How to know if child has leukemia
Signs and Symptoms of Childhood Leukemia
Many of the symptoms of childhood leukemia can have other causes as well, and most often these symptoms are not caused by leukemia. Still, if your child has any of them, it’s important to have your child seen by a doctor so the cause can be found and treated, if needed.
Leukemia begins in the bone marrow, which is where new blood cells are made. The symptoms of leukemia are often caused by problems in the bone marrow. As leukemia cells build up in the marrow, they can crowd out the normal blood cells. As a result, a child may not have enough normal red blood cells, white blood cells, and blood platelets. These shortages show up on blood tests, but they can also cause symptoms. The leukemia cells might also invade other areas of the body, which can also cause symptoms.
Symptoms from low red blood cell counts (anemia): Red blood cells carry oxygen to all of the cells in the body. A shortage of red blood cells can cause symptoms such as:
- Feeling tired (fatigue)
- Feeling weak
- Feeling cold
- Feeling dizzy or lightheaded
- Shortness of breath
- Paler skin
Symptoms from a lack of normal white blood cells: White blood cells help the body fight off germs. Children with leukemia often have high white blood cell counts, but most of these are leukemia cells that don’t protect against infection, and there aren’t enough normal white blood cells. This can lead to:
- Infections, which can occur because of a shortage of normal white blood cells. Children with leukemia can get infections that don’t seem to go away, or they may get one infection after another.
- Fever, which is often the main sign of infection. But some children might have a fever without having an infection.
Symptoms from low blood platelet counts: Platelets in the blood normally help stop bleeding. A shortage of platelets can lead to:
- Easy bruising and bleeding
- Frequent or severe nosebleeds
- Bleeding gums
Bone or joint pain: This pain is caused by the buildup of leukemia cells near the surface of the bone or inside the joint.
Swelling of the abdomen (belly): Leukemia cells can collect in the liver and spleen, making these organs bigger. This might be noticed as a fullness or swelling of the belly. The lower ribs usually cover these organs, but when they are enlarged the doctor can often feel them.
Loss of appetite and weight loss: If the spleen and/or liver get big enough, they can press against other organs like the stomach. This can make the child feel full after eating only a small amount of food, leading to a loss of appetite and weight loss over time.
Swollen lymph nodes: Some leukemias spread to lymph nodes, which are normally small (bean-sized) collections of immune cells in the body. Swollen nodes may be seen or felt as lumps under the skin in certain parts of the body (such as on the sides of the neck, in underarm areas, above the collarbone, or in the groin). Lymph nodes inside the chest or abdomen can also swell, but these can only be seen on imaging tests, such as CT or MRI scans.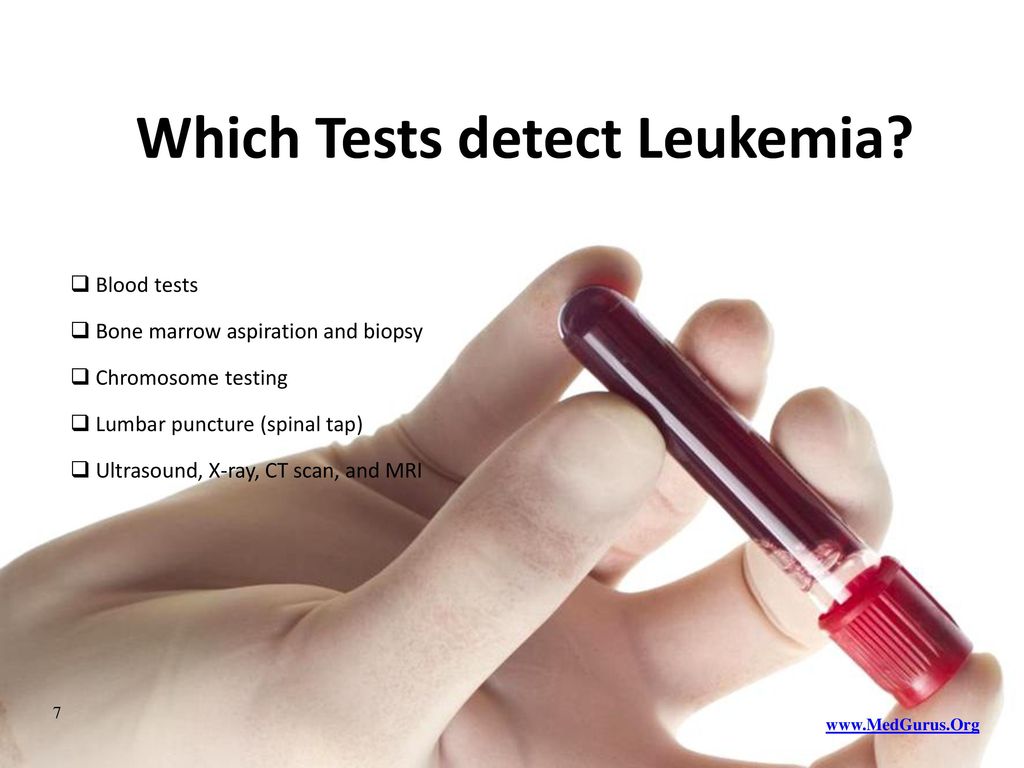
In infants and children, lymph nodes often get bigger when they are fighting an infection. An enlarged lymph node in a child is much more often a sign of infection than leukemia, but it should be checked by a doctor and followed closely.
Coughing or trouble breathing: Some types of leukemia can affect structures in the middle of the chest, such as lymph nodes or the thymus (a small organ in front of the trachea, the breathing tube that leads to the lungs). An enlarged thymus or lymph nodes in the chest can press on the trachea, causing coughing or trouble breathing.
In some cases where the white blood cell count is very high, the leukemia cells can build up in the small blood vessels of the lungs, which can also cause trouble breathing.
Swelling of the face and arms: An enlarged thymus might press on the superior vena cava (SVC), which is a large vein that carries blood from the head and arms back to the heart. This can cause the blood to “back up” in the veins.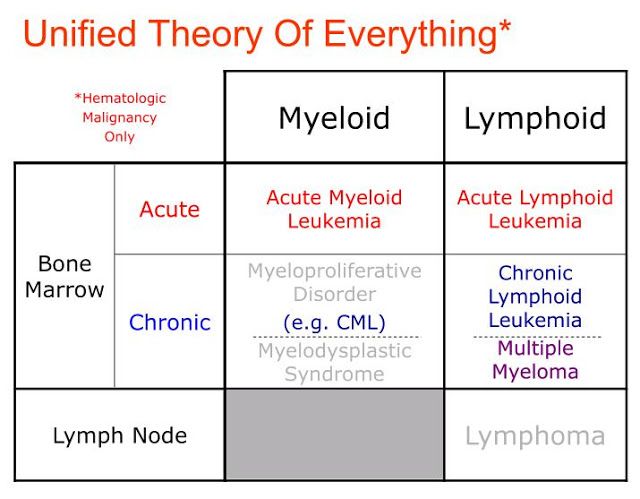 This is known as SVC syndrome. It can result in swelling in the face, neck, arms, and upper chest (sometimes with a bluish-red skin color). Symptoms can also include headaches, dizziness, and a change in consciousness if it affects the brain. The SVC syndrome can be life-threatening, so it needs to be treated right away.
This is known as SVC syndrome. It can result in swelling in the face, neck, arms, and upper chest (sometimes with a bluish-red skin color). Symptoms can also include headaches, dizziness, and a change in consciousness if it affects the brain. The SVC syndrome can be life-threatening, so it needs to be treated right away.
Headaches, seizures, vomiting: A small number of children have leukemia that has already spread to the brain and spinal cord when it is first found. This can lead to symptoms such as headaches, trouble concentrating, weakness, seizures, vomiting, problems with balance, and blurred vision.
Rashes or gum problems: In children with acute myeloid leukemia (AML), leukemia cells may spread to the gums, causing swelling, pain, and bleeding.
If AML spreads to the skin, it can cause small, dark spots that look like common rashes. A collection of AML cells under the skin or in other parts of the body is called a chloroma or granulocytic sarcoma.
Extreme fatigue and weakness: A rare but very serious consequence of AML is extreme tiredness, weakness, and slurring of speech. This can occur when very high numbers of leukemia cells thicken the blood and slow the circulation through small blood vessels of the brain.
Again, most of the symptoms above are more likely to be caused by something other than leukemia. Still, it’s important to have these symptoms checked by a doctor so the cause can be found and treated, if needed.
Leukemia in Children | Cedars-Sinai
ABOUT CAUSES DIAGNOSIS TREATMENT NEXT STEPS
What is leukemia in children?
Leukemia is cancer of the blood. It’s the most common form of cancer in childhood. The cancer cells grow in bone marrow and go into the blood. The bone marrow is the soft, spongy center of some bones. It makes blood cells. When a child has leukemia, the bone marrow makes abnormal blood cells that don’t mature. The abnormal cells are usually white blood cells (leukocytes). The bone marrow also makes fewer healthy cells. The abnormal cells reproduce very quickly. They don’t work the same as healthy cells.
The abnormal cells are usually white blood cells (leukocytes). The bone marrow also makes fewer healthy cells. The abnormal cells reproduce very quickly. They don’t work the same as healthy cells.
The types of blood cells include:
- Red blood cells (erythrocytes). Red blood cells carry oxygen. When a child has a low level of healthy red blood cells, this is called anemia. A child may feel tired, weak, and short of breath.
- Platelets (thrombocytes). Platelets help with blood clotting and stop bleeding. When a child has low levels of platelets, he or she bruises and bleeds more easily.
- White blood cells (leukocytes). These fight infection and other disease. When a child has low levels of white blood cells, he or she is more likely to have infections.
There are different types of leukemia in children. Most leukemias in children are acute, which means they tend to grow quickly. Some of the types of leukemia that occur in children include:
- Acute lymphocytic (lymphoblastic) leukemia (ALL).
 This is the most common type of leukemia in children.
This is the most common type of leukemia in children. - Acute myelogenous (myeloid, myelocytic, non-lymphocytic) leukemia (AML). This is the second most common type of leukemia in children.
- Hybrid or mixed lineage leukemia. This type is rare. It is a mix of ALL and AML.
- Chronic myelogenous leukemia (CML). This type is also rare in children.
- Chronic lymphocytic leukemia (CLL). This type is extremely rare in children.
- Juvenile myelomonocytic leukemia (JMML). This is a rare type of cancer that doesn’t grow quickly (acute) or slowly (chronic).
What causes leukemia in children?
The exact cause of leukemia in children is not known. There are certain conditions passed on from parents to children (inherited) that increase the risk for childhood leukemia. But, most childhood leukemia is not inherited. Researchers have found changes (mutations) in genes of the bone marrow cells.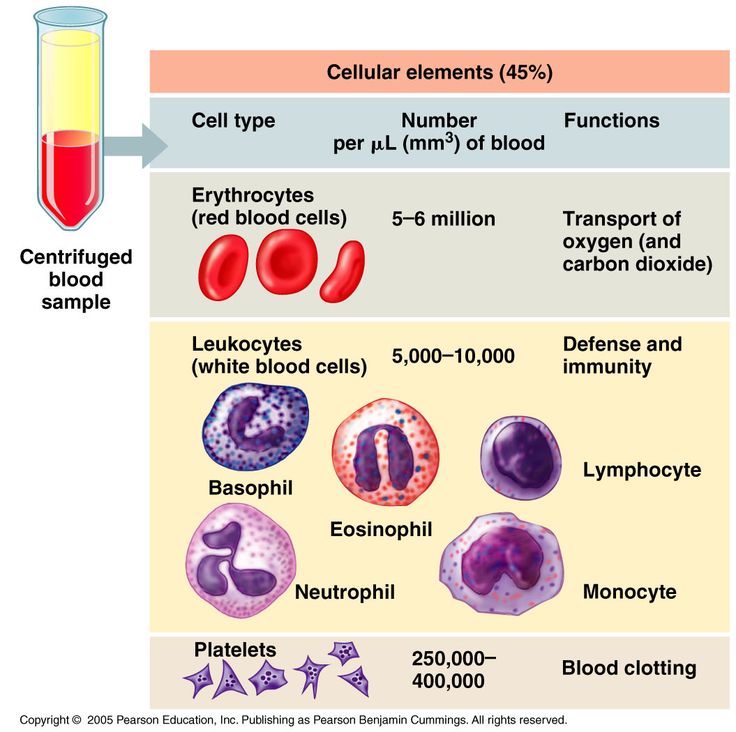 These changes may occur early in a child's life or even before birth. But they may occur by chance (sporadic).
These changes may occur early in a child's life or even before birth. But they may occur by chance (sporadic).Who is at risk for childhood leukemia?
The risk factors for childhood leukemia include:
- Exposure to high levels of radiation
- Having certain inherited syndromes, such as Down syndrome and Li-Fraumeni syndrome
- Having an inherited condition that affects the body's immune system
- Having a brother or sister with leukemia
What are the symptoms of leukemia in children?
The symptoms depend on many factors. The cancer may be in the bone marrow, blood, and other tissue and organs. These may include the lymph nodes, liver, spleen, thymus, brain, spinal cord, gums, and skin.
Symptoms can occur a bit differently in each child. They can include:
- Pale skin
- Feeling tired, weak, or cold
- Dizziness
- Headaches
- Shortness of breath, trouble breathing
- Frequent or long-term infections
- Fever
- Easy bruising or bleeding, such as nosebleeds or bleeding gums
- Bone or joint pain
- Belly (abdominal) swelling
- Poor appetite
- Weight loss
- Swollen lymph glands (nodes)
The symptoms of leukemia can be like other health conditions.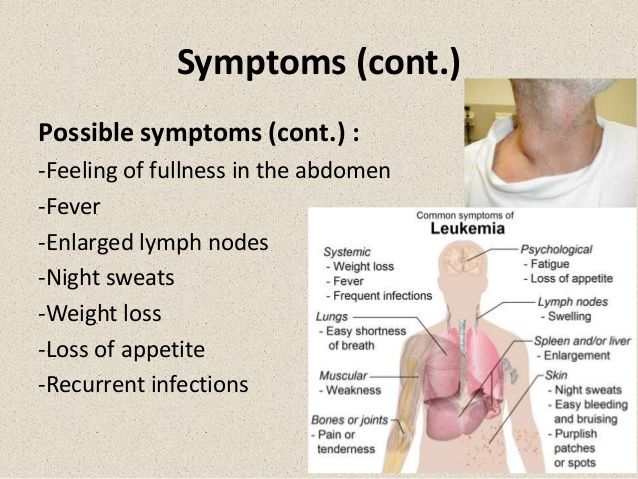 Make sure your child sees a healthcare provider for a diagnosis.
Make sure your child sees a healthcare provider for a diagnosis.
How is leukemia diagnosed in children?
Your child's healthcare provider will ask many questions about your child's symptoms. He or she will examine your child. Your child's healthcare provider may recommend blood tests and other tests. A complete blood count (CBC) provides the number of red blood cells, different types of white blood cells, and platelets. If the results are abnormal, your child's healthcare provider may recommend that your child see a pediatric cancer specialist (pediatric oncologist). The oncologist may want your child to have additional tests including:
- Bone marrow aspiration or biopsy. Bone marrow is found in the center of some bones. It’s where blood cells are made. A small amount of bone marrow fluid may be taken. This is called aspiration. Or solid bone marrow tissue may be taken. This is called a core biopsy. Bone marrow is usually taken from the hip bone. This test is done to see if cancer (leukemia) cells are in the bone marrow.

- Lab tests of blood and bone marrow samples. Tests like flow cytometry and immunohistochemistry. These tests determine the exact type of leukemia. DNA and chromosome tests may also be done.
- X-ray. An X-ray uses a small amount of radiation to take pictures of bones and other body tissues.
- Ultrasound (sonography). This test uses sound waves and a computer to create images.
- Lymph node biopsy. A sample of tissue is taken from the lymph nodes. It’s checked with a microscope for cancer cells.
- Lumbar puncture. A special needle is placed into the lower back, into the spinal canal. This is the area around the spinal cord. This is done to check the brain and spinal cord for cancer cells. A small amount of cerebral spinal fluid (CSF) is removed and sent for testing. CSF is the fluid around the brain and spinal cord.
When leukemia is diagnosed, the doctor will find out the exact type of leukemia it is.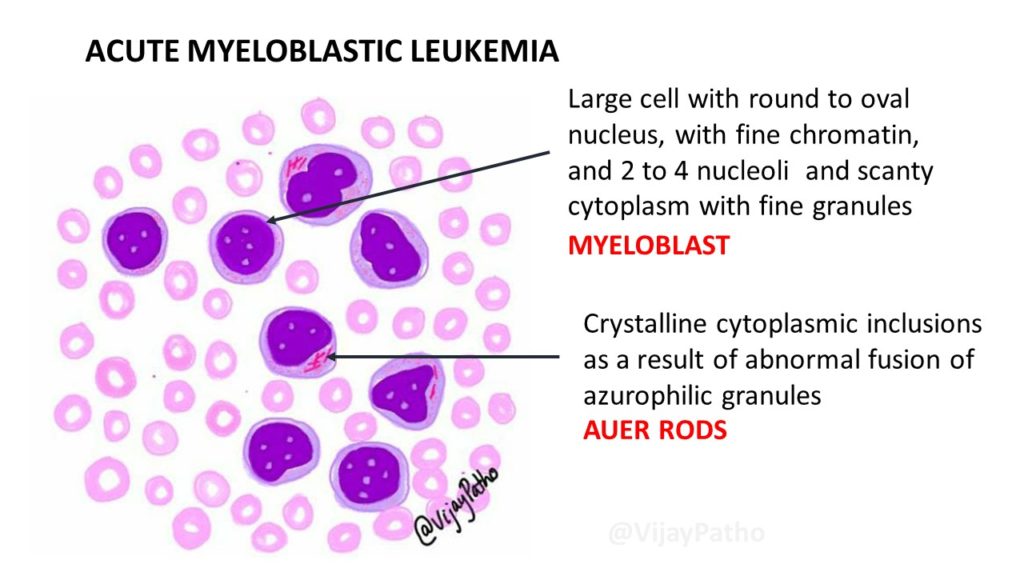 Leukemia is not assigned a stage number like most other cancers. Instead, it's classified into groups, sub-types, or both.
Leukemia is not assigned a stage number like most other cancers. Instead, it's classified into groups, sub-types, or both.
ALL (acute lymphocytic leukemia) is the most common leukemia in children. It's separated into 2 groups based on the type of lymphocyte the leukemia started in. That would be B cells or T cells. About 8 out of 10 cases of ALL in children are B-cell ALLs. These can be further classified into sub-types. The other 2 out of 10 cases are T-cell ALLs.
AML (acute myelogenous leukemia) is the other kind of leukemia that's common in children. Doctors use 2 different systems to classify AML. The French-American-British (FAB) system divides AML into 8 sub-types based on how the cells look under the microscope. The World Health Organization (WHO) classification system is newer. It groups AML into many groups based on things like the details of the gene changes in the cancer cells as well as the FAB sub-types.
Classifying leukemia is very complex. But it's an important part of making treatment plans and predicting treatment outcomes. Be sure to ask your child's healthcare provider to explain the stage of your child's leukemia to you in a way you can understand.
Be sure to ask your child's healthcare provider to explain the stage of your child's leukemia to you in a way you can understand.
How is leukemia treated in children?
Your child may first need to be treated for low blood counts, bleeding, or infections. Your child may receive:
- Blood transfusion with red blood cells for low blood counts
- Blood transfusion with platelets to help stop bleeding
- Antibiotic medicine to treat any infections
Treatment will depend on the type of leukemia and other factors. Leukemia can be treated with any of the below:
- Chemotherapy. These are medicines that kill cancer cells or stop them from growing. They may be given into the vein (IV) or spinal canal, injected into a muscle, or taken by mouth. Chemotherapy is the main treatment for most leukemias in children. Several medicines are often given at different times. It’s usually done in cycles, with rest periods in between. This gives your child time to recover from the side effects.

- Radiation therapy. These are high-energy X-rays or other types of radiation. They are used to kill cancer cells or stop them from growing. Radiation may be used in certain cases.
- High-dose chemotherapy with a stem cell transplant. Young blood cells (stem cells) are taken from the child or from someone else. This is followed by a large amount of chemotherapy medicine. This causes damage to the bone marrow. After the chemotherapy, the stem cells are replaced.
- Targeted therapy. These medicines may work when chemotherapy doesn’t. For example, it may be used to treat children with chronic myeloid leukemia (CML). Targeted therapy often has less severe side effects.
- Immunotherapy. This is treatment that helps the body's own immune system attack the cancer cells.
- Supportive care. Treatment can cause side effects. Medicines and other treatments can be used for pain, fever, infection, and nausea and vomiting.
- Clinical trials. Ask your child's healthcare provider if there are any treatments being tested that may work well for your child.
With any cancer, how well a child is expected to recover (prognosis) varies. Keep in mind:
- Getting medical treatment right away is important for the best prognosis.
- Ongoing follow-up care during and after treatment is needed.
- New treatments are being tested to improve outcome and to lessen side effects.
What are possible complications of leukemia in a child?
A child may have complications from the tumor or from treatment. They may also be short-term or long-term.
Treatment may have many side effects. Some side effects may be minor. Some may be serious and even life-threatening. Your child may take medicines to help prevent or lessen side effects. You’ll be given instructions about what you can do at home.
Possible complications of leukemia can include:
- Serious infections
- Severe bleeding (hemorrhage)
- Thickened blood from large numbers of leukemia cells
Possible long-term complications from the leukemia or the treatment can include:
- Return of the leukemia
- Growth of other cancers
- Heart and lung problems
- Learning problems
- Slowed growth and development
- Problems with the ability to have children in the future
- Bone problems such as thinning of bones (osteoporosis)
What can I do to prevent leukemia in my child?
Most childhood cancers, including leukemia, can’t be prevented.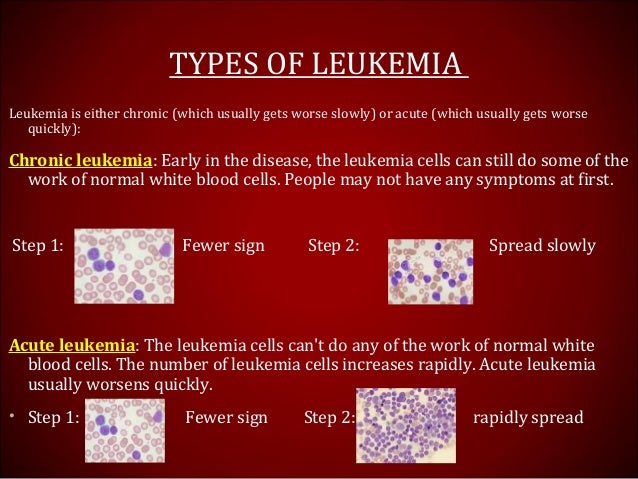 The risk from X-rays and CT scans is very small. But healthcare providers advise against them in pregnant women and children unless absolutely needed.
The risk from X-rays and CT scans is very small. But healthcare providers advise against them in pregnant women and children unless absolutely needed.How can I help my child live with leukemia?
A child with leukemia needs ongoing care. Your child will be seen by oncologists and other healthcare providers to treat any late effects of treatment and to watch for signs or symptoms of the cancer returning. Your child will be checked with imaging tests and other tests. And your child may see other healthcare providers for problems from the cancer or from treatment.
You can help your child manage his or her treatment in many ways. For example:
- Your child may have trouble eating. A dietitian may be able to help.
- Your child may be very tired. He or she will need to balance rest and activity. Encourage your child to get some exercise. This is good for overall health. And it may help to lessen tiredness.
- Get emotional support for your child. Find a counselor or child support group can help.

- Make sure your child attends all follow-up appointments.
When should I call my child’s healthcare provider?
Call the healthcare provider if your child has:
- Fever
- Symptoms that get worse
- New symptoms
- Side effects from treatment
Key points about leukemia in children
- Leukemia is cancer of the blood. The cancer cells develop in the bone marrow and go into the blood. Other tissue and organs that may be affected include the lymph nodes, liver, spleen, thymus, brain, spinal cord, gums, and skin.
- When a child has leukemia, the bone marrow makes abnormal blood cells that do not mature. The abnormal cells are usually white blood cells (leukocytes). And with leukemia, the bone marrow makes fewer healthy cells.
- Common symptoms of leukemia in children include feeling tired and weak, easy bruising or bleeding, and frequent or long-term infections.
- Leukemia is diagnosed with blood and bone marrow tests.
 Imaging may be done to look for signs of leukemia in different parts of the body.
Imaging may be done to look for signs of leukemia in different parts of the body. - Chemotherapy is the main treatment for most leukemias in children.
- A child with leukemia may have complications from the leukemia and from the treatment.
- Ongoing follow-up care is needed during and after treatment.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
- Know the reason for the visit and what you want to happen.
- Before your visit, write down questions you want answered.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
- Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
- Ask if your child’s condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if your child does not take the medicine or have the test or procedure.
- If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Leukemia in children and adolescents
What is leukemia?
Watch this video
Leukemia is a cancer of the blood and bone marrow. It is the most common cancer in children and adolescents. In the United States, about 3,500–4,000 cases of childhood leukemia are diagnosed each year.
Leukemia occurs when the normal functioning of the bone marrow is disrupted. Bone marrow is the soft inner part of the bone. It works like a factory for the production of blood cells: it produces all the blood cells. Their formation begins with the formation of hematopoietic cells (hematopoietic cells). If the bone marrow is functioning properly, these blood-forming cells become cells that eventually turn into red blood cells, white blood cells, and platelets. nine0011
If the bone marrow is functioning properly, these blood-forming cells become cells that eventually turn into red blood cells, white blood cells, and platelets. nine0011
-
Acute lymphoblastic leukemia (ALL)
-
Acute myeloid leukemia (AML)
-
Chronic myeloid leukemia (CML)
-
Juvenile myelomonocytic leukemia (JMML)
-
Acute lymphoblastic leukemia (ALL) in infants
-
Relapse of acute lymphoblastic leukemia (ALL)
Patients with leukemia do not have proper maturation of hematopoietic cells. The blood produces too many immature blood cells or leukemic cells.
When this happens, the function of the blood is disturbed.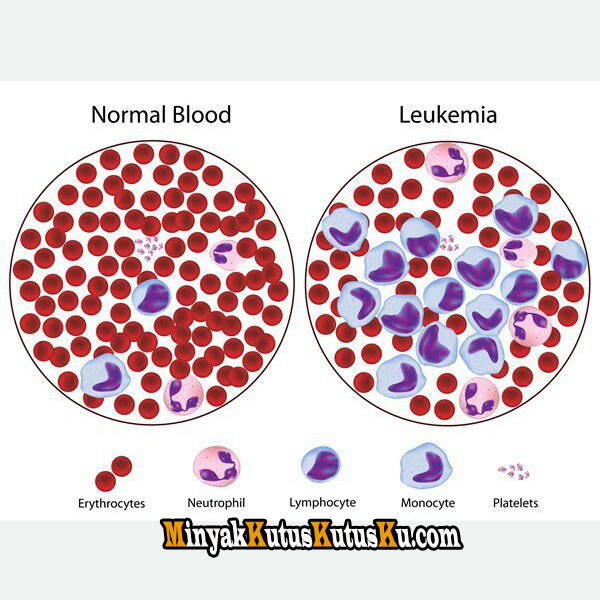 It becomes insufficient in it:
It becomes insufficient in it:
- Erythrocytes - their task is to deliver oxygen to the organs of the body. A person has a strong feeling of fatigue due to anemia. nine0011
- Leukocytes - their task is to fight infections and diseases. The person gets sick.
- Platelets - they are responsible for blood clotting. A person easily bleeds and bruises.
Leukemias are either acute or chronic. In acute cases, the symptoms develop rapidly: without treatment, the disease will progress rapidly. In a chronic course, the disease and symptoms develop slowly. nine0011
Acute leukemia most often occurs in children.
The process of hematopoiesis leading to the formation of blasts.
Signs and symptoms of leukemia
Signs and symptoms include:
- Fever
- Frequent infections
- Weakness
- Increased fatigue
- Easily occurring bleeding and bruising
- Pain in bones and joints
Diagnosis of leukemia
- Medical examination and medical history
- Blood tests
- Puncture and biopsy of bone marrow
- Chest x-ray
Treatment of leukemia
Treatment depends on the type of leukemia and risk group. The most common treatment is chemotherapy.
The most common treatment is chemotherapy.
Other possible treatments:
- Targeted therapy
- Immunotherapy
- Hematopoietic cell transplant (also called bone marrow or stem cell transplant)
Leukemia treatment prognosis (outcome)
When discussing cancer survival statistics, physicians often use a number called 5-year survival, referring to the percentage of patients who live at least 5 years after they are diagnosed with cancer. In acute leukemia, children with no disease after five years are likely to be completely cured. This is explained by the fact that after so many years the return of this cancer is very rare. Survival rates are a conditional value. For information about survival in the specific case your family is facing, it is best to contact your child's primary care physician. nine0005
Acute leukemia
The overall 5-year survival rate for acute lymphoblastic leukemia (ALL) in children is approximately 90%.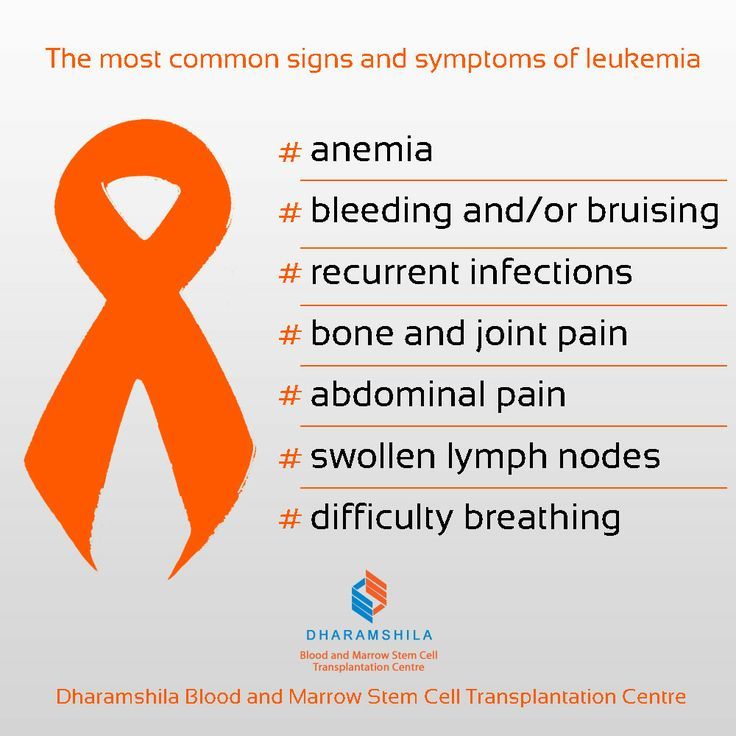
The overall 5-year survival rate for children with acute myeloid leukemia (AML) is 65–75%. However, survival rates vary by AML subtype and other factors. For example, the cure rate for acute promyelocytic leukemia (APML), one subtype of AML, is currently above 90%, but rates for some other subtypes of AML are lower. nine0005
Chronic leukemias
For chronic leukemias, a 5-year survival rate is less useful because children can live with leukemia for a long time without actually being cured. In the past, 5-year survival rates for chronic myeloid leukemia (CML) were 60-80%, but they are now much higher.
-
Date modified: June 2018
How to recognize leukemia by blood test? — Foundation for the fight against leukemia
Hematologist, MD Sergey Semochkin about acute lymphoblastic leukemia
Warning: count(): Parameter must be an array or an object that implements Countable in /home/l/leikozunet/leikozu. net/public_html/wp-content/themes/leikozu/page-single.php on line 48
net/public_html/wp-content/themes/leikozu/page-single.php on line 48
Hematologist, Professor of the Department of Oncology, Hematology and Radiation Therapy, Russian National Research Medical University. N. I. Pirogov of the Ministry of Health of Russia, Doctor of Medical Sciences Sergey Semochkin told: is it possible to recognize acute lymphoblastic leukemia (ALL) at an early stage and make a diagnosis by a blood test; explained how ALL is treated and who is eligible for bone marrow transplantation (BMT). nine0005
What are the early symptoms of acute lymphoblastic leukemia? Can they be seen and recognized by ALL?
In this case, everything is quite simple, because the word "acute" means that the disease is sudden and often the symptoms are very expressive. The most common symptom is fever; increase in body temperature. Fever can be both subfebrile and pronounced, up to 39 degrees. There will be changes associated with damage to the bone marrow. A decrease in hemoglobin will lead to weakness and fatigue.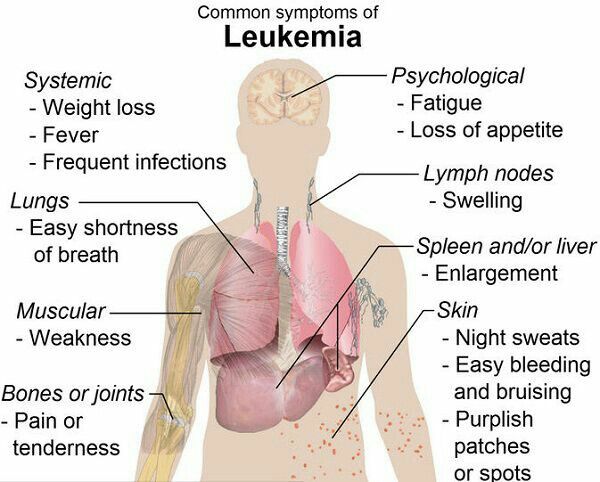 Lymph nodes may increase, discomfort in the abdominal cavity may appear due to the fact that the size of the liver and spleen increase. There may be manifestations of bleeding - even during brushing your teeth. In some patients, ALL may begin with neurological manifestations such as headaches, dizziness, and other problems. Symptoms are extensive, but in this case it is quite acute, suddenly appeared. nine0005
Lymph nodes may increase, discomfort in the abdominal cavity may appear due to the fact that the size of the liver and spleen increase. There may be manifestations of bleeding - even during brushing your teeth. In some patients, ALL may begin with neurological manifestations such as headaches, dizziness, and other problems. Symptoms are extensive, but in this case it is quite acute, suddenly appeared. nine0005
Watch video on our website .
Can a diagnosis be made by a blood test? What will he show?
As a rule, there are pronounced indicators in a blood test: hematopoietic sprouts are changed, the number of leukocytes goes beyond the normal range - it can fall below normal values, or it can become prohibitively huge. I have met patients in whom the number of leukocytes at a rate of 4 to 9 thousand increased to 200 thousand per μl. Platelets are also very much reduced in some cases, but the main thing is the change in the number of leukocytes. A very important marker is the release of tumor cells into the blood, when immature early cells appear in the blood, which are called blasts. If blast cells were detected in the blood test, then this is most likely either acute leukemia or myelodysplastic syndrome. nine0005
A very important marker is the release of tumor cells into the blood, when immature early cells appear in the blood, which are called blasts. If blast cells were detected in the blood test, then this is most likely either acute leukemia or myelodysplastic syndrome. nine0005
How does a patient get to a hematologist?
A blood test with characteristic changes is a reason to immediately call an ambulance and hospitalize the patient in a specialized hospital. In the treatment of children and adolescents, the oncohematologist, as a rule, has one or two days without diagnosis, treatment should be started as early as possible. The diagnosis includes a repeated blood test, then verification of the diagnosis, for which a bone marrow biopsy is performed. In young children, it is performed under general anesthesia, in adults - under local anesthesia. With the help of a small needle, I puncture the sternum or ilium. In children, a puncture of the sternum is not done. The resulting bone marrow sample, which looks like an ordinary test tube with blood, will be sent to the laboratory, where a whole range of studies will be carried out to confirm the diagnosis.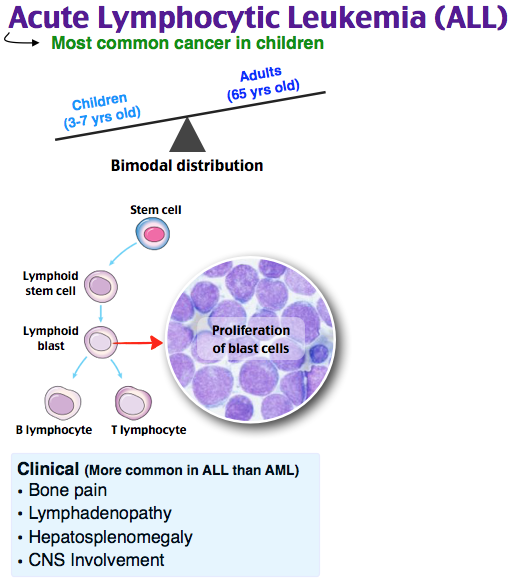 The main criterion is an increase in the number of blast cells. It is impossible to determine the variant of leukemia only by appearance and by the number of blast cells. Back at 19In 13, it was established that there is a lymphoid, and there is a myeloid variant of leukemia. For verification, special laboratory methods are used: immunological and chemical. There is a special device - a flow cytometer, with the help of which markers characterizing this type of cells are determined. To determine the subtype of acute leukemia, a range of genetic studies are being used to reach more targeted therapies in these patients.
The main criterion is an increase in the number of blast cells. It is impossible to determine the variant of leukemia only by appearance and by the number of blast cells. Back at 19In 13, it was established that there is a lymphoid, and there is a myeloid variant of leukemia. For verification, special laboratory methods are used: immunological and chemical. There is a special device - a flow cytometer, with the help of which markers characterizing this type of cells are determined. To determine the subtype of acute leukemia, a range of genetic studies are being used to reach more targeted therapies in these patients.
What are the causes of ALL? There is an opinion that this type of leukemia is very strongly interconnected with environmental problems, is inherited and often occurs in those who have already had some kind of oncological disease. Is it true or not? nine0149
The true cause of leukemia in adults can be identified only in 5% of cases, in 95% it is completely unclear what led to what. The kids are a little more interesting.
The kids are a little more interesting.
How does leukemia occur? A certain primary mutation occurs in the genetic material of the cell, which by itself does not always lead to leukemia. Subsequently, others join this mutation, and when the disease nevertheless occurs, many molecular events have already accumulated in the cell, the combination of which led to the onset of the disease. The peak of acute lymphoblastic leukemia occurs in children from two to four years, then the incidence falls. The next peak falls on 18-29years, then decline again. After 60 years - again a small increase.
Some innate component of this problem can be traced in some young children. There are cases of ALL in the fetus or newborn, when the child is born already with the disease, or becomes ill during the first year of life. Cord blood studies have shown that newborns have leukemic breakdowns, congenital mutations that can lead to leukemia. And this mutation is caused by a hereditary factor that worked during fetal development. According to various sources, the total number of such babies ranges from 1 to 5%. Further, much depends on the infectious situation that has developed around the child. Numerous childhood infections contribute to the formation of a normal immune system that neutralizes the hereditary factor. nine0005
According to various sources, the total number of such babies ranges from 1 to 5%. Further, much depends on the infectious situation that has developed around the child. Numerous childhood infections contribute to the formation of a normal immune system that neutralizes the hereditary factor. nine0005
If we talk about environmental problems, no clear connection has been found with them.
Does UV, microwave, sunlight, radiation affect?
In Hiroshima and Nagasaki, the increased morbidity persisted for about 12 years. After Chernobyl, the thyroid gland was damaged in many, but the incidence of leukemia did not increase. It all depends on the type of isotopes released into the environment. This did not happen in Fukushima either, because the concentration of radioactive substances was greatly diluted with sea water. nine0005
The harmful effects of ultraviolet radiation are scientifically proven only in relation to melanoma. There is no clear connection with ALL. We do not allow our former patients to visit the solarium and do not recommend sunbathing, because although the connection has not been proven, this factor cannot be completely ruled out either.
When it comes to microwave radiation, home microwave ovens are completely safe.
How is ALL treated? What awaits the patient?
The concept of ALL treatment, which is still the basis of ALL treatment protocols, was developed by the American pediatrician Donald Pinkel back in 1962 year. It includes four stages: remission induction, consolidation, effects on the central nervous system and a long stage of maintenance therapy for two to three years. All over the world, treatment is carried out according to clinical protocols developed as a result of collaborative research. According to some studies, strict adherence to protocols improves patient survival by 15-20% compared with individualized treatment. All actions are written in the protocol: from the first day to the last. It contains instructions on how and at what point to evaluate emerging complications and what to do with them. In Russia, there are two centers actively conducting such protocols. Center them. Dmitry Rogachev, where Alexander Isaakovich Karachunsky for many years, from the beginning of 1990s, conducts a series of protocols "Moscow - Berlin". Protocol design is reviewed every five years to improve the treatment of certain categories of patients. for many years since the beginning of the 90s, a series of Moscow-Berlin protocols. The design of protocols aimed at improving the treatment of certain categories of patients changes every five years. In adult practice, this is the National Research Center for Hematology, where they conduct collaborative research on acute lymphoblastic leukemia in adults.
Dmitry Rogachev, where Alexander Isaakovich Karachunsky for many years, from the beginning of 1990s, conducts a series of protocols "Moscow - Berlin". Protocol design is reviewed every five years to improve the treatment of certain categories of patients. for many years since the beginning of the 90s, a series of Moscow-Berlin protocols. The design of protocols aimed at improving the treatment of certain categories of patients changes every five years. In adult practice, this is the National Research Center for Hematology, where they conduct collaborative research on acute lymphoblastic leukemia in adults.
When is a bone marrow transplant (BMT) indicated? nine0149
Unlike acute myeloid leukemia, there are fewer indications for allogeneic (from a donor) BMT. It is prescribed to patients who have not achieved remission within the time specified by the protocol or have an unfavorable cytogenetic variant of the disease. In pediatric practice, more than 90% of children recover, and approximately 15-20% are candidates for allogeneic BMT. In adults, the percentage of patients in need of transplantation is somewhat higher, due to the fact that high-risk genetic operations are becoming much more and the response to standard treatment is worse. When we discussed chronic myeloid leukemia, the Philadelphia chromosome appeared there - a translocation (9;22). In ALL, this is an absolutely negative prognostic factor. In children, this mutation occurs in less than 5% of cases; in people older than 50-60 years, about half of B-linear ALL will be with the Philadelphia chromosome. Unlike chronic myeloid leukemia, the use of tyrosine kinase inhibitors in acute lymphoblastic leukemia has not been as successful. That is why in the adult practice of BMT it is necessary to perform approximately 30% of patients. The age threshold for allogeneic BMT is around 55, which is reasonable.
In adults, the percentage of patients in need of transplantation is somewhat higher, due to the fact that high-risk genetic operations are becoming much more and the response to standard treatment is worse. When we discussed chronic myeloid leukemia, the Philadelphia chromosome appeared there - a translocation (9;22). In ALL, this is an absolutely negative prognostic factor. In children, this mutation occurs in less than 5% of cases; in people older than 50-60 years, about half of B-linear ALL will be with the Philadelphia chromosome. Unlike chronic myeloid leukemia, the use of tyrosine kinase inhibitors in acute lymphoblastic leukemia has not been as successful. That is why in the adult practice of BMT it is necessary to perform approximately 30% of patients. The age threshold for allogeneic BMT is around 55, which is reasonable.
How often does ALL relapse? nine0149
If we are talking about adults, then relapses occur in almost 40% of cases. There are early relapses that happen right on therapy.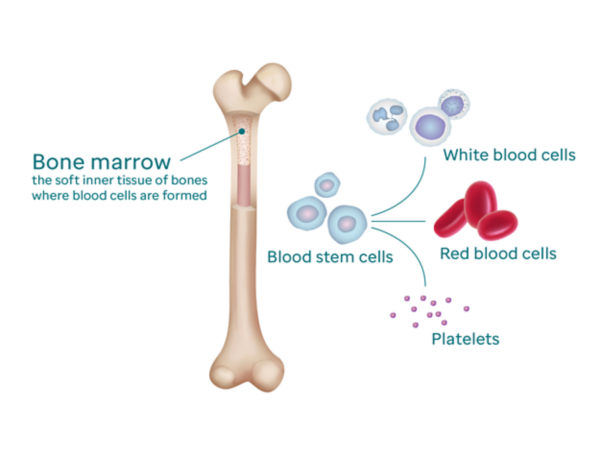 In this case, it is necessary to change the treatment, make it more intense and difficult. In such cases, as a rule, TCM is indicated. Late recurrence can occur after 20 years. Unfortunately, we cannot remove the cause that causes this disease - it can return.
In this case, it is necessary to change the treatment, make it more intense and difficult. In such cases, as a rule, TCM is indicated. Late recurrence can occur after 20 years. Unfortunately, we cannot remove the cause that causes this disease - it can return.
Can pregnancy be planned after ALL?
Long-term chemotherapy interferes with fertility, so it is better to cryopreserve the sperm/ovum, and even better the embryo - this is a more reliable method. In men, as a rule, spermatogenesis is seriously disturbed, but in women the situation is somewhat better. The chances of getting pregnant and having a healthy baby are high. If at least five years have passed in remission, there are no restrictions. nine0005
Can pregnancy be a trigger for relapse?
Rather not. This is not as common as with some other diseases, where pregnancy can really become a provoking factor.
Is ALL hereditary?
Lymphoblastic leukemia is a rare disease, so it is very unlikely that a child born to parents after ALL will have it.
How will ALL be treated in the future?
It seems that the basis of the treatment of oncological diseases in the future will be the activation of one's own immunity. We need to tune the immune system in such a way that it recognizes and eliminates cancer cells. We are now at an early stage in the development of CAR-T therapy, but after some time the technology will improve so much that it will most likely become one of the main methods of therapy for a number of oncohematological diseases. The essence of the method is that the patient's own T-lymphocytes are collected and sent to a special laboratory. This laboratory may be in another city, country - it does not matter. In the laboratory, these T-lymphocytes are reprogrammed: they receive information about the tumor cells present in the patient's body. After reprogramming, T-lymphocytes are injected back into the patient, they find cancer cells and remission occurs. The main challenges are to create a quality recognition process and develop standard treatment protocols.