How frequently do braxton hicks occur
Braxton Hicks contractions | Pregnancy Birth and Baby
Braxton Hicks contractions | Pregnancy Birth and Baby beginning of content4-minute read
Listen
If you feel tightening or cramping in your abdomen during your pregnancy, you may be having Braxton Hicks contractions. This is normal and not a sign that you’re ready to give birth.
Braxton Hicks contractions are sometimes called ‘false’ or ‘practice’ contractions.
What are Braxton Hicks contractions?
Braxton Hicks contractions are a tightening in your abdomen that comes and goes. They are contractions of your uterus in preparation for giving birth. They tone the muscles in your uterus and may also help prepare the cervix for birth.
Braxton Hicks contractions don’t cause labour and aren’t a sign that labour is beginning.
If you’re not sure whether what you’re experiencing is Braxton Hicks contractions or actual labour, contact your doctor or midwife. They will be able to tell by doing a vaginal examination — if there are no signs that your cervix is changing, it is not labour.
What do they feel like?
Braxton Hicks contractions feel like muscles tightening across your belly, and if you put your hands on your belly when the contractions happen, you can probably feel your uterus becoming hard.
The contractions come irregularly and usually last for about 30 seconds. While they can be uncomfortable, they usually aren’t painful.
If the pain or discomfort of your contractions eases off, they’re probably Braxton Hicks contractions.
When do you get them?
Braxton Hicks contractions occur from early in your pregnancy but you may not feel them until the second trimester. If this is your first pregnancy, you might start to feel them from about 16 weeks. In later pregnancies, you may feel Braxton Hicks contractions more often, or earlier. Some women won’t feel them at all.
Some women won’t feel them at all.
In late pregnancy, you may experience Braxton Hicks contractions more often — perhaps as much as every 10 to 20 minutes. This is a sign that you are preparing for labour — known as prelabour.
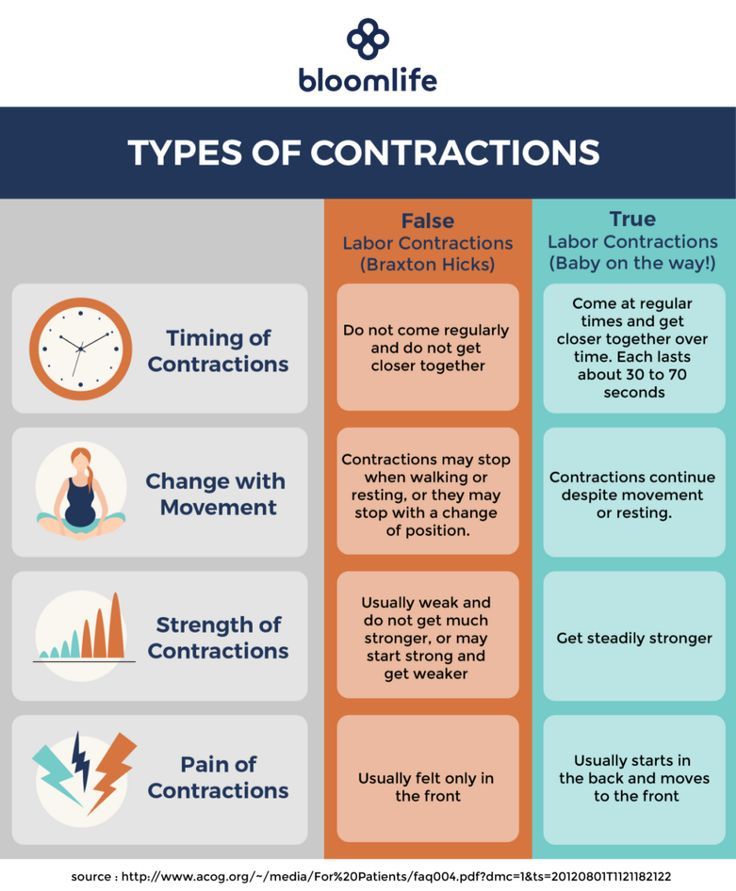
How are Braxton Hicks contractions different from labour pain?
There are some differences between Braxton Hicks contractions and true labour contractions that will help your doctor or midwife decide whether you are in labour:
Braxton Hicks contractions:
- don’t result in your cervix thinning and opening
- usually last for about 30 seconds
- can be uncomfortable, but usually aren’t painful
- come and go at irregular times
- usually occur no more than once or twice an hour (until late in the pregnancy), a few times a day
- usually stop if you change position or activity or go for a walk
- usually go if you have a warm bath or shower
Real labour contractions:
- result in your cervix thinning and opening
- last 30 to 70 seconds
- become very regular
- get closer together
- last longer as time goes by
- get stronger or come more often when you walk
- get stronger over time
Should I call my doctor or midwife?
If you are less than 37 weeks pregnant, contractions can be a sign of premature labour. Contact your doctor or midwife immediately if:
Contact your doctor or midwife immediately if:
- you feel pain, pressure or discomfort in your pelvis, abdomen or lower back
- the contractions become stronger, closer together and more regular
- there is fluid leaking or gushing from your vagina
If you are full-term, you may choose to wait until a bit later in your labour, depending on what you have arranged with your doctor or midwife. If your waters break, or your contractions are strong and 5 minutes apart, it’s time to go to the hospital.
As any stage of pregnancy, you should contact your doctor or midwife immediately if you:
- you have persistent pain in your abdomen
- you have vaginal bleeding
- you notice your baby’s movements have slowed or stopped
- you feel very unwell
If you are in doubt, don’t hesitate to call your doctor or midwife for advice.
How can I ease the discomfort?
Braxton Hicks contractions are normal and don’t need treatment. But if you feel uncomfortable, you can try:
But if you feel uncomfortable, you can try:
- lying down
- taking a walk
- relaxing in a warm bath
- having a massage
It may help to practise your breathing exercises during your Braxton Hicks contractions.
Sources:
Raising Children Network (23 weeks pregnant), RANZCOG (Labour and birth), Elsevier Patient Education (Braxton Hicks Contractions)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Giving birth - stages of labour
- Health professionals involved in your pregnancy
- Signs of premature labour
Need more information?
Pregnancy at week 22
By week 22, some parts of your baby’s body are fully formed, while some women experience Braxton Hicks contractions about now.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 35
You'll probably be having lots of Braxton Hicks contractions by now. It's your body's way of preparing for the birth. They should stop if you move position.
Read more on Pregnancy, Birth & Baby website
Giving birth - contractions
Contractions are when the muscles in your uterus tighten and then relax. They occur throughout the later stages of your pregnancy.
Read more on Pregnancy, Birth & Baby website
What happens to your body in childbirth
During childbirth, the body’s hormones and muscles, as well as the shape of the pelvis, all work together to bring the baby safely into the world.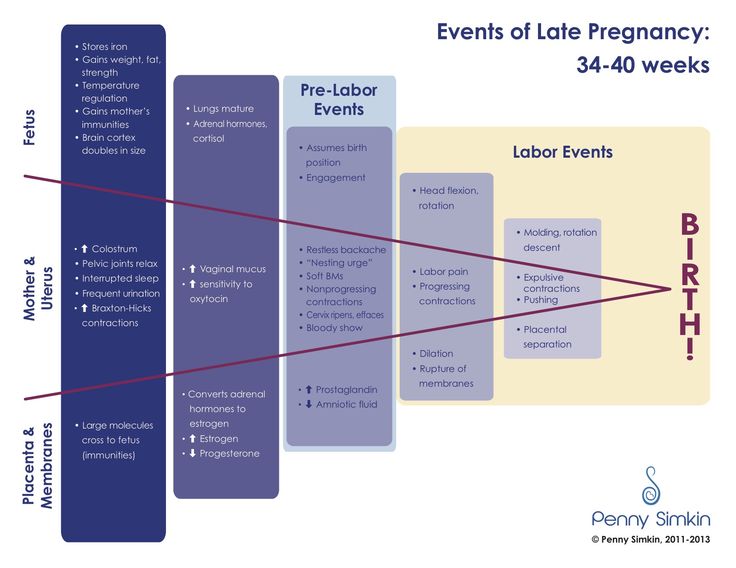
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth - uterus
The uterus is your growing baby’s home during pregnancy. Learn how the uterus works, nurtures your baby and how it changes while you are pregnant.
Read more on Pregnancy, Birth & Baby website
Preterm labour - MyDr.com.au
Going into labour before your 37th week of pregnancy is called preterm labour, or premature labour. Find out what it means for you and your baby.
Read more on myDr website
38 weeks pregnant | Raising Children Network
38 weeks pregnant? In this pregnancy week by week guide, find out how your baby is growing, how your body is changing and how to look after yourself.
Read more on raisingchildren.net.au website
26 weeks pregnant | Raising Children Network
26 weeks pregnant? In this pregnancy week by week guide, find out how your baby is growing, how your body is changing and how to look after yourself.
Read more on raisingchildren.net.au website
Giving birth - early signs of labour
You can know the early signs of labour, even if you cannot predict when your labour will begin. Find out also what to do if something appears to be wrong.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth
From conception to giving birth, a woman's body goes through many physical changes. Learn what happens to your body during pregnancy and labour.
Learn what happens to your body during pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Frequent Braxton-Hicks: Causes, Risks, and Treatment
Frequent Braxton-Hicks: Causes, Risks, and TreatmentMedically reviewed by Carolyn Kay, M.D. — By Madison Manske on July 30, 2020
As you begin mentally preparing for labor and delivery, your body may do some preparation drills. One such physical preparation can be the onset of Braxton-Hicks contractions.
Braxton-Hicks are non-labor (or “false labor”) contractions that occur regularly during your pregnancy as your body begins to prepare itself for the real thing. The frequency of these contractions can vary based on factors like your activity and hydration levels.
Regardless of the frequency, Braxton-Hicks contractions are quite normal and can really help you know more about what to expect as you count down to the big day.
Braxton-Hicks contractions are common during the second and third trimesters of pregnancy. Unlike real labor contractions, the cervix doesn’t dilate during Braxton-Hicks contractions. These contractions also tend to be pretty painless.
Braxton-Hicks occur when the uterus muscles tighten and loosen, and they may increase as you approach your due date. They generally come at random times throughout the day and may stop with certain movements or body positions.
You may experience more frequent Braxton-Hicks contractions if you’re:
- on your feet a lot
- dehydrated
- overhydrated
- experiencing stress
- close to your due date
Regardless of the cause, frequent Braxton-Hicks aren’t cause for concern. But if they don’t ease up, you may want to check in with your doctor in case you might be in labor.
But if they don’t ease up, you may want to check in with your doctor in case you might be in labor.
Related: Learn how to tell Braxton-Hicks from labor contractions
It’s important to know the difference between frequent Braxton-Hicks and the frequent and painful contractions associated with uterine irritability.
Uterine irritability refers to a disorganized pattern of activity in the uterus that’s sometimes observed during external fetal monitoring, although it’s not necessarily a diagnosis.
It can result in contractions similar to those experienced with Braxton-Hicks in that the cervix doesn’t dilate as it does during real labor contractions.
Contractions associated with uterine irritability don’t respond to hydration or rest and may feel more like menstrual cramps. They’re also stronger and occur more frequently than Braxton-Hicks contractions. While they may be annoying, they’re mostly harmless and should go away.
However, some underlying causes need treatment.
Possible causes of uterine irritability
Uterine irritability may affect women differently, and the exact cause isn’t clear. Some things may increase its related contractions, such as:
- stress
- dehydration
- an untreated infection
- a urinary tract infection
- lifting heavy things
Talk to your doctor if you think you may have uterine irritability. In most cases, contractions will go away on their own and pose no risk to the mom or baby.
Talk to your doctor if you’re worried about frequent Braxton-Hicks. You may want to record the frequency and pain level of your contractions for your doctor. They’ll use this information to determine treatment, if necessary.
Call your doctor if you experience more than eight contractions in 1 hour or have:
- decreased movement in the stomach
- leaking amniotic fluid
- vaginal bleeding
- painful contractions every 10 minutes or less
Your doctor may recommend that you try some of these things at home to help treat false labor contractions:
- get plenty of rest
- drink water and stay hydrated
- avoid caffeine
- keep an empty bladder
- avoid lifting heavy things
- eat smaller portions more frequently
- reduce your stress and anxiety levels (try these tips)
Braxton-Hicks contractions are a very normal part of pregnancy. They can occur more frequently if you experience stress or dehydration.
They can occur more frequently if you experience stress or dehydration.
If at any point you’re worried that your false labor contractions are real, consult your doctor. They’ll be more than happy to check and see how things are moving along.
Last medically reviewed on July 30, 2020
- Parenthood
- Pregnancy
- 3rd Trimester
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Labor and birth. (2018).
womenshealth.gov/pregnancy/childbirth-and-beyond/labor-and-birth - Other labor and delivery FAQs. (2017).
nichd.nih.gov/health/topics/labor-delivery/topicinfo/more_information/questions - Preterm birth.
 (2019).
(2019).
cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm - Raines DA, et al. (2020). Braxton Hicks contractions.
ncbi.nlm.nih.gov/books/NBK470546/#
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Carolyn Kay, M.D. — By Madison Manske on July 30, 2020
related stories
What Do Braxton-Hicks Feel Like?
How to Predict When Your Baby Will Drop
Braxton-Hicks Contractions vs. Real Contractions
Have a Question About Labor and Delivery?
What to Expect During a Vaginal Delivery
Read this next
What Do Braxton-Hicks Feel Like?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Are those contractions you are feeling? Braxton-Hicks or “false labor” contractions can be exciting — or alarming.
 It helps to know what can cause…
It helps to know what can cause…READ MORE
How to Predict When Your Baby Will Drop
Medically reviewed by Debra Rose Wilson, Ph.D., MSN, R.N., IBCLC, AHN-BC, CHT
Your baby dropping is one of the first signs that your body is getting ready for labor. A registered nurse and mother of four tells you what you need…
READ MORE
Braxton-Hicks Contractions vs. Real Contractions
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Braxton-Hicks contractions can be confused with real contractions. Learn how to determine which you’re having.
READ MORE
Have a Question About Labor and Delivery?
Medically reviewed by Janine Kelbach, RNC-OB
Get answers to common questions such as, who can be in the delivery room with you, the average length of delivery, and assisted birth methods.
READ MORE
What to Expect During a Vaginal Delivery
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Every delivery is as unique and individual as each mother and infant. Each woman may have a completely new experience with each labor and delivery. Of…
READ MORE
Is It Safe to Consume Flaxseeds During Pregnancy?
Given the inconclusive and conflicting stances about eating flaxseeds during pregnancy, it might be better to err on the side of caution.
READ MORE
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt. Learn more about pregnancy after…
READ MORE
What Is a Nurse Midwife and How to Tell If They Are Right for You
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
A nurse midwife is a nurse with education, training, and certification to provide prenatal, delivery, and women's care.

READ MORE
Your 6-Week Ultrasound: What to Expect
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
We'll tell you all about the 6-week ultrasound, including why your doctor may have ordered it, what the risks are, and what it means if no heartbeat…
READ MORE
Does Swaddling Increase the Risk of SIDS?
Medically reviewed by Mia Armstrong, MD
Is swaddling safe, or is it a risk factor for SIDS? Here's what the most recent research says.
READ MORE
Braxton-Hicks contractions or false labor contractions are irregular contractions and relaxation of the muscles of the uterus as a way of preparing for true labor. They are thought to start around 6 weeks of gestation but are not usually felt until the 2nd or 3rd trimester.
False contractions are a normal part of pregnancy. They may be uncomfortable, but not painful. Women describe them as a feeling that feels like mild menstrual cramps or tightness in a specific area of the abdomen that quickly resolves.
They are also irregular in duration and intensity, occur infrequently, are unpredictable and not rhythmic, and are more uncomfortable than painful.
Braxton Hicks contractions tend to increase in frequency and intensity towards the end of pregnancy. Women often mistake Braxton Hicks contractions for real labor. However, unlike real contractions, they do not dilate the cervix and result in the birth of a baby.
Braxton Hicks contractions occur when the muscle fibers of the uterus contract and relax. The exact etiology of Braxton Hicks contractions is unknown. However, there are circumstances that can cause them:
- when the woman is very active,
- when the bladder is full,
- after sexual activity,
- when the woman is dehydrated.

Common among all these circumstances is the potential stress on the fetus and the need for increased blood flow to the placenta to provide oxygen to the fetus.
- Change position or activity level: if you were very active, lie down; if you have been sitting for a long time, go for a walk.
- Relax: take a warm bath, massage, read a book, listen to music or take a nap.
If you have Braxton Hicks contractions or if they continue and become more frequent and intense, you should see your doctor.
When assessing for Braxton Hicks contractions, there are a few key questions to ask yourself. We have prepared a table for you with questions, the answers to which will help you understand what kind of contractions you have:
| Braxton Higgs contractions | Real labor pains | |
|---|---|---|
| How often do contractions occur? | Irregular and do not increase over time. | Occurs at regular intervals and gets stronger over time. |
| How long do contractions last? | Unpredictable. They can last less than 30 seconds or up to 2 minutes. | Lasts 30 to 90 seconds and gets longer over time. |
| How strong are the contractions? | Usually weak and either stay the same or get weaker and then disappear. | Increase over time. |
| Where do contractions feel? | Often only felt in the front of the abdomen or in one specific area. | Begin in the middle of the back and wrap around the belly towards the midline. |
| Do abbreviations change with movement? | May stop if activity level changes or if woman's position changes. | Continue and may even get worse with movement or change of position. |
Back to the list of articles
False contractions - causes, symptoms, diagnosis and treatment
False contractions are irregular uterine contractions that cause pain, but there is no cervical dilatation. Occur in late pregnancy, more often after the 20th week. The main manifestations: cramping pains in the lower abdomen or in the lumbar region without a clear periodicity. Methods for diagnosing this condition are cardiotocography, examination of the cervix in mirrors with the determination of its degree of maturity, ultrasound of the genitals with an assessment of uterine blood flow. Specific treatment depends on the duration of pregnancy and the causes of this condition.
Occur in late pregnancy, more often after the 20th week. The main manifestations: cramping pains in the lower abdomen or in the lumbar region without a clear periodicity. Methods for diagnosing this condition are cardiotocography, examination of the cervix in mirrors with the determination of its degree of maturity, ultrasound of the genitals with an assessment of uterine blood flow. Specific treatment depends on the duration of pregnancy and the causes of this condition.
General information
False contractions are also called “training contractions” or “Braxton-Hicks contractions” after the English doctor who first described this phenomenon. Back in 1872, he noted that many women feel such contractions long before the expected birth. This caused fear and confusion among women in connection with the timing of real childbirth, so J. Braxton Hicks began to warn pregnant women in advance about the possibility of such a phenomenon. False contractions normally occur in 33% of pregnant women. Multiparous women feel false contractions at an earlier date compared to primiparas.
Multiparous women feel false contractions at an earlier date compared to primiparas.
False contractions
Causes
The contractile activity of the uterus depends on the work of the pituitary gland. In the later stages (from 37 weeks), the preparation of the body for future childbirth gradually begins, hormones that have contractile ability (oxytocin, cortisone-like substances) are released. Under their influence, contractions periodically occur in the myometrium. At early gestation, the causes of false contractions can be:
- Pathology of the pituitary and endocrine glands. Increased levels of thyroid, adrenal, and posterior pituitary hormones in the blood can increase the readiness of muscle cells to contract. An increase in the level of prolactin provokes excessive formation of male steroid hormones in the female body, which can also lead to false contractions.
- Uterine hypertonicity. The increased readiness of the myometrium to contract prematurely can be caused by various factors.
 Both hormonal causes (reduced progesterone levels) and changes in the fetal-uterine blood flow (like hypoxia of the uterine muscles) play a role here.
Both hormonal causes (reduced progesterone levels) and changes in the fetal-uterine blood flow (like hypoxia of the uterine muscles) play a role here. - Underdevelopment of the neuro-receptor apparatus of the uterus. The ratio of the number of estrogen and progesterone receptors is not constant and normally changes at different stages of pregnancy. A pathological increase in the number of estrogen receptors contributes to the occurrence of premature uterine contractions.
Patients with preeclampsia, congenital anomalies of the reproductive apparatus and immune diseases are at risk for the occurrence of false contractions in early pregnancy. The development of false contractions is facilitated by overstretching of the uterus during multiple pregnancy or the presence of a postoperative scar. Very often, pathological contractile activity of the muscular layer of the uterus is observed with intrauterine infection and isthmic-cervical insufficiency.
Pathogenesis
In the last month of pregnancy, the contractile activity of the myometrium increases. The synthesis of biologically active substances and hormones that stimulate the tension of muscle fibers increases. The number of excitatory uterine contractions of nerve impulses increases. In the brain, a focus coordinating labor activity is formed - the “dominant of childbirth”.
Periodically occurring during this period, false contractions help maintain normal uterine tone and stimulate fetoplacental blood flow. The vessels of the placenta do not have their own muscle layer, periodic uterine contractions displace venous blood from them, which is replaced by arterial blood. Thus, the fetus receives more oxygen and nutrients.
False contractions
Symptoms of false contractions
False contractions are felt by a pregnant woman as an irregular tension in the lower abdomen. The sensations may resemble discomfort during menstruation. Pains of a pulling, aching nature can spread to the lumbar region, sometimes they are accompanied by a feeling of fullness in the genital area. The abdomen during the period of the fight becomes dense, rounded, "hardens". With a high pain threshold, Braxton-Hicks contractions may not be felt at all and may be detected by chance, for example, during a doctor's appointment.
Pains of a pulling, aching nature can spread to the lumbar region, sometimes they are accompanied by a feeling of fullness in the genital area. The abdomen during the period of the fight becomes dense, rounded, "hardens". With a high pain threshold, Braxton-Hicks contractions may not be felt at all and may be detected by chance, for example, during a doctor's appointment.
False contractions begin and end suddenly, they have no clear rhythm. Attacks often develop at night, when the pituitary gland increases the production of oxytocin. They are distinguished from true contractions by the fact that the force of contractions does not increase over time, and the intervals between contractions do not decrease. False contractions disappear with a change in position or cessation of physical activity. They may appear and end several times a day.
Diagnosis
The presence of Braxton-Hicks training contractions can be suspected already on the basis of the patient's complaints. During the examination, the tone of the uterus is assessed, which often tenses in response to palpation. Be sure to conduct an examination in the mirrors to determine the degree of maturity of the cervix and its length. If it is shorter than 25 mm, then this is considered a risk of preterm labor and requires appropriate therapy (installation of a pessary, circling).
During the examination, the tone of the uterus is assessed, which often tenses in response to palpation. Be sure to conduct an examination in the mirrors to determine the degree of maturity of the cervix and its length. If it is shorter than 25 mm, then this is considered a risk of preterm labor and requires appropriate therapy (installation of a pessary, circling).
A swab for flora is taken from the pregnant woman's genital tract, a nitrazine test is performed to rule out spotting, infection or amniotic fluid leakage. To assess the general condition of the expectant mother, laboratory tests are carried out, such as a general analysis of urine and blood, a biochemical study, an assessment of the excretory function of the kidneys (Zimnitsky's test). The patient consults a general practitioner, if necessary, a nephrologist and endocrinologist.
Methods for assessing the condition of the uterus and fetus are used as special studies. It is very important to examine the placenta for functional consistency, location and intensity of blood flow. To do this, it is carried out:
To do this, it is carried out:
- Cardiotocography. Simultaneously allows you to track the contractile activity of the uterus, the presence of contractions and the state of the heart activity of the fetus. Based on the results, it can be decided whether the fetus suffers from a lack of oxygen during contractions.
- Ultrasound of the fetal and uterine blood flow. During the study, anomalies of the vascular bed of the placenta, uterus, fetus are revealed. Sometimes there is a premature "aging" of the placenta, because of this, the level of blood circulation decreases, hypoxic conditions may develop in the fetus or in the myometrium, which cause abnormal contractions.
Cardiotocography
Treatment of false contractions
Treatment tactics are selected depending on the gestational age at which false contractions occurred. Starting from 37 weeks of gestation, with normal tests, the treatment of false contractions is not carried out. From 22 to 37 weeks, therapy is primarily aimed at eliminating the cause that caused uterine contractions. With endocrine pathology, hormonal correction is prescribed, maintaining an adequate level of progesterone, as the main prolonging pregnancy hormone.
From 22 to 37 weeks, therapy is primarily aimed at eliminating the cause that caused uterine contractions. With endocrine pathology, hormonal correction is prescribed, maintaining an adequate level of progesterone, as the main prolonging pregnancy hormone.
Tocolytic (relaxing myometrium) therapy is used for increased uterine propensity to contract. A proven remedy is magnesium sulfate (magnesia). When administered intravenously and intramuscularly, it has an anticonvulsant effect. In addition, the drug prevents fluid retention in the body of a pregnant woman and activates the fetal-uterine blood flow. Sometimes the introduction of a drug is used as a diagnostic test: false contractions stop at the same time, but it does not affect true contractions.
Selective beta-agonists (hexoprenaline), inhibitors of prostaglandin synthesis (indomethacin) and antispasmodics (drotaverine) are also used from tocolytics according to indications. For the prevention of intrauterine fetal hypoxia and circulatory disorders in the uterus and placenta, cytoprotectors and antiplatelet agents (pentoxifylline) are prescribed..jpg)