How soon can you miscarry
Miscarriage | NHS inform
A miscarriage is the loss of your baby before 24 weeks. Early miscarriages happen in the first 12 weeks of pregnancy. Late miscarriages happen between 12 and 24 weeks.
Most of the time there’s no clear reason why it happens, but it’s very unlikely to be caused by anything you did or didn’t do.
About 1 out of 5 pregnancies miscarry. Since many miscarriages aren't recorded the figure might be higher.
When to get medical help
Always get medical help if:
- you're bleeding from your vagina
- you've got strong, cramping pain
- your waters break
- your baby's movements have changed, or you haven't felt them move for a while
If you're registered, contact your midwife or local maternity unit. If you’re not registered, contact your GP or the NHS 24 111 service.
What causes a miscarriage?
Doctors think most miscarriages are caused when the building blocks controlling the development of a baby (the chromosomes) aren’t right. Babies with too many or not enough chromosomes won't develop properly. This leads to a miscarriage.
Miscarriages can also be caused by:
- issues with your placenta
- cervical weakness - when your cervix (neck of your womb) starts to open
Early miscarriages
An early miscarriage happens in the first 12 weeks of pregnancy. Most women who miscarry do so in the first 12 weeks of their pregnancy.
Many women have a miscarriage before they even know they’re pregnant. If this happens it can feel like a late period with heavy bleeding.
Symptoms of an early miscarriage
You might be having an early miscarriage if:
- you're bleeding from your vagina
- you've cramps in your lower abdomen – these can feel like bad period pains
- there's fluid or tissue coming from your vagina
- your breasts are no longer tender and any morning sickness has passed
Bleeding
Having some light bleeding's fairly common in the first 12 weeks of pregnancy and doesn't necessarily mean you're having a miscarriage.
If you start bleeding, you should always contact your GP or midwife and get advice about what to do.
What happens during an early miscarriage
If you’re in the early weeks of pregnancy:
- you’ll probably be asked to go to the early pregnancy unit at your local hospital straight away
- you’ll have some tests and usually an ultrasound scan
- your body usually completes the miscarriage naturally
Depending on your stage of pregnancy, you may deliver a small baby. That can be a shock and is an understandably upsetting time.
Late miscarriages
A late miscarriage happens after 12 weeks and before 24 weeks.
For many parents who lose their baby after a late miscarriage, the word ‘miscarriage’ doesn't properly express the impact of their loss. The loss of a baby at any time's a terrible shock and a late miscarriage can be especially hard.
Symptoms of a late miscarriage
You might be having a late miscarriage if:
- you're bleeding from your vagina – this can be heavy and you might have blood clots
- you've strong, cramping pains
Always get medical help if:
- you're bleeding
- your baby’s movements have changed or you haven’t felt any movements for a while.

- your waters break and your baby's born very quickly
Contact your midwife or local maternity unit if you’re registered with them. If you’re not registered, contact your GP or phone the NHS 24 111 service.
What happens during a late miscarriage
If you’re later on in pregnancy:
- you may be asked to go to the maternity ward
- you’ll have some tests and usually an ultrasound scan
- you're likely to go through labour in hospital and might have your labour induced
While you deliver your baby you're likely to have heavier bleeding and labour-like pains.
Making difficult decisions
If you're having a miscarriage, your doctor or midwife will:
- talk to you about what will happen next
- help you, and your partner if you have one, decide what you’d like to do
You may have many difficult decisions to make at this time and will have overwhelming emotions. Take your time. Your midwife or doctor can help, and there are many organisations that can support you, your baby’s father and your family.
Get support from SANDS
Get support from SiMBA
After a miscarriage
Depending on your circumstances and stage of pregnancy, your midwife or doctor may ask if you'd like to see or hold your baby.
Some parents decide they don't want to see their baby, and others choose not to for faith or cultural reasons. This is a decision only you can make. It can be very hard when you're feeling overwhelmed. Whatever you decide is okay.
If you’re worried about what your baby looks like, your midwife or doctor can describe them to help you decide.
If your symptoms continue
You’ll probably have some bleeding for a week or two. If you continue to have symptoms after your miscarriage, it may mean that some of the pregnancy tissue's still in your womb.
Some women may need medicine or a short operation to treat this.
If you’re worried about seeking treatment, maybe a friend can come with you. Having support's really important at this difficult time.
Taking time off work
Many women will want to take time off work after having a miscarriage.
If you have a miscarriage before the end of the 24th week, you’re entitled to:
- take sick leave
- any sick pay you'd normally qualify for
If you lose your baby after the end of the 24th week, you’re entitled to:
- take maternity leave
- any maternity pay you qualify for
Speak to your employer about which choices may be right for you and your family.
Working Families has more about your rights at work after a miscarriage
Repeated miscarriages
Most women go on to have a successful pregnancy and a healthy baby after a miscarriage. But unfortunately, some women have repeated miscarriages.
If you've had:
- 1 or 2 miscarriages - you're not more likely than anyone else to have another one
- 3 or more miscarriages - your GP can refer you to a specialist to see whether there’s a specific cause
Miscarriage - Causes - NHS
There are many reasons why a miscarriage may happen, although the cause is often not identified.
If a miscarriage happens during the first trimester of pregnancy (the first 3 months), it's usually caused by problems with the unborn baby (foetus). About 3 in every 4 miscarriages happen during this period.
If a miscarriage happens after the first trimester of pregnancy, it may be the result of things like an underlying health condition in the mother.
These late miscarriages may also be caused by an infection around the baby, which leads to the bag of waters breaking before any pain or bleeding. Sometimes they can be caused by the neck of the womb opening too soon.
First trimester miscarriages
First trimester miscarriages are often caused by problems with the chromosomes of the foetus.
Chromosome problems
Chromosomes are blocks of DNA. They contain a detailed set of instructions that control a wide range of factors, from how the cells of the body develop to what colour eyes a baby will have.
They contain a detailed set of instructions that control a wide range of factors, from how the cells of the body develop to what colour eyes a baby will have.
Sometimes something can go wrong at the point of conception and the foetus receives too many or not enough chromosomes. The reasons for this are often unclear, but it means the foetus will not be able to develop normally, resulting in a miscarriage.
This is very unlikely to recur. It does not necessarily mean there's any problem with you or your partner.
Placenta problems
The placenta is the organ linking your blood supply to your baby's. If there's a problem with the development of the placenta, it can also lead to a miscarriage.
Things that increase your risk
An early miscarriage may happen by chance. But there are several things known to increase your risk of problems happening.
Your age can also have an influence:
- in women under 30, 1 in 10 pregnancies will end in miscarriage
- in women aged 35 to 39, up to 2 in 10 pregnancies will end in miscarriage
- in women over 45, more than 5 in 10 pregnancies will end in miscarriage
A pregnancy may also be more likely to end in miscarriage if you:
- are obese
- smoke
- use drugs
- drink lots of caffeine
- drink alcohol
Second trimester miscarriages
Long-term health conditions
Several long-term (chronic) health conditions can increase your risk of having a miscarriage in the second trimester, especially if they're not treated or well controlled.
These include:
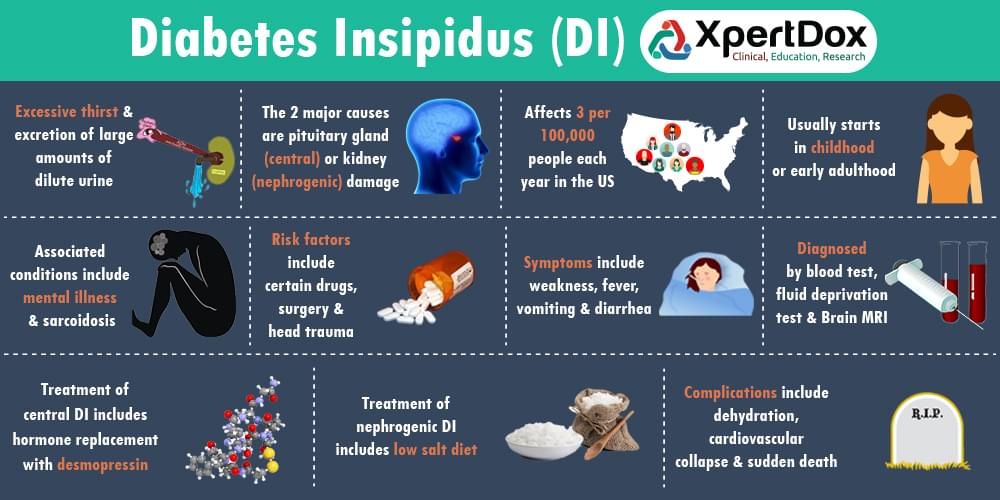
- diabetes (if it's poorly controlled)
- severe high blood pressure
- lupus
- kidney disease
- an overactive thyroid gland (hyperthyroidism)
- an underactive thyroid gland (hypothyroidism)
- antiphospholipid syndrome (APS)
Infections
The following infections may also increase your risk:
- rubella (german measles)
- cytomegalovirus (CMV)
- bacterial vaginosis
- HIV
- chlamydia
- gonorrhoea
- syphilis
- malaria
Food poisoning
Food poisoning, caused by eating contaminated food, can also increase the risk of miscarriage. For example:
For example:
- listeriosis – most commonly found in unpasteurised dairy products, such as blue cheese
- toxoplasmosis – which can be caught by eating raw or undercooked infected meat
- salmonella – most often caused by eating raw or partly cooked eggs
Read more about foods to avoid in pregnancy.
Medicines
Medicines that increase your risk include:
- misoprostol – used for stomach ulcers
- retinoids – used for eczema and acne
- methotrexate – used for conditions such as rheumatoid arthritis
- non-steroidal anti-inflammatory drugs (NSAIDs) – such as ibuprofen; these are used for pain and inflammation
To be sure a medicine is safe in pregnancy, always check with your doctor, midwife or pharmacist before taking it.
Read more about medicines during pregnancy.
Womb structure
Problems and abnormalities with your womb can also lead to second trimester miscarriages. Possible problems include:
- non-cancerous growths in the womb called fibroids
- an abnormally shaped womb
Weakened cervix
In some cases, the muscles of the cervix (neck of the womb) are weaker than usual. This is known as a weakened cervix or cervical incompetence.
A weakened cervix may be caused by a previous injury to this area, usually after a surgical procedure. The muscle weakness can cause the cervix to open too early during pregnancy, leading to a miscarriage.
Polycystic ovary syndrome (PCOS)
Polycystic ovary syndrome (PCOS) is a condition where the ovaries are larger than normal. It's caused by hormonal changes in the ovaries.
It's caused by hormonal changes in the ovaries.
PCOS is known to be a leading cause of infertility as it can prevent the release of an egg (ovulation). There's some evidence to suggest it may also be linked to an increased risk of miscarriage.
Misconceptions about miscarriage
An increased risk of miscarriage is not linked to:
- your emotional state during pregnancy, such as being stressed or depressed
- having a shock or fright during pregnancy
- exercise during pregnancy – but discuss with your GP or midwife what type and amount of exercise is suitable for you during pregnancy
- lifting or straining during pregnancy
- working during pregnancy – or work that involves sitting or standing for long periods
- having sex during pregnancy
- travelling by air
- eating spicy food
Recurrent miscarriages
If you have had a miscarriage, it's natural to worry that you'll have another if you get pregnant again. But most miscarriages are a one-off event.
But most miscarriages are a one-off event.
About 1 in 100 women experience recurrent miscarriages (3 or more in a row) and many of these women go on to have a successful pregnancy.
Page last reviewed: 09 March 2022
Next review due: 09 March 2025
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with severe consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this. However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it.
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage in this period is also considered early. Its most common causes are:
Endocrine disorders
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.
Imbalance of hormones in a woman's body is very likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time.
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 about C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Reduced immunity
Reduced immunity during pregnancy also refers to immune causes. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage between 12 and 22 weeks
Such a miscarriage is considered late. Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
In isthmic-cervical insufficiency, there is only one method of treatment - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina. The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children.
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.
Miscarriages due to hemostasis disorders
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis).
Blood coagulation disorders leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (bleeding tendencies). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop.
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.
When planning a pregnancy, a genetic examination should be carried out and, if necessary, treatment should be started.
It is advisable to be examined for hidden hemostasis defects even for those who consider themselves healthy. This will allow you to predict the occurrence of complications and prevent loss. Early therapy can prevent miscarriage at 98% of cases. If defects in hemostasis are already detected during pregnancy, it can be difficult to maintain it.
What to do after a miscarriage?
Find the cause! The ideal option is to be examined by future parents: it is much more reasonable to postpone conception and spend two or three months to identify the causes than to risk getting pregnant again, spend two months waiting, and then lose everything again and still go to the doctors.
Until you understand the reason, it will not evaporate. In most cases, the answers lie on the surface. Take care of your health and your future baby.
Sign up for a consultation with an obstetrician-gynecologist by phone +7 (495) 150-60-01
Tyan Oksana Alexandrovna
Head of the department, obstetrician-gynecologist Doctor of the highest category Work experience: 26 years
Volkova Polina Dmitrievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the highest category Experience: 35 years
Postnikova Nadezhda Anatolyevna
Obstetrician-gynecologist, ultrasound specialist Work experience: 35 years
Moiseeva Alla Vitalievna
Obstetrician-gynecologist, doctor of ultrasound diagnostics Doctor of the first category Work experience: 37 years
Zabolotnova Olga Valentinovna
Obstetrician-gynecologist Doctor of the first category Experience: 25 years
Shchelokova Elena Nikolaevna
Obstetrician-gynecologist Doctor of the highest category Work experience: 38 years
Pass or medical card number:
Contact phone: *
Select the day of your appointment:
Additional information:
I am not a robot
By clicking the "Submit Application" button, you agree to the terms Privacy Policy and User Agreement
What is a miscarriage and why it can happen
###1### What is a miscarriage
First of all, you should define the terms. Miscarriage in gynecological practice is called spontaneous termination of pregnancy in the first 20–22 weeks. Why 20-22 weeks? There is such a consensus: doctors save a fetus born with a weight of 500 grams or more. The chances of saving someone who was born weighing less than 500 grams are zero. At 20–22 weeks, the fetus just usually reaches such a mass.
Miscarriage in gynecological practice is called spontaneous termination of pregnancy in the first 20–22 weeks. Why 20-22 weeks? There is such a consensus: doctors save a fetus born with a weight of 500 grams or more. The chances of saving someone who was born weighing less than 500 grams are zero. At 20–22 weeks, the fetus just usually reaches such a mass.
The frequency of miscarriages is quite high: they end in 15-20% of pregnancies.
That is, for a practicing doctor, this is a fairly common situation, although in the life of each person, of course, this can happen only once or not at all.
Medical statistics, which make it possible to translate medicine into the language of numbers and make it a more accurate science, indicate that of these 15-20% of pregnancies that end in miscarriages, 80% or more occur in the first 12 weeks. That is, the longer the gestational age, the less likely it is that a spontaneous miscarriage will occur. Thus, if I, as a doctor, meet a woman who is diagnosed with a threatened miscarriage, give her an ultrasound and see a fetus with a heartbeat, I can immediately tell her that the probability of a miscarriage is no longer 15%, but 5%. If I see a situation where the gestation period is already more than 12 weeks, then the probability is already 2-3%.
If I see a situation where the gestation period is already more than 12 weeks, then the probability is already 2-3%.
How does a miscarriage happen? Regardless of the reason, the scenario is the same.
First the fetus dies; then detachment from the walls of the uterus begins (then the woman has spotting, which is classified as a “threatening miscarriage”), and then the exfoliated is thrown out of the uterine cavity. The problem is that the same symptoms can be observed in both an ectopic pregnancy and a normal, healthy intrauterine pregnancy. If the ultrasound shows a live intrauterine pregnancy, in most cases the cause of bleeding during pregnancy remains unknown. It is the appearance of bloody discharge against the background of a live intrauterine pregnancy that is designated by doctors as a “threatening miscarriage”. In the vast majority of cases, despite the formidable diagnosis, such a pregnancy is completely safely completed. Of course, any woman passionately wants to know what this bloody discharge is because of, because she thinks: now I will find out what it is because of, I will remove this factor from my life, and everything will be fine, they will stop with me. We have to disappoint a woman: in most cases, we do not know the reason.
We have to disappoint a woman: in most cases, we do not know the reason.
Accidental and habitual miscarriage
All miscarriages are divided into two large types - sporadic (accidental) and habitual. In essence, they are determined by the same range of causes, only the proportion of each of the causes in two cases will be very different. In turn, all causes can be divided into two large groups: internal causes caused by fetal problems, and external causes caused by problems in the mother's body. Accordingly, sporadic miscarriages are most often determined by causes associated with the fetus, and habitual miscarriages are determined by the mother's body.
Medical statistics show that more than half of sporadic miscarriages in the first 12 weeks are due to genetic disorders in the fetus.
Moreover, the shorter the gestational age, the higher the likelihood that the cause was a genetic disorder in the fetus. These are generalized data from numerous studies, mostly Western ones. Let's look at this most common reason first. The fact is that no matter how kings of nature we think we are, the same laws of nature apply to us as to an ant, an insect, a blade of grass.
Let's look at this most common reason first. The fact is that no matter how kings of nature we think we are, the same laws of nature apply to us as to an ant, an insect, a blade of grass.
Nobody canceled these biological laws: the best and the strongest survive in the good sense of the word, in the biological sense.
A biological individual cannot always produce 100% quality cells (in this case we are talking about germ cells). So, 1 ml of a man's sperm contains on average 20 million spermatozoa, and normally about 10% of them, that is, 2 million, are pathological forms. And such a spermogram will be considered normal. In a woman, too, poor-quality eggs can mature, and the older we get, the more likely it is that a poor-quality egg will mature. It's not because we're deliberately doing something wrong - lifting something heavy, drinking an extra cup of coffee, overworking at home/work. Unlike spermatozoa, which are constantly renewed, all the eggs of a future woman are laid at the moment when her mother is at the 20th week of pregnancy.
And new eggs are never laid again, they are only used up, only lost throughout the life of a girl/woman.
That is, if you are 35 years old, then the egg that came out of your ovary this month has been lying in the ovary waiting for its turn to ovulate for more than 35 years. Therefore, of course, in a 20-year-old woman and in a 40-year-old woman, not only the quantity, but also the quality of the eggs will be different. Because everything unfavorable that is around us in terms of nutrition, environment, air and water affects the first only 20 years, and the second - already 40.
The dependence of the frequency of spontaneous miscarriage due to genetic disorders in the fetus on the age of the eggs (and, consequently, on the age of the woman) was shown thanks to the introduction of in vitro fertilization technology - IVF. A very good study was conducted on a group of patients over 40 who underwent IVF. Half of them were implanted with their own fertilized eggs, and the other half - donor eggs taken from women under 25 years old. In the group that carried embryos from donor eggs, the miscarriage rate corresponded to that of women under 25 years of age and was three to four times lower than in the group that was implanted with embryos obtained from their 40-year-old eggs. Thus, the probability of miscarriages and genetic disorders of the fetus is determined by the biological age of the woman. It's the kind of thing we can't reverse in any way, and it should be taken into account when a pregnancy is postponed to a later date.
In the group that carried embryos from donor eggs, the miscarriage rate corresponded to that of women under 25 years of age and was three to four times lower than in the group that was implanted with embryos obtained from their 40-year-old eggs. Thus, the probability of miscarriages and genetic disorders of the fetus is determined by the biological age of the woman. It's the kind of thing we can't reverse in any way, and it should be taken into account when a pregnancy is postponed to a later date.
Thus, if a defective egg meets a normal sperm or vice versa, then the resulting pregnancy with a poor-quality embryo is rejected at a certain stage and a miscarriage occurs.
And here comes the most interesting, because we still do not know which mechanism in the body recognizes that the pregnancy is of poor quality. But this mechanism exists, and it works very well, otherwise all abnormal pregnancies would lead to the birth of not quite healthy or completely unhealthy people, and humanity would have already degenerated. We do not know this mechanism, but we can say: if a woman has a spontaneous miscarriage, then these mechanisms work for her and from a biological point of view she is healthy. It is much worse if we see a different situation (although it is quite rare): far beyond the 20-week period, we do an ultrasound and find severe defects in the fetus. Because of these defects, after birth, he may either be disabled or not be able to survive at all, but now he lives inside the uterus, which suggests that the mechanisms that recognize healthy and unhealthy pregnancy did not work in this woman.
We do not know this mechanism, but we can say: if a woman has a spontaneous miscarriage, then these mechanisms work for her and from a biological point of view she is healthy. It is much worse if we see a different situation (although it is quite rare): far beyond the 20-week period, we do an ultrasound and find severe defects in the fetus. Because of these defects, after birth, he may either be disabled or not be able to survive at all, but now he lives inside the uterus, which suggests that the mechanisms that recognize healthy and unhealthy pregnancy did not work in this woman.
Therefore, with all the emotional and psychological disadvantages that a spontaneous miscarriage brings for a woman, there is a big plus in this event, which is not obvious to the patient.
This is a universal biological mechanism that allows you to keep us and our offspring healthy and prevents the birth of a handicapped child.
If the majority of spontaneous miscarriages are caused by genetic disorders, the question arises which pregnancies should then be saved. Unfortunately, any gynecologist has encountered cases in his practice when attempts to “pull out” a pregnancy with incredible efforts lead to a deplorable result. That is, the pregnancy threatened to terminate, the woman was given numerous medications, and she persisted, but after the 20th week it turned out that the fetus had serious developmental disorders. It should be said separately about medicines. Serious Western studies (there is such a term as "double-blind placebo-controlled study", it guarantees the quality and statistical significance of the results as much as possible) show that there is not a single medication, except for progesterone, a female hormone that can affect pregnancy.
Unfortunately, any gynecologist has encountered cases in his practice when attempts to “pull out” a pregnancy with incredible efforts lead to a deplorable result. That is, the pregnancy threatened to terminate, the woman was given numerous medications, and she persisted, but after the 20th week it turned out that the fetus had serious developmental disorders. It should be said separately about medicines. Serious Western studies (there is such a term as "double-blind placebo-controlled study", it guarantees the quality and statistical significance of the results as much as possible) show that there is not a single medication, except for progesterone, a female hormone that can affect pregnancy.
If a pregnancy is doomed to death, it will die; if it must survive, it will survive, unless, of course, we are talking about a healthy woman who has biological mechanisms currently unknown to us for culling poor-quality pregnancies.
We, in Russia, have a different practice, caused not by scientific objective data, but rather by cultural differences - the fact that our medicine has been isolated from the world community for a long time.
The second most common cause of miscarriage is infection. This is the same failure. Severe flu is an obvious reason for sporadic miscarriage. Pregnancy does not destroy the disease, but its consequence - the general poor condition of the woman's body, the environment that ensures the life of the fetus. Unlike genetic reasons, when the embryo was laid "bad", in the case of infection, the embryo was laid healthy and of high quality. But suddenly the woman fell ill with a severe flu - a temperature of 40, vomiting, dehydration. It is difficult for a tiny creature to survive in such adverse conditions, and it dies. The death of the embryo is due to environmental disturbances - high temperature, dehydration, intoxication.
If a second miscarriage occurs, it is difficult to attribute it to the flu: it is hard to believe that a woman gets the same severe flu from year to year at the same time. Here it is - the difference between sporadic and habitual miscarriage.
The first one happens really by chance - it's a classic "failure". The second is a pattern: when we see a woman with a habitual miscarriage, she, as a rule, has an interruption at about the same time. Then we assume that there is a reason that does not exist very clearly in the body: it does not prevent a woman from living outside the state of pregnancy, but it makes itself felt when a normal pregnancy occurs. This reason, which does not exist very noticeably in a woman's body, prevents her from carrying a pregnancy to term. It leads to the fact that normal conditions for the survival of a healthy fetus are not created, and it dies, and this happens from time to time. This is the fundamental difference between a habitual miscarriage and a sporadic one. In this case, we will conduct a series of studies (quite expensive) to find out what the reason is.
The second is a pattern: when we see a woman with a habitual miscarriage, she, as a rule, has an interruption at about the same time. Then we assume that there is a reason that does not exist very clearly in the body: it does not prevent a woman from living outside the state of pregnancy, but it makes itself felt when a normal pregnancy occurs. This reason, which does not exist very noticeably in a woman's body, prevents her from carrying a pregnancy to term. It leads to the fact that normal conditions for the survival of a healthy fetus are not created, and it dies, and this happens from time to time. This is the fundamental difference between a habitual miscarriage and a sporadic one. In this case, we will conduct a series of studies (quite expensive) to find out what the reason is.
Today, there is a consensus in the world scientific community that recurrent miscarriage is considered a case when a woman has two miscarriages in a row. If a woman had one miscarriage and she comes to me and asks what is the probability that this will happen again, these are the same 15-20%. If this situation occurred twice in a row, then the probability that this will happen again is already about 30–35%, and if three times in a row, it is almost 40%.
If this situation occurred twice in a row, then the probability that this will happen again is already about 30–35%, and if three times in a row, it is almost 40%.
In about 2% of married couples, wives suffer from recurrent miscarriage.
If in the case of sporadic miscarriages, the fetus and its disorders are most often “to blame”, then in case of habitual miscarriages, its environment, the woman’s body, is usually “to blame”. As with sporadic miscarriages, genetics can be the cause. But if in sporadic miscarriage genetics is the cause of 70–80% (up to 6 weeks in general 90%) of all interruptions, then in the case of habitual miscarriage, genetic disorders are found only in 2–3% of patients. The same is true for infections: in a recurrent miscarriage, the likelihood that repeated abortions are due to infection is no more than 1%.
Hormonal disorders in a woman's body, on the other hand, are more likely to cause habitual rather than accidental miscarriage.
Disturbances in the structure of the uterus - a septum inside the uterus, a bicornuate uterus, the presence of synechia (the so-called adhesions inside the uterus) - these are all things that can also lead to repeated miscarriages.
Approximately 40% of women diagnosed with "recurrent miscarriage" are found to have various immune disorders that cause the fetus to be rejected by the mother's body. Immune disorders are divided into autoimmune and alloimmune. Autoimmune disorders are situations where a woman's immune system works against its own genes, proteins. One of the most common diseases of this kind among women with recurrent miscarriage is antiphospholipid syndrome. Phospholipids are the "glue" that holds cells together. A woman with antiphospholipid syndrome produces factors (antibodies) against her own phospholipids, which are abundant in the placenta. As a result of the syndrome, blood clots form in the small vessels of the placenta, which disrupt blood circulation, and therefore disrupt the function of the placenta to deliver nutrients to the fetus. Pregnancy under such conditions cannot “stretch” for a long time - sooner or later, the death of a healthy embryo / fetus occurs. Women suffering from antiphospholipid syndrome carry a pregnancy in no more than 10% of cases. Its treatment allows you to reverse the statistics - gestation occurs as early as 90% of cases. A woman is given drugs that thin the blood and prevent the formation of blood clots - the placenta performs its function, and the pregnancy is carried.
Its treatment allows you to reverse the statistics - gestation occurs as early as 90% of cases. A woman is given drugs that thin the blood and prevent the formation of blood clots - the placenta performs its function, and the pregnancy is carried.
Alloimmune causes are aggressive factors directed against foreign proteins, that is, the paternal part of the fetal genome. In general, our immune system is required to produce antibodies and get rid of any foreign and pathologically altered cells. Why a pregnancy consisting of 50% of "foreign" genes is not rejected (not to mention 100% of genetic foreignness when a surrogate mother carries a "foreign" embryo in the IVF program) is not yet entirely clear. By the way, scientists believe that when it is found out what is the mechanism that prevents the rejection of pregnancy cells with "foreign genes", this can help in the development of a cure for cancer. After all, cancer consists of pathologically altered cells, which, for some reason, are also not rejected, not destroyed by the immune system. One way or another, during pregnancy, a woman in relation to foreign genes / proteins of the placenta and fetus develops a condition called immunological tolerance - “we do not notice and do not attack strangers”. In the case of a habitual miscarriage, this tolerance does not exist: the mother's immune system recognizes foreign genes and proteins of pregnancy, attacks them, and thereby leads to repeated miscarriages.
One way or another, during pregnancy, a woman in relation to foreign genes / proteins of the placenta and fetus develops a condition called immunological tolerance - “we do not notice and do not attack strangers”. In the case of a habitual miscarriage, this tolerance does not exist: the mother's immune system recognizes foreign genes and proteins of pregnancy, attacks them, and thereby leads to repeated miscarriages.
Quite often, in about 40% of all cases, after conducting the necessary examination of both spouses, we, unfortunately, do not find any reasons explaining why this couple has repeated miscarriages.
There is such a term as "unexplained recurrent miscarriage", as well as "unexplained infertility". Maybe in five years, medicine will find something new in this area, new explanations, but so far this has not happened. This is a psychologically difficult moment for both the doctor and the patients.
Two worlds, two approaches
When a woman is at risk of miscarriage, the actions of a doctor in Russia and abroad will be fundamentally different, and this is due not so much to different scientific data as to cultural differences that have arisen during the isolation of our medical school. Abroad, such women are simply sent home: they are "prescribed" bed rest, a general clinical examination, and sexual rest. Time will tell how this situation will end: either the pregnancy will continue, or a miscarriage will occur if it was of poor quality, and it’s good that it was “rejected” by the body.
Abroad, such women are simply sent home: they are "prescribed" bed rest, a general clinical examination, and sexual rest. Time will tell how this situation will end: either the pregnancy will continue, or a miscarriage will occur if it was of poor quality, and it’s good that it was “rejected” by the body.
In Russia, the psychological attitude of the population towards medicine is slightly different and medicine is slightly different.
In our country, threatened miscarriage is an indispensable indication for hospitalization: there the patient is prescribed "no-shpu", drugs that relax the uterus, hemostatic drugs. This is not a matter of biological or medical differences - it is a matter of psychology for most of our population: if a doctor did not give a pill, then he did not seek to help. And it is quite difficult to convey to people that the laws of nature apply here - you cannot influence them. According to our Russian protocol, I have no right not to offer hospitalization in case of a threatened miscarriage. However, scientific medical facts clearly show that hospitalization does not fundamentally change anything in the prognosis: the likelihood of spontaneous miscarriage does not decrease from this. Western studies show that there are no medications that can cure sporadic miscarriage. If the pregnancy persists, then it is nature that preserves the pregnancy, not the cure. There are such medicines for a habitual miscarriage: if it was possible to identify the cause of repeated abortions, it can be influenced. This treatment is prescribed either before the onset of pregnancy, or in the early stages of pregnancy, before any symptoms of threatened miscarriage appear.
However, scientific medical facts clearly show that hospitalization does not fundamentally change anything in the prognosis: the likelihood of spontaneous miscarriage does not decrease from this. Western studies show that there are no medications that can cure sporadic miscarriage. If the pregnancy persists, then it is nature that preserves the pregnancy, not the cure. There are such medicines for a habitual miscarriage: if it was possible to identify the cause of repeated abortions, it can be influenced. This treatment is prescribed either before the onset of pregnancy, or in the early stages of pregnancy, before any symptoms of threatened miscarriage appear.
After the first miscarriage, we examine the woman, but this is the usual list of studies that are needed before any pregnancy. Of course, tests can be added to it based on the nuances of the medical history of a particular woman.
But it is important to understand that nothing can be done to reduce the likelihood of a recurrence in a subsequent pregnancy to zero.