Blighted ovum medication
Treatment, Symptoms, Causes, and Outlook
Blighted Ovum: Treatment, Symptoms, Causes, and OutlookMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Corey Whelan on December 13, 2017
What is a blighted ovum?
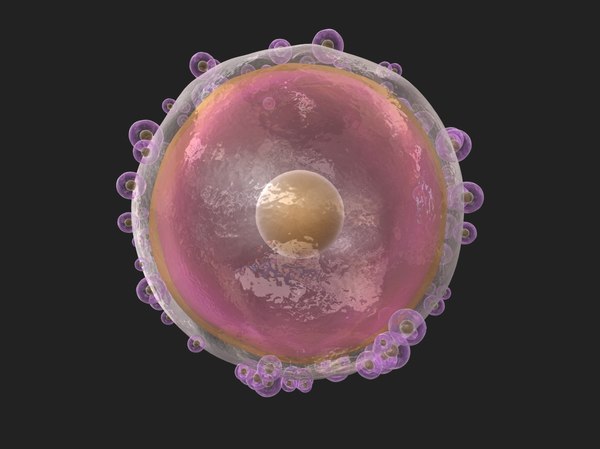
A blighted ovum is a fertilized egg that implants itself in the uterus but doesn’t become an embryo. The placenta and embryonic sac form, but remain empty. There’s no growing baby. It’s also known as anembryonic gestation or anembryonic pregnancy.
Even though there’s no embryo, the placenta still produces human chorionic gonadotropin (hCG). This is a hormone designed to support pregnancy. Blood and urine pregnancy tests look for hCG, so blighted ovum can result in a positive pregnancy test even though the pregnancy isn’t actually proceeding. Pregnancy-related symptoms, such as sore breasts and nausea, may also occur.
A blighted ovum eventually leads to miscarriage. It’s not able to turn into a viable pregnancy.
What are the symptoms?
A blighted ovum sometimes ends before you realize you’re pregnant. When this happens, you may just think you’re having a heavier-than-normal menstrual period.
A blighted ovum may have the same symptoms associated with pregnancy, such as:
- a positive pregnancy test
- sore breasts
- a missed period
As the pregnancy ends, symptoms may include those of miscarriage. These can include:
- vaginal spotting or bleeding
- abdominal cramping
- disappearance of breast soreness
Pregnancy tests measure hCG levels, so a blighted ovum can continue to result in positive test results before the tissues are passed.
What are the causes?
This condition isn’t caused by anything that you did or didn’t do, either during or before your pregnancy.
The exact cause of blighted ovum isn’t known. It’s thought to be caused by chromosomal abnormalities occurring within the fertilized egg. This may be the result of genetics, or of poor-quality eggs or sperm.
Blighted ovum may be linked to abnormalities within chromosome 9. If you have repeated blighted ovum pregnancies, consider talking to your doctor about a chromosomal analysis of your embryos.
If you have repeated blighted ovum pregnancies, consider talking to your doctor about a chromosomal analysis of your embryos.
You may be at a significantly higher risk of blighted ovum than the general population if your partner is biologically related to you.
A blighted ovum can occur so early that it goes unrecognized. However, many women who receive a diagnosis of this condition go on to have subsequent healthy pregnancies. It’s not clear if blighted ovum occurs most typically in first-time pregnancies or if they sometimes occur more than once. Most women who have a blighted ovum do go on to have successful pregnancies and healthy babies.
How is this diagnosed?
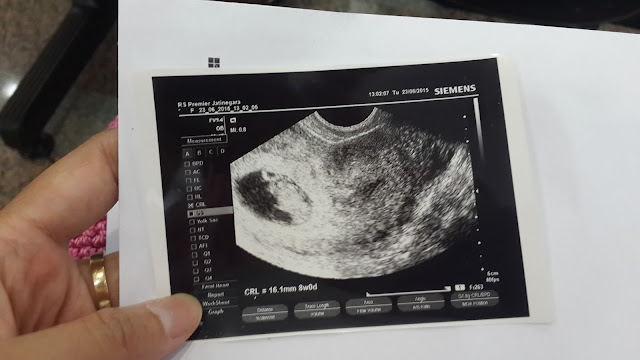
A blighted ovum is often discovered on the first ultrasound given during a prenatal appointment. The sonogram will show the placenta and empty embryonic sac. A blighted ovum usually occurs between the 8th and 13th weeks of pregnancy.
What are the treatment options?
If blighted ovum is discovered during a prenatal appointment, your doctor will discuss treatment options with you.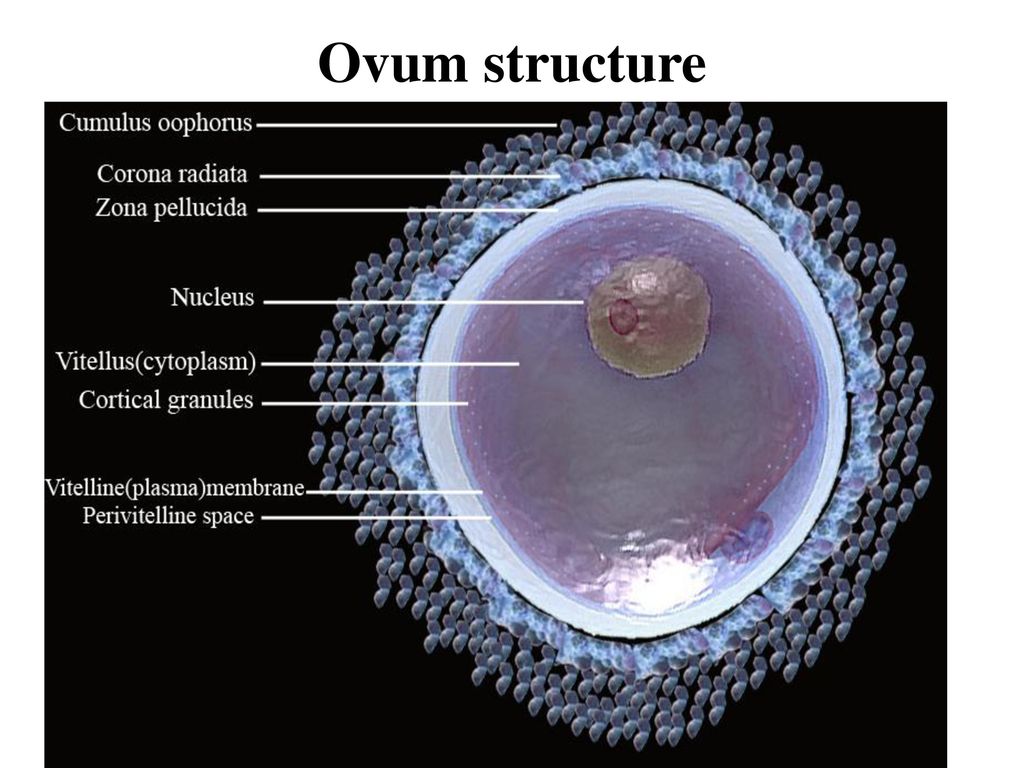 These may include:
These may include:
- waiting for miscarriage symptoms to occur naturally
- taking medication, such as misoprostol (Cytotec), to bring on a miscarriage
- having a D and C (dilation and curettage) surgical procedure to remove the placental tissues from the uterus
The length of your pregnancy, medical history, and emotional state will all be taken into account when you and your doctor are deciding upon a treatment option. You’ll want to discuss the side effects and the standard risks associated with any type of medication or surgical procedure, including a D and C.
Even though there wasn’t a baby, there has been a loss of a pregnancy. Miscarriages can be emotionally difficult, and waiting for the pregnancy to end can take longer than anticipated. For this reason, some women decide to terminate surgically or with medication. Other women are uncomfortable with these choices and prefer to let the miscarriage happen on its own.
Discuss all of your options with your doctor. Let them know if you’re uncomfortable with any of the options available to you.
Let them know if you’re uncomfortable with any of the options available to you.
Can this be prevented?
A blighted ovum can’t be prevented.
If you’re concerned about this condition, talk to your doctor about possible genetic causes and testing procedures, which might help you avoid it. Also discuss with your doctor about exposure to toxins in the environment. It may be linked to blighted ovum and miscarriage.
Are there any complications with future pregnancies?
Just as with any miscarriage, your body and emotional well-being need time to heal. It’s important to remember that most women who go through a blighted ovum go on to have successful pregnancies.
You and your doctor will discuss how long you should wait before trying to conceive again. It’s typically recommended that you wait three full menstrual cycles so that your body has time to recuperate fully and is ready to support pregnancy. During this time, focus on healthy lifestyle habits for your body and mental health, such as:
- eating well
- keeping stress at bay
- exercising
- taking a daily prenatal supplement that contains folate
Having a blighted ovum once doesn’t mean you’re destined to have another one. However, there are factors associated with this type of miscarriage that you should discuss with your doctor. These factors include genetics, egg quality, and sperm quality. Your doctor may recommend testing for these types of conditions. Tests may include:
However, there are factors associated with this type of miscarriage that you should discuss with your doctor. These factors include genetics, egg quality, and sperm quality. Your doctor may recommend testing for these types of conditions. Tests may include:
- preimplantation genetic screening (PGS), a genetic analysis of embryos that can be done prior to implantation into the uterus
- semen analysis, which is used to determine sperm quality
- follicle stimulating hormone (FSH) or anti-mullerian hormone (AMH) tests, which can be used to help improve egg quality
The takeaway
The specific cause of blighted ovum is unknown, but chromosomal anomalies appear to be a main factor. Having a blighted ovum doesn’t mean you’ll have another one. Most women who experience this go on to have healthy pregnancies.
Last medically reviewed on December 13, 2017
- Parenthood
- Pregnancy
- Pregnancy Health
How we vetted this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Baghbani F, et al. (2014). Association of heteromorphism of chromosome 9 and recurrent abortion (ultrasound diagnosed blighted ovum): A case report.
ncbi.nlm.nih.gov/pmc/articles/PMC4094662/ - Balanced translocations. (2014).
rarechromo.org/information/Other/Balanced%20translocations%20FTNP.pdf - Blighted ovum. (2016).
pregnancybirthbaby.org.au/blighted-ovum - de La Rochebrochard E, et al. (2002). Paternal age and maternal age are risk factors for miscarriage; results of a muticentre European study. DOI:
10.1093/humrep/17.6.1649 - Overcoming a ‘pseudo pregnancy’: Blighted ovums can cause miscarriage. (n.d.).
doctorsthatdo.org/overcoming-a-pseudo-pregnancy - Shekoohi S, et al. (2013). Chromosomal study of couples with a history of recurrent spontaneous abortions with diagnosed blighted ovum.

ncbi.nlm.nih.gov/pmc/articles/PMC3927383/ - Tobah YB. (2016). What causes a blighted ovum? What symptoms can I expect?
mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/expert-answers/blighted-ovum/faq-20057783 - When is the best time for pregnancy after miscarriage? (2016).
mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/pregnancy-after-miscarriage/art-20044134?pg=2
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Dec 13, 2017
By
Corey Whelan
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Corey Whelan on December 13, 2017
related stories
How Long Does a Miscarriage Last?
How to Tell if You’re Having a Miscarriage Without Bleeding
What I’ve Learned from Counseling Couples Through Miscarriage
7 Causes for a False-Positive Pregnancy Test
What’s a Chemical Pregnancy?
Read this next
How Long Does a Miscarriage Last?
Medically reviewed by Holly Ernst, PA-C
The loss of a pregnancy before 20 weeks is considered a miscarriage.
 The length of time a miscarriage lasts varies from woman to woman, as do the risk…
The length of time a miscarriage lasts varies from woman to woman, as do the risk…READ MORE
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
A miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
What I’ve Learned from Counseling Couples Through Miscarriage
Most women tell me it doesn’t get better, but it does get easier.
READ MORE
7 Causes for a False-Positive Pregnancy Test
Reputable home pregnancy tests can be accurate, but they aren’t foolproof and can cause confusion. Here are 7 reasons you may receive a false-positive…
READ MORE
What’s a Chemical Pregnancy?
Medically reviewed by Debra Rose Wilson, Ph.
 D., MSN, R.N., IBCLC, AHN-BC, CHT
D., MSN, R.N., IBCLC, AHN-BC, CHTA chemical pregnancy is an early pregnancy loss that occurs shortly after implantation. Chemical pregnancies may account for 50 to 75 percent of all…
READ MORE
Antidepressants in Pregnancy Aren't Linked to Increased Neurological Issues in Children
A cohort study of antidepressant use in pregnancy found that the rate of neurological disorders in children born to those who took antidepressant…
READ MORE
These Guided Pregnancy Journals Will Help You Document All the Feels
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
The pregnancy and postpartum periods are full of emotions (rightfully so!), and these pregnancy journals are a great place to document it all.
READ MORE
What You Need to Know If You’re Having a High Risk Pregnancy
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
A high risk pregnancy is any pregnancy that comes with increased health risks for either the pregnant parent, the fetus, or both.
READ MORE
What Are Conjoined Twins?
Conjoined twins are identical twins who are born connected and likely share one or more organs. We explain how they develop and when separation is…
READ MORE
The Acupressure Points for Inducing Labor
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Are you pregnant and past your due date? Help induce labor naturally by pressing on these acupressure points along the body.
READ MORE
Treatment, Symptoms, Causes, and Outlook
Blighted Ovum: Treatment, Symptoms, Causes, and OutlookMedically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Corey Whelan on December 13, 2017
What is a blighted ovum?
A blighted ovum is a fertilized egg that implants itself in the uterus but doesn’t become an embryo. The placenta and embryonic sac form, but remain empty. There’s no growing baby. It’s also known as anembryonic gestation or anembryonic pregnancy.
The placenta and embryonic sac form, but remain empty. There’s no growing baby. It’s also known as anembryonic gestation or anembryonic pregnancy.
Even though there’s no embryo, the placenta still produces human chorionic gonadotropin (hCG). This is a hormone designed to support pregnancy. Blood and urine pregnancy tests look for hCG, so blighted ovum can result in a positive pregnancy test even though the pregnancy isn’t actually proceeding. Pregnancy-related symptoms, such as sore breasts and nausea, may also occur.
A blighted ovum eventually leads to miscarriage. It’s not able to turn into a viable pregnancy.
What are the symptoms?
A blighted ovum sometimes ends before you realize you’re pregnant. When this happens, you may just think you’re having a heavier-than-normal menstrual period.
A blighted ovum may have the same symptoms associated with pregnancy, such as:
- a positive pregnancy test
- sore breasts
- a missed period
As the pregnancy ends, symptoms may include those of miscarriage. These can include:
These can include:
- vaginal spotting or bleeding
- abdominal cramping
- disappearance of breast soreness
Pregnancy tests measure hCG levels, so a blighted ovum can continue to result in positive test results before the tissues are passed.
What are the causes?
This condition isn’t caused by anything that you did or didn’t do, either during or before your pregnancy.
The exact cause of blighted ovum isn’t known. It’s thought to be caused by chromosomal abnormalities occurring within the fertilized egg. This may be the result of genetics, or of poor-quality eggs or sperm.
Blighted ovum may be linked to abnormalities within chromosome 9. If you have repeated blighted ovum pregnancies, consider talking to your doctor about a chromosomal analysis of your embryos.
You may be at a significantly higher risk of blighted ovum than the general population if your partner is biologically related to you.
A blighted ovum can occur so early that it goes unrecognized.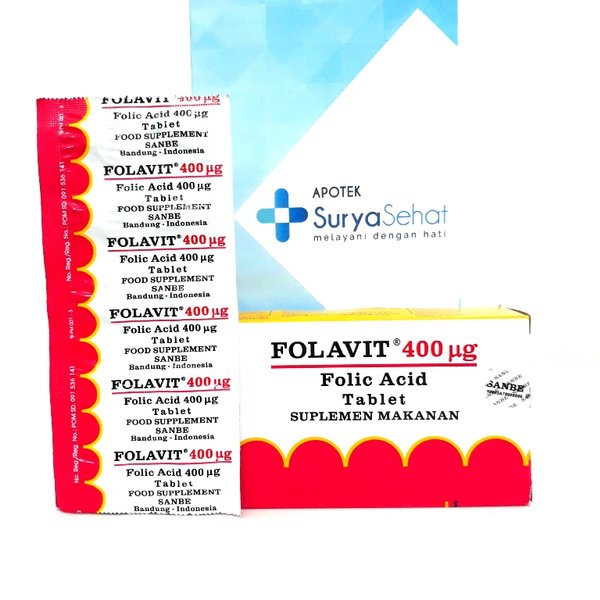 However, many women who receive a diagnosis of this condition go on to have subsequent healthy pregnancies. It’s not clear if blighted ovum occurs most typically in first-time pregnancies or if they sometimes occur more than once. Most women who have a blighted ovum do go on to have successful pregnancies and healthy babies.
However, many women who receive a diagnosis of this condition go on to have subsequent healthy pregnancies. It’s not clear if blighted ovum occurs most typically in first-time pregnancies or if they sometimes occur more than once. Most women who have a blighted ovum do go on to have successful pregnancies and healthy babies.
How is this diagnosed?
A blighted ovum is often discovered on the first ultrasound given during a prenatal appointment. The sonogram will show the placenta and empty embryonic sac. A blighted ovum usually occurs between the 8th and 13th weeks of pregnancy.
What are the treatment options?
If blighted ovum is discovered during a prenatal appointment, your doctor will discuss treatment options with you. These may include:
- waiting for miscarriage symptoms to occur naturally
- taking medication, such as misoprostol (Cytotec), to bring on a miscarriage
- having a D and C (dilation and curettage) surgical procedure to remove the placental tissues from the uterus
The length of your pregnancy, medical history, and emotional state will all be taken into account when you and your doctor are deciding upon a treatment option. You’ll want to discuss the side effects and the standard risks associated with any type of medication or surgical procedure, including a D and C.
You’ll want to discuss the side effects and the standard risks associated with any type of medication or surgical procedure, including a D and C.
Even though there wasn’t a baby, there has been a loss of a pregnancy. Miscarriages can be emotionally difficult, and waiting for the pregnancy to end can take longer than anticipated. For this reason, some women decide to terminate surgically or with medication. Other women are uncomfortable with these choices and prefer to let the miscarriage happen on its own.
Discuss all of your options with your doctor. Let them know if you’re uncomfortable with any of the options available to you.
Can this be prevented?
A blighted ovum can’t be prevented.
If you’re concerned about this condition, talk to your doctor about possible genetic causes and testing procedures, which might help you avoid it. Also discuss with your doctor about exposure to toxins in the environment. It may be linked to blighted ovum and miscarriage.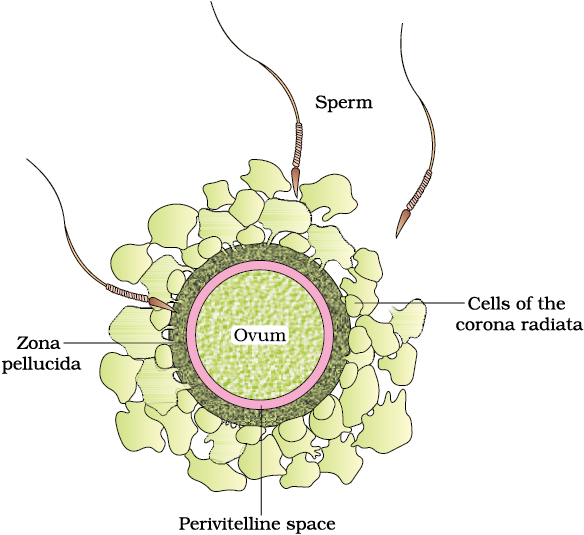
Are there any complications with future pregnancies?
Just as with any miscarriage, your body and emotional well-being need time to heal. It’s important to remember that most women who go through a blighted ovum go on to have successful pregnancies.
You and your doctor will discuss how long you should wait before trying to conceive again. It’s typically recommended that you wait three full menstrual cycles so that your body has time to recuperate fully and is ready to support pregnancy. During this time, focus on healthy lifestyle habits for your body and mental health, such as:
- eating well
- keeping stress at bay
- exercising
- taking a daily prenatal supplement that contains folate
Having a blighted ovum once doesn’t mean you’re destined to have another one. However, there are factors associated with this type of miscarriage that you should discuss with your doctor. These factors include genetics, egg quality, and sperm quality.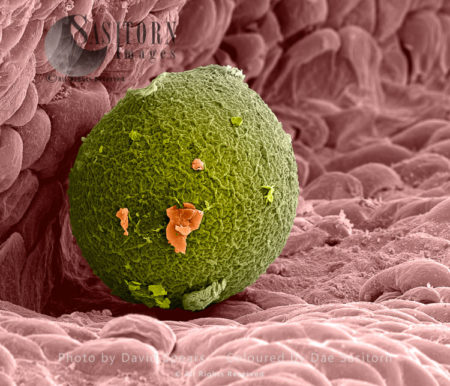 Your doctor may recommend testing for these types of conditions. Tests may include:
Your doctor may recommend testing for these types of conditions. Tests may include:
- preimplantation genetic screening (PGS), a genetic analysis of embryos that can be done prior to implantation into the uterus
- semen analysis, which is used to determine sperm quality
- follicle stimulating hormone (FSH) or anti-mullerian hormone (AMH) tests, which can be used to help improve egg quality
The takeaway
The specific cause of blighted ovum is unknown, but chromosomal anomalies appear to be a main factor. Having a blighted ovum doesn’t mean you’ll have another one. Most women who experience this go on to have healthy pregnancies.
Last medically reviewed on December 13, 2017
- Parenthood
- Pregnancy
- Pregnancy Health
How we vetted this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Baghbani F, et al. (2014). Association of heteromorphism of chromosome 9 and recurrent abortion (ultrasound diagnosed blighted ovum): A case report.
ncbi.nlm.nih.gov/pmc/articles/PMC4094662/ - Balanced translocations. (2014).
rarechromo.org/information/Other/Balanced%20translocations%20FTNP.pdf - Blighted ovum. (2016).
pregnancybirthbaby.org.au/blighted-ovum - de La Rochebrochard E, et al. (2002). Paternal age and maternal age are risk factors for miscarriage; results of a muticentre European study. DOI:
10.1093/humrep/17.6.1649 - Overcoming a ‘pseudo pregnancy’: Blighted ovums can cause miscarriage. (n.d.).
doctorsthatdo.org/overcoming-a-pseudo-pregnancy - Shekoohi S, et al. (2013). Chromosomal study of couples with a history of recurrent spontaneous abortions with diagnosed blighted ovum.

ncbi.nlm.nih.gov/pmc/articles/PMC3927383/ - Tobah YB. (2016). What causes a blighted ovum? What symptoms can I expect?
mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/expert-answers/blighted-ovum/faq-20057783 - When is the best time for pregnancy after miscarriage? (2016).
mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/pregnancy-after-miscarriage/art-20044134?pg=2
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Dec 13, 2017
By
Corey Whelan
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
Share this article
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT — By Corey Whelan on December 13, 2017
related stories
How Long Does a Miscarriage Last?
How to Tell if You’re Having a Miscarriage Without Bleeding
What I’ve Learned from Counseling Couples Through Miscarriage
7 Causes for a False-Positive Pregnancy Test
What’s a Chemical Pregnancy?
Read this next
How Long Does a Miscarriage Last?
Medically reviewed by Holly Ernst, PA-C
The loss of a pregnancy before 20 weeks is considered a miscarriage.
 The length of time a miscarriage lasts varies from woman to woman, as do the risk…
The length of time a miscarriage lasts varies from woman to woman, as do the risk…READ MORE
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
A miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
What I’ve Learned from Counseling Couples Through Miscarriage
Most women tell me it doesn’t get better, but it does get easier.
READ MORE
7 Causes for a False-Positive Pregnancy Test
Reputable home pregnancy tests can be accurate, but they aren’t foolproof and can cause confusion. Here are 7 reasons you may receive a false-positive…
READ MORE
What’s a Chemical Pregnancy?
Medically reviewed by Debra Rose Wilson, Ph.
 D., MSN, R.N., IBCLC, AHN-BC, CHT
D., MSN, R.N., IBCLC, AHN-BC, CHTA chemical pregnancy is an early pregnancy loss that occurs shortly after implantation. Chemical pregnancies may account for 50 to 75 percent of all…
READ MORE
Antidepressants in Pregnancy Aren't Linked to Increased Neurological Issues in Children
A cohort study of antidepressant use in pregnancy found that the rate of neurological disorders in children born to those who took antidepressant…
READ MORE
These Guided Pregnancy Journals Will Help You Document All the Feels
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
The pregnancy and postpartum periods are full of emotions (rightfully so!), and these pregnancy journals are a great place to document it all.
READ MORE
What You Need to Know If You’re Having a High Risk Pregnancy
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
A high risk pregnancy is any pregnancy that comes with increased health risks for either the pregnant parent, the fetus, or both.

READ MORE
What Are Conjoined Twins?
Conjoined twins are identical twins who are born connected and likely share one or more organs. We explain how they develop and when separation is…
READ MORE
The Acupressure Points for Inducing Labor
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Are you pregnant and past your due date? Help induce labor naturally by pressing on these acupressure points along the body.
READ MORE
How to improve the quality of eggs - City Hospital No. 12, Barnaul: Articles
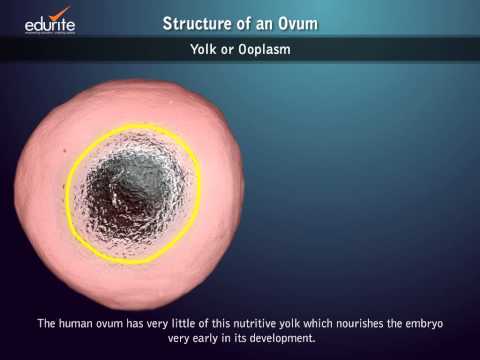
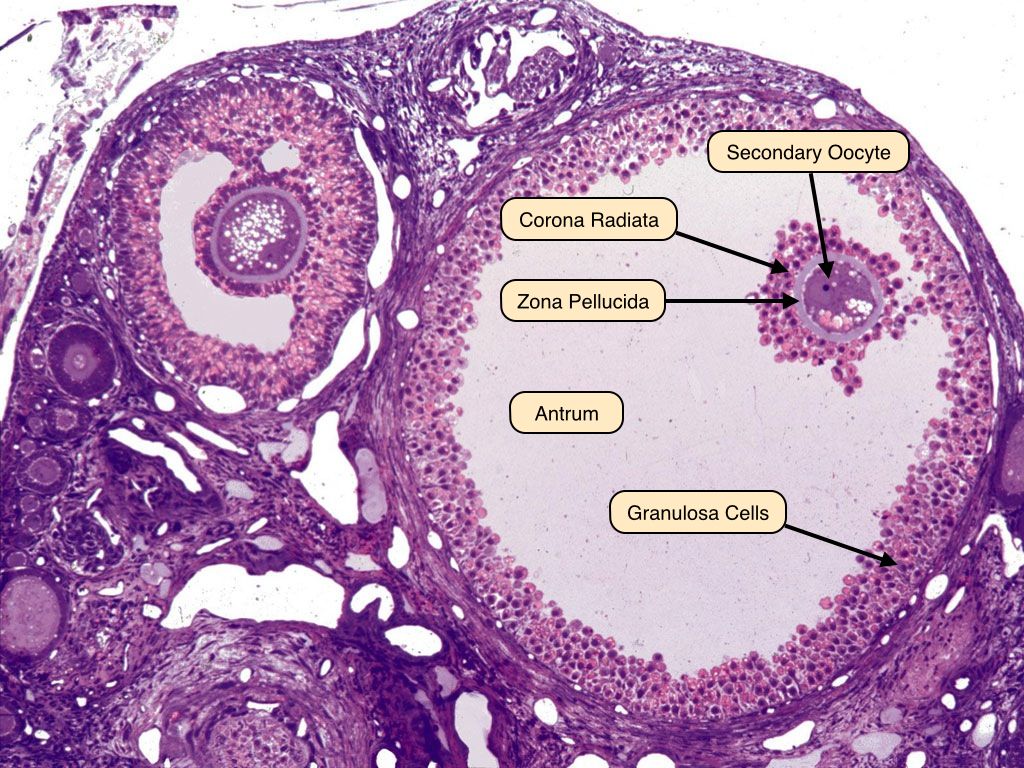
An egg is called a female gamete and becomes an embryo when fertilized by a spermatozoon. A woman has a finite number of eggs determined by SO, called ovarian reserve. Primordial cells, precursors of the egg, are formed in the early female embryo. The maximum number is recorded in 5-month-old embryos, reaching millions. Most of these cells are degraded before birth. Their number does not exceed 1 million at birth and decreases by about three times by the age of seven.
The maximum number is recorded in 5-month-old embryos, reaching millions. Most of these cells are degraded before birth. Their number does not exceed 1 million at birth and decreases by about three times by the age of seven.
Since the egg is in the body of a woman from birth and it took many years to cleanse the pores, all the factors affecting the body are the same. However, unlike organs, eggs do not have a regenerative mechanism, that is, they do not have the ability to regenerate. Like the skin, liver, kidneys, lungs, etc., they never renew themselves. In other words, the state of the egg is greatly influenced by the lifestyle of the girl from the moment of conception.
The maturation of the egg begins in the follicle, a special "sac" inside the ovary. The influence of individual sex hormones on the menstrual cycle leads to the formation of dominant follicles, which release germ cells after about 14 days (ovulation process). Fallopian tube pheromones (special fingers at the end facing the abdominal cavity) register the egg in the lumen of the fallopian tube. There he waits for spermatozoa and, if fertilization occurs, slows down the mobility of the smooth muscles of the ducts and the epithelium of the ciliary body and begins to move towards the uterus. This route takes about a week from a fertilized egg. If spermatozoa are not found, vaginal discharge begins with destruction of the uterine lining due to menstruation.
There he waits for spermatozoa and, if fertilization occurs, slows down the mobility of the smooth muscles of the ducts and the epithelium of the ciliary body and begins to move towards the uterus. This route takes about a week from a fertilized egg. If spermatozoa are not found, vaginal discharge begins with destruction of the uterine lining due to menstruation.
Outward signs of poor egg quality
Egg reproductive performance is known to decline with age. Unfortunately, therefore, one of the characteristic indicators of the state of germ cells is the youth of a woman. In a woman's body, upon reaching the age of 38-40, the mechanism of hormonal changes associated with the functional completion of the offspring in the woman's body starts. The process runs smoothly, but still tends to reduce egg quality. Statistically, the risk of genetic diseases increases with age, the frequency of pregnancies decreases and the frequency of childbearing decreases, but medicine knows many cases of women giving birth to perfectly healthy first children, so this information should not be taken as insistent. .
.
It is also possible with a high degree of probability to determine the state of the egg by changing the nature of the menstrual cycle. As egg production decreases, it decreases and culling becomes rare. Such pictures are typical of the onset of early menopause, but may also be temporary due to stress or illness. Laboratory tests and ultrasound can accurately determine the fertility of eggs.
How to improve eggs before IVF
In vitro fertilization (IVF) helps sperm to meet and penetrate the egg. In addition, he follows the providence of nature, so the result of the program greatly affects the state of the source material. Before IVF, the eggs selected by puncture should be as fertilized as possible. This increases the chances of fertilization and embryo transfer.
The state of the eggs is affected by the period of preparation for women to lead the most healthy lifestyle. During this time, it must be excluded.
- Alcohol consumption, smoking, drug use
- Heavy (empty) foods, heavy foods containing carcinogens, trans fatty acids, preservatives, extra calories, simple carbohydrates.

- Exposure to harmful substances-.
- Set with great nervous shock and stress.
Even if egg production is low, it has little effect on embryo development. Therefore, it is very important to get the best eggs from women before in vitro fertilization. On the other hand, females are said to make up about 15-20% of high quality eggs after 40 years of travel.
In addition to a healthy lifestyle and a complete diet, one of the factors that increase the production of eggs is a regular sex life. Sex regularly affects the supply of oxygen and nutrition to the internal organs of the pelvis and promotes the metabolism of organs. Good ovarian health, of course, affects the health of the egg.
Food plays an important role in women's reproductive abilities. To do this, it is important to consider not only calories, but also macrobalance and the consumption of many foods containing vitamins and minerals. Pursuit unsaturated fatty acids, which are abundant in vegetable oils, have a positive effect on the reproductive organs and are the leading linseed oil. Two tablespoons a day is enough to meet the required amount of these beneficial substances. It is recommended to receive such "oil therapy" during pregnancy preparation or replace it with omega a-3 capsules.
Two tablespoons a day is enough to meet the required amount of these beneficial substances. It is recommended to receive such "oil therapy" during pregnancy preparation or replace it with omega a-3 capsules.
In the example of in vitro fertilization, drug therapy is given to improve the eggs. Also, if there is evidence based on anesthesia or laboratory studies.
What harms eggs?
The productivity of eggs is directly dependent on the immune system and the condition of the whole body, so those that impair health will directly and indirectly damage the eggs. If you point to the most important factors, it is lifestyle. Both healthy and unhealthy. For this idea
- food?
- Exercise stress
- sleep time
- Emotional state.
Among the bad habits, cigarettes are the first to harm women's reproduction, with the exception of serious drugs. Cigarette smoke contains many harmful substances and penetrates every tissue of the body. Eggs are easily suppressed by toxic substances. In such a situation, the risk of a difficult pregnancy and abnormal growth of the fetus increases. Alcohol is harmful because the body is toxic. You will know that moderate quantity and quality alcohol can stand up to women. Drinking red wine in a festive place will not be harmful. However, smoking is required.
Eggs are easily suppressed by toxic substances. In such a situation, the risk of a difficult pregnancy and abnormal growth of the fetus increases. Alcohol is harmful because the body is toxic. You will know that moderate quantity and quality alcohol can stand up to women. Drinking red wine in a festive place will not be harmful. However, smoking is required.
You need eight sleeps to restore your body. Chronic sleep deprivation inevitably causes the function of the nervous system and reduces immunity, which also affects the nature of the germ cells.
Good mental health is very important for an expectant mother who performs in vitro fertilization. You need to learn how to deal with anxiety without using pharmacology. For this reason, it is advisable to focus on the z-step in implementation, while initially being cautiously optimistic.
An active lifestyle not only improves the condition of the body, but also maintains a high mental and emotional state. Moderate exercise promotes metabolism and contributes to the normal function of the endocrine system, which is important for egg health.
Gynecological diseases, especially polycystic ovaries (PCA), endometriosis and genital infections, can reduce egg production and cause infertility. In this case, it is necessary to perform treatment according to the condition.
Is it possible to improve the condition of eggs after 40 years?
Eggs can be improved in any way during the breeding season. To do this, it is necessary to meet all the same conditions that are recommended for women during the training period. There are many pharmacological preparations that help the ovaries recover. It contains substances such as Innochitol, DGEA, folic acid, polyunsaturated fatty acids and L-arginine, normalizing the function of the female reproductive organ. But only doctors can prescribe medicine. Otherwise, you will harm your health or be disturbed by hormonal balance.
To improve pregnancy and egg function, it is recommended to introduce foods rich in minerals such as vitamins C, E, B, D, zinc and iodine.
In modern reproductive medicine, women can keep 40 eggs obtained by freezing (freezing). Such cells can be thawed for many years and are suitable for fertilization and transplantation.
I have selected 22 basic questions about prostatitis and treatment. All answers were written by Speransky Alexey Gennadievich, a leader in the healthy field of men. I hope this article is useful and necessary.
Summary of articles
Symptoms of prostatitis: pain, burning, discharge, stinging, incontinence
There are usually three types of prostatitis.
- Uureters: difficulty, rapid, nighttime urination.
-Pain Symptoms of pain in the perineum, lower abdomen and groin. The pain may radiate to the scrotum or sacrum.
- Mamba type which shows both urination and pain.
What causes prostatitis?
With bacterial prostatitis
The prostate is infected from nearby organs.
- Crushing inflammatory nests (tonsillitis, sinusitis, caries) in the blood and lymphatic vessels.
The most common bacteria found in prostatitis. Escherichia coli, Cleb Sierra, Proteus, Staffirococcus Gold, Enterococcus
The role of sexually transmitted diseases: chlamydia, mycoplasma, trichomonas.
The activity of the inflammatory process and the consequences of the consequences are influenced by the characteristics of microorganisms, the state of the internal organs of the pelvis, blood circulation, related diseases and other causes.
With non-sterilized previous glands
This is a constant phenomenon that plays an important role. Impaired blood flow causes swelling of the prostate and exudation of tissue, creating a state of inflammation that is not associated with bacteria.
STDs and prostatitis
The problem of sexually transmitted diseases involved in the onset of prostatitis is widely discussed in the scientific medical community. This issue has not been received.
We believe that we assume that there is a direct relationship between the onset and progression of prostatitis and the transition and infection.
Why is prostatitis dangerous?
Prostatitis is not life threatening, but the process is chronic and worsens QOL.
Incipient prostatitis. How to determine? First signs
The first sign of prostatitis is a change in the nature of urination: difficult, rapid urination, frequent urination, especially at night. Discomfort during urination, pain with strong groin.
Age of prostatitis? Is this a disease of the young and/or old?
Prostatitis is an inflammatory disease, so it can occur regardless of age. However, prostate adenoma and hyperplasia are aging diseases found in men after 50 years of age, accompanied by benign tumors in the prostate.
Chronic prostatitis. Is it possible to cure?
The diagnosis of chronic prostatitis means that the pattern of prostate tissue changes that lasts a lifetime. Like other chronic diseases, prostatitis alternates between a period of exacerbation and a period of remission (a period when the patient is not taken care of). With suitable treatment and lifestyle, the remission period is very long and vague complaints no longer bother the patient.
With suitable treatment and lifestyle, the remission period is very long and vague complaints no longer bother the patient.
Bacterial and other types of prostatitis
There are several classifications but was most commonly used by the United States National Institutes of Health in 1995.
Category I: Acute prostatitis Category II Chronic bacterial prostatitis. Category III Bacterial Prostatitis/Chronic Pelvic Pain - No sign of obvious infection and it has been for more than 3 months; -Subclass III A. Chronic inflammatory pelvic pain (leukocytes are secreted and pathogens are released). -Su b-class III B. Chronic non-flattened pelvic pain (no leukocytes in secret prostate). Category IV asymptomatic occupational fluid prostatitis (but has leukocytes in prostate secretions but no vague complaints).
To make it easier to understand, it is expressed in three types.
Acute prostatitis: occurs with severe pain, fever, urination, etc. The secret of the prostate is a mass of white blood cells, indicating a clear process of inflammation. In principle, this occurs for the first time in this patient. If these symptoms appear in patients with chronic prostatitis, they may be associated with an exacerbation of chronic prostatitis.
In principle, this occurs for the first time in this patient. If these symptoms appear in patients with chronic prostatitis, they may be associated with an exacerbation of chronic prostatitis.
Chronic bacterial prositis - symptoms that regularly irritate patients are usually minor than acute prostatitis. In diagnostics, an increase in leukocytes in the secretion of the prostate can be identified as the causative agent of inflammation.
The most problematic diagnosis is not bacterial prositis or so-called chronic pelvic pelvic pelvic organ pain. Spasms of the pelvis, disruption of the interaction between the muscles of the bladder and the sphincter, an anatomical disorder of m-stagnation (stenosis) of the urethra, and an increase in pressure inside the sheet of the prostate gland can lead to inflammation.
Who treats prostatitis - andrologist or urologist?
Prostatitis is treated both in urology and in Android.
Androgist is a urology specialty in male and reproductive diseases.
Methods and regimens for the treatment of prostatitis
All treatment of the prostate consists of drug therapy.
is a drug that improves prostate and bladder contraction by relaxing the sphincter.
Good results can be obtained from the simultaneous prescription of drugs and normalization (prostate massage, prostatitis-anrogen composite agent, ALDIS, etc.).
What tests are done for prostatitis?
Diagnosis of prostatitis requires consultation with a physician (andrologist) to collect patient complaints, medical history, prostate prostate and ultrasound tests.
Ultrasound diagnosis of the prostate (Torji) and microscopic examination of prostate secretion taken after prostate massage are used for diagnosis.
Inoculation of bacterial flora with prostate secretion can also be used to measure the sensitivity of the inoculated flora to antibiotics.
Surgical interventions and operations for prostatitis
For prostatitis, its function has not found practical application. An exception is a prostate abscess, a process in which a focus with purulent contents is formed.
An exception is a prostate abscess, a process in which a focus with purulent contents is formed.
Is it possible to cure prostatitis on my own?
If symptoms are severe, it is best to seek specialist treatment. Temporary factors attach more importance to treatment, because the stronger the inflammation, the higher the likelihood of irreversible changes in the organ.
But for prevention it is better to do it yourself, doctors will not do it.
Hypothermia, prolonged sedentary congestion, sexually transmitted infections, and avoidance of irregular sexual contact are all effective ways to prevent prostatitis.
Prostatitis drugs: finalgon, vitaprost, prostamol, ceftriaxone, doxycycline, omnix and others
Prostatitis drugs are divided into groups according to the mechanism of action.
Antibiotics (antibiotics) are prescribed only for the diagnosis of chronic bacterial prostatitis. The most commonly used groups are fluoroquinolones, macrolides and duxycyclines.
Alpha-blockers: prescribed to restore reduced urination and increase bladder contraction and lateral relaxation.
Numerous groups of biological stimulants and phytopreparations: Vitapron, prostatitis, prostate wax.
There is no universal cure for all types of prostatitis, and effective treatment is possible only with a correct diagnosis. Prostatitis medications are often prescribed for people with very different conditions but similar symptoms.
Nuts, roots, parsley, cucumber, honey, bees, leeches and other folk remedies for prostatitis
Folk remedies have a right to exist, but you should understand that choosing the right folk remedy for you is very difficult. For requests to treat prostatitis with folk remedies, the search engine produces 70 million results.
The effectiveness of civilian methods has not been investigated by anyone. What helped the patient with such therapy (if it helped) will not help you far.
Exacerbation of prostatitis after treatment.
 Remission, relapse
Remission, relapse All chronic inflammatory processes have periods of exacerbation and remission, when nothing bothers you. The duration of remission varies and depends on many factors, including whether prophylactic therapy is used. In general, patients who do not anticipate deterioration in their health and regularly take preventive measures, exacerbations occur less often.
Prostate massage at home. Is massage always necessary for prostatitis?
Prostate massage can be done at home if you are married to a urology nurse. Any medical procedure has its own nuances. Prostate adenoma (with acute obstruction of the urinary tract), prostate massage is undesirable and contraindicated in tumors.
Alcohol and prostatitis
Alcohol does not cause prostatitis by itself, but contributes, because it is a factor that increases the stagnation and swelling of the prostate.
Sex life and prostatitis
There is a direct relationship between the intensity of sexual activity and prostate disease. If the nuance of the prostate lasts for a long time, stagnation phenomena will occur, the metabolic process will deteriorate, blood circulation will be disturbed, and an inflammatory process will be obtained. For prostate health, a regular life is more important than the strength of sexual intercourse. Excessive sexual activity with different partners and exposure to infectious diseases is a label for prostatitis.
If the nuance of the prostate lasts for a long time, stagnation phenomena will occur, the metabolic process will deteriorate, blood circulation will be disturbed, and an inflammatory process will be obtained. For prostate health, a regular life is more important than the strength of sexual intercourse. Excessive sexual activity with different partners and exposure to infectious diseases is a label for prostatitis.
Does prostatitis affect women?
Of course, the impact of women with prostatitis on prostatitis health. The prostate produces the liquid component of semen along with the vesicles and enters the opponent's sexual zone during sexual activity. The main risks may be the transmission of venereal diseases and bacterial prostatitis, which cause inflammatory diseases in women.
Pregnancy and prostatitis
The prostate produces a liquid part containing sperm nutrients, so prostatitis often reduces sperm quality and cannot be pregnant.
Prevention.
 What to do to avoid prostatitis?
What to do to avoid prostatitis? Prevention is directly related to the climate and profession where the patient lives.
Prevention of prostatitis begins with the prevention of factors that develop prostatitis and minimize. To avoid low body temperature, you need to alternate the time to sit down and move your body. For prostatitis, a regular sex life is important.
If you still have any questions, or if you would like to make a doctor's reservation, please call: 8 965 873 67 or online.
The main goal of a hospitalized doctor is to treat pneumonia and recover until you have enough physical strength to continue treatment at home. Write when body temperature, respiratory rate, heart rate, blood pressure and blood oxygen concentration are within the normal range. Appetite and concentration should also be improved.
However, simply returning to Japan does not mean that he was completely cured. Unfortunately, you will not be running a marathon in the near future. Lung function may differ from pneumonia. However, it is possible to fully recover to the level of activity before the diagnosis.
Lung function may differ from pneumonia. However, it is possible to fully recover to the level of activity before the diagnosis.
Unfortunately, many people who have damaged their lungs due to pneumonia (especially the colon virus) may not have the same level of activity.
Pneumonia is a serious infection that damages lung tissue. When you breathe, your lungs may not expand enough, or some lung tissue may be irreversible. This can affect the amount of oxygen that enters the body and the amount of carbon dioxide that leaves the body. As a result, you may feel tired or sometimes short of breath.
After pneumonia, muscle strength often decreases. This can be caused by lack of activity and weight loss.
In addition, those with various problems such as lung disease and heart disease often have severe symptoms. In such cases, oxygen can be administered at home.
Doctors give instructions and, like this, gradually restore consciousness at home. It can be considered to use medications, gradually increase the level of exercise and perform breathing techniques.
Recovering from Coronavirus Pneumonia
For many Covid-19 patients, getting rid of the virus is only half the battle. Many people are still suffering from the unpleasant consequences of the SARS-COV-2 virus, which affects vital organs, especially the lungs.
Decreased lung function, pneumonia, low blood oxygen saturation and shortness of breath, pulmonary fibrosis and chronic lung failure are some of the most serious damage caused by mild Covid-19. People with chronic respiratory diseases or weakened immune systems will have a particularly hard time.
Difficulty breathing often occurs after Covid-19. Furthermore, even in young and healthy patients, it has been reported that lung function decreases after recovery, and some of them require supplemental oxygen devices or artificial respiration, which can impair their quality of life (QoL). Acute respiratory illnesses and a weakened immune system make people more susceptible to other illnesses. Environmental factors such as air pollution also exacerbate the condition.
Here are some things you can do to protect your lung health after COVID-19.
Practice breathing exercises regularly
Since Covid-19 has begun to affect the lungs, infections such as shortness of breath and poor oxygen supply are common symptoms. Covid patients are often advised to do simple deep breathing exercises or meditation postures to improve breathing and improve blood flow to the lungs and bronchi.
Diaphragmatic breathing, a deep breathing movement, promotes deeper breathing and movement of the lungs and chest muscles. You can also improve your oxygen supply by taking deep breaths while lying on your stomach.
Pranayama is considered an excellent exercise for increasing lung capacity. Patients with difficulty breathing and low oxygen levels can also improve their lung health by exercising with Responder.
Eat foods that increase lung capacity
A good diet rich in vitamins and minerals improves immunity. There are foods that detoxify and help you breathe easier.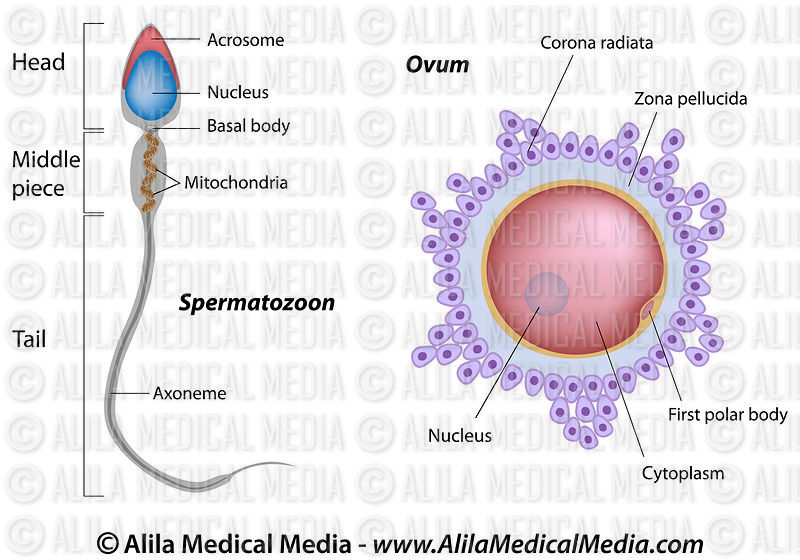 Here are some easy ways to improve lung health at home.
Here are some easy ways to improve lung health at home.
Avoid excessive consumption of processed and refined foods, as well as seasonal foods such as beets, green tea, blueberries, tomatoes, nuts and seeds to increase lung capacity. Citrus fruits like oranges and lemons should also be in abundance. Garlic and turmeric are powerful foods rich in antioxidants and are said to have antiviral properties.
In particular, eat plenty of foods rich in omega-3s, which can help reduce lung inflammation and reduce the risk of other respiratory diseases.
Also, experts recommend keeping track of nutrients. Weight loss diets that deprive you of essential nutrients should be avoided for some time after recovery.
Avoid smoking
Not only does smoking increase the risk of contracting or transmitting Covid, it also causes irreversible damage to the already fragile lungs. Smoking and tobacco put extra strain on vital organs, making it more likely to develop other lung diseases and infections in the long term.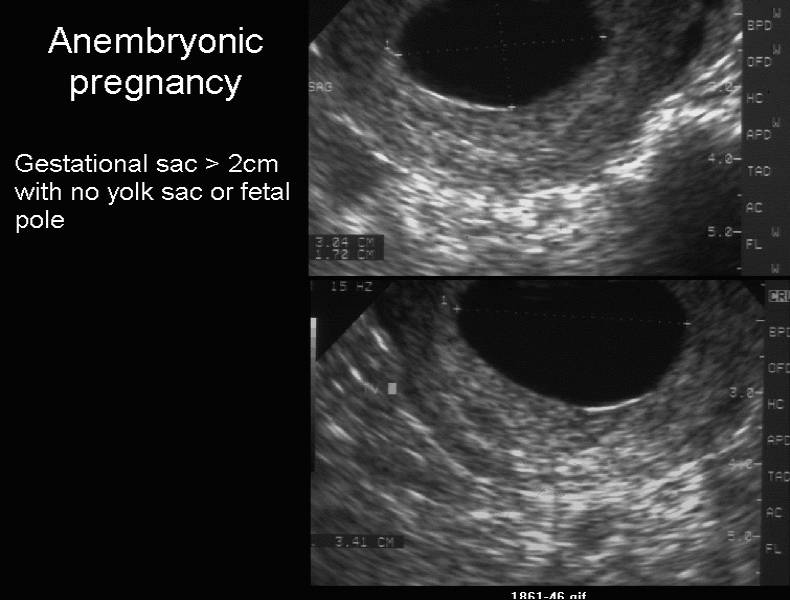
Cardio training improves respiratory function
All activities that activate breathing are effective in restoring vital ability and function in recovery. Experts recommend patients in exercise or sports with moderate or fast-o-minimum. You can increase your heart rate and improve blood flow.
Choose home exercises and aerobic exercises that are good for your respiratory health, walking regularly (safe). Yoga asana is also useful for restoring functions and improving immunity. Aerobic exercise is also effective.
Don't forget to exercise regularly, let's do it slowly. It is also recommended that athletes start recovering from rehabilitation movements that are good for lung health before moving on to other fast and violent movements.
Avoid exposure to pollution or smoke
People who have just received COVID-19 treatment or who have reduced lung function should avoid any activity that could interfere with unnecessary fumes, polluted environments, and respiratory function.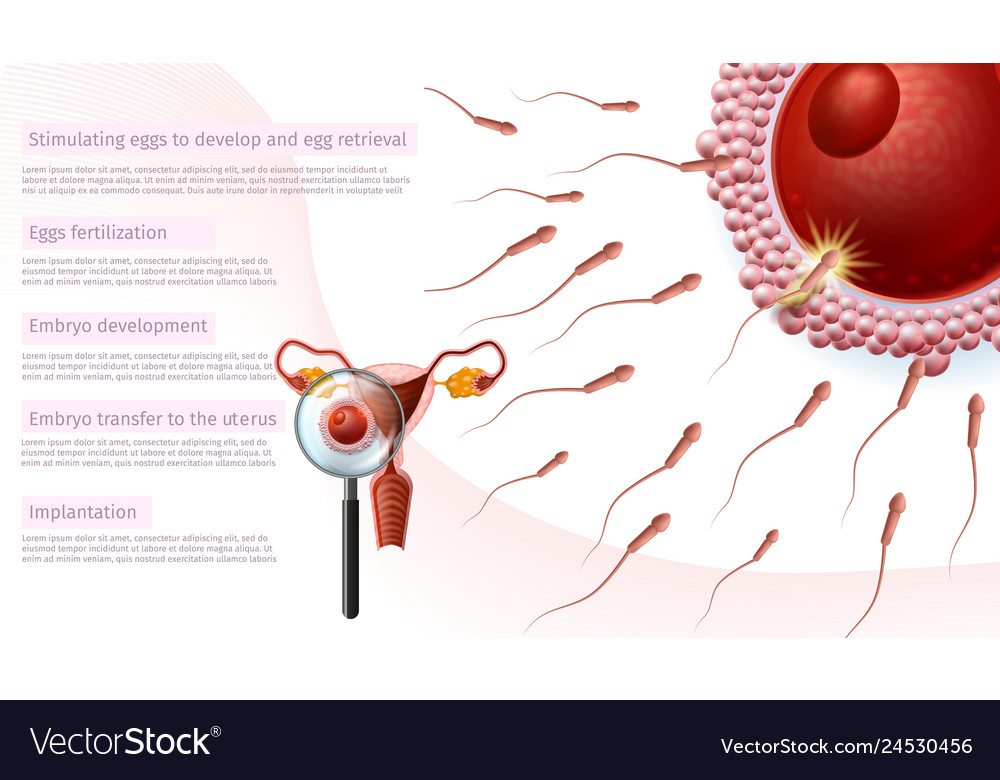 Pollution not only increases the risk of relapse, but is also exposed to carcinogens and other dangerous stimuli and can be deposited into the lung cavity and obstruct breathing.
Pollution not only increases the risk of relapse, but is also exposed to carcinogens and other dangerous stimuli and can be deposited into the lung cavity and obstruct breathing.
If you have to go outside, take the necessary precautions, take your medicine and get sick. Side suction and detox method are also effective.
1. Breathing method (n.d.) 2. Lemgoral vital ability and aging. (2018) 3. Mayo Clinic staff. (2017) 4. Sivakumar G. Acute effect on deep breathing (2-10 minutes) for pulmonary function [Summary]. Indian Physiological Journal "Pharmaceuticals", 55 (2), 154-9 5 . Tobacco use and compliance in the DEPA basement (2008, May) 6. Your lungs and exercise (2016). Breeze, 12(1).
Nearly all living cells contain cholesterol scaffolds that carry fat into circulation. Without this substance, the nervous system, immune system and digestive system cannot function normally. However, as cholesterol indicators increase, they begin to deposit onto the wall of the blood vessel. As a result, a plaque forms, blood vessels narrow, and elasticity is broken. Causes of high cholesterol and how to deal with it
As a result, a plaque forms, blood vessels narrow, and elasticity is broken. Causes of high cholesterol and how to deal with it
When cholesterol becomes dangerous
Most parts (about 70-80%) are made in the body, and only a few come from outside. However, not all cholesterol is bad, and only bad ball low-density lipoprotein (LDL) is bad. The "good ball" is needed to transfer excess cholesterol from tissue to the liver, process and excretion. Therefore, it is beneficial for the body that it contains a lot of “good” cholesterol.
As the number of LDL markers increases, excess processing and excretion of excess cholesterol are impaired. Blood vessels supplied to the kidneys, intestines, and lower extremities gradually reach the excess blood vessels that cause arteriosclerosis. Damage to the blood vessels that supply the brain, causing symptoms such as dizziness and fainting, and then a stroke. Atherosclerosis is dangerous for the cardiovascular systems. The deterioration of the blood vessels leads to coronary artery disease (coronary heart disease), in the future myocardial infarction.
High cholesterol does not affect health until a serious illness develops. Therefore, even young people are advised to regularly take an analysis of total cholesterol. and take immediate action in case of deviations from the norm.
If blood cholesterol is elevated: what to do
The problem must be completely resolved. Be sure to consult with a cardiologist to choose the best way to deal with high cholesterol. The early stages of lowering the index can often be achieved without the use of drugs. Your doctor can give advice depending on the degree of risk.
- Avoid bad habits. Smoking and strong alcohol damage blood vessels, so don't put extra stress on them.
- The easiest way to keep blood vessels in good shape is to increase physical activity. At least 30 minutes of aerobic exercise every day, such as walking, jogging, or biking, is effective. By exercising for hours, you will be able to move more.
- Lose weight - High cholesterol is often associated with high body weight.
 Obesity increases the risk of diabetes, high blood pressure and heart disease. To protect yourself from these diseases, you should try to lose weight.
Obesity increases the risk of diabetes, high blood pressure and heart disease. To protect yourself from these diseases, you should try to lose weight. - Diet management - cut out trans fats (fast food, processed foods), eat more fiber, include fish for men, replace black tea with green tea, etc. Also, avoid foods high in animal fats such as butter, ice cream, and sausages.
- Adjust your mode. In a study published by Sleeptrusted Source, researchers found that too much or too little sleep negatively affects cholesterol levels. They interviewed a group of 1666 men and 2329women aged 20 and over. Less than 5 hours of sleep has been associated with higher triglyceride levels and lower LDP in women. Sleeping more than eight hours had a similar effect. Men were less sensitive to excessive sleep than women.
In addition, depending on the state of health and test results, drug therapy may be prescribed.
Don't have time to read long articles? Subscribe on social networks. Read short notes about beauty and wellness while listening to the background of the video.
Read short notes about beauty and wellness while listening to the background of the video.
Megapharmacy in social networks: vkontakte, Telegram, OK, Viber
How to lower cholesterol in the blood
There are several classes of cholesterol-lowering drugs, but statins are the standard of care. Products containing these substances are said to help reduce LDL by 40-60% and increase “good” cholesterol. However, with a sufficiently high yield, statins cause many negative reactions. Another disadvantage is that you have to drink constantly. Therefore, physicians are required to comprehensively assess all risks and use them with extreme caution.
What is the best cholesterol level to start taking statins? This question can only be answered by a specialist after a comprehensive examination of the patient. Ideally, total cholesterol should be 5.2 mmol/l or less and LDL should be 6-130 mg/dl or less, but statins are not always prescribed, even if this figure rises. Do not use the drug if you are at risk of a heart attack or stroke. If there is a history of myocardial infarction, it can be prescribed even with normal LDL levels.
Do not use the drug if you are at risk of a heart attack or stroke. If there is a history of myocardial infarction, it can be prescribed even with normal LDL levels.
The American Heart Association divides patients into four groups who are encouraged to prescribe these drugs. This includes patients.
- If a high cholesterol condition has existed for the past 10 years and is due to diabetes and hypertension with a long history of smoking.
- I have atherosclerosis. This group also includes patients with cardiovascular disease (CVS) who have undergone stent retention in a coronary artery.
- When LDL is 190 mg/dl or more.
- A diabetic patient whose LDL value is continuously increasing.
One or more patients in these groups should start low to medium dose statins. Perhaps by reviewing your lifestyle and considering your diet, you can lower your cholesterol levels without the use of medicine. However, if a statin is prescribed, it is not possible to discontinue it without consulting a cardiologist.
Keep in mind that complications due to arteriosclerosis, which are in contact with your health with the utmost responsibility, are irreversible and cannot be completely cured. Drugs do not solve existing problems, but only prevent new problems.
It is natural for any person to generate gas. This is a natural reaction that tries to expel excess air in the body.
In many cases, the reason is the specialty of eating habits and the import of specific products. Knowing the food that generates gas can keep you out of trouble.
Which foods cause gas?
All products that can increase gas flashes have certain characteristics.
- Hard to digest.
- Hard to digest.
- Including it in food will not only swallow a lot of air, not only generate gas, but will also make you hungry.
There are 12 types of foods that can increase gas outbreaks.
1. 1.
Beans have been rated as a food that generates gas. The reason is that it contains a lot of Raffino, a compound sugar that is hard to break down in the body. In addition, beans are a source of composite fiber and can increase gas flares.
The reason is that it contains a lot of Raffino, a compound sugar that is hard to break down in the body. In addition, beans are a source of composite fiber and can increase gas flares.
However, not all bean plants produce gas. For example, there are research findings that roasted beans have more gas than black grain beans (varieties with black spots on a white background).
2. Abran family foods such as broccoli
These foods are rich in raffino and dietary fiber. Among them are vegetables.
- cauliflower
- Brussels sprouts.
- Brussels sprouts.
- White cabbage sprout.
3. Whole grain flour.
All grains, except rice, contain raffin and contain a lot of dietary fiber. As a result, gas is more likely to arise, which leads to a feeling of bloating.
Some foods, such as wheat, barley and rye, contain proteins called gluten. And as you know, many people are sensitive to such proteins, from intolerance to celiac disease (a serious autoimmune disease).
4. Fogo
A vegetable used in many dishes and salads. It can be included in meals as well as heated.
Onions contain fructose and are degraded in the intestines during digestion. It is only the digestion of this sugar that facilitates the generation of gas.
5. Garlic
It is often used in dishes, sauces and salads.
It can also increase gas flashes. Some patients show intolerance to garlic and some of the first symptoms increase their bloating and gas.
6. Dairy products
Dairy products contain protein and are a valuable source of calcium, but they can cause gas and bloating in people with lactose intolerance.
According to some reports, more than 75% of people with age lose the ability to digest lactose contained in dairy products [2].
Lactase deficiency can cause symptoms such as bloating, bloating, pain, diarrhea, or conversely, constipation after consumption of dairy products.
7. Sugar substitutes
Sugar alcohols used as sugar substitutes are growing in popularity.
Such food remains undigested until it enters the intestines. Only in the intestine does it begin to decompose and at the same time becomes a breeding ground for the bacteria living there.
It is these bacteria, or rather their vital activity, that increase gas formation.
8. Soda
Sugary carbonated drinks are one of the main causes of increased gas production.
Excessive consumption of carbonated drinks leads not only to excessive consumption of sugar, but also to excessive gas formation.
Frequent shortness of breath to expel excess gas in the stomach.
However, in some cases, gases can accumulate in the intestines.
In addition, some soft drinks contain sugar alcohols, which complicates matters. It turns out that sugary carbonated drinks predispose to gas formation.
9. beer
This is a fermented and carbonated drink.
The process of fermentation and carbonation of carbohydrates leads to additional gas and bloating. Beer also contains gluten, which can exacerbate symptoms in people with food intolerances.
Beer also contains gluten, which can exacerbate symptoms in people with food intolerances.
10. Chewing gum
When you chew gum, you unconsciously swallow a large amount of air, which can accumulate in the stomach and enter the intestines.
Many chewing gums contain sugar substitutes. And in general, it can have certain consequences in the form of an increase in gas production.
11. Lollipops
Lollipops are an excellent source of sugar. When you breathe in the air, you also add fuel to the fire.
Some manufacturers use sugar substitutes to increase demand, which also increases the likelihood of increased gas production.
12. Fatty foods
Such foods slow down digestion and make the body work at a high speed. As with fried foods, a lot of gas accumulates in the intestines.
How to deal with increased gas formation?
Both of these products are often included in the daily diet and are difficult to give up. However, there are a few simple tricks you can follow to reduce gas.
However, there are a few simple tricks you can follow to reduce gas.
- Beans and legumes are soaked in water before cooking.
- Get into the habit of eating slowly so as not to swallow too much air.
- Chewing gum, sweets and carbonated drinks should be limited or completely avoided.
- Keep a food diary to know which foods cause gas.
- Reduce dietary fiber.
- For example, some medicines can help with flatulence, such as cancer medicines and medicines to reduce gas.
List of foods that reduce gas
Experts say that the most effective remedy is to eliminate foods that cause increased gas. However, there are foods that can reduce gas production. What
- tender meat.
- foods such as meat.
- This is an egg.
- Seafood.
- leafy vegetables.
- Certain foods such as tomatoes, grapes and melons.
- This is fig.
- Peppermint oil has the effect of relieving irritable bowel symptoms, which also causes gas generation.

Increased gas: warning signs
In many cases, there is no need to worry about increased gas. Rather, it is often caused by disordered eating habits.
However, the occurrence of excess gas may be the first sign of disease and digestive dysfunction. Therefore, it is necessary to consult a doctor.
Must be excluded during check.
- Gastrian road reflux.
- Hypersensitivity bowel syndrome.
- There are also types of enzyme disorders such as lactase.
- I have food poisoning.
- Intestinal infection
- Become constipated.
- Intestinal condition is bad.
- Specific gynecological disease
An outbreak of gas is a natural process, but sometimes it becomes uncontrollable and can indicate some kind of problem in the body.
By correcting your diet, you can remove most bloated episodes.
Ovulation inducing preparations. Pregnancy injections and pills
There are three types of ovulation inducers: follicle stimulating hormone (FSH), lutein maker (LH), HCG drug, and progesterone.
To get pregnant, you need to meet three basic conditions.
1) A woman is ovulating. 2) Sperm fertilized by an egg. 3) The embryo is firmly attached to the uterus.
handle.
1) A drug that enhances the secretion of FSH and LH, which helps pregnancy, promotes ovulation, which is the development of follicles in the ovaries. 2) HCG helps increase the size of enlarged follicles to release eggs to be fertilized by sperm. 3) Progeosterone prepares to fix the embryo into the inner layer of the uterus and helps to transport the embryo.
A bit of theory: the mechanism of ovulation
Ovulation is when mature eggs are released from the ovaries. The egg then travels through the fallopian tube to the uterus. This usually occurs in the middle of the menstrual cycle, 1 to 4 days after the onset of menstrual bleeding. Women with normal cycles probably won't ask themselves, "Can you get pregnant?" In a normal cycle, ovulation usually occurs regularly.
If you were consulted about why you didn't get pregnant or "you can't get pregnant in one year", you probably didn't ovulate. Women cannot get pregnant without ovulating.
Women cannot get pregnant without ovulating.
If you have a question about why you are not pregnant, you can take an ovulation test. You can buy it at a pharmacy. If there is no continuous ovulation, be sure to consult a doctor.
Ovulation may not occur for various reasons, such as hormonal imbalance and pelvic inflammatory disease. If you don't get pregnant within one year due to not ovulating, you may be given injections and pills to make it easier for your doctor to get pregnant, i.e. medication.
Who is eligible for ovulation stimulation
If the question of why you cannot get pregnant is about you, you can take the test. If your spouse does the same, you can determine the cause of infertility.
Physicians should recommend ovulation induction after a series of tests to obtain accurate evidence of the cause of independent pregnancy problems. In this case, we prescribe a drug that promotes ovulation.
- The patient noticed an unusual phenomenon that eggs mature and are released from the ovaries.
- The couple tried to get pregnant for over a year, but failed.
- Spouse over 35 to 40 not pregnant for six months.
In this case, ovulation stimulation is prohibited in the following cases.
- infertility
- Presence or absence of inflammation of the attached device, presence of disease
- Those with uterine lesions
- When opening of the fallopian tube is bad
FSH and LH preparations. Goal - ovulation
The follicle is affected by FSH and the egg begins to mature in a "pouch" on the surface of the ovaries. To promote follicle growth, the following medications seem to be often prescribed to help ease pregnancy.
- Klostilbegit; "klostilbegit";
- "Klostilbegit"; "Puregon"?
- "Pureogon?"
- Drugs that are useful for pregnancy are selected individually, depending on the results of tests and ultrasound. This document describes the most famous drugs, but not all existing drugs.
"Klostilbegit"
"Cute drugs that are easy to get pregnant" - Crozil l-Fetto is the name given to women who have fulfilled their dreams of giving to children. Promotes the secretion of pituitary hormones. LH (lutein o-hormo n-hormone) - oterus ovulation, that is, eggs are released from the follicles. Milk proractin in the mammary gland.
The instructions say that these drugs that make pregnancy easier should not be taken 5-6 times or more in a lifetime. Otherwise, the ovaries may be depleted early and as a result all the eggs may be used and pregnancy may not be possible. "Clostir Extt", which promotes the maturation of eggs, in principle from 5 to 9day after the onset of menstruation. This pill helps pregnancy and takes once a day.
This drug has an adverse effect on the development of the endometrium. If ultrasound tests reveal that the endometrium is thinner than 8 mm, another drug should be used to promote ovulation. If the endometrium is thin, a fertilized egg is difficult to install in the uterus, and even if you become pregnant, you cannot answer the question "how to get pregnant. "
"
Puregon is included in the list of gonodoric drugs to stimulate the production of pituitary hormones (FSH and LH). Puragon helps the ovaries develop some follicles and ovulate during the menstrual cycle. It is suitable for ovulation induction with both natural pregnancy and artificial insemination in in vitro fertilization.
It complements the absence of FSH and LH, which is the sex hormone, and enhances the concentration of estrogen, the female hormone. As a result, the ovarian follicles begin to grow, and the inner layer of the uterus (endometrium) grows, preparing for the possibility of pregnancy.
Gonadotropin (pituitary activation) such as Pure Gon and Menogon starts to get hemorrhagic hemorrhage on the second day. The period is 10 days, but you need to adjust it with the help of a doctor by observing the reaction of the ovaries with ultrasound.
Ultrasound tests confirm that the follicles have grown to the desired size (20 to 25 mm) and a human gonadotropin (HCG) injection is given. These are also hormones that help pregnancy. HCG is administered one day after the last administration of menogon and puregon. HCG hormones contain drugs such as Pristen, Hrongon, Profra and Gonakor. HCG hormone preparations are only prescribed in doses of 5,000 to 10,000 IU. Ovulation occurs one day after the injection. To aid treatment, he does not have sex for 24 hours after the day before injecting the HCG drugs and after having sex.
These are also hormones that help pregnancy. HCG is administered one day after the last administration of menogon and puregon. HCG hormones contain drugs such as Pristen, Hrongon, Profra and Gonakor. HCG hormone preparations are only prescribed in doses of 5,000 to 10,000 IU. Ovulation occurs one day after the injection. To aid treatment, he does not have sex for 24 hours after the day before injecting the HCG drugs and after having sex.
HCG preparations
Progesterone preparation
If the result of the preparation is positive, proterorone is prescribed. It helps pregnancy "correction". Dufaston and other prozhe locks that are easy to get pregnant are prescribed individually.
In order to solve problems that cannot be given or have children, there are many cases where the above hormone therapy is performed. And because of the development of medicine, more and more women forgot that the thread "can not be born", stood on the bulletin board and realizes the happiness of becoming a mother.
1. Can I get pregnant with polycystic properties? In the case of polycystic ovaries, the chance of a retrieval is very low. The greater the number and size of cysts, the lower the chances of becoming a child.
Frequently asked questions about getting pregnant
2. Can I get pregnant even if I have uterine fibroids? If you have fibroids, the chance of pregnancy will be much lower. The larger the diameter of the nodes, the lower the likelihood of pregnancy.
3. Can I get pregnant from endometriosis? Even if you are diagnosed with endometriosis, you may be pregnant, but it is very rare. Severe endometriosis can cause infertility.
4. Can I get pregnant if my fallopian tubes are blocked? High probability of pregnancy, ectopic pregnancy. It must be removed surgically. However, it is possible to get pregnant with IVF. Implantation of a fertilized egg in the uterus and obstruction of the fallopian tubes is not a problem. In this case, the answer to the question “is it possible to get pregnant?” - "Yes".
5. If the first pregnancy ended in an abortion, can I get pregnant again? Doctors do not recommend terminating a first pregnancy with a surgical abortion. In this case, infertility is more likely. However, this is not the norm and some women successfully give birth to children after multiple abortions.
6. Is it possible to get pregnant from chewing gum? 6.
7. Is it possible to get pregnant if the uterus is bent? Curvature of the uterus is diagnosed as "infertility", but this is by no means an indication, and there are women with a curvature of the uterus who successfully give birth to many children.
8. Can I have a future pregnancy if the fetus from a previous pregnancy was frozen? If a previous pregnancy did not produce an embryo within nine months, the cause should be investigated. Pregnancy is possible.
9. Is it possible to get pregnant after multiple miscarriages? Pregnancy is possible, but it is necessary to find out why previous pregnancies were not tolerated.
10. Can I get pregnant if I have a hormonal imbalance? This is possible, but there may be problems maintaining the pregnancy. Hormone therapy is effective.
11. Is it possible to get pregnant with cervical erosion? Erosion (ectopic) does not affect fertility.
12. Is it possible to get pregnant after 40? Women can get pregnant before menopause.
13. Can I get pregnant with rubella? Does not affect fertility, but may interfere with fetal development.
14. Can I get pregnant after a medical abortion? Medical abortion does not affect the ability to conceive a child in the future.
15. Is it possible to get pregnant with thin endometrium? The thickness of the endometrium does not affect fertility. However, in a thinned embryo, the embryo cannot "take root" and the pregnancy cannot continue.
16. Can I get pregnant after an ectopic pregnancy? 16. However, in the case of an ectopic pregnancy, it is possible that the new zygote will not be able to enter the uterus and will become fixed in the duct.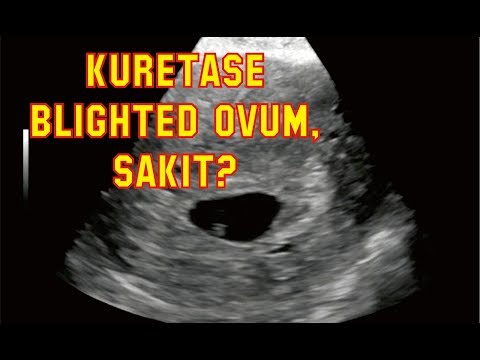 Talk to your doctor about how to prevent another ectopic pregnancy.
Talk to your doctor about how to prevent another ectopic pregnancy.
17. Can I get pregnant even if I have irregular periods? Yes, it's possible. It is wise to find out what causes an irregular menstrual cycle in order to rule out hormonal problems or other abnormalities that may affect the course of pregnancy.
18. Can I get pregnant with an STD? Sexually transmitted diseases, especially sexually transmitted diseases, are the second leading cause of infertility. In such cases, pregnancy is unlikely.
There are a number of so-called folk remedies that promote ovulation and help to conceive a child naturally, but their effectiveness has not been proven by specialists.
Ovulation Stimulation Folk Remedies
When assisting ovulation at home, you can use sage, ghost, aloe vera, etc., which stimulate the necessary processes. The effect is obtained because the vegetable estrogen contained in the herbs works in a similar way to female hormones and causes ovarian storage. The storytelling action is most effective at the beginning of the menstrual cycle. In the second stage, the progesterone secreted from the woman's body and the northern uterus decoction, which is a drug-like drug, is more suitable. The use of essential oils based on siprostradina, basil and anisides, which promote the secretion of estrogen in the body, can promote ovulation. Special diets can help you ovulate just like taking a vitamin, but these places should consult with reproductive medicine and nutritionists to help you choose the most effective and appropriate methods.
The storytelling action is most effective at the beginning of the menstrual cycle. In the second stage, the progesterone secreted from the woman's body and the northern uterus decoction, which is a drug-like drug, is more suitable. The use of essential oils based on siprostradina, basil and anisides, which promote the secretion of estrogen in the body, can promote ovulation. Special diets can help you ovulate just like taking a vitamin, but these places should consult with reproductive medicine and nutritionists to help you choose the most effective and appropriate methods.
In most arts (reproductive care technology), which contains in vitro fertilization (reproductive care technology), the call for such y-ovulation is performed, and the essence is the ovaries receive. This is an incentive. Therefore, it can increase the chance of success in the entire program. Currently, ovulation-induction is performed according to various protocols and medications using it are prescribed. In addition to the trigger, a drug is prescribed to prepare the endometrium for implantation of a fertilized egg. In many cases, gonadotropin, progesterone, chromphene citrate and gonadotropinluticin tropica and an antagonist are included in the regimen. Usually protocols contain drugs from different groups.
In many cases, gonadotropin, progesterone, chromphene citrate and gonadotropinluticin tropica and an antagonist are included in the regimen. Usually protocols contain drugs from different groups.
The clinician selects the dose from the selected stimulus protocol and the patient's individual characteristics. Dose adjustments are made according to the results of follicular ultrasound monitoring. Let's take a closer look at the listed group of drugs.
The essence of the ovaries is the stimulus of the ovaries to get some fertilization in most technology (reproductive care medical care) that contains in vitro fertilization (reproductive care), and receive some fertilization drugs and receive some fertilization. implemented. Therefore, it can increase the chance of success in the entire program. Currently, ovulation-induction is performed according to various protocols and medications using it are prescribed. In addition to the trigger, a drug is prescribed to prepare the endometrium for implantation of a fertilized egg.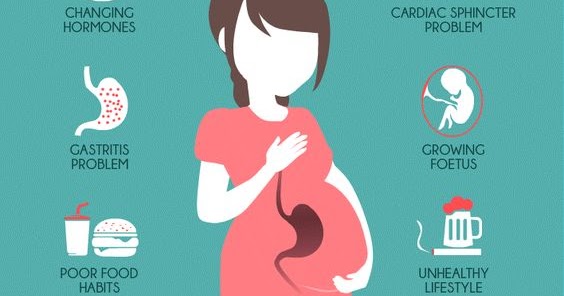 In many cases, gonadotropin, progesterone, chromphene citrate and gonadotropinluticin tropica and an antagonist are included in the regimen. Usually protocols contain drugs from different groups.
In many cases, gonadotropin, progesterone, chromphene citrate and gonadotropinluticin tropica and an antagonist are included in the regimen. Usually protocols contain drugs from different groups.
Find a doctor by referral IVF drugs
The doctor chooses the dose from the selected stimulus protocol and individual patient characteristics. Dose adjustments are made according to the results of follicular ultrasound monitoring. Let's take a closer look at the listed group of drugs.
The essence of the ovaries is the stimulus of the ovaries to get some fertilization in most technology (reproductive care medical care) that contains in vitro fertilization (reproductive care), and receive some fertilization drugs and receive some fertilization. implemented. Therefore, it can increase the chance of success in the entire program. Currently, ovulation-induction is performed according to various protocols and medications using it are prescribed. In addition to the trigger, a drug is prescribed to prepare the endometrium for implantation of a fertilized egg. In many cases, gonadotropin, progesterone, chromphene citrate and gonadotropinluticin tropica and an antagonist are included in the regimen. Usually protocols contain drugs from different groups.
In many cases, gonadotropin, progesterone, chromphene citrate and gonadotropinluticin tropica and an antagonist are included in the regimen. Usually protocols contain drugs from different groups.
Gonadotropins
Helps the growth of follicles (FSH) and follicles.
- Luteinization (LH), estrogen secretion, induces ovulation.
- Some ovulatory agents contain FSH, while others contain both FSH and LH. Commonly used are Menopor, Elomba, Pyragon and Gonar F.
While taking gonadotropins, side effects such as bloating, emotional disorders, and ovarian hyperstimulation syndrome may develop. These phenomena usually disappear immediately after the follicle puncture.
GnRH is produced in the hypothalamus and released in small doses every hour and a half. Under its influence, gonadotropins are formed in the pituitary gland. GnRH agonists are synthetic analogues of this hormone. When more α-GnRH enters the body than nature intended, the pituitary gland becomes insensitive to the hormone and ovulation stops. Thus, the combination of gonadotropin and a-GnRH gives the doctor complete control over the course of the ovarian cycle. The main objectives of such protocols are:
Thus, the combination of gonadotropin and a-GnRH gives the doctor complete control over the course of the ovarian cycle. The main objectives of such protocols are:
Gonadotropin-releasing hormone (a-GnRH) agonists
prolong ovulation period
- prolong pregnancy; prolong pregnancy
- If necessary, slow down the hypersynthesis of gonadotropins.
- Therefore, ovulation should coincide with the time of full maturation of the follicles. For this purpose, drugs such as Decapeptil and Diferelin are often used.
Side effects of α-GnRH administration are associated with changes in the level of sex hormones and are relatively rare. These effects include decreased libido, mood disturbances, and hot flashes. Since agonists do not accumulate in the body, these changes disappear without a trace when taking gonadotropins.
Antagonists generally solve the same tasks as the previous group of drugs, only in a slightly different way. It inhibits the formation of gonadotropins in the pituitary gland and neutralizes the activity of its own gonadotropin-releasing hormone. GnRH Anti-GnRH is used in various protocols to control ovulation, coinciding with the full maturation of follicles. Side effects from the use of antagonists are due to lower estrogen levels and are transient. Specialists in this group usually prescribe Oglartran, which is available in the form of a syringe tube.
It inhibits the formation of gonadotropins in the pituitary gland and neutralizes the activity of its own gonadotropin-releasing hormone. GnRH Anti-GnRH is used in various protocols to control ovulation, coinciding with the full maturation of follicles. Side effects from the use of antagonists are due to lower estrogen levels and are transient. Specialists in this group usually prescribe Oglartran, which is available in the form of a syringe tube.
Gonadotropin-releasing hormone (ant-GnRH) antagonists
Progesterone and estrogen are necessary to prepare the endometrium for embryonic egg implantation. These hormones are normally secreted by a special gland, the so-called corpus luteum, where the follicle opens. If fertilization is successful, the corpus luteum continues to actively secrete progesterone for 10-12 weeks, preventing the release of new eggs and menstruation. From now on, the necessary concentration of progesterone will be supplied by the placenta.
Progesterone and estradiol preparations
Therefore, a certain level of progesterone is necessary to maintain and maintain pregnancy.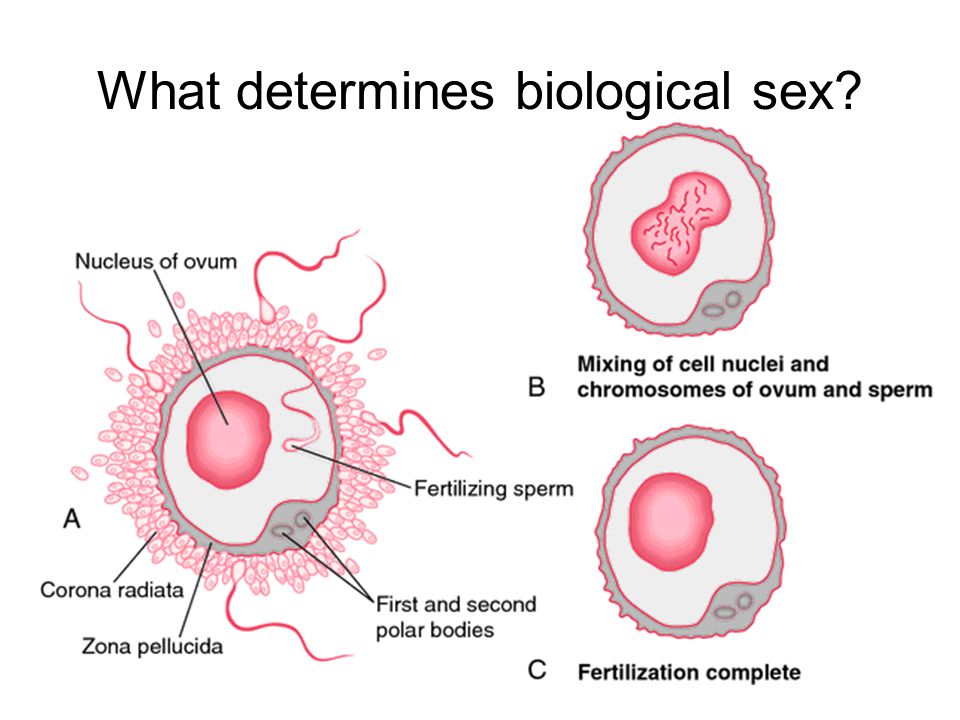 For this purpose, you can use drugs in the form of capsules and tablets: Utrozhestan, Duphaston.
For this purpose, you can use drugs in the form of capsules and tablets: Utrozhestan, Duphaston.
After completion of any stimulation protocol, the follicle should be prepared for puncture to allow final oocyte maturation. For this purpose, chorionic gonadotropin is prescribed 34-36 hours before aspiration of the follicles. In addition, in some protocols, the absence of LH extrusion peaks indicates that ovulation does not occur. Thus, the introduction of human chorionic gonadotropin is the trigger dose that initiates this process.
Chorionic gonadotropin
Ovulation occurs 40-42 hours after injection. Otherwise, the egg will already break away from the follicle and the entire stimulation cycle will go awry. Give this drug once.
Strictly speaking, human chorionic gonadotropin (hCG) is a hormone that is secreted by fetal cells in the placenta as early as 6-8 days after implantation of the ovum and whose measurement is used to diagnose pregnancy. In medicine, hCG preparations obtained from the urine of pregnant women and genetically modified microbial preparations are used. It comes out under different product names like transfer, projection, and chorus, but there really isn't any difference between the two.
In medicine, hCG preparations obtained from the urine of pregnant women and genetically modified microbial preparations are used. It comes out under different product names like transfer, projection, and chorus, but there really isn't any difference between the two.
How you take your medication depends on your stimulation protocol and should be strictly followed by your doctor. Most drugs are administered intramuscularly or subcutaneously. Many of them have unique characteristics regarding the use and storage associated not only with the drug itself, but also with the form of release offered by the manufacturer. Therefore, we recommend doing the first injection in our treatment room. There, the nurse explains how the medicine is administered and, more importantly, shows it to you. We strongly do not recommend giving injections according to instructions on the Internet - the price of a mistake can be very high.
How to use prescribed drugs
Many infertile women have hormonal disorders that affect the development and maturation of follicles.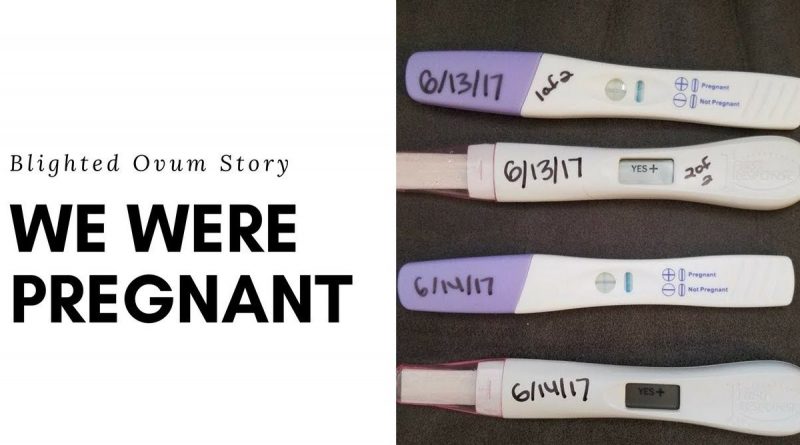 Let me tell you what it is, which sensations are normal and which are not.
Let me tell you what it is, which sensations are normal and which are not.
How long IVF stimulation lasts depends on what drugs are used and what protocols are used. In this case, the prevention of premature ovulation plays an important role. This is achieved by suppressing the secretion of luteinizing hormone, which reaches an overwhelming peak. To inhibit this process, two types of drugs are used: gonadotropin-activating hormones and agonists. The type of drug and how long it is used determines how the ecosystem is stimulated.
How stimulation works before IVF: how many days it lasts, what the consequences may be
Protocol for the use of gonadotropin-releasing hormone antagonists. This group of drugs can immediately stop the natural synthesis of the lutein hormone. It is prescribed approximately 6-8 days after the start of gonadotropins and promotes the growth and maturation of several follicles at once.
- With a long protocol, hormone therapy is started a week before the expected menstruation.
 This puts the woman's body into a brief state of menopause, which can be reached in the next menstrual cycle, with all follicles the same (this process is called "follicular synchronization"). After the menstrual reaction, the introduction of gonadotropins, which stimulate the growth of follicles, begins. The puncture is carried out after about 3-4 weeks.
This puts the woman's body into a brief state of menopause, which can be reached in the next menstrual cycle, with all follicles the same (this process is called "follicular synchronization"). After the menstrual reaction, the introduction of gonadotropins, which stimulate the growth of follicles, begins. The puncture is carried out after about 3-4 weeks. - Protocols for the use of gonadotropin-releasing hormone agonists. There can be 3 types depending on the duration./li>
The Ultradrin protocol is technically no different from the Long protocol, except that the agonists are started at least 2-3 months before artificial insemination. This method of stimulation is recommended for severe endometriosis, when it is necessary to normalize existing disorders first.
All events occur during the same menstrual cycle in which gonadotropin-releasing hormone agonists and gonadotropins are administered. It takes about two weeks until the follicle is received.
Many IVF protocols artificially activate the ovaries.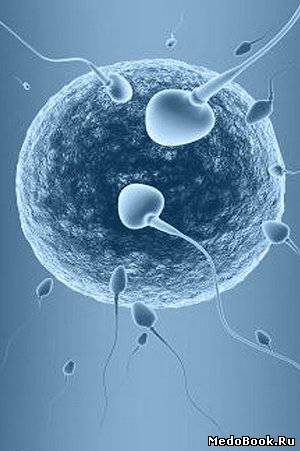 In vitro fertilization in a natural cycle, that is, without or with minimal hormonal activation, is performed in a small number of women. Such methods are sometimes recommended not only with a normal menstrual cycle, but also with a too weak menstrual cycle or, conversely, with too strong classical stimulation. Otherwise, Classic ECO is recommended. with stimulation.
In vitro fertilization in a natural cycle, that is, without or with minimal hormonal activation, is performed in a small number of women. Such methods are sometimes recommended not only with a normal menstrual cycle, but also with a too weak menstrual cycle or, conversely, with too strong classical stimulation. Otherwise, Classic ECO is recommended. with stimulation.
Who needs ovarian stimulation in IVF
First, an ultrasound examination is performed to determine the condition of the follicular apparatus. When using long-term schemes, gonadotropin-releasing hormone pre-initiates the release of gonadotropin architecture. Otherwise, gonadotropins are administered from about the 2nd to the 3rd day and at the same time promote the development of multiple follicles. At the same time, gonadolibrin agonists or antagonists are used to prevent premature ovulation. When the follicle size reaches 18-20 mm, insert the ovulation inducer. Helps separate eggs, including male and female, from the walls of the follicle.
Procedure
Approximately 34-36 hours later, the ovaries are perforated to collect follicles. In laboratory conditions, eggs are extracted from the follicles, fertilized with sperm, and the embryos are cultured before implantation in the uterine cavity. After the puncture, the woman begins taking progesterone preparations.
Depending on the stage of treatment, different groups of drugs are used. Promotes the simultaneous development and maturation of many follicles in the same sense as gonadotropins (recombinant hormones or menopausal hormones). At this stage of reproduction, unpleasant situations await when the follicles begin to develop, but preventively "molt", i.e. premature ovulation occurs. To prevent this, it blocks the peak of ovarian hormones. Ovulation begins when its concentration in the blood rises. Both gonadotropin-releasing hormone agonists and antagonists can be used for blocking.
Ovarian stimulants
Follicles continue to grow during hormone therapy. When the size reaches 18-20 mm, an ovulation inducer is introduced. Ultimately, it seems that they will also help prepare for artificial insemination. Chorionic gonadotropin often acts as an inductor. After the end of ovarian stimulation, the gynecologist prescribes progesterone preparations for successful conception and maintaining pregnancy. It prepares the endometrium for the placement of the embryo. This stage is very important because the corpus luteum, often found in stimulated cycles, is defective.
When the size reaches 18-20 mm, an ovulation inducer is introduced. Ultimately, it seems that they will also help prepare for artificial insemination. Chorionic gonadotropin often acts as an inductor. After the end of ovarian stimulation, the gynecologist prescribes progesterone preparations for successful conception and maintaining pregnancy. It prepares the endometrium for the placement of the embryo. This stage is very important because the corpus luteum, often found in stimulated cycles, is defective.
Ovulation induction usually lasts 2 weeks for the "short" protocol and 3-4 weeks for the "long" protocol. The next two weeks after the follicle puncture is the time of implantation of the fertilized egg. If this treatment is successful, serum chorionic gonadotropin β-blast levels begin to rise after 14 days.
How long can the stimulation last? The reception table is clearly held and issued to women.
How to behave during stimulation
In most cases, ovulation induction is carried out without complications.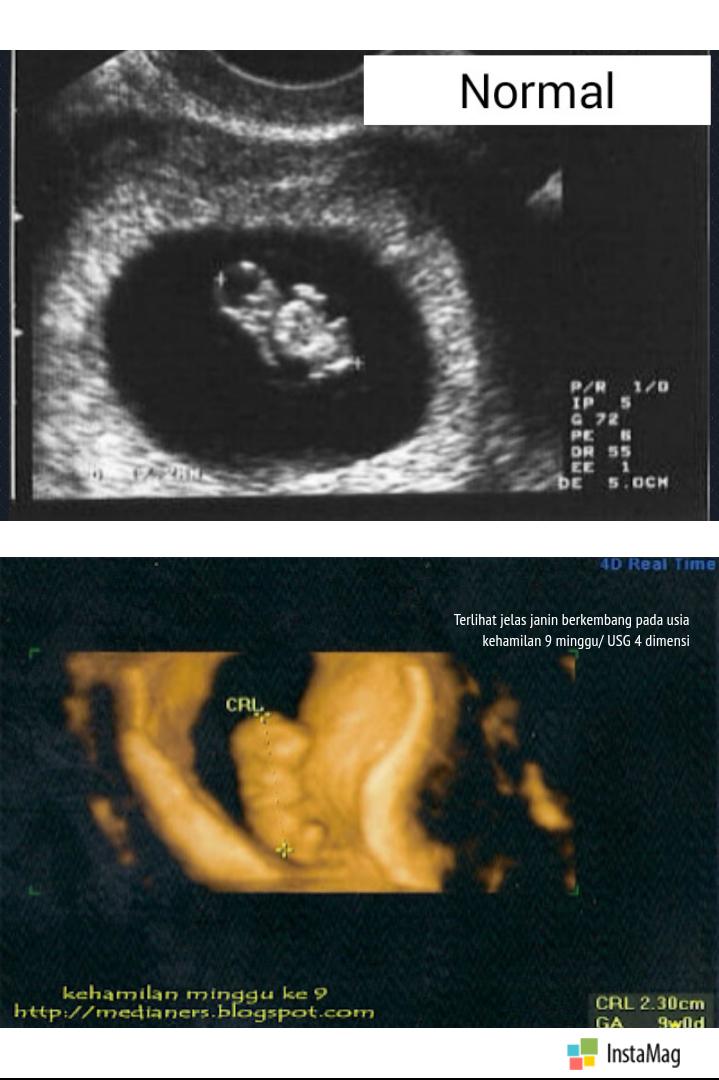 However, at a rate of 5 to 10%, a hybridized syndrome may occur. The initial pattern will appear a few days after ovulation induction (usually 48 hours) and the final pattern will appear 10 days or more later. For early diagnosis for women, it is important to assess the feeling of stimulation. First sign
However, at a rate of 5 to 10%, a hybridized syndrome may occur. The initial pattern will appear a few days after ovulation induction (usually 48 hours) and the final pattern will appear 10 days or more later. For early diagnosis for women, it is important to assess the feeling of stimulation. First sign
Possible complications
Help nausea.
- Pain in the abdomen, especially pain in the groin (protrusion of the ovaries).
- The area around the belly is a little exciting.
- These symptoms are caused by exposure to hormone therapy, increased blood clarity and released into the plasma on the way outside the blood vessels. If you do not notice this condition, the pleural effusion begins to overgrow in the chest cavity, causing shortness of breath. The decrease in plasma circulating plasma lies in the amount of urine as filtration in the kidneys decreases. These are symptoms that can show serious progress in ovarian syndrome. This condition increases the risk of complications of thrombocytosis.
 Therefore, if you feel uncomfortable with the stimulus, you need to contact your doctor immediately. Over time, treatment has become safe and effective using reproductive health care.
Therefore, if you feel uncomfortable with the stimulus, you need to contact your doctor immediately. Over time, treatment has become safe and effective using reproductive health care.
Taking hormonal drugs affects the synthesis of blood vessels. Expand blood vessels and increase the distance between cells. As a result, body fluid is easily transported to the external blood vessel. As a result, the overall state changes as the stimulus continues to stimulate in the Vitro fertilization protocol.
Why the head, chest, ovaries can hurt when stimulated
Headache occurs when the blood vessels of the brain dilate. When fluids are released into the cells of the mammary glands, compression of the nerve leads to dyspnea disorders and the development of chest pain. The ovaries are normal, but may be slightly diseased, that is, if there is no a-irrigation syndrome. This is because the blood flow to these organs is increased through hormones. This increases the volume and compresses the end of the nerve.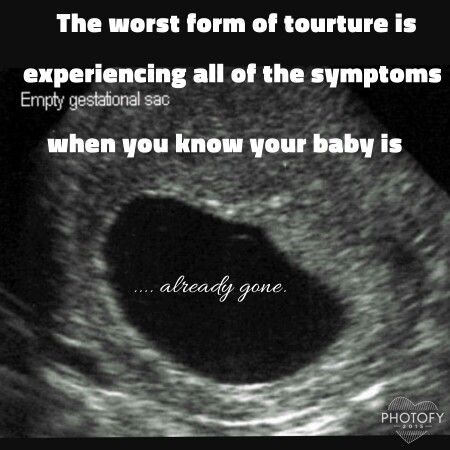 These symptoms usually do not require much discomfort for women, so there is no need for pharmacological correction.
These symptoms usually do not require much discomfort for women, so there is no need for pharmacological correction.
CM-Clinic Reproductive Medicine is compatible with reproductive medical specialists suitable for each case. In order to choose the method of optimal stimulation, the first step is to examine the woman in detail. First, evaluate the ovarian reserve and predict the response of the ovary against stimulation. In response, a specific protocol, drug and initial dose is selected. At the same time, we also prevent complications. Set the optimal number of fertilized eggs to establish the optimal conditions for establishing a pregnancy. If there is a hereditary disease, the couple is diagnosed before the transplant. With them, you can treat as effectively and safely as possible.
Treatment at the SM-Clinic Reproductive Center
SM-Clinic represents cutting-edge results in reproductive medicine and excels. Get expert advice in reproductive medicine to protect your future and that of your children
In the 1980s of the last century, in vitro fertilization began a steady step in reproduction.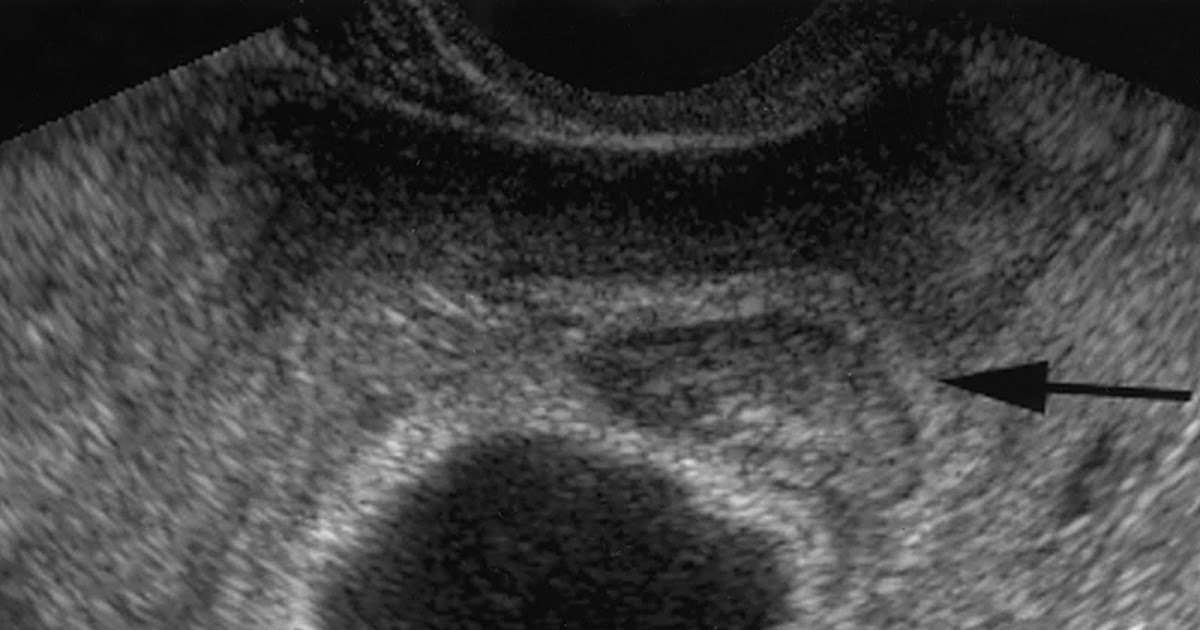 The number of couples relying on this program, looking for the joy of becoming a mother, is growing year after year. However, in vitro fertilization is the only way to fulfill a child's old dream, doctors always weigh the benefits and risks after in vitro fertilization. Taking into account the latest developments in medicine, only a woman's careful attitude to the body allows for the most effective and safe treatment.
The number of couples relying on this program, looking for the joy of becoming a mother, is growing year after year. However, in vitro fertilization is the only way to fulfill a child's old dream, doctors always weigh the benefits and risks after in vitro fertilization. Taking into account the latest developments in medicine, only a woman's careful attitude to the body allows for the most effective and safe treatment.
In vitro fertilization is a multi-step program. The introduction will conduct a detailed study of the couple to determine the cause of the decrease in reproductive capacity and avoid the failure that may occur. Composite tests such as ultrasound tests, hormonal tests, sperm tests, and infectious disease assessment are performed.
The essence of the IVF procedure
After checking, start the ovarian stimulation method. Perform both short-term protocols (stimulating the same cycle as hormone drug administration) and long-term protocols (gonadriberin agonist administration in a previous stimulus to synchronize the ovarian follicle formation process). It's possible. When the follicle reaches 18-20 mm, open the piercing. The embryo then cultured the egg from the follicle solution. It is prepared by a special method and bound to the spermatozoon in the laboratory. It hatches in 3-5 days and is transferred to the uterine cavity. Transplantation can be performed both in a stimulated cycle and in another cycle (first frozen and preserved). After about two weeks, measure the concentration of choriconadotropin in the blood and confirm the pregnancy.
It's possible. When the follicle reaches 18-20 mm, open the piercing. The embryo then cultured the egg from the follicle solution. It is prepared by a special method and bound to the spermatozoon in the laboratory. It hatches in 3-5 days and is transferred to the uterine cavity. Transplantation can be performed both in a stimulated cycle and in another cycle (first frozen and preserved). After about two weeks, measure the concentration of choriconadotropin in the blood and confirm the pregnancy.
There is a risk of in vitro fertilization for women, but it's not that big compared to the general public, so you don't have to be afraid. The gynecologist calculates the complications that may occur for each patient and strives to minimize the possibilities. O.
Should I be afraid of IVF consequences?
External pregnancy is generated in the fallopian tube, excluding the uterine cavity, and is usually caused by dysfunction of the tissue tube. The disease rate during natural pregnancy is 1-2%, which occurs at the same percentage even after in vitro fertilization. To prevent this complication, a woman with an abnormally altered fallopian tube (called a fallopian tube resection) is removed during the preparation stage.
To prevent this complication, a woman with an abnormally altered fallopian tube (called a fallopian tube resection) is removed during the preparation stage.
- A multiple pregnancy is a pregnancy with two or more fertilized eggs. In in vitro fertilization, it can be formed as a result of two or more rewritings, but this is associated with the formation of identical twins (absolutely the same twins are born). A little.
- Ovarian torsion is a condition in which the reproductive stalk in women is distorted and arterial blood flow is obstructed. In this condition, ovarian tissue may be necrotic. Ovarian torsion is a very rare occurrence that occurs at a rate of 0.1% or less per cycle.
- And, although many patients are afraid, we will also touch on the risk of a tumor, which has not been scientifically confirmed.
Ovarian stimuli in infertility treatment for ovarian cancer has been shown to slightly increase the incidence of ovarian cancer compared to a normal reproductive contrast group.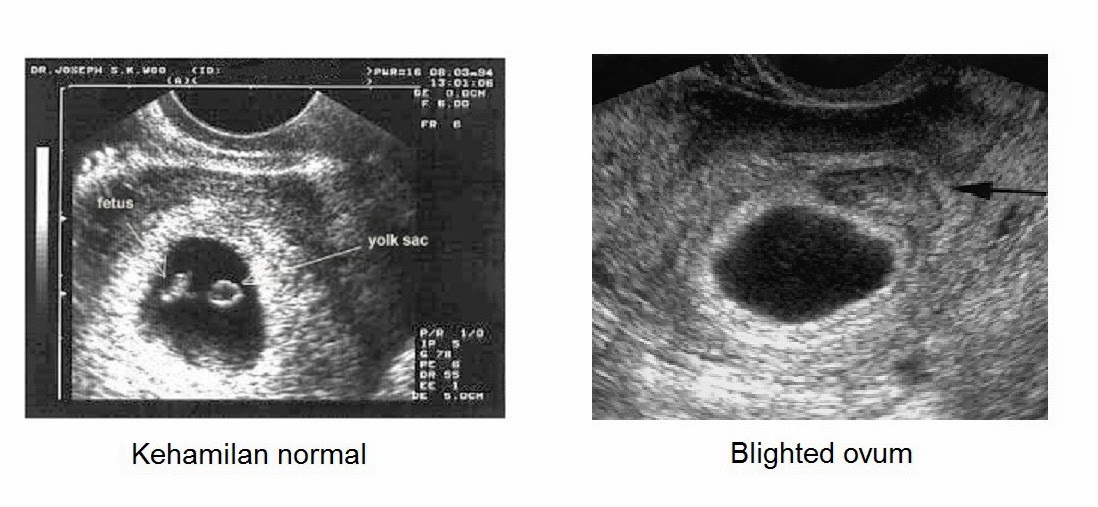 However, an increase in risk associated with tumors has been shown not for stimulation, but in the infertility of the patient. In general, ovulation is known to increase the risk of ovarian cancer and the use of hormonal contraceptives that prevent ovulation reduces the risk.
However, an increase in risk associated with tumors has been shown not for stimulation, but in the infertility of the patient. In general, ovulation is known to increase the risk of ovarian cancer and the use of hormonal contraceptives that prevent ovulation reduces the risk.
- For women who have a slow onset of breast cancer fetuses and first pregnant women, the risk of developing breast cancer is increased. This explains that the baseline risk of infertility in women is high. Serious large studies have shown that the tumor does not increase even if the ovaries are stimulated by the risk of an instant baseline of infertility.
- Uterine cancer (endometrial cancer). Studies have shown that polycystic ovaries and obese women increase the risk of endometrial cancer with increased ovulation stimulation. However, in these patients, the baseline risk of uterine cancer was six times higher regardless of the stimulus in a normal-weight woman.
- Therefore, hormonal stimulation of the ovulation process does not increase the risk of tumors.
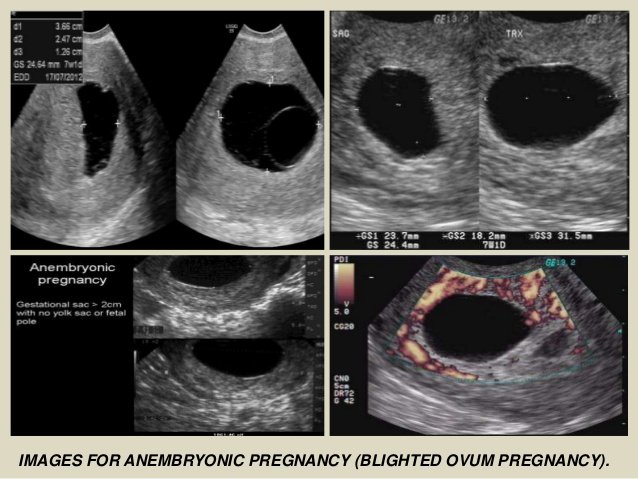 The increase in the possibility of malignant tumors in the uterus, ovaries and mammary glands is mainly due to infertility and baseline risk and due to its cause. Therefore, it is very important to have a normal weight and a suitable hormonal background, and if there is a deviation.
The increase in the possibility of malignant tumors in the uterus, ovaries and mammary glands is mainly due to infertility and baseline risk and due to its cause. Therefore, it is very important to have a normal weight and a suitable hormonal background, and if there is a deviation.
In the process of excessive stimulation, the risk of ovarian syndrome may increase. It is characterized by larger ovaries, enlarged blood vessels, and edema in which fluid accumulates in the abdomen and thoracic cavity. Against the background of a blood thief, the risk of thrombosis increases, which prevents thrombosis.
Risks in the process of inducing superovulation
Ovariate syndrome can last up to the 12th week of pregnancy. In the first days, a few days after the follicle puncture, and in the second half, about 10 days after stimulation, that is, the time when pregnancy is secreted and villogenadotropin is secreted.
In clinical sites, the three severity levels are different. Soft ones make up 5-10%, and heavy ones are often found. Appropriate planning of an ovulation induction program can reduce the risk of these complications, and if an onset develops, the latest medications can quickly stop existing symptoms.
Soft ones make up 5-10%, and heavy ones are often found. Appropriate planning of an ovulation induction program can reduce the risk of these complications, and if an onset develops, the latest medications can quickly stop existing symptoms.
The first symptoms of hyper-asthenia syndrome are as follows.
Feels full in the stomach.
- Enlargement of the abdominal circumference-hemophilia of the stomach;-included germophilia of the abdominal circumference;-Education in the circumference of the abdominal cavity-gastric hemorrhage
- My stomach hurts.
- Sometimes I will participate later.
- irregular breathing
The amount of urine is reduced and the urine is completely out of the urine.
- If you have any symptoms after starting treatment, be sure to check with your doctor.
- Pregnancy that occurs after in vitro fertilization is usually a risk. In fact, luteal phase failure is often seen in the ovaries.
 To make up for the lack of progesterone, a bio-rewarding analogue is prescribed. This prevents a natural pregnancy from ending and prevents placental failure.
To make up for the lack of progesterone, a bio-rewarding analogue is prescribed. This prevents a natural pregnancy from ending and prevents placental failure. - During in vitro fertilization, there are situations where risks are classified. These are the following.
Inflammation of the uterus and attached device.
Risks during childbearing
Repeat rubbing the uterine cavity.
Risk factors contributing to the development of complications
Intervention on the internal organs of the pelvis.
- Obstruction of the ovarian tube (partial or total).
- Overweight or obese
- Polycystic ovary
- Ant-Muller hormone value is 4 ng/ml or more.
- For patients at risk, select the most reasonable treatment. If the risk of fallopian tube pregnancy is high, a fallopian tube ligation is performed. If there is a risk of over-setting syndrome, the use of preserved regimens, etc. is applicable. It is recommended that obese women normalize their weight before entering an in vitro fertilization program.

- Physicians should use technologies that are appropriate for this age, over time, the number of follicles left in the ovaries is small, the quality of eggs decreases, and infertility rates accumulate by the age of five. In addition, the frequency of miscarriage increases. So about 15% for 30 years, about 30% for 40 years, and about 50% for women aged 45 and over naturally.
- All patients 40 years of age and older will be assessed for ovaries (number of follicles remaining in the ovaries) prior to in vitro fertilization planning. To do this, the values of ant-Mulle hormone (AMH) should be measured, an ultrasound test of the ovaries is carried out on the 5th-7th day of the menstrual cycle, and a study of the number of male cells. If the AMH value is 1 ng/mL or less, the response to the ovarian stimulus is considered low. But everything may not be. Approximately 10-20% of patients with lower AMH show a good response to stimulation therapy in in vitro fertilization programs.

Fertility treatment for women over 40 is a struggle with time and the low chance of pregnancy. And because of the large individual differences depending on the patient, there is no universal stimulus protocol for patients with low responses in the in vitro fertilization program. However, there are several ways to increase the impact of reproductive medicine as a doctor's weapon. The preliminary use of male steroids and somatotropin (very expensive drugs), which has a positive effect on the formation of follicles, seems promising.
Consequences after IVF after 40-50 years
If the ovaries are very low, they are preferable, for example, in vitro fertilization in a natural cycle and in vitro fertilization with minimal incentives so as not to be depleted.
The risk assessment associated with fertility treatment has its own characteristics. Therefore, although this risk is relatively low, it will exist in both females and females.
In addition, infertility is suffered by the couple and gives a high motivation for success, making risk assessment difficult. However, SM-Clinic's Reproductive Medicine Specialists will be responsible for addressing the problem of overcoming infertility and will be responsible for the selection of treatments that will affect treatment outcomes.
However, SM-Clinic's Reproductive Medicine Specialists will be responsible for addressing the problem of overcoming infertility and will be responsible for the selection of treatments that will affect treatment outcomes.
In this way, reproductive medicine can achieve high efficacy while reducing the possibility of side effects.
Physician's expert opinion
In vitro fertilization increases the risk of genital cancer. As a result, it was found that the risk is not an in vitro fertilization method, but a pathological condition associated with infertility (polycystic ovaries, obesity, endocrine diseases, etc.).
In vitro fertilization may be harmful to health. For the use of reproductive medicine, it is necessary to take a large number of hormonal drugs that are metabolized in the liver. Therefore, before starting an in vitro fertilization program, a biochemical study is carried out to assess the functional activity of hepatocytes. If it is normal, the treatment will not harm the body.