Causes of baby death after delivery
What is a neonatal death?
What is a neonatal death? | Pregnancy Birth and Baby beginning of content4-minute read
Listen
A neonatal death is when a baby dies within the first 4 weeks after they are born. Dealing with a neonatal death can be very difficult for the whole family, but there is help and support available.
What is a neonatal death?
A neonatal death (also called a newborn death) is when a baby dies during the first 28 days of life. Most neonatal deaths happen in the first week after birth.
Neonatal death is different from stillbirth. A stillbirth is when the baby dies at any time between 20 weeks of pregnancy and the due date of birth.
Globally around 2.4 million children die in the first 28 days after birth. This is around half of all child deaths under the age of 5.
Neonatal death is rare in Australia, and rates are falling — there are about 700 neonatal deaths a year in Australia.
What are the causes of a neonatal death?
It’s not always known why a baby dies. However, the risk of neonatal death may be greater if a baby is born prematurely, is low birthweight, or has birth defects.
Prematurity and low birthweight cause about 1 in 4 neonatal deaths. Premature babies can develop life-threatening complications such as breathing problems, bleeding on the brain, infections and problems in their intestines (necrotising enterocolitis).
Low birthweight — if the baby weighs less than 2.5kg at birth — can also cause serious health problems such as difficulty breathing and feeding.
The most common birth defects that cause neonatal death include heart defects, lung defects, genetic conditions and brain conditions such as neural tube defect or anencephaly.
Sometimes a neonatal death may be caused by problems during the pregnancy, such as pre-eclampsia, problems with the placenta, or infections.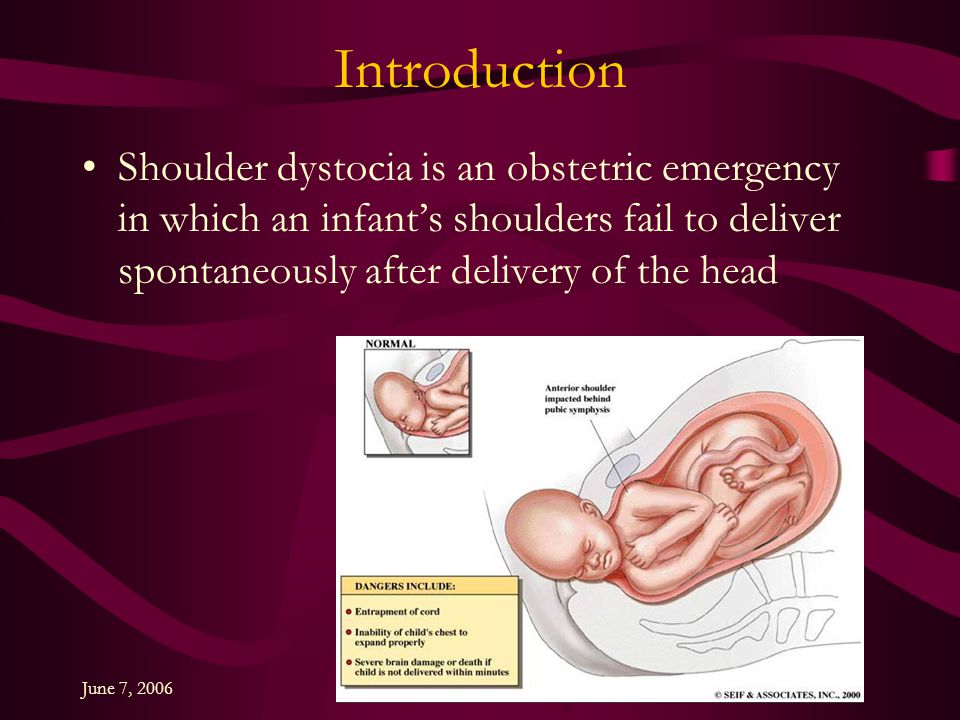 It can also be caused by complications during the labour — for example, if the baby didn’t get enough oxygen.
It can also be caused by complications during the labour — for example, if the baby didn’t get enough oxygen.
What happens after a neonatal death?
If your baby dies, you might want to spend some time with them. You should take as long as you like. Some parents create memories of the baby by taking photos, handprints and footprints.
When you are ready to say goodbye, the hospital or a funeral director will take your baby to a funeral home. There will then be a burial or cremation.
By law, you must register both the birth and the death with Births, Deaths and Marriages in your state or territory.
In Australia, not all neonatal deaths are investigated by conducting an autopsy, also known as a post mortem examination. An autopsy is an examination to try to work out why the baby has died.
An autopsy cannot be done without the parents’ consent and it is up to you whether to agree to an autopsy after a neonatal death. The only time when an autopsy may be carried out without consent is if the case is referred to a coroner. This might happen if the death occurred in suspicious circumstances or if it was something to do with the health care the baby received.
This might happen if the death occurred in suspicious circumstances or if it was something to do with the health care the baby received.
An autopsy is done by a trained pathologist. If you agree to an autopsy, you can decide how detailed you would like it to be — whether it involves just examining the baby or removing organs to test why the death has happened.
Sometimes no cause of death can be found, even after an autopsy. It’s a good idea to discuss the benefits and downsides of an autopsy with a doctor, midwife or social worker. They will guide you through what needs to be done and will answer any questions you might have.
Learn more here about what happens after a neonatal death and what changes might occur to your body.
Where to find help
The death of a newborn baby can be devastating, both for the parents and for the whole family. So it’s important to get as much support as possible to help you through this difficult time.
Your doctor, midwife, maternal child health nurse or social worker will be able to guide you through what happens after the baby has died.
Sands Australia provides information and support for anyone who has experienced stillbirth or newborn death. You can speak to someone 24 hours a day on their helpline, 1300 072 637.
Red Nose Grief and Loss has information and resources. You can call their helpline 24 hours a day on 1300 308 307.
Lifeline supports anyone having a personal crisis — call 13 11 14 or chat online.
You can call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse.
Sources:
World Health Organization (Newborn deaths and illnesses), Raising Children Network (Neonatal death - a guide), March of Dimes (Neonatal death), The Royal Women’s Hospital Melbourne (Learning why a baby has died), Queensland Courts (Reportable deaths), Australian Institute of Health and Welfare (Stillbirth and neonatal deaths in Australia), Sands (Stillborn and newborn death), myDr (Low-birth-weight babies)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2021
Back To Top
Related pages
- Your body after stillbirth or neonatal death
- Dealing with a neonatal death
- Birth trauma (emotional)
Need more information?
Baby and Infant Death
Baby and Infant Death A neonatal death is when a baby is born alive but dies within the first 28 days of life
Read more on Gidget Foundation Australia website
Death of a baby - Better Health Channel
Miscarriage, stillbirth or neonatal death is a shattering event for those expecting a baby, and for their families. Grief, relationship stresses and anxiety about subsequent pregnancies are common in these circumstances.
Read more on Better Health Channel website
When Your Baby is Stillborn or Dies Soon After Birth | Guiding Light - Red Nose Grief and Loss
Read more on Red Nose website
Breast care for breastfeeding mothers after the death of a child | Sydney Children's Hospitals Network
Time after the death of your infant can be physically and emotionally exhausting
Read more on Sydney Children's Hospitals Network website
Smoking | Red Nose Australia
Read more on Red Nose website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Why babies die? | Sands
Why are the figures Sands uses for baby deaths from 2020, and not more recent?
There are two main sources of figures for baby deaths for the whole UK. For both, the process to make sure the data is complete and accurate is complex and takes time. This leads to a lag between the end of the year and the release of the figures for that year.
The figures for baby deaths need to be compared with the numbers of live births to understand the rate of deaths, not just the total number of deaths. This ‘validation’ of the figures adds to the time it takes to prepare the data.
The most recent data available for the UK is for 2020. Figures for UK baby deaths in 2021 will be published in late 2022.
We need timely statistics. Can anything be done to speed this up?
Sands has fed back the importance of timely data to both bodies who produce national data . They have listened to the feedback and both are working hard to further minimise the lag.
Who collects the data?
There are two main sources of statistics for baby deaths:
- Deaths notified to the national register for births and deaths, and the stillbirth register (this is when parents register their baby’s birth and death, or stillbirth). This data is collected in each UK country and collated by the Office for National Statistics (ONS)
- Deaths notified by the hospital to the national audit programme which collects data for the whole UK on baby deaths from 22 weeks gestation to 4 weeks of life – the programme is run by MBRRACE-UK
When are the figures published?
The registration data has less detail than the hospital data and is published sooner.
For deaths in a calendar year:
- ONS publishes figures at the end of the following year
- MBRRACE-UK publishes data in the autumn of the second year
What is the difference between ONS and MBRRACE-UK data?
- ONS
ONS collates registration data from each of the four UK countries. This includes basic information about the baby (such as gender and date of birth/death/stillbirth) and the parent/s (such as names and age), and a cause of death.
The most recent ONS UK data set is for 2020.
We use ONS figures to monitor trends in mortality, year on year, and to hold governments to a account for progress against targets to cut rates of baby deaths
- MBRRACE-UK
When a baby dies between 22 weeks gestation and 4 weeks of life, the hospital staff complete an MBRRACE-UK notification form which includes more detail about the baby and mother’s health, the care, and cause of death.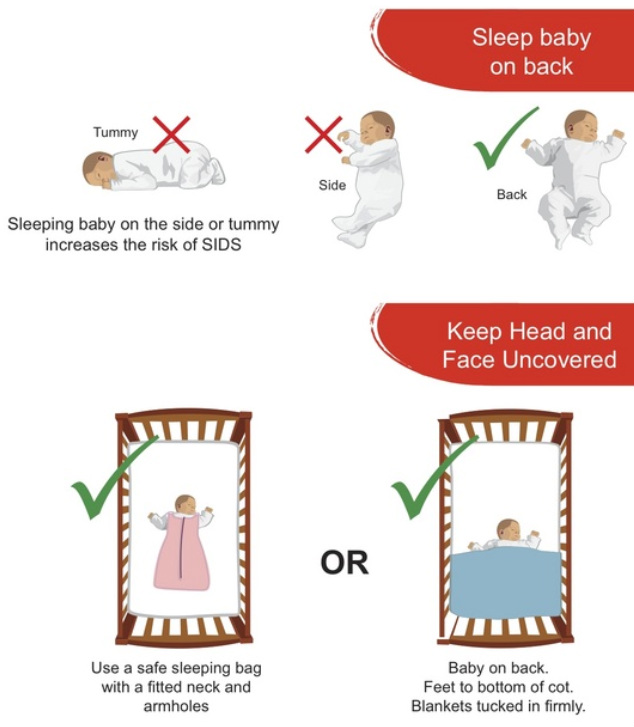
MBRRACE-UK publishes the data in an annual report (called the perinatal surveillance report). It includes a summary infographic and Trust/Health Board-level outcomes.
The most recent data and report, published in October 2021, looked at deaths in 2019.
We use MBRRACE-UK data to understand more about factors affecting baby deaths, for example the impact of ethnicity and social deprivation. We can look at trends in outcomes at Trust/Health Board level. The data helps identify where we should be focusing our energies in preventing deaths
What about statistics for each country in the UK?
MBRRACE-UK collects hospital data on baby deaths on behalf of all 4 UK countries, and reports for the UK in the annual reports.
Registration data is gathered separately in each UK country. The countries publish their own data on slightly different timetables. ONS then pulls the figures together for the whole UK.
Scotland:
National Records for Scotland report annual stillbirth and neonatal deaths during the following year. The latest figures are for 2020.
The latest figures are for 2020.
For Northern Ireland
The Northern Ireland Statistics Research Agency collects the registration data. It’s published annually in the Register General’s report, in the following year
The most recent report is on 2020 deaths.
Wales
Registration data for Wales is reported by ONS, alongside figures for England (see below).
England
ONS publish stillbirth figures for England and Wales in the following year. During the pandemic, ONS has reported provisional stillbirth figures sooner than the confirmed figures, to help understand the impact of COVID 19 in pregnancy
ONS reports neonatal deaths for England and Wales lightly later than stillbirths. This is because it takes longer to ensure the deaths data is complete.
There are different datasets available on the ONS website, reporting different aspects.
How does Sands use statistics about baby deaths?
We work to hold UK governments to account on their and our targets to cut baby deaths, and push for changes that will make maternity and neonatal care safer.
We work strategically with national bodies, for example the Maternity Consortium, and parliamentary groups such as the Health Select Committee and the All Party Parliamentary Group on Baby Loss, raising the issue of safety and inequalities in outcomes.
Sands action has led to a confidential enquiry into Asian baby deaths, to run along an MBRRACE-UK enquiry into Black baby deaths. To enhance the enquiries with the perspective of Black and Asian parents’ experiences, we will be canvassing bereaved families to hear and share their views.
Independent examination of neonatal death. Price. Examples.
Examination of the causes of death of newborns is a post-mortem examination of the corpse of a newborn child. The basis for the appointment of such an examination is the traces of violent actions on the body of the child or the suspicion that such actions were committed. The death of a newborn may occur as a result of intentional actions of the mother or another person, as a result of accidental injuries during childbirth, especially independent, outside the walls of a specialized medical institution. Also, death can be caused by congenital diseases or injuries received during the passage of the child through the birth canal. The most dangerous injuries include craniocerebral injuries during rapid delivery or head presentation of the fetus. The lethal outcome, in addition, is due to intrauterine asphyxia, which is the result of premature detachment of the placenta or tight entanglement of the neck with the umbilical cord. Establishing the true cause of death and the mechanism of its occurrence is the main task of a forensic medical examination, in which a complete examination of the corpse of a newborn is performed, including external examination, autopsy, special analyzes, and so on.
Also, death can be caused by congenital diseases or injuries received during the passage of the child through the birth canal. The most dangerous injuries include craniocerebral injuries during rapid delivery or head presentation of the fetus. The lethal outcome, in addition, is due to intrauterine asphyxia, which is the result of premature detachment of the placenta or tight entanglement of the neck with the umbilical cord. Establishing the true cause of death and the mechanism of its occurrence is the main task of a forensic medical examination, in which a complete examination of the corpse of a newborn is performed, including external examination, autopsy, special analyzes, and so on.
In forensic practice, active and passive infanticide are distinguished. With active infanticide, actions are performed aimed at the rapid termination of the vital functions of a newborn - strangulation by hand or with the help of improvised means, closing the openings of the nose and mouth, mechanical compression of the abdomen and chest, inflicting injury with a blunt object or cutting and piercing weapon, drowning. Leaving a child without care and necessary assistance is considered passive infanticide. In this case, death occurs most often from hypothermia or bleeding from the vessels of an unligated umbilical cord, less often due to hunger, a sudden cessation of the functioning of the respiratory or cardiovascular system. Signs of a neglected newborn include blood and cheese on the newborn's body and no food in the stomach.
Leaving a child without care and necessary assistance is considered passive infanticide. In this case, death occurs most often from hypothermia or bleeding from the vessels of an unligated umbilical cord, less often due to hunger, a sudden cessation of the functioning of the respiratory or cardiovascular system. Signs of a neglected newborn include blood and cheese on the newborn's body and no food in the stomach.
Peculiarities of examination of the causes of death of newborns
Distinctive features of the examination of the causes of death of newborns are caused by a number of goals and objectives that cannot be set in principle during the examination of the corpse of an adult. These research issues include:
- Determining whether a deceased child is a newborn.
- Whether this child was mature and full-term during life.
- Whether the deceased child was viable, that is, whether any congenital diseases or birth injuries incompatible with life are found in him.

- Was this child born alive or dead? Did death occur after he was removed from the womb?
- What is the intrauterine life expectancy of this child?
- How long after birth was the baby alive?
These tasks, due to their exclusivity, require the use of special research methods. An unusual technique and research methodology is to conduct the following expert activities:
- Opening of the cranial cavity of a newborn corpse.
- Making a number of incisions in the area below the patella to identify the ossification nuclei.
- Gastrointestinal and pulmonary swimming test.
- Carrying out a number of anthropometric studies.
- Study and subsequent description of overlays on the surface of the skin.
- Examination of specific signs of the development of the genital organs.
- Additional examination of the umbilical cord, as well as the placenta (if they are submitted for examination).

Establishing the maturity, full term, newborn and viability of an infant in the process of performing an examination of the causes of death of newborns
In forensic practice, a newborn is an infant within the first twenty-four hours after the fact of birth. If it is necessary to make a decision on infanticide, the newborn baby is established on the basis of the following criteria:
- The presence of cheese-like grease on the body of an infant.
- The presence of blood on the body of an infant in the absence of visible injuries.
- Presence of a birth tumor.
- Detection of original feces (meconium).
- The umbilical cord is juicy, there are no signs of a demarcation ring in the area of rejection.
Maturity of an infant is understood as the level of fetal development at which extrauterine life is possible. An infant is considered mature if it exhibits the following characteristics:
- Weight exceeds 2500 grams.

- Skin elastic, pink. Developed subcutaneous fat layer.
- There are two to three centimeters long hair on the head.
- The cartilages of the nose and ears are elastic.
- The length of the umbilical cord is from forty-five to sixty centimeters.
- Nails are elastic. On the hands, the nails extend beyond the edge of the nail phalanx. On the legs - reach its edge.
- In boys, the testicles descend into the scrotum. In girls, the small labia are covered with large ones. In the lower epiphysis of the thigh, the ossification nucleus reaches sizes from five to seven millimeters.
A full-term infant is one born after forty to forty-two weeks of intrauterine development. Full-term babies have a height of forty-eight to fifty-two centimeters, chest circumference from thirty-two to thirty-four centimeters. Also, babies show all the necessary signs of maturity.
A viable infant is one who can continue extrauterine life. A viable child has no congenital malformations and birth injuries incompatible with life. Under the conditions of childbirth outside a medical facility, babies with a body length exceeding forty centimeters, a head circumference of at least twenty-eight centimeters, and a weight of more than one and a half kilograms are considered viable. For babies born in a maternity hospital, if medical care is available, viability is established at lower rates.
A viable child has no congenital malformations and birth injuries incompatible with life. Under the conditions of childbirth outside a medical facility, babies with a body length exceeding forty centimeters, a head circumference of at least twenty-eight centimeters, and a weight of more than one and a half kilograms are considered viable. For babies born in a maternity hospital, if medical care is available, viability is established at lower rates.
Determination of the fact of the birth of a live (dead) child during the examination of the causes of death of newborns
Determination of the fact that the baby was born alive is carried out by establishing the presence of air in the lungs, intestines and stomach. To detect air, a gastric or pulmonary swimming test is performed, which is widely used in forensic practice. Also, before the autopsy of the infant's corpse, an X-ray examination of the whole body and isolated lungs and gastrointestinal tract is performed. However, in some cases, these samples are unreliable, for example, air entering the gastrointestinal tract and lungs may be due to artificial respiration. In addition, with secondary atelectasis of the lungs, air, on the contrary, may be absent in a previously breathing child. As a result, to establish the birth of a live child, histological and spectral methods for examining the tissues of the lungs, umbilical cord and birth tumor are used.
In addition, with secondary atelectasis of the lungs, air, on the contrary, may be absent in a previously breathing child. As a result, to establish the birth of a live child, histological and spectral methods for examining the tissues of the lungs, umbilical cord and birth tumor are used.
Determination of intrauterine and extrauterine life expectancy of an infant when conducting an examination of the causes of death of newborns
Determining the duration of intrauterine life of a fetus is based on making correspondences with body length. With a body length of more than twenty-five centimeters, the duration of the intrauterine period is determined in months - by dividing the body length in centimeters by 5. If the body length does not reach twenty-five centimeters, then the square root is taken from the body length indicator to determine the number of months of intrauterine life.
When conducting an examination of the causes of death of newborns, there are a number of signs according to which the duration of the extrauterine life of a newborn baby is established. So, a demarcation inflammatory line appears on the umbilical cord, which after six hours after birth is weakly expressed, and a day later it is already very clearly visible. The umbilical cord dries up on the second or third day after childbirth, and disappears after five to seven days. A gastrointestinal test is also used to determine life expectancy after birth. For its implementation, the stomach is bandaged on both sides, and the intestines - in several places. Further, according to the degree of air movement in the gastrointestinal tract, the approximate life expectancy is calculated. The presence of air only in the stomach indicates that the child lived only a few minutes after birth. The air in the small and large intestine speaks of several hours of life. Another indicator used in this case is the content in the intestines of the child of the original feces - meconium, which is completely removed from the intestines by the end of the third day of the baby's life.
So, a demarcation inflammatory line appears on the umbilical cord, which after six hours after birth is weakly expressed, and a day later it is already very clearly visible. The umbilical cord dries up on the second or third day after childbirth, and disappears after five to seven days. A gastrointestinal test is also used to determine life expectancy after birth. For its implementation, the stomach is bandaged on both sides, and the intestines - in several places. Further, according to the degree of air movement in the gastrointestinal tract, the approximate life expectancy is calculated. The presence of air only in the stomach indicates that the child lived only a few minutes after birth. The air in the small and large intestine speaks of several hours of life. Another indicator used in this case is the content in the intestines of the child of the original feces - meconium, which is completely removed from the intestines by the end of the third day of the baby's life.
Legal basis for the examination of the causes of death of newborns
The Criminal Code of the Russian Federation distinguishes cases of murder by a mother of her child in a separate group of crimes. Accordingly, the measure of restraint in such cases is specifically stipulated in Article 106 of the Criminal Code of the Russian Federation. The punishment of a mother for killing her own child is more lenient and amounts to a restriction of liberty for a period of two to four years. Punishment may also be expressed in the form of forced labor for up to five years or in the form of imprisonment for the same period. The article stipulates that such a preventive measure is intended for mothers who killed their child directly during childbirth or immediately after their completion, as well as the murder of a newborn child by his own mother, who is in a state of mental disorder while maintaining sanity, or by a mother who is in conditions psychotraumatic circumstances.
Accordingly, the measure of restraint in such cases is specifically stipulated in Article 106 of the Criminal Code of the Russian Federation. The punishment of a mother for killing her own child is more lenient and amounts to a restriction of liberty for a period of two to four years. Punishment may also be expressed in the form of forced labor for up to five years or in the form of imprisonment for the same period. The article stipulates that such a preventive measure is intended for mothers who killed their child directly during childbirth or immediately after their completion, as well as the murder of a newborn child by his own mother, who is in a state of mental disorder while maintaining sanity, or by a mother who is in conditions psychotraumatic circumstances.
This is due to the fact that the complex hormonal and physiological processes occurring in the mother's body during childbirth and on the first day after its completion, aggravated by the lack of someone's help, can lead to unexpected, unpredictable actions on the part of the mother, especially if she is in a stressful situation.
Questions to be put before a specialist conducting an examination of the causes of death of newborns
In each specific case of an examination of the causes of death of newborns, the number and composition of questions addressed to an expert may vary depending on the goals and objectives of the study. The above list of questions is general and subject to correction depending on the characteristics of the appointed expertise and the set of expert measures. In general, the specialist is asked the following questions:0003
- Was the deceased child a newborn?
- What is the sex of the newborn baby?
- What are the general physiological parameters of the infant?
- What evidence, found during examination of the child's body or during the production of an autopsy, testifies in favor of the fact that he was a newborn?
- Was there a child. Whose corpse is presented for examination, full-term?
- What are the indicators of the maturity of an infant?
- Was this infant viable?
- Does the infant have a birth injury, congenital disease, or malformation?
- Was this baby born alive?
- How long is the prenatal period for this baby?
- How long did the child live after birth?
- Was the baby cared for after birth?
- Are there injuries, injuries or other signs of external influence on the baby's body?
- Are these injuries life-threatening?
- What is the mechanism of this damage?
- Is there air in the infant's lungs and gastrointestinal tract?
- Has meconium been found in the infant's intestines?
- Was a cheese-like lubricant found on the body of a newborn baby?
- Were there traces of the mother's blood on the child's body?
- Are there signs of a demarcation ring on the umbilical cord?
- What is the cause of death of a newborn baby?
Expertise in a criminal case
According to the Decision of the Plenum of the Supreme Court of the Russian Federation of December 21, 2010 N 28 "On judicial expertise in criminal cases" expertise in a criminal case can be carried out either by the state an expert institution, or a non-profit organization established in accordance with the Civil Code of the Russian Federation and the Federal Law "On non-profit organizations", carrying out forensic activities in accordance with the statutes adopted by them.
Commercial organizations and laboratories, individual entrepreneurs, educational institutions, as well as non-profit organizations for which expert activity is not statutory, do not have the right conduct a criminal investigation. Expertise prepared by these organizations within the framework of criminal process, may be recognized as inadmissible evidence, i.e. evidence obtained from violation of the requirements of the procedural law.
Inadmissible evidence may not be used in the process of proof, including examination or be announced at the court session, and are subject to exclusion from the materials of the criminal case.
Since ANO "Forensic Expert" is an autonomous non-profit organization , and conducting judicial expertise is its main statutory activity (see section "Documents organization"), then it has the right to conduct examinations, including in criminal cases.
Prevention of infant mortality - Khanty-Mansiysk regional hospital
Infant age - the period from birth to 1 year - is one of the most critical periods in a child's life. This period is associated with the child's adaptation to environmental conditions. Significant changes occur in the body, especially they relate to the respiratory and cardiovascular and nervous systems. At the same time, the regulatory functions of the endocrine and nervous systems are not yet mature enough and various external factors can have a significant impact on the child's body. That is why the largest number of child deaths are recorded in the first year of life. Infant mortality - the mortality of children under one year old, is the main component of child mortality. Identification of pathology and the appointment of timely treatment is the prerogative of neonatologists and pediatricians. But in recent years, according to statistics, deaths of children from non-medical causes, such as death from external factors, sudden infant death syndrome, death from suffocation and asphyxia, have become more frequent.
This period is associated with the child's adaptation to environmental conditions. Significant changes occur in the body, especially they relate to the respiratory and cardiovascular and nervous systems. At the same time, the regulatory functions of the endocrine and nervous systems are not yet mature enough and various external factors can have a significant impact on the child's body. That is why the largest number of child deaths are recorded in the first year of life. Infant mortality - the mortality of children under one year old, is the main component of child mortality. Identification of pathology and the appointment of timely treatment is the prerogative of neonatologists and pediatricians. But in recent years, according to statistics, deaths of children from non-medical causes, such as death from external factors, sudden infant death syndrome, death from suffocation and asphyxia, have become more frequent.
This leaflet will introduce you to simple but very effective measures to prevent infant death from sudden death syndrome and from external causes.
Sudden Infant Death Syndrome (SIDS) and death of children from external causes are the leading causes of death in children from 1 month to 1 year.
Sudden Infant Death Syndrome is not a disease or a painful condition. The fact that this happens without warning, without any prerequisites, makes sudden infant death syndrome a severe, unbearable ordeal for parents.
What causes sudden death syndrome?
Scientists have studied a large number of cases of sudden infant death syndrome over the past 40 years, but so far a clear answer to this question has not been found. Most experts believe that this syndrome affects children who have a number of vulnerabilities:
-
immaturity
-
abnormal heart function
-
respiratory system diseases
-
immaturity of the awakening system
-
low birth weight
as well as children who are exposed to certain external influences, such as sleeping on their stomach or on a soft bed, during a critical period of their development.
Factors that increase the risk of SIDS:
- Premature or very low birth weight (less than 1500g)
- Mother's age less than 20 years
- Having many children, especially if the children are close in age - the risk of SIDS increases with each new child you have.
- The risk of SIDS is higher in twins, even if they were born at term and were not small
- The risk of SIDS is increased in siblings (under 1 year of age) of a child who died of SIDS
- Children with life-threatening conditions such as respiratory arrest, sudden pallor or bluing with loss of muscle tone who require resuscitation
- Male child - male infants of all nationalities die from SIDS 30 to 50% more often than girls
How to prevent sudden infant death syndrome?
It is possible to significantly reduce the risk of SIDS by following simple guidelines developed by the world's pediatric communities. Following these simple rules of safe sleeping for an infant can significantly reduce not only the risk of SIDS, but also death from external causes, such as suffocation, blockage of the airways, and the baby's head getting stuck between different objects.
Following these simple rules of safe sleeping for an infant can significantly reduce not only the risk of SIDS, but also death from external causes, such as suffocation, blockage of the airways, and the baby's head getting stuck between different objects.
Rules to follow:
1. Put your baby to sleep on their back! If your baby is strong enough to roll onto his stomach on his own, don't worry about it while he sleeps. It is enough to make sure that there are no soft objects in the cradle or bed where the child sleeps, in which the child can bury his face - this increases the risk of SIDS or suffocation. Attention! Do not use towels and various pads when trying to lay the child on his back, they can cause suffocation of the child.
2. Be careful when choosing a place for your child to sleep! Prepare a crib for your baby to sleep in advance. The mattress must be firm. The crib should not contain any toys, pillows, blankets, scarves and other items that can block the child's airways.
3. Co-sleeping with a child on a couch, in a chair carries an extremely high risk of SIDS or strangulation of the child!
4. Do not use devices claimed by manufacturers to prevent the risk of SIDS, their effectiveness and safety have not been proven!
5. Do not leave your child sleeping for a long time in a car seat, stroller, baby swing, inflatable seat, baby carrier, sling. If the baby falls asleep in one of these places, move him to a crib or crib as soon as possible. If your child is in a sling or special carrier, make sure their nose and mouth are free and not pressed against your body or clothing.
6. Sleep in the same room, not the same bed! It is better if the first six months the child sleeps in the same room as you. Do not put your baby in bed with you - this increases the risk of SIDS even in non-smoking mothers. Putting an infant to bed with you can also lead to suffocation, blocking the airways, and crushing the child.
7. Do not overheat your child. To avoid overheating your baby while sleeping, dress your baby with one more layer of clothing than an adult would wear in the room in order to feel comfortable. Watch for symptoms of overheating such as drops of sweat, damp hair. Do not cover your child's face with a hat or hood. If your baby is full-term, a few days after birth, he does not need a cap at home at all.
8. Register for pregnancy and follow your doctor's instructions. Careful and considerate prenatal care is important to protect the health of your unborn baby, reduce the risk of preterm birth and very low birth weight baby (both risk factors for SIDS). Therefore, follow all the doctor's prescriptions during pregnancy, both in terms of examination and in terms of treatment.
9. Do not smoke! Virtually all studies have determined that smoking during pregnancy increases the risk of SIDS.
10. Do not drink alcohol and prohibited substances during pregnancy!
Do not drink alcohol and prohibited substances during pregnancy!
Alcohol and illegal substance use are risk factors for SIDS. And, of course, these factors can significantly affect the health of your unborn child.
11. Keep your child away from cigarette smoke!
Keep the air around your child in your home, car, and anywhere else free of cigarette smoke. If someone close to you smokes, make sure they do it outside the house or apartment. If you yourself smoke, it is best to quit this bad habit.
12. Vaccinate your child!
Immunoprophylaxis of infectious diseases through vaccination according to the recommended schedule can reduce the risk of SIDS by up to 50%. Premature babies and children who have undergone pathological conditions during childbirth and during the neonatal period (the first 28 days of life) may be shown additional immunoprophylactic measures. Consult on this issue with neonatologists in the departments of pathology of newborns or a local pediatrician.
13. Breastfeed if you can.
Exclusive breastfeeding for 4-6 months reduces this risk of SIDS by about 70%.
14. Offer your baby a pacifier when you put him to bed.
The exact mechanism of this measure is currently not defined, however, given this relationship, it is recommended to give the child a dummy at bedtime during the first year of life. If the baby drops the pacifier during sleep, do not try to put it back. Don't force your baby to suck on a pacifier if he doesn't want to. Do not use a pacifier until breastfeeding is well established. As a rule, it takes 3-4 weeks after delivery.
Is it possible to swaddle a baby?
Swaddling can help prevent SIDS because it is easier for a swaddled baby to stay on their back while sleeping. Swaddling moderately restricts the child's mobility and creates a certain feeling of comfort and safety. However, it should be remembered that excessive or too tight swaddling can lead to overheating of the child. If you are swaddling your baby, use thin blankets and make sure the room is not too hot. And, of course, never put a swaddled baby on your stomach. When the baby gets older and starts to try to roll over or can get out of the swaddle, it is best to stop swaddling, as this can lead to unsafe diaper constriction or face covering.
If you are swaddling your baby, use thin blankets and make sure the room is not too hot. And, of course, never put a swaddled baby on your stomach. When the baby gets older and starts to try to roll over or can get out of the swaddle, it is best to stop swaddling, as this can lead to unsafe diaper constriction or face covering.
For prevention of Sudden Infant Death Syndrome, you can consult your local pediatrician or neonatologist who was involved in nursing your child in the neonatal period.
Safety in the car.
If you plan to transport your child in a car, be sure to use an infant carrier to protect your child from injury in the event of a car accident. Do not think that if you strictly follow the rules of the road, then nothing threatens you, there are other, less experienced road users.
Never leave a child unattended in a car, even if you plan to leave for a short time, take the child with you.
Bath safety.
Recently, cases of death of children from drowning while swimming have become more frequent.