Baby projectile vomit after formula
Baby Vomiting After Feeding Formula: Causes and Treatment
Your little one is happily gulping their formula while cooing at you. They finish off the bottle in no time flat. But shortly after feeding, it seems to all come out as they vomit.
There are several reasons why your baby might be vomiting after a formula feeding, but it’s important to remember that it can be — and often is — very normal.
It’s common for babies to throw up sometimes after feeding on formula or breast milk. Their shiny new digestive systems are still learning what to do with all the yummy milk coming down into their tummy.
However, if your baby often has a hard time keeping their formula down on a regular and frequent basis, let your pediatrician know.
Having a baby around means getting used to soft mushy stuff coming out fairly often. This includes spit-up and vomit.
Spit-up and vomit might seem pretty much the same — and require similar amounts of cleaning to get them off of your sweater and the sofa — but they’re very different. Spitting up is an easy, gentle dribble of milk. Baby may even smile at you as the curd-like spit-up flows from their mouth.
Spit-up is normal in healthy babies, especially if they’re under the age of 1.
On the other hand, vomit takes more effort, as it comes from deeper in your little one’s stomach. It’s a sign that your baby’s stomach is saying nope, not now, please. You might see your baby strain and recoil just before they projectile vomit. This force happens because vomit is squeezed out by the stomach muscles.
Your baby might also look more uncomfortable during and after vomiting. And vomit looks and smells different. This is because it’s usually formula, breast milk, or food (if your baby is eating solids) mixed with stomach juices.
If you’re not sure whether your baby is vomiting or spitting up, look for other vomiting symptoms, like:
- crying
- gagging
- retching
- turning red
- arching their back
That said, there doesn’t seem to be agreed-upon definitions of these two terms among healthcare providers, caregivers, and others. Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Overfeeding
It’s easier for your baby to overfeed when they’re drinking from a bottle than when they’re breastfeeding. They can also gulp down milk faster from a bottle and rubber nipple. What’s more, because formula is always available, it’s easier for you to give them more milk than they need by accident.
Babies have tiny stomachs. A 4- to 5-week-old infant can only hold about 3 to 4 ounces in their tummy at a time. This is why they need lots of smaller feedings. Drinking too much formula (or breast milk) in one feeding can overfill your baby’s stomach, and it can only come out one way — vomit.
Not burping properly
Some babies need to be burped after every feeding because they swallow lots of air as they gulp down milk. Bottle feeding your baby breast milk or formula may lead to more air-swallowing, as they can gulp even faster.
Too much air in the stomach can make your baby uncomfortable or bloated and trigger vomiting. Burping your baby right after feeding them formula may help prevent this.
To help prevent your baby from swallowing too much air and vomiting after formula feeding, check your baby’s bottle. Make sure you’re using a smaller bottle that’s just big enough to hold a few ounces of milk. Also, check to make sure the nipple hole is not too big, and don’t let your baby continue gulping when the bottle is empty.
Baby or infant reflux
Baby can have acid reflux, indigestion, or occasionally gastroesophageal reflux disease (GERD just like grown-ups! This happens because their stomach and food tubes are still getting used to holding down milk.
Baby reflux happens when milk travels back up toward your baby’s throat and mouth. This usually just causes some painless spitting up, but it can irritate your baby’s throat and trigger gagging and vomiting.
Sometimes, smaller feedings can help prevent baby reflux. If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
Constipation
While simple constipation would be an uncommon cause of vomiting in an otherwise healthy infant, sometimes baby vomiting happens because of what isn’t happening at the other end.
Most babies who are formula-fed need to poop at least once a day. Anything less than your baby’s typical pattern, though, might indicate they’re constipated.
If your baby is vomiting after a formula feeding, they might be constipated if they have other symptoms, including:
- gassiness
- not pooping for longer than 3–4 days
- a swollen or bloated stomach
- a firm or hard stomach
- crying bouts or irritableness
- straining very hard but not pooping or pooping only a little
- small, hard pellet-like poop
- dry, dark poop
Stomach bug
If your baby doesn’t usually vomit after having formula, they might have a stomach bug.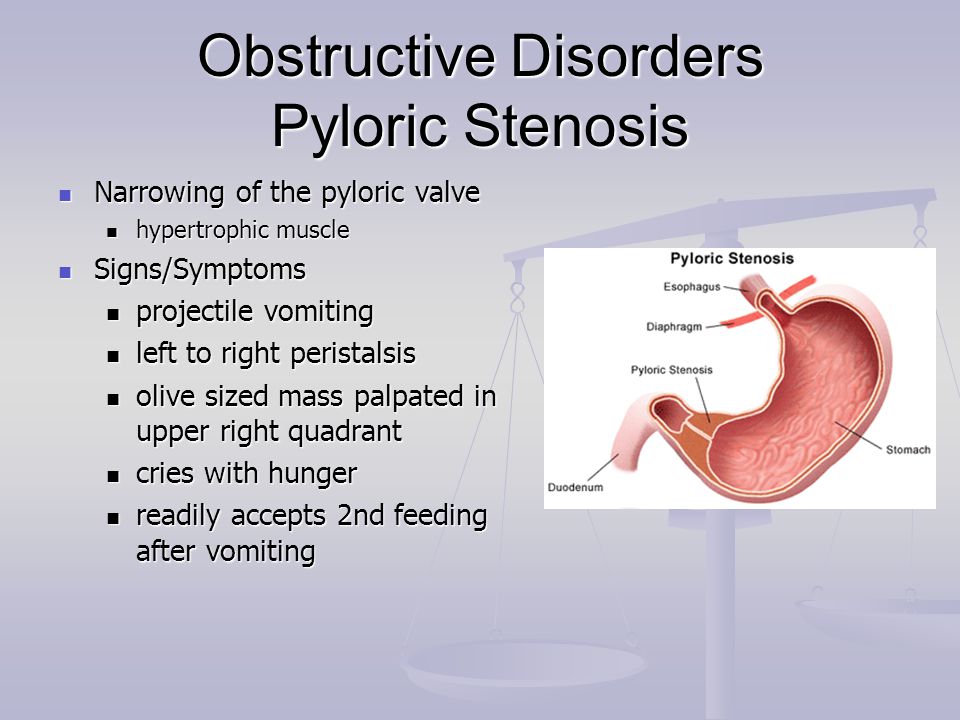 Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Other symptoms of a stomach bug include:
- crying
- stomach cramps
- stomach rumbling
- bloating
- diarrhea or watery poop
- mild fever (or none at all in babies)
Allergy
In rare cases, the cause of your baby’s vomiting might be in the formula. Although it’s uncommon for babies to be allergic to cow’s milk, it may happen to up to 7 percent of babies under the age of 1.
Most children outgrow a milk allergy by the time they’re 5 years old, but it can cause vomiting and other symptoms in babies. A cow’s milk allergy might cause vomiting right after your baby eats. It can also cause vomiting and other symptoms hours or rarely days later.
If your baby has an allergy to milk or something else, they might have other symptoms of an allergic reaction, like:
- skin rash (eczema)
- diarrhea
- cough
- hives
- difficulty breathing
- wheezing
Lactose intolerance
An allergy to milk is different than being lactose intolerant. Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Your baby might get temporary lactose intolerance after getting a tummy bug or gastroenteritis, although this is uncommon.
Other symptoms include:
- diarrhea or watery poops
- constipation
- bloating
- gassiness
- stomach pain
- stomach rumbling
Note that lactose intolerance is rare in babies under the age of 1.
Other causes
Some common health conditions can cause vomiting at any time, including after breastfeeding or formula feeding. Some rare genetic conditions can also cause vomiting in babies.
Other causes of vomiting in babies include:
- colds and the flu
- ear infections
- some medications
- overheating
- motion sickness
- galactosemia
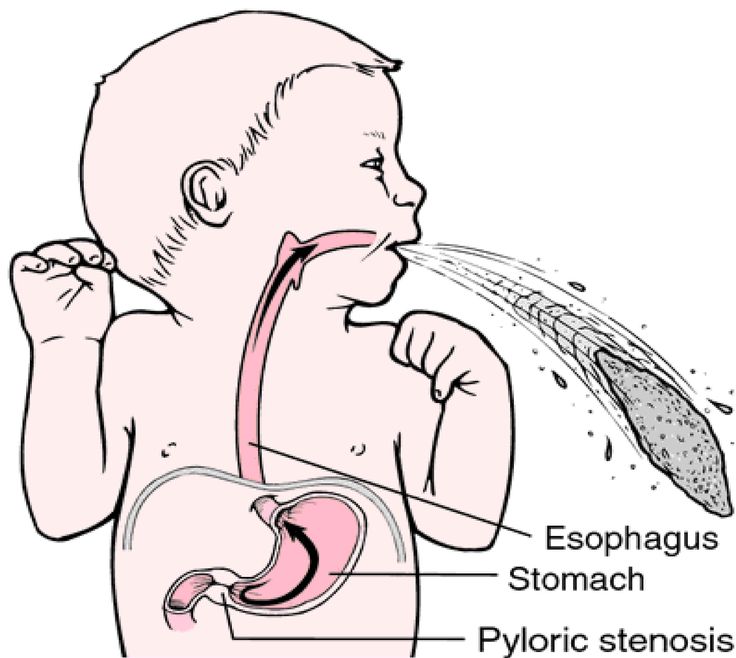
- pyloric stenosis
- intussusception
In most cases, minor tweaks can help stop your baby’s vomiting.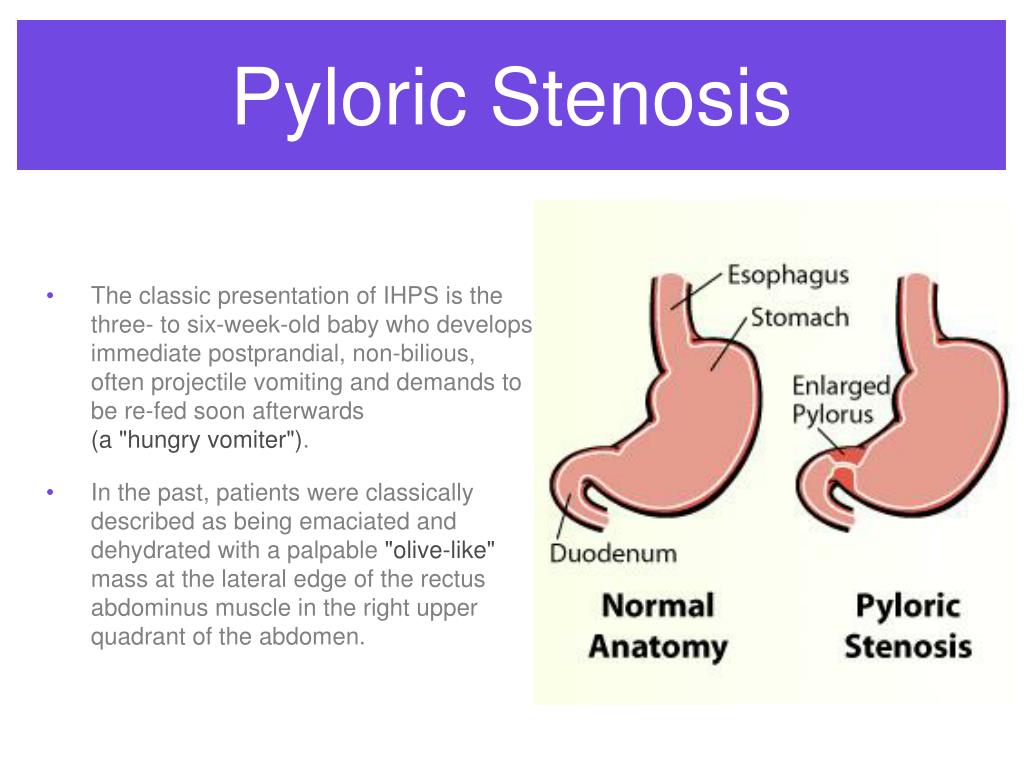 Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
- feed your baby smaller amounts of formula more often
- feed your baby slowly
- burp your baby after the feeding
- hold your baby’s head and chest up while feeding
- hold your baby upright after a feeding
- make sure your baby doesn’t move around or play too much right after a feeding
- try a smaller bottle and smaller-hole nipple to feed
- check the ingredient list on your baby’s formula
- ask your baby’s doctor if you should try a different kind of formula
- talk to your baby’s doctor about a possible allergic reaction
- dress your baby in looser clothing
- make sure their diaper isn’t on too tightly
If your baby has the stomach flu, you’ll both usually just have to ride it out for a day or two. Most babies and children with a stomach bug don’t need treatment.
If your baby is vomiting, see your doctor or pediatrician right away if they:
- are vomiting often
- are vomiting forcefully
- aren’t gaining weight
- are losing weight
- have a skin rash
- are unusually sleepy or weak
- have blood in their vomit
- have green bile in their vomit
Also, see your doctor urgently if your baby has any sign of dehydration from all the vomiting:
- dry mouth
- crying without shedding tears
- a weak or quiet cry
- floppiness when picked up
- no wet diapers for 8 to 12 hours
It’s pretty common for babies to vomit, especially after feeding. This happens for many reasons, including that these little people are still just getting used to keeping down their milk.
Check with your doctor about what you can do. See your doctor urgently if your baby vomits often for any reason.
Baby Vomiting After Feeding Formula: Causes and Treatment
Your little one is happily gulping their formula while cooing at you. They finish off the bottle in no time flat. But shortly after feeding, it seems to all come out as they vomit.
They finish off the bottle in no time flat. But shortly after feeding, it seems to all come out as they vomit.
There are several reasons why your baby might be vomiting after a formula feeding, but it’s important to remember that it can be — and often is — very normal.
It’s common for babies to throw up sometimes after feeding on formula or breast milk. Their shiny new digestive systems are still learning what to do with all the yummy milk coming down into their tummy.
However, if your baby often has a hard time keeping their formula down on a regular and frequent basis, let your pediatrician know.
Having a baby around means getting used to soft mushy stuff coming out fairly often. This includes spit-up and vomit.
Spit-up and vomit might seem pretty much the same — and require similar amounts of cleaning to get them off of your sweater and the sofa — but they’re very different. Spitting up is an easy, gentle dribble of milk. Baby may even smile at you as the curd-like spit-up flows from their mouth.
Spit-up is normal in healthy babies, especially if they’re under the age of 1.
On the other hand, vomit takes more effort, as it comes from deeper in your little one’s stomach. It’s a sign that your baby’s stomach is saying nope, not now, please. You might see your baby strain and recoil just before they projectile vomit. This force happens because vomit is squeezed out by the stomach muscles.
Your baby might also look more uncomfortable during and after vomiting. And vomit looks and smells different. This is because it’s usually formula, breast milk, or food (if your baby is eating solids) mixed with stomach juices.
If you’re not sure whether your baby is vomiting or spitting up, look for other vomiting symptoms, like:
- crying
- gagging
- retching
- turning red
- arching their back
That said, there doesn’t seem to be agreed-upon definitions of these two terms among healthcare providers, caregivers, and others. Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Plus, their symptoms may overlap. For example, spitting up may sometimes be forceful, and vomiting may sometimes seem painless.
Overfeeding
It’s easier for your baby to overfeed when they’re drinking from a bottle than when they’re breastfeeding. They can also gulp down milk faster from a bottle and rubber nipple. What’s more, because formula is always available, it’s easier for you to give them more milk than they need by accident.
Babies have tiny stomachs. A 4- to 5-week-old infant can only hold about 3 to 4 ounces in their tummy at a time. This is why they need lots of smaller feedings. Drinking too much formula (or breast milk) in one feeding can overfill your baby’s stomach, and it can only come out one way — vomit.
Not burping properly
Some babies need to be burped after every feeding because they swallow lots of air as they gulp down milk. Bottle feeding your baby breast milk or formula may lead to more air-swallowing, as they can gulp even faster.
Too much air in the stomach can make your baby uncomfortable or bloated and trigger vomiting. Burping your baby right after feeding them formula may help prevent this.
To help prevent your baby from swallowing too much air and vomiting after formula feeding, check your baby’s bottle. Make sure you’re using a smaller bottle that’s just big enough to hold a few ounces of milk. Also, check to make sure the nipple hole is not too big, and don’t let your baby continue gulping when the bottle is empty.
Baby or infant reflux
Baby can have acid reflux, indigestion, or occasionally gastroesophageal reflux disease (GERD just like grown-ups! This happens because their stomach and food tubes are still getting used to holding down milk.
Baby reflux happens when milk travels back up toward your baby’s throat and mouth. This usually just causes some painless spitting up, but it can irritate your baby’s throat and trigger gagging and vomiting.
Sometimes, smaller feedings can help prevent baby reflux. If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
If not, don’t worry! Most little ones outgrow baby reflux by the time they’re 1 year old.
Constipation
While simple constipation would be an uncommon cause of vomiting in an otherwise healthy infant, sometimes baby vomiting happens because of what isn’t happening at the other end.
Most babies who are formula-fed need to poop at least once a day. Anything less than your baby’s typical pattern, though, might indicate they’re constipated.
If your baby is vomiting after a formula feeding, they might be constipated if they have other symptoms, including:
- gassiness
- not pooping for longer than 3–4 days
- a swollen or bloated stomach
- a firm or hard stomach
- crying bouts or irritableness
- straining very hard but not pooping or pooping only a little
- small, hard pellet-like poop
- dry, dark poop
Stomach bug
If your baby doesn’t usually vomit after having formula, they might have a stomach bug. Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Also known as gastroenteritis or the “stomach flu,” a stomach bug is a very common cause of vomiting in babies. Your little one may vomit several times for up to 24 hours.
Other symptoms of a stomach bug include:
- crying
- stomach cramps
- stomach rumbling
- bloating
- diarrhea or watery poop
- mild fever (or none at all in babies)
Allergy
In rare cases, the cause of your baby’s vomiting might be in the formula. Although it’s uncommon for babies to be allergic to cow’s milk, it may happen to up to 7 percent of babies under the age of 1.
Most children outgrow a milk allergy by the time they’re 5 years old, but it can cause vomiting and other symptoms in babies. A cow’s milk allergy might cause vomiting right after your baby eats. It can also cause vomiting and other symptoms hours or rarely days later.
If your baby has an allergy to milk or something else, they might have other symptoms of an allergic reaction, like:
- skin rash (eczema)
- diarrhea
- cough
- hives
- difficulty breathing
- wheezing
Lactose intolerance
An allergy to milk is different than being lactose intolerant.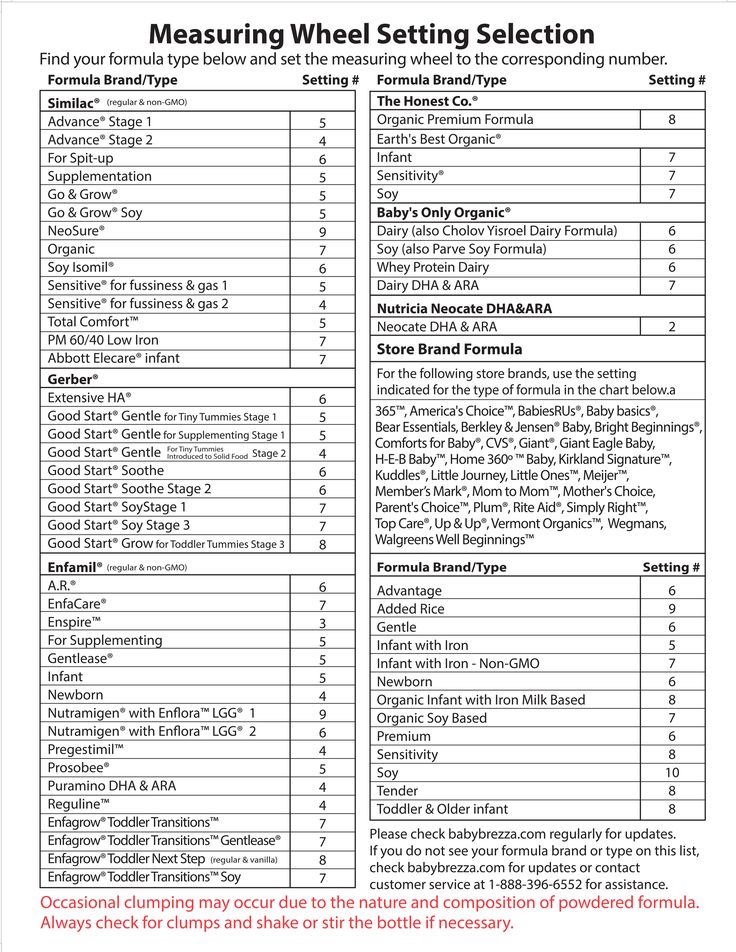 Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Lactose intolerance usually causes digestive symptoms like diarrhea. It can also make your baby vomit after drinking formula containing cow’s milk.
Your baby might get temporary lactose intolerance after getting a tummy bug or gastroenteritis, although this is uncommon.
Other symptoms include:
- diarrhea or watery poops
- constipation
- bloating
- gassiness
- stomach pain
- stomach rumbling
Note that lactose intolerance is rare in babies under the age of 1.
Other causes
Some common health conditions can cause vomiting at any time, including after breastfeeding or formula feeding. Some rare genetic conditions can also cause vomiting in babies.
Other causes of vomiting in babies include:
- colds and the flu
- ear infections
- some medications
- overheating
- motion sickness
- galactosemia
- pyloric stenosis
- intussusception
In most cases, minor tweaks can help stop your baby’s vomiting. Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
Remedies to stop your baby’s vomiting after formula depend on what’s causing it. Try some of these tried and tested methods to see what helps your baby:
- feed your baby smaller amounts of formula more often
- feed your baby slowly
- burp your baby after the feeding
- hold your baby’s head and chest up while feeding
- hold your baby upright after a feeding
- make sure your baby doesn’t move around or play too much right after a feeding
- try a smaller bottle and smaller-hole nipple to feed
- check the ingredient list on your baby’s formula
- ask your baby’s doctor if you should try a different kind of formula
- talk to your baby’s doctor about a possible allergic reaction
- dress your baby in looser clothing
- make sure their diaper isn’t on too tightly
If your baby has the stomach flu, you’ll both usually just have to ride it out for a day or two. Most babies and children with a stomach bug don’t need treatment.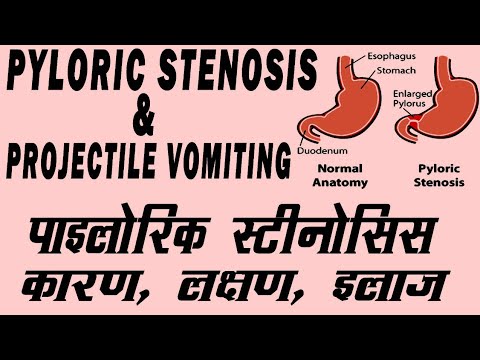
If your baby is vomiting, see your doctor or pediatrician right away if they:
- are vomiting often
- are vomiting forcefully
- aren’t gaining weight
- are losing weight
- have a skin rash
- are unusually sleepy or weak
- have blood in their vomit
- have green bile in their vomit
Also, see your doctor urgently if your baby has any sign of dehydration from all the vomiting:
- dry mouth
- crying without shedding tears
- a weak or quiet cry
- floppiness when picked up
- no wet diapers for 8 to 12 hours
It’s pretty common for babies to vomit, especially after feeding. This happens for many reasons, including that these little people are still just getting used to keeping down their milk.
Check with your doctor about what you can do. See your doctor urgently if your baby vomits often for any reason.
Spitting up and vomiting in infants
Spitting up and vomiting in babies is a common reason for visiting a doctor.
Regurgitation and vomiting is a reflex action that occurs when receptors located in various anatomical zones are irritated, incl. in the stomach, esophagus, pharynx, oral cavity. The signal is transmitted to the vomiting center, which is located in the medulla oblongata and a gag reflex occurs.
What is the difference between regurgitation and vomiting?
The difference lies in the volume and kinetics (movement) of the gastric contents expelled to the outside. When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i.e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
In children of the first year of life, this is defined by the term "fountain vomiting" .
Regurgitation is observed only in children of the first year of life and, mainly, up to 6 months. Contribute to this anatomical and physiological features of the esophagus and stomach of the baby. Their esophagus is short and wide, the angle of connection of the esophagus with the stomach is less pronounced, and its obturator function is weak. These regurgitations are physiological. They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
If regurgitation persists in a child older than 1 year, then this is a sign of a pathological process.
Vomiting, unlike regurgitation, is accompanied by vegetative symptoms - increased salivation, pallor of the skin, palpitations. This is due to the fact that next to the vomiting center there are additional centers of autonomic regulation, which are reflexively excited, and active biological substances such as serotonin, dopamine, histamine and others are released into the blood.
Regurgitation and vomiting, from the moment of eating, may occur during feeding, after feeding for the first 20-30 minutes or delayed, sometimes after several hours.
Regurgitation and vomiting that occurs immediately after feeding unchanged breast milk or formula may be due to narrowing of the esophagus. If they persist until the next feeding, and the milk / mixture is curdled, has a sour or musty smell, then this is the result of a long standing food in the stomach. The reason for this may be the low tone of the muscle layer of the stomach and, as a result, its peristalsis or narrowing of the output section due to an anomaly in the development or high tone of the sphincter of the lower stomach. With narrowing of the duodenum, bile is present in the regurgitated masses.
With narrowing of the duodenum, bile is present in the regurgitated masses.
Gastroesophageal reflux is a common cause of regurgitation in infants. It is likely that there is a complex problem here, starting with the immaturity of the gastrointestinal tract and disorders of the central nervous system. Perinatal injuries of the central nervous system accompany every second child. Their manifestations are varied. Regurgitation and vomiting can be facilitated by an increase in intracranial pressure, disorders in the segment of the cervical spine, and so on. Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
We should not forget about allergic gastrointestinal reactions in the form of regurgitation and vomiting. The most common cause of this is cow's milk protein. With intolerance to cow's milk protein, inflammation of the mucous membrane of the esophagus, stomach and intestines occurs. And, as a result of this, regurgitation and vomiting, pain and increased gas formation, diarrhea or constipation.
With intolerance to cow's milk protein, inflammation of the mucous membrane of the esophagus, stomach and intestines occurs. And, as a result of this, regurgitation and vomiting, pain and increased gas formation, diarrhea or constipation.
Rare endocrine disorders (adrenogenital syndrome) are manifested by vomiting in children from the first weeks of life. In such cases, vomiting is frequent, there may be an admixture of bile, the child loses weight due to loss of fluid and nutrients, and severe metabolic disorders develop.
Vomiting can also be caused by an intestinal infection. Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
As you can see, the causes of regurgitation and vomiting in children of the first year of life are quite diverse, but most often these are transient conditions that disappear with the growth of the child.
Prevention of regurgitation in children of the first months of life is quite simple. Don't overfeed your baby. If he cries, it does not always mean that he is hungry. Excess feeding leads to increased gas formation and colic, during which the child is worried, straining, thereby increasing the likelihood of spitting up. After feeding, hold the baby more upright so that he can burp the swallowed air. This will take 15-20 minutes. If the child is bottle-fed, do not change his formula milk without the recommendation of a pediatrician.
If the child has frequent regurgitation and vomiting, it is necessary to consult a pediatrician or gastroenterologist to diagnose the cause. To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
what to do - useful information for patients, Vitbiomed clinic blog +
Text: Irina Frolova
Vomiting in a child is a serious symptom that should not be ignored. Vomiting may be accompanied by or without additional symptoms, diarrhea, and/or high fever. In this article, we will talk about the possible causes of vomiting without fever and diarrhea and what parents need to do.
Causes of vomiting without fever and diarrhea
Viral gastroenteritis
This disease is also called intestinal or stomach flu. Usually its causative agent is a virus from the group of rotaviruses, less often - norovirus. The disease begins abruptly, with indomitable vomiting, accompanied by rumbling and pain in the abdomen. Diarrhea may also develop after 12 to 24 hours, but this is not necessary.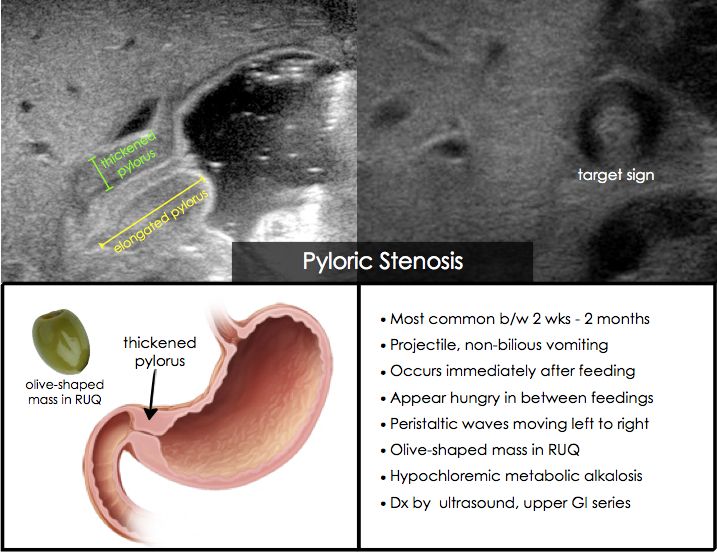 Rotavirus infection often occurs with an increase in temperature to febrile values.
Rotavirus infection often occurs with an increase in temperature to febrile values.
Food allergy
Sometimes the only reaction to a food intolerance is vomiting. In this case, vomiting occurs almost immediately after consumption of the product. The most common food allergies are nuts, fish, seafood, milk, eggs, and soy products.
Gastrointestinal disorders
Non-viral gastritis, pancreatitis, cholecystitis and biliary dyskinesia may cause vomiting. As a rule, in children they are caused by errors in nutrition, but there may be other reasons. To make a diagnosis and prescribe treatment, you need to visit a gastroenterologist.
Taking certain medications
Vomiting can be caused by not following the rules for taking certain medications, such as taking drugs on an empty stomach that irritate the stomach lining. Such drugs, in particular, include paracetamol, ibuprofen, iron preparations, theophylline.
Motion sickness
Motion sickness often causes nausea and vomiting. In this case, the child may experience pain in the abdomen, he may sweat a lot, and then vomiting begins. You can get sick not only on a trip, but even when watching movies shot with camera shake and fast-paced frames.
In this case, the child may experience pain in the abdomen, he may sweat a lot, and then vomiting begins. You can get sick not only on a trip, but even when watching movies shot with camera shake and fast-paced frames.
Cough
A severe cough can sometimes lead to vomiting, especially in children with reflux.
Migraine
About 10% of children suffer from migraine - cases of migraine have been reported in children of two years of age. A migraine attack is often accompanied by vomiting.
Stress
Vomiting can occur during a stressful situation in both children and adults.
Concussion
This is a dangerous condition that occurs after a fall and/or a blow to the head. Vomiting is often its main symptom, but headaches, visual disturbances, speech and gait disturbances may also occur. If you suspect a concussion, you should immediately call a doctor.
Appendicitis
Usually accompanied by severe abdominal pain and requires an ambulance.
Foreign body in the gastrointestinal tract
Sometimes children swallow various objects - buttons, batteries, and so on. This can lead to serious consequences, including intestinal obstruction, a sign of which is also vomiting.
How to determine the severity of vomiting
- Mild - 1-2 times a day
- Medium - 3-7 times a day
- Severe - more than 8 times a day or after any meal, water
How dangerous vomiting is
It causes dehydration, and the more severe the vomiting, the more severe the dehydration. With severe dehydration, the functions of various body systems are disrupted; in severe cases, death can occur without infusion therapy. Children become dehydrated very quickly, and at the first suspicion of dehydration, it is necessary to call a doctor.
How to tell if you are dehydrated
- The child has dark urine and has not urinated for 8 hours
- Child has dry mouth
- The child cries without tears
If these signs appear, an ambulance should be called.