Sinus congestion pregnant
Relief for Ongoing Nasal Congestion Is Possible
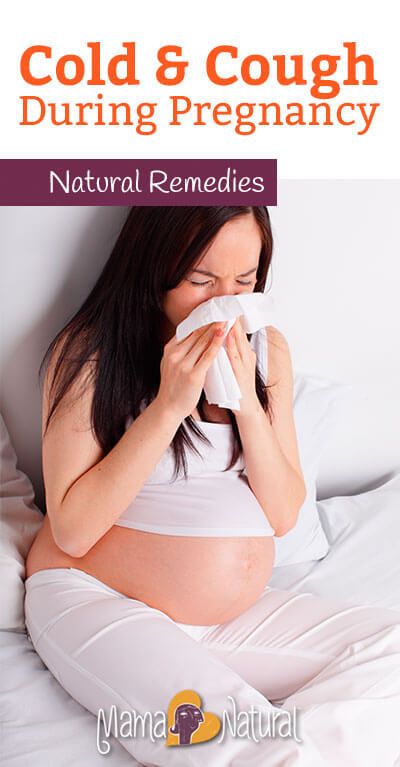
If you're expecting a baby, you may be dealing with a stuffy nose that doesn’t seem to go away. This hassle is called pregnancy rhinitis. The cause of this condition isn’t really clear. However, it may be caused by hormonal changes.Having a history of allergies or asthma does not raise your risk of getting pregnancy rhinitis.
More than just a stuffy nose
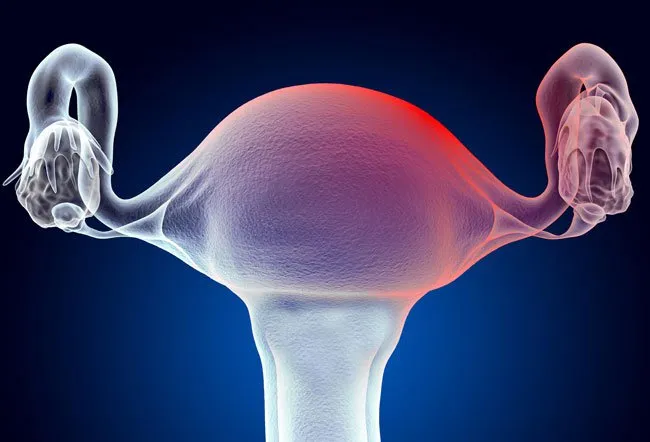
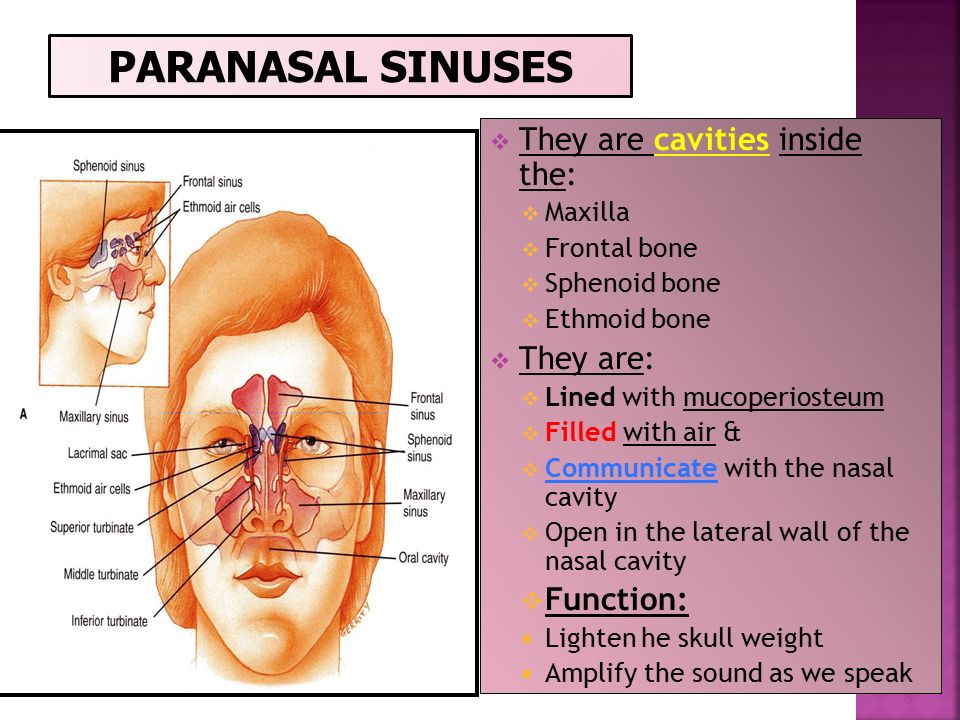
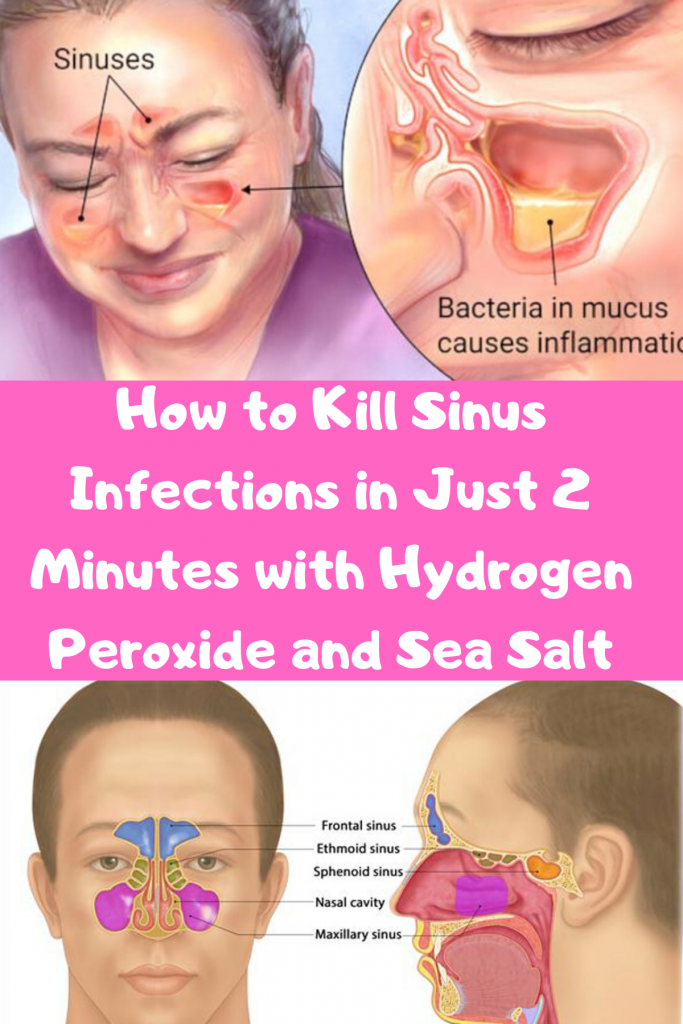
Pregnancy rhinitis is an inflammation of the mucous membranes lining the nose. This causes nasal congestion. Increased blood flow to the nasal passages and enlargement of the nasal veins also play a role.
Symptoms occur during pregnancy. They can last for several weeks. On top of feeling uncomfortable, your sleep may be disrupted. This is because the congestion gets worse when you lie down. This may make you to feel more tired during the day. Long-lasting congestion also can lead to complications. These can include sinusitis and ear infections.
Be cautious when seeking treatment
Many women use non-prescription, over-the-counter (OTC) decongestant sprays to open up their nasal passages. Know that these medicines don’t work for pregnancy rhinitis. These medicines may give you temporary relief. However, they may actually make your symptoms worse and lead to a complete nasal blockage.
How can you get relief from pregnancy rhinitis? Experts say you can breathe easy with these measures:
-
Don’t use OTC nasal decongestants.
-
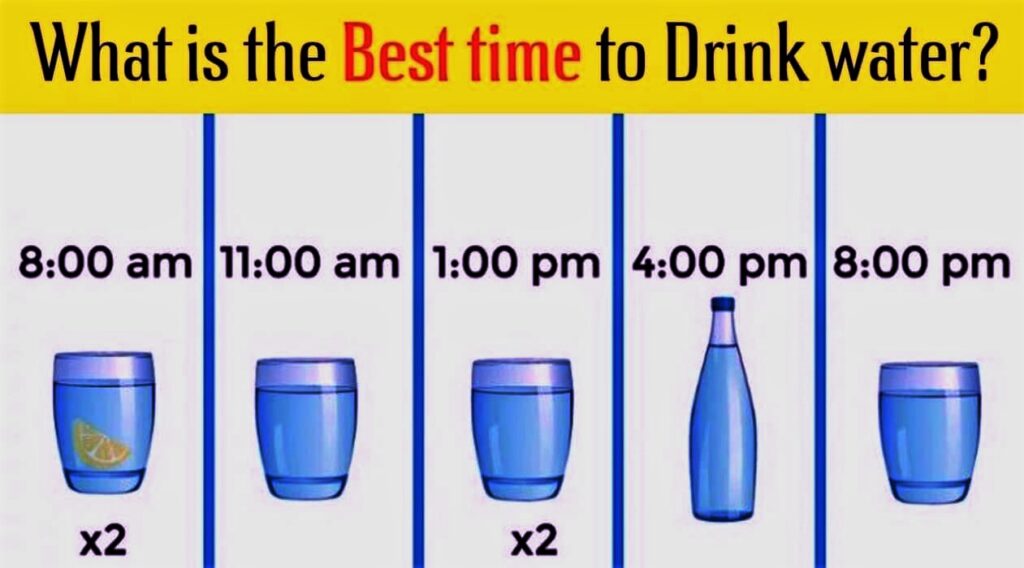
Drink plenty of fluids.
-
Increase the humidity levels in your home. Use a humidifier.
-
Don’t use nasal irritants, such as cigarette smoke.
-
Get moving. Regular, moderate-intensity exercise can reduce congestion. It can also help you sleep better. But first, check with your healthcare provider to see what exercises are safe for you.
-
When you go to sleep, raise the head of your bed. For instance, use an extra pillow or a wedge.
-
Ask your healthcare provider about using OTC nasal strips and saline sprays or drops.
The good news? Even if you don’t do anything, you can expect your stuffy nose to clear up soon after your baby is born. It often goes away within two weeks of childbirth.
Online Medical Reviewer: Bowers, Nancy, RN, BSN, MPH Foley, Maryann, RN, BSN
Date Last Reviewed: 4/12/2016
© 2000-2019 The StayWell Company, LLC. 800 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
© 2000-2019 The StayWell Company, LLC. 800 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Baby (and tissues!) on board: Tips for managing pregnancy rhinitis | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
October 6, 2020
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
D. Obstetrics and Gynecology
When you think of side effects or symptoms brought on by pregnancy, nasal congestion and runny nose are not typically among the first to come to mind.
But maybe they should. Having a stuffy nose, difficulty breathing or sleeping, and snoring when pregnant can be alarming, especially amid the COVID-19 pandemic and the start of flu season.
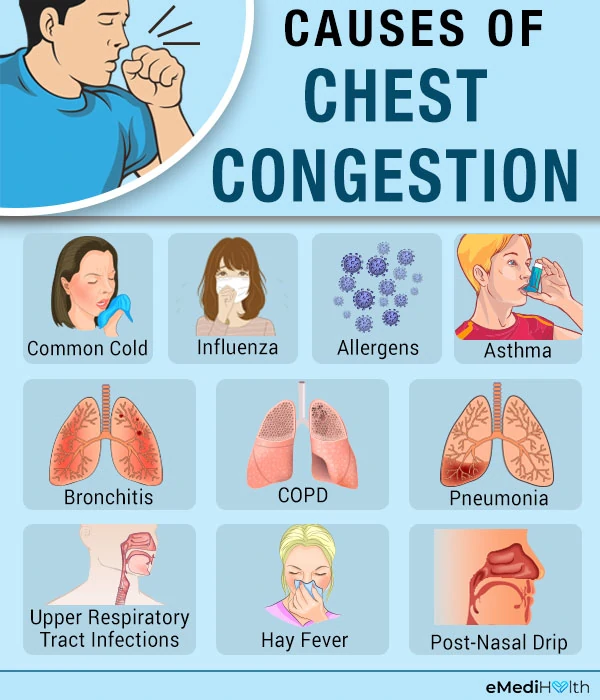
Pregnancy rhinitis, also called gestational rhinitis, is a common ailment in the second and third trimesters, affecting approximately 20% of women. Characterized by inflammation and swelling of the mucous membranes in the nose, pregnancy rhinitis symptoms include congestion (nasal obstruction), sneezing, postnasal drip, and runny nose. These symptoms can also lead to poor sleep when your growing belly might already be making it difficult to rest.
These symptoms can also lead to poor sleep when your growing belly might already be making it difficult to rest.
All these issues can dramatically affect your mood and quality of life. The good news is that, for most patients, pregnancy rhinitis is temporary and there are safe, effective treatments available.
I've invited my colleague, Ashleigh Halderman, M.D., an ear, nose, and throat specialist at UT Southwestern to explain in more detail the causes of pregnancy rhinitis and how patients can manage their symptoms.
What causes pregnancy rhinitis?
Dr. Ashleigh HaldermanThe root cause of rhinitis can be allergic (affected by environmental irritants) or non-allergic (caused by infection). However, we are still learning how rhinitis is related to pregnancy.
We know that smoking, as well as having chronic rhinitis before pregnancy, predisposes patients to developing pregnancy rhinitis. Research suggests a few more potential causes:
Research suggests a few more potential causes:
- Having extra fluid in the body: During pregnancy, the body makes more blood and fluids, which can cause swelling, even in unexpected places such as the nasal passages. Blood vessels in the nose can swell with this additional volume, causing stuffiness.
- Higher levels of estrogen: Estrogen in older formulations of birth control pills has been associated with a side effect of nasal obstruction. However, in studies of the menstrual cycle, we don't see congestion with fluctuating estrogen levels. So, the connection remains unclear for now.
- Creation of human growth hormone: The placenta creates a variant of the human growth hormone (HGH), which has been associated with nasal symptoms in other conditions. For example, tumors that grow on the pituitary glands secrete growth hormones, which can cause severe nasal congestion.
Gestational rhinitis is under-researched. Data to date suggest no known association of rhinitis with pre-existing asthma, maternal age, duration of pregnancy, or the number of times a patient has been pregnant. However, a recent study found that patients carrying female babies were diagnosed significantly more often than patients carrying male babies.
However, a recent study found that patients carrying female babies were diagnosed significantly more often than patients carrying male babies.
Related reading: How to manage allergies and asthma during pregnancy
How long do symptoms last?
The annoying, uncomfortable symptoms of pregnancy rhinitis typically last six weeks or longer. For most patients, symptoms typically resolve two weeks after delivery.
Approximately a third of patients who had chronic rhinitis before pregnancy will have the same level of symptoms during, and a third will experience worsening of rhinitis symptoms. However, the remaining third will have less severe or no symptoms during pregnancy. I've had many women tell me they've felt the best, sinus-wise, when they were pregnant. However, there's no specific reason why this occurs.
Related reading: 5 weird pregnancy symptoms you might not know about
What treatments are available?
The first step toward relief is a visit with your doctor to rule out infection, such as COVID-19, influenza, or sinusitis. We may also recommend testing for concerns such as sinusitis or pregnancy tumor (pyogenic granuloma) – a non-cancerous growth of blood vessels that may appear during pregnancy.
We may also recommend testing for concerns such as sinusitis or pregnancy tumor (pyogenic granuloma) – a non-cancerous growth of blood vessels that may appear during pregnancy.
From there, your doctor and Ob/Gyn may suggest:
- Getting regular exercise: Working out has been shown to significantly help relieve nasal congestion and regulate the sleep cycle. All the more reason to bust a move during pregnancy!
- Elevating your mattress: Try positioning the mattress so your whole body is situated at a 45-degree angle. While not widely studied, patients have reported that this helps clear the nasal passages enough to sleep.
- Using a humidifier: Adding a little moisture to the air can help alleviate nasal irritation. Many patients use them at night to wake up feeling less stuffy.
- Trying a sinus wash: Nasal saline sprays or sinus irrigation systems such as a neti pot can help clear the sinuses. Make sure to use distilled or boiled (and cooled) water – using water straight from the tap is not recommended.

Topical decongestants such as Afrin can be incredibly and immediately effective, but there is a risk of dependency. If you use this type of treatment more than once or twice a week, your nose can become "addicted" to it, which can lead to rhinitis medicamentosa – the spray will stop working as well, and your symptoms may get worse. Also, unlike gestational rhinitis, rhinitis medicamentosa won’t resolve after you deliver. It will only resolve when you stop using topical decongestants.
In general, pregnant patients can take decongestants that include pseudoephedrine as directed. However, we always recommend talking with your Ob/Gyn first, especially if you have high blood pressure.
Your Ob/Gyn might also recommend a steroid nasal spray, such as Flonase or Rhinocort, for severe symptoms. If you were using a spray to manage chronic rhinitis prior to pregnancy, your Ob/Gyn might advise you to keep using it during pregnancy. It is generally considered safe to use these products while breastfeeding, under your Ob/Gyn's guidance.
Your body will change in interesting ways during pregnancy. If you have new or unusual symptoms, call your doctor. We'll help you sort out what's normal from what could be a sinus infection or respiratory illness.
To talk with a doctor about nasal symptoms during pregnancy, call 214-645-8300 or request an appointment online.
More in: Your Pregnancy Matters
Pediatrics; Your Pregnancy Matters
- Anne Ambia, M.
 D.
D.
April 11, 2023
Your Pregnancy Matters
- Becky Ennis, M.D.
April 4, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
March 14, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
February 14, 2023
Your Pregnancy Matters
- Melissa Mauskar, M.D.
February 7, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
January 31, 2023
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.
 D.
D. - Kyler Elwell Silver, M.D.
January 24, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
January 10, 2023
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
December 20, 2022
More Articles
Features of the course of sinusitis in pregnant women
Nasal congestion is a common complaint during pregnancy [1, 2]. It is believed that every fifth pregnant woman suffers from some degree of nasal obstruction [3]. The most common causes of nasal congestion during pregnancy are acute respiratory viral infection (ARVI), rhinitis and sinusitis [4]. If the diagnosis of acute respiratory viral infections in pregnant women usually does not cause difficulties, then the differential diagnosis of sinusitis during pregnancy is a difficult task, since often prolonged nasal congestion is regarded by doctors as rhinitis of pregnant women. There are no laboratory criteria for diagnosing rhinitis during pregnancy, and the use of a number of diagnostic methods for diagnosing sinusitis (radiological, endoscopic, invasive) is limited during the gestation period [5, 6].
It is known that the frequency of rhinosinusitis in pregnant women is about 1.5%, which is 6 times higher than the frequency of this pathology in the general population [7]. The degree of influence of sinusitis on the course of pregnancy is currently not well understood. Although, according to some authors, sinusitis does not increase the risk of preterm birth [8], it significantly affects the condition of the pregnant woman and the fetus, since prolonged nasal congestion in pregnant women causes a violation of the emotional status, sleep disorders, daytime fatigue and can lead to such complications such as hypertension, preeclampsia, intrauterine growth retardation [9-eleven]. In addition, late diagnosis of sinusitis and the lack of adequate pathogenetic therapy can lead to the development of orbital and intracranial complications, including during gestation [12].
Treatment of pregnant women with pathology of the paranasal sinuses is a difficult task due to the narrow range of possible drug therapy and the limitation of invasive procedures. Therefore, it is relevant to study the characteristics of the course of sinusitis in pregnant women, which will make it possible to make a correct diagnosis in a timely manner and prevent the development of complications.
Therefore, it is relevant to study the characteristics of the course of sinusitis in pregnant women, which will make it possible to make a correct diagnosis in a timely manner and prevent the development of complications.
The purpose of the study was to study the features of the diagnosis and course of acute sinusitis in pregnant women.
Material and methods
From September 2014 to September 2018, 816 pregnant women consulted an otorhinolaryngologist at CDC with complaints of nasal congestion and/or discharge from the nose. Of these, 38 (4.7%) had experienced acute sinusitis during pregnancy. The study group consisted of 27 (27/38) pregnant women with sinusitis, who were under our supervision at the time of the disease. The remaining 11 (11/38) women were treated for sinusitis in other hospitals. The comparison group consisted of 778 pregnant women with allergic and vasomotor rhinitis without signs of sinusitis.
All patients underwent an anamnesis, a conventional examination of the ENT organs, and a clinical blood test.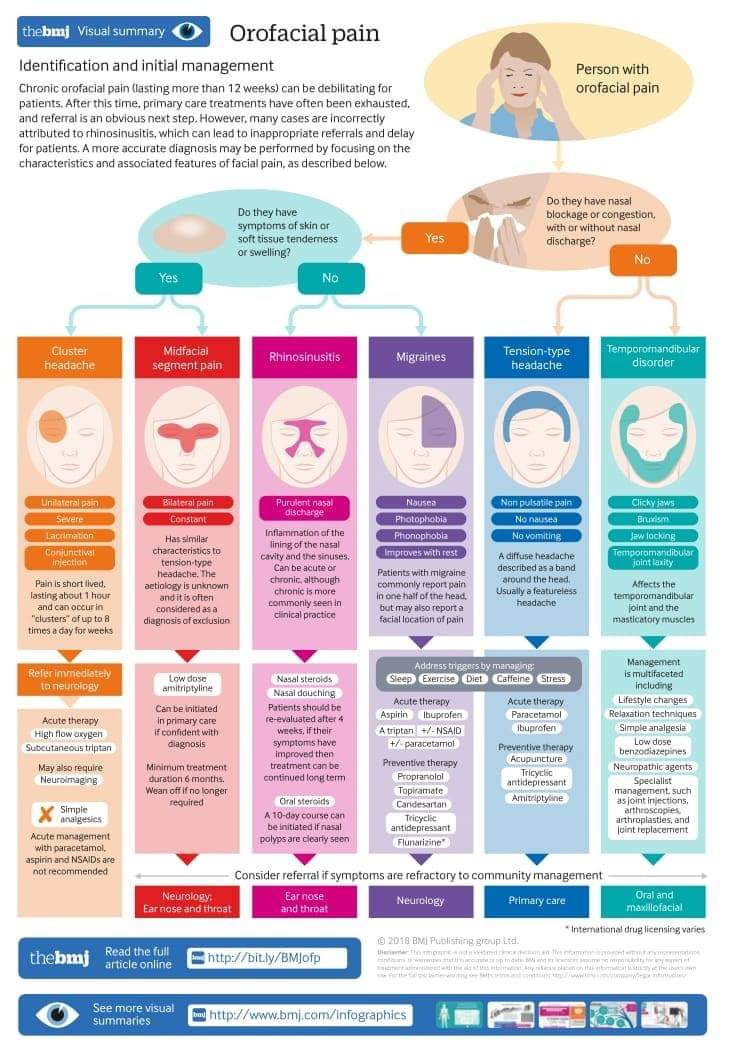 The severity of changes in the nasal cavity, changes in the palatine tonsils, posterior pharyngeal wall and laryngopharynx during the examination were assessed in points [13]. Statistical data processing was performed using the Mann–Whitney test.
The severity of changes in the nasal cavity, changes in the palatine tonsils, posterior pharyngeal wall and laryngopharynx during the examination were assessed in points [13]. Statistical data processing was performed using the Mann–Whitney test.
Results and discussion
The mean onset of sinusitis during pregnancy was 19.8±1.9 weeks of gestation. When analyzing the anamnesis, it was revealed that in the study group, the onset of sinusitis was preceded by an exacerbation of chronic rhinitis - in 30% (8/27) of cases (allergic (4%, 1/27) and vasomotor (26%, 7/27) rhinitis, acute respiratory disease in 26% (7/27) of cases.Thus, only 56% (15/27) of women had prerequisites for the development of sinusitis during pregnancy, and the acute onset of the disease was observed only in 26% (7/27) of cases. In this case, women with chronic forms of rhinitis at the time of treatment in most cases (5/8, 63%) received decongestants for 4.6 ± 2.9weeks and only in one case (1/8, 13%) - intranasal corticosteroids.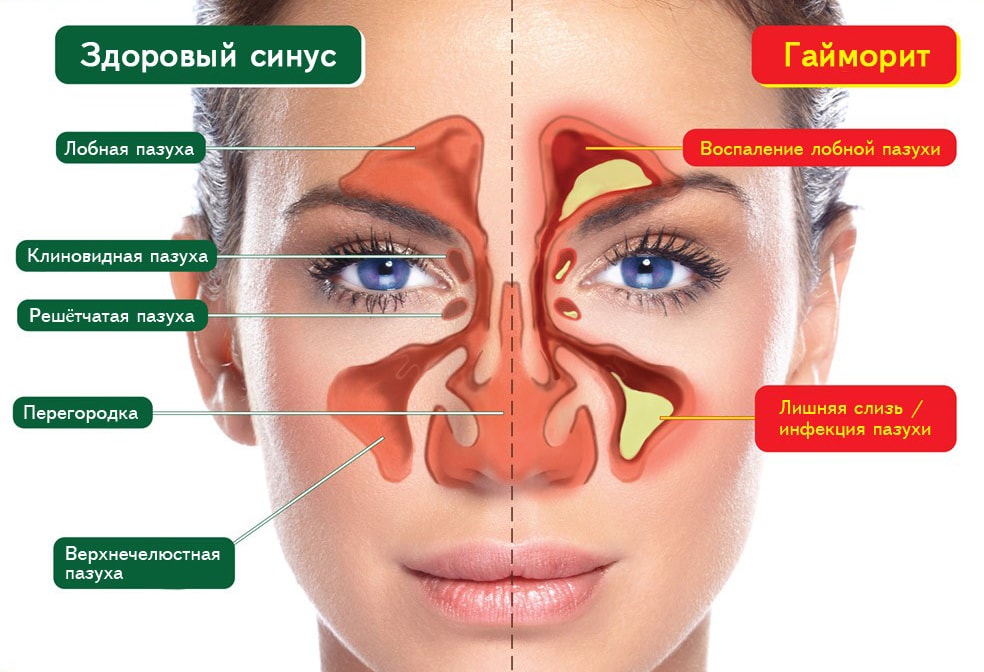
The diagnosis of sinusitis in pregnant women was made on the basis of data from the examination of the ENT organs and complaints, according to the recommendations of EPOS 2012 [14].
All pregnant women were determined to have two or more symptoms of acute sinusitis, allowing a clinical diagnosis: nasal congestion (27/27, 100%), discharge from the nasal cavity or posterior pharyngeal wall (89%, 24/27, of which 88 % (21/24) of cases - purulent), pressure or pain in the face (22%, 6/27), decreased or loss of smell (37%, 10/27). In addition, in 11% (3/27) of cases, women complained of coughing, in 11% (3/27) of cases - of weakness, in 7% (2/27) - of an increase in body temperature to subfebrile numbers. Thus, sinusitis in the study group proceeded without a pronounced intoxication syndrome and fever.
Endoscopic signs of sinusitis, as recommended by EPOS 2012, include nasal polyps, mucopurulent discharge, predominantly in the middle meatus, and edema or obstruction, predominantly in the middle meatus.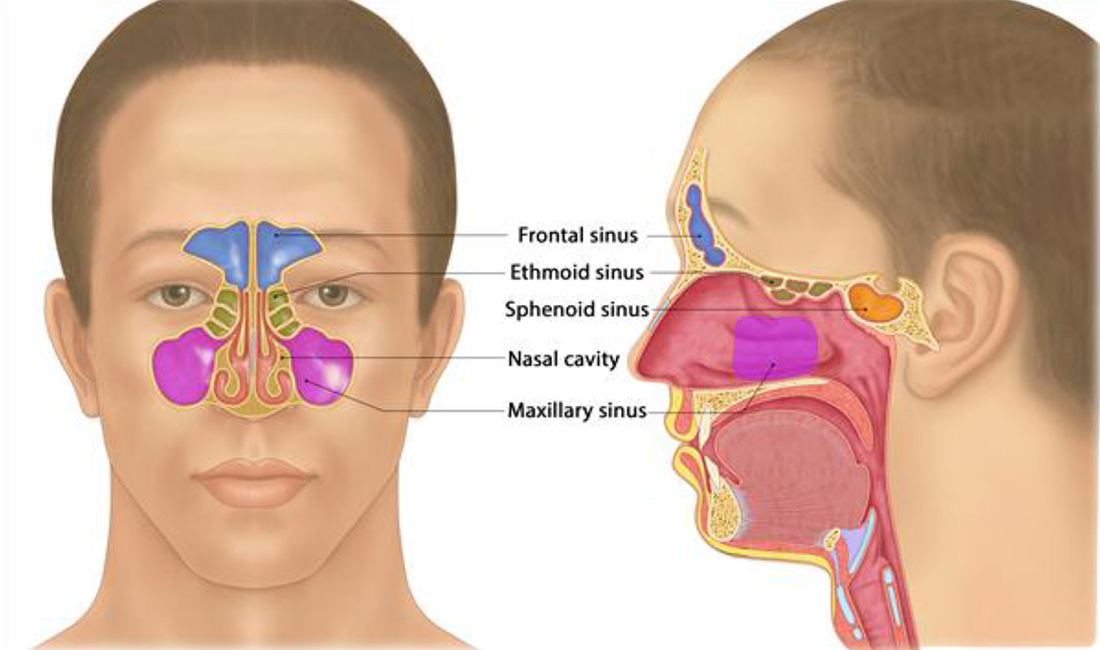 Since the use of rigid endoscopy during gestation is limited, other diagnostic methods should be considered in the diagnosis of sinusitis in pregnant women. For example, if only 22% of pregnant women complained of pressure or pain in the face, then pain on palpation and percussion of the paranasal sinuses at the time of examination was observed in half of the patients (52%, 14/27).
Since the use of rigid endoscopy during gestation is limited, other diagnostic methods should be considered in the diagnosis of sinusitis in pregnant women. For example, if only 22% of pregnant women complained of pressure or pain in the face, then pain on palpation and percussion of the paranasal sinuses at the time of examination was observed in half of the patients (52%, 14/27).
Due to radiation exposure limitations during pregnancy, radiological confirmation of sinusitis is not warranted. Of women with sinusitis, magnetic resonance imaging of the paranasal sinuses was performed in only 11% (3/27) of cases with suspected sphenoiditis, frontal sinusitis, and an odontogenic cause of sinusitis requiring special treatment tactics. Only one patient (4%, 1/27) underwent sinus ultrasound, the diagnostic value of which in detecting sinusitis, according to some authors, is low [14]. According to the results of the examination, the inflammatory process in the frontal and sphenoid sinuses was not detected in any case, the odontogenic nature of sinusitis was detected only in 1 patient, which required tooth extraction after the inflammatory process subsided in the paranasal sinuses.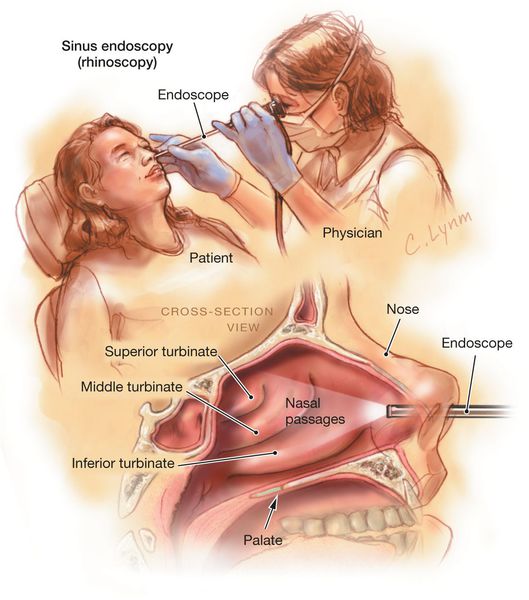
In a clinical blood test during the inflammatory process in the paranasal sinuses, the average level of leukocytes was higher in the study group compared to pregnant women with chronic rhinitis (10.9±1.3 and 8.9±0.1 10 9 /l respectively), although these differences were not significant ( p >0.05), the percentage of stab nuclei also turned out to be higher (5.5±3.5 and 3.4±0.4, respectively, p >0.05) and segmented (70.4±3.9 and 65.4±1.0, respectively, p >0.05) neutrophils. Only differences in ESR were significant: 31.5±3.5 mm/h in patients with sinusitis and 15.6±0.6 mm/h in pregnant women with chronic rhinitis ( p <0.01).
When assessing endoscopic findings in pregnant women with sinusitis, compared with the comparison group, the degree of changes in the nasal cavity was significantly higher (3.3±0.4 and 1.6±0.1 points, respectively, р <0.05) and lower the severity of changes in the palatine tonsils (1.6±0.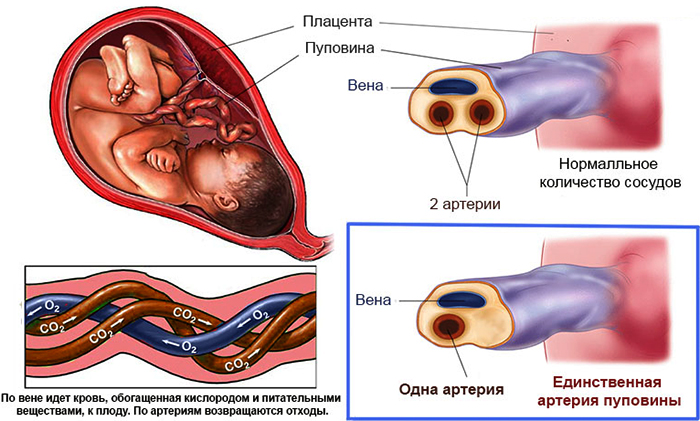 4 and 2.6±0.1 points, respectively), the posterior pharyngeal wall (1.5±0.2 and 1.9±0.04 points, respectively) and hypopharynx (3.0±0.6 and 4.4±0.1 points, respectively).
4 and 2.6±0.1 points, respectively), the posterior pharyngeal wall (1.5±0.2 and 1.9±0.04 points, respectively) and hypopharynx (3.0±0.6 and 4.4±0.1 points, respectively).
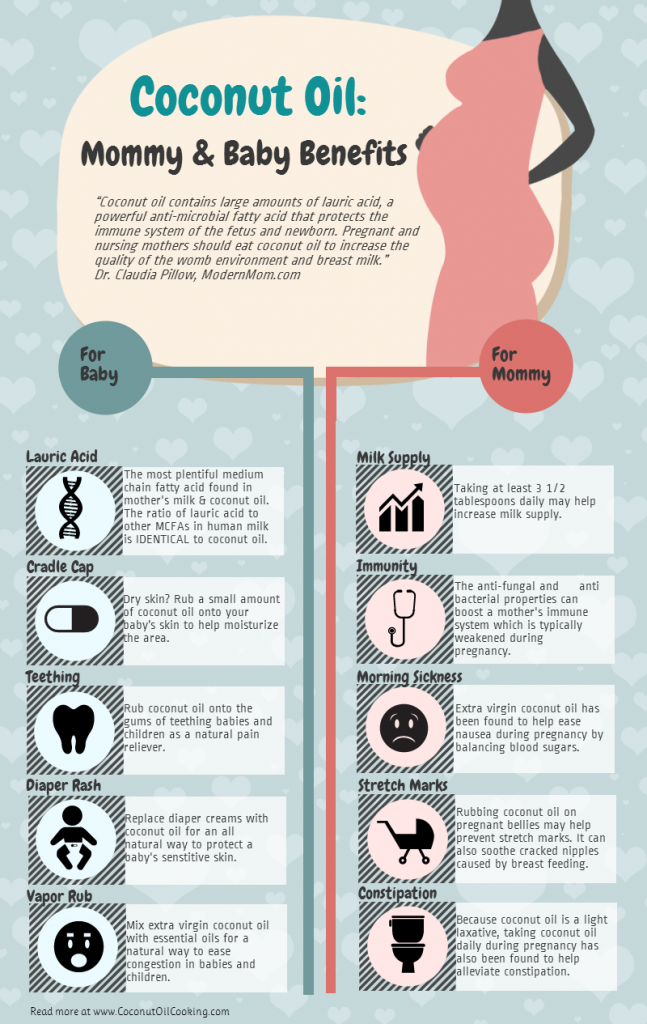
Treatment of pregnant women with sinusitis in all cases included decongestants, the use of which in pregnant women is allowed according to the instructions (tramazolina hydrochloride), saline solutions for washing the nasal cavity and antiseptic solutions for the nasal cavity, intranasal corticosteroids. According to the EPOS guidelines (2012), intranasal corticosteroids can be used as monotherapy for acute purulent sinusitis [14].
Systemic antibiotic therapy for 7 days was prescribed in only 52% (14/27) of cases in the presence of facial pain and/or fever. Preference was given to penicillins, from the II trimester - amoxicillin in combination with clavulanic acid, or macrolides. Puncture treatment was required in 22% (6/27) of cases, while the pain syndrome persisted against the background of conservative treatment for 2 days. According to the results of a microbiological study of aspirate from the maxillary sinuses, in half of the cases no growth of the flora was found, in the rest the flora was represented by opportunistic bacteria. Protracted sinusitis (lasting up to 2–3 weeks) was noted in 6 patients (22%, 6/27), mainly due to the refusal of patients to take systemic antibiotic therapy (in 4 cases), in 1 case - as a result of the prescription of physiotherapy by doctors of the outpatient department. treatment and homeopathic medicines, which caused the patient to increase nasal congestion, worsening the course of sinusitis, which required the appointment of systemic antibiotic therapy.
According to the results of a microbiological study of aspirate from the maxillary sinuses, in half of the cases no growth of the flora was found, in the rest the flora was represented by opportunistic bacteria. Protracted sinusitis (lasting up to 2–3 weeks) was noted in 6 patients (22%, 6/27), mainly due to the refusal of patients to take systemic antibiotic therapy (in 4 cases), in 1 case - as a result of the prescription of physiotherapy by doctors of the outpatient department. treatment and homeopathic medicines, which caused the patient to increase nasal congestion, worsening the course of sinusitis, which required the appointment of systemic antibiotic therapy.
Of the 27 women in the study group, in 3 (11%) cases, sinusitis was recurrent. The causes of recurrence were the odontogenic nature of the inflammation of the paranasal sinuses (1/3), the ongoing inflammation of the mucous membrane of the nasal cavity of an allergic nature (2/3).
The prevalence of sinusitis in pregnant women with complaints of nasal congestion and / or discharge from the nose, according to our study, was 4.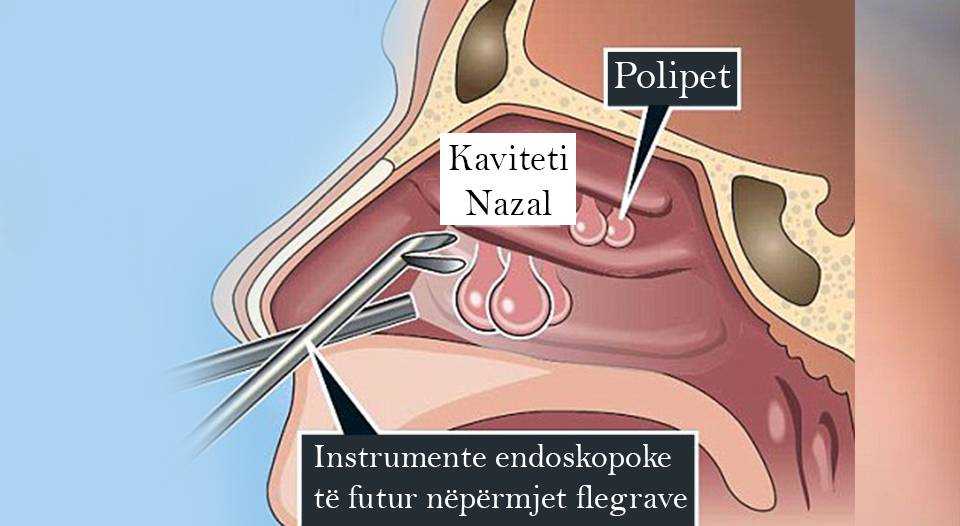 7%, an erased onset of the disease was noted in 74% of cases. The course of sinusitis in pregnant women had an erased clinical picture - without a pronounced intoxication syndrome, fever, in 78% of cases - without complaints of pressure or pain in the face, which indicates the complexity of early diagnosis of sinusitis during gestation. In a third of cases, the development of sinusitis was associated with inadequate treatment of chronic rhinitis during pregnancy. Due to the limitations of X-ray and endoscopic methods for diagnosing sinusitis in pregnant women, anamnestic and clinical data are significant: nasal congestion and the nature of nasal discharge, pain on palpation and percussion of the paranasal sinuses in half of the cases, an increase in ESR and a tendency to increase in the percentage of stab nuclei in peripheral blood. and segmented neutrophils. Prolonged or recurrent sinus inflammation has been associated with inadequate control of sinusitis during pregnancy, uncontrolled allergic reaction, odontogenic nature of the disease, or women's refusal of therapy.
7%, an erased onset of the disease was noted in 74% of cases. The course of sinusitis in pregnant women had an erased clinical picture - without a pronounced intoxication syndrome, fever, in 78% of cases - without complaints of pressure or pain in the face, which indicates the complexity of early diagnosis of sinusitis during gestation. In a third of cases, the development of sinusitis was associated with inadequate treatment of chronic rhinitis during pregnancy. Due to the limitations of X-ray and endoscopic methods for diagnosing sinusitis in pregnant women, anamnestic and clinical data are significant: nasal congestion and the nature of nasal discharge, pain on palpation and percussion of the paranasal sinuses in half of the cases, an increase in ESR and a tendency to increase in the percentage of stab nuclei in peripheral blood. and segmented neutrophils. Prolonged or recurrent sinus inflammation has been associated with inadequate control of sinusitis during pregnancy, uncontrolled allergic reaction, odontogenic nature of the disease, or women's refusal of therapy.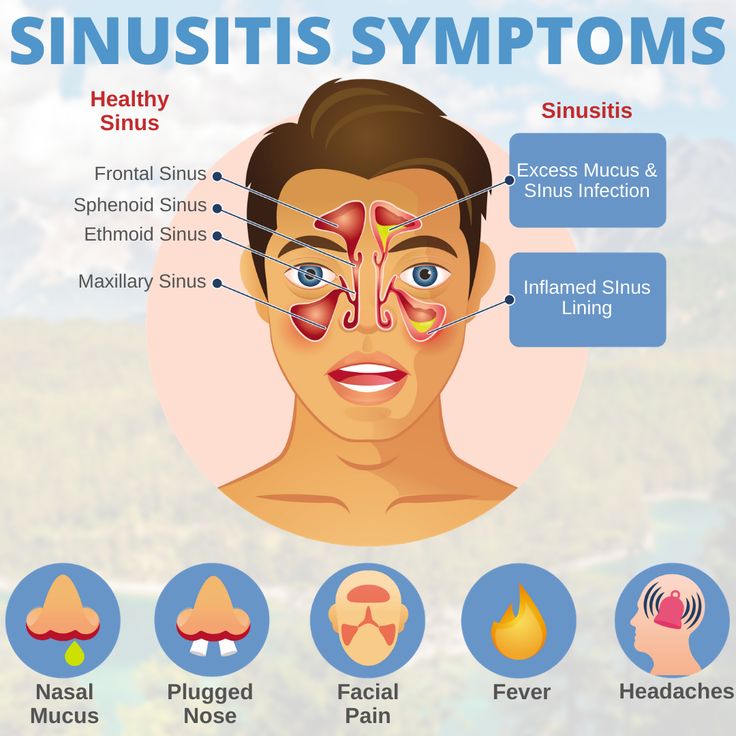
The authors declare no conflict of interest.
The authors declare no conflicts of interest.
Credits
Karpishchenko S.A. – Doctor of Medical Sciences, Prof., Head. Department of Otorhinolaryngology with the clinic of the St. Petersburg State Medical University. acad. I.P. Pavlova; St. Petersburg, 197022, st. Leo Tolstoy, d. 6-8; e-mail: [email protected]; https://orcid.org/0000-0003-1124-1937
Ryabova M.A. – MD, prof. Department of Otorhinolaryngology with the clinic of the PSPbGMU named after acad. I.P. Pavlova; St. Petersburg, 197022, st. Leo Tolstoy, d. 6-8; e-mail: [email protected]; https://orcid.org/0000-0002-6714-9454
Shumilova N.A. – Candidate of Medical Sciences, Assistant of the Department of Otorhinolaryngology with the Clinic of the St. Petersburg State Medical University. acad. I.P. Pavlova; St. Petersburg, 197022, st. Leo Tolstoy, d. 6-8; e-mail: schumilov211@yandex. ru; https://orcid.org/0000-0001-5191-9154
ru; https://orcid.org/0000-0001-5191-9154
Georgieva L.V. – full-time postgraduate student of the Department of Otorhinolaryngology with a clinic, otorhinolaryngologist at the Center for Early Diagnosis of Allergic Diseases in Women of Childbearing Age Polyclinics with CDC Clinics of the Scientific and Clinical Research Center of St. Petersburg State Medical University named after I.I. acad. I.P. Pavlova; St. Petersburg, 197022, st. Leo Tolstoy, d. 6-8; e-mail: [email protected]; https://orcid.org/0000-0002-5307-4420
Nikitin K.A. – MD, prof. Department of Otorhinolaryngology with the clinic of the PSPbGMU named after acad. I.P. Pavlova; St. Petersburg, 197022, st. Leo Tolstoy, d. 6-8; e-mail: [email protected]; https://orcid.org/0000-0001-7172-1188
How to quote:
Karpishchenko S.A., Ryabova M.A., Shumilova N.A., Georgieva L.V., Nikitin K.A. Features of the course of sinusitis in pregnant women. Journal of Otorhinolaryngology . 2019;84(3):37-40. https://doi.org/otorino201984031
Treatment of sinusitis during pregnancy
Any inflammatory processes during pregnancy can provoke various pathologies in the development of the newborn. And if you try to treat colds on your own or take antibiotics, then this will have an extremely negative impact on the health of the unborn baby. Treatment of sinusitis during pregnancy in the clinic of Dr. Sichinava allows you to quickly get rid of cold symptoms and at the same time absolutely does not harm the baby and his mother.
Sinusitis is an inflammation of the nasopharynx that affects several sinuses. Depending on the affected sinuses, the following symptoms appear in a pregnant woman:
- Sphenoid sinuses - a pregnant woman feels pain in the crown, occiput, accompanied by sinusitis;
- Frontal sinuses - paroxysmal headaches in the forehead, light hurts the eyes, eyelids swell, hyperthermia is observed;
- Ethmoid labyrinth - incessant aching headache, which is concentrated at the bridge of the nose, runny nose with purulent discharge, high fever, shortness of breath, pain in the eyes.
Sinusitis is divided into several categories according to the type of pathogen:
- Purulent;
- Viral;
- Odontogenic;
- Allergic;
- Fungal.
Sinusitis is an infectious disease that can be contracted while on the road, at a antenatal clinic, in a shop or while walking in a busy city centre. The risk of infection increases significantly with a decrease in immunity during pregnancy.
In the treatment of sinusitis according to the method of Dr. Sichinava, there is no need to take antibiotics and other potent medications that are contraindicated during pregnancy. The nasal sinuses are washed by introducing a phytodrainage spray.
Phytospray was developed by the clinic specialists and can be used both during pregnancy and for children from the age of four. When exposed to this drug on the nasopharynx, not only the sinuses are cleaned, but also the lacrimal, auditory tubes, which often remain unhealed.
The use of phytospray for sinusitis eliminates the need for such procedures as "cuckoo", YAMIK, punching. The advantages of using a phytodrainage spray over traditional sinusitis treatments are as follows:
- Swelling reduced after the first treatment;
- Accumulated mucus is quickly absorbed and excreted;
- All sinuses open;
- No complications;
- Spray acts on mucous membranes and deep tissue layers;
- Phytospray effect persists for 2 days;
- Sinusitis is completely cured after a course of 8 treatments.
Conservative treatment of ENT diseases is successfully used in infectious and viral colds such as:
- Adenoids in children;
- Treatment of sinusitis in pregnancy;
- Sinusitis;
- Sphenoiditis;
- Fronts;
- Ethmoiditis.
After a course of treatment in our clinic, the mucous membranes of the nasopharynx acquire the ability to resist various pathogenic microorganisms that cause various diseases when they enter the upper respiratory tract.