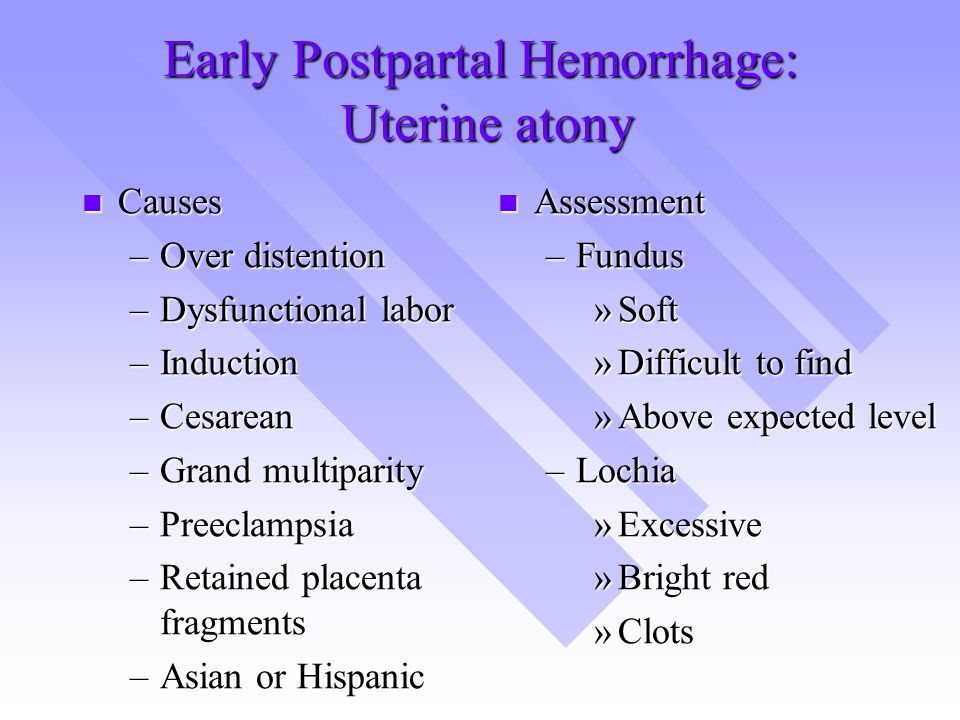
Medication. If these methods don’t work, your doctor might give you a shot of medicine that will make the uterus contract and help you deliver your placenta.
Manual removal. If your doctor diagnoses you with a retained placenta, they may want to remove the placenta by hand. They will often try another method first. Your doctor will give you an epidural or anesthetic medicine and manually separate the placenta inside the uterus.
Surgery. If massage, medication, or other options don’t work, your doctor might decide to do surgery. You will have an operation to safely remove the placenta. If the placenta has grown into the uterus wall and invaded other tissues, you may need to have your uterus removed.
Having surgery or a manual placenta removal can have risks, including infection and life-threatening bleeding. It can also cause endometritis, which is inflammation in the uterine lining. Your doctor may give you antibiotics to help stop infection and endometritis.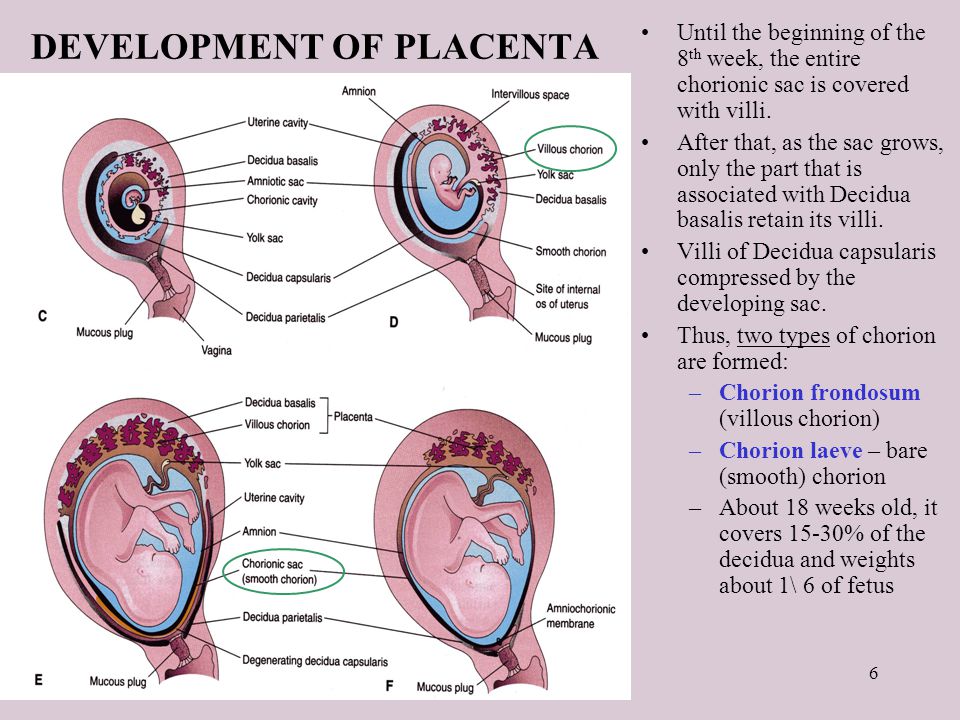
A retained placenta is not very common, but it can happen. Part of giving birth to a baby is also pushing out your placenta and your doctor will closely watch for it to come.
Placental accreta. What is placental accreta?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Placenta accreta is an anomaly of chorionic villus ingrowth with trophoblast invasion into the basal sheath, myometrium, perimetrium, and surrounding organs. Manifested by the absence of signs of separation of the placenta, profuse uterine bleeding in the afterbirth period, symptoms of involvement of adjacent organs (pelvic pain, blood in the feces and urine, constipation, etc.). For diagnosis, ultrasound of the pelvic organs, color doppler, MRI pelviometry, determination of the level of AFP are used.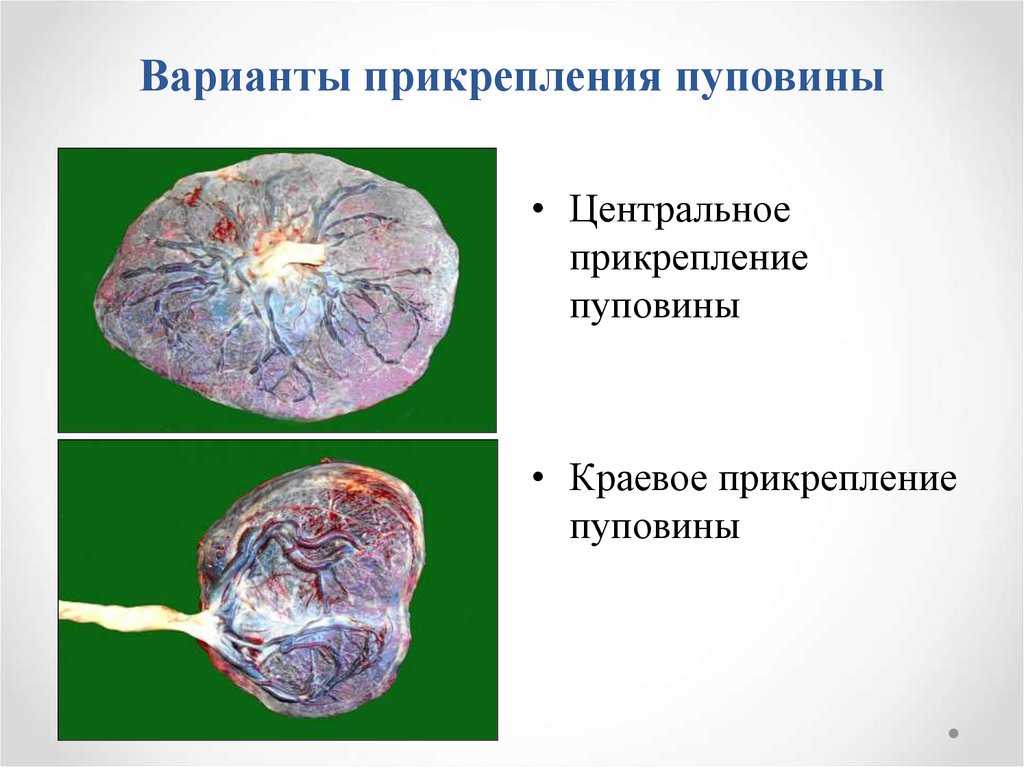 Treatment involves manual separation of the placenta, supravaginal amputation of the uterus, hysterectomy, metroplasty, bottom caesarean section.
Treatment involves manual separation of the placenta, supravaginal amputation of the uterus, hysterectomy, metroplasty, bottom caesarean section.
ICD-10
O43.2
- Causes
- Pathogenesis
- Classification
- Symptoms of placenta accreta
- Complications
- Diagnostics
- Treatment of placental accreta
- Prognosis and prevention
- Prices for treatment
General
Placenta accreta was first described in 1836 by the English gynecologist James Simpson, the morphological basis of the disorder in 1889was identified by the German pathologist Frederick Hart. Over the past 50 years, there has been a more than tenfold increase in the incidence of pathology - from 1: 30,000 pregnant women in the 1950s and 60s to 1: 2,500 in 2007, which is directly related to the rapid increase in the number of caesarean sections. Often, pathological deep invasion of the chorion is combined with placenta previa.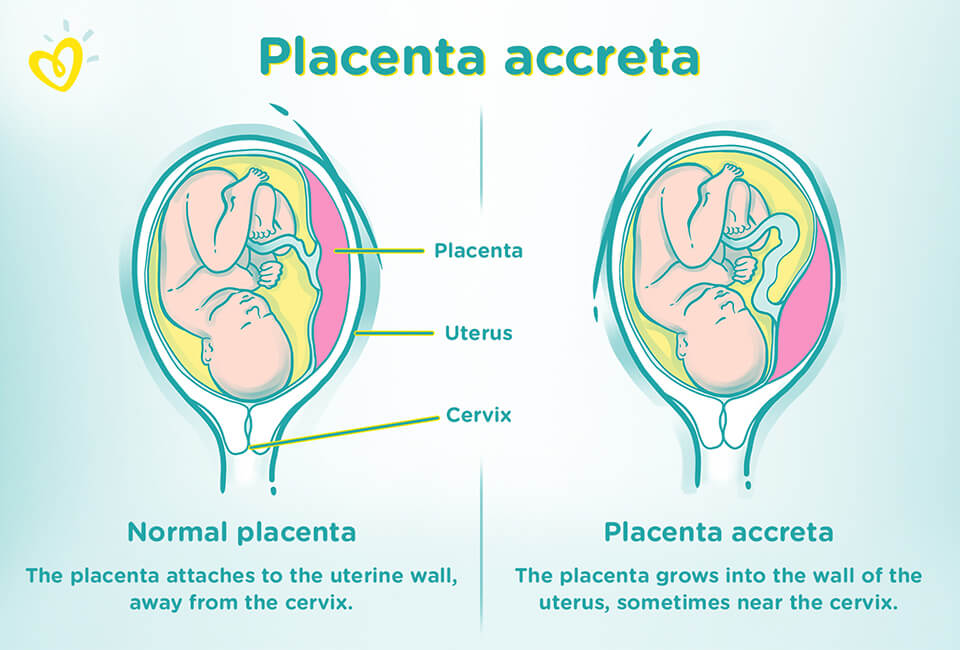 According to studies, after the first operative delivery, the risk of placental tissue increment during its presentation increases by 10%, and after the 4-5th - by 60% or more.
According to studies, after the first operative delivery, the risk of placental tissue increment during its presentation increases by 10%, and after the 4-5th - by 60% or more.
placenta accreta
Causes
Both local dystrophic changes in the endometrium and disturbances in blastogenesis contribute to the pathological ingrowth of chorionic villi into the uterine membranes. The risk of developing the disorder increases as a woman's age increases and the number of pregnancies she bears increases. According to most specialists in the field of obstetrics, the main causes of placental tissue augmentation are:
- Cicatricial changes in the uterine wall. The prerequisites for the occurrence of local endometrial dystrophy are scars after surgical interventions, invasive manipulations - caesarean section, myomectomy, abortion, diagnostic curettage. Dystrophic changes are provoked by violations of circulatory processes and cicatricial degeneration of the epithelium.
- Diseases of the uterus. The normal architectonics of the epithelial membrane can be disturbed in nonspecific and specific endometritis caused by pathogens of chlamydia, gonorrhea, tuberculosis, and other infectious diseases of the genital organs. The increment is often observed in Asherman's syndrome, deformation of the uterine cavity with one large or multiple submucosal fibroids.
- High proteolytic activity of the chorion. In some cases, anomalies of blastogenesis are manifested not by violations of gametogenesis and the formation of fetal malformations, but by an increased invasive ability of the chorion. Deeper implantation is observed when the enzymatic balance is disturbed in the hyaluronidase-hyaluronic acid system between the blastocyst and the decidua.
Additional risk factors contributing to abnormal ingrowth of chorionic villi are low location or placenta previa, multiple pregnancies, post-term pregnancy, developmental anomalies (bicornuate uterus, the presence of an intrauterine septum).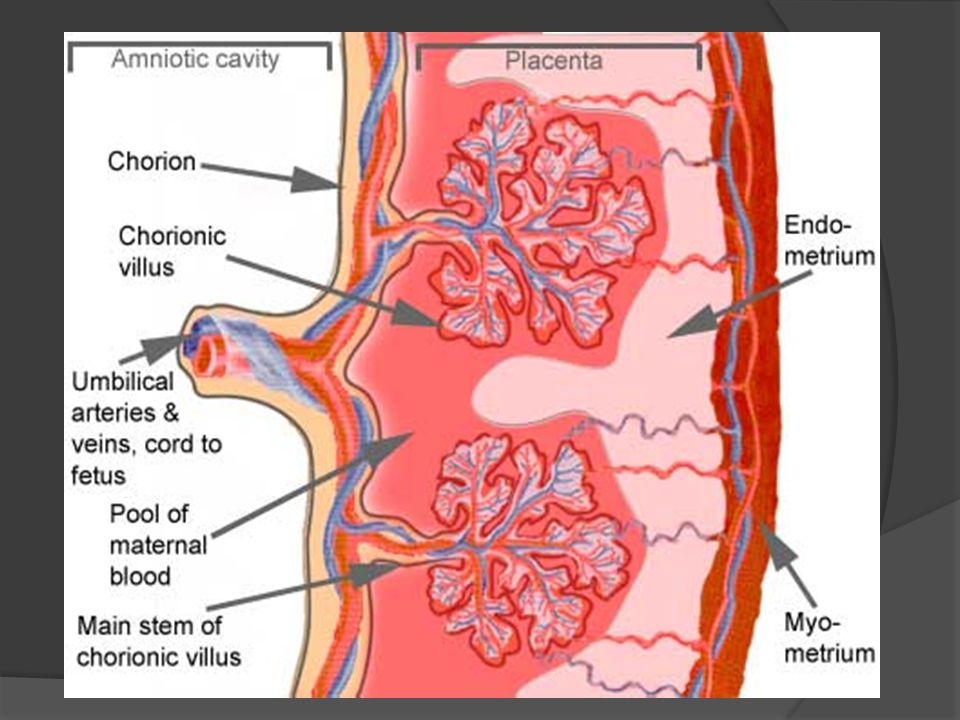 Pathology is more often detected in patients suffering from chronic glomerulonephritis, severe forms of gestosis, in which microcirculatory disorders are noted in various organs, including the endometrium and myometrium.
Pathology is more often detected in patients suffering from chronic glomerulonephritis, severe forms of gestosis, in which microcirculatory disorders are noted in various organs, including the endometrium and myometrium.
Pathogenesis
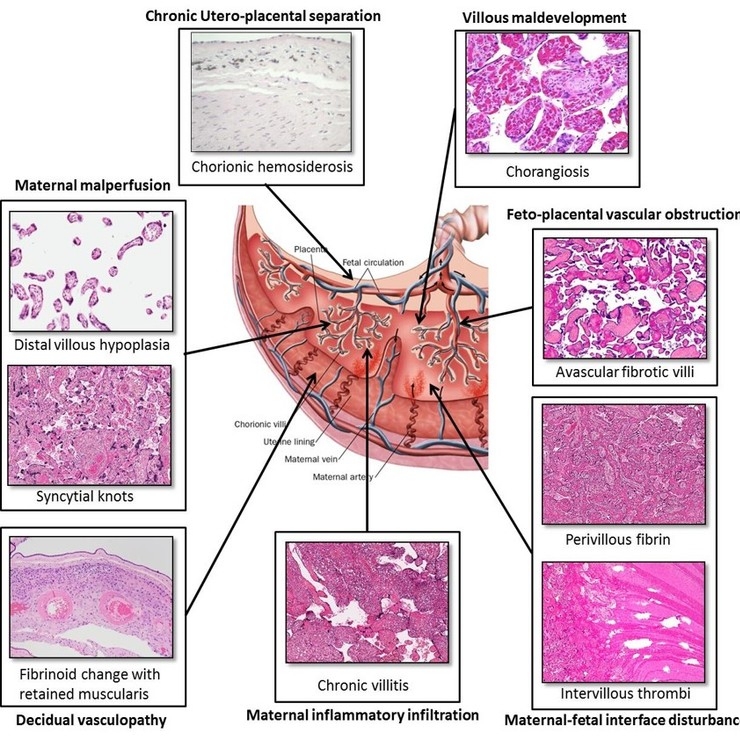
The mechanism of placenta accreta is based on the discrepancy between the penetrating ability of the trophoblast and the thickness and structure of the decidua. Insufficient thickness of the endometrium may be due to physiological malnutrition (the functional layer of the mucosa is usually thinner in the lower uterine segment) and pathological processes. The situation is exacerbated by an increase in the proteolytic activity of enzymes that promote the introduction of the blastocyst into the uterine wall. In the presence of post-traumatic, inflammatory, dystrophic changes, cicatricial degeneration of the spongy layer of the falling placental membrane is observed, along which its rejection occurs in the third stage of labor.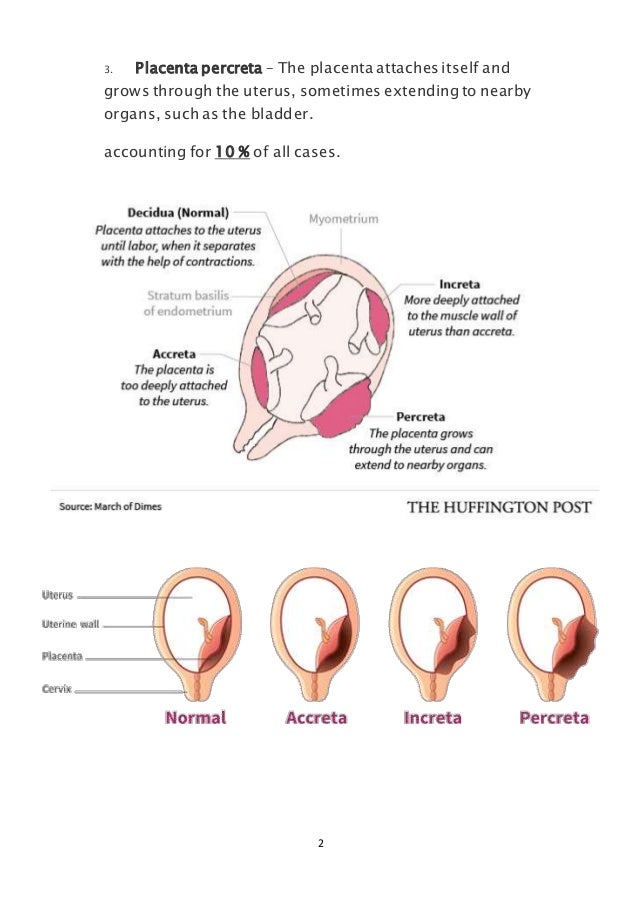 When the placental villi grow into the compacted tissue, their spontaneous separation from the uterine wall becomes impossible.
When the placental villi grow into the compacted tissue, their spontaneous separation from the uterine wall becomes impossible.
Significant thinning of the epithelium is accompanied by a partial or complete absence of the spongy layer. As a result, chorionic villi are separated from the myometrium by accumulations of fibrinoid, and in more severe cases, they directly contact muscle fibers and even grow into them to different depths. Placental septa are partially formed from myocytes, there is abundant vascularization of the myometrium, which is subject to the placental platform. After childbirth, cavernosally altered muscle tissue cannot contract under the influence of oxytocin, which leads to the development of massive uterine bleeding.
Classification
The criteria for systematization of the main variants of placental accreta are the area of abnormal attachment of placental tissue, the depth of its growth into the uterus. This approach provides a more accurate prediction of complications and the choice of optimal medical tactics. The increment is complete with the involvement of the entire placenta in the process and partial with the presence of areas of normal and pathological placentation. Depending on the depth of penetration into the membranes of the uterus, the following types of disorders are distinguished:
This approach provides a more accurate prediction of complications and the choice of optimal medical tactics. The increment is complete with the involvement of the entire placenta in the process and partial with the presence of areas of normal and pathological placentation. Depending on the depth of penetration into the membranes of the uterus, the following types of disorders are distinguished:
- False increment (placenta adhaerens). Has a more favorable prognosis in terms of preserving the uterus. It occurs much more often than the true. Occurs with cicatricial degeneration of the spongy layer. Chorionic villi grow tightly into the decidua and reach the basement membrane, but do not penetrate to the myometrium. The placenta does not separate on its own, the use of special techniques for manually separating the placental tissue and the uterus makes it possible to do without abdominal surgery.
- True increment. It develops against the background of atrophy of the spongy layer, manifested by the penetration of the chorionic villi to the muscle fibers (placenta accreta), into the myometrium (ingrown placenta) and beyond the uterus (germinated placenta).
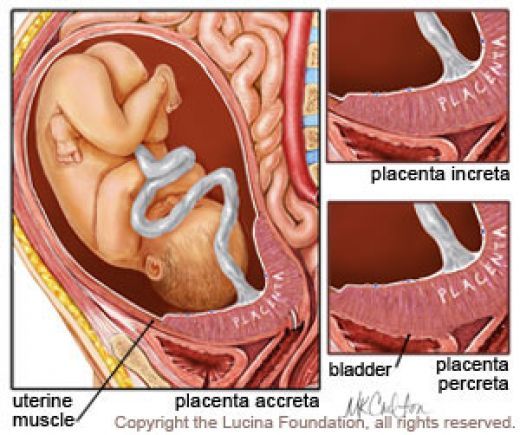 Manual separation of the placenta is not possible. Often the only way to save the life of the puerperal is the surgical removal of the uterus. The frequency of placenta accreta is about 78% of all cases of true increment, ingrown - 15%, germinated - 7%.
Manual separation of the placenta is not possible. Often the only way to save the life of the puerperal is the surgical removal of the uterus. The frequency of placenta accreta is about 78% of all cases of true increment, ingrown - 15%, germinated - 7%.
Symptoms of placenta accreta
There are no clinical signs of the disorder during pregnancy. Pathology is manifested in childbirth by the absence of external signs of separation of the child's place within half an hour after the expulsion of the child: the uterine fundus does not rise above the navel, there is no protrusion of the placenta above the symphysis, the remaining end of the umbilical cord does not lengthen, retracts after straining the woman and shortens with pressure on the stomach. With a complete false and true increment, postpartum bleeding does not occur, with a partial increment and an attempt to manually separate the accreted placenta, profuse uterine bleeding begins. The germination of the placenta into the peritoneum and other organs is indicated by pelvic pain of varying intensity, difficulty in defecation, blood in the urine or feces.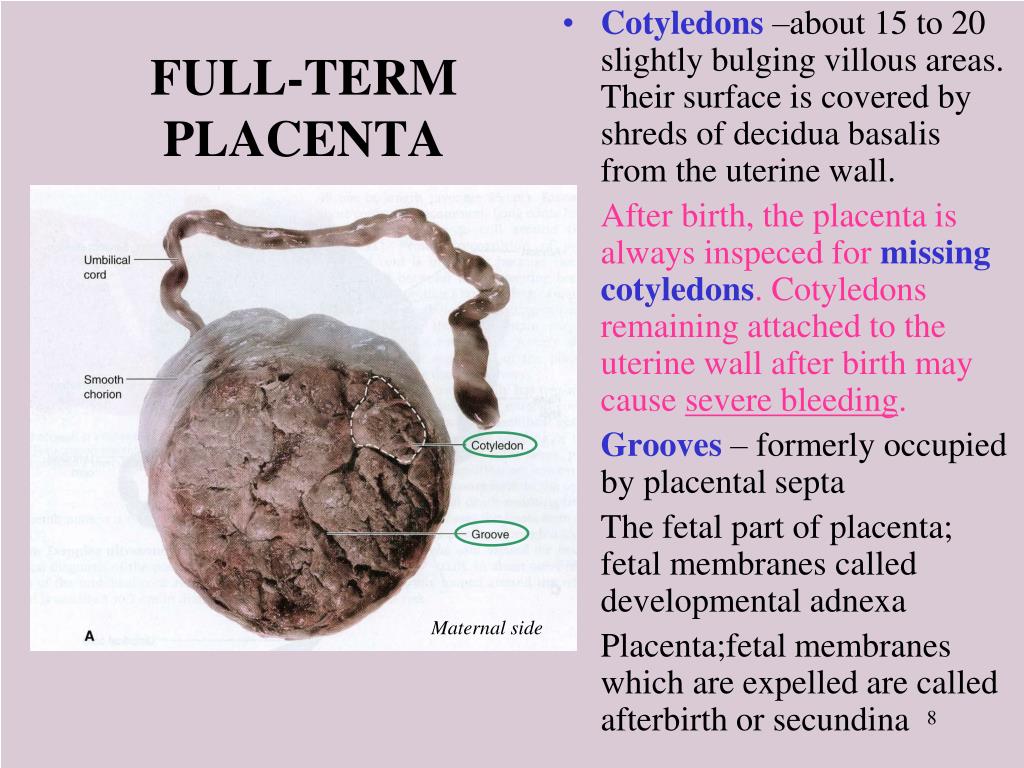
Complications
In violation of blastogenesis, placenta accreta can be combined with fetal malformations, although it does not serve as their direct cause. In the prenatal period, women with impaired placentation often develop fetoplacental insufficiency, fetal hypoxia with a delay in its development, and premature aging of the placenta. In childbirth, the increment of placental tissue is complicated by uterine bleeding, which, without emergency assistance, can lead to significant blood loss, the occurrence of hemorrhagic shock, and the death of a woman. In rare cases, puerperas develop air embolism, respiratory distress syndrome, DIC.
Diagnostics
For the timely detection of pathology, a screening examination is performed for all pregnant women at risk - those who have given birth multiple times, women with uterine anomalies, low-lying or placenta previa, patients who have previously undergone a caesarean section, myomectomy, repeated abortions. The most informative are the methods of ultrasound diagnosis of placenta accreta:
The most informative are the methods of ultrasound diagnosis of placenta accreta:
- Echography. Signs of a possible abnormal attachment of placental tissue according to ultrasound of the uterus and fetus are considered to be a decrease in the distance between the retroplacental vessels and perimetry to 10 mm or less, the presence of cysts in the thickness of the placenta, hyperechoic inclusions. The probability of increment increases when hypo- and anechoic areas with lacunar type blood flow are found in the muscular wall of the uterus.
- Color Doppler Imaging (CDO). The method is considered the gold standard in prenatal augmentation diagnosis. During the study, the localization of abnormal vascular zones is accurately determined. The pathognomonic sign of the disorder is the expansion of the subplacental venous complex. CDI also provides an accurate assessment of the depth of penetration of the chorionic villi into the myometrium.
In recent years, for diagnostic purposes, obstetricians and gynecologists are increasingly prescribing MRI pelviometry, which, in doubtful cases, makes it possible to reliably visualize irregularities in the uterine wall, pathological heterogeneity of the structure of the myometrium and placental tissue.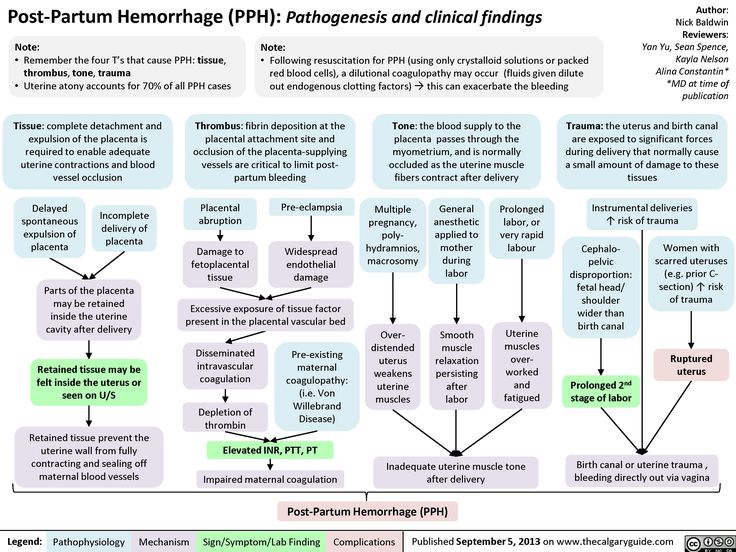 An indirect laboratory sign of the disorder is an increase in the level of alpha-fetoprotein.
An indirect laboratory sign of the disorder is an increase in the level of alpha-fetoprotein.
When identifying pathology in childbirth, it is important to quickly perform a differential diagnosis between false and true increments using manual separation of the placenta. With a tight attachment, the placental tissue can be completely separated and, thus, profuse bleeding can be stopped. The impossibility of separating the placenta in a single array, tissue ruptures, and the absence of individual lobules remaining in the uterus testify to the true increment. The disease is differentiated from other disorders accompanied by massive uterine bleeding: uterine hypotension, DIC, coagulopathy, pregnancy with a normally attached placenta in the tubal angle of a doubled or bicornuate uterus, etc. According to indications, the patient is consulted by a urologist, proctologist, surgeon, anesthesiologist-resuscitator.
Treatment of placental accreta
Identification of pathology serves as an indication for surgical intervention.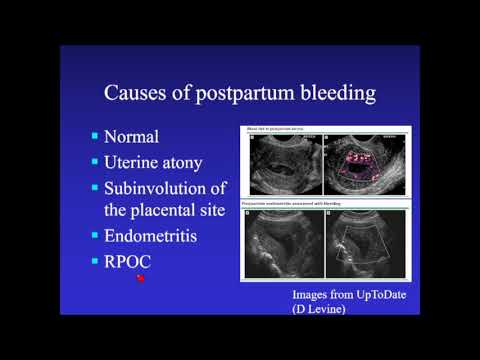 With antenatal diagnosis of increment, natural childbirth is contraindicated, the operation is performed in a planned manner at 37-39 weeks of gestational age simultaneously with a caesarean section, if detected during childbirth - urgently for health reasons. The recommended scope of intervention is determined by the type of placental accreta:
With antenatal diagnosis of increment, natural childbirth is contraindicated, the operation is performed in a planned manner at 37-39 weeks of gestational age simultaneously with a caesarean section, if detected during childbirth - urgently for health reasons. The recommended scope of intervention is determined by the type of placental accreta:
- Manual separation with afterbirth extraction. An obstetric aid for the extraction of an unseparated placenta with fetal membranes is carried out under intravenous anesthesia with a false increment. During the intervention, the obstetrician manually separates and removes tightly attached placental tissue.
- Removal of the uterus. With the penetration of chorionic villi to the myometrium or their ingrowth into smooth muscle fibers, supravaginal amputation or hysterectomy is traditionally performed. Despite the trauma, until recently, such operations were the only way to stop the bleeding.
- Organ-preserving interventions.
 Antenatal diagnosis followed by a bottom caesarean section or metroplasty allows you to save the uterus even with a true increment. Such operations are rarely performed in Russia yet, but positive experience has been gained in performing them abroad.
Antenatal diagnosis followed by a bottom caesarean section or metroplasty allows you to save the uterus even with a true increment. Such operations are rarely performed in Russia yet, but positive experience has been gained in performing them abroad.
When the uterine wall grows, combined urogynecological and proctogynecological interventions are recommended, aimed at the complete removal of placental tissue. Often, sparing surgical methods are supplemented with endovascular methods to prevent or stop uterine bleeding (uterine artery embolization, temporary balloon occlusion). During an emergency operation, the puerperal is shown restoring the volume of circulating blood with infusion therapy (transfusion of whole blood, its components, colloid and crystalloid solutions). Symptomatic treatment includes the appointment of uterotonics (while maintaining the uterus), hemostatics, drugs to maintain pressure and cardiac activity.
Prognosis and prevention
A favorable outcome of placenta accreta is possible only with timely diagnosis and the choice of the optimal method of treatment.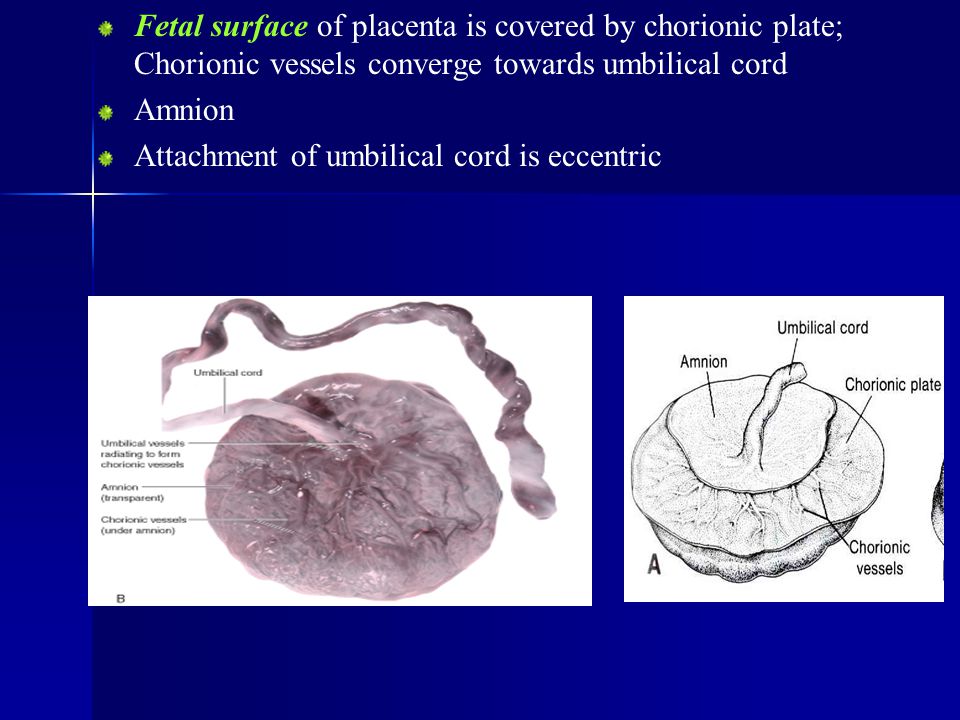 To improve the prognosis, antenatal screening and planned surgical delivery with the operation of the recommended volume are used. Primary prevention involves the rejection of unreasonable diagnostic and therapeutic intrauterine interventions, pregnancy planning, treatment of inflammatory diseases of the uterus, caesarean section strictly in the presence of obstetric or extragenital indications.
To improve the prognosis, antenatal screening and planned surgical delivery with the operation of the recommended volume are used. Primary prevention involves the rejection of unreasonable diagnostic and therapeutic intrauterine interventions, pregnancy planning, treatment of inflammatory diseases of the uterus, caesarean section strictly in the presence of obstetric or extragenital indications.
You can share your medical history, what helped you in the treatment of placenta accreta.
Sources
- Placenta accreta. treatment strategy. Realities. Immediate prospects / Pamfamirov Yu.K., Samoylenko A.V. / Modern innovations. – 2017.
- Diagnosis, prevention and organ-preserving methods of delivery of pregnant women with placenta accreta / Khasanov A.A.// Kazan Medical Journal. – 2016.
- Radiation diagnostics and organ-preserving operations in placenta accreta / Gayazov D.R., Teregulova L.E., Teregulov A.Yu., Yusupova A.F.// Practical medicine.
 – 2017.
– 2017. - Organ-preserving surgical treatment of puerperas with pathology of placenta attachment: Abstract of dissertation / Agrba I.B. – 2014.
- This article was prepared based on the site materials: https://www.krasotaimedicina.ru/
IMPORTANT
Information from this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Plastic found in the human placenta
Microplastic particles were found in the human placenta for the first time, both in the tissues of the mother and the fetus. Previously, in the human body, plastic was found only in the digestive system. The results of the study are published in the journal Environment International .
Over the past century, global plastics production has reached 320 million tons per year, and more than 40 percent of this volume comes from single-use packaging, which leads to the rapid creation of plastic waste.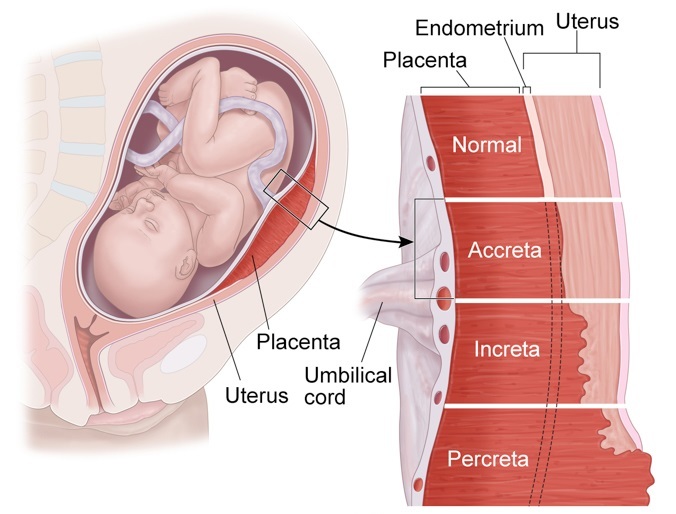 It accumulates in the ground and in water, is transported over long distances by winds and currents, and under the influence of waves, bacteria and ultraviolet radiation is destroyed to the smallest particles - micro- and nanoplastics.
It accumulates in the ground and in water, is transported over long distances by winds and currents, and under the influence of waves, bacteria and ultraviolet radiation is destroyed to the smallest particles - micro- and nanoplastics.
Microplastics - particles up to five millimeters in diameter - are not only formed during the destruction of larger pieces, but are also made immediately in this form - for example, microgranules for gels, scrubs and other cosmetics. Plastic microparticles can get anywhere: they have already been found in food, tea bags, table salt, the digestive tract of marine animals and humans.
Alessandro Svelato from the Department of Obstetrics and Gynecology, Italian Hospital San Giovanni Calibita Fatebenefratelli and his colleagues, ecologists and anatomists, tested whether plastic can enter the placenta.
Six healthy women were selected for the study who agreed to donate their placentas for the study. They noted in the questionnaire whether they used cosmetics with microgranules for two weeks before the birth, and whether they treated their teeth invasively. Childbirth was handled in such a way as to prevent women from coming into contact with plastic: midwives used cotton gloves, beds in the delivery room were covered only with cotton sheets, the umbilical cord was cut with metal scissors.
Childbirth was handled in such a way as to prevent women from coming into contact with plastic: midwives used cotton gloves, beds in the delivery room were covered only with cotton sheets, the umbilical cord was cut with metal scissors.
After the birth, the remaining placentas were immediately collected and cut into pieces, which were divided into three portions - tissues from the baby's side, from the mother's side, and directly the chorioamniotic (fetal) membrane. The samples were delivered to the laboratory, where they were examined using Raman microspectroscopy, a method that allows you to determine the molecular composition of a substance from its emission spectrum under the influence of a laser. The obtained data were compared with the spectra of known substances from the SLOPP Microplastics Library and the KnowItAll software library.
It turned out that four of the six placentas contained fragments of plastic. In total, 12 particles 5-10 micrometers in size, spherical or irregular in shape, were found in all samples.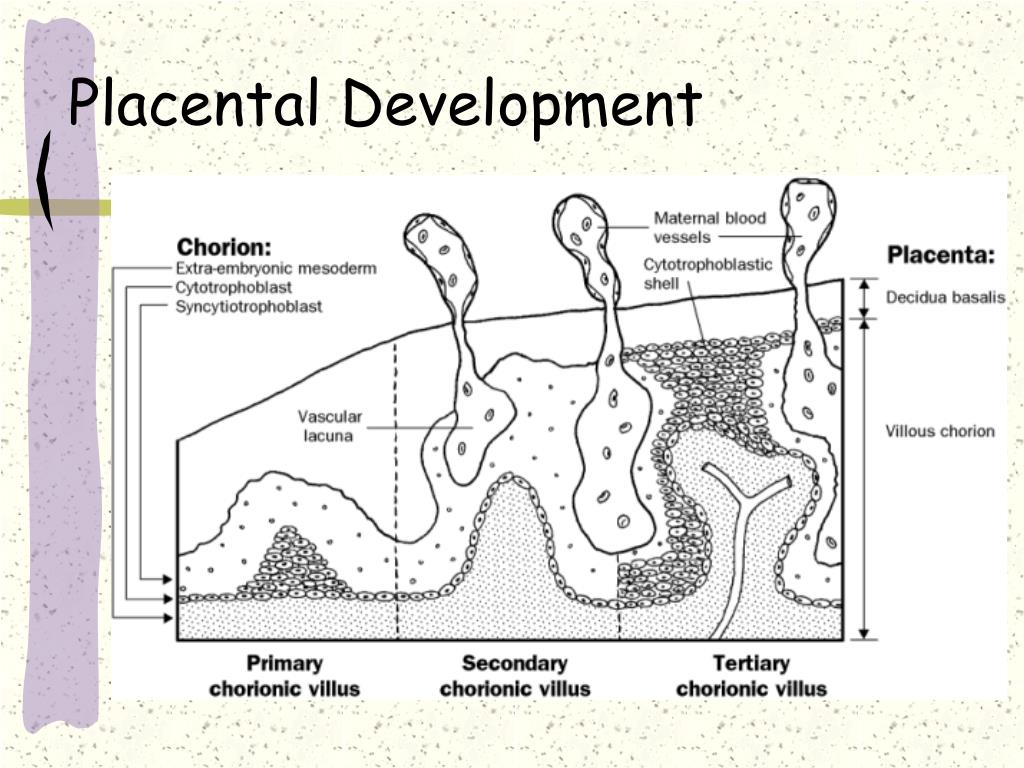 Five were found in tissues on the fetal side, four on the maternal side, and three in the chorioamniotic membranes. Three of the particles turned out to be polypropylene, a material from which packaging film is usually made. Of the rest, only pigments were identified - these are dyes that are found in artificial coatings, paints, adhesives, plasters, cosmetics and personal care products. For example, one particle turned out to be yellow iron hydroxide, which is often used in foundation creams; the other particle was the pigment violantron, which is used to dye cotton and polyester fabrics. Dyes for soap, lipstick, mascara and other make-up products have also been found.
Five were found in tissues on the fetal side, four on the maternal side, and three in the chorioamniotic membranes. Three of the particles turned out to be polypropylene, a material from which packaging film is usually made. Of the rest, only pigments were identified - these are dyes that are found in artificial coatings, paints, adhesives, plasters, cosmetics and personal care products. For example, one particle turned out to be yellow iron hydroxide, which is often used in foundation creams; the other particle was the pigment violantron, which is used to dye cotton and polyester fabrics. Dyes for soap, lipstick, mascara and other make-up products have also been found.
Thus, it turned out that microplastics, having entered the human body, can reach the tissues of the placenta at all levels. Notably, small portions of the placenta were analyzed (23 grams for a total weight of about 600 grams), suggesting that the number of particles in the whole placenta is much higher.
Microplastic particles are perceived by the body as foreign bodies and can provoke local immune reactions and inflammation, not to mention that they can carry dangerous chemicals.