How to do a well child check
Well-Child Visits: Appointments, Immunizations, and More
Well-child visits are a time when parents can check up on their child’s health and make sure they’re growing and developing normally. Well-child visits usually start a few days after children are born and continue until they turn 18.
There are two kinds of doctors who treat children:
- A pediatrician takes care of children when they’re born up until they become teenagers. Most pediatricians see children up to age 18; however, in some cases, they may continue to see patients until age 21. Some pediatricians have experience with specific diseases, such as pediatric cancer.
- A family physician (FP) is a doctor who takes care of patients of all ages. FPs are trained to take care of children, but they also have training in other areas, such as women’s health or general internal medicine.
The type of doctor you choose depends on what you’re looking for. If you want a doctor who can care for your child through adulthood, you may choose an FP. Or you may decide you’d rather have a doctor who specializes just in children.
Start looking for your child’s doctor early, at least 3 months before your baby is due. Start by checking which doctors are covered under your insurance policy.
If you don’t already have a pediatrician, you can browse doctors in your area through the Healthline FindCare tool.
You can also ask for recommendations from friends, co-workers, and other healthcare providers. The American Academy of Pediatrics and the American Board of Family Medicine maintain lists of board-certified doctors in your area.
Next, schedule a prenatal appointment (an appointment before your child is born). A prenatal appointment is a great time for you to interview your selected physician. During your office visit, consider the following:
- What’s the doctor’s personality like?
- Is the office staff pleasant?
- When is the office open and how busy is it?
- If your child has an emergency or you need to contact the office after hours, who would take care of that?
During a well-child visit, your doctor will:
- perform a physical exam
- give the child any necessary shots, such as immunizations or vaccinations
- track how your child is growing and ask about development and behavior
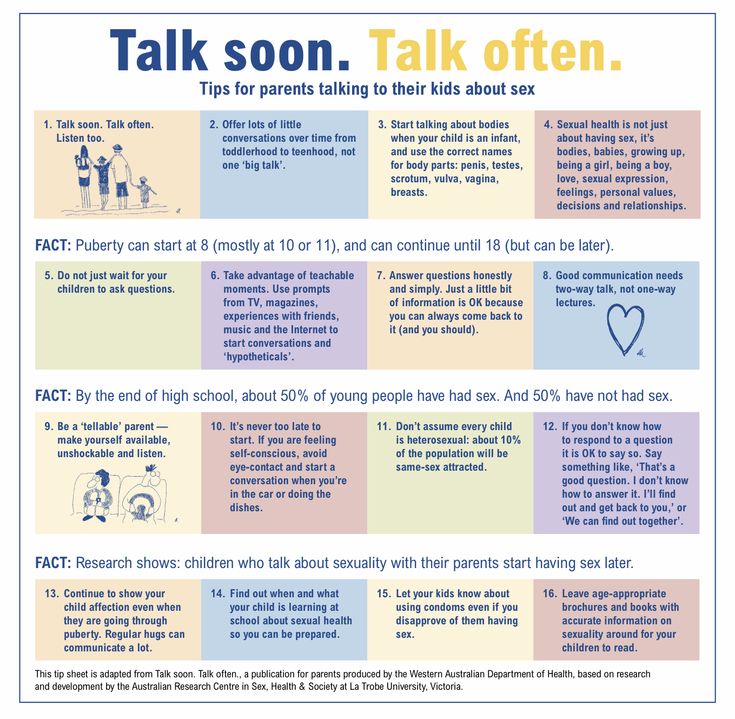
- talk about illness prevention, nutrition and physical fitness, and health and safety issues
- talk about how to handle emergencies and sudden illness
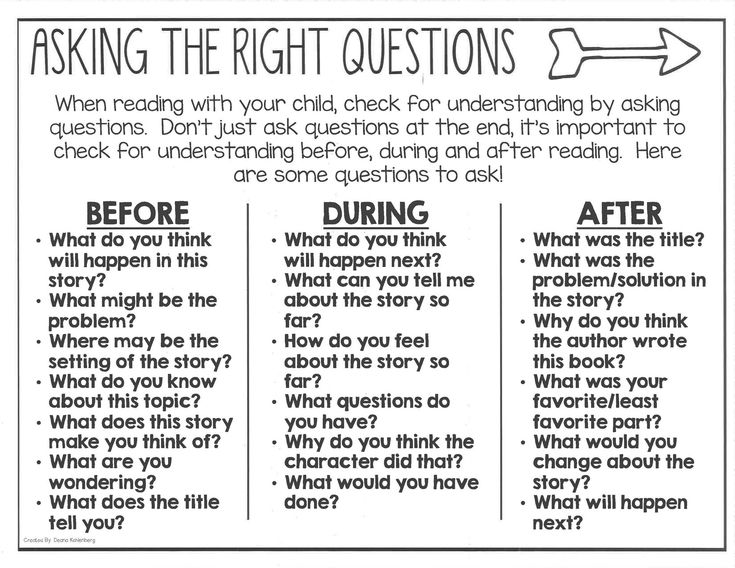
Make sure your doctor isn’t doing all the talking.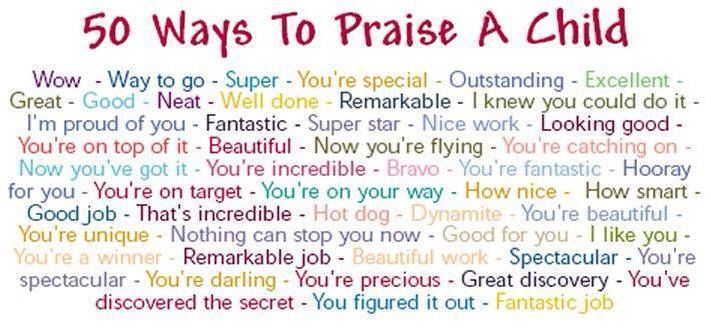 The well-child visit is your best opportunity to bring up any worries about your child’s growth and development, especially if your child isn’t reaching important milestones.
The well-child visit is your best opportunity to bring up any worries about your child’s growth and development, especially if your child isn’t reaching important milestones.
Remember, your doctor may be an expert in children’s health, but you’re the expert on your child.
Also, don’t be afraid to ask questions, medical or otherwise. Your child’s doctor can give you valuable advice on how to promote your child’s learning and development, how to potty train, tips on playground safety, and more.
Vaccinations are an important part of your child’s well-child visit. Some parents worry that these shots can lead to certain health problems.
Researchers at the Centers for Disease Control and Prevention (CDC) have done a number of studies on vaccine use and autism, and they have disproven that there’s a link between the two. Vaccines aren’t only safe, but they also play an important role in keeping all children healthy.
The American Academy of Pediatrics has a recommended schedule of visits for children starting soon after they’re born. You should visit a doctor for a well-child checkup and immunizations, if due.
You should visit a doctor for a well-child checkup and immunizations, if due.
The chart below gives a general idea of when immunizations are given. Note that there can be some variation depending on your child and your doctor’s recommendations.
| Age | Immunizations |
| 3 to 5 days after birth | hepatitis B (Hep B) |
| 1 month old | checkup |
| 2 months old | rotavirus (RV) Hep B diphtheria, tetanus, pertussis (DTaP) Haemophilus influenzae type b (Hib) pneumococcal (PCV) inactivated poliovirus (IPV) |
| 4 months old | RV DTaP Hib PCV IPV |
| 6 months old | RV Hep B DTaP Hib PCV IPV influenza (flu) |
| 9 months old | checkup |
| 12 months old | measles, mumps, rubella (MMR) hepatitis A (Hep A) varicella (chickenpox) Hib PCV Flu |
| 15 months old | DTaP |
| 18 months old | checkup |
| 24 months old | flu |
| 30 months old | checkup |
| 3 years old | flu |
| 4 years old | DTaP IPV MMR varicella flu |
After age 4, a well-child visit should take place every year and should include a physical exam and a growth, developmental, behavioral, and learning assessment.
You can check out the CDC’s recommended immunization schedule.
Your child’s doctor will look at your child’s growth and development at each well-child visit. This includes measuring your child’s weight and height and specific milestones, such as:
At 6 months old
The child should respond to their own name, roll over, and have good hand-eye coordination.
At 1 year old
The child should be able to take a few steps and say simple words, such as “da-da” or “ma-ma.”
At 2 years old
The child should be able to say two- to four-word phrases, begin to run, and start to show signs of being ready for potty training.
At 4 years old
The child should be social with other children, copy some letters and numbers, and have good language skills.
Well-child visits: MedlinePlus Medical Encyclopedia
URL of this page: //medlineplus.gov/ency/article/001928.htm
To use the sharing features on this page, please enable JavaScript.
Childhood is a time of rapid growth and change. Children have more well-child visits when they are younger. This is because development is faster during these years.
Each visit includes a complete physical exam. At this exam, the health care provider will check the child's growth and development in order to find or prevent problems.
The provider will record your child's height, weight, and other important information. Hearing, vision, and other screening tests will be part of some visits.
Even if your child is healthy, well-child visits are a good time to focus on your child's wellness. Talking about ways to improve care and prevent problems helps keep your child healthy.
At your well-child visits, you will get information on topics such as:
- Sleep
- Safety
- Childhood diseases
- What to expect as your child grows
Write down your questions and concerns and bring them with you. This will help you get the most out of the visit.
Your provider will pay special attention to how your child is growing compared to normal developmental milestones. The child's height, weight, and head circumference are recorded on a growth chart. This chart remains part of the child's medical record. Talking about your child's growth is a good place to begin a discussion about your child's general health. Ask your provider about the body mass index (BMI) curve, which is the most important tool for identifying and preventing obesity.
Your provider will also talk about other wellness topics such as family relationship issues, school, and access to community services.
There are several schedules for routine well-child visits. One schedule, recommended by the American Academy of Pediatrics, is given below.
PREVENTIVE HEALTH CARE SCHEDULE
A visit with a provider before the baby is born can be particularly important for:
- First-time parents.
- Parents with a high-risk pregnancy.
- Any parent who has questions about issues such as feeding, circumcision, and general child health issues.

After the baby is born, the next visit should be 2 to 3 days after bringing the baby home (for breastfed babies) or when the baby is 2 to 4 days old (for all babies who are released from a hospital before they are 2 days old). Some providers will delay the visit until the baby is 1 to 2 weeks old for parents who have had babies before.
After that, it is recommended that visits occur at the following ages (your provider may have you add or skip visits depending on your child's health or your parenting experience):
- By 1 month
- 2 months
- 4 months
- 6 months
- 9 months
- 12 months
- 15 months
- 18 months
- 2 years
- 2 1/2 years
- 3 years
- Each year after that until age 21
Also, you should call or visit a provider any time your baby or child seems ill or whenever you are worried about your baby's health or development.
RELATED TOPICS
Elements of the physical exam:
- Auscultation (listening to heart, breath, and stomach sounds)
- Heart sounds
- Infantile reflexes and deep tendon reflexes as the child gets older
- Neonatal jaundice -- first few visits only
- Palpation
- Percussion
- Standard ophthalmic exam
- Temperature measurement (see also normal body temperature)
Immunization information:
- Immunizations -- general overview
- Babies and shots
- Diphtheria immunization (vaccine)
- DPT immunization (vaccine)
- Hepatitis A immunization (vaccine)
- Hepatitis B immunization (vaccine)
- Hib immunization (vaccine)
- Human papilloma virus (vaccine)
- Influenza immunization (vaccine)
- Meningococcal (meningitis) immunization (vaccine)
- MMR immunization (vaccine)
- Pertussis immunization (vaccine)
- Pneumococcal immunization (vaccine)
- Polio immunization (vaccine)
- Rotavirus immunization (vaccine)
- Tetanus immunization (vaccine)
- TdaP immunization (vaccine)
- Varicella (chickenpox) immunization (vaccine)
Nutrition advice:
- Appropriate diet for age -- balanced diet
- Breastfeeding
- Diet and intellectual development
- Fluoride in diet
- Infant formulas
- Obesity in children
Growth and development schedules:
- Infant -- newborn development
- Toddler development
- Preschooler development
- School-age child development
- Adolescent development
- Developmental milestones
- Developmental milestones record -- 2 months
- Developmental milestones record -- 4 months
- Developmental milestones record -- 6 months
- Developmental milestones record -- 9 months
- Developmental milestones record -- 12 months
- Developmental milestones record -- 18 months
- Developmental milestones record -- 2 years
- Developmental milestones record -- 3 years
- Developmental milestones record -- 4 years
- Developmental milestones record -- 5 years
Preparing a child for an office visit is similar to test and procedure preparation.
Preparation steps differ, depending on the child's age:
- Infant test/procedure preparation
- Toddler test/procedure preparation
- Preschooler test/procedure preparation
- School-age test/procedure preparation
- Well baby visits
Hagan JF Jr, Navsaria D. Maximizing children's health: screening, anticipatory guidance, and counseling. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 12.
Kelly DP, Natale MJ. Neurodevelopmental and executive function and dysfunction. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 48.
Kimmel SR, Ratliff-Schaub K. Growth and development. In: Rakel RE, Rakel DP, eds. Textbook of Family Medicine. 9th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 22.
Updated by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
How to develop healthy self-esteem in a child: 3 win-win strategies
Ekaterina Ushakhina
Parents want their child to have a healthy self-esteem, to grow up happy and believe in himself. But what is worth and not worth doing for this? How to educate in such a way as to help the child develop harmoniously?
Melinda Wenner Moyer - science journalist, author, NYU professor and author of How to Raise a Good Person - talks all about self-esteem.
How to raise a good person
We don't know how to build children's self-esteem?
Research has shown that strategies that parents typically use to improve their child's self-esteem often backfire. Some of them actually undermine the child's self-confidence. And some of them push him onto the path of narcissism, nurturing in him an unhealthy idea of his own superiority over everyone else, that he deserves a luxurious life, and that others should be blamed for all his failures.
And some of them push him onto the path of narcissism, nurturing in him an unhealthy idea of his own superiority over everyone else, that he deserves a luxurious life, and that others should be blamed for all his failures.
When we develop in our children the feeling that they are naturally kind, sweet, worthy of love and respect, they stop obsessing over their self-esteem, they do not care what others think of them, they just live their own full lives. But how to cultivate adequate self-esteem in children and not inadvertently spoil them? It's easier than it might seem.
Source
Self-esteem or self-admiration
There is a widespread fear that if children are encouraged to develop healthy self-esteem in every possible way, they can unwittingly turn them into narcissistic narcissists. Narcissism, or narcissism, is far from the same as adequate self-esteem, and this property of character develops according to other laws. It is impossible to over-inflate a child's self-esteem and thereby turn him into a narcissist. There is a big difference between self-sufficient children, confident in their own personal worth, and narcissistic children, or narcissists.
There is a big difference between self-sufficient children, confident in their own personal worth, and narcissistic children, or narcissists.
Children with adequate self-esteem accept and love themselves for who they are, and do not make their sense of self-esteem dependent on the opinions of others.
On the other hand, narcissists are in constant self-comparison mode, convinced that they are the best, but have an overwhelming need to constantly prove their superiority.
How do children become narcissists?
Narcissists are children who are put on a pedestal by their parents. Such parents are convinced that their children are smarter and better than everyone else, and treat them accordingly.
Narcissists are prone to boasting and boasting, criticizing others so that those around them love and admire them, but such behavior eventually turns against them, alienating them from the very people they want to win over to their side. Worse, they rarely seek help to solve their problems. Perhaps because they do not understand that they need it.
Perhaps because they do not understand that they need it.
Note that narcissism begins to form no earlier than seven or eight years.
Up to this age, children can, of course, behave like narcissists, but their declarations from the series “I am the greatest man in the world” are quite appropriate for their level of development and are not a sign that the child will certainly grow up to be Donald Trump.
Self-Esteem Strategy #1: Tell your children you love them for who they are, not for what they do show him your unconditional love and whether he understands your feelings.
On the one hand, we have high expectations for our children, and on the other hand, we do not want them to consider prosperity the most important goal in life. How to combine these two things? There is nothing wrong with wanting a child to be successful; it’s bad when it seems to a child that your love for him depends on his actions and achievements.
Tell your children regularly that you love them, no matter what happens.
If you reward children for good grades or threaten to punish them for bad grades, perhaps you should rethink your behavior. This approach to education is dictated by good intentions and is quite understandable, but by applying it, you unwittingly inspire children with the idea that their significance (value) depends on their school grades.
Sometimes parents express this dependence in passive-aggressive ways - through the so-called conditionally positive and conditionally negative attitude towards the child.
Parents are more kind and generous to their child when they do well in school or win a chess tournament. And they are more impatient and less kind when he receives not the highest mark or just a prize for participating in some competition.
This approach is detrimental to children's self-esteem and emotional health.
Source
Words of encouragement are especially important when you feel your child has low self-esteem. It is quite difficult to determine this, but you can focus on the "red flags". Children with low self-esteem may call themselves "stupid" or "bad", believe that everyone hates them, they are withdrawn, unsociable, avoid difficult tasks, and may intentionally hurt themselves.
Children with low self-esteem may call themselves "stupid" or "bad", believe that everyone hates them, they are withdrawn, unsociable, avoid difficult tasks, and may intentionally hurt themselves.
Another option is also possible: they decide to compensate for their low self-esteem by humiliating other people, engaging in bullying, trying to exercise their power and impose their opinion on people, invent excuses for their failures.
How can you turn moments of disappointment in your own child into an opportunity for his personal growth?
1. Cool down and only then talk to the child. Take a few deep breaths and wait until you can look at the situation through the eyes of a child. Then take note of the child's opinion about what happened: "You must be very upset that everything went wrong."
2. Choose a mild criticism. Start by analyzing the reasons why the child behaved the way they did and not the other way. “I know you didn’t mean it…”, or “You must have not understood what you were doing”, or “I think you tried…” - these phrases will help to start a conversation. Then describe the problem itself. Remember that it was the child's behavior that was bad, not him.
Then describe the problem itself. Remember that it was the child's behavior that was bad, not him.
3. Help your child find ways to solve the problem. Discuss a few ideas, such as writing an apology letter or offering some help.
Self-Esteem Strategy #2: Praise your child, but do it right
What we say to children affects their self-esteem. Research shows this is even more true when it comes to how and why we praise them.
Psychologist Eddie Brummelman has conducted a series of studies showing that when parents over-praise children with low self-esteem, it only makes things worse and their self-esteem drops even lower.
Excessive praise is, in fact, not well-deserved praise. For example, your daughter shows you a sketchy drawing of a man, and you say: “Awesome drawing!” In a 2014 study, Brummelman and colleagues found that parents are more likely to over-praise children with low self-esteem than children with high self-esteem, probably believing that generous praise will stimulate them to increase self-confidence.
Brummelman showed that excessive praise actually makes children with low self-esteem even more self-doubt and avoid difficult tasks.
It is better to praise a child for his efforts, for diligence, and not for skills or abilities. Say more often: “You worked so hard!” - and less often: "You're so smart!"
Praise not only contributes to the formation of motivation, it also affects the level of self-esteem. Children who are praised for their intelligence or skills are more likely to give up when faced with setbacks, they retreat faster in the face of difficulties than those who are praised for hard work; they do not cope well with complex tasks, they have a suppressed sense of self-esteem.
Self-Esteem Strategy #3: Allow your child to experience failure and then rethink how they feel about it
One of the most important responsibilities of parents is to protect their children and keep them safe. However, with an overly heightened parental instinct, the results can be reversed. If we begin to protect children not only from serious dangers, but also from difficult problems and failures, we slow down their development, hold back initiative, and even make them lose self-respect.
If we begin to protect children not only from serious dangers, but also from difficult problems and failures, we slow down their development, hold back initiative, and even make them lose self-respect.
A child with adequate self-esteem is a child who is confident in his own strengths and abilities, who feels that he can cope with any situation, but who also knows that if something goes wrong, he will still be loved and accept it the way it is.
To have such self-confidence, the child must be able to make mistakes, he must know that this is normal and that this will not change the attitude of parents towards him.
Researchers and educators say that now parents are trying too hard to protect their children from any trouble.
Don't stop children from learning something new, as competence is built from the acquired knowledge and skills. This is how self-esteem is formed - from the ability to carry out some kind of activity.
When children are struggling with homework, we should not immediately jump up and rush to help them. Overprotection makes children realize that they are not able to do anything on their own.
Overprotection makes children realize that they are not able to do anything on their own.
Based on the book How to Raise a Good Person.
Article cover: unsplash.com
Orthopedic examination of children in their first year of life - Family Doctor Clinic.
The specialty of an orthopedic doctor is a mystery for many parents. Let's find out what an orthopedist does and why children need to visit him.
The task of an orthopedist is to timely diagnose and treat congenital and acquired disorders of the musculoskeletal system. In the first year of a child's life, an orthopedist is mainly involved in the diagnosis and treatment of congenital disorders.
Ideally, the orthopedist should examine the newborn for the first time in the maternity hospital on the 3rd - 5th day of life. During this period, special attention is paid to rather gross violations of the formation of the musculoskeletal system or intranatal (occurred during childbirth) injuries.
What can be recognized or suspected at this age?
Firstly, gross malformations of the laying and development of the musculoskeletal system, such as aplasia (absence) or hypoplasia (insufficient development) of the limbs or their segments, non-closure of the hard palate (the so-called "cleft palate") and similar deformities. Such congenital malformations, as a rule, are not isolated and are combined with multiple malformations of internal organs, therefore, such children require the closest and most comprehensive examination by other specialists.
Also at this time, small malformations are detected - for example, syndactyly (fusion of fingers or toes together) or polydactyly (presence of additional fingers).
During the examination, the range of motion in the joints is checked and, just at this age, the orthopedist can identify, probably the most important, both in terms of the frequency of occurrence and the severity of the consequences, in the absence of adequate diagnosis and treatment, the pathology - hip dysplasia, and, especially, congenital hip dislocation . It is at this age that when checking the range of motion in the hip joint, it is possible to identify the symptom of a “click” or, more correctly, “slipping” - a slight dislocation and reduction of the hip in the hip joint. Also in the maternity hospital, clubfoot is most often diagnosed - a pathology of the development of the ankle joint.
It is at this age that when checking the range of motion in the hip joint, it is possible to identify the symptom of a “click” or, more correctly, “slipping” - a slight dislocation and reduction of the hip in the hip joint. Also in the maternity hospital, clubfoot is most often diagnosed - a pathology of the development of the ankle joint.
Of the intranatal injuries diagnosed at this age, the most common are cephalohematoma (bleeding under the periosteum of the bones of the cranial vault - more often the parietal bone), characterized by an elastic swelling located within the boundaries of the bone, and a fracture of the clavicle, easily detected by palpation (palpation).
But, unfortunately, not all maternity hospitals have a full-time orthopedist. In this case, the neonatologist partially assumes its functions, and in case of suspicion of the presence of orthopedic pathology, the child is discharged from the maternity hospital with a strong recommendation for an early examination by an orthopedist.
The first examination from the beginning of the observation of the child at the place of residence should occur at the age of 1 month. Examination at this age is also mainly aimed at identifying congenital orthopedic pathology or acquired intranatally. Of all the possible examinations by an orthopedist in the first year of a child's life, an examination at the age of 1 month is probably the most important in terms of timely recognition of congenital pathology and the timeliness of prescribing adequate treatment.
What does an orthopedic examination include?
Before the start of the examination, anamnesis data are collected. Doctors are interested in all the nuances of the pregnancy, especially such as polyhydramnios, increased uterine tone, fetal presentation, how the delivery took place. After collecting an anamnesis, they proceed to a clinical examination.
The child must be seen fully naked. First, a visual examination is carried out, which assesses the correctness of the child's physique, the purity and color of the skin, the shape and position of the head, the proportions of the body segments, the symmetry and position of the limbs at rest, as well as the volume of active movements. This part of the inspection, despite its simplicity, provides a lot of important information. Violation of the correct physique or proportion of body segments is often a marker of multiple congenital pathology or the presence of genetic diseases. Deviation of the head away from the middle position may be one of the signs of torticollis, and the presence of cephalohematoma noticeably changes its shape. Forced or unnatural position of the limb is also an important symptom for the diagnosis of congenital orthopedic pathology (as an example, a strong external rotation of the lower limb in congenital hip dislocation).
This part of the inspection, despite its simplicity, provides a lot of important information. Violation of the correct physique or proportion of body segments is often a marker of multiple congenital pathology or the presence of genetic diseases. Deviation of the head away from the middle position may be one of the signs of torticollis, and the presence of cephalohematoma noticeably changes its shape. Forced or unnatural position of the limb is also an important symptom for the diagnosis of congenital orthopedic pathology (as an example, a strong external rotation of the lower limb in congenital hip dislocation).
Next, the doctor begins the manual - the most important - part of the examination, which reveals the volume of passive movements in the joints of the skeleton, soft tissue turgor and muscle tone. The areas of the joints and bone formations accessible for palpation are also examined by palpation (that is, by probing). Such an examination gives the maximum useful information for the doctor because at this time restrictions on movements in the joints are detected or, conversely, excessive mobility, the presence of bone or joint deformities, pain during movement, muscle protection, and much more. Based on the totality of the information received, called the clinical picture, the doctor decides on the appointment of additional examination methods. Currently, the method of ultrasound diagnostics is very widely used, and ultrasound of the hip joints is even included in the protocol for the mandatory examination of children. If necessary, additional examination methods are prescribed, such as an x-ray, a biochemical blood test, as well as consultations of other medical specialists.
Based on the totality of the information received, called the clinical picture, the doctor decides on the appointment of additional examination methods. Currently, the method of ultrasound diagnostics is very widely used, and ultrasound of the hip joints is even included in the protocol for the mandatory examination of children. If necessary, additional examination methods are prescribed, such as an x-ray, a biochemical blood test, as well as consultations of other medical specialists.
At the conclusion of the examination, recommendations are given to parents on child care, gymnastics, massage, or a plan of therapeutic measures is signed.
If the child is orthopedically healthy, then the next examination is scheduled at 3 months.
An examination at 3 months of age largely duplicates the previous examination both in terms of informational value and in terms of the examination methodology, but, of course, there are some peculiarities.
When examining a three-month-old child, an orthopedist has the opportunity to detect some pathologies that do not always appear in the first 1-2 months of life.
The most striking example of such pathologies can be muscular torticollis, which appeared as a result of a birth injury, which led to a partial rupture of the muscle fibers of the "nodding" muscle. The clinical picture in this type of torticollis often does not appear immediately, but only when an already significant scar is formed in the area of injury.
Taking an anamnesis at this age allows you to find out from parents about the appearance of motor skills in a child, as well as the presence of complaints about the restriction of the child's movements, their pain, forced position of the limbs, and the like.
During a clinical examination, the previous examination is also duplicated, which is supplemented by checking the dynamics of changes in muscle tone, the appearance of motor skills in a child.
If the examination of the child by an orthopedist at 3 months did not reveal any pathology, then in this case the next examination of the child should be performed at the age of 6 months.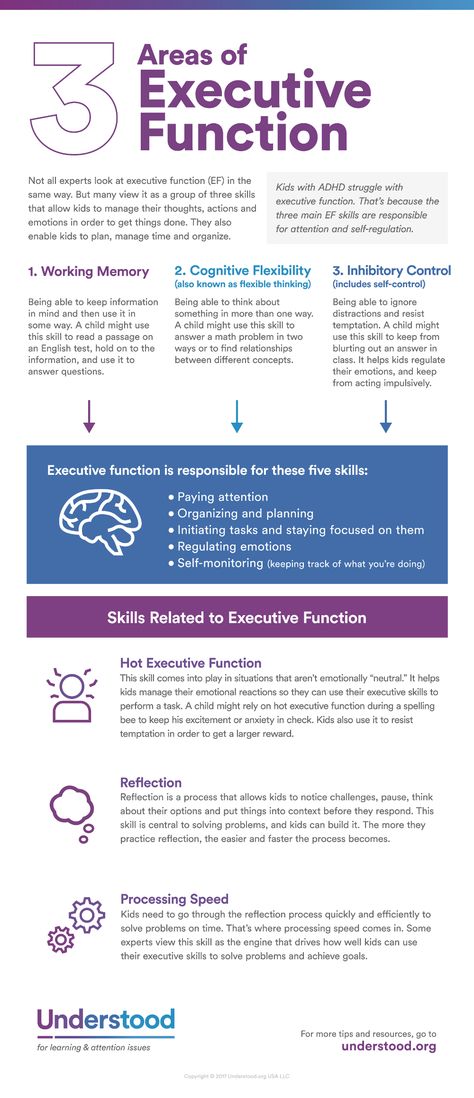
Inspection at 6 months sums up the intermediate result of the development of the child. The main purpose of examining a healthy child at this age is to test the child's motor skills. First of all, the child's ability to turn over, readiness for the "sitting" position is checked. In the presence of previous examinations by an orthopedist, the probability of primary diagnosis of congenital orthopedic disorders is quite small, so the main attention is paid to the dynamics of the child's development and the effectiveness of therapeutic measures.
But do not belittle the importance of a 6-month examination of a child by an orthopedist, since it is during an examination at this age that an orthopedist can identify the presence of metabolic disorders in a child - such as rickets, phosphate - diabetes, and the like. Also, during this examination, the child's readiness for the "sitting" position and other motor skills are revealed and recommendations are made to create conditions for the development of the child in the next six months.