How to prevent oral thrush in babies
Oral Thrush (for Parents) - Nemours KidsHealth
en español: Muguet (candidiasis oral)
Reviewed by: Michelle P. Tellado, MD
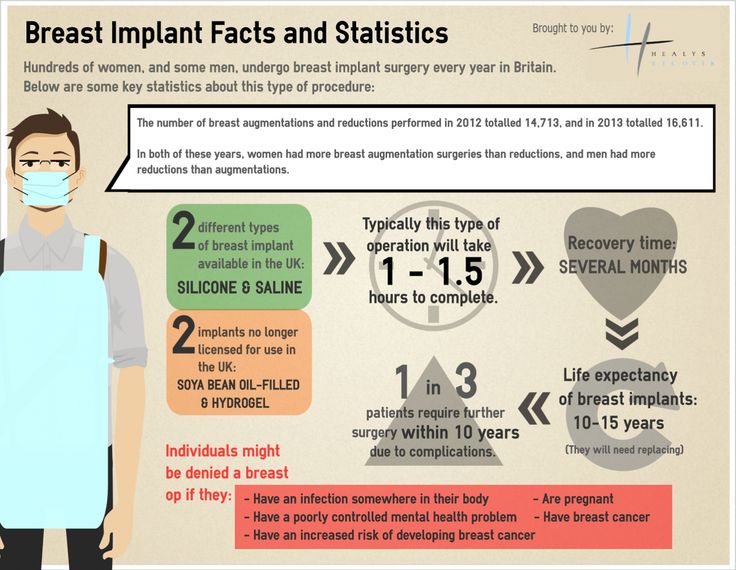
What Is Oral Thrush?
Oral thrush is a very common yeast infection in babies. It causes irritation in and around a baby's mouth.
What Are the Signs and Symptoms of Oral Thrush?
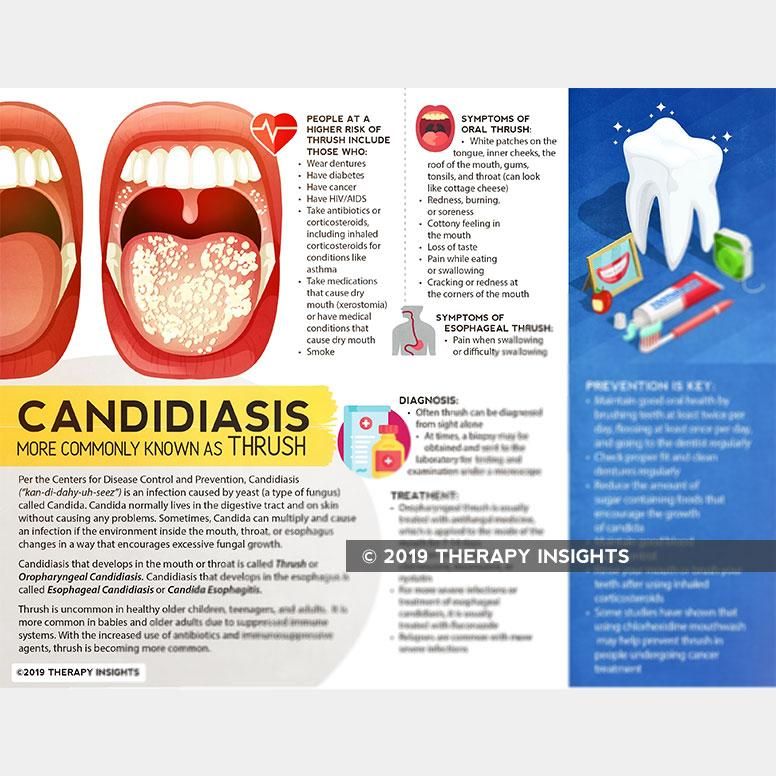
Oral thrush (also called oral candidiasis) can affect anyone, but is most common in babies younger than 6 months old and in older adults.
A baby with oral thrush might have cracked skin in the corners of the mouth or white patches on the lips, tongue, or inside the cheeks that look a little like cottage cheese but can't be wiped away.
Some babies may not feed well or are uncomfortable when sucking because their mouth feels sore, but many babies don't feel any pain or discomfort.
What Causes Oral Thrush?
Oral thrush is caused by the overgrowth of a yeast (a type of fungus) called Candida albicans.
Most people (including infants) naturally have Candida in their mouths and digestive tracts, which is considered normal growth. Usually, a healthy immune system and some "good" bacteria control the amount of this fungus in the body.
But if the immune system is weakened (from an illness or medicines like chemotherapy) or not fully developed (as in babies), Candida in the digestive tract can overgrow and lead to an infection. Candida overgrowth also causes diaper rash and vaginal yeast infections. Babies can have oral thrush and a diaper rash at the same time.
Candida overgrowth also can happen after a baby has been given antibiotics for a bacterial infection because antibiotics can kill off the "good" bacteria that keep the Candida from growing. Oral thrush also can happen after the use of steroid medicines.
How Is Oral Thrush Treated?
See your doctor if you think your baby may have thrush. Some cases go away without medical treatment within a week or two, but the doctor may prescribe an antifungal solution for your baby's mouth. This medicine is usually applied several times a day by "painting" it on the inside of the mouth and tongue with a sponge applicator.
This medicine is usually applied several times a day by "painting" it on the inside of the mouth and tongue with a sponge applicator.
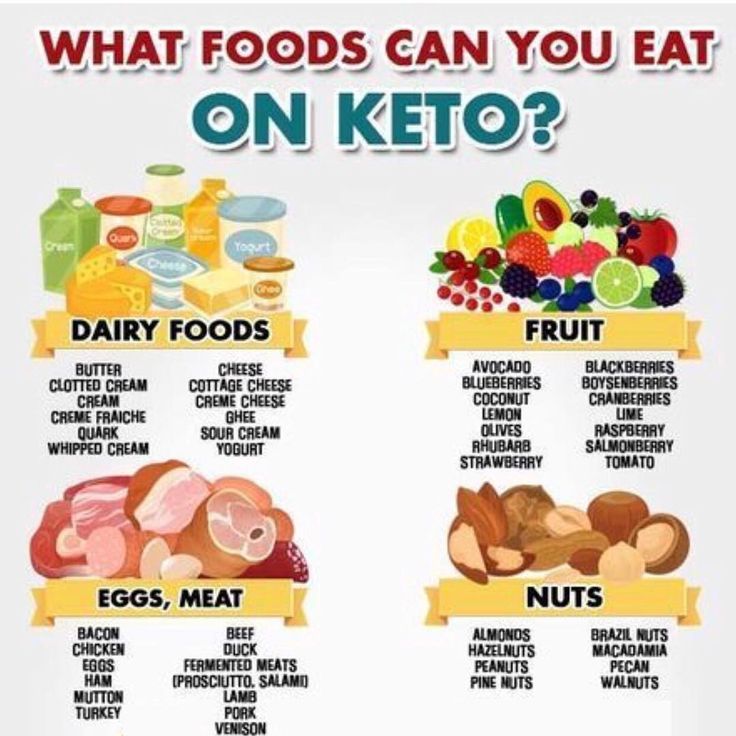
Depending on your baby's age, the doctor also might suggest adding yogurt with lactobacilli to your baby's diet. The lactobacilli are "good" bacteria that can help get rid of the yeast in your child's mouth.
If your baby keeps getting oral thrush, especially if he or she is older than 9 months old, talk with your doctor because this might be a sign of another health issue.
Can Oral Thrush Be Prevented?
Oral thrush is a common infection in babies, but you can help prevent it:
- If you formula-feed your baby or use a pacifier, thoroughly clean the nipples and pacifiers in hot water or a dishwasher after each use. That way, if there's yeast on the bottle nipple or pacifier, your baby won't be reinfected. Store milk and prepared bottles in the refrigerator to prevent yeast from growing.
- If you breastfeed and your nipples are red and sore, you might have a yeast infection on your nipples, which you and your baby can pass back and forth.
 Talk to your doctor, who might recommend using an antifungal ointment on your nipples while your baby is treated with the antifungal solution.
Talk to your doctor, who might recommend using an antifungal ointment on your nipples while your baby is treated with the antifungal solution.
To prevent diaper rash, change diapers often.
Reviewed by: Michelle P. Tellado, MD
Date reviewed: September 2019
Share:
/content/kidshealth/misc/medicalcodes/parents/articles/thrush
What is Oral Thrush in Babies and How to Prevent It?
Is your baby extra fussy these days – especially during feedings? If you’re nursing, have you also noticed your nipples are all of a sudden sore and red? Chances are you both may have a yeast infection called oral thrush.
Ew, what?! Where? How?
Before you freak out, know that oral thrush is actually a very common and usually harmless breastfeeding problem.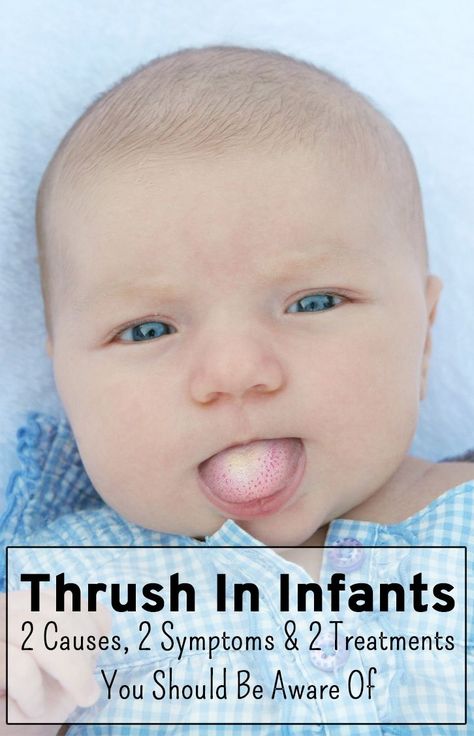 Here’s what you need to know to help you and your baby feel better, plus steps to prevent another occurrence.
Here’s what you need to know to help you and your baby feel better, plus steps to prevent another occurrence.
What is thrush?
Oral thrush, an infection in the mouth, is caused by a yeast-like fungus called Candida albicans. Candida can normally live in our mouth, intestines and genital areas without causing any problems, but sometimes it can grow out of control quickly and become a pain for you and your baby.
“Babies are more at risk of getting and passing thrush to their mothers during breastfeeding,” said Shelbie Radom, RN, at Banner McKee Medical Center in Loveland, CO. “Newborns can get a Candida infection from their mother during birth or may be at higher risk if they have serious health conditions or were born prematurely. It can also occur after mom or baby have taken antibiotics, which can reduce good bacteria in our bodies.”
Symptoms of thrush
If you take a peek inside your baby’s mouth and notice white patches on the tongue that don’t rub off or go away, this could be a tell-tale sign they have thrush. Thrush can also be painful, so you may also notice changes in their feeding habits. It’s not unusual for babies to become fussier while nursing, bottle-feeding or sucking on their pacifier or thumb.
Thrush can also be painful, so you may also notice changes in their feeding habits. It’s not unusual for babies to become fussier while nursing, bottle-feeding or sucking on their pacifier or thumb.
“One sign is if your baby has been breastfeeding without difficulty and then suddenly begins to come on and off the breast crying as if in pain,” Radom said. “Another symptom can be an increased or worsening diaper rash that is angry red, painful and hard to treat.”
If you’re nursing, chances are you may also have a yeast infection too! It’s not uncommon for you and your baby to pass it back and forth from their mouth to your breast and back again. Symptoms of nipple thrush include burning or sore nipples. You may also experience shooting pains during or after feedings.
Treating oral thrush
Before you Google “home remedies for thrush,” Radom cautions against doing so until after consulting with your baby’s doctor or your lactation consultant.
“Old home remedies may work in mild cases or for very healthy mothers and babies, but thrush is difficult to treat and may require several weeks of treatment, so these remedies may compound the problem,” Radom said.
To prevent ongoing infection or reinfection, the key is for both you and your baby to get treated at the same time. If your baby’s doctor determines it is indeed thrush, they may prescribe an antifungal medication, which is applied topically to the insides of their mouth and tongue for 10 days. If you have nipple thrush, your doctor will likely recommend a prescription antifungal cream as well for your nipples.
Important tip: “Always finish all antibiotics prescribed, even when symptoms are gone,” Radom said.
Preventing thrush altogether
Candida is a sneaky, resilient little booger … er, yeast. It thrives in warm, moist environments, so your nipples and baby’s mouth (even baby’s diaper area!) are perfect places for yeast and bacteria to hide and spread.
While thrush can be difficult to deal with and sometimes hard to prevent, here are five steps you can do at home that may help:
- Wash your hands. Make sure you wash your hands before and after nursing and after diaper changes.
 This way you can not only prevent the spread of Candida but also many other common illnesses too.
This way you can not only prevent the spread of Candida but also many other common illnesses too. - Keep anything that comes in contact with your baby’s mouth and your breasts clean. Even if thrush is not a concern, you should always regularly wash items that have been in your baby’s mouth in hot, soapy water. You should sterilize bottles, nipples, pacifiers, teethers and even breast pump parts that touch your nipples.
- Change your nursing bra and breast pads regularly. Milk leakage in your nursing bra and nursing pad can be a breeding ground for yeast and bacteria to grow. Change out nursing pads and properly wash your nursing bras when they get wet.
- Add probiotics or yogurt to your daily diet. Taking a probiotic or eating yogurt with active cultures to your diet may help build good bacteria that manages the growth of yeast.
- Let “the girls” hang out to dry after nursing. If you are breastfeeding, allow your nipples to completely dry between feedings before putting your bra back on.

Don’t let a little fungus get you down, mama! Talk to your doctor if you have any questions or concerns to find the best treatment option for you and your baby. To find a Banner Health specialist near you, visit bannerhealth.com.
For more parent-friendly advice, check out:
- 7 Common Breastfeeding Challenges and How to Solve Them
- 5 Common Teething Questions Answered
- Safe Sleep Practices for Baby
Children's Health Parenting Pregnancy
Children's stomatitis - causes, symptoms, types of stomatitis, methods of diagnosis and treatment of children's stomatitis in the "SM-Clinic" for children and adolescents
Signs of stomatitis in a child depend on the form of pathology and the cause that caused the disease.
Herpetic or viral stomatitis
It is caused by the introduction of the herpes simplex virus type 1, and can have two forms in children: acute primary and secondary recurrent. In newborns and breastfed infants, it is rare due to the presence in the body of a large number of antibodies received from the mother, or it occurs in a mild form almost imperceptibly. At an older age, the pathology manifests itself acutely, with severe symptoms of intoxication. The most common ways of infection: household items, toys, close contact with carriers, airborne.
In newborns and breastfed infants, it is rare due to the presence in the body of a large number of antibodies received from the mother, or it occurs in a mild form almost imperceptibly. At an older age, the pathology manifests itself acutely, with severe symptoms of intoxication. The most common ways of infection: household items, toys, close contact with carriers, airborne.
Symptoms of herpetic stomatitis in babies are:
- ulceration on the mucosa simultaneously in several places of approximately the same type and size;
- an increase in temperature, often to high values \u200b\u200band even before the first rashes appear;
- undulating reappearance of painful sores, which each time is accompanied by a rise in temperature;
- swelling of the gums, their redness;
- the appearance of an unpleasant, putrid odor from the mouth.
Candidiasis stomatitis
In the people, this disease is commonly called children's thrush. Most often this form affects children under 3 years of age. It is fungal in nature, caused by the yeast-like fungus Candida. This type of stomatitis is preceded by a burning sensation in the mouth, excessive dryness of the affected mucosa, an unpleasant taste and smell. The child behaves restlessly, refuses to eat; observed sleep and eating disorders. Soon, the inner side of the cheeks, tongue, gums and even lips are covered with small whitish dots, which, merging and forming a dense white coating of curdled consistency, multiply rapidly. In advanced cases, plaque acquires a dirty gray color. It is almost impossible to remove it, under it a swollen, inflamed surface is found, which, at the slightest physical impact, begins to bleed.
Most often this form affects children under 3 years of age. It is fungal in nature, caused by the yeast-like fungus Candida. This type of stomatitis is preceded by a burning sensation in the mouth, excessive dryness of the affected mucosa, an unpleasant taste and smell. The child behaves restlessly, refuses to eat; observed sleep and eating disorders. Soon, the inner side of the cheeks, tongue, gums and even lips are covered with small whitish dots, which, merging and forming a dense white coating of curdled consistency, multiply rapidly. In advanced cases, plaque acquires a dirty gray color. It is almost impossible to remove it, under it a swollen, inflamed surface is found, which, at the slightest physical impact, begins to bleed.
Angular stomatitis
Sometimes it is considered as a kind of candida, because it can be caused by the same Candida fungi or streptococci. In this case, the corners of the lips are affected, which makes it difficult for the child to open his mouth, eat, and even talk. It is more common in children of school age. When affected by streptococci, a purulent crust forms on the surface of the ulcers, which, when removed, immediately grows again. The disease is recurrent in nature and is often popularly referred to as "zayed".
It is more common in children of school age. When affected by streptococci, a purulent crust forms on the surface of the ulcers, which, when removed, immediately grows again. The disease is recurrent in nature and is often popularly referred to as "zayed".
Aphthous stomatitis
Aphthous stomatitis is accompanied by the following symptoms:
- temperature increase;
- loss of appetite;
- burning and itching in the mouth.
- the appearance on the inner surface of the cheeks, gums, tongue and palate of painful white sores with a red border and a cloudy film on top - aphthae, which have clear and even edges characteristic of this type of disease.
Often this form of pathology occurs against the background of severe weakness, drowsiness of the baby. In some children, aphthous stomatitis is rare, in others it is observed up to 2 or more times a year.
Bacterial stomatitis
One of the diseases of "dirty hands". The cause of development is a bacterial infection that has entered the mouth. The introduction occurs especially quickly when the integrity of the mucosa is violated: with a wound in the mouth, a bitten inner surface of the cheeks or lips, a newly erupted tooth, etc. The same form of the disease includes infections obtained during passage through the birth canal, especially in the case of a mother with venereal diseases, scarlet fever, etc.
The cause of development is a bacterial infection that has entered the mouth. The introduction occurs especially quickly when the integrity of the mucosa is violated: with a wound in the mouth, a bitten inner surface of the cheeks or lips, a newly erupted tooth, etc. The same form of the disease includes infections obtained during passage through the birth canal, especially in the case of a mother with venereal diseases, scarlet fever, etc.
External symptoms directly depend on the type of bacteria, and its manifestation depends on the state of the child's immune system. Often manifested by inflammation of the gums or the appearance of a dirty gray film on them. The child experiences pain while eating, especially sharp when eating spicy and pickled foods, citrus fruits, etc. The mucous membrane of the mouth is edematous and acquires a darker shade, burns and itches. Then bubbles appear on it, which quickly ulcerate or crack, begin to bleed. The process is very painful and is accompanied by a putrid specific smell from the mouth. Against this background, the temperature often rises to high values, the head and joints hurt, symptoms of intoxication of the body may be present. The child becomes weak, lethargic and capricious.
Against this background, the temperature often rises to high values, the head and joints hurt, symptoms of intoxication of the body may be present. The child becomes weak, lethargic and capricious.
Common symptoms for any form of stomatitis are fever, ulceration of the oral mucosa and swollen lymph nodes.
How to treat stomatitis in a child?
Children's stomatitis
Stomatitis is an inflammation in a child's mouth that can cause sores on the tongue, gums, cheeks, and throat. This situation is more common in children under 3 years of age, but can also occur in adolescence. In most cases, stomatitis is caused by the herpes virus, and in this case is called herpetic gingivostomatitis.
Treatment is based on a pediatrician who recommends that the child's mouth be kept clean at all times and that medication be used to relieve symptoms and, in some cases, relieve discomfort.
What can cause stomatitis in children?
Stomatitis can occur for several reasons, but the most common causes are:
- reduced immune system defenses,
- habit of putting dirty hands and objects (toys) in the mouth,
- as a result of infection with influenza viruses, herpes simplex or varicella, Coxsackie, enteroviruses,
- candidiasis (thrush).
Other pathogens are bacteria and fungi. Also, the cause may be temperature or mechanical injuries of the oral cavity, allergic reactions. Deficiency of vitamins B or C plays a role.
Main symptoms
Children's stomatitis usually presents with symptoms such as irritability and poor appetite, because when food enters the wound, it causes pain. Other symptoms that may occur with stomatitis:
- Mouth ulcers or inflammation of the gums;
- Pain in mouth and throat when swallowing;
- Can be temperatures above 38 °C;
- Wounds on the lips;
- Bad breath.
These symptoms may appear simultaneously, but most often only ulcers appear. In addition to stomatitis, there are other diseases that can cause mouth ulcers, such as the Coxsackie virus, which causes foot-and-mouth disease. Therefore, it is important that the pediatrician assess the symptoms in time and do tests in order to correctly diagnose.
What is observed in the mouth of a child with stomatitis?
On examination, there may be painful erosions, ulcers, and blisters on the lining of the inside of the cheeks, gums, lips, tongue, and, less commonly, the back of the throat. Enlarged lymph nodes in the neck and under the lower jaw are also common.
Enlarged lymph nodes in the neck and under the lower jaw are also common.
Gums may be slightly swollen, red, ulcerated and bleed easily.
When the cause is viral, oral lesions may last 7 to 10 days, although general symptoms resolve sooner.
Can the pathogen be easily diagnosed?
Microbiological examination can be carried out, but the methods used are not simple.
Samples must be transported and cultured in a suitable medium. Results will be available in approximately 15 days. Rapid diagnostic methods are also available, such as direct staining of the contents of the vesicles with fluorescent antibodies.
Is there any specific treatment?
Treatment of stomatitis must be prescribed by a pediatrician or dentist and lasts approximately 2 weeks. However, it is important to be careful with the food the child eats and maintain proper oral hygiene to avoid the multiplication of microorganisms in the ulcer.
Most often, gingivostomatitis resolves spontaneously and requires only symptomatic pain management or antiseptics to aid local healing.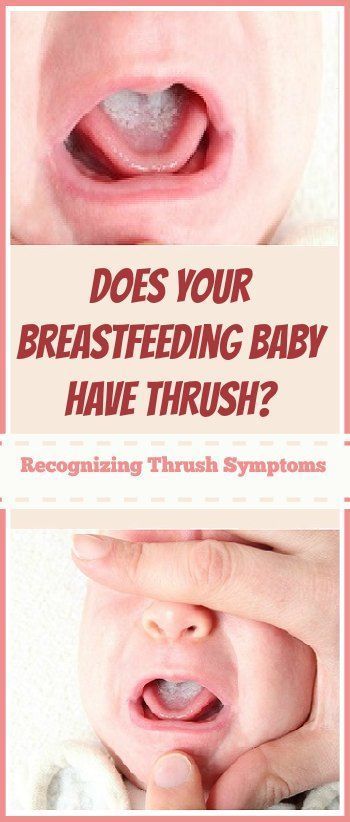 In children, special attention should be paid to their hydration by offering them liquids in fractional form, cold or at room temperature. Sour, salty or spicy foods should be avoided.
In children, special attention should be paid to their hydration by offering them liquids in fractional form, cold or at room temperature. Sour, salty or spicy foods should be avoided.
Discomfort can be reduced with paracetamol or ibuprofen taken by mouth. If a yeast infection is suspected, topical application or antifungal rinses are usually effective. In some cases, the use of antiviral drugs such as acyclovir may be recommended for gingivostomatitis caused by herpes viruses. This medication helps heal wounds in the mouth, but should only be used with a pediatrician's prescription. Therapy of herpes infection with acyclovir is not required for mild infection in children with sufficiently strong immunity.
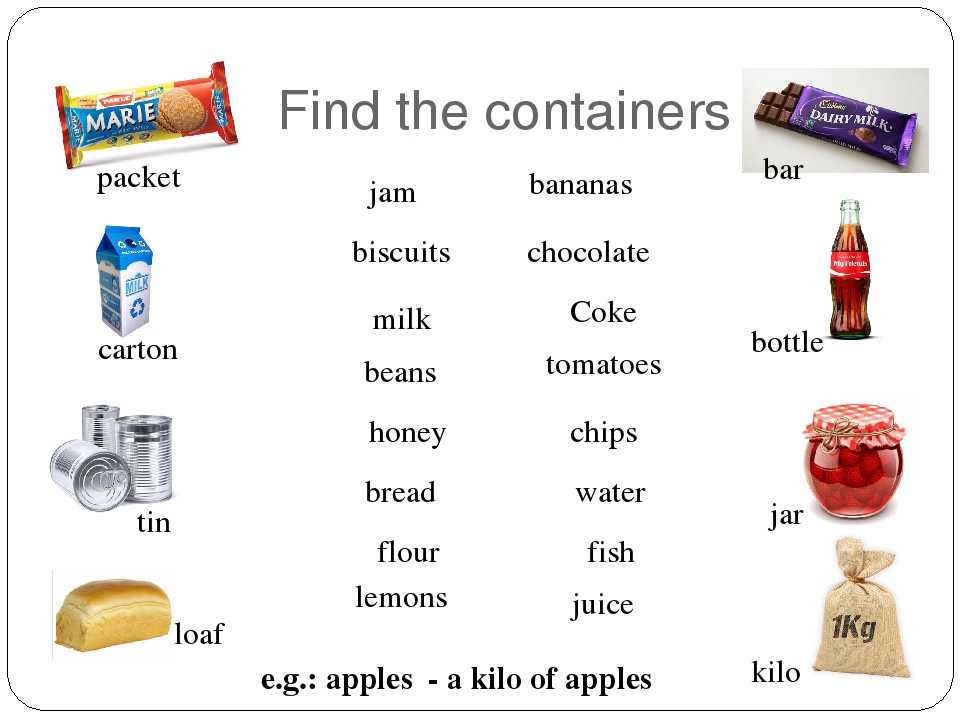
How to feed an infant or child with stomatitis?
It is important that the baby's feeding is not interrupted when there is an illness. However, it is important to be careful to avoid aggravating symptoms:
- Avoid acidic foods such as orange, kiwi or pineapple;
- Offer cold liquids such as fruit juices or smoothies;
- Eating pureed or liquid foods such as soups;
- Choose cold foods such as yogurt, fruit compotes and gelatin.