How to avoid toxoplasmosis during pregnancy
CDC - Toxoplasmosis - General Information
On This Page
- When should I be concerned about toxoplasmosis?
- How can Toxoplasma affect my baby?
- How do I know if I have been infected with Toxoplasma?
- How is toxoplasmosis spread?
- Do I have to give up my cat if I’m pregnant or planning on becoming pregnant?
- Is there treatment available for toxoplasmosis?
- What are the best ways to protect myself or my baby against toxoplasmosis?
- Can I breastfeed my baby if I contracted a Toxoplasma infection during pregnancy?
When should I be concerned about toxoplasmosis?
Generally, if you were infected with Toxoplasma before becoming pregnant your baby is protected by your immunity. Some experts suggest waiting for 6 months after a recent infection to become pregnant.
How can
Toxoplasma affect my baby?If you are newly infected with Toxoplasma while you are pregnant, or just before pregnancy, then you can pass the infection on to your baby. You may not have any symptoms from the infection. Most infected infants do not have symptoms at birth but can develop serious symptoms later in life, such as blindness or mental disability. Occasionally, infected newborns have serious eye or brain damage at birth.
How do I know if I have been infected with
Toxoplasma?Your health care provider may suggest one or more varieties of blood tests to check for antibodies to Toxoplasma.
How is toxoplasmosis spread?
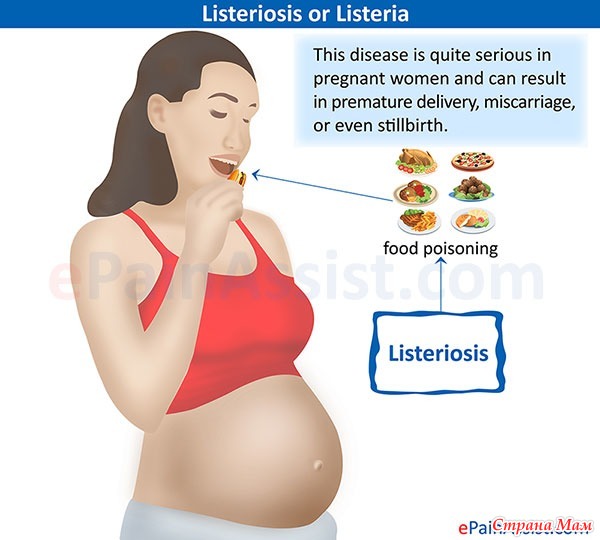
Cats play an important role in the spread of toxoplasmosis. They become infected by eating infected rodents, birds, or other small animals. The parasite is then passed in the cat’s feces. Kittens and cats can shed millions of parasites in their feces for as long as 3 weeks after infection. Mature cats are less likely to shed Toxoplasma if they have been previously infected. Cats and kittens prefer litter boxes, garden soils, and sandboxes for elimination, and you may be exposed unintentionally by touching your mouth after changing a litter box, or after gardening without gloves. Fruits and vegetables may have contact with contaminated soil or water also, and you can be infected by eating fruits and vegetables if they are not cooked, washed, or peeled.
Fruits and vegetables may have contact with contaminated soil or water also, and you can be infected by eating fruits and vegetables if they are not cooked, washed, or peeled.
Cats play an important role in the spread of toxoplasmosis.
Do I have to give up my cat if I’m pregnant or planning on becoming pregnant?
No. You should follow these helpful tips to reduce your risk of environmental exposure to Toxoplasma:
- Avoid changing cat litter if possible. If no one else can perform the task, wear disposable gloves and wash your hands with soap and water afterwards.
- Ensure that the cat litter box is changed daily. The Toxoplasma parasite does not become infectious until 1 to 5 days after it is shed in a cat’s feces.
- Feed your cat commercial dry or canned food, not raw or undercooked meats.
- Keep cats indoors.
- Avoid stray cats, especially kittens. Do not get a new cat while you are pregnant.
- Keep outdoor sandboxes covered.

- Wear gloves when gardening and during contact with soil or sand because it might be contaminated with cat feces that contain Toxoplasma. Wash hands with soap and water after gardening or contact with soil or sand.
More on: Handwashing
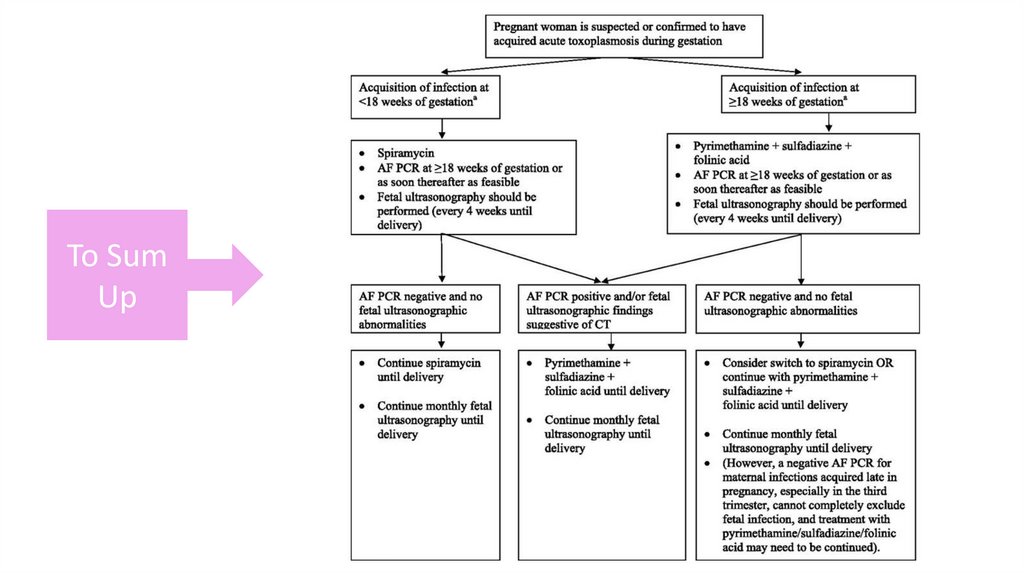
Is there treatment available for toxoplasmosis?
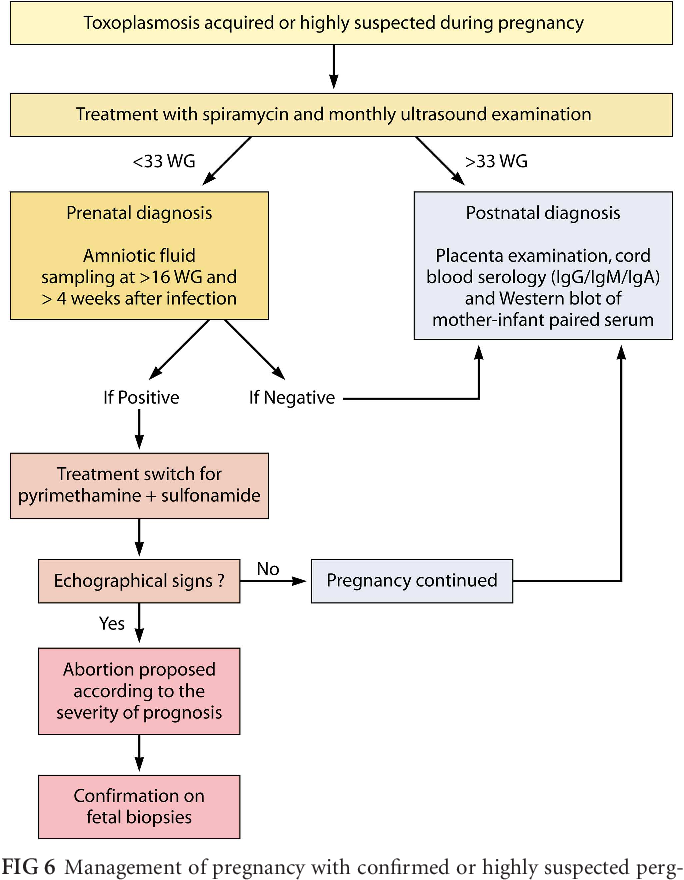
If you are infected during pregnancy, medication is available. You and your baby should be closely monitored during your pregnancy and after your baby is born.
What are the best ways to protect myself or my baby against toxoplasmosis?
Cat owners and women who are exposed to cats should follow these tips to reduce exposure to Toxoplasma.
- Avoid changing cat litter if possible. If no one else can perform the task, wear disposable gloves and wash your hands with soap and water afterwards.
- Ensure that the cat litter box is changed daily. The Toxoplasma parasite does not become infectious until 1 to 5 days after it is shed in a cat’s feces.
- Feed your cat commercial dry or canned food, not raw or undercooked meats.
- Keep cats indoors.
- Avoid stray cats, especially kittens. Do not get a new cat while you are pregnant.
- Keep outdoor sandboxes covered.
- Wear gloves when gardening and during contact with soil or sand because it might be contaminated with cat feces that contain Toxoplasma. Wash hands with soap and water after gardening or contact with soil or sand.
- Wash your hands and safely diaper and feed your baby.
Along with washing your hands, you should also:
- Cook food to an internal temperatures high enough to kill harmful pathogens like Toxoplasma. The only way to tell if food is safely cooked is to use a food thermometer. You can’t tell if food is safely cooked by checking its color and texture (except for seafood).
- Use a food thermometer to ensure foods are cooked to a safe internal temperature. Learn how to place the thermometer correctlyin different food to get an accurate reading.

- Whole cuts of beef, veal, lamb, and pork, including fresh ham: 145°F (then allow the meat to rest for 3 minutes before carving or eating)
- Fish with fins: 145°F or cook until the flesh is opaque and separates easily with a fork
- Ground meats, such as beef and pork: 160°F
- All poultry, including ground chicken and turkey: 165°F
- Leftovers and casseroles: 165°F
- Check this chart for a detailed list of temperatures and foods
- Freeze meat for several days at sub-zero (below 0° F) temperatures before cooking to greatly reduce chance of infection. *Freezing does not reliably kill other parasites that may be found in meat (like certain species of Trichinella) or harmful bacteria.
- Avoid drinking untreated water.
- Do not drink unpasteurized goat’s milk.
- Do not eat raw or undercooked oysters, mussels, or clams (these may be contaminated with Toxoplasma that has washed into seawater).
- For more information on safe food handling to help reduce foodborne illness visit the Food Safety website.
Can I breastfeed my baby if I contracted a
Toxoplasma infection during pregnancy?Yes. Breast milk transmission of Toxoplasma infection is not likely. While Toxoplasma infection has been associated with infants who consumed unpasteurized goat’s milk, there are no studies documenting breast milk transmission of Toxoplasma infection in humans. If a nursing woman were to experience cracked and bleeding nipples or breast inflammation within several weeks following recent Toxoplasma infection (when the organism is still in her bloodstream), it is theoretically possible that she could transmit Toxoplasma to the infant through her breast milk. Immune suppressed women could have Toxoplasma in their bloodstream for longer periods of time. However, the likelihood of human milk transmission is still very small.
External
Back To Top
Toxoplasma Prevention Before You Become Pregnant - Food Safety for Moms to Be
En español
Toxoplasma: Prevention
Before You Become PregnantDid you know that you could feel healthy, but still have toxoplasmosis? This foodborne illness is caused by the parasite, Toxoplasma gondii, and it could be harmful to you and your baby if you become pregnant. Here are some answers to frequently asked questions about toxoplasmosis.
"What is Toxoplasma gondii?"
It's a parasite found in raw and undercooked meat; unwashed fruits and vegetables; contaminated water; dust; soil; dirty cat-litter boxes; and outdoor places where cat feces can be found. It can cause an illness called toxoplasmosis, which can be particularly harmful to you and your baby.
"I'm not pregnant - so why should I be concerned about toxoplasmosis?"
If you have a cat and are thinking about becoming pregnant, you may be at risk for toxoplasmosis. T. gondii infects essentially all cats that spend any time outdoors. Cats get this parasite by eating small animals or raw meat that's infected. The parasite is then passed on through the cat's feces. It doesn't make the cat sick, so you may not know if your cat has the parasite.
T. gondii infects essentially all cats that spend any time outdoors. Cats get this parasite by eating small animals or raw meat that's infected. The parasite is then passed on through the cat's feces. It doesn't make the cat sick, so you may not know if your cat has the parasite.
You can become exposed to T. gondii by accidental ingestion of contaminated cat feces, which can occur if you touch your hands to your mouth after gardening, cleaning a litter box, or touching anything that comes in contact with cat feces. Over time, the parasite can enter your blood stream. It usually takes about a week. If you become pregnant while the parasite is still in your blood, it can pass through the placenta to your unborn child. You can also get toxoplasmosis by eating raw or undercooked meat or drinking water contaminated with T. gondii. So, you should eat thoroughly cooked meat.
See the Apply the Heat for the recommended cooking temperatures for meat.
"How would I know if I have toxoplasmosis?"
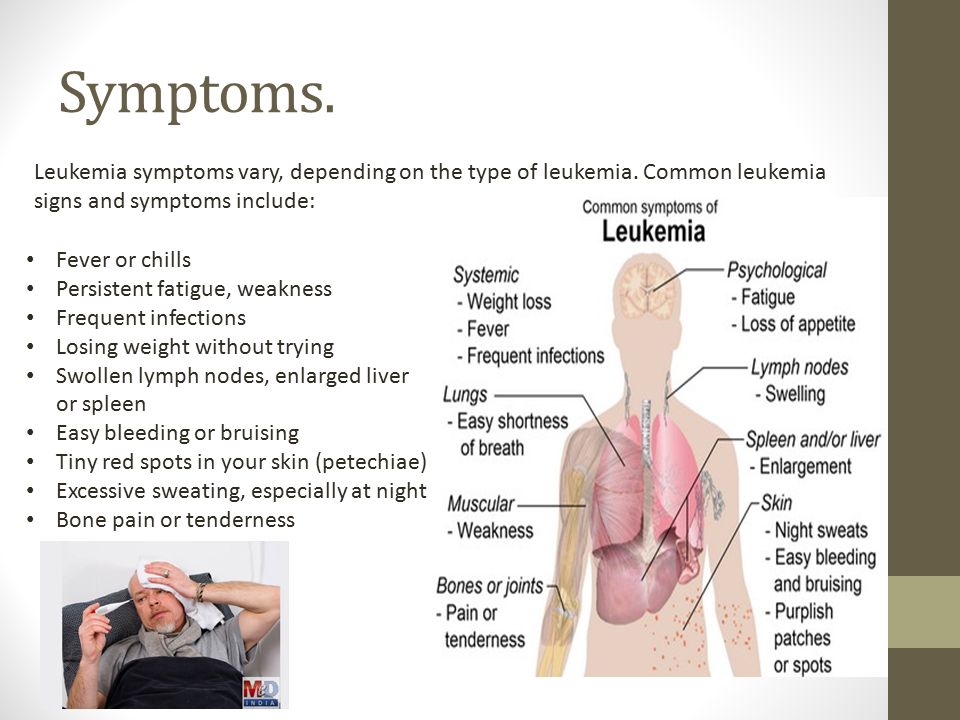
Toxoplasmosis can be difficult to detect. However, symptoms typically include: swollen glands, fever, headache, muscle pain, or a stiff neck. Only 10% of women infected with the parasite have noticeable symptoms - so you could have toxoplasmosis without even being aware that you're ill. If you do experience any of the above symptoms, see your doctor or healthcare provider immediately.
However, symptoms typically include: swollen glands, fever, headache, muscle pain, or a stiff neck. Only 10% of women infected with the parasite have noticeable symptoms - so you could have toxoplasmosis without even being aware that you're ill. If you do experience any of the above symptoms, see your doctor or healthcare provider immediately.
Fact: About 85% of pregnant women in the U.S. are at risk of being infected with toxoplasmosis.
(American Journal of Epidemiology)
"How could toxoplasmosis affect my baby?"
In babies, T. gondii can cause hearing loss, intellectual disability, and blindness. Some children can develop brain or eye problems years after birth. Children born infected with T. gondii can also require years of special care, including special education and ophthalmology care. Early identification and treatment of children infected with T. gondii is essential in order to minimize the parasite's effects.
Facts:
- It's estimated that toxoplasmosis infects between 300 and 4,000 fetuses in the U.
 S. each year.
S. each year.
(Centers for Disease Control and Prevention) - About 50% of toxoplasmosis infections in the U.S. each year are acquired from food.
(Centers for Disease Control and Prevention)
"If I've had toxoplasmosis, how long should I wait before I become pregnant?"
Some experts suggest waiting for 6 months after infection to become pregnant. Women who become infected can be treated with medications to clear up the infection.
"How can I prevent toxoplasmosis?"
If you have a cat, you should:
- Have someone else change the litter box, if possible. If you have to clean it, wear disposable gloves and wash your hands thoroughly with soap and warm water afterwards.
- Change the litter box daily. The parasite doesn't become infectious until 1 to 5 days after it's shed in the feces.
- Wear gloves when gardening in a garden or handling sand from a sandbox because cats may have excreted feces in them.
 Be sure to wash your hands with soap and warm water afterwards.
Be sure to wash your hands with soap and warm water afterwards. - Cover outdoor sandboxes to prevent cats from using them as litter boxes.
- Feed your cat commercial dry or canned food. Never feed your cat raw meat because it can be a source of the T. gondii parasite.
- Keep indoor cats indoors. Be especially cautious if you bring outdoor cats indoors.
- Avoid stray cats, especially kittens.
- Don't get a new cat while you're pregnant.
"If I own a cat that goes outside, should I be tested?"
Yes, to be safe. Also, see your doctor or healthcare provider if you have questions about toxoplasmosis.
Note: See your doctor or healthcare provider if you have questions about toxoplasmosis.
For more information on how to prevent toxoplasmosis, see Toxoplasma.
Toxoplasmosis and pregnancy
Pruzhany st. Mitskevicha, 27 (016 32) 3-41-80, 3-42-95
Mitskevicha, 27 (016 32) 3-41-80, 3-42-95
- Order a ticket
- Question and answer
- Consultation
Toxoplasmosis is a fairly rare opportunistic infection caused by protozoa that parasitize mainly in the body of representatives of the feline family - Toxoplasma. This disease is especially dangerous for people with severe immune system disorders and for pregnant women. In the latter case, the time of infection of a woman with toxoplasma matters: it happened before or during pregnancy. nine0005
If a woman falls ill even before pregnancy, then her unborn child is absolutely not threatened. However, it is much worse if the expectant mother "catch" toxoplasmosis already during pregnancy. In this case, the pathogens of toxoplasmosis can penetrate the mother's placenta to the fetus, causing various disorders in it, ranging from congenital toxoplasmosis to severe congenital malformations and intrauterine death.
For the prevention of the disease, it is important to remember that the source of toxoplasmosis is most often domestic cats (and especially kittens), which excrete the infectious agent into the environment along with feces, as well as raw minced meat and insufficiently thermally processed meat. nine0005
nine0005
When registering for pregnancy, every woman undergoes a serological examination to detect toxoplasmosis in order to prevent possible infection. A positive test result and the detection of IgG to toxoplasma indicate that the expectant mother has already been in contact with the pathogen before pregnancy and can now be absolutely calm. In this case, toxoplasmosis is absolutely not dangerous for her baby, and there is no need to repeat this analysis both in this and in all subsequent pregnancies. However, if antibodies to Toxoplasma were not detected according to the results of the study (the test result is negative), you must be careful and strictly follow the rules below in order not to endanger the health of the unborn baby. In order to prevent toxoplasmosis, a pregnant woman (as well as all other categories of persons) should:
- avoid eating raw and undercooked meat, and never taste raw minced meat, as these products may contain pathogens of toxoplasmosis
- Wash fruits and vegetables thoroughly under running water before eating
- wash cutting boards and utensils, hands with warm soapy water after contact with raw meat and unwashed fruits and vegetables
- do not drink water from open sources nine0009 do not let domestic cats outside and in no case pet stray cats and dogs that can be sick with toxoplasmosis
- feed domestic cats only canned and dry food, or well-cooked food
- avoid contact with cat litter during pregnancy, and if this is not possible, remove cat excrement daily using gloves and thoroughly washing hands afterwards with warm water and soap
- use gloves when in contact with soil and sand, while working in the garden, etc.
- during pregnancy, regularly, at intervals of 1-2 months, undergo examination for the presence of toxoplasmosis, so that in case of infection, timely prevention of the disease in the fetus can be started
If, despite all the precautions you have taken, you still get toxoplasmosis, do not panic and contact your infectious disease doctor as soon as possible. He will help you choose an effective and at the same time safe treatment for pregnancy. nine0005
Freelance district infectious disease specialist But T.A.
Tips
Tips for parents on preventing bad habits in teenagers
Until the ambulance arrives.
All Tips
Articles
Prevention of helminthiases
On the prohibition of the sale of electronic smoking systems to minors
All articles
Toxoplasmosis and pregnancy - prevention
Toxoplasmosis is a rather dangerous infectious disease that can lead to serious pathologies. At the same time, a person cannot get infected from a person. Infection occurs as a result of organ transplantation, blood transfusion or in utero, that is, from mother to child. nine0005
At the same time, a person cannot get infected from a person. Infection occurs as a result of organ transplantation, blood transfusion or in utero, that is, from mother to child. nine0005
Prevention of toxoplasmosis
Pregnancy for almost every woman is the expectation of a long-awaited baby. In this regard, every expectant mother worries about his health even during her planning and pregnancy. After all, quite often the health of a child who has not yet been born is threatened by many different infections, including the genitourinary system.
Toxoplasmosis is an infectious disease caused by the intracellular parasite Toxoplasma gondii. We can say that for a person this disease is practically not dangerous. nine0005
Usually, the patient becomes infected by swallowing this intracellular pathogen. For humans, cats are often the source of infection, which become infected by eating contaminated raw meat. Animals release the pathogen into the environment with faeces, which retains its infectious properties for at least one year.
In addition, the infection can also be transmitted to humans through unpasteurized milk and meat that has undergone weak heat treatment. A person with toxoplasmosis is not a carrier of the infection, and therefore another person cannot become infected from it. The exception is organ transplantation, blood transfusion and intrauterine infection (mother-fetus). nine0005
Symptoms of toxoplasmosis
With the gradual course of inflammatory processes in the fetus, hydrocephalus or dropsy of the brain develops, changes in the eyes are observed. The chronic course of toxoplasmosis causes quite serious changes in the central nervous system, the process of which is irreversible. As a rule, this is blindness, mental retardation of the child and other pathologies.
Consequences of infection with toxoplasmosis in pregnant women
Doctors pay special attention to this disease during pregnancy. If a woman catches this infection while carrying a child, then there is a high probability that the fetus will also be infected with toxoplasmosis, because the infection spreads through the placenta.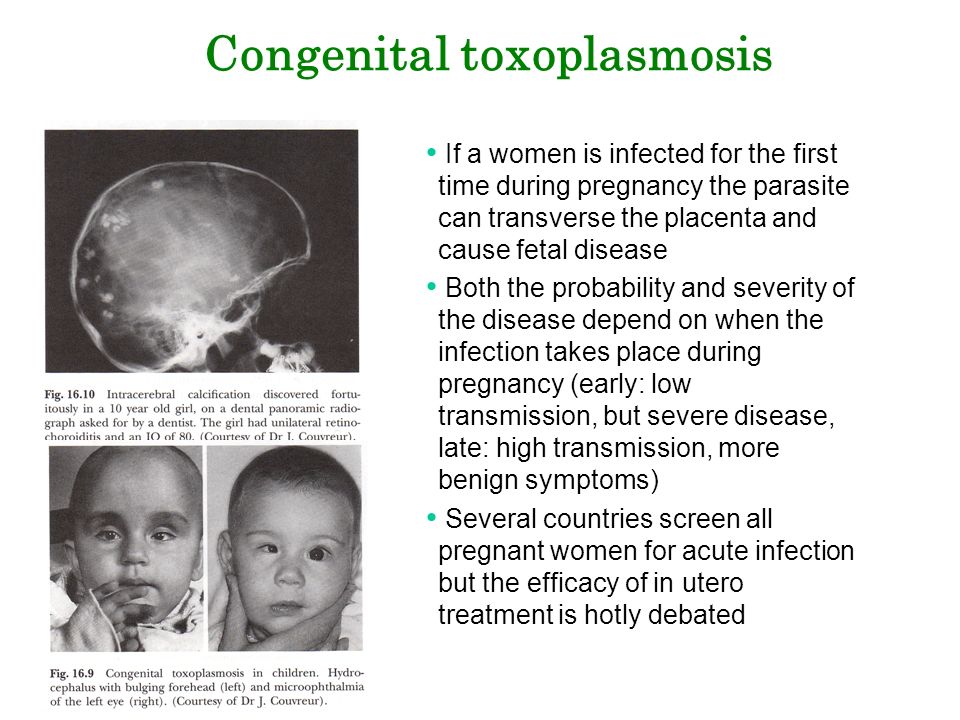 nine0005
nine0005
It is worth noting that contracting a disease in the first trimester has more severe consequences than in the third. The consequences are different, including spontaneous miscarriage or intrauterine death. If the fetus survives, then there is a high probability that the child will be born with congenital toxoplasmosis. Less than 25% of newborns diagnosed with congenital toxoplasmosis have visible signs of infection from birth: low weight, enlarged spleen and liver, anemia, jaundice, and convulsions. The rest of the children have no symptoms at birth, however, over time, the possible manifestation of blindness, deafness and mental retardation. nine0005
True, not all women who had toxoplasmosis during pregnancy give birth to a child with this congenital disease. The probability that the infection will be transmitted by the mother to the child is on average 45-50%.
Fortunately, the incidence of toxoplasmosis infection during pregnancy is negligible and amounts to 1 to 5 cases per one thousand women in the position.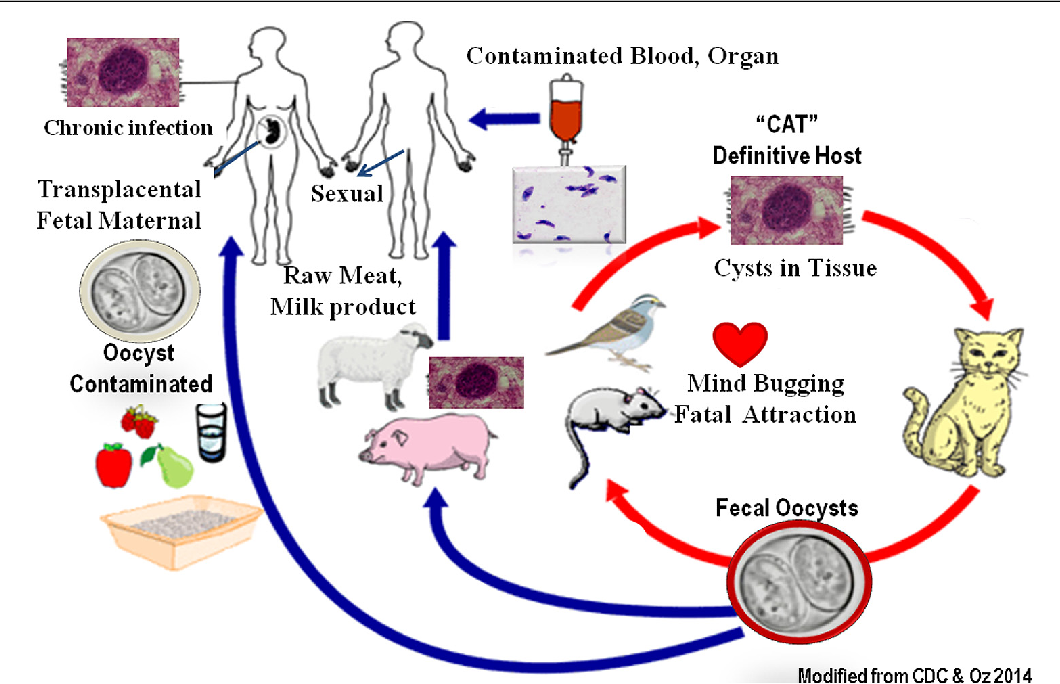
If at some time in the past (before pregnancy) a woman had been ill with toxoplasmosis, then her body developed protective factors, the so-called antibodies, which formed immunity to this pathogen. They then provide protection to the fetus from congenital infection if, during pregnancy, the expectant mother meets again with Toxoplasma gondii. We can safely say that a woman who has antibodies to toxoplasmosis by the beginning of pregnancy has no reason to worry. It is worth emphasizing that about 30% of the population already has immunity to this disease. nine0005
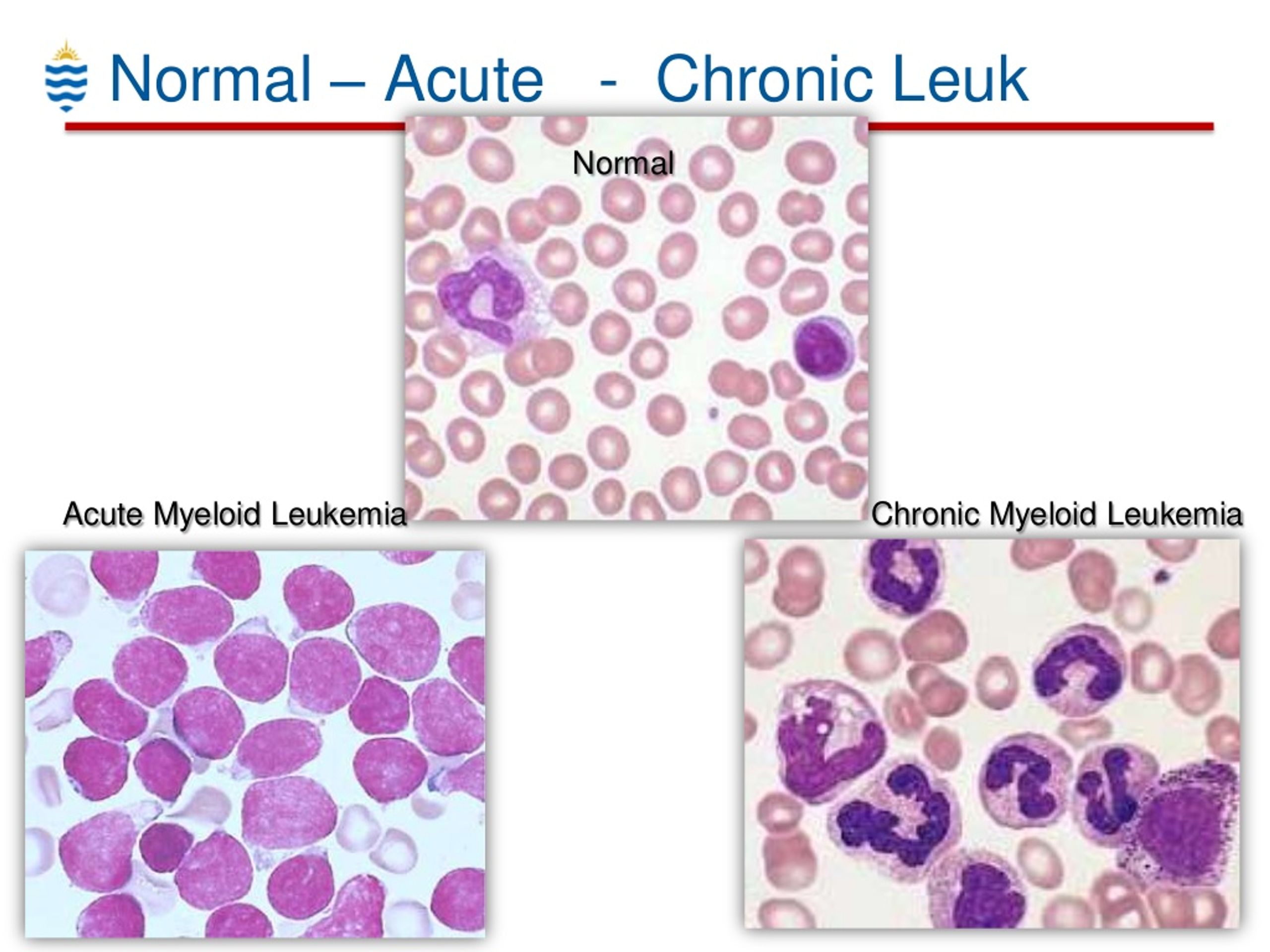
Diagnosis of toxoplasmosis
As already described above, the most severe forms of the disease occur in children who become infected during the prenatal period of development. For this reason, it is very important to diagnose this disease during pregnancy.
If IgG and IgM antibodies are detected in a pregnant woman's blood, then, as a rule, doctors recommend an IgG avidity test. At 12-14 weeks of pregnancy, in the case of high IgG avidity, often above 40%, virtually eliminates the possibility of infection with toxoplasmosis during the period of gestation and, accordingly, infection of the fetus.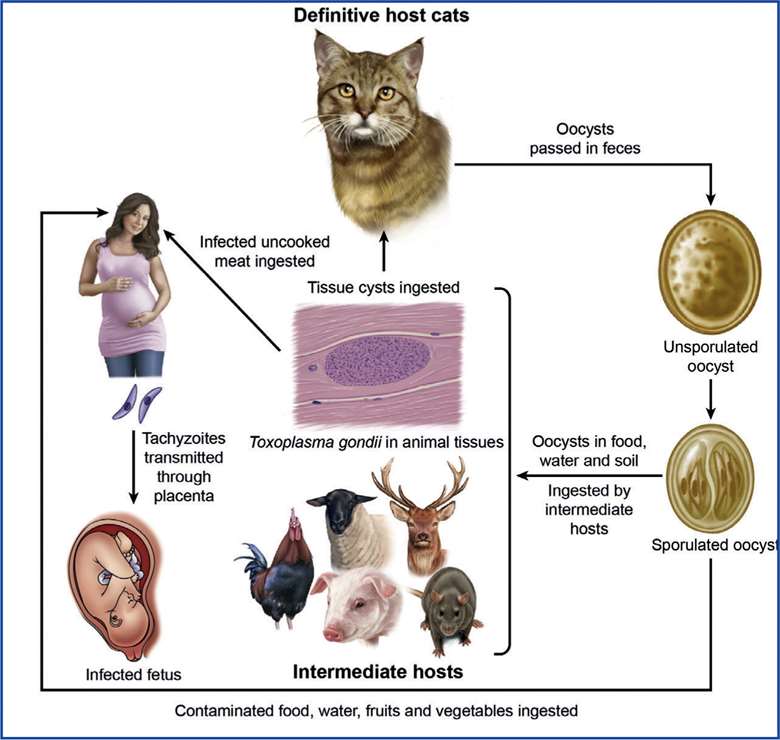 At the same time, low avidity is not an indicator that a person has recently been infected. In this case, it is recommended to repeat the test after two to three weeks, which determines whether the amount of antibody titer is growing. nine0005
At the same time, low avidity is not an indicator that a person has recently been infected. In this case, it is recommended to repeat the test after two to three weeks, which determines whether the amount of antibody titer is growing. nine0005
It should be noted that the absence of chronic forms of the disease is also indicated by the presence of intradermal tests with toxoplasmin and negative serological reactions (in the absence of HIV). The presence of IgM without the manifestation of clinical symptoms of toxoplasmosis suggests that the primary infection occurred before this within 13 months.
To establish the fact of infection of the fetus by a woman in position, amniotic fluid is often analyzed for Toxoplasma DNA. This diagnostic method is called polymerase chain reaction, abbreviated as PCR. In the event that this analysis is negative, then there is no reason to worry, since the fetus is perfectly healthy. nine0005
However, to clarify the diagnosis, as well as to determine the degree of infection of an unborn child, it is also recommended to conduct an additional examination.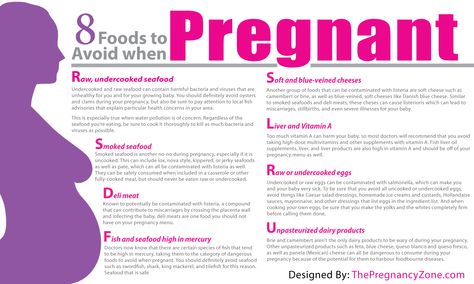
Instrumental diagnostic methods include many different methods that allow you to determine the manifestations of Toxoplasma gondii. Thus, if there are symptoms that the central nervous system (brain) has been affected, either computed tomography or magnetic nuclear resonance is performed. This examination makes it possible to determine precisely the foci of brain inflammation that were caused by toxoplasmosis. nine0005
Another test option is a biopsy, during which a piece of tissue affected by toxoplasmosis is taken and examined under a microscope. It should be noted that this method of examination is used very rarely.
If a woman, conducting research during the period of planning a child, or at the first visit to the doctor regarding a real pregnancy, finds out that there is no immunity to the pathogen Toxoplasma gondii (never had this disease before), then she is recommended to take certain measures to help avoid infection during pregnancy. nine0005
Basic recommendations for pregnant women to help protect themselves from toxoplasmosis
- If a cat lives in your house, then you should not let it out on the street, as well as feed the animal with raw meat.
 It is very important not to clean up after the cat, but to entrust this procedure to other members of your family. Do not lean the cat against your face and do not let it into your bed, as possible infection with toxoplasmosis by inhalation of the infectious agent from the surface of the coat. Wash your hands thoroughly after a cat. nine0010
It is very important not to clean up after the cat, but to entrust this procedure to other members of your family. Do not lean the cat against your face and do not let it into your bed, as possible infection with toxoplasmosis by inhalation of the infectious agent from the surface of the coat. Wash your hands thoroughly after a cat. nine0010 - All meat products must be well cooked. The causative agent Toxoplasma gondii in meat dies when it is cooled to - 20 degrees for two days or heated to + 66 degrees. Refuse to eat meat dishes with blood.
- Drink only pasteurized milk and clean water;
- When working with soil, whether in the garden or in the garden, be sure to wear gloves;
If you need an analysis to determine whether you had toxoplasmosis before your pregnancy and whether the disease is dangerous for you, it is recommended that you make an appointment with an experienced gynecologist. He will readily give you answers to all your questions and conduct the necessary tests.