How to increase milk supply when pregnant
5 Ways to Prepare for Breastfeeding While Pregnant – Nourisher
Breastfeeding feels like the first test of motherhood. It’s quite unfair actually. You’ve JUST made it to the finish line of your pregnancy, gone through labor and dealt with the emotional shock of meeting a tiny human that is half of your DNA. Instead of taking a good nap (or having that long awaited glass of wine) there is a startling jolt of reality that this baby is 100% dependent on you. He or she will be placed on your breast and before you know it, it’s go time!
Here are five ways to prepare for breastfeeding before your baby arrives.
Learn (and Practice!) the Main Breastfeeding Positions
We here stories like this from Nourisher moms all of the time!
“Minutes after my son was born a nurse hovered over me watching me try and latch him on for the first time. I knew what to look for in a latch, but unsurprisingly, he didn’t get it right away. “Maybe try him in the football hold,” she recommended.
Panic set in. The football hold? I had no idea what she was talking about! How could I already be bad at this, it had only been ten minutes? I mumbled something incoherent before she gracefully lifted him up and placed his body under my arm with his head in my palm. Baby latched and I breathed a sigh of relief.”
Case in point, study the various breastfeeding positions so that you know the different ways to hold your baby right from the start.
Take an In Person or Online Breastfeeding Class
The first time you hear the words “latch” “engorgement” “let down” and “colostrum” should be in an environment where you can absorb information — i.e. not in a hospital room with a screaming hungry newborn.
Learn the basics of breastfeeding before your baby arrives. This way the process will get off to a less-chaotic start. Most hospitals hold classes on breastfeeding and lactation consultants offer in-person training. But if getting dressed and out the door at 8 or 9 months pregnant doesn’t sound like your thing, take an online class! Nourisher friend Lindsey Shipley of the Lactation Link offers amazing online tutorials and webinars.
Understand Where Your Milk Supply Comes From
You don’t know it yet, but your milk supply will become a focal point of your day in a few weeks or months. Unfortunately you have no way of knowing if your milk supply will be abundant, just right, or if you’ll have a low supply. Regardless of where your body will fall on the milk-supply spectrum, it’s important to know where your supply comes from and how you can influence production.
Supply and Demand
The greatest way to maintain a healthy milk supply is to feed or pump frequently. Your body will produce on a supply and demand basis, so the more demand, the more supply.
Meeting Calorie Goals
Breastfeeding mothers don’t have to eat one specific type of diet, but they do need to be hitting the correct calorie amount in order to make milk. It’s all too easy to stop taking care of your body when your baby arrives.
Milkful Nursing Bars are a wholesome, convenient, energy-packed snack made specifically for breastfeeding moms. Eating one or two bars a day ensures you’re eating healthy ingredients and not snacking on cheap sugar products or failing to meet your calorie count. We recommend buying bars ahead of time (they have a shelf life of 5 months) and keeping several in your hospital bag for when baby arrives.
Eating one or two bars a day ensures you’re eating healthy ingredients and not snacking on cheap sugar products or failing to meet your calorie count. We recommend buying bars ahead of time (they have a shelf life of 5 months) and keeping several in your hospital bag for when baby arrives.
Additionally, learn what foods you can and can’t eat when breastfeeding. Hint: It’s more relaxed than pregnancy!
Hydrating
Drinking water to thirst is extremely important for breastfeeding women. Always keep a water bottle on hand so that your body is never straining for liquid to make milk.
Order Your Breast Pump, Necessary Accessories and Milk Storage Solution
Pumping is an entirely different facet of breastfeeding. Some women are exclusive pumpers, meaning their baby primarily drinks expressed breastmilk from a bottle rather than from their bodies. Some women pump breastmilk once or twice a day so that they have a bottle on-hand for occasional feedings from other people. And then some women never pump breastmilk because they are never separated from their child.
And then some women never pump breastmilk because they are never separated from their child.
How do you know which category you will fall into? For starters, consider what will happen at the end of your maternity leave. If there is a set date that you will be returning to work and you still want to continue breastfeeding, you’ll need to pump.
If your plans don’t involve daily separation from your child but you think you’ll want an occasional break from feeding, you’ll need to pump.
Now, you don’t need to feel pressure to pump right away. In fact, many lactation consultants recommend holding off on pumping until a breastfeeding routine is established. But we recommend having your pumping gear ready so that you can easily transition to this next stage of breastfeeding.
Here’s what we recommend purchasing during your pregnancy in preparation for pumping:
1. An electric or manual pump
A dual pump means you can pump from both breasts at the same time (a massive timesaver!)
2. A hands-free pumping bra
A hands-free pumping bra
This bra is not necessary if you’re going the manual route, but a hands-free bra means you aren’t sitting there holding your breast shields up to your body for 20 minutes at a time.
3. A breast milk storage solution
If you know pumping will eventually be a big part of your routine, go straight for the breast milk bags. These store up to 6 ounces of breast milk and are cost effective. You can also purchase 2.7 ounce vials that are easier to fill and defrost for feedings in the early weeks.
4. Bottles
Some babies prefer one style of bottle to another so you can either purchase a few different styles or borrow from a mommy-friend. Once your baby sets a preference, it’s a good idea to stick to one brand so you’re not trying to mix and match parts in the middle of the night.
5. Bottle brush and sanitizing steam bags
Have a new clean brush ready that is only dedicated to washing bottles, and buy a steam sanitizer bag for easy sterilization.
Mentally Prepare Yourself For a Newborn’s Breastfeeding Schedule
Alright mamas-to-be it’s time to buckle in. Breastfeeding is a job, and most likely the routine is going to kick your butt the first couple of weeks.
Newborn babies need to eat at every two hour mark until they get back up to their birth weight. Every two hours, 24/7. That means a typical day could have feedings at 6 a.m., 8 a.m., 10 a.m., 12 p.m., 2 p.m., 4 p.m., 6 p.m., 8 p.m., 10 p.m. 12 a.m., 2 a.m., 4 a.m.
The good news is that it is over quickly. The bad news is when you’re in that schedule, it feels like there is no way can you keep going. Trust us, you can!
Psych Yourself Up for the Routine
Go into that crazy feeding schedule knowing you will be challenged but you will make it through. Try to think of each feeding as a positive because it means your child is gaining weight quickly. Once you are given the go-ahead by your pediatrician you can relax into 3-4 hour stretches between feedings.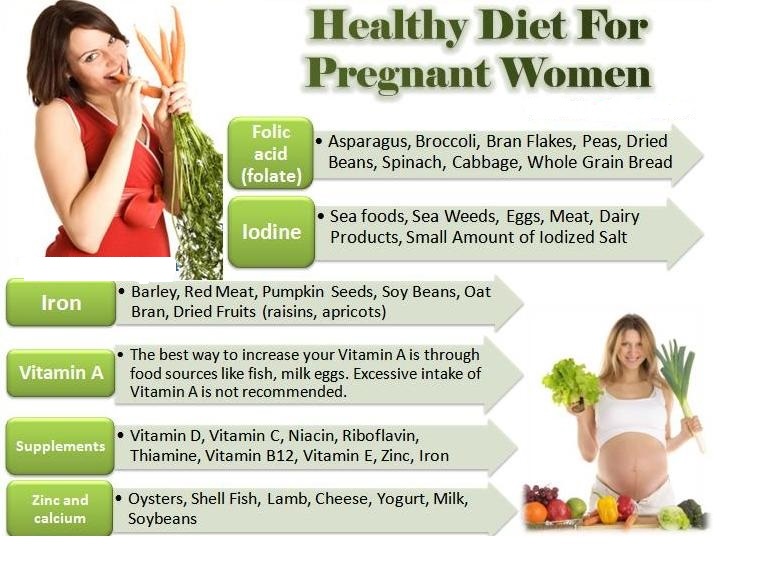
Know Pain is Only Temporary
Understand that it’s natural for breastfeeding to feel painful at first, but your body toughens up and it gets easier. Many women fail when they begin breastfeeding because it’s uncomfortable. When a baby latches in the first few weeks there is about a 10 second “ow ow ow” where you hold your breath and tense up while your nipples sting. (We would equate it to the pain of a clothespin on your finger.)
Pretty soon you’ll stop having to hold your breath and before you know it, latching is no big deal. Breastfeeding can feel uncomfortable at first, but with all new things, it becomes the norm quickly as your body and mind adjust.
Keep Reading 9 Healthy and Delicious Recipes for Eating Milkful Nursing Bars ›
Disclaimer: Some portions of this site may provide you with health-related information or information about Nourisher products based upon information that you provide. However, that information and other content provided through the site (collectively, “Content”) are presented in a summary fashion and intended to be used for educational purposes only.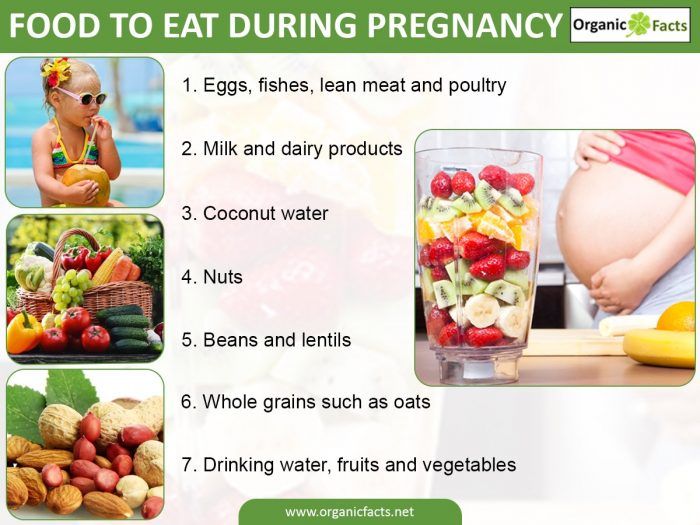 The Content is not intended to be and should not be interpreted as a recommendation for a specific treatment plan or course of action. Your use of this site or the Content does not create a doctor/patient relationship. This site does not offer medical advice and nothing provided through this site, including any content, is intended to constitute professional advice for medical diagnosis or treatment. You should not use this site or any Content to diagnose a health or fitness problem or disease. Use of this site or any Content does not replace medical consultations with a qualified health or medical professional to meet the health and medical needs of you or any other party. Do not disregard the medical advice of a physician or health professional, or delay in seeking such advice, because of any information you obtain from the Site.
The Content is not intended to be and should not be interpreted as a recommendation for a specific treatment plan or course of action. Your use of this site or the Content does not create a doctor/patient relationship. This site does not offer medical advice and nothing provided through this site, including any content, is intended to constitute professional advice for medical diagnosis or treatment. You should not use this site or any Content to diagnose a health or fitness problem or disease. Use of this site or any Content does not replace medical consultations with a qualified health or medical professional to meet the health and medical needs of you or any other party. Do not disregard the medical advice of a physician or health professional, or delay in seeking such advice, because of any information you obtain from the Site.
Pregnant and Breastfeeding - La Leche League GB
If you’re expecting a baby and are continuing to breastfeed your older child, many questions may be going through your mind. Mothers can breastfeed while pregnant; some go on to nurse both their new baby and their older child after the birth. This is known as ‘tandem nursing’.
Mothers can breastfeed while pregnant; some go on to nurse both their new baby and their older child after the birth. This is known as ‘tandem nursing’.
Breastfeeding during pregnancy is a special, unique relationship and one that may constantly evolve to take into account your changing needs and those of your older child. Breastfeeding can help you meet your child’s needs more easily, especially if he is tired or unwell, and it continues to give him important nutritional and immunological benefits. However, breastfeeding whilst pregnant can often invoke intense feelings. Extra support at this time can be crucial and you may find talking things over at your local LLL meetings really helpful.
Is it safe?
Nutrition
Morning sickness
Milk supply and colostrum
Managing when you are not enjoying it
Coping with questions and comments
Deciding to wean
Tandem feeding
Further Reading
Is it safe?
Research tells us there’s usually no reason why a mother shouldn’t breastfeed while pregnant. Although breastfeeding may help a slow labour to progress, the amount of oxytocin normally released is not usually enough to cause the cervix to open before it is ready to do so. Oxytocin is also released during sex, which is generally considered to be safe during pregnancy. If you are expecting multiples or considered to be at risk for miscarriage/early delivery you may be advised to stop breastfeeding. You could discuss this with a breastfeeding-friendly caregiver.
Although breastfeeding may help a slow labour to progress, the amount of oxytocin normally released is not usually enough to cause the cervix to open before it is ready to do so. Oxytocin is also released during sex, which is generally considered to be safe during pregnancy. If you are expecting multiples or considered to be at risk for miscarriage/early delivery you may be advised to stop breastfeeding. You could discuss this with a breastfeeding-friendly caregiver.
Nutrition
You won’t be depriving your unborn baby of nutrients by continuing to breastfeed so long as you eat reasonably well. Getting plenty of rest and eating nutrient dense food will help you stay well-nourished and healthy.
The UK Department of Health recommends that all pregnant women take a vitamin D and folic acid supplement (often taken in the form of the Healthy Start vitamins).
Calcium needs during pregnancy and the first six months of breastfeeding it is normal to experience a gradual loss of bone density. Even if breastfeeding continues, recovery of bone mineral content (BMC) starts from around 3–6 months and is generally complete by about 12 months after birth. If a mother has breastfed there may even be a small overall increase. When a mother becomes pregnant again before 12 months BMC actually continues to increase and tandem nursing mothers have no increased risk for osteoporosis. During pregnancy your body absorbs more calcium from the food you eat. If you feel your diet is low in calcium, then eating foods rich in calcium (eg leafy greens, nuts and seeds) may be a good idea but otherwise there’s no need for any extra.
Even if breastfeeding continues, recovery of bone mineral content (BMC) starts from around 3–6 months and is generally complete by about 12 months after birth. If a mother has breastfed there may even be a small overall increase. When a mother becomes pregnant again before 12 months BMC actually continues to increase and tandem nursing mothers have no increased risk for osteoporosis. During pregnancy your body absorbs more calcium from the food you eat. If you feel your diet is low in calcium, then eating foods rich in calcium (eg leafy greens, nuts and seeds) may be a good idea but otherwise there’s no need for any extra.
Morning sickness
Pregnant mothers often have nausea, whether breastfeeding or not, though breastfeeding while pregnant may make it worse. Eating frequent healthy snacks can help manage nausea, as can getting more rest. Some mothers find motion sickness wristbands work for them.
Milk supply and colostrum
Around the fourth or fifth month (sometimes before) your milk production is likely to reduce due to pregnancy hormones. The composition of your milk will also change and become more similar to weaning milk. Your child may nurse less or wean completely. Some children resume nursing at a later stage. The drop in milk production is due to hormonal changes and nursing more frequently or pumping won’t increase production in the same way it does when you are not pregnant. Your baby may need age appropriate supplements and a baby under 12 months may need his weight monitored. Continuing to breastfeed during pregnancy has no effect on the milk supply that you will have following the birth of your new baby. Colostrum is produced during pregnancy whether or not it is being removed.
The composition of your milk will also change and become more similar to weaning milk. Your child may nurse less or wean completely. Some children resume nursing at a later stage. The drop in milk production is due to hormonal changes and nursing more frequently or pumping won’t increase production in the same way it does when you are not pregnant. Your baby may need age appropriate supplements and a baby under 12 months may need his weight monitored. Continuing to breastfeed during pregnancy has no effect on the milk supply that you will have following the birth of your new baby. Colostrum is produced during pregnancy whether or not it is being removed.
Managing when you are not enjoying it
You may experience nipple soreness, increased nausea and/or feelings of irritability caused by pregnancy hormones. Limiting nursing times, (eg to a few minutes or even a few sucks), ensuring a deep latch, distraction, and offering other snacks/liquids can all help to make nursing through pregnancy more manageable. Support from family and friends can help you get more rest.
Support from family and friends can help you get more rest.
Coping with questions and comments
Pregnancy and breastfeeding can be an emotionally challenging time. It can be difficult if you hear negative comments from others. Talking about the importance of breastfeeding to you and your child can sometimes help people appreciate that this is something you have carefully considered and that it is your choice for your family. Sharing information/research and surrounding yourself with supportive people can also help. Your local LLL group will be a good source of support.
Deciding to wean
The decision to stop breastfeeding is a very personal one and one only you or your child will make. It is useful not to have too many expectations when you get pregnant.
Tandem feeding
Continuing to nurse your older child after your new born arrives can help maintain and strengthen your special bond. Mothers often say that tandem feeding helps their older child to be more accepting of their newborn sibling and helps them through the emotional transition of having to now share their mum.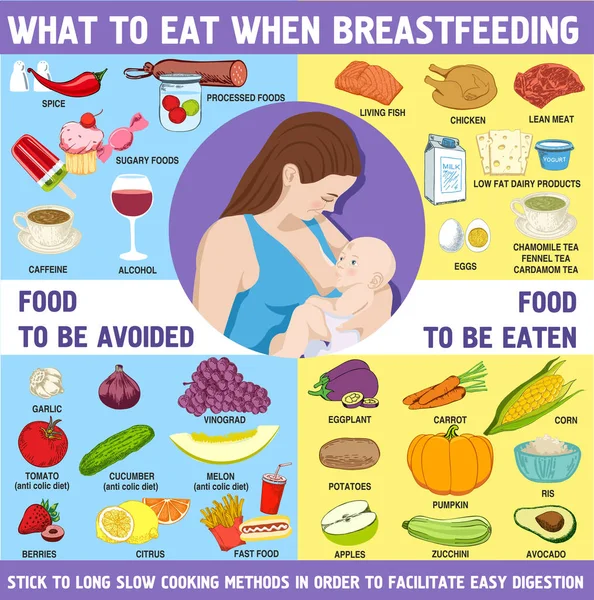 Tandem feeding can also foster a special bond between the siblings. Our page Tandem Nursing has more information.
Tandem feeding can also foster a special bond between the siblings. Our page Tandem Nursing has more information.
Written by Mhairi Kasapidis, Sue Upstone & mothers of La Leche League GB.
Further Reading
Birth & Breastfeeding
Is My Baby Getting Enough Milk?
Nipple Pain
Safe Sleep & the Breastfed Baby
Still Nursing?
Tandem nursing
Thinking of Weaning?
Toddlers and Food
When Mum Can’t Be There
LLLI page on tandem nursing
References
The Womanly Art of Breastfeeding. LLLI, London: Pinter & Martin, 2010.
Adventures in Tandem Nursing. Flower, H. Schaumburg, IL: LLLI, 2003.
Breastfeeding Answers Made Simple. Mohrbacher, N. Amarillo, TX: Hale Publishing, 2010.
How Weaning Happens, Bengson, D.Schaumburg, IL: LLLI, 1999. (link contains book review)
Mothering Your Nursing Toddler. Bumgarner, NJ. Schaumburg, IL: LLLI, 2000. (link contains book review)
Sweet Sleep Nighttime and Naptime Strategies fro the Breastfeeding Family.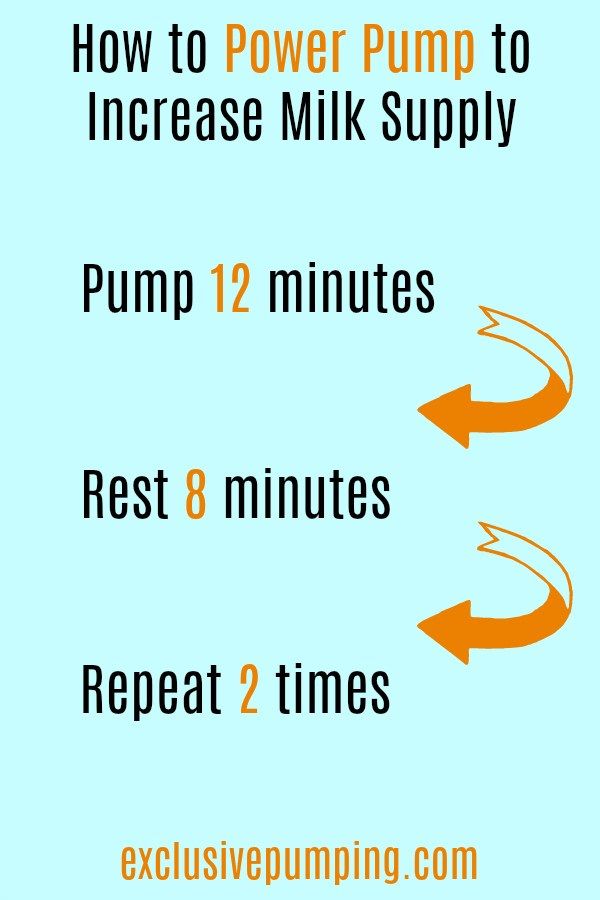 Wiessinger, D.et al. Pinter & Martin, 2014.
Wiessinger, D.et al. Pinter & Martin, 2014.
Prentice A. Maternal calcium metabolism and bone mineral status. Am J Clin Nutr 2000 May;71(5 Suppl):1312S-1312s
This information is available to buy in printed form from the LLLGB Shop
Copyright LLLGB 2016
How to increase the amount of milk for a nursing mother? - an article in the blog of the medical center Health for Children in Moscow
Breastfeeding is the key to good health and mental peace of the child for years to come. But besides this, breastfeeding solves most of the mother's issues: from financial issues to the convenience of building your day and bonding with your child. Galina Vladimirovna Loseva, our most sought-after pediatrician with more than 20 years of experience, tells how to increase the amount of milk for good nutrition of a child
The problem of lack of milk can occur both in the early neonatal period, when lactation is becoming established, and later, for example, during lactation crises, which can occur at certain periods of time (3-6 weeks, 3-4 months, 6 months), as well as after temporary weaning during the mother’s illness or the need to take certain medications that are incompatible with breastfeeding.
Ways to increase lactation:
- Feeding on demand , especially during early lactation. Frequent feedings in the first weeks of life are essential for maximizing the number of prolactin receptors to ensure sufficient milk production in the long term. Without these receptors, lactation will be at risk by 2-3 months of age. It is advisable to attach the baby to the breast as soon as possible after childbirth. If possible, do not use bottle supplements without a good reason. Night feedings are obligatory, the need for them usually lasts up to about 6 months. nine0013
- Proper breastfeeding. The baby must include both the nipple and areola. His mouth should be wide open with his lower lip turned outward
- You can use post-feeding pumping to increase milk production. And at the same time, freeze milk to create a reserve in case the mother leaves or a case of illness in which it is necessary to interrupt breastfeeding.
- Rational nutrition for breastfeeding women.
 The menu should contain cereals, vegetables, fish, meat, eggs, fruits, dairy products are better than sour-milk, a small amount of nuts is acceptable. The use of strict hypoallergenic diets in a woman without an allergic history is unacceptable. Spicy dishes, spices, fried foods are excluded, this can affect the taste and smell of milk. nine0013
The menu should contain cereals, vegetables, fish, meat, eggs, fruits, dairy products are better than sour-milk, a small amount of nuts is acceptable. The use of strict hypoallergenic diets in a woman without an allergic history is unacceptable. Spicy dishes, spices, fried foods are excluded, this can affect the taste and smell of milk. nine0013 - Drinking enough liquid - water, green tea, compotes, fruit drinks. Drinks should preferably be warm or hot. It is recommended to take liquid 20-40 minutes before feeding.
- Eliminate alcohol, nicotine, including passive smoking.
- Compliance with the rest regimen , psycho-emotional peace, positive attitude. This is largely determined by the attitude of close people who can help a nursing mother in household chores, caring for other children, etc. nine0013
- Warm shower, light breast massage just before feeding.
- If you still need supplementary feeding, then it is better to give it with a pipette, spoon, syringe without a needle.
- Pharmacy products: Laktogon, Femilak. From herbs, galega, cumin, anise are considered safe. However, relying only on these funds is not worth it if the above points are not observed. They can be used as ancillary, as an addition to the diet of a nursing mother, which may be insufficient for certain reasons. nine0013
The material was provided by a pediatrician with more than 20 years of experience Galina Vladimirovna Loseva.
All recommendations should be applied after full-time consultation with a specialist doctor.
Pumping when mom needs to go away | Philips Avent
Search Support IconSearch Keywords
Home ›› Weaning
Home ›› Expressing milk during temporary weaning of the mother from the baby . Perhaps you are already using a breast pump to continue breastfeeding when you go to work, or you just want to have more free time between feedings. nine0003 3 Philips Avent products to help you pump and store your milk comfortably:
Not sure when to start expressing milk or when to start using a breast pump? Don't worry, we've put together a quick guide to help you learn how to express milk and learn about the benefits of using a breast pump. We'll also give you tips on how to express your milk when you're away from home, how to keep it adequate, and how to store it safely. nine0003
When should I start expressing milk?
Most women begin to express milk after six months, but there are circumstances that force them to do so earlier.
If you intend to express milk as early as possible, the answer to the question “When can I start expressing milk?” will be: "A few hours after birth." Some mothers find that expressing milk is effective at a very early stage, especially if the baby has latch-on problems, as pumping improves the flow of milk to the breast. nine0058
Other mothers start expressing after breastfeeding is established because they want someone in the household to help with feeds while they are away or with feeds after they return to work.
There are no specific rules about when to start pumping, so you can do whatever works best for you. Whatever your needs, you can pump to make your schedule less dependent on feedings.
How to express breast milk: general questions
How long should I express milk? How much milk do I need to express? What equipment do I need for this? Every mother has questions about this topic, however, once she starts expressing milk, she easily adapts to this process.
Most moms find a breast pump to be the easiest way to express breast milk. The principle of operation of different breast pumps may vary slightly, so read the instructions for use before using the device. Remember that it can take 1-2 minutes for milk to come out of your breast during pumping, so don't worry if you don't see it right away! nine0003
Not sure how long to express milk? If you are not in a hurry, try to express milk until you feel that your chest is empty. Due to the individual characteristics of each woman, the pumping time will be different.
The amount of milk expressed will depend on when you last breastfed and how long you have been using the pump and are accustomed to using it. Even your internal state and time of day can affect the amount of milk. If you have problems with lactation, check out our tips for increasing your milk supply. Generally, the best time to express is in the morning. During sleep, there is an increase in the level of hormones responsible for the production of milk. nine0003
Even your internal state and time of day can affect the amount of milk. If you have problems with lactation, check out our tips for increasing your milk supply. Generally, the best time to express is in the morning. During sleep, there is an increase in the level of hormones responsible for the production of milk. nine0003
Should breastfeeding be combined with pumping? Wait about an hour between pumping and the next feeding. So you will be sure that the baby will have enough milk! Feed your baby as much as it takes to keep him full and happy. Use a breast pump to fully express milk from your breasts and save excess milk.
How to Express Breast Milk: Practical Tips
Whether you are expressing milk at home (for a night feed) or at work, there are a few key points to keep in mind to help you. nine0003
1. Plan ahead. If you have to leave your baby, start using a breast pump a few weeks in advance. This way you will store enough milk for your baby and get used to using a breast pump.
2. Be ready. You may be aware of the so-called "oxytocin reflex", which stimulates the flow of milk due to the release of the hormone oxytocin. Oxytocin increases the secretion of breast milk that can be expressed. The production of the hormone can be caused in many ways, even just by looking at the child. Therefore, many mothers find it effective to look at a photo of their baby while pumping while away from home. After you finish pumping, you can also use bra pads to keep your breasts dry and protect your clothes from milk stains. nine0058
3. Get comfortable. The more comfortable you feel, the easier it will be to express milk. Find a quiet, private place and feel free to change the lighting and music to your liking. It is helpful to find a seat with good support so that you can sit comfortably with the pump in front of you.
Get comfortable. The more comfortable you feel, the easier it will be to express milk. Find a quiet, private place and feel free to change the lighting and music to your liking. It is helpful to find a seat with good support so that you can sit comfortably with the pump in front of you.
4. Express as many times as you would like to breastfeed your baby. To maintain the required supply of milk, express it as often as you normally feed your baby. Thus, if the baby usually has three feedings during your absence, then you need to express milk at least three times. nine0003
How to choose the best breast pump for expressing milk
There are several different types of breast pumps, each with its own advantages. Choose the one that will help you feel comfortable in your daily life. Perhaps you prefer to have a device that is designed to be used on the go? Or do you need a breast pump that will allow you to express milk quickly?
Storage and preparation of milk after pumping
After you have expressed your milk, remember to freeze or refrigerate it. Then, before feeding the baby, it must be thawed and warmed up. Here are some tips on how to store breast milk:
Then, before feeding the baby, it must be thawed and warmed up. Here are some tips on how to store breast milk:
- Use sterile milk storage containers or freezer bags to collect and store milk.
- Do not fill the container to the upper limit, because when frozen, breast milk "expands", the optimal portion for storage is 60-120 ml. nine0013
- Label the container with the pumping date or write the pumping date on the container with a permanent marker.
- Store milk in the refrigerator at 2-4°C for up to 24 hours.
- After cooling the expressed milk in the refrigerator for 0.5 hours, the milk can be frozen in the freezer and stored there for 3 months.
- Place the milk closer to the back of the refrigerator or freezer rather than in the door to keep the milk at a constant temperature. nine0013
- Thawed milk placed in the refrigerator should be used within 24 hours.
- Do not refreeze thawed milk.
- Transport milk in an insulated container with an ice pack.
Use these tips to prepare your expressed milk for breastfeeding:
- Thaw or warm breast milk under running warm water, in a bain-marie, or with a bottle warmer. nine0013
- Do not use a microwave oven to heat milk.
- Do not heat milk to boiling point.
- Shake the milk bottle before feeding until smooth.
- Check milk temperature before feeding. The most optimal temperature is the average between body temperature and room temperature. To check the temperature of milk, you can drop it on your skin.
Advice for first-time moms
If you are just starting to express milk, remember that this process may not be entirely comfortable. The more relaxed you are, the easier it will be to express milk. Sometimes this will be difficult to do, for example if you are trying to express milk during a busy work day or in an unfamiliar place; therefore, it is necessary to practice well at home and show patience.