How long can an ectopic pregnancy go unnoticed
Ectopic pregnancy - Symptoms - NHS
Symptoms of an ectopic pregnancy usually develop between the 4th and 12th weeks of pregnancy.
Some women don't have any symptoms at first. They may not find out they have an ectopic pregnancy until an early scan shows the problem or they develop more serious symptoms later on.
Main symptoms
You may have an ectopic pregnancy if you miss a period, have a positive pregnancy test, and have other signs of pregnancy.
Contact your GP or call NHS 111 if you have a combination of any of these symptoms and you think you might be pregnant – even if you haven't had a positive pregnancy test.
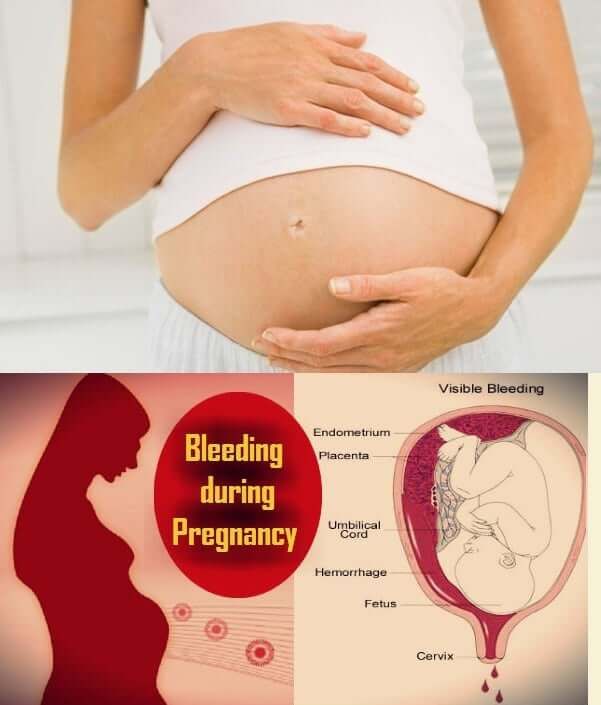
Vaginal bleeding
Vaginal bleeding tends to be a bit different to your regular period. It often starts and stops, and may be watery and dark brown in colour.
Some women mistake this bleeding for a regular period and don't realise they're pregnant.
Vaginal bleeding during pregnancy is relatively common and isn't necessarily a sign of a serious problem, but you should seek medical advice if you experience it.
Tummy pain
You may experience tummy pain, typically low down on one side. It can develop suddenly or gradually, and may be persistent or come and go.
Tummy pain can have lots of causes, including stomach bugs and trapped wind, so it doesn't necessarily mean you have an ectopic pregnancy.
But you should get medical advice if you have it and think you might be pregnant.
Shoulder tip pain
Shoulder tip pain is an unusual pain felt where your shoulder ends and your arm begins.
It's not known exactly why it occurs, but it can be a sign of an ectopic pregnancy causing some internal bleeding, so you should get medical advice right away if you experience it.
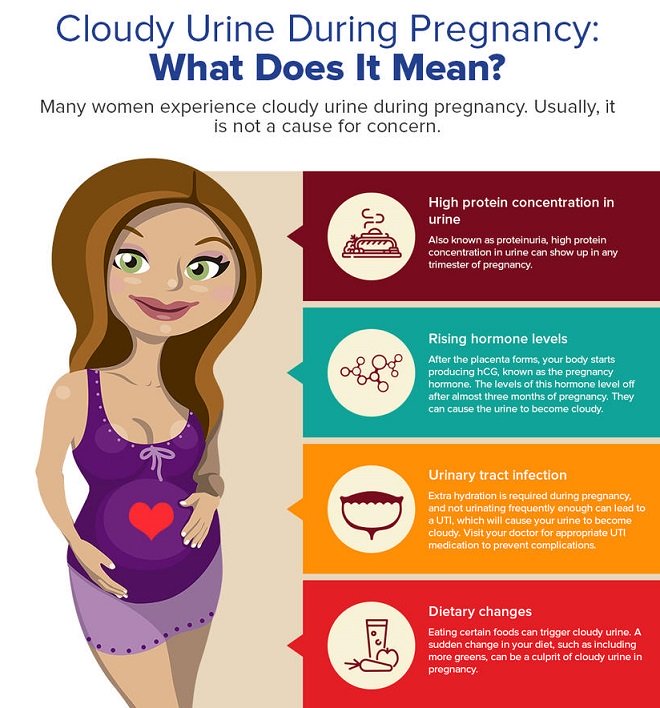
Discomfort when going to the toilet
You may experience pain when going for a pee or poo. You may also have diarrhoea.
Some changes to your normal bladder and bowel patterns are normal during pregnancy, and these symptoms can be caused by urinary tract infections and stomach bugs.
But it's still a good idea to seek medical advice if you experience these symptoms and think you might be pregnant.
Symptoms of a rupture
In a few cases, an ectopic pregnancy can grow large enough to split open the fallopian tube. This is known as a rupture.
Ruptures are very serious, and surgery to repair the fallopian tube needs to be carried out as soon as possible.
Signs of a rupture include a combination of:
- a sharp, sudden and intense pain in your tummy
- feeling very dizzy or fainting
- feeling sick
Call 999 for an ambulance or go to your nearest accident and emergency (A&E) department immediately if you experience these symptoms.
Page last reviewed: 23 August 2022
Next review due: 23 August 2025
Ectopic Pregnancy 101 | by Every Mother Counts
Everything you need to know about an ectopic pregnancy, an increasingly more common pregnancy complication.
One of every 50 pregnancies results in an ectopic pregnancy, which is where embryonic development occurs somewhere other than inside the uterus. What many people don’t realize is how potentially life threatening they can be. Recently, two friends of Every Mother Counts experienced ectopic pregnancies and we thought it was time to discuss this increasingly more common pregnancy complication.
What is an ectopic pregnancy?
When a fertilized egg can’t travel smoothly through the fallopian tube to the uterus where a normal pregnancy develops, it may try to implant somewhere else. In 98 percent of ectopic cases, the fertilized egg implants and grows inside the fallopian tube. The other 2 percent develop in other areas of the abdominal cavity or in the cervix.
The other 2 percent develop in other areas of the abdominal cavity or in the cervix.
How often do they happen?
They occur in about 2 percent of pregnancies, which is a significant increase from the 1970s when only 0.45 percent of pregnancies were ectopic. It’s thought that the increase has to do with improved diagnostic technologies, plus increased rates of sexually transmitted diseases and other conditions that cause pelvic inflammatory disease and scarring of the reproductive organs.
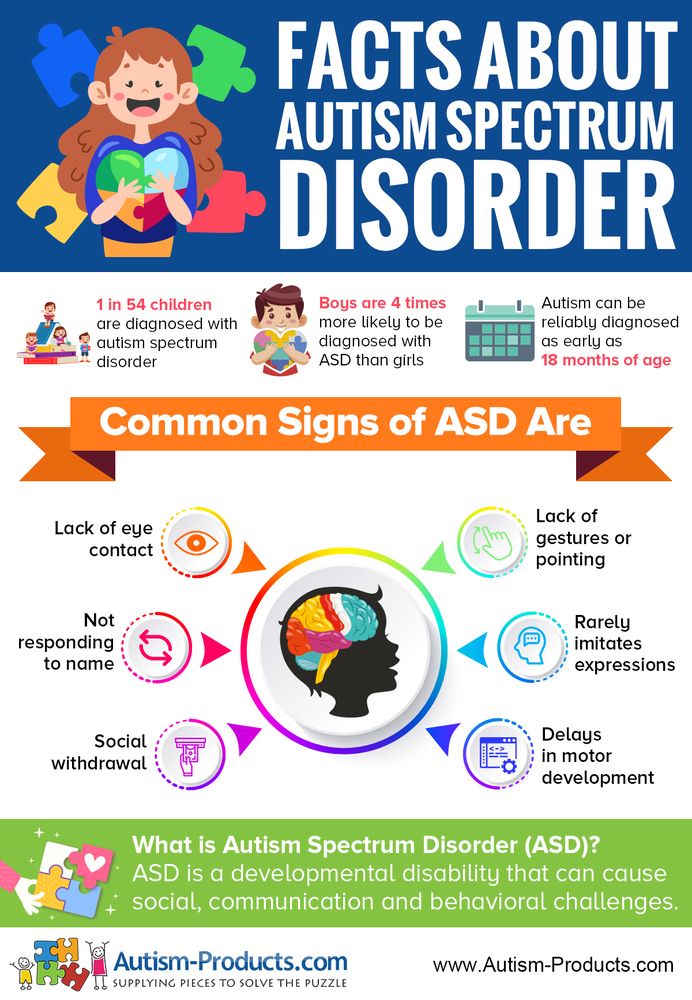
What are the symptoms?
The symptoms most commonly associated with ectopic pregnancy are abdominal pain, spotting, bleeding, nausea, weakness, dizziness and low blood pressure. If the tube has already ruptured, a mother may show symptoms of shock (pale skin, weakness, loss of consciousness, confusion, rapid pulse).
How is it diagnosed?
When a pregnant woman comes to her physician with abdominal pain, with or without bleeding, or if she has similar symptoms and is unaware that she’s pregnant, the first step is to confirm the pregnancy. This involves a blood test to evaluate her pregnancy hormone levels and an ultrasound to visualize the location of the developing fetus plus a pelvic exam. Once an ectopic pregnancy is diagnosed, treatment depends on how far along the pregnancy is and the severity or stability of mom’s condition.
This involves a blood test to evaluate her pregnancy hormone levels and an ultrasound to visualize the location of the developing fetus plus a pelvic exam. Once an ectopic pregnancy is diagnosed, treatment depends on how far along the pregnancy is and the severity or stability of mom’s condition.
What happens to the fetus?
The fetus rarely survives longer than a few weeks because tissues outside the uterus do not provide the necessary blood supply and structural support to promote placental growth and circulation to the developing fetus. If it’s not diagnosed in time, generally between 6 and 16 weeks, the fallopian tube will rupture. This is long before a fetus could survive outside of the mother’s body. The sad truth is that when a pregnancy is ectopic, the fetus will not survive.
How is it treated?
There is no medical technique for transferring an ectopic pregnancy to the uterus where it could develop into a healthy pregnancy and baby.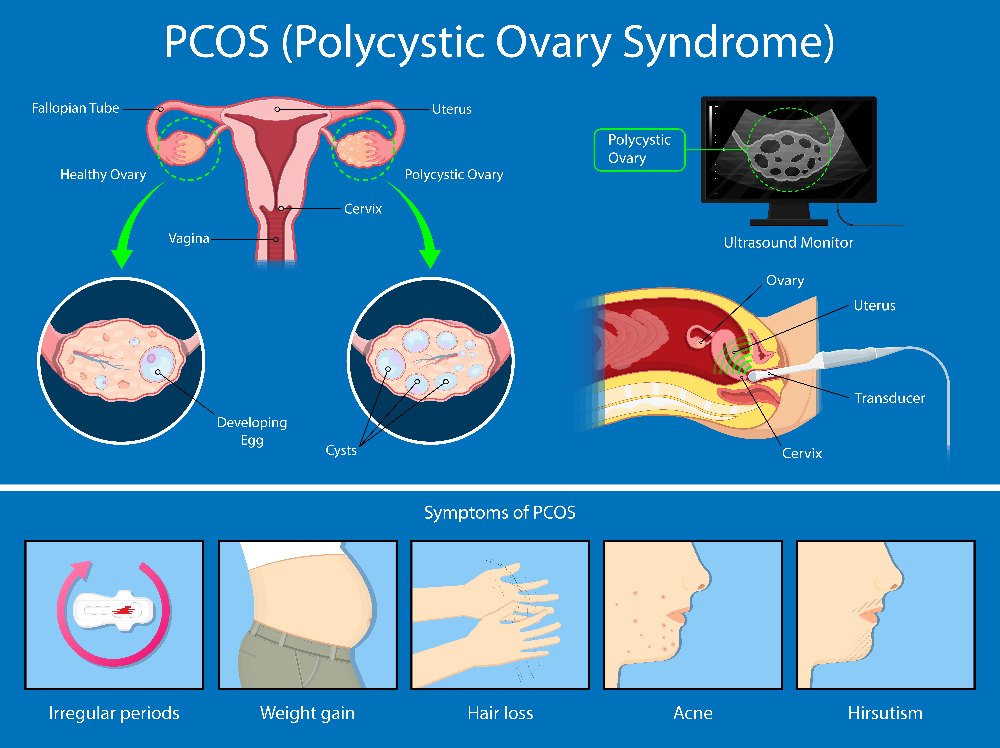 The only treatment that ensures mom’s survival is termination of the pregnancy. This is called a therapeutic abortion because it is required to save mom’s health or life.
The only treatment that ensures mom’s survival is termination of the pregnancy. This is called a therapeutic abortion because it is required to save mom’s health or life.
Occasionally, a mother’s ectopic pregnancy will resolve without treatment if the pregnancy spontaneously absorbs. The problem is we don’t have specific data that predicts which women will recover without treatment and which ones will suffer severe consequences. That’s why most cases of ectopic pregnancy are treated by aborting the pregnancy. That’s done in one of two ways:
- By injecting the mother with a drug called methotraxate, or
- By surgically by removing the tube and fetus
Methotrexate is commonly used for treating cancer because it destroys rapidly dividing cells. In pregnancy, the rapidly dividing cells are embryonic and placental, which shrink and are absorbed by the mother’s body. It’s estimated that 35 percent of patients can be treated successfully with methotrexate when the fetus is in an early stage of development, the tube has not ruptured and there’s no extensive abdominal damage.
Surgical removal of the tube and fetus may be done either through a small incision in the naval or a larger incision in the low abdomen that’s similar to one used for a C-section.
What happens to the mother?
Sometimes, ectopic pregnancies result in miscarriages, but more often, the fallopian tube where the fetus is implanted stretches and becomes inflamed and extremely painful. Most cases of ectopic pregnancy require emergency medical treatment because the growing fetus can cause the fallopian tube to rupture and as a result, massive internal bleeding can occur.
In developed, high-income countries where emergency health care is easily accessible, severe injury or death is rare. That’s because an ectopic pregnancy’s hallmark symptom — severe abdominal pain — drives women to get medical help immediately.
Prior to the age of modern medicine and even today in countries where safe diagnostic and surgical techniques are unavailable, ectopic pregnancy can result in maternal death in more than 50 percent of cases.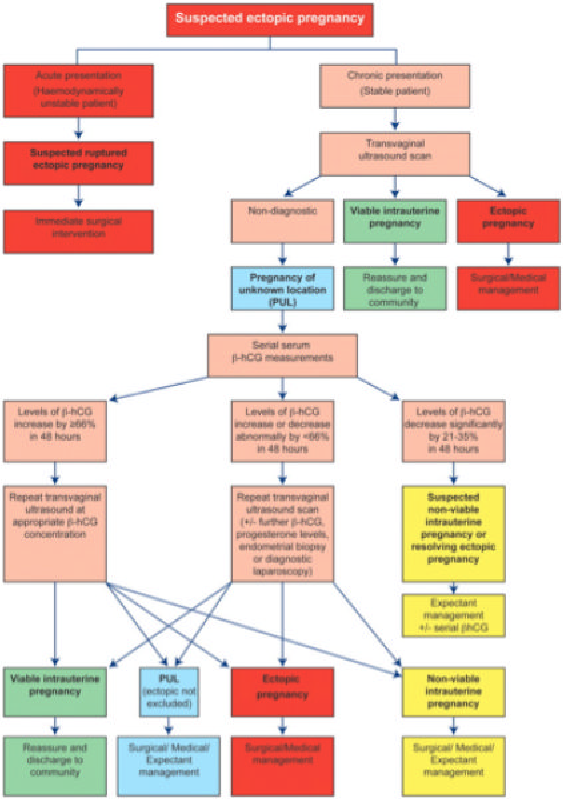 In fact, it’s the leading cause of maternal mortality in the first trimester. When women can access the right healthcare, risk for death drops to less than five in 10,000 pregnancies.
In fact, it’s the leading cause of maternal mortality in the first trimester. When women can access the right healthcare, risk for death drops to less than five in 10,000 pregnancies.
Accurate statistics for maternal outcomes in developing countries are difficult to come by. Jessica Bowers, Every Mother Counts’ Portfolio Director has a masters in International Development from George Washington University and has travelled extensively in developing countries, working in areas where maternal health outcomes are dire. Bowers says, “Ectopic pregnancies usually occur so early in pregnancy and health centers may not have the technology or see the patient early enough to detect it, or may not have a record keeping system that records it.”
Can mom get pregnant again?
Many women can get pregnant again and go on to deliver healthy babies, but it depends on what caused her ectopic pregnancy in the first place, how much abdominal damage occurred, whether she still has a remaining fallopian tube and her willingness to risk having another complication.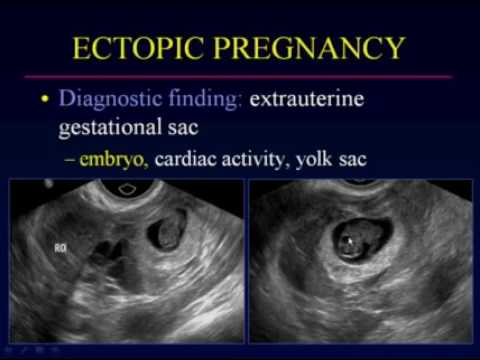 When a woman has had one ectopic pregnancy, she has a 15 percent chance of having another. If she’s had two ectopics, the recurrence rate is 30 percent.
When a woman has had one ectopic pregnancy, she has a 15 percent chance of having another. If she’s had two ectopics, the recurrence rate is 30 percent.
What happened to our friends?
Jennifer Pastiloff, writer, yoga retreat leader and founder of the Manifest Station, experienced pain and bleeding shortly after discovering she was pregnant last year. She had known from the start that something was wrong and when her doctor diagnosed her pregnancy as ectopic, she was successfully, but painfully treated with methotrexate. Jennifer wrote an eloquent essay for The Rumpus about hopping on a plane to lead a yoga retreat shortly after receiving the injection. When the pain became too intense for her to continue teaching, she went to the emergency room for pain medication and reassurance that everything would be all right. The methotrexate worked, though not without a great deal of discomfort.
Christine Koenitzer is one of EMC’s running ambassadors and she’s experienced two ectopic pregnancies this year. Though her ectopic was treated surgically just two weeks ago (after methotrexate didn’t work), she’s recovered well enough that she’ll be participating in the JoyRide and Kilometers Ridgfield 5K race this weekend in Connecticut as a fundraiser for Every Mother Counts.
Though her ectopic was treated surgically just two weeks ago (after methotrexate didn’t work), she’s recovered well enough that she’ll be participating in the JoyRide and Kilometers Ridgfield 5K race this weekend in Connecticut as a fundraiser for Every Mother Counts.
Frozen pregnancy, IVF, Infertility, Causes and prevention
Frozen pregnancy is the cessation of fetal development in the early stages. A frozen pregnancy can go unnoticed for several weeks if a woman does not do an ultrasound during this period and does not undergo an examination by a doctor.
Make an appointment
Causes of miscarriage
There are many causes of miscarriage, most of which are beyond the control of either doctors or women if the child was conceived naturally.
Among the most common causes:
- chromosomal or gene mutations;
- infectious diseases of viral etiology;
- endocrine disorders;
- use of certain drugs or ingestion of toxins;
- antiphospholipid syndrome;
- pathology of the endometrium;
- anomalies in the development of the genital organs.
The causes of miscarriage usually begin to be clarified only after the second such case, because one episode of miscarriage is not a pathology. No woman is immune from this. But if miscarriage has become habitual, diagnostics are needed to find the causes of this phenomenon with their subsequent elimination.
IVF after a missed pregnancy
One episode of a missed pregnancy is not an indication for IVF. This procedure is used solely to increase the chances of pregnancy. However, some IVF methods do help reduce the risk of miscarriage.
Among them:
PGD. Preimplantation genetic diagnosis makes it possible to detect mutations in the resulting embryos in time. Only a "healthy" embryo is selected for transfer. As a result, the risk of planting an embryo in the uterus, which may die due to improper development, is almost eliminated.
ICSI. For the fertilization of the egg, the best sperm is selected, which most likely carries high-quality genetic material.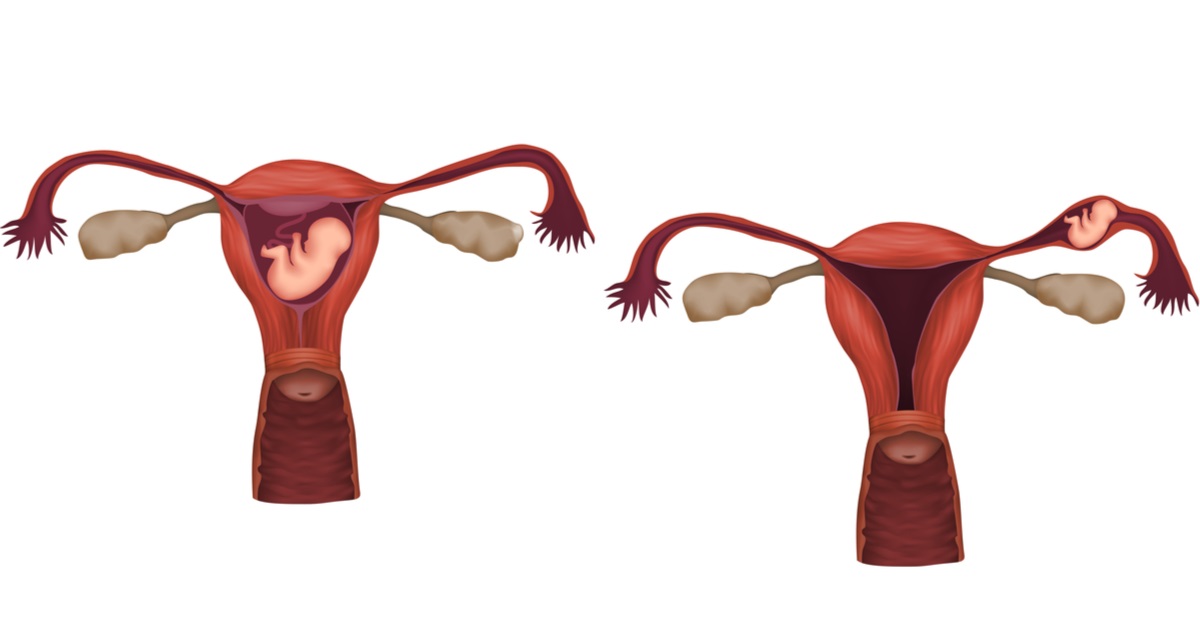
Use of donor oocytes. If a woman has genetic disorders, or she is over 40 years old, the likelihood of mutations increases significantly. These risks are mitigated by using high-quality donor biological material.
Infertility after missed pregnancy
In itself, a miscarriage is not a direct cause of infertility. However, it can be caused by a disease that not only reduces the chances of carrying a child, but also interferes with the woman's fertility, preventing the onset of pregnancy (for example, polycystic ovary syndrome, endometritis, genital infections).
Many women have a miscarriage after a miscarriage in order to remove the ovum. This procedure, too, in some cases can lead to infertility if the basal layer of the endometrium is damaged, or if infection occurs. In this case, acute endometritis develops, which threatens the reproductive function of a woman.
In most cases, infertility does not develop after a missed pregnancy. A woman is able to conceive a child again and bear it. To prevent miscarriage, you need to undergo a series of examinations. They are standard for women planning both first and second pregnancies.
Miscarriage after IVF
The risk of miscarriage after natural fertilization is 10-15%. The probability of miscarriage after IVF is much higher, and reaches 30-35%. This has nothing to do with the technique of artificial insemination.
Reasons for this statistic:
- Age difference. Most expectant mothers who conceive naturally are under the age of 30. Most women who resort to IVF have crossed the 35-year mark.
- Status of reproductive health. IVF is done not for pleasure, but according to indications. As a rule, these are gynecological and other diseases that not only reduce fertility, but also increase the risk of miscarriage.
To reduce the chance of miscarriage after IVF, hormonal support is prescribed in the early stages. Any change in her condition should be reported to the doctor.
Any change in her condition should be reported to the doctor.
Prevention of miscarriage
Usually, to prevent miscarriage, doctors recommend that a woman lead a healthy lifestyle, do not drink or smoke, avoid stress and hard physical labor. However, in reality, all these factors only slightly affect the risk of miscarriage.
Usually, little depends on the woman - in 70% of cases, such an embryo is initially not viable (for various reasons).
What can an expectant mother do to minimize the risk of miscarriage?
- Plan your pregnancy well in advance. See a doctor and get tested to check if there are any diseases that increase the risk of miscarriage. If they are found, first you need to be cured, and then get pregnant.
- Avoid large crowds after pregnancy. This will protect against infections transmitted by airborne droplets.
- Take your doctor's prescribed hormonal products to support pregnancy in case of endocrine disorders.

- Avoid contact with potentially toxic chemicals. Before using any medication, consult a doctor, or at least read the instructions for use.
After a missed pregnancy, you should not despair. Make another attempt - in most cases it will be successful. Just before that, do not forget to contact a gynecologist and get ready for pregnancy, as all women who are worried about the health of their unborn child do.
Ectopic pregnancy - causes and treatment
If the fixation and subsequent development of the ovum occurs outside the uterus, then the pregnancy is called ectopic. It occurs in 2% of all pregnancies. The embryo can be fixed on the ovary, in the abdominal cavity, in the cervix, in the fallopian tubes. An ectopic pregnancy in the early stages is no different from a normal one.
An egg is released from the ovary during ovulation and enters the fallopian tube. Fertilization occurs when a sperm and an egg meet in the ampulla of the fallopian tube.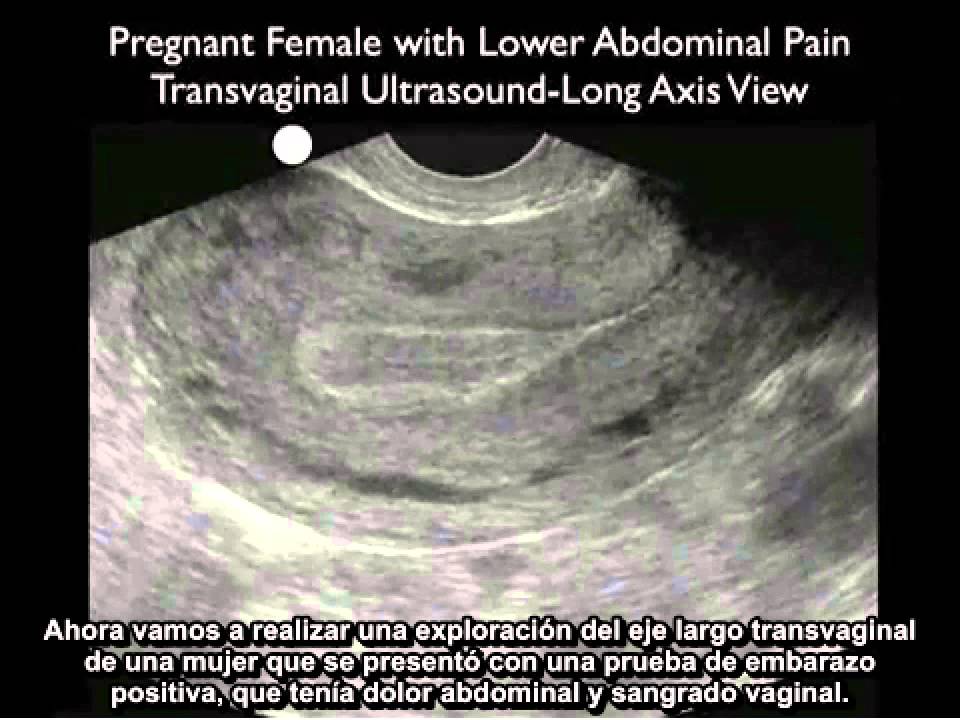 Normally, at the end of the first week after fertilization, the embryo enters the uterine cavity and implantation occurs. A fertilized egg can develop normally only in the uterus.
Normally, at the end of the first week after fertilization, the embryo enters the uterine cavity and implantation occurs. A fertilized egg can develop normally only in the uterus.
Types
- tubal - the embryo develops in the fallopian tubes;
- abdominal - the embryo is attached to the walls of the peritoneum;
- ovarian - the embryo is attached to the walls of the cervix;
- cervical - the embryo is attached to the cavity of the ovary.
Very rare bilateral ectopic pregnancy, as well as heterotopic pregnancy (combination of uterine and ectopic). An ectopic pregnancy of any type is considered a medical emergency.
Let's take a look at tubal pregnancy next, because it is the most common and accounts for 98-99% of all pregnancies outside the uterus.
Signs of ectopic pregnancy
As long as the fetal egg does not overstretch the wall of the fallopian tube, pregnancy is no different from normal and is characterized by standard signs:
- delayed menstruation;
- positive test;
- early toxicosis;
- drowsiness;
- breast enlargement and soreness;
- change in taste preferences.
During menstruation, scanty dark-colored blood discharge is possible. It is impossible for a woman to determine an ectopic pregnancy at home, and diagnostics and specialist advice are required.
Until a certain point, the fertilized egg develops normally. But the embryo grows and it ceases to have enough nutrients. At some point, he ruptures the fallopian tube and bleeding occurs. At the same time, the blood practically does not flow out, only small spotting discharges may appear, the main bleeding occurs in the abdominal cavity.
An ectopic pregnancy may show symptoms after 2 weeks of delayed menstruation. A woman may feel:
- weakness, dizziness;
- pain in rectum radiating to back;
- loss of appetite;
- pain in the lower abdomen, sometimes with nausea and vomiting;
- scanty spotting.
Particular attention should be paid to pain in the lower abdomen. This symptom is also characteristic of a normal uterine pregnancy.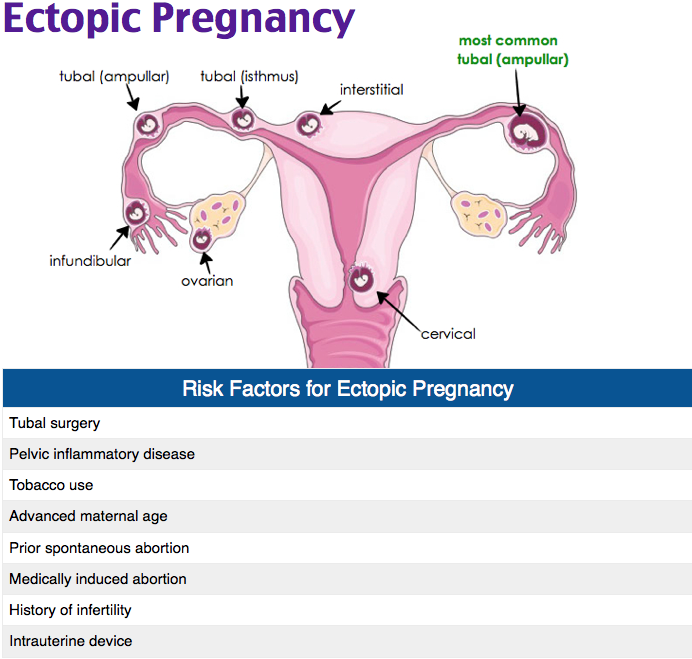 But in a normal pregnancy, the pain is temporary. With tubal, as a rule, the pain increases, intensifies and does not stop.
But in a normal pregnancy, the pain is temporary. With tubal, as a rule, the pain increases, intensifies and does not stop.
If you experience any of the symptoms listed, seek medical attention immediately. The condition can worsen sharply at any moment, which threatens the health and life of a woman.
Causes of ectopic pregnancy
Causes are all conditions that interfere with the movement of a fertilized egg into the uterine cavity:
- chronic inflammatory processes of the pelvic organs;
- violation of patency - the appearance of adhesions and scarring of tissues;
- violation of the peristalsis of the fallopian tube
- the exit from the pipe is closed;
- pathology of the endometrium;
- transferred infectious diseases;
- congenital factor - pipes are twisted and very long;
- single fallopian tube.
Risk factors:
- history of ectopic pregnancy;
- adhesive process in the small pelvis;
- interventions on the fallopian tubes;
- intrauterine contraception;
- surgery;
- pregnancy after prolonged infertility, after IVF procedure;
- anatomical features;
- bad habits;
- age from 35 years;
- hormonal and endocrine disorders.
Diagnosis
It is very difficult to detect a tubal pregnancy during a routine gynecological examination. Methods for diagnosing ectopic pregnancy:
- beta-hCG test is the only biochemical indicator for diagnosing ectopic pregnancy. In a normal course, the increase in hCG should double every 2-3 days. Suspicion will be a sluggish increase in hCG, no more than 1.5 times every 2-3 days. A low rise in beta-hCG may be with an undeveloped uterine or ectopic pregnancy;
- An early ultrasound of an ectopic pregnancy should be transvaginal to determine where the embryo has attached. It is desirable to carry out for 5-7 days after the delay of menstruation.
Blood progesterone testing is not indicated for the diagnosis of tubal pregnancy. Only according to the beta-hCG data, it is impossible to make a diagnosis, it is necessary to do a transvaginal ultrasound.
Complications
Termination of an ectopic pregnancy usually occurs for 4-6 weeks and develops as a rupture of the tube or as a tubal abortion.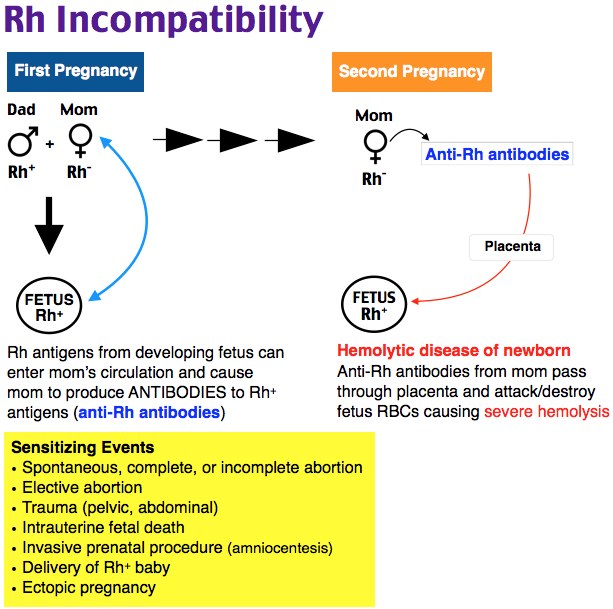
Signs of interruption by type of tube rupture:
- delayed menstruation;
- intra-abdominal bleeding, characterized by a sharp decrease in blood pressure, pallor, cold sweat, dizziness, fainting, nausea, vomiting;
- sharp and very severe pain in the abdomen.
May occur after 6 weeks of pregnancy. An extremely dangerous situation for a woman's life and require immediate surgical intervention.
Signs of interruption by type of tubal abortion:
- delayed menstruation;
- bleeding from labia;
- constant aching, dull pain in the lower abdomen, may radiate to the lower back, groin, rectum.
Tubal abortion proceeds for a long time, without acute manifestations. With detachment of the fetal from the fallopian tube, blood enters the abdominal cavity in small portions and therefore there are no sharp symptoms. On gynecological examination, an increase in the size of the uterus and appendages, pain on palpation of the posterior fornix of the vagina is determined.
What complications can be:
- severe bleeding;
- repeated ectopic pregnancy;
- infertility.
Ectopic pregnancy and consequences
- probability of normal pregnancy and childbirth - about 50%;
- repeated ectopic pregnancy - about 20%;
- 15-20% miscarriages;
- 25% infertility.
Ectopic pregnancy, what treatment is used
If an ectopic pregnancy is suspected, a woman should be urgently hospitalized in a hospital, even if there are no complaints of well-being. The main threat is that the pregnancy can be terminated at any time.
The effectiveness of treatment is determined by timely diagnosis at an early stage and the choice of using laparoscopic access.
In the hospital, after 48-72 hours, repeat ultrasound, determine the level of beta-hCG and conduct a gynecological examination. If the increase in beta-hCG is less than 50% in 48-72 hours and the fetal egg is not detected, then the patient will be shown a diagnostic laparoscopy.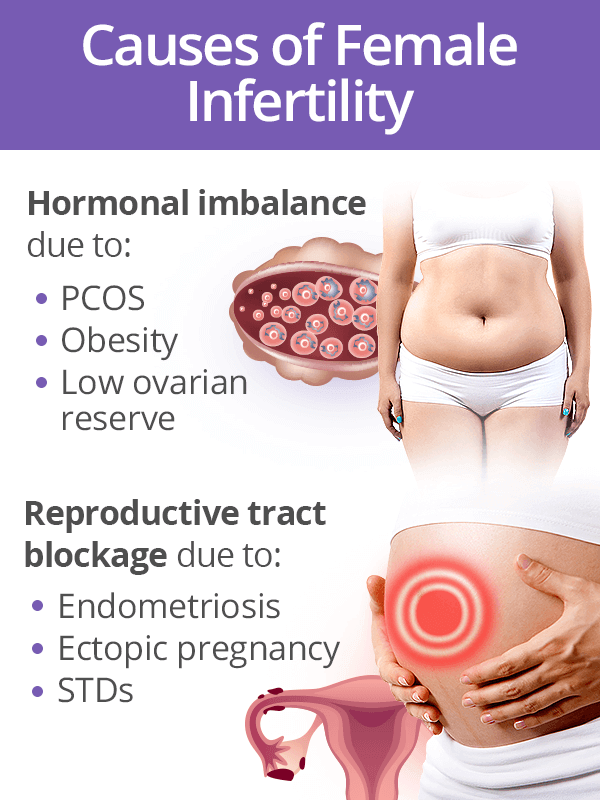 Such diagnostics will help not to wait for the rupture of the tube, blood loss and shock.
Such diagnostics will help not to wait for the rupture of the tube, blood loss and shock.
Currently in Russia, ectopic pregnancy is treated only surgically:
- radical (tubectomy) — removal of the tube along with ectopic pregnancy. It is used for rupture or overstretching of the pipe;
- organ-preserving (tubotomy) - the tube is cut and the fetal egg is removed. The method is used with timely detection and slight stretching of the pipe.
Only surgery can remove the fetal egg, which is attached outside the uterine cavity. The most common is laparoscopy. The surgeon removes the fetal egg and partially or completely the fallopian tube through small punctures. After 3 days, the woman is allowed to go home.
Opening of the abdominal cavity is usually used when laparoscopic access is difficult (pronounced adhesive process, a large amount of blood in the abdominal cavity, obesity).
The nature of the operation depends on the condition of the woman, the volume of blood loss, location and size of the ovum. With laparoscopic access, the incidence of recurrent ectopic pregnancy is lower than with laparotomy.
With laparoscopic access, the incidence of recurrent ectopic pregnancy is lower than with laparotomy.
Recovery from an ectopic pregnancy
It is important to have a complete examination in order to understand the cause of an ectopic pregnancy and eliminate it. Observe physical and sexual rest for at least a month after surgery. Measures should be aimed at restoring reproductive function after surgery:
- prevention of adhesions - physiotherapeutic methods, reflexology, injections of longidase, lidase;
- oral contraceptives are recommended for the duration of rehabilitation therapy. As a rule, 6 months after an ectopic pregnancy, you can become pregnant again.
If a tubal pregnancy was diagnosed in time, then the chances of conceiving and bearing a healthy child are quite high. When planning a pregnancy, be sure to consult a doctor.
How to avoid ectopic pregnancy
Prevention involves reducing the likelihood of the causes that lead to the development of ectopic pregnancy:
- timely treatment of inflammatory diseases of the genital organs;
- reliable contraception as abortion prevention;
- the use of contraception is strictly under medical supervision;
- pregnancy planning, complete examination;
- treatment of hormonal disorders.