Signs of a breast infection
Breast Infection (Mastitis): Symptoms, Causes, Treatments
Written by WebMD Editorial Contributors
In this Article
- How the Breast Is Built
- Breast Infection Causes
- Breast Infection Symptoms
- When to Seek Medical Care
- Breast Infection Exams and Tests
- Breast Infection Treatment
- Breast Infection Home Remedies
- Medications for Mastitis
- Surgery for an Abscess
- Next Steps
- Follow-Up Care After a Breast Infection
- Mastitis Prevention
- Outlook for Breast Infections
How the Breast Is Built
The breast is composed of several glands and ducts that lead to the nipple and the surrounding colored area called the areola. The milk-carrying ducts extend from the nipple into the underlying breast tissue like the spokes of a wheel. Under the areola are lactiferous ducts. These fill with milk during lactation after a woman has a baby. When a girl reaches puberty, changing hormones cause the ducts to grow and cause fat deposits in the breast tissue to increase. The glands that produce milk (mammary glands) that are connected to the surface of the breast by the lactiferous ducts may extend to the armpit area.
Breast Infection Causes
Mastitis is an infection of the tissue of the breast that occurs most frequently during the time of breastfeeding. It can occur when bacteria, often from the baby's mouth, enter a milk duct through a crack in the nipple.
Breast infections most commonly occur one to three months after the delivery of a baby, but they can occur in women who have not recently delivered and in women after menopause. Other causes of infection include chronic mastitis and a rare form of cancer called inflammatory carcinoma.
In healthy women, mastitis is rare. However, women with diabetes, chronic illness, AIDS, or an impaired immune system may be more susceptible.
About 1%-3% of breastfeeding mothers develop mastitis. Engorgement and incomplete breast emptying can contribute to the problem and make the symptoms worse.
Chronic mastitis occurs in women who are not breastfeeding. In postmenopausal women, breast infections may be associated with chronic inflammation of the ducts below the nipple. Hormonal changes in the body can cause the milk ducts to become clogged with dead skin cells and debris. These clogged ducts make the breast more open to bacterial infection. Infection tends to come back after treatment with antibiotics.
Breast Infection Symptoms
Breast infections may cause pain, redness, and warmth of the breast along with the following symptoms:
- Tenderness and swelling
- Body aches
- Fatigue
- Breast engorgement
- Fever and chills
- Abscess: A breast abscess can be a complication of mastitis. Noncancerous masses such as abscesses are more often tender and frequently feel mobile beneath the skin. The edge of the mass is usually regular and well defined. Indications that this more serious infection has occurred include the following:
- Tender lump in the breast that does not get smaller after breastfeeding a newborn (If the abscess is deep in the breast, you may not be able to feel it.
 )
) - Pus draining from the nipple
- Persistent fever and no improvement of symptoms within 48-72 hours of treatment
- Tender lump in the breast that does not get smaller after breastfeeding a newborn (If the abscess is deep in the breast, you may not be able to feel it.
When to Seek Medical Care
Call your health care provider as soon as you feel any suspicious lump, whether you are breastfeeding or not. Call for an appointment if:
- You have any abnormal discharge from your nipples.
- Breast pain is making it difficult for you to function each day.
- You have prolonged, unexplained breast pain.
- You have any other associated symptoms such as redness, swelling, pain that interferes with breastfeeding, a mass or tender lump in the breast that does not disappear after breastfeeding.
- If you are breastfeeding, call your doctor if you develop any symptoms of breast infection so that treatment may be started promptly.
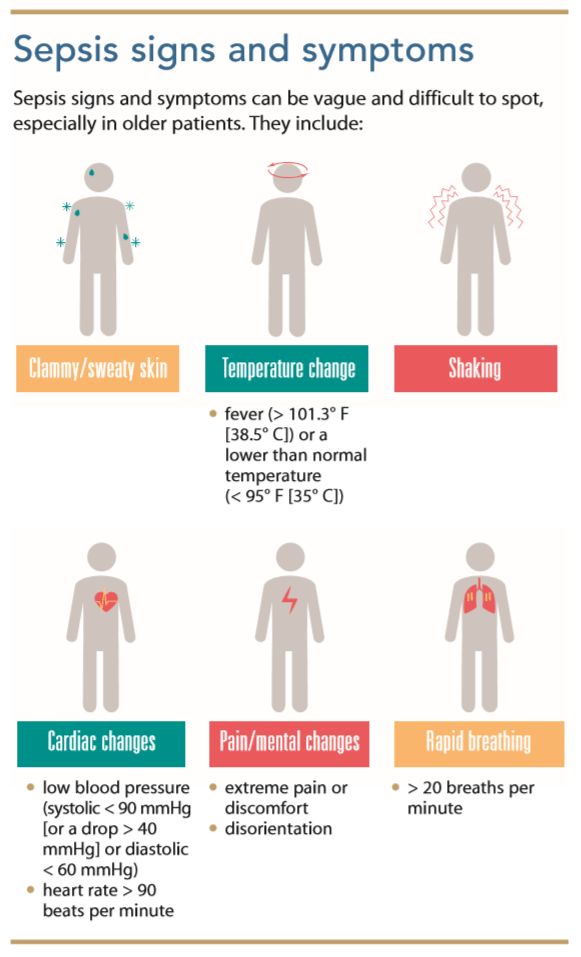
You may need to be evaluated in a hospital's emergency department if the breast pain is associated with other signs of an infection (such as a fever, swelling, or redness to the breast) and if your health care provider cannot see you promptly.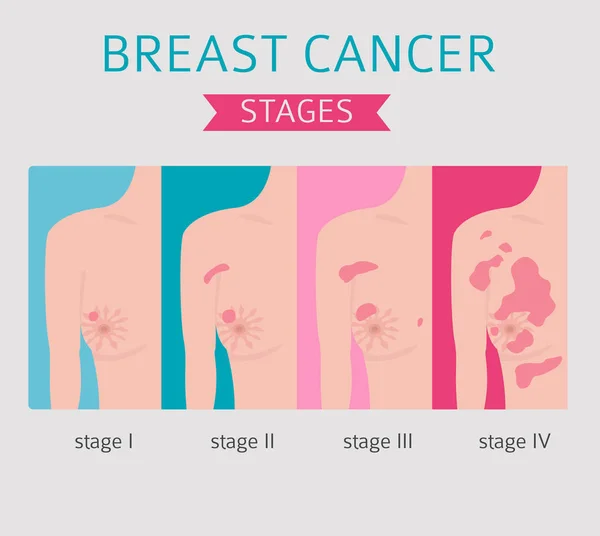 The below symptoms require emergency treatment:
The below symptoms require emergency treatment:
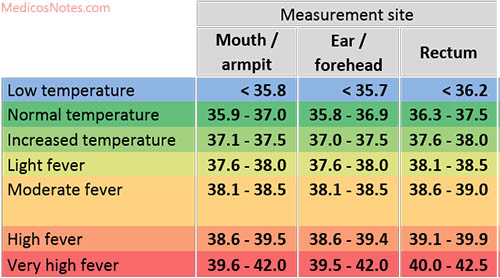
- A persistent high fever greater than 101.5°F
- Nausea or vomiting that is preventing you from taking the antibiotics as prescribed
- Pus draining from the breast
- Red streaks extending toward your arm or chest
- Dizziness, fainting, or confusion
Breast Infection Exams and Tests
The diagnosis of mastitis and a breast abscess can usually be made based on a physical exam.
- If it is unclear whether a mass is due to a fluid-filled abscess or to a solid mass such as a tumor, a test such as an ultrasound may be done. An ultrasound may also be helpful in distinguishing between simple mastitis and abscess or in diagnosing an abscess deep in the breast. This noninvasive test allows your doctor to directly visualize the abscess by placing an ultrasound probe over your breast. If an abscess is confirmed, aspiration or surgical drainage, and IV antibiotics, are often required.
- Cultures may be taken, either of breast milk or of material taken out of an abscess through a syringe, to determine the type of organism causing the infection.
 This information can help your doctor decide what kind of antibiotic to use.
This information can help your doctor decide what kind of antibiotic to use. - Nonbreastfeeding women with mastitis, or those who do not respond to treatment, may have a mammogram or breast biopsy. This is a precautionary measure because a rare type of breast cancer can produce symptoms of mastitis.
Breast Infection Treatment
Breast infections require treatment by a health care provider.
Breast Infection Home Remedies
After you see a doctor, try the following to help your breast infection heal.
- Pain medication: Take acetaminophen (Tylenol) or ibuprofen (such as Advil) for pain. These drugs are safe while breastfeeding and will not harm your baby. Your doctor may prescribe a prescription strength pain reliever if your pain is severe and not relieved with over-the-counter medication.
- In mild cases of mastitis, antibiotics may not be prescribed at all. If you are prescribed antibiotics, finishing the prescription even if you feel better in a few days is very important.
- Frequent feedings: Do not stop breastfeeding from the affected breast, even though it will be painful and you may be taking antibiotics. Frequent emptying of the breast prevents engorgement and clogged ducts that can only make mastitis worse.
- If needed, use a breast pump to relieve pressure and completely empty the breast.
- You can also breastfeed from the unaffected side and supplement with infant formula as needed.
- The infection will not harm the baby because the germs that caused the infection probably came from the baby’s mouth in the first place.
- Breastfeeding should be avoided in the infected breast when an abscess is present.
- Pain relief: A warm compress applied before and after feedings can often provide some relief. A warm bath may work as well.
- If heat is ineffective, ice packs applied after feedings may provide some comfort and relief.
- Avoid using ice packs just before breastfeeding because it can slow down milk flow.
- Drink plenty of water -- at least 10 glasses a day. Eat well-balanced meals and add 500 extra calories a day while breastfeeding. Dehydration and poor nutrition can decrease milk supply and make you feel worse.
Medications for Mastitis
For simple mastitis without an abscess, oral antibiotics are prescribed. Cephalexin (Keflex) and dicloxacillin (Dycill) are two of the most common antibiotics chosen, but a number of others are available. The antibiotic prescribed will depend on your specific situation, your doctor’s preference, and any drug allergies you may have. This medicine is safe to use while breastfeeding and will not harm the baby.
Chronic mastitis in nonbreastfeeding women can be complicated. Recurrent episodes of mastitis are common. Occasionally, this type of infection responds poorly to antibiotics. Therefore, close follow-up with your doctor is mandatory.
If the infection worsens in spite of oral antibiotics or if you have a deep abscess requiring surgical treatment, you may be admitted to the hospital for IV antibiotics.
Surgery for an Abscess
If an abscess is present, it must be drained. After injection of a local anesthetic, the doctor may drain an abscess near the surface of the skin either by aspiration with a needle and syringe or by using a small incision. This can be done in the doctor’s office or emergency department.
If the abscess is deep in the breast, however, it may require surgical drainage in the operating room. This procedure is usually done under general anesthesia to minimize pain and completely drain the abscess. Antibiotics and heat on the area are also used to treat abscesses.
Next Steps
Mastitis does not cause cancer, but cancer can mimic mastitis in appearance. If a breast infection is slow to go away, your health care provider may recommend a mammogram or other tests to rule out cancer.
Follow-Up Care After a Breast Infection
If you have a breast infection, you may be seen for a recheck in 24-48 hours.
- Take all antibiotics as prescribed.
- Take your temperature three times a day for the first 48 hours after treatment begins. Watch for fever.
- Call your doctor if you develop a high fever, vomiting, or increasing redness, swelling, or pain in the breast.
- Follow up with your doctor in one to two weeks to make sure that the infection has gone away. If the infection spreads or an abscess develops, you may require IV antibiotics or surgical treatment.
Mastitis Prevention
Sometimes mastitis is unavoidable. Some women are more susceptible than others, especially those who are breastfeeding for the first time. In general, good habits to prevent mastitis include the following:
- Breastfeed equally from both breasts.
- Empty breasts completely to prevent engorgement and blocked ducts.
- Use good breastfeeding techniques to prevent sore, cracked nipples.
- Allow sore or cracked nipples to air dry.
- Prevent moisture from accumulating in breast pads or bras.
- Avoid dehydration by drinking plenty of fluids.
- Practice careful hygiene: Handwashing, cleaning the nipples, keeping your baby clean.
Outlook for Breast Infections
When treated promptly, the majority of breast infections go away quickly and without serious complications. Most women can and should continue to breastfeed despite an episode of uncomplicated mastitis. With proper treatment, symptoms should begin to resolve within one to two days.
A breast abscess may require surgical drainage, IV antibiotics, and a short hospital stay. A small incision is made and usually heals quite well. Prognosis for complete recovery is also good.
Postmenopausal women with breast abscesses have a high rate of return after simple drainage and frequently need to follow up with a surgeon for more definitive treatment. Chronic infection can result if an abscess is not completely drained, and this can result in a poor cosmetic outcome.
Women's Health Guide
- Screening & Tests
- Diet & Exercise
- Rest & Relaxation
- Reproductive Health
- Head to Toe
Signs You Might Have a Breast Infection
Most Recent,Breast Cancer,Women
September 14, 2022
Your breast is suddenly hard or itchy, swollen or leathery. What’s going on? You might have a breast infection.
What’s going on? You might have a breast infection.
Let’s take a look at how to find the cause and how to make it better.
Who Gets Breast Infections?
Any adult woman can have inflamed breasts, but the specifics are different within two categories:
Breastfeeding women. Especially during the first six weeks of breastfeeding, mothers might be engorged, meaning their breasts are filled with milk, extra large and often hard.
- Nipple trauma is common at this time, as the nipple adjusts to baby’s mouth and pumping equipment. Cracks, dryness and bleeding can lead to mastitis, which is the medical term for inflammation of the breast tissue.
- Milk ducts can get blocked in the early weeks. When they don’t drain completely, inflammation can form.
- If baby has the fungal infection called thrush, that infection in their mouth might transfer to you, causing infection.
- Yeast infections might work their way into the breasts.
Trouble often starts if the skin cracks. Then a staph infection, strep or other bacteria can sneak in, causing achiness, fatigue or even flu-like symptoms.
Non-breastfeeding women. Women of all ages can get breast infections, and the reasons vary.
- Bacteria can work its way in during a nipple piercing.
- Trouble can start after you pull a hair out of your areola (the dark part of your nipple).
- Breast implants and reduction surgeries can lead to inflammation.
- Blood sugar issues such as diabetes or hyperglycemia might be at the root of the cause, and so can depressed immune systems.
- You’re wearing your bra the wrong way or have a reaction to a bug bite.
- Studies show that smoking also increases the chance of breast infection.
An abscess, a swollen part of the body that has puss inside, also can cause an inflamed breast. A pimple is one example. If you don’t release the puss, you’ll get more of it, and the situation will worsen.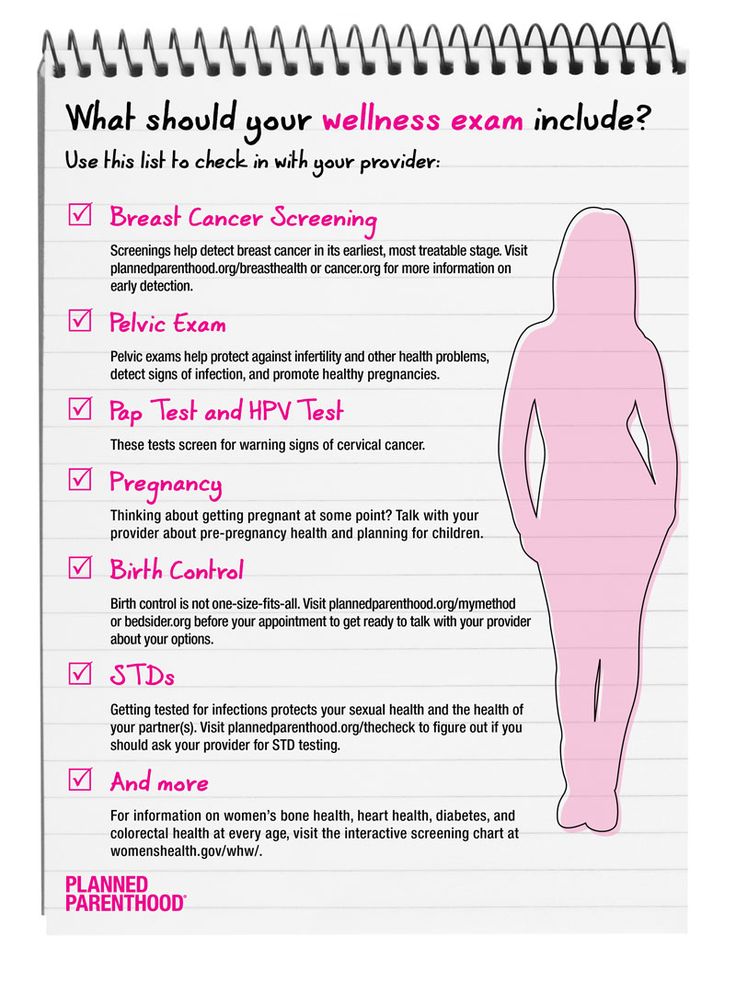 In that case, have a doctor drain it via aspiration or outpatient surgery.
In that case, have a doctor drain it via aspiration or outpatient surgery.
Inflammatory breast cancer and cellulitis are possibilities, but chances are your issue is one of the others. See a specialist if the symptoms don’t improve on their own or with the treatments your doctor recommends.
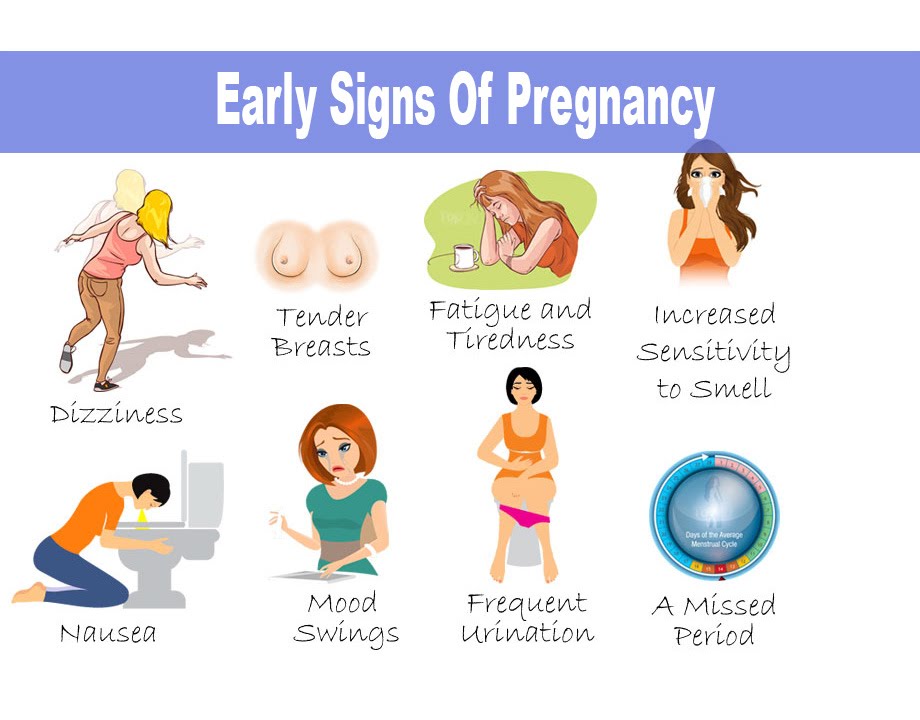
Breast Infection Symptoms
Your breast infection will likely make itself known via some sort of inflammation. Any of these symptoms might indicate a problem.
- Tenderness
- Pain
- Fever
- Chills
- Myalgia (body aches)
- Hardness
- Itchiness
- Red skin
- Swollen
- Warmth
- Leathery or orange peel-like skin texture
- Discharge
- A lump
How Are Breast Infections Treated?
Many inflammations go away within a day or two. In most situations, if your breast is inflamed because you have a microbial or yeast infection, the discomfort will persist and you’ll be prescribed antibiotics.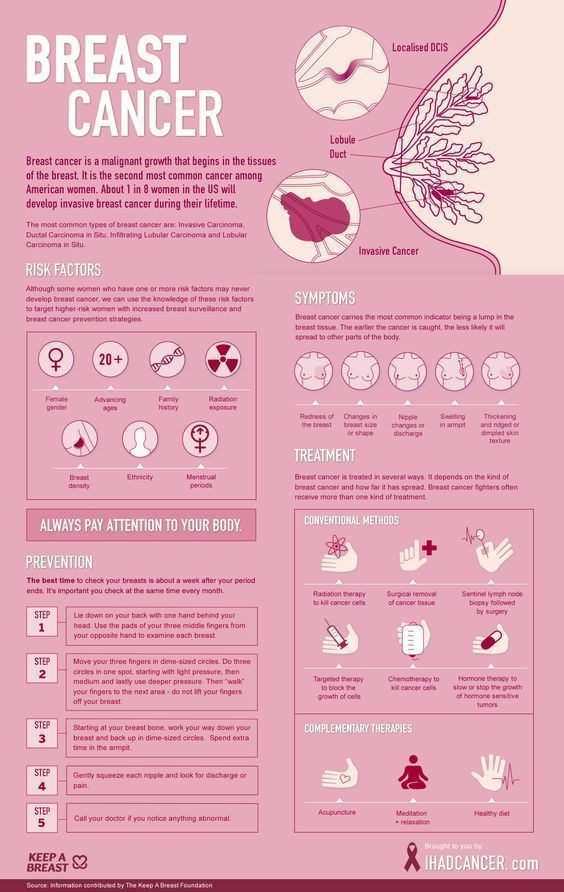 Over-the-counter pain killers such as aspirin, ibuprofen and acetaminophen will lessen symptoms but not cure the infection.
Over-the-counter pain killers such as aspirin, ibuprofen and acetaminophen will lessen symptoms but not cure the infection.
In the meantime, use common sense. A warm or cold washcloth held to the irritated area might make it feel better. While you can breastfeed if you have a breast infection, you might consider taking a break if it’s too painful. Use a pump to retain your milk flow until the problem heals; empty your breasts fully on a regular basis. Also, change baby’s position during nursing to make sure the nipple and breast tissue are evenly inside baby’s mouth. A specialist can teach you how. Massage your breasts if that feels healing. Taking a daily probiotic might help too, according to a recent study.
If the inflammation persists, you’ll need to return to the doctor for an imaging test. If the test shows you have an abscess, you’ll require more aggressive treatment.
Breast inflammation and infections are uncomfortable and inconvenient, but they’re treatable.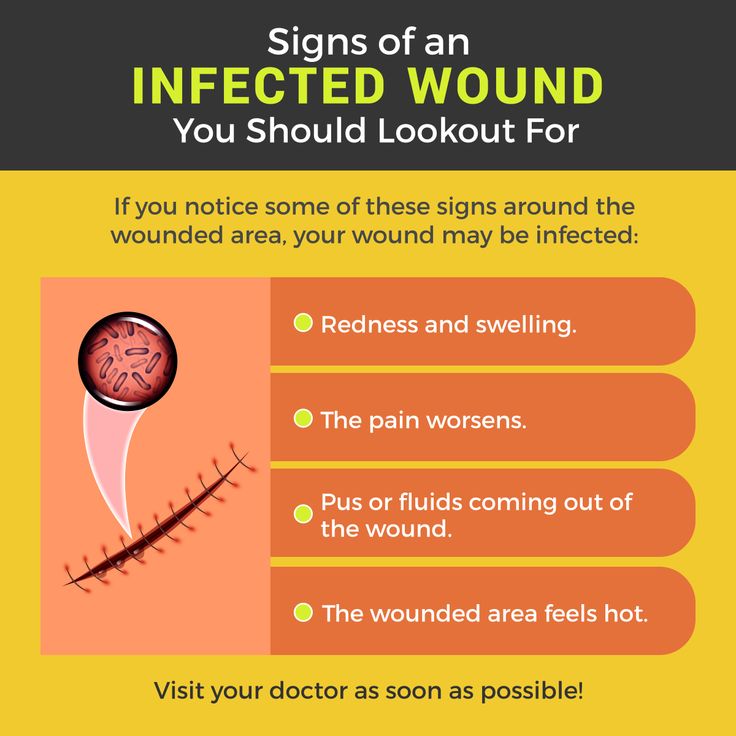 Seek out care, follow the instructions, and your breasts will feel fine within a week or two.
Seek out care, follow the instructions, and your breasts will feel fine within a week or two.
Choose to Stay in Touch
Sign up to receive the latest health news and trends, wellness & prevention tips, and much more from Orlando Health.
Sign Up
Treatment of infections and inflammation of the mammary glands in the Vyborgsky district of St. Petersburg
In this article, we have described the most common diseases of the mammary glands. The material is for informational purposes only. If you are worried about any tightness in the chest or pain, be sure to contact a mammologist to conduct a diagnostic study.
Orthopedist
Appointment online
Phones:
+7 (812) 30-888-03
+7 (812) 242-53-50
Clinic address: St. Petersburg, Vyborgsky district, Parnas metro station, st. Asafiev, 9, building 2, lit. А
Our doctors
Kasyanova Marina Nikolaevna
Surgeon, oncologist, mammologist, proctologist, doctor of ultrasound diagnostics, Ph. D.
D.
Borisov Sergey Vladimirovich
Surgeon, pediatric surgeon, oncologist, mammologist, doctor of ultrasound diagnostics (children, adults)
Prices for services
- Mammologist's consultation
- Procedures
Please note! Prices are for adult patients. Please see the Pediatrics section for the cost of children's appointments.
| Reception (inspection, consultation) Mammologist Primary | 2 200 |
| Reception (examination, consultation) of a mammologist repeated | 1 800 |
| Reception (examination, consultation) ) Ph.D. primary | 2 500 |
| Appointment (examination, consultation) with an oncologist (mammologist), Ph.D. Repeated | 2 100 |
| Opening and drainage of purulent mastitis (1 square) without the cost of anesthesia | 5 100.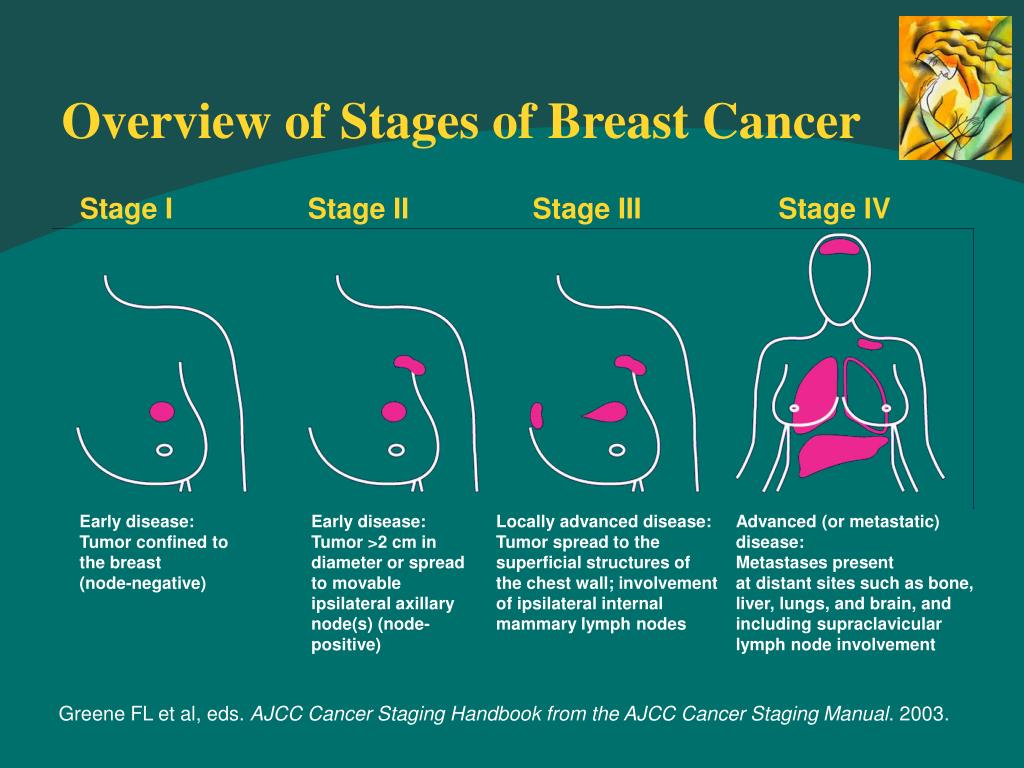 00 00 | 550.00
| Dressing after opening for purulent mastitis | 1000.00 |
| Small -iginal aspiration biopsy (TAB) of breast cysts (1 cyst), without the cost of histology | 2 100.00 |
lactation mastitis
The most common type mastitis. With this condition, which occurs when a woman is breastfeeding, women's nipples become cracked and sore, allowing bacteria from the baby's mouth to enter the ducts and multiply rapidly in the milk. Sometimes the infection comes from a blocked milk duct. In both cases, the chest becomes hard, reddened, hot and sore.
The doctor may also prescribe antibiotics and painkillers. In some cases, lactational mastitis progresses and forms an abscess, a more serious condition that may require drainage.
Non-lactational mastitis
Non-lactational mastitis is similar to lactational mastitis but occurs in non-breastfeeding women. In some cases, this condition occurs after a lumpetomy followed by radiation therapy in women with diabetes or in those who have reduced immune functions in the body.
In some cases, this condition occurs after a lumpetomy followed by radiation therapy in women with diabetes or in those who have reduced immune functions in the body.
Although rare, this condition is usually accompanied by high fever and headache and is treated with antibiotics. Consult your doctor for diagnosis and treatment.
Chronic subarreal abscess
Is a common infection of the breast, although it is uncommon. If an infection is found before an abscess develops, it can often be treated with antibiotics. Most often it is necessary to make an incision and drain the abscess.
Mastalgia (chest pain)
Classified as cyclic pain (associated with menstrual periods) or non-cyclic. The latter may come from the chest or may come from somewhere else, such as near the muscles or joints, felt in the chest. In some cases, pain can range from minor discomfort to severe. Many women with mastalgia worry more about the fear of cancer than the pain itself.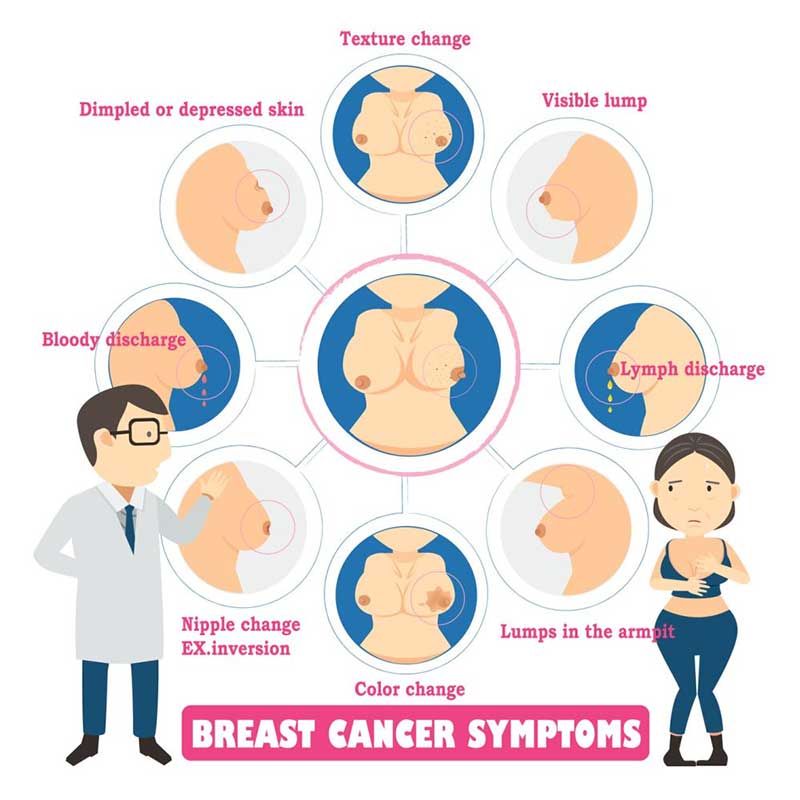
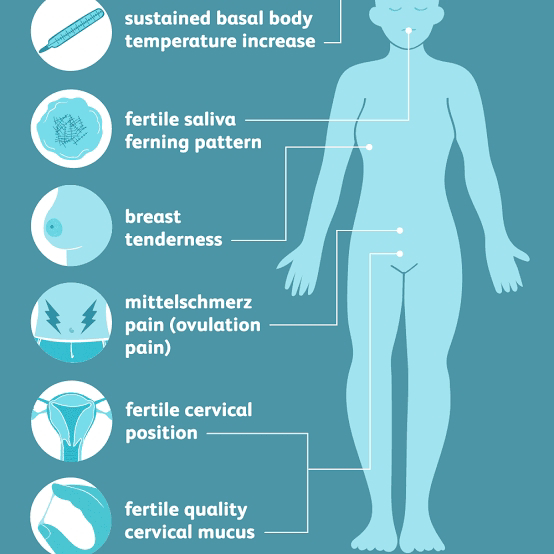
Cyclic chest pain
The most common type of chest pain is associated with the menstrual cycle and is almost always hormonal. Some women begin to experience pain during ovulation, which continues until the start of the menstrual cycle. The pain may be subtle or so severe that the woman cannot wear tight clothing or endure close contact of any kind. The pain may be felt in only one breast or in the area under the arm.
Doctors continue to study the role of hormones in cyclic mastalgia. One study showed that some women with cyclic mastalgia experienced a decrease in the ratio of progesterone to estrogen in the second half of their menstrual cycle. Other studies have shown that an abnormality in the hormone prolactin can affect breast pain. Hormones can also influence cyclical stress-related chest pain - sensations can increase or change in texture with hormone changes that occur during times of stress.
Hormones cannot give a general response to cyclic breast pain because the pain is often more severe in one breast than the other (steroids tend to affect both breasts equally).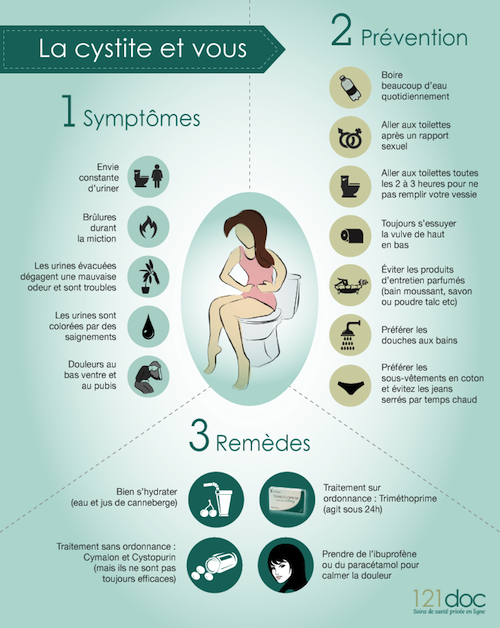
Treatment includes:
- avoiding caffeine
- vitamin E
- low fat diet
- In some cases, various additional hormones and hormone blockers are also prescribed. These may include:
- birth control pills
- BROMOKRIPTIN (which blocks prolactin in the hypothalamus)
- Danazole, male hormone
- thyroid hormones
- Tamoxifen, estrogen blocker
The pectoral pain in the breasts is not cyclical in the pectoral of
does not change during the menstrual cycle. As a rule, the pain is present all the time and is located only in one specific place.
One of the causes of non-cyclic chest pain is trauma or impact. Other causes may include arthritic pain in the chest cavity and in the area of the neck that reaches the chest.
Doctors usually do a physical examination and a mammogram. In some cases, a biopsy is also needed. If the pain is determined to be caused by a cyst, it will be aspirated. Depending on where the pain occurs, treatment may include analgesics, anti-inflammatory drugs, and compresses.
Depending on where the pain occurs, treatment may include analgesics, anti-inflammatory drugs, and compresses.
Orthopedist
Online appointment
Phones:
+7 (812) 30-888-03
+7 (812) 242-53-50
Clinic address: St. Petersburg, metro Vyborgsky district Parnassus, st. Asafiev, 9, to 2, lit. A
Inflammation of the mammary gland treatment - Modern methods of treatment at the MCHC
Inflammation of the mammary gland or mastitis in 80-90% of cases is associated with pregnancy and childbirth. This is a benign process in the tissues of the gland, limited (abscess) or diffuse (phlegmon), which requires timely intervention and antibiotics. Inflammation of the mammary gland requires timely and immediate treatment, it can be carried out at the medical center of I. Medvedev.
Inflammation of the mammary gland: general questions
Mastitis is a non-specific inflammation of the breast tissue, mainly associated with childbirth and lactation, or with mastopathy (non-lactational mastitis). Rarely, mastitis is chronic, usually acute.
Rarely, mastitis is chronic, usually acute.
Causes of breast inflammation:
- milk stasis
- incomplete emptying of the gland during feeding
- cracked nipples
- improper breastfeeding
- poor hygiene
- secretion stagnation
- Calcifications in the ducts
Symptoms of mastitis
Classic signs of breast inflammation: pain, redness, swelling, fever, dysfunction.
- engorgement, edema
- skin reddening
- bursting pains
- infiltrate
- pus in milk
- skin changes like gangrene, infiltrate
Inflammation is usually associated with a violation of the patency of the ducts and the addition of a secondary infection, which gets from the nipple into the gland tissue through the milk ducts and lymphatic vessels. With a normal level of immunity, the process is limited by a capsule, an abscess is formed, with immunodeficiency, pus spreads through the tissues - a phlegmonous form.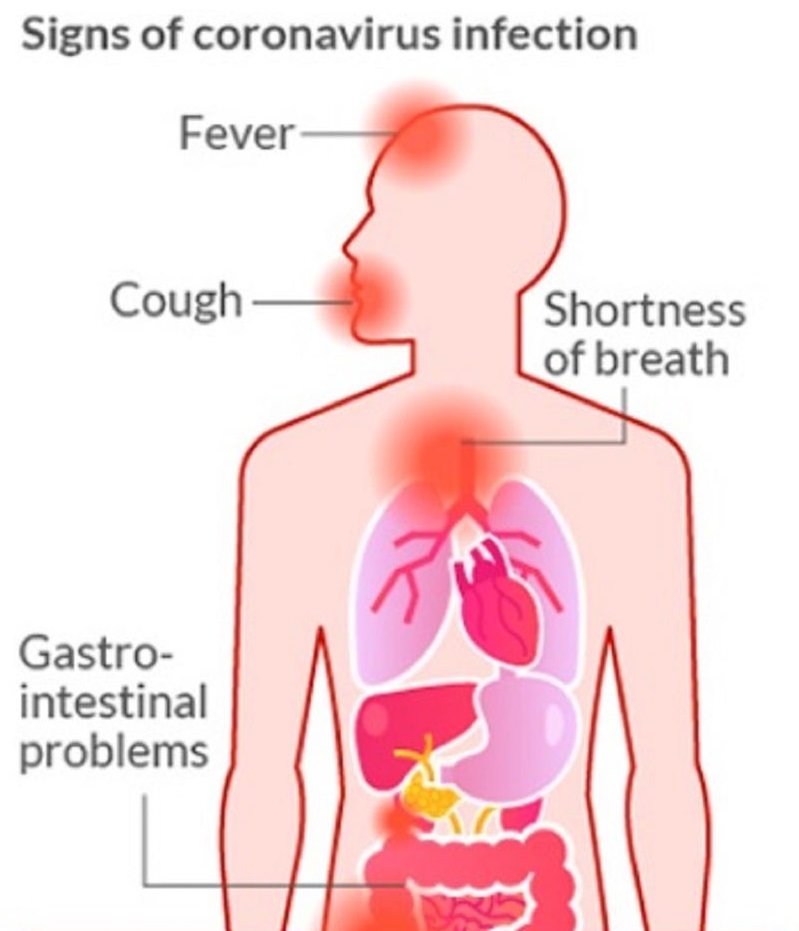
Diagnosis of inflammation of the mammary gland (mastitis)
Usually, mastitis is quite easy to diagnose by the patient herself, but it is still worth contacting a specialist. In the medical center of I. Medvedev, receptions and emergency care are provided 363 days a year, and the treatment is based on minimally invasive and conservative methods.
If the patient has breast pain, treatment begins with diagnosis. It includes:
- examination and palpation
- Breast ultrasound
- if necessary, puncture with histology of the contents of the punctate
Treatment
At first, when mastitis is not yet purulent, but serous in nature, cold compresses, frequent pumping (or feeding), antibiotics can be completely dispensed with if the inflammation lasts longer than a day. Preferred in this case are penicillins, including inhibitor-protected ones. When a woman has inflammation of the breast, the treatment is different, depending on the stage of the process.
If an abscess has already formed, there is no point in prolonging it. Abscess puncture under ultrasound control can resolve the process conservatively, if not, then it is necessary to perform resection of the gland segment in which the abscess lies, with drainage of the cavity.
As for breastfeeding, it is contraindicated if there is pus in the milk, if not, then no restrictions are imposed.
Inflammation of the mammary gland and hyperplasia
Dishormonal processes, with a predominance of estrogens, also cause pain and discomfort in the gland, but, unlike mastitis, this is a non-inflammatory process. Breast hyperplasia treatment is fundamentally different from mastitis, here hormone therapy comes to the fore. Hyperplasia - proliferation of gland tissues with the formation of cysts, swelling of cells, discharge from the nipple. It refers to mastopathy, fibroadenoma and adenomas.
An important role in this disease is played by increased synthesis of prolactin, therefore drugs suppressing its production are widely used, including herbal medicine.