How to prevent breast engorgement
Preventing Breast Engorgement - Lancaster, PA & Elizabethtown, PA: May-Grant Obstetrics & Gynecology
Preventing Breast Engorgement - Lancaster, PA & Elizabethtown, PA: May-Grant Obstetrics & Gynecology
For the first few days after giving birth, breasts remain soft and produce colostrum – the first milk. The amounts may seem small, but colostrum is available in just the right amount for the size of your baby’s stomach. Colostrum is rich in nutrients and immune factors which feed your newborn baby and protect him from diseases.
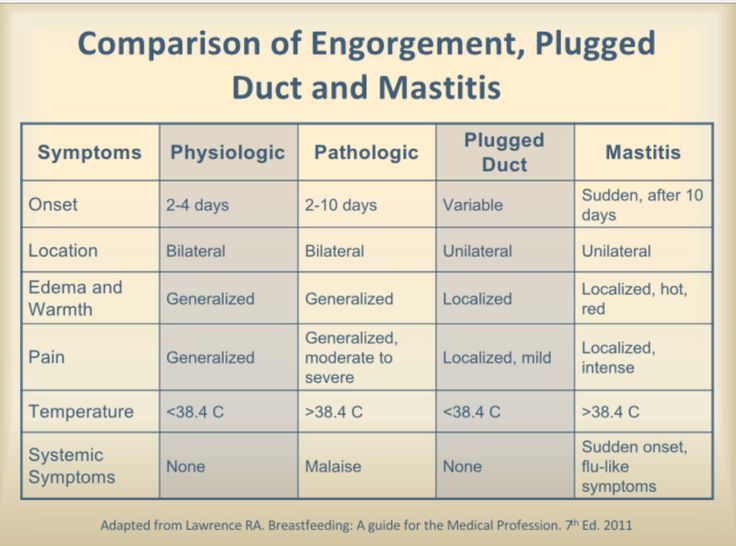
Within 72-96 hours, you will notice changes in your breasts. They will become full, firm, warm, and perhaps tender as milk production increases and colostrum begins to change to mature milk. Breast fullness and mild to moderate swelling are normal. It is caused by milk and extra blood and fluid in the breasts. Your body will use the extra fluids to make milk for your baby. This breast fullness and swelling may last a day or two.
Your breasts will adjust over time, making the exact amount of milk that your baby needs. In cases of extreme or prolonged, painful engorgement, get help from a lactation consultant or healthcare professional. Your baby helps you manage engorgement by removing milk frequently. This means you should breastfeed at least 8-12 times each 24 hours. If your baby is not latching properly or feeding frequently, you may use a breast pump to keep your breasts from becoming overly full. Engorgement reduces the elasticity of the breasts and nipples, leading to more latch problems and sore nipples.
If breast fullness or swelling becomes severe, your breasts may redden and become very painful. If the excessive milk is not removed from the breast, chemical signals are released which can decrease milk production. Unrelieved, prolonged engorgement leads to a lowered milk supply.
A temperature over 100.4 oF or 38 oC may be a sign of an infection. Call your healthcare professional.
Call your healthcare professional.
Prevention
- Begin breastfeeding as soon as possible after birth and frequently thereafter to prevent painful engorgement.
- Avoid early use of bottles and pacifiers while baby is learning to breastfeed.
- Avoid unnecessary supplements, as this can lower milk supply.
- Breastfeeding at least 8-12 times in 24 hours is the most important thing you can do to prevent engorgement.
- Be sure that your baby is latching well. An improper latch can reduce the amount of milk your baby removes from your breasts which can lead to engorgement.
- Let baby nurse until he finishes each breast. Do not limit baby’s time at the breast.
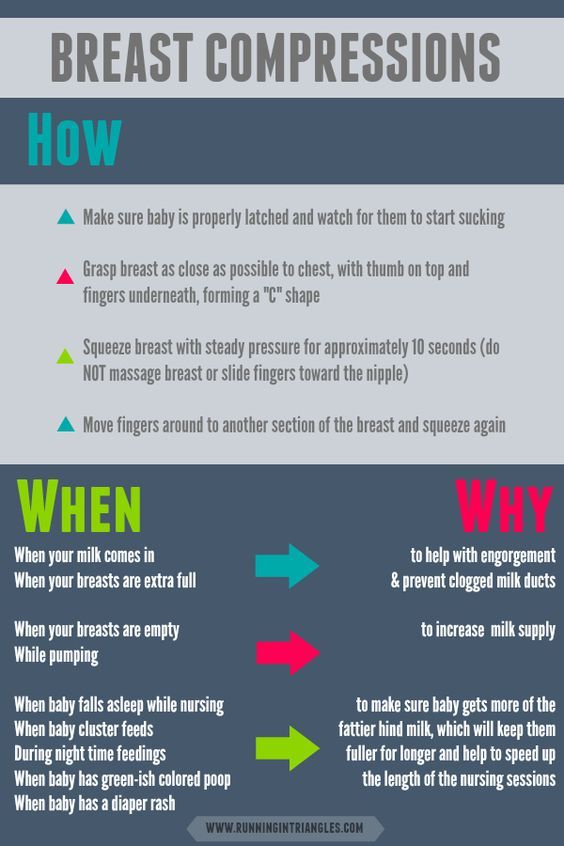
- Gently massage and compress the breast when your baby pauses between sucks.
- This can help drain the milk from the breast.
- Ask for help from your nurse, lactation consultant or healthcare professional so that latch problems are resolved as soon as possible.

- If you must miss a feeding or if baby is not nursing well, use hand expression or a breastpump to remove the milk.
- Seek help if:
- Engorgement becomes severe or you are in pain.
- If you develop a temperature over 100.4 F or 38 C.
- Your baby has trouble latching on.
Treatment for Engorgement
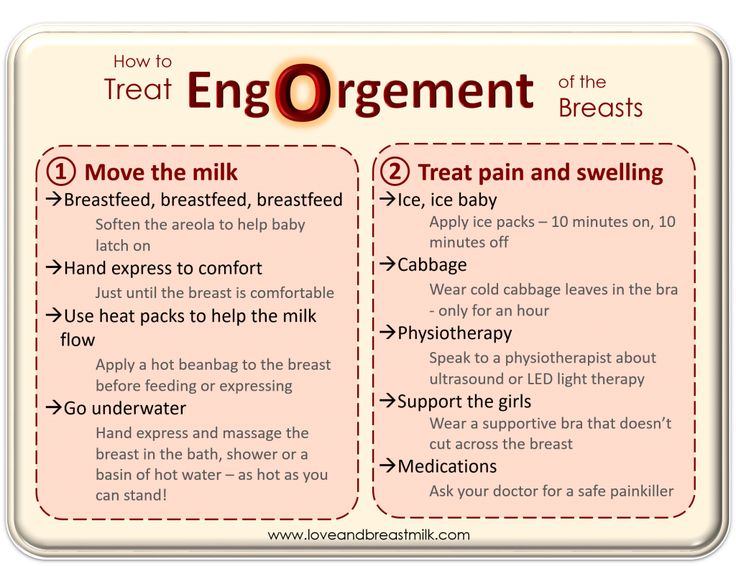
- Use relaxation techniques and gentle breast massage to help improve milk flow and reduce engorgement.
- To start milk flow, use warm moist heat on the breasts for a few minutes, or take a brief warm shower before breastfeeding. Note: Using heat for extended periods of time (over 5 minutes) may make swelling worse.
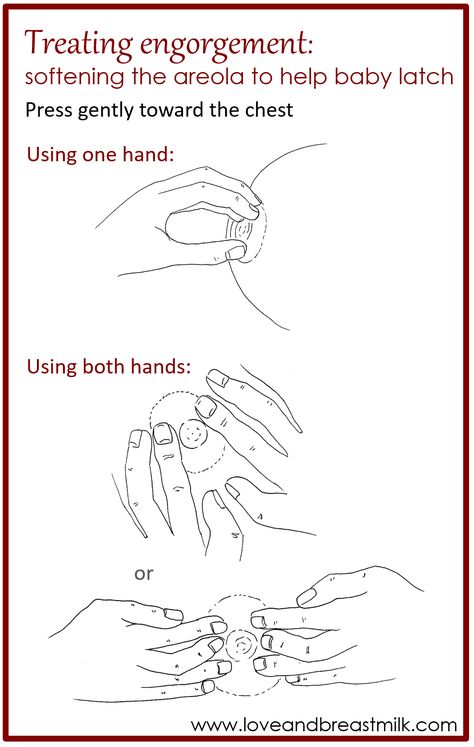
- Hand expression or brief use of a breastpump will soften the nipple and areolar tissue, making it easier for baby to latch well and deeply.
- Pumping once to completely drain the breasts after baby nurses can resolve engorgement for some women. Then return to frequent breastfeeding to manage breast fullness.
- Gently massage and compress the breast when your baby pauses between sucks. This helps drain the breast, leaving less milk behind.
- Although research data is scarce, cabbage leaf compresses have been used for generations to reduce pain and swelling from breast engorgement. Apply clean, whole leaves of cabbage to breasts for approximately 20 minutes between feedings 3 to 4 times a day until engorgement subsides.
- A bag of frozen vegetables wrapped in a thin towel works well as a cold compress. Some women find a cold compress before nursing reduces swelling and helps relieve pain.
- If your breasts are uncomfortably full, express a little milk by either hand expressing or pumping with a quality breastpump on a low setting. Express just enough until you are comfortable; avoid over stimulating. Use manual expression or a quality breastpump on a low setting.
- Ask your healthcare professional about medications such as ibuprofen to reduce pain and inflammation.
- A well-fitted, supportive nursing bra makes some women feel better. Others prefer to go braless during engorgement.
- Fever higher than 100.4 degrees F or severe pain may signal a breast infection. Call your healthcare professional if this occurs.
Causes and Tips for Relief
What is breast engorgement?
Breast engorgement is breast swelling that results in painful, tender breasts. It’s caused by an increase in blood flow and milk supply in your breasts, and it occurs in the first days after childbirth.
If you’ve decided not to breastfeed, you may still experience breast engorgement. It can happen in the first few days after delivery. Your body will make milk, but if you don’t express it or nurse, the milk production will eventually stop.
Breast engorgement is the result of increased blood flow in your breasts in the days after the delivery of a baby. The increased blood flow helps your breasts make ample milk, but it can also cause pain and discomfort.
Milk production may not occur until three to five days postpartum. Engorgement may occur for the first time in the first week or two after delivery. It can also reoccur at any point if you continue to breastfeed.
Not producing enough milk? Here are 5 tips to increase breast milk production.
Certain conditions or events may make you more likely to experience the swollen fullness that’s commonly associated with breast engorgement. These causes include:
- missing a feeding
- skipping a pumping session
- creating an overabundance of milk for the baby’s appetite
- supplementing with formula between nursing sessions, which may reduce nursing later
- weaning too quickly
- nursing a baby that’s ill
- difficulty with latching and sucking
- not expressing breast milk when it first comes in because you don’t plan to breastfeed
The symptoms of breast engorgement will be different for each person. However, breasts that are engorged may feel:
- hard or tight
- tender or warm to touch
- heavy or full
- lumpy
- swollen
The swelling may be contained to one breast, or it may occur in both. Swelling can also extend up the breast and into the nearby armpit.
Swelling can also extend up the breast and into the nearby armpit.
The veins running under the breast’s skin may become more noticeable. This is a result of the increased blood flow, as well as the tightness of the skin over the veins.
Some with breast engorgement may experience a low-grade fever and fatigue in the first days of milk production. This is sometimes called a “milk fever.” You can continue to nurse if you have this fever.
However, it’s a good idea to alert your doctor to your increased temperature. That’s because some infections in the breast can cause fever, too, and these infections need to be treated before they become bigger issues.
Mastitis, for example, is an infection that causes inflammation of the breast tissue. It’s most commonly caused by milk trapped in the breast. Untreated mastitis can lead to complications such as a collection of pus in the clogged milk ducts.
Report your fever and any other symptoms you’ve recently experience to your doctor. They will want you to monitor for signs of an illness or infection so you can seek immediate treatment.
They will want you to monitor for signs of an illness or infection so you can seek immediate treatment.
The treatments for breast engorgement will depend on whether you’re breastfeeding or not.
For those who are breastfeeding, treatments for breast engorgement include:
- using a warm compress, or taking a warm shower to encourage milk let down
- feeding more regularly, or at least every one to three hours
- nursing for as long as the baby is hungry
- massaging your breasts while nursing
- applying a cold compress or ice pack to relieve pain and swelling
- alternating feeding positions to drain milk from all areas of the breast
- alternating breasts at feedings so your baby empties your supply
- hand expressing or using a pump when you can’t nurse
- taking doctor-approved pain medication
For those who don’t breastfeed, painful engorgement typically lasts about one day. After that period, your breasts may still feel full and heavy, but the discomfort and pain should subside. You can wait out this period, or you can use one of the following treatments:
You can wait out this period, or you can use one of the following treatments:
- using a cold compress or ice packs to ease swelling and inflammation
- taking pain medication approved by your doctor
- wearing a supportive bra that prevents your breasts from moving significantly
You can’t prevent breast engorgement in the first days after giving birth. Until your body knows how to regulate your milk production, you may overproduce.
However, you can prevent later episodes of breast engorgement with these tips and techniques:
- Feed or pump regularly. Your body makes milk regularly, regardless of nursing schedule. Nurse your baby at least every one to three hours. Pump if your baby isn’t hungry or you’re away.
- Use ice packs to decrease supply. In addition to cooling and calming inflamed breast tissue, ice packs and cold compresses may help decrease milk supply. That’s because the cool packs turn off the “let down” signal in your breasts that tells your body to make more milk.

- Remove small amounts of breast milk. If you need to relieve the pressure, you can hand express some breast milk or pump a bit. Don’t pump or express too much, however. It could backfire on you, and your body may end up trying to produce more milk to make up for what you just removed.
- Wean slowly. If you’re too quick to stop nursing, your weaning plan may backfire. You could end up with too much milk. Slowly wean your child so your body can adjust to the decreased need.
If you don’t breastfeed, you can wait out breast milk production. In a matter of days, your body will understand it doesn’t need to produce milk and the supply will dry up. This will stop the engorgement.
Don’t be tempted to express or pump milk. You’ll signal to your body that it needs to produce milk, and you may prolong discomfort.
Breast engorgement is swelling and inflammation that occurs in your breasts because of increased blood flow and milk supply. In the days and weeks after giving birth, your body will begin to produce milk.
In the days and weeks after giving birth, your body will begin to produce milk.
Until your body knows how much you need, it may produce too much. This can lead to breast engorgement. Symptoms include hard, tight breasts that are swollen and tender. Regular nursing or pumping can help prevent breast engorgement.
If you continue to experience the painful swelling of breast engorgement, reach out to a lactation consultant or a lactation support group at your local hospital. Both of these resources can help you with your questions and provide support.
Also, call your doctor if the engorgement doesn’t subside in three to four days or if you develop a fever. They’ll ask you to monitor for other signs that may indicate a more serious problem, such as a breast infection.
Breast engorgement symptoms and first aid
search support iconSearch Keywords
Home ›› How to relieve the unpleasant symptoms of breast engorgement
Home ›› How to relieve the unpleasant symptoms of breast engorgement
↑ 0 Top Let's look at all the important issues, including prevention, symptoms, and help with engorgement. Breast engorgement occurs for various reasons. The most common: - Skipping a feeding or pumping session. - Making more milk than the baby eats. - Insufficient outflow of milk (improper latching on to the breast by the baby). - Inflammation. Although engorgement and mastitis may appear similar, they are actually completely different conditions. 3. Make sure the baby is latching on correctly. To learn how to properly breastfeed a baby, a mother can seek advice from a breastfeeding specialist. Proper gripping of the breast during feeding is important for complete emptying of the breast. It also helps prevent other problems such as sore, irritated or cracked nipples. 4. Wean the baby gradually. Philips Avent 2-in-1 thermal pads can both warm and cool your breasts to both stimulate and soothe your breasts after feeding. Mom only needs to place them in a bra for 15-30 minutes before or after feeding (depending on the desired result).
One of the most common breastfeeding problems faced by mothers is breast engorgement.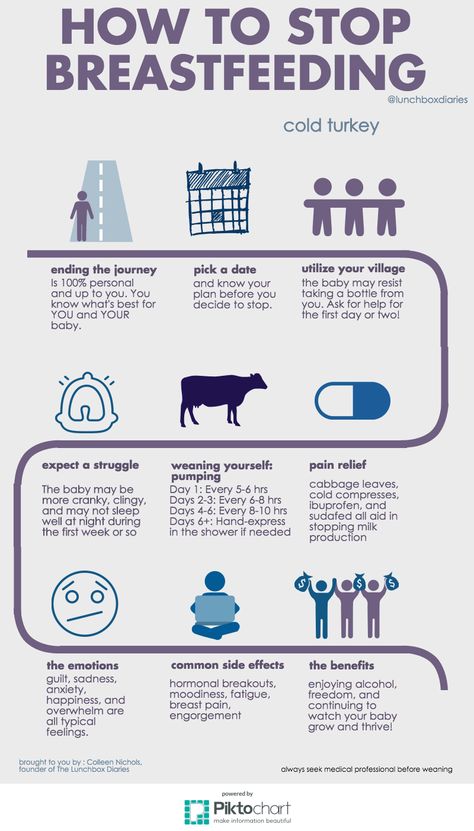 While occasional engorgement while breastfeeding is normal, it can be uncomfortable and lead to other problems if not addressed and dealt with. It is important for mothers to understand what breast engorgement is and how to alleviate it.
While occasional engorgement while breastfeeding is normal, it can be uncomfortable and lead to other problems if not addressed and dealt with. It is important for mothers to understand what breast engorgement is and how to alleviate it.
What is breast engorgement?
Engorgement is an increase in the size of the mammary glands, in which the breast becomes painful and sensitive. This condition is associated with increased blood flow and increased milk production, so it very often occurs during the first few days after childbirth. In addition, engorgement may develop within one to two weeks after childbirth or at any time during breastfeeding. Although this is quite normal during breastfeeding, it can be uncomfortable and sometimes lead to other complications. Therefore, the main thing is to deal with engorgement of the mammary glands immediately when it occurs.
How long does engorgement last?
All women are different, and, accordingly, the duration of this condition may vary. Some experience mild symptoms for only one day, while others may experience this condition for up to two weeks.
Breast engorgement symptoms
Breast engorgement symptoms vary, but the most common are:
 How can a mother determine what exactly she has: engorgement or mastitis? Mastitis is an inflammation of the breast that typically results in fever (>38.5°C) and reddening of the breast, while engorgement is the result of excessive milk production and incomplete emptying of the breast. Engorgement can lead to problems such as blockage of the milk ducts or infection of the mammary glands, so it is important to start treating engorgement at the first sign of engorgement.
How can a mother determine what exactly she has: engorgement or mastitis? Mastitis is an inflammation of the breast that typically results in fever (>38.5°C) and reddening of the breast, while engorgement is the result of excessive milk production and incomplete emptying of the breast. Engorgement can lead to problems such as blockage of the milk ducts or infection of the mammary glands, so it is important to start treating engorgement at the first sign of engorgement.
Prevention of engorgement
There are several ways to prevent this condition. Prevention of breast engorgement in the first days after childbirth can be difficult as the mother's body adapts to the changes. But you can try to avoid it as follows:

Electronic breast pump will help you to comfortably and efficiently express the right amount of milk between feedings, if necessary, or instead of feeding when the mother is away from the baby.  When it's time to stop breastfeeding, moms shouldn't do it abruptly. It is best to wean the baby gradually, gradually reducing the number of daily feedings. This will gradually slow down milk production and prevent breast engorgement.
When it's time to stop breastfeeding, moms shouldn't do it abruptly. It is best to wean the baby gradually, gradually reducing the number of daily feedings. This will gradually slow down milk production and prevent breast engorgement.
Helping with breast engorgement
Breastfeeding with engorgement is not only safe, but necessary to prevent symptoms from getting worse and provide relief. While the body is learning how to produce the right amount of milk, moms can use the Philips Avent bra pads to absorb excess milk and prevent stains on clothes all day long. Philips Avent
Philips Avent
Multifunction thermal pads
SCF258/02
Overall rating / 5
- review review reviews Reviews
-
-{discount-value}
- Pictures It is important to achieve optimal outflow of milk during feedings.
 To stimulate the outflow of milk, during feeding, you can gently massage the breast.
To stimulate the outflow of milk, during feeding, you can gently massage the breast. - Express milk. There are situations when a nursing mother cannot be with the baby during feeding. It is important to empty your breasts by expressing milk to prevent engorgement and other problems.
- When feeding, change positions and alternate breasts. Changing your position while breastfeeding can be beneficial, as it improves the outflow of milk from different parts of the mammary glands. In addition, mothers can change their breasts during one feeding so that the baby can empty both of them.
Remember that minor pain and discomfort is completely natural during breastfeeding, but if these symptoms persist or worsen, the mother should consult a doctor.
Philips Avent Articles & Tips
Baby+ App
Download the app and track your baby's development and growth with trackers and keep those special moments forever.
Download app:
Pregnancy+ app
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
You are about to visit the Philips USA website.
Solving nine breastfeeding problems in the first month
Expert advice on solving major breastfeeding problems in the first month.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is as much a skill as driving a car, and in the first month mother and baby may encounter some obstacles along the way. It takes time and experience to make it familiar to both of you. Solving breastfeeding problems in the first month helps to establish good milk production and increase the duration of breastfeeding in the future. Below you will find tips on how to overcome the main breastfeeding challenges that mothers often face from the end of the first week to the end of the first month after giving birth.
Issue #1. A painful lump appeared in the breast
Lumps and lumps in the breast of a breastfeeding woman can appear for various reasons. One of the most common is blockage of the milk ducts, which results in a hard and painful lump that can become inflamed.
Solutions 1-3
- Massage the inflamed area, especially while breastfeeding or expressing, to clear the blockage.
- Gently apply warm flannel to your breasts or take a warm shower before feeding to relieve discomfort.
- Continue breastfeeding as usual to avoid milk accumulation that can cause mastitis.
- Try to express milk from the inflamed breast after feeding to ensure that it is completely emptied. This will help to remove the blockage and restore the patency of the duct. See what breast pumps* Medela has to offer and choose the right one for you.
- Try ultrasound therapy. If you have repeated blocked ducts, your lactation consultant or healthcare professional may suggest this procedure to help restore milk flow. The procedure is performed by a physiotherapist.
- Call your healthcare provider, if you notice signs of infection (breast redness and tenderness or flu-like symptoms such as fever, aches, malaise and headache) or if you think the lump is not related to breastfeeding .
Problem #2. The breast is red and sore
If one or both mammary glands are red and sore, and this is not due to blockage of the ducts, mastitis, that is, inflammation of the breast tissue, is not excluded. Mastitis is characterized by redness, burning, and soreness of the breasts, combined with flu-like symptoms: You feel hot and cold, your joints ache, and your temperature rises above 38.5 °C (101.3 °F). Seek medical attention immediately if you experience these symptoms. Mastitis needs to be treated as soon as possible, as your condition can worsen in just a few hours. 3
Mastitis is characterized by redness, burning, and soreness of the breasts, combined with flu-like symptoms: You feel hot and cold, your joints ache, and your temperature rises above 38.5 °C (101.3 °F). Seek medical attention immediately if you experience these symptoms. Mastitis needs to be treated as soon as possible, as your condition can worsen in just a few hours. 3
Mastitis can be caused by the following causes:
- untreated blocked ducts,
- Bacteria entering the breast through cracked and damaged nipples,
- Improper breastfeeding,
- long periods between feedings,
- breasts too full,
- wearing a bra that is too tight or that cuts into the skin,
- Abrupt weaning,
- excess milk.
Solutions 3
In addition to seeking medical attention:
- Continue to breastfeed or express milk frequently. Your milk is still safe for your baby.
 Its release will help eliminate blockage of the ducts and prevent painful accumulation of milk. Sudden cessation of feeding or pumping may exacerbate symptoms. After feeding, it is advisable to express any remaining milk.
Its release will help eliminate blockage of the ducts and prevent painful accumulation of milk. Sudden cessation of feeding or pumping may exacerbate symptoms. After feeding, it is advisable to express any remaining milk. - Give the child the inflamed breast first. This way the child can empty it completely. If it hurts too much, start feeding on the healthy breast, and when milk begins to flow, go back to the first one.
- Have a good rest, drink and eat. You need to get enough fluids and good nutrition.
- Massage the sore area under a warm shower or apply a warm flannel or warm pack to clear blockages and relieve symptoms before feeding or pumping.
- Apply a cooling pack after feeding, , to reduce inflammation.
Problem #3. My strength is running out
Breastfeeding in the first weeks can be very tiring and seem endless. The baby will ask for a breast every few hours, day and night, and you have not yet grown stronger after giving birth.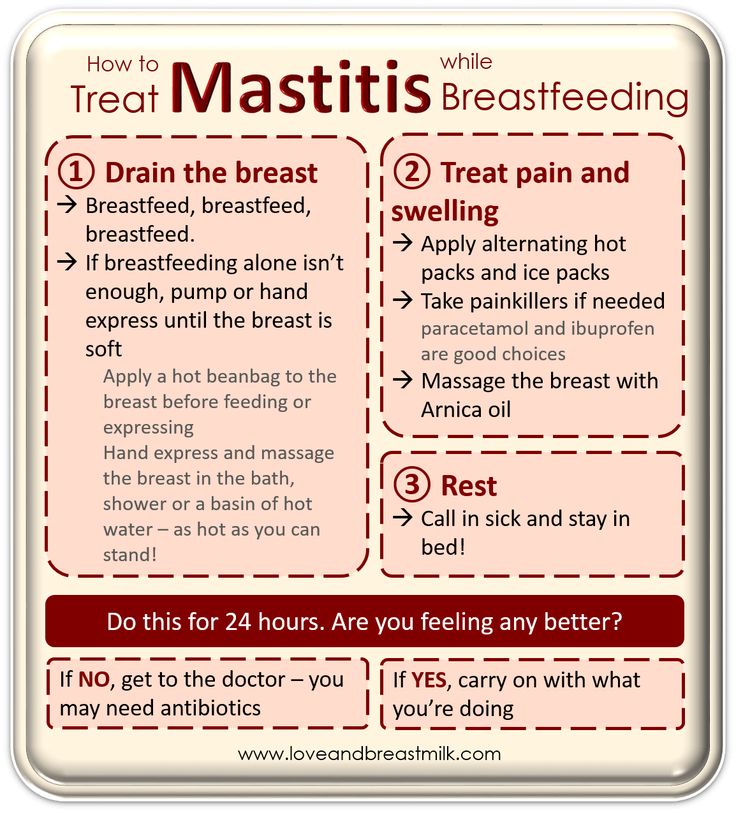
Solutions
- Take care of yourself. This may be easier said than done when you have a newborn in your arms, but still try to get as much rest as possible, eat healthy and regular meals, and drink plenty of water. Do not refuse the help of your partner, relatives and friends, or even hire an assistant if you can afford it.
- Feed lying down. This will allow you to relax and reduce stress on sore spots, stitches or c-section scars.
- Do not skip feedings. Your partner may offer to bottle feed your baby while you are resting. However, despite this temptation, it should be remembered that milk production is best established in the first four weeks through breastfeeding. When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding.
Problem #4.
 How can I increase breast milk production?
How can I increase breast milk production? It's easy to question whether your breastmilk supply is adequate, especially when your baby has developmental spikes between the third and fourth weeks. It may seem to you that the child asks for breasts more often because he does not have enough milk. However, if the number of wet and soiled diapers doesn't change—see Breastfeeding: What to Expect in the First Month—the baby is likely to breastfeed more often to calm down. The baby is surrounded by many new sounds and images that are easy to get tired of, and at the breast he feels safe. 4
Solutions 4.5
- Do not try to supplement your baby with formula, unless doctors are concerned about weight gain or fluid loss. Continue breastfeeding your baby. This will help naturally increase breast milk production.
- Do not feed on a schedule. Feed your baby on demand. Thus, the production of breast milk will adapt to his needs.
- Use the breast pump, , to help increase breast milk production while continuing to breastfeed.
Problem #5. I have too much milk
Hyperlactation, or too much milk, can also be difficult for you and your baby. You may experience discomfort from swollen and leaking breasts, and your baby may have difficulty latch-on, choke on the milk flowing too fast, and be unable to empty the breast properly. 6
Solutions
- Express some breast milk at the beginning of a feed to reduce the force of the flush. Don't pump too much as this can aggravate the situation - pump only as much as needed to ease the discomfort. Try hand pumping or use a breast pump (check out the Medela* breast pump range and choose the right one for you).
- Use the towel or pad to soak up excess milk, or place the milk collection pad** on the other breast while you breastfeed first.
- The child must feel supported. Hold him firmly (this gives a sense of security) and in a comfortable position so that he can turn his head. Talk to the baby during the first rapid flush, then he will not be frightened by surprise and will not push the breast.
- Contact a lactation consultant or health care professional who will monitor you and suggest single-sided feedings or hourly breast changes (“breast duty”) to normalize your milk supply.
- Be patient . Problems with milk production usually go away after a few weeks.
Problem #6. I have different breasts!
You have noticed that the baby prefers one breast, or that one breast produces more milk than the other, and as a result, the mammary glands have acquired a different size and shape. This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks.
If this makes you uncomfortable, try the following tricks.
Solutions
- Offer less demanded breasts first during feeding as babies usually suckle more vigorously at the beginning of a feed.
- Use the breast pump to increase breast milk production in the smaller breast.
- Don't give up on bigger breasts. Breastfeeding should continue with fuller breasts to avoid blocked ducts and mastitis.
- See a doctor. Sometimes an ear infection is the reason for a baby to latch on only one side. However, some positions may cause him discomfort, so try to keep the child more upright. In addition, a breast infection can change the taste of milk and cause milk to be rejected as well.
Issue #7. A blister has appeared on the nipple
With frequent feeding, sometimes painful friction occurs, and a blood bubble may appear on the breast,
nipple or areola. 7
7
Solutions
- Ask a lactation consultant or specialist to check the baby's latch on. A shallow grip can cause blistering of the nipples and areolas.
- Talk to your doctor about what medication you can take to relieve pain if needed.
- Try other feeding positions to avoid pressure on the painful area.
- Lubricate inflammation with pure lanolin.
- Use Breast Pads** to avoid rubbing your blister with clothing and help it heal faster with air circulation, or try cooling hydrogel pads** to help relieve pain and promote healing.
- Try expressing milk. Using a breast pump can be an alternative way to get breast milk without bladder irritation. Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel.
- Do not pierce the vial as this may lead to infection.
- Seek medical attention, if the problem persists and causes you pain.
Problem #8. Painful white spot on the nipple
When the opening of the milk duct is blocked by milk or a thin layer of skin grows over it, a small white or yellowish spot may appear on the tip of the nipple. For some, these blocked ducts, sometimes called milk vesicles or blisters, cause pinpoint pain, especially during feeding or pumping. Others do not experience any discomfort. White blisters may persist for several days or weeks until the skin breaks and hardened milk comes out. 8
Solutions
- Follow the tips above to solve friction bubble problems.
- Remove the blockage, if you see that the milk cork is starting to bulge. Try to squeeze it out very gently with clean nails.
- Continue breastfeeding or pumping, to clear the milk duct.
 If the milk duct clears during feeding, it will not harm the baby in any way.
If the milk duct clears during feeding, it will not harm the baby in any way. - Apply hot wet flannel to the bottle just before feeding or pumping. This will help open the blocked duct. You can also try rubbing the area quickly with a clean, damp cloth.
- Hand express some milk before feeding, trying to push out hardened milk clots. If this does not help, feed the baby or express milk as usual. Repeat several times a day.
- Soak a cotton swab with olive oil and place it in the bra, pressing it against the bubble nipple. This will help soften the skin.
- Seek medical attention, if problem persists. Your doctor may remove the plug with a sterile needle. This should be done immediately after feeding, when the bubble is as inflated as possible.
Issue #9. My nipples hurt while breastfeeding
At the start of breastfeeding, my nipples may become more tender, sore, and even inflamed, but this usually goes away after a few days. If your baby's latch is checked by a specialist and the inflammation persists or the nipples hurt with every feeding, you may need medical attention to resolve this problem. 2.7
If your baby's latch is checked by a specialist and the inflammation persists or the nipples hurt with every feeding, you may need medical attention to resolve this problem. 2.7
The following symptoms and signs that appear on one or both breasts during or after feeding may indicate a bacterial infection or thrush:
- burning, itching or moderate to severe pain in the nipples
- nipple pain aggravated by contact with clothing,
- nipple pain persists despite attempts to attach baby differently,
- nipples hurt to touch,
- stitching, shooting, burning or deep aching pain,
- chest pain during feeding and almost an hour after,
- hot pink nipples,
- discoloration and texture of the areola (hot pink color, darkening, dryness or peeling),
- white rash on chest or areola.
Also check if your child has the following symptoms and signs:
- thick white patches or coating on the tongue,
- white indelible spots on the cheeks,
- bright red spotted rash on buttocks not helped by diaper rash creams.

Solutions 7
- Seek medical attention. He will most likely suggest testing for infections to make a diagnosis. Bacterial and fungal (yeast) infections are treated differently, so appropriate treatment should be started as soon as possible. There are other reasons that can cause similar nipple pain, such as eczema, psoriasis or vasospasm (narrowing of the blood vessels) in the mother and problems with latch or tongue frenulum in the child. Therefore, it is very important to make an accurate diagnosis.
- Strict hygiene. Wash hands before and after feeding and applying any medication, and after changing diapers. Change bra pads regularly, wash bras, tank tops and towels in high temperature water, thoroughly wash breast cups and anything your baby puts in her mouth, such as nipples.
- Let the nipples dry after feeding, as all infections love a warm and humid environment.

- See your doctor again if there is no improvement after a few days. Do not let the problem run its course, otherwise the situation may worsen.
Related materials. Breastfeeding: what to expect in the first month
Breastfeeding: what to expect after the first month
Breastfeeding problems after the first month
Literature
Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med. 2009;4(2):111-113.- Breastfeeding Academy Protocol Committee, "AVM Clinical Protocol #20: Breast engorgement." Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
2 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe and Frauenheilkunde . 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding.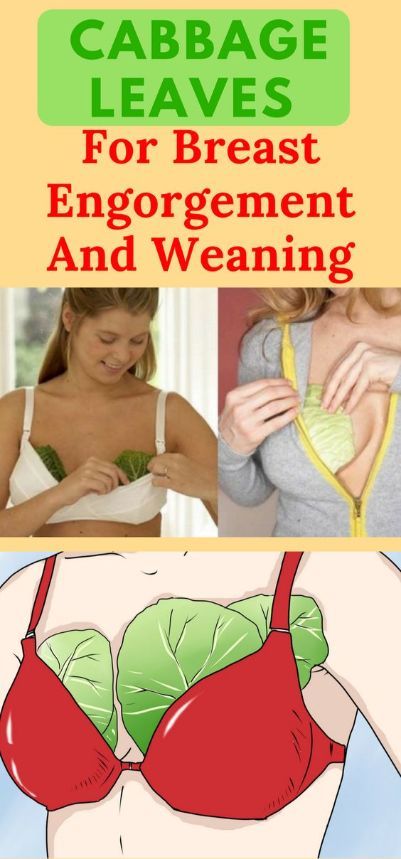 Geburtskhilfe und Frauenheilkünde. ABM Clinical Protocol# 4: Mastitis , Revized 2014. . H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
Geburtskhilfe und Frauenheilkünde. ABM Clinical Protocol# 4: Mastitis , Revized 2014. . H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
4 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". F Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
5 Amir L. Breastfeeding managing ‘supply’ difficulties. Aust fam physician . 2006;35(9):686. - - Amir L., "Breastfeeding: problems of 'supply'. Aust fam physical.