Liver problems during pregnancy itching
Cholestasis of Pregnancy | Cedars-Sinai
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is cholestasis of pregnancy?
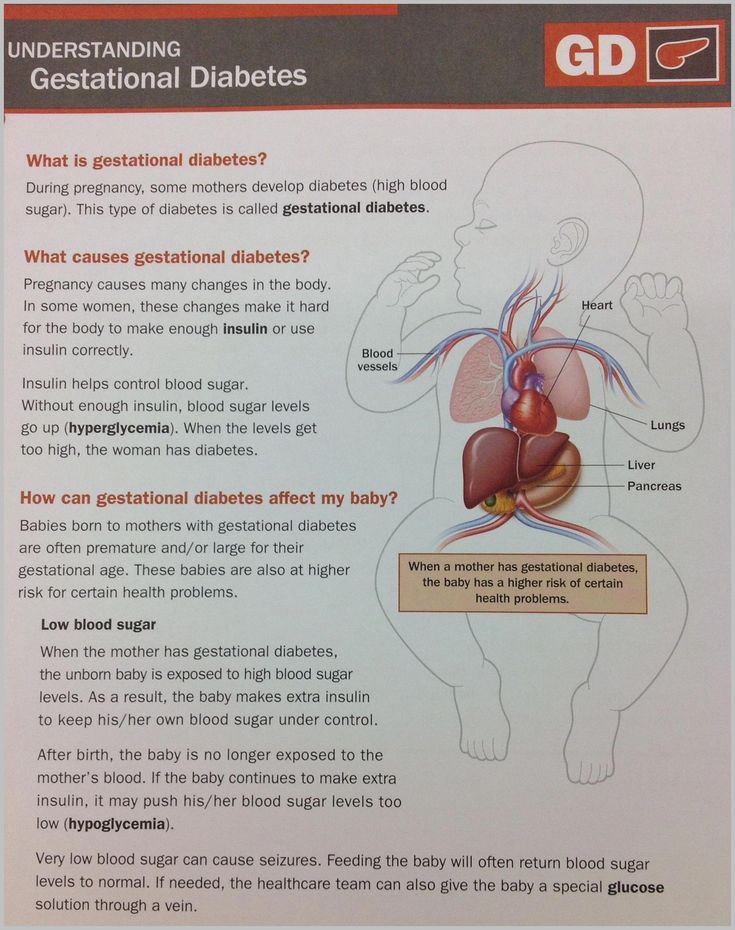
Cholestasis of pregnancy is a liver problem. It slows or stops the normal flow of bile from the gallbladder. This causes itching and yellowing of your skin, eyes, and mucous membranes (jaundice). Cholestasis sometimes starts in early pregnancy. But it is more common in the second and third trimesters. It most often goes away within a few days after delivery. The high levels of bile may cause serious problems for your developing baby (fetus).
What causes cholestasis of pregnancy?
Healthcare providers don't know what causes cholestasis of pregnancy. They do know that this happens:
- Your liver makes bile.
Bile helps break down fats during digestion.
- The gallbladder stores the bile.
- The hormones your body releases during pregnancy change the way the gallbladder works. This may cause bile to slow or stop flowing.
- Bile builds up in the liver and spills into the bloodstream.
What are the symptoms of cholestasis of pregnancy?
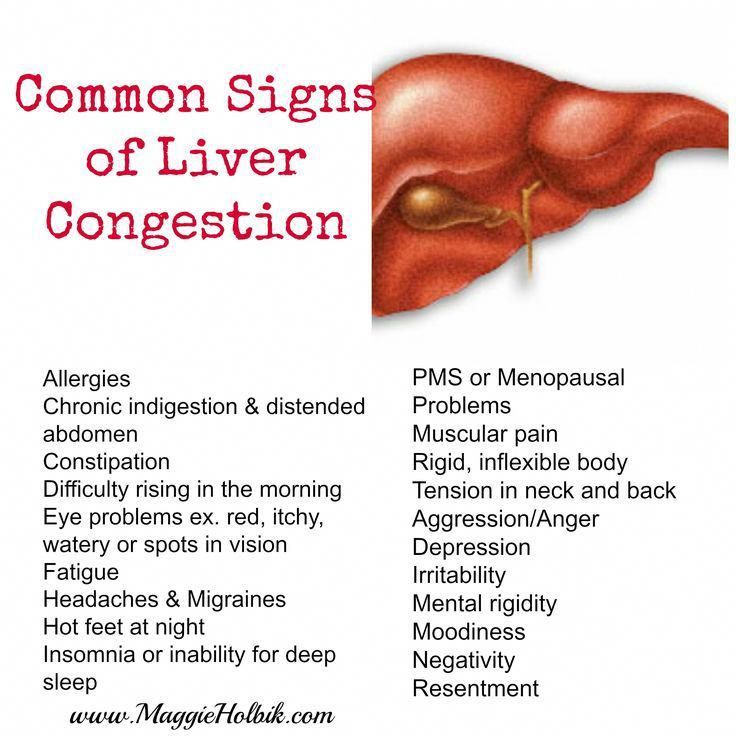
The main symptom of cholestasis of pregnancy is severe itching. This is sometimes called pruritus. It may be all over the body. But it is more common on the palms of the hands and soles of the feet. It may also be worse at night. Other symptoms may include:
- Pain in the belly (abdomen), although this is not common
- Light color of stool (bowel movements)
- Yellow color of skin, eyes, and mucous membranes (jaundice), although this is not common
The symptoms of cholestasis sometimes look like other health conditions. Always see your healthcare provider for a diagnosis.
Always see your healthcare provider for a diagnosis.
How is cholestasis of pregnancy diagnosed?
Your healthcare provider is likely to think you have cholestasis of pregnancy if you have severe itching. Lab tests will help to confirm the diagnosis. You may have these tests:
- Liver function tests, including the amount of bile acid in the blood. This test result is high in cholestasis of pregnancy.
- Other lab tests, including prothrombin time. This checks how well your blood clots.
You may also have other tests such as an ultrasound exam of the tubes that carry bile (bile ducts).
How is cholestasis of pregnancy treated?
You and your healthcare provider will discuss the best treatment for you based on:
- Your pregnancy
- Your overall health and health history
- How sick you are
- How well you can handle certain medicines, procedures, or therapies
The goals of treating cholestasis of pregnancy are to relieve the itching and prevent complications. Treatment may include:
Treatment may include:
- Medicine. To help relieve itching and help lower the level of bile.
- Measuring serum total bile acid. The level of bile in your blood may be checked. This helps your healthcare provider figure out treatment.
- Fetal monitoring. The healthcare provider may check your developing baby for any problems.
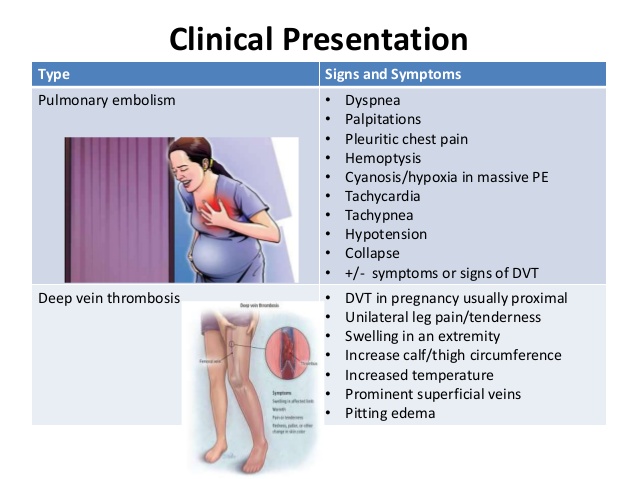
- Early delivery. You may deliver your baby early, between 37 to 38 weeks of pregnancy. This will lessen the risk to your baby. This may be by vaginal delivery with medicine to start labor. Or you may have a cesarean delivery. Your healthcare provider may decide that you should deliver even earlier, depending on your symptoms, test results, and pregnancy history.
What are possible complications of cholestasis of pregnancy?
There is a serious risk of complications in your developing baby if you have cholestasis of pregnancy. The complications include:
- Fetal distress. This means your developing baby is not doing well. For example, the baby may not be getting enough oxygen.
- Preterm birth. You may be at greater risk for giving birth too early.
- Meconium in amniotic fluid. This means your baby has a bowel movement before birth. This may cause very serious breathing problems.
- Breathing (respiratory) problems. Your baby may have breathing problems as a newborn.
Cholestasis of pregnancy can also lead to vitamin K deficiency. This will need to be treated before you give birth, because it can cause you to bleed too much.
When should I call my healthcare provider?
Call your healthcare provider if you have:
- Severe itching
- Yellow coloring of your eyes, skin, or mucous membranes (jaundice)
Key points about cholestasis of pregnancy
- Cholestasis of pregnancy is a condition that slows or stops the normal flow of bile in the gallbladder.
- It can cause severe itching. This is the most common symptom.
- The goals of treating cholestasis of pregnancy are to relieve itching and prevent complications for your developing baby.
- Babies of women with cholestasis are often delivered early (usually around 37 weeks) because of the risks.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Medical Reviewer: Irina Burd MD PhD
Medical Reviewer: Donna Freeborn PhD CNM FNP
Medical Reviewer: Heather Trevino
© 2000-2022 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Itching and intrahepatic cholestasis of pregnancy
Itching is common in pregnancy. Usually it's thought to be caused by raised levels of certain chemicals in the blood, such as hormones.
Later, as your bump grows, the skin of your tummy (abdomen) is stretched and this may also feel itchy.
However, itching can be a symptom of a liver condition called intrahepatic cholestasis of pregnancy (ICP), also known as obstetric cholestasis (OC).
ICP needs medical attention. It affects around 1 in 140 pregnant women in the UK.
Symptoms of ICP
The main symptom is itching, usually without a rash. For many women with ICP, the itching is often:
- more noticeable on the hands and feet, but can be all over the body
- worse at night
Other symptoms can include:
- dark urine
- pale poo
- yellowing of the skin and whites of the eyes (jaundice), but this is less common
Symptoms of ICP typically start from around 28 weeks of pregnancy, but it's possible to develop the condition earlier.
Non-urgent advice: Call your midwife or GP if you have itching that's:
- mild or distressing, possibly worse at night
- anywhere on your body, but may be worse on the palms of your hands and soles of your feet
Feeling itchy like this can be a sign of ICP and needs to be checked.
Mild itching
Wearing loose clothes may help prevent itching, as your clothes are less likely to rub against your skin and cause irritation.
You may also want to avoid synthetic materials and opt for natural ones, such as cotton, instead. These are "breathable" and allow the air to circulate close to your skin.
You may find having a cool bath or applying lotion or moisturiser can help soothe the itching.
Some women find that products with strong perfumes can irritate their skin, so you could try using unperfumed lotion or soap.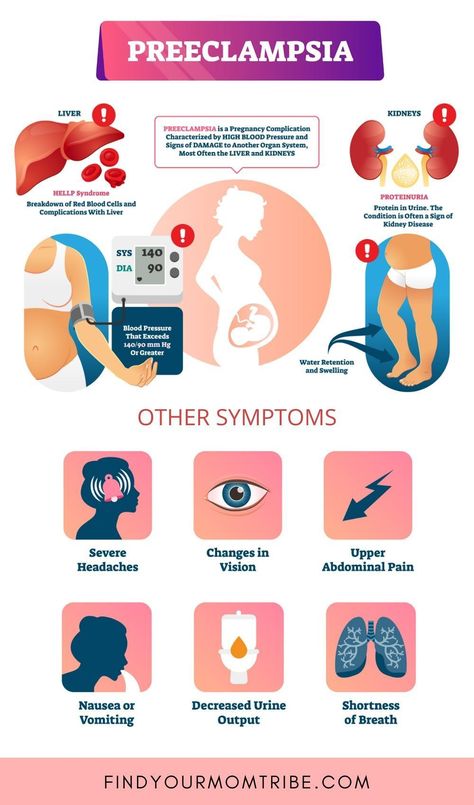
Mild itching is not usually harmful to you or your baby, but it can sometimes be a sign of a more serious condition, particularly if you notice it more in the evenings or at night.
Let your midwife or doctor know if you are experiencing itching so they can decide whether you need to have any further investigations.
Intrahepatic cholestasis of pregnancy
Intrahepatic cholestasis of pregnancy (ICP) is a potentially serious liver disorder that can develop in pregnancy.
Normally, bile acids flow from your liver to your gut to help you digest food.
In ICP, the bile acids do not flow properly and build up in your body instead. There's no cure for ICP, but it should go once you've had your baby.
ICP seems to run in families, but it can happen even if there is no family history. It is more common in women of south Asian origin, affecting around 1 in 70 to 80 pregnancies.
It is more common in women of south Asian origin, affecting around 1 in 70 to 80 pregnancies.
If you have had ICP in a previous pregnancy, you have a high chance of developing it again in another pregnancy.
Some studies have found that babies whose mothers have ICP have a higher chance of being born prematurely or stillborn.
Because of the link with stillbirth, you may be offered induction of labour. This could be any time from 35 weeks, depending on the level of bile acids in your blood.
If you have ICP, you will probably be advised to give birth in hospital under a consultant-led maternity team.
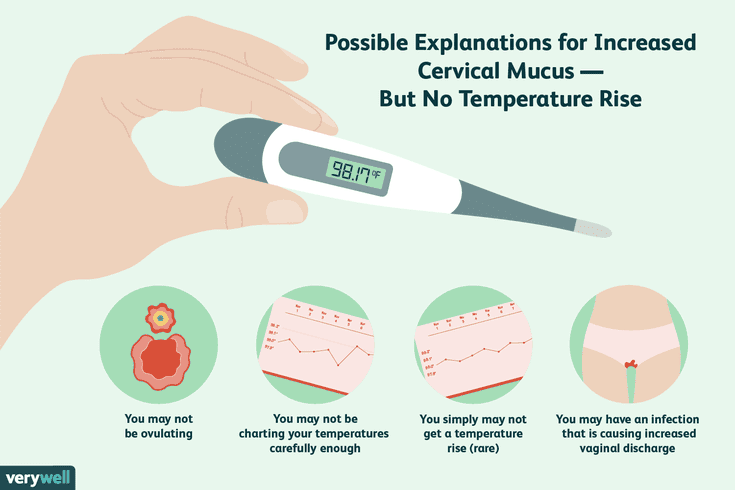
Diagnosis and treatment of ICPICP is diagnosed by excluding other causes of the itch. Your doctor will probably talk to you about your medical and family history and advise you to have some blood tests.
These will include tests to check your liver function (LFT) and measure your bile acid levels (BA).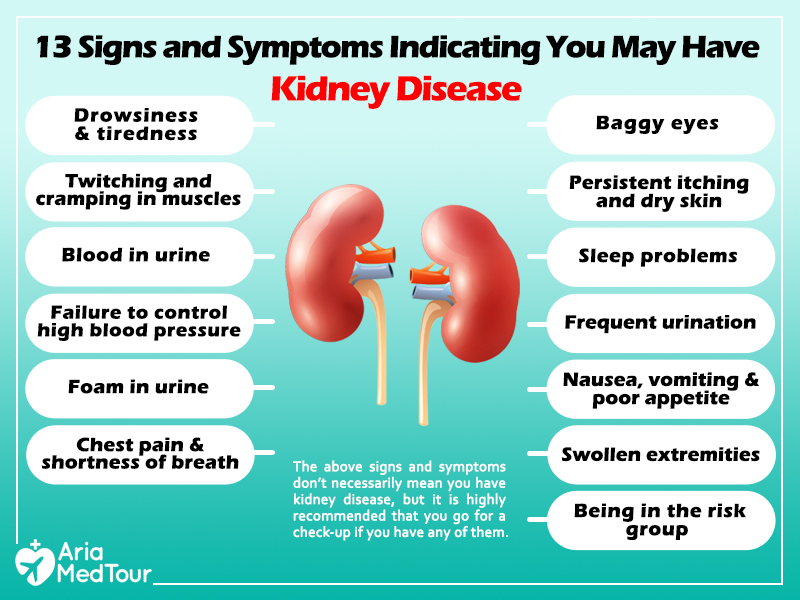
If you are diagnosed with ICP, you will have regular liver blood tests (LFTs) and bile acid measurement tests so your doctor can monitor your condition.
Initially, you may be given these tests every week. You may then be given more, or less, frequent tests depending on the results and your symptoms.
Creams and medicines for ICPCreams, such as aqueous cream with menthol, are safe to use in pregnancy and can provide some relief from itching.
A medicine called ursodeoxycholic acid (UDCA) can be prescribed to try to relive itching. But recent evidence suggests it may not be effective in reducing bile acids and easing itching.
UDCA is considered safe to take in pregnancy, although it is prescribed on what is known as an "informed consent" basis as it has not been properly tested in pregnancy. It is usually only prescribed by a hospital doctor.
It is usually only prescribed by a hospital doctor.
A possible alternative, which can be helpful if itchiness is keeping you awake at night, is antihistamine medicine, such as chlorphenamine. Chlorphenamine tends to cause drowsiness so it can also help with sleep problems as well as itchiness. If you do feel drowsy do not drive or operate machinery.
You may also be offered a vitamin K supplement. This is because ICP can affect your absorption of vitamin K, which is important for healthy blood clotting.
Most experts on ICP only prescribe vitamin K if the mother-to-be reports pale poo, has a known blood clotting problem, or has very severe ICP from early in pregnancy.
If you are diagnosed with ICP, your midwife and doctor will discuss your health and your options with you.
Further information
There is information about obstetric cholestasis on the Royal College of Obstetricians & Gynaecologists (RCOG) website, including what it means for you and your baby, and the treatment that's available.
You can also get information about intrahepatic cholestasis of pregnancy (ICP) on the British Liver Trust website.
The charity ICP Support provides information about ICP. You can also watch a video about living with intrahepatic cholestasis of pregnancy (ICP) on the ICP support website featuring mums and clinical experts.
Community content from HealthUnlockedPregnancy hepatosis / Blog / Clinic EXPERT
Marchenko Natalya Valerievna
59.9 thousand views
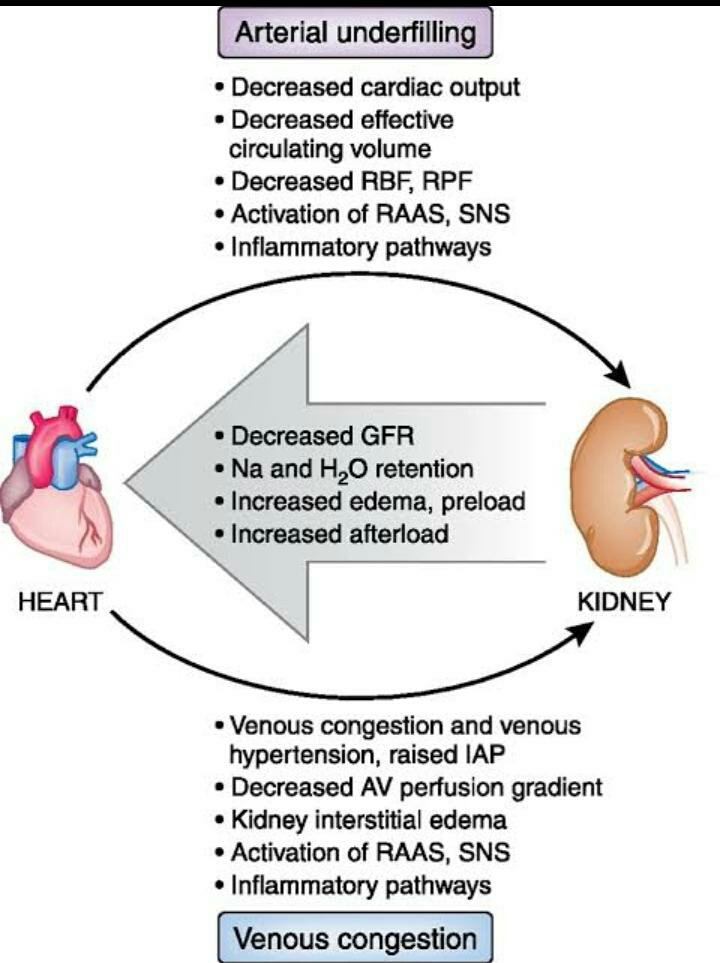
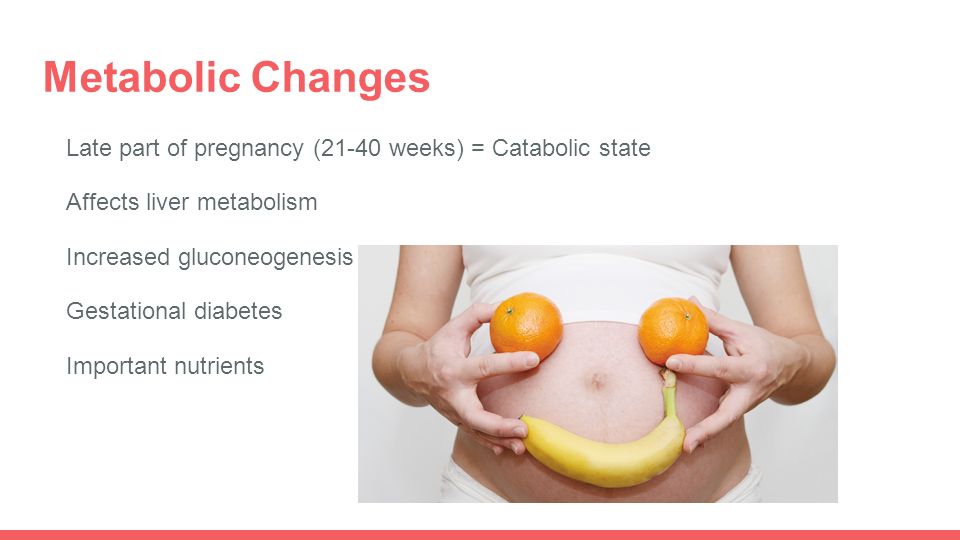
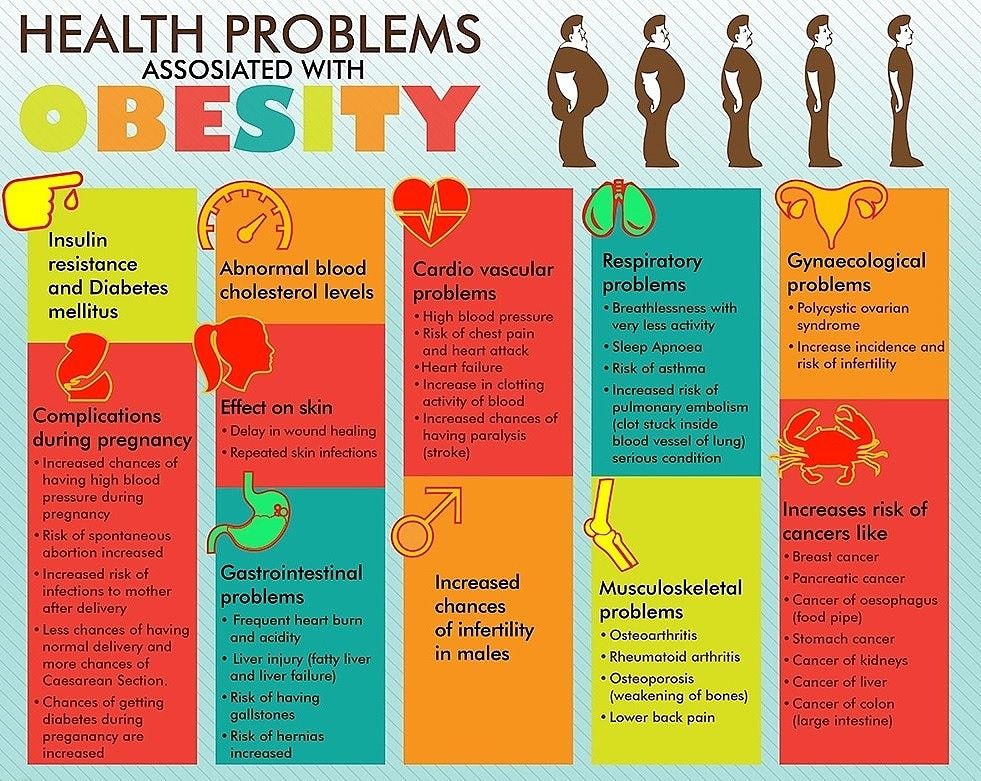
During pregnancy, the liver works for two due to the hormonal changes in the body and the development and functioning of the new one. Not every liver can stand it. In some cases, a previously healthy liver or with an already existing pathology, in 2% of women, pregnancy becomes a “triggering” factor when the process can get out of control.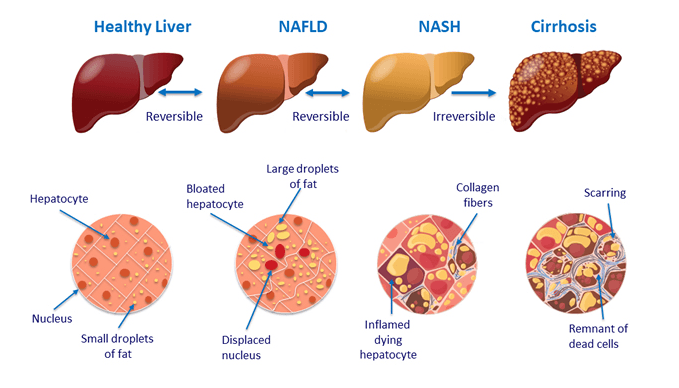
One of the most common manifestations of liver disorders during pregnancy is cholestatic hepatosis of pregnant women, which is characterized by a violation of the formation and outflow of bile. Some time after childbirth, this condition disappears. What happens in the liver during pregnancy?0003
- pruritus, mainly at night,
- disturbance of digestion processes, so less of them enter the intestines,
- toxic effect on liver cells (hepatocytes) and bile ducts, which leads to inflammation of the liver tissue.
5 key questions about hepatosis in pregnancy
№1. After the first appearance of hepatosis, can it recur in subsequent pregnancies?
Most often this condition develops in the third trimester - at 31-33 weeks. Early onset of symptoms is a poor prognostic factor. Unfortunately, the disease is prone to recurrence in subsequent pregnancies with a high risk of a more severe course. Therefore, the presence of hepatosis in pregnant women once is regarded as the need for early registration in subsequent pregnancies with regular and close monitoring of liver function under the supervision of not only a gynecologist, but also a hepatologist.
#2. Is the condition really hepatosis?
The final diagnosis is made only by a hepatologist, based on these complaints, anamnesis of the pregnant woman and a comprehensive examination. Of course, it is necessary to apply all the necessary methods of differential diagnosis to exclude other causes of liver pathology - viral and autoimmune hepatitis, acute fatty hepatosis and exacerbation of hereditary forms of liver damage.
What are the characteristic symptoms of cholestatic hepatosis of pregnancy?
- Itching of the skin of varying intensity, up to debilitating, worse at night. This is because bile pigments enter the bloodstream, irritating skin receptors.
- 10-20% develop jaundice, which develops due to an increase in direct bilirubin in the blood. More often itching occurs a few weeks before jaundice.
- Nausea and decreased appetite as signs of intoxication.
- Light stool is a characteristic symptom of jaundice, which appears due to a lack of bile in the intestines.
- Dark urine (dark beer color) - the body removes excess bile pigments through the kidneys, and they give the urine a dark color.
- Changes in blood tests are characterized by an increase in specific markers of cholestasis - alkaline phosphatase and gammaglutamyl transpeptidase. Increases total and direct bilirubin, total cholesterol, activity of AlAT, AsAT. Blood proteins are usually within normal limits. Urobilinogen is detected in urine.
Take care of yourself and see your doctor immediately if you experience these symptoms. A condition identified and corrected in time will not harm the child.
#3. Which specialist should be contacted?
There is a certain examination algorithm. In the case of an existing liver disease before pregnancy or the first appearance of these symptoms during pregnancy, a woman needs to be examined by several specialists:
- hepatologist - this specialist in liver diseases, who evaluates the need for a comprehensive examination and excludes other causes of liver pathology.
- endocrinologist - to exclude diabetes in pregnancy, as the root cause of itching.
- dermatologist - to rule out primary skin diseases.
All our specialists are experts in their field, adhere to the recommendations of reputable international associations for the study of the liver and domestic standards and clinical guidelines for the diagnosis and management of liver pathology in pregnant women.
#4. What tests are required and why?
| General:
| Biochemistry:
| Markers of viral and autoimmune hepatitis | Ultrasound of the abdominal organs |
This is the minimum required examination to rule out liver pathology during pregnancy. We understand that the list of analyzes is quite large. However, it is necessary to conduct a complete laboratory study in order to make an accurate diagnosis as quickly as possible so that neither the child nor the woman carrying him is harmed. After the examination, if indicated, the hepatologist may prescribe more specific tests and treatment.
We understand that the list of analyzes is quite large. However, it is necessary to conduct a complete laboratory study in order to make an accurate diagnosis as quickly as possible so that neither the child nor the woman carrying him is harmed. After the examination, if indicated, the hepatologist may prescribe more specific tests and treatment.
#5. What else might be needed?
We prescribe an informative and safe study - ultrasound with liver elastography using an expert-level device, to assess structural changes - liver enlargement, the presence of fatty infiltration, assess the condition of the gallbladder, and also identify the presence and stage of liver fibrosis. Today it is one of the most accurate diagnostic methods.
What threatens the development of cholestasis in pregnancy?
| Forecast for Mother | FORMENT FROM |
| Premature birth , even with multiple recurrence, it does not lead to the formation |
How is hepatosis of pregnant women treated?
Hepatosis is treatable and risks to the fetus can be reduced if therapy is started on time. Treatment is carried out in a hospital if there are indications, or on an outpatient basis with a mild course and no signs of fetal disorders.
Treatment is carried out in a hospital if there are indications, or on an outpatient basis with a mild course and no signs of fetal disorders.
Treatment goes in three directions:
- Elimination of clinical manifestations.
- Elimination of the threat of abortion.
- Improvement of uteroplacental blood flow.
Medicines used in treatment - hepatoprotectors, sorbents, antioxidants and other means. The choice of drugs depends on the symptoms, the results of the examination, the condition of the fetus and other factors. We take into account all the nuances.
What is the management of labor?
In severe cases, increased itching, jaundice, deterioration of blood counts and fetal disorders, early delivery (up to 37 weeks) is indicated.
If cholestasis of pregnancy is treatable, which is characterized by the disappearance of itching, improved sleep, blood counts, no signs of fetal distress and liver dysfunction, then delivery is indicated at 38 weeks, possibly through the natural birth canal.
Management tactics in the postpartum period
- Compliance with the diet - the exclusion of fatty, fried, spicy foods, of course, alcohol.
- Early use of combined oral contraceptives is strictly contraindicated. You need to choose another method of contraception.
- Control examination 1–2 weeks after delivery: alkaline phosphatase, GGTP, total and direct bilirubin, ALT, AST, cholesterol, followed by consultation and observation by a hepatologist.
- Ultrasound of the abdominal organs in the first year - 1 time in 6 months and then - annually, unless the attending physician prescribes a different control scheme.
- The use of hepatotoxic drugs (contraceptives, antibiotics, non-steroidal anti-inflammatory drugs, etc.) - strictly according to indications. If there is a vital need to take them, take hepatoprotectors prescribed by the attending hepatologist.
- In subsequent pregnancies, contact a hepatologist from an early date and monitor liver function with his help.
Pregnancy hepatosis - symptoms, treatment and advice from the best hepatologists in Russia
You're here for a reason, right? You don’t know where the symptoms came from, or there are changes in the tests, you are afraid of how this will affect the child. We understand your concern. Therefore, we are ready to help you find out the cause of your condition. And suggest what to do next.
Programs for checking the liver during pregnancy from hepatologists of the gastro-hepatocenter EXPERTMore
What is the essence of benign cholestatic hepatosis of pregnant women?
During pregnancy, the liver experiences double load due to hormonal changes in the body. If before pregnancy there were already changes in the liver, in 2% of women it becomes a “triggering” factor when the process can get out of control.
One of the manifestations of disorders of the liver during pregnancy - cholestatic hepatosis of pregnant women - a condition with a violation of the formation and outflow of bile.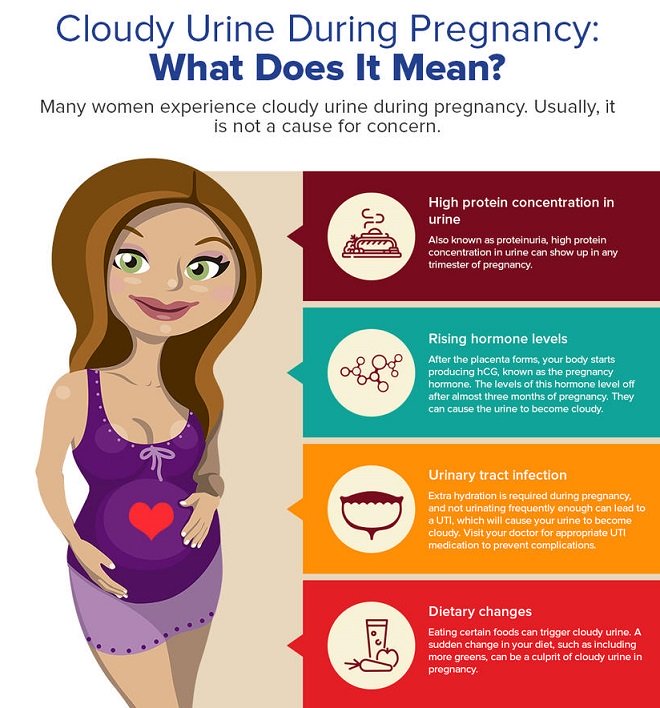 Some time after birth, it goes away.
Some time after birth, it goes away.
What happens in the liver
The exchange of cholesterol and bile acids is disturbed in the liver cells, the production and outflow of bile through the intrahepatic bile ducts is reduced.
And, as a result, bile acids:
- provoke skin itching,
- enter the intestines less, disrupting the digestion process,
- toxic effect on liver cells and bile ducts, causing inflammation in the liver tissue.
5 important questions about hepatosis in pregnancy
№1. When does it appear and can it happen again in the next pregnancy?
Most often this is the third trimester - 31-33 weeks. The earlier symptoms appear, the more serious the situation . The disease is prone to recurrence in subsequent pregnancies. Therefore, if at least once hepatosis has already been, it is necessary to take tests from an early date and monitor the performance of the liver under the supervision of a hepatologist.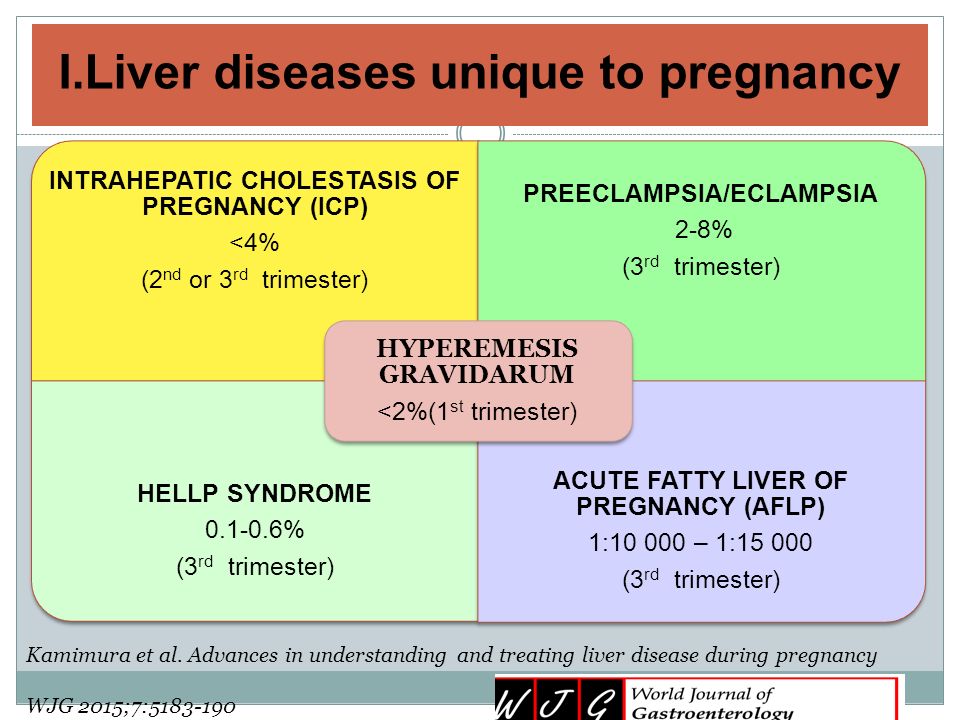
#2. Is this really hepatitis?
The final diagnosis is made by a doctor based on the data of a comprehensive examination and only after excluding other causes - viral hepatitis, autoimmune hepatitis, acute fatty hepatosis and other pathologies.
The following signs indicate cholestatic hepatosis:
- Excruciating itching of the skin, which can intensify at night - appears because bile pigments enter the bloodstream and irritate skin receptors. Itching can be of varying intensity. From mild to so strong that many scratch the skin until it bleeds.
- 10-20% jaundice . Appears due to an increase in direct bilirubin in the blood. Itching occurs a few weeks before jaundice.
- Nausea and loss of appetite.
- Light stool - a symptom appears due to a lack of bile in the intestines.
- Dark urine - the body excretes excess bile pigments through the kidneys, and they give the urine a dark color.

- Changes in blood tests : increased specific markers of cholestasis - alkaline phosphatase and GGTP. Bilirubin, ALT, AST, cholesterol may increase. Blood proteins are usually within normal limits. Urobilinogen is detected in urine.
Take care of yourself and don't panic. A condition identified and corrected in time will not harm the child.
#3. Who to contact?
There is a certain examination algorithm. If you had changes in the liver before pregnancy or have the symptoms described above, then you need an examination:
- hepatologist - this specialist evaluates the need for a comprehensive examination and excludes other causes of liver disease.
- endocrinologist - to exclude diabetes in pregnancy, as a cause of itching.
- dermatologist - to rule out skin diseases as the cause of itching.
All our specialists are experts in their field, adhere to the recommendations of reputable international associations for the study of the liver and domestic standards for the diagnosis and management of pregnant women.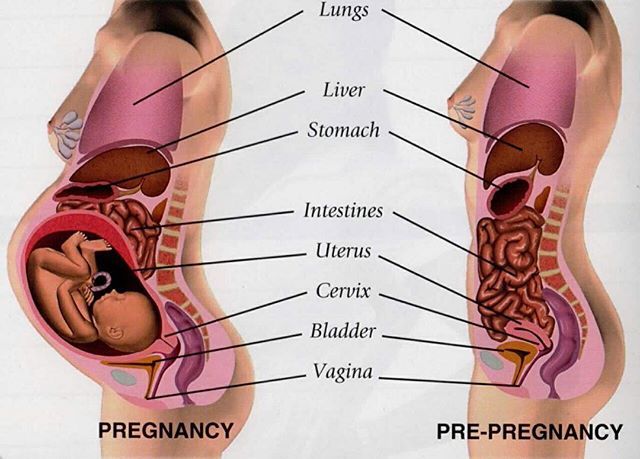
No. 4. What tests should be taken and why?
| General:
|
 times with recurrent cholestasis
times with recurrent cholestasis