Pregnancy pain relief options
What Pain Meds Can I Take?
Written by WebMD Editorial Contributors
Reviewed by Nivin Todd, MD on January 20, 2021
In this Article
- Acetaminophen
- NSAIDs
- Opioid Painkillers
When you’re pregnant, you’re not immune to aches and pains. In fact, you might feel some new twinges that are caused by hormone changes and your growing belly.
Your doctor has likely told you that you shouldn’t take any medicine without checking with them first. You might wonder: Do you need to check with them even if you just want to pop a pain reliever?
The simple answer is: yes. You should ask your doctor before you take any medication, even if it’s just an over-the-counter pill designed to relieve pain. Such medicine may seem harmless enough, but the rules change when you’re carrying a baby.
Some medicines aren’t safe to take when you’re pregnant -- even over-the-counter ones.
Acetaminophen
This common over-the-counter medication may be your pain reliever of choice if you have a fever, a headache, or joint or muscle pain. You can buy acetaminophen over the counter by itself or in combination with other medicines. Your doctor can also prescribe it at higher doses, alone, or combined with other medications as well.
Most pregnant women can take acetaminophen if their doctor gives them the thumbs-up. It’s the most common pain reliever that doctors allow pregnant women to take. Some studies have found that about two-thirds of pregnant women in the U.S. take acetaminophen sometime during their nine-month stretch.
Just steer clear of acetaminophen if you’re allergic to it, if you have liver problems, or if your doctor says it’s not safe for you.
Even if your doctor says it’s OK to take acetaminophen, take as little of it as you can for as short a time as possible. Acetaminophen isn’t linked to big problems like miscarriage or birth defects, but studies suggest that babies could later feel the effects.
Some research suggests that taking acetaminophen daily for long periods (28 days or longer) could put your baby at greater risk of mild developmental delays or attention deficit hyperactivity disorder (ADHD).
Other research has shown that taking acetaminophen daily, or almost daily, during the second half of your pregnancy increases your baby’s odds of wheezing or having asthma.
None of the research proves that acetaminophen causes these problems and further studies are necessary to understand the link.
NSAIDs
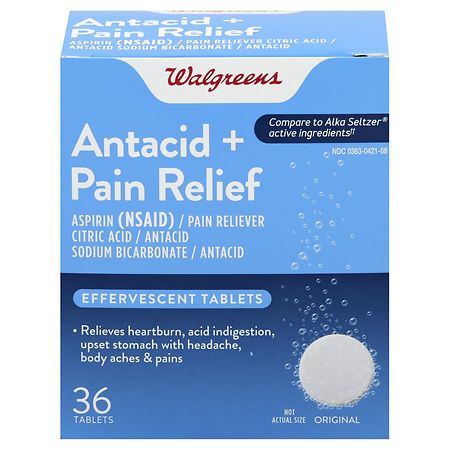
You may have taken ibuprofen plenty of times in your adult life, but your doctor will likely ask you to take something else to treat fever, headaches, and muscle pain when you’re pregnant. Non-steroidal anti-inflammatory drugs (NSAIDs) are sold over the counter and by prescription, but there are safer choices for pregnant women.
Some studies have found that taking NSAIDs (ibuprofen, naproxen, aspirin, celecoxib) during the early part of pregnancy may increase your risk of miscarriage.
Research has also looked at the connection between NSAIDs and birth defects. Some studies suggest that there may be a slight increase in the chances of a problem with your baby’s heart or gastrointestinal (digestive) system if you take NSAIDS early in your pregnancy.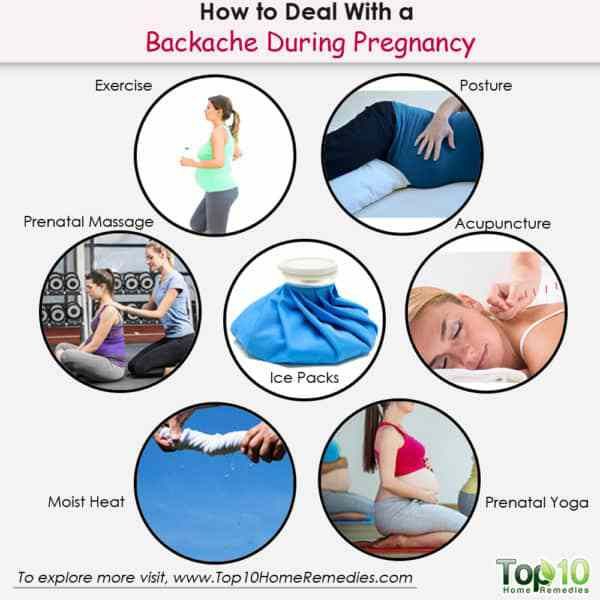
But more research is needed to prove that NSAIDs cause these problems. Even though the link hasn’t been proven, your doctor may suggest you take acetaminophen instead.
NSAIDs are definitely not recommended during the last 3 months of your pregnancy because they can cause a blood vessel in your baby’s heart to close before it should. If this happens, it can cause high blood pressure in your baby’s lungs.
Taking NSAIDS can also make it harder for you to go into labor or can reduce the level of amniotic fluid that surrounds your baby in your womb. For these reasons, you should only use NSAIDs under your doctor’s supervision to ensure no problems crop up.
Opioid Painkillers
Opioids (codeine, morphine, oxycodone) are a class of strong medicines that doctors can prescribe to treat pain. They’re also the most commonly abused prescription medications in the U.S.
Some studies suggest that opioid use can increase your odds of having a baby with certain birth defects, such as a heart problem.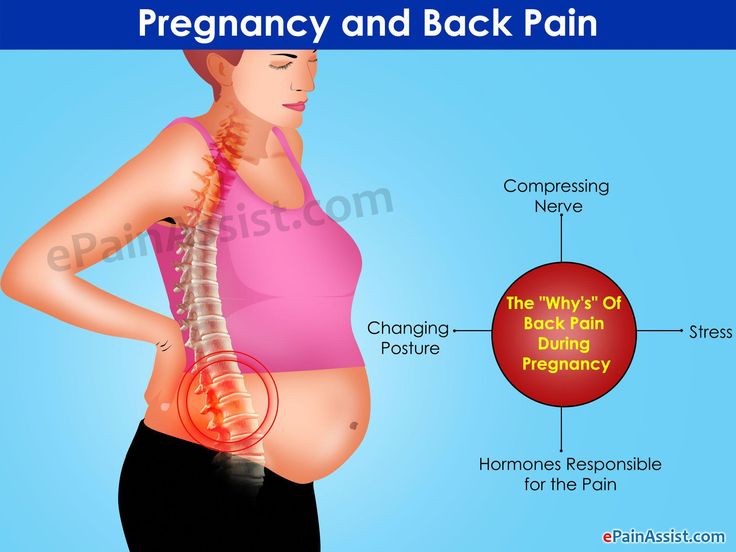 They also may raise your chances of premature birth, preterm labor, or even having a stillbirth.
They also may raise your chances of premature birth, preterm labor, or even having a stillbirth.
If you already take opioids, your doctor may not want you to stop taking them once you’re pregnant, because a sudden stop could harm your health or your pregnancy. Instead they may want to reduce the amount of medicine you take at a gradual pace to prevent any withdrawal symptoms.
But if you take opioids during your pregnancy, your baby will be exposed to them in the womb and could become addicted. They will go through withdrawals from them after they're born. This is called neonatal abstinence syndrome, or NAS. NAS can be serious, and could cause your baby to be too small or have breathing problems, even if you take the opioid exactly as prescribed.
Childbirth - pain relief options
Actions for this page
Summary
Read the full fact sheet- Childbirth is usually a painful experience.

- There is a range of options for pain relief in labour including non-medical techniques and medical pain relief options such as nitrous oxide, pethidine and epidural anaesthesia.
- Particularly if you are having your first baby, consider all options and be flexible.
- If you planned to give birth without using pain relief, but find the labour pains are overwhelming, don’t be reluctant to ask the doctor, nurse or midwife for pain relief.
Labour and childbirth is usually a painful experience and women vary in their response to it. Some women are keen to avoid drugs or other medical interventions while others are happy to consider all available options. For a woman having her first baby, the experience of labour (and her reaction to it) is unpredictable.
For this reason, it is a good idea to be aware of the options for pain relief that are available and to know something about the different methods. You may have a plan for how you hope to manage your labour, but it is best to be prepared to be flexible.
You may have a plan for how you hope to manage your labour, but it is best to be prepared to be flexible.
Non-medical pain relief options for childbirth
Research suggests that adequate preparation can help to reduce pain or at least modify the perception of pain and reduce anxiety, which can help you to better cope with labour. There are several non-drug pain relief options:
- Being in good physical condition is important. Exercise gently and regularly throughout your pregnancy, avoid cigarettes and alcohol, and eat a healthy, balanced diet.
- Knowing what to expect during the various stages of labour can help reduce anxiety. Antenatal classes are strongly recommended.
- Breathing techniques may help you to ‘ride the waves’ of each contraction.
- Constant, close support from your partner (or a trusted friend or loved one) for the duration of labour can reduce anxiety.
- Using distractions like music can help to take your mind off the pain.
- Hot or cold packs, massage, a warm shower or immersion in a warm bath, and keeping active may all be helpful.
- Hypnosis, acupuncture and acupressure are areas in which there has been little research but these may be considered also.
Transcutaneous electrical nerve stimulation (TENS)
TENS is a technique in which nerves in the lower back are stimulated using a small hand-held device controlled by the woman. It has no known side effects for mother or baby and many women find it helpful either alone or in combination with other methods of pain relief.
Medical pain relief options for childbirth
The three main medical pain-relieving options for labour include:
- Nitrous oxide
- Pethidine
- Epidural anaesthesia.
Nitrous oxide
Nitrous oxide, known as ‘laughing gas’, is mixed with oxygen and administered to the mother through a face mask or a tube held in the mouth. The gas takes a few seconds to work, so it is important to breathe from the mask as soon as a contraction starts.
Nitrous oxide doesn’t stop the pain entirely, but takes the ‘edge’ off the intensity of each contraction. Many women prefer nitrous oxide because it allows them direct control – you can hold the mask yourself and take deep breaths whenever you feel the need.
Nitrous oxide doesn’t interfere with contractions and it doesn’t linger in either the woman’s or the baby’s body.
Possible problems with using nitrous oxide include:
- Nausea and vomiting
- Confusion and disorientation
- Claustrophobic sensations from the face mask
- Lack of pain relief – in some cases, nitrous oxide doesn’t offer any pain relief at all (this applies to around one-third of women).
Pethidine
Pethidine is a strong pain reliever (related to morphine and heroin), usually injected directly into a muscle in the buttock. It may also be administered intravenously (directly into a vein). Depending on various factors, the effect of pethidine can last anywhere from two to four hours. Pethidine can make you feel sick, so anti-nausea medications are usually administered at the same time.
Pethidine can make you feel sick, so anti-nausea medications are usually administered at the same time.
Possible problems with pethidine for the mother include:
- Giddiness and nausea
- Disorientation and altered perception
- Respiratory depression (reduced breathing)
- Lack of pain relief, in some cases.
Possible problems with pethidine for the baby include:
- The unborn baby is exposed to the drug via the umbilical cord and may experience respiratory depression at birth, particularly if several doses are given or the baby delivers soon after a pethidine injection. This effect can be reversed by an injection given to the baby.
- The baby’s sucking reflex may also be depressed, as well as other normal reflexes. Debate persists over the effects of pethidine on newborns.
Epidural anaesthesia
Epidural injections are the most effective pain relief available. They are used for vaginal births and also for caesarean sections, because they allow the mother to stay awake and alert during the baby’s birth. Anaesthetic is injected into the lining of the spinal cord through the back, which makes the mother feel numb from the waist down. Your baby’s heart rate will be monitored continuously.
Anaesthetic is injected into the lining of the spinal cord through the back, which makes the mother feel numb from the waist down. Your baby’s heart rate will be monitored continuously.
Possible side effects and complications of epidural anaesthesia include:
- The anaesthesia may not be complete and you may still experience some pain. This may require the procedure to be repeated.
- After the epidural has been inserted, your blood pressure may drop, causing you to feel faint and nauseated. This may also cause stress to your baby. This is treated by giving intravenous fluid.
- An epidural often causes some muscle weakness in the legs, so women who have had an epidural anaesthetic may be confined to bed.
- The lack of sensation in the lower body means that you will not be able to tell when you need to urinate. A urinary catheter will be inserted in most cases.
- Epidurals can lengthen the second stage of labour.
- The likelihood of having a normal vaginal delivery is reduced.
- If you are unable to push effectively, due to altered sensation and reduced muscle strength, the baby may have to be delivered by forceps or vacuum cup.
- Around one per cent of women experience headache immediately following the procedure.
- Some women experience itchiness after having an epidural. This can usually be effectively treated using antihistamines.
- Some women experience pain or tenderness where the epidural was injected.
- Around one in 550 women experience ongoing patches of numbness on the back near the injection site.
- Very rare complications include infection, blood clots and difficulty breathing.
An epidural does not:
- Increase the length of the first stage of labour
- Increase the likelihood of a caesarean section
- Cause long-term backache.
Where to get help
- Your doctor
- Obstetrician
- Midwife
Things to remember
- Childbirth is usually a painful experience.
- There is a range of options for pain relief in labour including non-medical techniques and medical pain relief options such as nitrous oxide, pethidine and epidural anaesthesia.
- Particularly if you are having your first baby, consider all options and be flexible.
- If you planned to give birth without using pain relief, but find the labour pains are overwhelming, don’t be reluctant to ask the doctor, nurse or midwife for pain relief.
- Continuous support for women during childbirth, 2007, Cochrane Database of Systematic Reviews, Issue 2. More information here.
- Using water for pain relief during labour, 2007, The Royal Women’s Hospital, Melbourne.
- Epidural information, 2013, The Royal Women’s Hospital, Melbourne.
- Pain relief during labour and birth, Women’s and Children’s Health Network, Department of Health, South Australian Government. More information here.
- Epidural anaesthesia – side effects, 2011, NHS Choices, UK.
 More information here.
More information here. - Epidural anaesthesia, NHS, UK. More information here.
This page has been produced in consultation with and approved by:
This page has been produced in consultation with and approved by:
Give feedback about this page
Was this page helpful?
More information
Content disclaimer
Content on this website is provided for information purposes only. Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional. The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances. The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
Reviewed on: 31-08-2014
Pregnancy pain reliever
- home
- Services
- Dentistry for pregnant women
- Pain reliever during pregnancy
Can I take painkillers during pregnancy if I have a toothache?
Dental problems during pregnancy occur due to hormonal changes and changes in the body. Often there is a deficiency of various substances, minerals, in the first place - calcium, on which the health of the teeth depends. Also, pathogenic microorganisms multiply more actively in the mouth of a pregnant woman. All this often leads to dental diseases and pain.
Also, pathogenic microorganisms multiply more actively in the mouth of a pregnant woman. All this often leads to dental diseases and pain.
When it is not possible to see a doctor immediately after the onset of pain, it is necessary to take painkillers. This is necessary, because due to acute and constant pain, a pregnant woman experiences stress, and this negatively affects the fetus. However, there are many nuances, and not every drug can be used by a future mother.
What diseases do pregnant women need painkillers for?
- Caries, medium and deep.
- Pulpitis.
- Periodontitis.
- Gingivitis.
- Inflammation of the mucous membranes in the oral cavity caused by various factors.
Which pain medications can be taken while pregnant?
It is best to consult a dentist before becoming pregnant in order to rule out situations where pain medication may be required. We invite you to contact the doctors of the Planet of Childhood clinic in Moscow to undergo a complete dental examination and receive individual recommendations.
When buying any medication, read the package leaflet carefully. The instructions will always tell you exactly how you should or should not use this drug during pregnancy. Also pay attention to other contraindications.
Here are some painkillers that pregnant and breastfeeding women are usually allowed to take:
- Papaverine - temporary relief, usually for mild pain;
- Paracetamol - relieves inflammation and fever that may occur due to dental disease;
- No-shpa - relieves pain;
- Ibuprofen - effective analgesic, but contraindicated in the third trimester;
- 1-Riabal is a gentle pain reliever.
Even after choosing a remedy from this list, you must first contact your doctor for advice. In any case, all these means cannot be called potent. Although they reduce pain or eliminate them for a while, you still need to come to the dental clinic as soon as possible with a toothache.
In addition to pills, special baby gels, which are usually used during teething in babies, can be a way out for the expectant mother. These gels relieve pain and itching.
These gels relieve pain and itching.
Chlorhexidine and Miramistin sprays are another option. These drugs are not absorbed into the blood, they affect only those places on which they are applied.
A cold compress can be used for swollen cheeks. Warm compresses are prohibited.
An alternative to tablets, sprays and gels is rinsing with special antiseptic preparations. You can prepare an antiseptic yourself. To do this, pour a teaspoon of soda and a teaspoon of salt into a glass of water. Mix the mixture thoroughly, then use for rinsing. Thanks to this simple recipe, pathogenic microbes in the mouth will multiply more slowly, and the pain will decrease.
Anesthesia in a gentle beriod
Answers questions
Sergeev Viktor Mikhailovich
dentist of the network of dental clinics "Smile"
Pregnancy is a long-awaited, and as doctors say, a completely normal physiological state of the female body. However, it is fundamentally different from the usual state of the female body, primarily by changing the hormonal background. The best motto that every woman should be guided by in anticipation of a child is better to prevent than to cure.
The best motto that every woman should be guided by in anticipation of a child is better to prevent than to cure.
What should I do if I have a toothache during pregnancy?
Unfortunately, there is no “magic pill” or “guaranteed remedy” for caries. Dental caries is a multifactorial, infectious disease.
The normal growth and development of the fetus during pregnancy depends on the health of the teeth of the expectant mother. The threat posed by untreated caries should not be underestimated. It is important to visit a dentist when planning a pregnancy, to cure foci of infection.
And during pregnancy, pay more attention to oral hygiene and good nutrition of the expectant mother.
If you still have a toothache during pregnancy, you should contact your dentist as soon as possible.
Therefore, in order for dental treatment in pregnant women to be limited to regular check-ups at the dentist, it is necessary to carefully maintain oral hygiene.
Unified reference telephone
+7 384 234-44-19
Painkillers for pregnant women
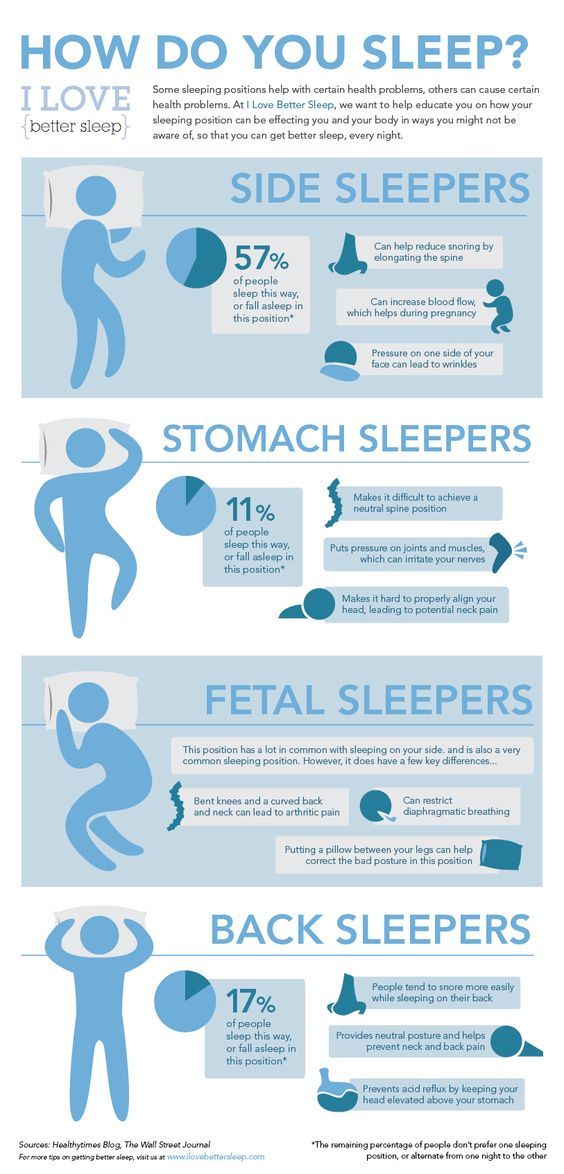
Let's say right away that the safest drugs are Paracetamol and Ibuprofen . Here it should only be noted that Ibuprofen is contraindicated in pregnant women in the 3rd trimester (in the 1st and 2nd trimesters it is approved for use). Pain tablets for pregnant women, see Chart #1 below.
Taking medications, dosages, duration of administration - you need to coordinate with your doctor. Because there may be certain conditions and chronic diseases in the mother's body that can make these drugs less safe than they are, for example, for a healthy pregnant woman.
Prenatal antibiotics
Can pregnant women drink an antibiotic, and which antibiotics can pregnant women take?
In the treatment of pregnant women, the drugs of choice are beta-lactam antibiotics, for example, a group of penicillins. In Table No. 1 you will see a list of the safest antibiotics (safety category "B").
In Table No. 1 you will see a list of the safest antibiotics (safety category "B").
Antibiotics of the following groups are prohibited for use: tetracyclines and fluoroquinolones. With caution (undesirable, but in some cases necessary) - sulfonamides and some representatives of aminoglycosides.
IMPORTANT: It is best to discuss this with your attending OB/GYN before starting antibiotics.
Anesthesia during lactation
Medicines and breastfeeding
When deciding on the appointment of the drug
to a nursing woman, the doctor takes into account:
- Drug toxicity index
- Dose and duration of administration of the drug
- Breastfeeding age
- Amount of milk consumed
- Effect of the drug on lactation
Ways to reduce the amount of medication
in the mother's milk to the baby
- Suspension of breastfeeding
- Refusal to feed the child during peak plasma concentrations of the drug
- Taking the drug during the child's longest sleep
What antibiotics can be used for pregnant and lactating women, as well as painkillers and injections for dental treatment - are listed in Table No.1 .
Table 1.
Medicines used in dentistry during pregnancy and lactation.
| Medicine | Pregnancy risk category * | Risk category for lactation * |
|---|---|---|
| Local anesthetics (injections for dental treatment) | ||
| Lidocaine | In (maybe) | Safe |
| mepivacaine | C (unwanted) | Safe |
| Analgesics | ||
| Paracetamol | In (maybe) | Safe |
| Ibuprofen (1st and 2nd trimesters) | In (maybe) | Safe |
| Ibuprofen (3rd trimester) | D (absolutely impossible) | Safe |
| Antibiotics | ||
| Penicillins | In (maybe) | Safe |
| Cephalosporins | In (maybe) | Safe |
| Clindamycin | In (maybe) | Safe |
| Metronisazole | In (maybe) | Safe |
* - in accordance with the classification of the Food and Drug Administration (FDA, USA). Description of risk categories "B", "C", "D" is given below Description of risk categories "B", "C", "D" is given below | ||
What are drug safety categories?
Today, fetal safety of drugs is classified according to recommendations from the FDA.
This classification was developed in the USA and is generally followed by physicians in all countries. You can see the drugs of choice for emergency dental interventions in pregnant and lactating women in Table No. 1 .
The level of drug safety is determined by risk categories, which are denoted by Latin letters A, B, C, D:
-
Category B drugs - Considered to be very safe.
-
Category C drugs - not recommended.
-
Category D drugs - dangerous to use (use only if the possible benefit outweighs the possible harm, and if there is no safer equivalent drug).
Anesthesia for high and low blood pressure
If the patient has high blood pressure or cardiac dysfunction (heart disease, heart rhythm disturbances, heart failure, etc.