How to stop your child from bedwetting
How to Stop Bedwetting: Bedwetting Solutions
At age 7, Billy was getting invitations for sleepovers from friends. He wanted to go, but there was a problem: how to stop bedwetting.
Bedwetting had been an ongoing issue for Billy, says his mother, Jane, (not their real names) of Bethesda, Md. Her two older children hadn't had the problem, but Billy couldn't seem to stay dry. "He wanted to start being dry so he could go to sleepovers," she says.
Billy has lots of company -- 20% of 5-year-olds and 10% of 6-year-olds are bedwetters, says the American Academy of Pediatrics. Most grow out of it and usually there's nothing serious going on. But statistics and research weren't making the sleepovers easier for Billy.
So Jane broached the topic with Billy's pediatrician and heard some good news. Bedwetting solutions abound, from simple "reward" systems to using urinary bed alarms -- the strategy that ended up working for Billy.
Here, what parents hoping to help their child stop bedwetting need to know about solutions.
Addressing Bedwetting Misconceptions
Before pediatricians suggest a specific bedwetting solution or treatment, most seek to educate parents.
Bedwetting "often runs in families," says Howard J. Bennett, MD, a pediatrician in Washington, D.C., author of WakingUp Dry, and Billy's pediatrician. Usually, the child becomes dry at about the same age as the parent did. And no matter what you may think, bedwetting is not due to laziness or spite, two common misconceptions, pediatricians say.
Getting your pediatrician's input, instead of trying remedies on your own, may speed things along, according to a study published in the Journal of Urology. Researchers found that when children followed their pediatrician's advice about bedwetting solutions they were dry earlier than a group of children whose parents picked the treatment to stop bedwetting on their own.
Bedwetting: Ruling Out Medical Problems
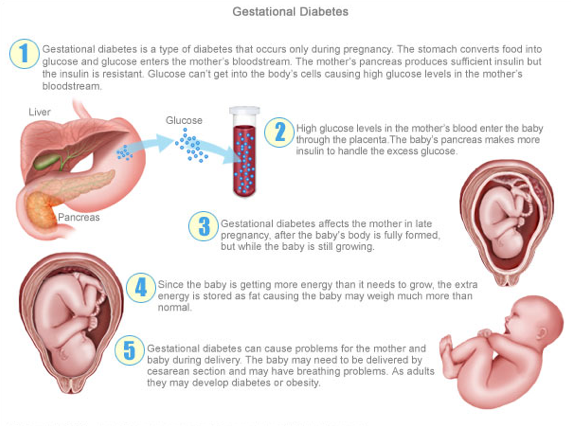
Next, physicians are careful to take a medical history and rule out medical causes, such as constipation or infection. Most bedwetting is what doctors call primary enuresis, meaning the child has always wet the bed. Doctors think it’s usually caused by a delay in the maturation of the mechanisms controlling the bladder.
Most bedwetting is what doctors call primary enuresis, meaning the child has always wet the bed. Doctors think it’s usually caused by a delay in the maturation of the mechanisms controlling the bladder.
But if bedwetting occurs after the child has been dry for a year or so, it’s termed secondary enuresis, and doctors must look more closely at the cause. Secondary enuresis could occur with psychological stress or trauma, and the child may need counseling or other treatment.
If no medical or psychological causes for bedwetting can be found, the family can move on to ways to help the child stop bedwetting.
How to Stop Bedwetting: Urinary Bed Alarms
Urinary bed alarms are generally regarded as the most effective bedwetting treatment for the long term.
Alarms are available in several different styles, but all include a moisture sensor and an alarm. One model, for instance, involves a moisture sensor worn on the underwear or pajamas, attached to an alarm box worn on the shirt. The sensor detects moisture almost immediately and sounds the alarm, alerting the child to get up and go to the bathroom.
The sensor detects moisture almost immediately and sounds the alarm, alerting the child to get up and go to the bathroom.
In a report summarizing the medical evidence on bedwetting treatments such as alarms, behavioral interventions such as giving rewards, and medications, alarms were found to be the most effective. The study was published in the Journal of Wound Ostomy Continence Nursing.
In another study, published in the Journal of Paediatric Child Health, researchers found that 79% of 505 children who wore bed alarms achieved dryness within about 10 weeks (half took longer, half took less time). Six months later, 73% of those children were still dry.
While many parents try the other strategies first even before discussing bedwetting with their pediatrician, some go straight to the bed alarm.
How to Stop Bedwetting: Rewards for Dry Nights
Eleanor and her husband, Ray, moved to another common strategy -- the reward system. This can involve giving the child a small toy after a dry night or rewarding him with a trip to the park or someplace else he wants to go. Eleanor and Ray bought little prizes, such as coloring books and rubber balls, and pasted them on the wall so Michael could look at them.
Eleanor and Ray bought little prizes, such as coloring books and rubber balls, and pasted them on the wall so Michael could look at them.
"When he had a successful night, he would pick a prize," Eleanor says. "That worked for a while."
Anything special to the child can be used as a reward, says Robert Mendelson, MD, a Portland, Ore., pediatrician who often counsels parents about bed-wetting issues. Load on the praise, too, he says. "Any time the child is dry in the morning, tell them how great they are," he says. "Congratulate them, tell them, 'You are getting to be a big boy or girl.'"
How to Stop Bedwetting: "Lifting"
Eleanor and Ray also tried a technique called "lifting." This strategy involves making sure your child goes to the bathroom right before his bedtime, and then waking him up after he has been asleep two or three hours and taking him to the toilet.
"We went to two times a night," Eleanor says. "One at 11 and the other at 2:30 a.m. My husband got the 2:30. "
"
Patience won out. "It didn't work immediately," she says. "We did this for over six weeks." Suddenly, one day he didn't wet. And the next, and the next. She doesn't know if it was the lifting or just time. "I think he just grew out it," say Eleanor, who is relieved.
"Lifting can be a helpful temporary measure while you are waiting for kids to get dry on their own," agrees Bennett.
How to Stop Bedwetting: Bladder Training
Helping your child delay urination during the day is another strategy. Using an egg timer, you ask your child to tell you when they have to go, then ask them to hold it for another few minutes. You start with about five minutes and add a couple minutes each time, they say. The goal is to get to 45 minutes.
But this process takes time and you should do it every day, he says. If old enough, a motivated child can do it on their own.
How to Stop Bedwetting: Fluid Restriction
Limiting fluids at night is widely suggested but can be difficult to do. Eleanor, 40, of West Covina, Calif., tried taking away liquids every night at 7 p.m. when she was attempting to help her son Michael, now 4 1/2, stay dry all night.
Eleanor, 40, of West Covina, Calif., tried taking away liquids every night at 7 p.m. when she was attempting to help her son Michael, now 4 1/2, stay dry all night.
Then she moved it up to 6 p.m. "He started begging me for a tiny drink, and I felt so bad," she says. Looking into his eyes as he begged for just a sip was too much for her, she says. "So I couldn't do that anymore."
"I don't recommend restricting fluids unless it is the kid's idea," says Bennett. "Otherwise the kids see it as a punishment."
Bedwetting Products: Waterproof Sheets
Plastic sheets and disposable underwear can save sanity and mattresses. You can also use the "double bubble" method of making a bed. Layer a plastic sheet, regular sheet and a blanket; then repeat the process.
Teach the child how to strip off the top layer and make a fresh bed. Keep some fresh pajamas or disposable underwear bedside, too, so they can easily change into dry ones.
Bedwetting Products: Super Training Pants
Super absorbent training pants designed for use at night can help, as well. Bennett tells parents they are fine to use when the child is 4, 5, or 6.
Bennett tells parents they are fine to use when the child is 4, 5, or 6.
By age 7, they usually suggests trying something else.
Bedwetting Treatment: Medications
Medications usually work while the child is taking them, but once they’re stopped the bedwetting typically starts again. And the medicines can have side effects.
Among the bedwetting treatment options are desmopressin (DDAVP), a synthetic copy of a body chemical that controls urine production, given at bedtime. It's available in tablets and nasal spray forms, but the nasal spray is no longer indicated for primary bedwetting treatment, according to an alert issued by the FDA in late 2007. The agency cites risks of the nasal spray causing low blood sodium levels, in turn possibly leading to seizures and death.
Bennett sometimes prescribes DDAVP in tablet form temporarily, perhaps to help a child stay dry on a sleepover or at camp. "It works immediately if you have the right dose," he says. He will try out a dose before it's needed to be sure he has picked an effective one.
Another medication option is imipramine (Tofranil, Tofranil-PM), an antidepressant that may work by reducing urine production, affecting the amount of time a child can hold urine in the bladder, or other ways.
Bedwetting medications may help in a social situation such as sleepovers but are usually a last resort, according to the American Academy of Pediatrics. They are not recommended for children younger than 5 years old.
Bedwetting Solutions: Success Stories
Jane's family had tried most of the do-it-yourself strategies with Billy before turning to the bed alarm because nothing else had worked.
Using the bed alarm takes commitment from parents and children, according to Bennett, who says he has worked as an unpaid consultant helping bed alarm companies with product design. And it takes different amounts of time to work, he says.
"Early on, even the alarm didn't wake him," Jane recalls. "We would have to go wake him up." Things got better. "It wakes them up quicker and quicker. It took us a couple months of the alarm going off, and then it worked well."
It took us a couple months of the alarm going off, and then it worked well."
"It took probably six months until he was totally dry. And then he had a recurrence about a year later. We put on the alarm again and in a week he was OK."
But Susan, her husband Mark, and their son Mike (not their real names), who was then 6, had a much more dramatic experience using the bed alarm. Within a week of using the alarm, he was dry. "He had a problem at least three or four times a week," Susan says. After the alarm worked, she says happily: "He went from a guy who wet the bed a few times a week to a guy who never had a problem."
Bedwetting Solutions: Getting to the Payoff
Encouragement is crucial as you work to help your child stay dry, Mendelson says. He encourages parents who wet the bed as children to tell their kids -- and to tell them at what age they became dry. It ''points out the hereditary nature of the problem" and helps children understand that eventually they will have control over the problem, he says.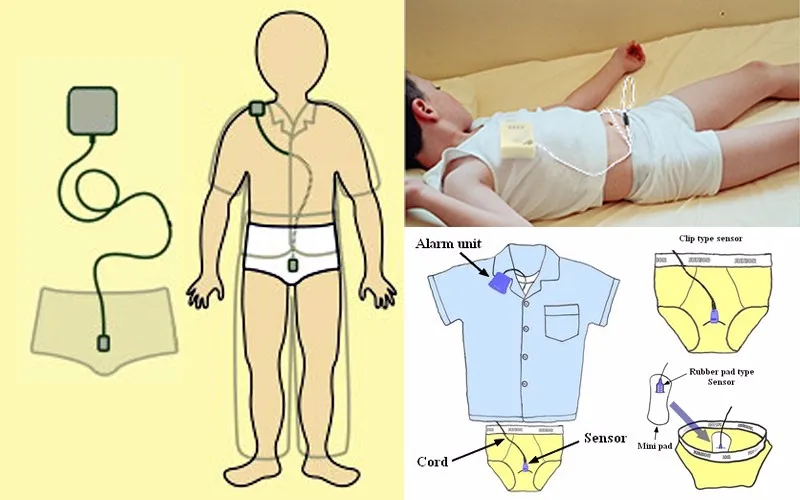
Whatever method helps a child stay dry, most parents -- and kids -- are relieved when dry nights prevail. Eleanor, who used the reward system, considers dry nights a milestone that may even surpass other important ones such as learning to walk or starting preschool.
"This one wins," she says happily. "It is the biggest milestone we have hit so far."
Bedwetting solutions: Expert pediatrician offers help for kids | Patient Education
Bedwetting, also known as nocturnal enuresis, is common in childhood and most children will grow out of it as they age. We asked UC Davis pediatrician Lena van der List about causes, strategies and solutions that can help families beat the bedwetting blues.
What causes bedwetting?
In the majority of young children who experience bedwetting, the main issue is sleep arousal. The brain is not signaling to awaken when the bladder is full, and, at times, doesn’t even signal the child to wake up when wet. Frequently, these kids are extremely heavy sleepers. Kids may also produce more urine than expected at night (which is called nocturnal polyuria) or have small bladder capacity (with frequent small urinations throughout the day and night), which may increase their risk for bedwetting.
Kids may also produce more urine than expected at night (which is called nocturnal polyuria) or have small bladder capacity (with frequent small urinations throughout the day and night), which may increase their risk for bedwetting.
What are other causes of bedwetting?
- Constipation, which, if appropriately treated, can alleviate the problem. Constipation causes bedwetting because a large amount of stool may actually push up against the bladder and prevent the bladder from expanding all the way. Doctors may prescribe a medication to help “clean out” the stool and keep your child more regular. The most commonly used medication is a laxative, polyethylene glycol, with the brand name Miralax.
- Urinary tract infections
- Genetic predisposition. If one parent experienced problems with nocturnal enuresis, on average, half of their children also will. If both parents did, then three-quarters of their children will.

- Sleep disorders like obstructive sleep apnea. It is estimated that 30% of kids with sleep apnea will also have nocturnal enuresis. A child with symptoms of sleep apnea may snore at night, have periods where they seem like they pause breathing or be excessively sleepy during the day - although some kids may exhibit more hyperactivity. Sleep apnea can be diagnosed with a sleep study (these are frequently performed by pulmonologists). If a child is found to have sleep apnea, the most common treatment is removing the tonsils and adenoids (tonsillectomy/adenoidectomy). This allows for a more open airway at night and resolves the apnea. One study from 2016 looked at kids with bedwetting before and after tonsillectomy/adenoidectomy were performed for obstructive sleep apnea. After the surgery, 76% showed complete resolution of bedwetting, however the studies have been mixed on this.
- There are other more serious conditions including diabetes, spinal cord issues that prevent a normal functioning bladder, and metabolic issues.
 While these are extremely rare, they should be considered in older kids with persistent enuresis that does not respond to typical treatment.
While these are extremely rare, they should be considered in older kids with persistent enuresis that does not respond to typical treatment.
How can pediatricians help with bedwetting kids?
When you visit your doctor with a bedwetting concern, they may ask you questions like how long has it been going on? What time does it occur most nights? How much fluid and what types of fluid does your child drink in a day? Has your child had any previous “dry” periods? How often do they stool and what is it like? Do they ever have continence issues during the day?
Your child’s physician will perform an exam, which may include a genital exam and a neurologic exam. He or she may perform a urinalysis (where they ask your child to pee in a cup) to make sure there isn’t an infection or signs of diabetes, or extremely diluted urine.
Some physicians may ask you to keep a diary documenting all elimination (stools, day and night-time urination), fluids consumed, or even at times the volume of urine to help pinpoint the problem.
If the doctor doesn’t find a medical problem, how can parents help stop bedwetting?
Well, the first criteria is that the child is motivated for it to stop. If the child is not bothered by the bedwetting, each of these proven methods is much less likely to work:
- Limit their nighttime fluid intake. A good rule of thumb is for the child to consume two-thirds of their fluid goal before the end of the school day and then one-third of the fluid after school with no more drinking in the last one to two hours before bed.
- Have a stable bedtime routine. Going pee before bed and first thing upon awakening should always be encouraged.
- Consider stopping pull ups or diapers at night once they are reliably potty trained during the day. For some kids, these may be used as a crutch and could continue to trick their brains into thinking they don’t have to wake up to urinate.
Do bedwetting alarms work?
Bedwetting alarms are recommended by the International Children’s Continence Society. It is worn attached to the pajamas or underwear and will alert the child as soon as wetness or moisture is detected. At first, the alarm may not wake the child so parents need to play active roles in waking up their kid, walking him or her to the bathroom. Their child should help change the sheets before going back to bed.
It is worn attached to the pajamas or underwear and will alert the child as soon as wetness or moisture is detected. At first, the alarm may not wake the child so parents need to play active roles in waking up their kid, walking him or her to the bathroom. Their child should help change the sheets before going back to bed.
The alarm needs to be used nightly and may take two to three months to work, but it has been shown to be very successful in up to two-thirds of children. It also costs about $60 and is typically not covered by insurance so this can be a barrier for some families. It is recommended that parents and kids continue to use the alarm until two weeks of consecutive dry nights!
Are there medications that can help?
The most commonly used medication for bedwetting is called desmopressin. It reduces the amount of urine produced overnight so it may be more beneficial in those kids that produce more urine at night. Studies have shown a 20-30% response. One side effect of the medication can be low sodium, so parents need to be aware of the signs, including confusion, weakness and even seizures.
One other bedwetting medication that is occasionally used is called imipramine. It belongs to a class of medications called tricyclics and is also used to treat depression. It is less frequently prescribed these days because if too much is taken, an overdose may occur. Before starting on this medication, the heart needs to be monitored with an EKG.
There are a few other medications that have been used, but they have a higher likelihood of side effects and are therefore not routinely recommended as a first line of treatment in kids.
What is dry bed training, and how do I do it?
Dry bed training is a more hands-on, parent-led approach.
- On the first night, awaken the child once every hour until 1 a.m., asking if he or she has to use the bathroom. At the 1 a.m. awakening, tell the child to try using the bathroom, even if he or she is dry.
- The second night, wake him or her only once, three hours after falling asleep.
- The third through fifth nights, wake the child once each night.
 Start at two-and-a-half hours after falling asleep, and keep diminishing the interval each night, so that on the fifth night, the child is awakened one hour after falling asleep.
Start at two-and-a-half hours after falling asleep, and keep diminishing the interval each night, so that on the fifth night, the child is awakened one hour after falling asleep. - On the sixth night, tell the child to self-awaken from then on.
One older study reported a great than 90% success rate with this method.
What do you recommend when a child has had a dry period for more than six months and then begins to wet the bed again?
This is referred to as secondary nocturnal enuresis. This is often related to a psychological stressor like a divorce or the birth of a new sibling. Exploring what may be bothering your child is a good idea. But the above other medical diagnoses should also be considered.
What’s the best way for parents to respond to bedwetting while still making sure they are being sensitive toward the child?
As kids get older, typically closer to around 6-8 years old, they begin to get self-conscious and embarrassed by bedwetting.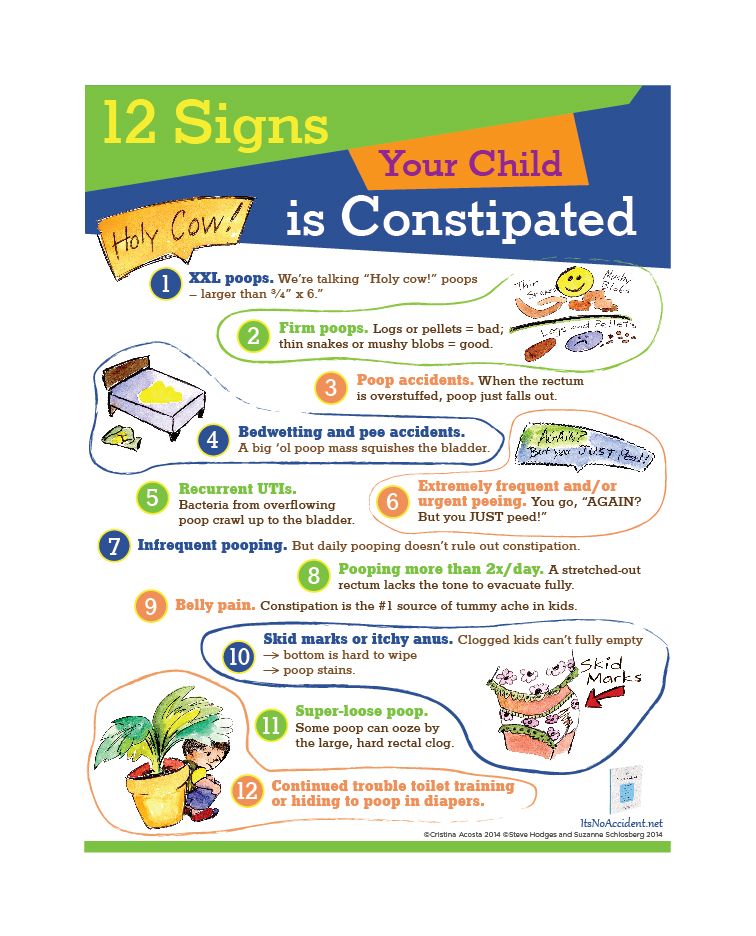 They may resist sleepovers. This can affect their self-esteem and friendships. It’s important that the child doesn’t feel like it’s their fault or something is wrong with them.
They may resist sleepovers. This can affect their self-esteem and friendships. It’s important that the child doesn’t feel like it’s their fault or something is wrong with them.
They should not be shamed. For example, never say “I can’t believe you did this again” or “You are costing us a lot of money having to wash your dirty sheets every night.” It’s important that bedwetting is not discussed in front of the child’s siblings or friends. Parents should reassure the child that it’s normal for his or her age. Act as an ally to the child and show that you’re going to tackle this as a team.
Parents may want to teach the child to do the laundry so they can wash their sheets and pajamas on their own. This should not be treated like a punishment; it is an opportunity for the child to have control over it and limit who knows about it. This also helps develop responsibility. If you approach it in this supportive and collaborative way, most kids will outgrow it.
General information
- Healthy Children Bedwetting
- Healthy Children Bedwetting in Children & Teens: Nocturnal Enuresis
- Healthy Children Radio: Bedwetting
- International Children’s Continence Society
- Enuresis alarms on Amazon
- Kids Considered podcast episode: Bedwetting Basics
Enuresis in children - simple words about a complex problem
Nocturnal enuresis is a disease that is involuntary urination during a night's sleep. Enuresis refers to the types of urinary incontinence, which in itself is one of the most common problems of childhood and adolescence. According to official statistics, 20% of children aged 5 years, 10% -15% of children aged 10 years and at least 3% of adolescents suffer from various forms of urinary incontinence. More accurate information about the prevalence of this pathology in children does not exist. This is partly due to the fact that neurologists, psychiatrists, urologists, nephrologists deal with it - and each specialist had his own view of the problem and his own statistics.
Enuresis refers to the types of urinary incontinence, which in itself is one of the most common problems of childhood and adolescence. According to official statistics, 20% of children aged 5 years, 10% -15% of children aged 10 years and at least 3% of adolescents suffer from various forms of urinary incontinence. More accurate information about the prevalence of this pathology in children does not exist. This is partly due to the fact that neurologists, psychiatrists, urologists, nephrologists deal with it - and each specialist had his own view of the problem and his own statistics.
As practice shows, among doctors there is no clear understanding of when exactly the symptom of "wet bed" should be considered a pathological phenomenon. It is widely believed that nocturnal enuresis up to 5 years is the norm. It must be said that this age was chosen very conditionally and is associated with the formation of the so-called. "mature type of urination", when the child acquires the ability to control his behavior associated with going to the toilet. It is not uncommon to encounter a situation where a doctor or parents do not pay attention to enuresis at all until the age of 14-15, citing the fact that the child will gradually “outgrow” the problem. This formulaic approach is unacceptable for two reasons.
It is not uncommon to encounter a situation where a doctor or parents do not pay attention to enuresis at all until the age of 14-15, citing the fact that the child will gradually “outgrow” the problem. This formulaic approach is unacceptable for two reasons.
Firstly, urinary incontinence (and enuresis in particular) at first may be the only symptom of much more serious diseases of the urinary system, nervous or endocrine system. Thus, enuresis occurs in children with urinary tract infections (cystitis), helminthiases, congenital malformations of the urogenital region or obstruction of the urinary tract, neurogenic bladder, abnormal development of the spine and spinal cord. In time to suspect such a situation, conduct a competent examination and treatment can only be a specialist urologist, who is well versed in the pathology of urination in children. Neither general practitioners, nor even parents, have such competence.
Secondly, almost all children with urination disorders are in a state of latent social maladaptation. They have a low level of self-esteem, often conflict situations arise in the children's team and family. All this negatively affects the development of the child and, in the end, leads to serious psychological problems.
They have a low level of self-esteem, often conflict situations arise in the children's team and family. All this negatively affects the development of the child and, in the end, leads to serious psychological problems.
According to a survey of Swedish psychologists, urinary incontinence for a primary school student is one of the three most severe "critical" stressful situations in life (after divorce and the death of parents).
In addition, recent studies have shown that nocturnal enuresis in children is almost identical in nature to the problem of frequent nocturnal urination in the elderly. Constant nighttime waking up and going to the toilet is the most debilitating symptom for adults, keeping them on medication or going under the surgeon's knife for years. Therefore, one should not assume that nocturnal enuresis is harmless and does not affect the well-being of the child.
There is still no unified protocol for the diagnosis and treatment of children with nocturnal enuresis. In practice, EMC Children's Clinic urologists adhere to the principles developed by the ICCS (International Urinary Incontinence Society). After a comprehensive diagnosis and exclusion of pathologies requiring immediate surgical or medical treatment, step-by-step treatment can be presented as follows:
In practice, EMC Children's Clinic urologists adhere to the principles developed by the ICCS (International Urinary Incontinence Society). After a comprehensive diagnosis and exclusion of pathologies requiring immediate surgical or medical treatment, step-by-step treatment can be presented as follows:
1st step: behavioral therapy;
2nd step: alarm – therapy;
Step 3: pharmacotherapy.
Behavior Therapy
This is a system of cognitive methods. The main help at this stage is to inform the family and the child himself about the observance of the daily regimen and especially the drinking regimen. If a violation of the drinking and urination regimen, which is behavioral and situational in nature, is detected, correction of these violations is required before any types of drug treatment under the supervision of a pediatrician. The drinking regimen should be organized so that the fluid intake is distributed evenly throughout the day and with a restriction in the evening. In the evening, quiet games and reading are recommended. Such therapy requires the support of parents, the desire of the child, patience and time.
In the evening, quiet games and reading are recommended. Such therapy requires the support of parents, the desire of the child, patience and time.
The child and parents need to learn how to learn how to properly empty the bladder and control the frequency of stools. It is useful to continue to keep a diary of urination frequency and enuresis episodes, as well as the time of defecation. The effectiveness of such therapy is monitored by a doctor every 1-3 months. At the same time, conversations are held with parents and the child, supporting the motivation to continue treatment.
Alarm therapy
After correcting the stereotype of the child's behavior for 4-6 months and in the absence of nocturnal overproduction of urine (diagnosed by the diary of urination), the use of a night alarm clock with sensors that respond to moisture (alarm therapy) can be added to the treatment. This method helps the child to wake up at the moment the urine gets wet. This type of treatment gives a particularly good effect in families with stable motivation not only for the child, but also for the parents. If there is no improvement during the first month of treatment, it should be discontinued and proceed to pharmacotherapy.
If there is no improvement during the first month of treatment, it should be discontinued and proceed to pharmacotherapy.
Pharmacotherapy
The third step is pharmacotherapy. We categorically do not recommend performing this stage on your own, guided by data from the Internet or the advice of non-specialists. For the treatment of nocturnal enuresis, both hormonal-type drugs and means of influencing the central nervous system are used. Only a pediatric urologist-andrologist, together with a neurologist and a pediatrician, can correctly select a drug regimen without harming the child.
Treatment of children with enuresis is a complex task that requires the participation of diverse highly qualified specialists: a pediatric urologist-andrologist, a pediatrician, a neurologist, a psychologist, specialists in radiation and ultrasound diagnostics, and rehabilitation specialists. At the EMC Children's Clinic, you can get an appointment with a pediatric urologist-andrologist, who has many years of experience in the specialized clinical center "Children's urinary pathology", which is the leading institution in the country for the problem of urinary incontinence. All necessary analyzes and studies can be performed on the basis of the clinic using modern equipment in the shortest possible time. Experienced psychologists will help in solving this problem.
All necessary analyzes and studies can be performed on the basis of the clinic using modern equipment in the shortest possible time. Experienced psychologists will help in solving this problem.
Treatment of nocturnal enuresis in children
Bedwetting has been known to mankind for many centuries. At the present stage of development of medicine, bedwetting is understood as involuntary urination during night or daytime sleep.
When a child first visits a doctor with a complaint of bedwetting, first of all, it is necessary to exclude malformations of the urinary tract and spine, infectious and inflammatory diseases of the urinary system, diseases of the central nervous system, and diabetes. An anamnesis plays an important role in determining the etiology of enuresis and choosing treatment tactics. Particular attention should be paid to the study of obstetric history, in particular, the presence of a threat of termination of pregnancy, preeclampsia, anemia, oligohydramnios, polyhydramnios, chronic intrauterine hypoxia, asphyxia during childbirth. The features of the development of the child in the first three years of life (bruises, concussions of the brain, neuroinfections, etc.) are clarified.
The features of the development of the child in the first three years of life (bruises, concussions of the brain, neuroinfections, etc.) are clarified.
Great importance is attached to finding out the style of upbringing, the requirements of parents for the formation of neatness skills in a child, the presence of leukocyturia, constipation, encopresis. Determine the genetic predisposition, the nature of urinary incontinence, the frequency of episodes; factors preceding the onset of the disease (psychic trauma, nervous shock, hypothermia, acute illness with fever, with or without changes in urine tests), the nature of the child’s night sleep, the presence of pathological sleep phenomena in the form of sleepwalking, sleepwalking, bruxism (grinding teeth ). A detailed, thorough history of the patient with enuresis will avoid many unnecessary examinations.
A fundamental role in the diagnosis of bladder dysfunction is assigned to the clinical analysis of urination. The function of the bladder is assessed by recording the rhythm of spontaneous urination for 2-3 days, special tables are filled in to identify the "mature type of urination" and the syndrome of imperative urination.
Treatment of psychogenic urinary incontinence .
When correcting neurotic disorders, psychotherapeutic and socio-pedagogical measures come to the fore, and then pharmacotherapy. Most often, psychotherapy is carried out against the background of drug treatment: one reinforces the other. Psychotherapy is used mainly in the form of suggestion in a state of somnolence and in a pre-sleep state. In a state of doubt (in the first stage of the hypnotic state), a suggestion is carried out to achieve a sense of inner stability, calmness, and indifference to the mental trauma suffered. In the pre-sleep state, they consistently inspire: 1) a state of somnolence; 2) the elimination of certain symptoms with an emphasis on neurotic urinary incontinence; 3) the transition of a hypnotic state into physiological sleep.
Treatment of neurosis-like involuntary urination due to dysfunction of the urethra and bladder.
The treatment of these disorders is usually long, sometimes lasting for years, and consists of certain physical exercises, daily routine, diet and medication. From physical exercises - this is swimming, cycling, jumping, running. In the morning, patients should do exercises that strengthen the muscles of the small pelvis: jump, jump over a rope, etc.
From physical exercises - this is swimming, cycling, jumping, running. In the morning, patients should do exercises that strengthen the muscles of the small pelvis: jump, jump over a rope, etc.
It is necessary to limit fluid intake in the evening: approximately 2-3 hours before going to bed, do not drink fluids. In the morning and in the middle of the day, fluid intake should not be limited. Try to empty your bladder before going to bed. When urging to urinate, it is recommended to release urine fractionally: release part of the urine, stop releasing, then release it again, etc. This helps to strengthen the sphincters. For the same purpose, before releasing a portion of urine, it is necessary to be patient, not to urinate.
Physiotherapy and related methods of treatment are central to the treatment of urinary incontinence, caused mainly by a violation of the tone of the bladder. The main indication for them is not urinary incontinence in general, but bladder dysfunction. One of the most common physiotherapy treatments for this type of urinary incontinence is galvanization of the bladder area according to Shcherbak. The procedure lasts 10-12 minutes, for a course of 10-12 procedures every other day. An effective way to get rid of bladder dysfunction and associated urinary incontinence is acupuncture.
One of the most common physiotherapy treatments for this type of urinary incontinence is galvanization of the bladder area according to Shcherbak. The procedure lasts 10-12 minutes, for a course of 10-12 procedures every other day. An effective way to get rid of bladder dysfunction and associated urinary incontinence is acupuncture.
Bedwetting has a detrimental effect on the child's psyche. Children are ashamed of their "vice", seek to hide it, react painfully to the ridicule of other children and to the reproaches of adults. They develop a desire to avoid the company of children, there is a feeling of inferiority, timidity, sensitivity, self-doubt, sometimes stubbornness, affective outbursts develop. (pathological development of personality). The wrong approach to children suffering from urinary incontinence (when they are shamed, forced to wash clothes, punished) leads to an increase in the disease.
A child's spiritual experiences cannot pass without a trace for the subsequent development of a person.