How many weeks can you feel baby move
Baby movements during pregnancy | Pregnancy Birth and Baby
Baby movements during pregnancy | Pregnancy Birth and Baby beginning of content5-minute read
Listen
An exciting landmark of pregnancy is when you first feel the sensation of your baby move. These movements are a sign that your baby is healthy and well.
Every baby is unique, it is important for you to get to know your baby’s individual movement pattern. At any point, if you are concerned about your babies movement pattern, please contact your midwife or doctor immediately. Do not wait until the next day.
When will I feel my baby moving?
You will start to feel your baby moving between 16 and 24 weeks of pregnancy. The location of your placenta will not affect this sensation. It is more common for women having their second or subsequent pregnancies to feel their baby move earlier.
If you have not felt your baby move by 24 weeks, you should contact your doctor or midwife.
What will my baby’s movement feel like?
The type of movement you feel will depend on what your baby is doing and their stage of growth and development. Each baby is different, with some more active than others.
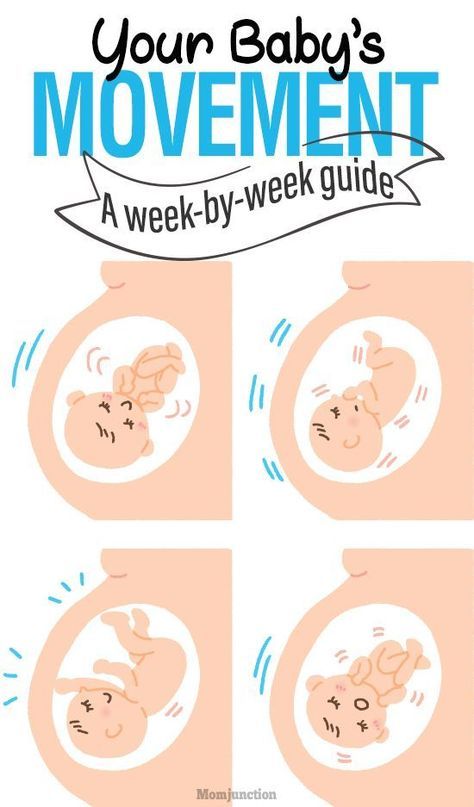
The first sensations you feel may be a fluttering (like 'butterflies in your tummy'), swishing, rolling or tumbling sensation or a tiny kick. These early sensations are often called ‘quickening’. As your pregnancy progresses, the movements will become more distinct, and you will more easily feel their kicks, jabbing and elbowing.
How often should I feel my baby moving?
There is no set number of movements you should feel. As you start to feel your baby's movements more consistently, usually by 24 to 28 weeks of pregnancy, you will get to know what a normal pattern of movement is for you and your baby. You should then consistently feel your baby's movements right up until they are born and even during labour.
You should then consistently feel your baby's movements right up until they are born and even during labour.
Babies tend to move more at certain times of day – they may be more active while you sleep, and sleep while you’re awake. Usually, unborn babies sleep for 20-40 minutes cycles (occasionally up to 90 minutes), and they don’t move when they’re asleep.
Should I track my baby’s movement?
There are no set number of movements a baby should have, so counting kicks or recording on a chart is no longer recommended.
It is important to make time regularly each day to notice your babies’ movements. If you are busy or not paying attention it can be easy to miss this very important signal from your baby. If you are busy or working, it may be helpful to set reminders for yourself to check in with your baby.
Common myths about baby movements
- It is not true that babies move less towards the end of pregnancy.
- Having something to eat or drink does not help stimulate your baby to move.

What should I do if my baby stops moving?
If you haven't felt any movement from your baby by 24 weeks, see your doctor or midwife.
At any stage of your pregnancy, if you are concerned about your baby's movements, contact your midwife or doctor immediately. Do not wait until the next day. A slowing down of movement may be a sign that your baby is unwell.
Your doctor or midwife will invite you into the hospital and check your baby’s heart rate using a CTG Machine. In some instances, you may also have an ultrasound.
What do I do if I have recurring concerns about my baby’s movements?
Remember you are the one who knows your baby’s movements best. It is important that whenever you are concerned about your baby’s movements to contact your doctor or midwife.
Contact your doctor or midwife again even if you have already seen them about your baby’s movements previously.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Available 7am to midnight (AET), 7 days a week.
Sources:
Australian Family Physician (Decreased fetal movements: a practical approach in primary care setting), Mater Mother's Hospital (Pregnancy – your baby’s movements and what they mean), Raising Children Network (16 weeks pregnant), Miracle Babies (Your baby’s movements), PSANZ SANDA (Baby's Movements), Red Nose (Decreased fetal movements (DFM)), Centre of Research Excellence in Stillbirth (Movement matters)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2022
Back To Top
Related pages
- Fetal heart rate monitoring
- Giving birth - early signs of labour
Need more information?
Baby movements during pregnancy | Red Nose Australia
When you're pregnant, you should feel baby move. But what does it means when those movements change, become less frequent, or stop?
But what does it means when those movements change, become less frequent, or stop?
Read more on Red Nose website
Your Baby's Movements - Miracle Babies
This information has been graciously reproduced with permission from Australian and New Zealand Stillbirth Alliance to provide information about what your baby’s movements mean
Read more on Miracle Babies Foundation website
Reducing the risk of stillbirth | Raising Children Network
You can reduce risk of stillbirth by eating well and exercising, sleeping on your side, and seeking immediate medical help if your baby’s movements change.
Read more on raisingchildren.net.au website
How baby learns in the womb - Ngala
From the moment of conception your baby is developing rapidly
Read more on Ngala website
Pregnant women not to trust smartphone heart rate apps
Pregnant women are being urged not to rely on smartphone apps that claim to listen to your baby's heartbeat.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 16
At week 16, you might begin to feel your baby moving, while hormonal changes may be affecting your libido.
Read more on Pregnancy, Birth & Baby website
Premature birth & premature babies | Raising Children Network
This essential guide for parents of premature babies covers gestational age, premature birth risk factors, premature labour and premature development.
Read more on raisingchildren.net.au website
Fetal alcohol spectrum disorder (FASD) | Raising Children Network
Drinking alcohol in pregnancy can cause birth defects and long-term health problems for babies and children. This is fetal alcohol spectrum disorder (FASD).
This is fetal alcohol spectrum disorder (FASD).
Read more on raisingchildren.net.au website
24 weeks pregnant | Raising Children Network
24 weeks pregnant? In this pregnancy week by week guide, find out how your baby is growing, how your body is changing and how to look after yourself.
Read more on raisingchildren.net.au website
Pregnancy at week 24
Your baby is continuing to grow rapidly and might respond to light and sound. You might also find their movements are getting stronger.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Fetal Movement - WebMD: When You Feel Baby Kick
Written by Stephanie Watson
Reviewed by Traci C. Johnson, MD on January 08, 2021
In this Article
- When Will I Feel My Baby Kicking?
- What Does the Baby's Kicking Feel Like?
- How Often Should I Feel My Baby Moving?
- Should I Monitor My Baby's Kicking?
- If You Don't Feel Your Baby Moving
- Timeline of Baby Movement
One of the most exciting moments in your pregnancy is when you feel those first little flutters of your baby kicking. These tiny movements reassure you that your baby is developing and help you feel closer to the little life inside of you.
When Will I Feel My Baby Kicking?
You should feel your baby's first movements, called "quickening," between weeks 16 and 25 of your pregnancy. If this is your first pregnancy, you may not feel your baby move until closer to 25 weeks. By the second pregnancy, some women start to feel movements as early as 13 weeks. You're more likely to feel baby move when you're in a quiet position, either sitting or lying down.
What Does the Baby's Kicking Feel Like?
Pregnant women describe their baby's movements as butterflies, nervous twitches, or a tumbling motion. At first, it may be hard to tell whether your baby has moved. Second- and third-time moms are more adept at distinguishing those first baby movements from gas, hunger pangs, and other internal motions.
By your second and third trimesters, the movements should be more distinct, and you'll be able to feel your baby's kicks, jabs, and elbows.
How Often Should I Feel My Baby Moving?
Early in your pregnancy, you may just feel a few flutters every now and then. But as your baby grows -- usually by the end of the second trimester -- the kicks should grow stronger and more frequent. Studies show that by the third trimester, the baby moves about 30 times each hour.
But as your baby grows -- usually by the end of the second trimester -- the kicks should grow stronger and more frequent. Studies show that by the third trimester, the baby moves about 30 times each hour.
Babies tend to move more at certain times of the day as they alternate between alertness and sleep. They are usually most active between 9 p.m. and 1 a.m., right as you're trying to get to sleep. This surge in activity is due to your changing blood sugar levels. Babies also can respond to sounds or touch, and may even kick your partner in the back if you snuggle too close in bed.
Should I Monitor My Baby's Kicking?
Once your baby's movements are well established (usually by week 28), some doctors recommend keeping track of all those little punches, jabs, and kicks to make sure your baby is still developing the way they should. This is known as a fetal movement assessment, fetal kick count, or fetal movement counting.
Obstetricians recommend moms do fetal movement counts. While reduced movements or counts done at home can be worrisome, they may not be reliable. If you feel your baby is moving or kicking less often than normal, contact your doctor.
While reduced movements or counts done at home can be worrisome, they may not be reliable. If you feel your baby is moving or kicking less often than normal, contact your doctor.
Counting is a lot harder when you have twins. You may not be able to tell which baby is moving. Even so, many doctors recommend it as a way to keep track.
If you are counting, it helps to chart your baby's kicks so that you can keep track of your baby's normal patterns of movement. To count movements, pick a time when your baby is usually most active (often, this is right after you've eaten a meal). Get into a comfortable position either sitting down in a comfortable chair or lying on your side. If you lie down, lie on your left side, so your baby will have better circulation.
Opinion varies as to how to count your baby's movements, but the American College of Obstetricians and Gynecologists recommends noting the time it takes for your baby to make 10 movements. You should feel at least 10 movements within a 2-hour period.
If you can't feel 10 movements in 2 hours despite eating something and fully focusing on the baby's movements, call your doctor for advice on what to do next.
If You Don't Feel Your Baby Moving
If you haven't yet reached 25 weeks and don't feel your baby move, or you're not sure that what you're feeling is actually your baby, don't panic. As your baby grows, you'll be able to better distinguish their movements. You'll also figure out at what times of the day your baby is most active. Some babies just naturally move less often than others.
A lack of movement also may mean that your baby is asleep. You may feel fewer kicks and jabs after the 32nd week as your baby gets bigger and has less room to move around in the uterus.
If your baby has started to move regularly and you don't feel at least 10 movements within a 2-hour period, or the movements have slowed significantly, it's time to call your doctor.
Timeline of Baby Movement
Here is a guide to your baby's possible movements.
Week 12: Your baby should start to move, but you probably won't be able to feel anything because the baby is still so small.
Week 16: Some pregnant women will start to feel tiny butterfly-like flutters. The feeling might just be gas, or it might be the baby moving.
Week 20: By this point in your baby's development, you may start to really feel your baby's first movements, called "quickening."
Week 24: The baby's movements are starting to become more established. You might also begin to feel slight twitches as your baby hiccups.
Week 28: Your baby is moving often now. Some of the kicks and jabs may take your breath away.
Week 36: Your uterus is getting crowded as the baby grows, and movements should slow down a bit. However, alert your doctor if you notice significant changes in your baby’s usual activity. You should feel consistent movement throughout the day.
Fetal movement - how and when does it occur
- At what time does fetal movement begin
- Fetal movement rate
- Methods for assessing the "sufficiency" of fetal movements
- Changes in fetal activity
- Determination of the condition of the fetus
“Dear patients, we are glad to welcome you to the website of the Fetal Medicine Center – a medical center of expert level in the field of modern prenatal medicine.
We see our mission in making the expectation of a child and its birth a happy, calm and most comfortable period for every woman. By providing professional medical support, we help couples plan pregnancy, control its harmonious course, conduct expert-level prenatal diagnostics, providing comprehensive care for the health of the expectant mother and baby.”
Roza Saidovna Bataeva
Head of the Fetal Medicine Center in Moscow
From the very beginning of pregnancy, every expectant mother begins to listen carefully to the sensations inside her growing belly. Can't wait to feel your baby move. When does the fetus begin to move? At what time can a pregnant woman begin to listen carefully to herself, waiting for the first movements of her child? Should I be worried if they are not felt or the baby suddenly calmed down? And can movements carry any other information, besides communicating with mom?
At what time does the fetal movement begin
The first movements of the future baby begin early - already at 7-8 weeks of pregnancy . It was at this time that the first muscles and the rudiments of the nervous system of the fetus are formed. Naturally, at this time, the movements of the embryo are still very primitive - these are muscle contractions in response to nerve impulses.
It was at this time that the first muscles and the rudiments of the nervous system of the fetus are formed. Naturally, at this time, the movements of the embryo are still very primitive - these are muscle contractions in response to nerve impulses.
Approximately from 10 weeks of pregnancy the fetus begins to move more actively in the uterus, and, encountering an obstacle on its way (walls of the uterus), change the trajectory of movements. However, the baby is still very small and the impacts on the uterine wall are very weak, the expectant mother cannot yet feel them. At 11-12 weeks of intrauterine life, a little man already knows how to clench his fists, grimace, frown, by 16 weeks of pregnancy he begins to react to loud, sharp sounds with increased motor activity, at 17 weeks the first facial expressions appear, and at 18 weeks he covers his face with his hands and plays with the umbilical cord, clenching and unclenching the fingers.
Gradually, with increasing gestational age, movements become more coordinated and more like conscious. When the baby grows up, the pregnant woman begins to feel his movements.
When the baby grows up, the pregnant woman begins to feel his movements.
When does fetal movement begin during the first and subsequent pregnancies
It is generally accepted that during the first pregnancy, the expectant mother feels the first fetal movements at 20 weeks of pregnancy, with repeated pregnancies - at 18 weeks. This is not entirely true. A mother who is expecting her first child, indeed, most often begins to feel the movements of the fetus a little later than a multiparous woman. This is due to the fact that "experienced" mothers know how the movements of the crumbs are felt at first and what they should feel. Some primigravidas perceive the first movements of the fetus as an increase in intestinal peristalsis, “gaziki”. Many women describe the first movements of the fetus as a feeling of fluid transfusion in the abdomen, "fluttering butterflies" or "swimming fish."
The first movements are usually rare and irregular. The time of the first sensations of fetal movements naturally depends on the individual sensitivity of the woman. Some future mothers feel the first movements as early as 15-16 weeks, and someone only after 20. Slender women, as a rule, begin to feel movements earlier than full ones. Women who lead an active lifestyle, work hard, usually feel the movements of the fetus later.
Some future mothers feel the first movements as early as 15-16 weeks, and someone only after 20. Slender women, as a rule, begin to feel movements earlier than full ones. Women who lead an active lifestyle, work hard, usually feel the movements of the fetus later.
By 20 weeks, due to the formation of the spinal cord and brain, as well as the accumulation of a certain amount of muscle mass in the fetus, movements become more regular and noticeable .
From 24 weeks of pregnancy, the movements of the fetus are already reminiscent of the movements of a newborn - the expectant mother feels how the fetus changes position, moves its arms and legs. The motor activity of the fetus increases gradually and its peak falls on the period from the 24th to the 32nd week of pregnancy. At this time, the activity of the baby's movements becomes one of the indicators of its normal development. After 24 weeks, the child begins to "communicate" with the mother with the help of movements, respond to the sounds of voice, music, and the emotional state of the mother. With an increase in the gestational age of more than 32 weeks, the motor activity of the fetus gradually decreases due to the fact that the baby is growing up and he simply does not have enough space for active movements. This becomes especially noticeable at the time of childbirth. By the end of the third trimester of pregnancy, the number of fetal movements may decrease somewhat, but their intensity and strength remain the same or increase.
With an increase in the gestational age of more than 32 weeks, the motor activity of the fetus gradually decreases due to the fact that the baby is growing up and he simply does not have enough space for active movements. This becomes especially noticeable at the time of childbirth. By the end of the third trimester of pregnancy, the number of fetal movements may decrease somewhat, but their intensity and strength remain the same or increase.
Fetal movement rate
The baby in the mother's belly moves almost constantly. At the 20th week of pregnancy, the fetus makes about 200 movements per day, and between the 28th and 32nd weeks, the number of movements reaches 600 per day. Naturally, a pregnant woman does not feel all the movements of the fetus, but only a small part of them. So, after 28 weeks, the frequency of fetal movement, according to the sensations of a woman, is usually 4 to 8 times per hour, with the exception of periods of fetal sleep (3-4 hours in a row).
In the third trimester, a pregnant woman may notice that her baby has regular sleep and wake cycles.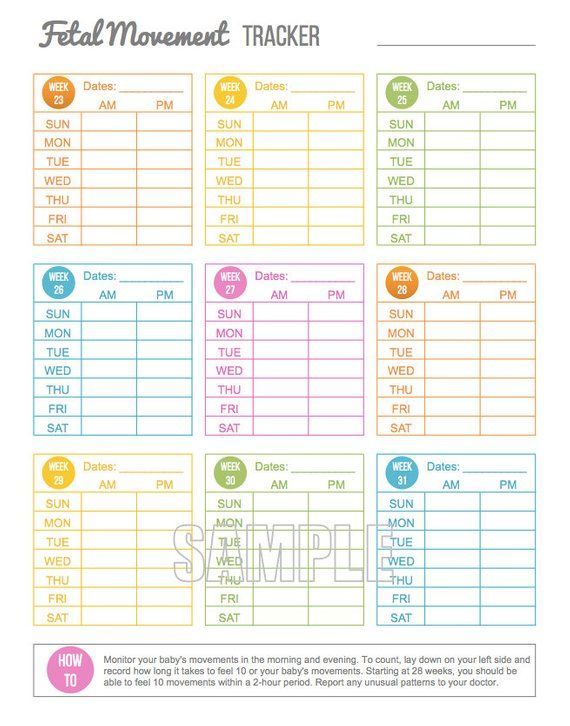 Children are usually most active from 19:00 to 4:00 in the morning, and the period of "rest" occurs more often from 4 to 9:00 in the morning. Of course, the movements of the fetus depend on the mood of the mother, if the mother is worried or happy, the baby can move more actively, or vice versa, calm down. The fact is that when a mother rejoices, her body significantly increases the amount of hormones of joy - endorphins, which regulate the work of the heart and blood vessels, including the vessels of the placenta. During stress or pronounced negative emotions, biologically active substances are also produced - stress hormones, they also affect the work of the heart and blood vessels. It is thanks to this biological interaction between the organisms of mother and baby that the fetus feels the state of the mother. When the expectant mother is resting, the baby usually becomes more active, if the pregnant woman is active, busy with some kind of work, the child most often calms down. The movements also change depending on the satiety of the expectant mother.
Children are usually most active from 19:00 to 4:00 in the morning, and the period of "rest" occurs more often from 4 to 9:00 in the morning. Of course, the movements of the fetus depend on the mood of the mother, if the mother is worried or happy, the baby can move more actively, or vice versa, calm down. The fact is that when a mother rejoices, her body significantly increases the amount of hormones of joy - endorphins, which regulate the work of the heart and blood vessels, including the vessels of the placenta. During stress or pronounced negative emotions, biologically active substances are also produced - stress hormones, they also affect the work of the heart and blood vessels. It is thanks to this biological interaction between the organisms of mother and baby that the fetus feels the state of the mother. When the expectant mother is resting, the baby usually becomes more active, if the pregnant woman is active, busy with some kind of work, the child most often calms down. The movements also change depending on the satiety of the expectant mother. Usually the baby begins to move actively after the mother eats, especially something sweet. At the same time, the level of glucose in the blood increases sharply, which causes the fetus to be more active.
Usually the baby begins to move actively after the mother eats, especially something sweet. At the same time, the level of glucose in the blood increases sharply, which causes the fetus to be more active.
Fetal movements are the language in which the unborn child speaks to the mother. Naturally, a pregnant woman should listen to the movements, because in some cases, changes in the movements of the fetus may indicate a violation of its intrauterine state and a not entirely successful pregnancy.
If, after 20 weeks of pregnancy, the expectant mother does not feel the movement of the fetus, it may be worthwhile to see a doctor and make sure that everything is in order with the baby.
Methods for assessing the "sufficiency" of fetal movements
Counting the number of movements
The easiest way to assess fetal movements is to count the number of movements of the pregnant woman herself. Self-assessment methods are very easy to use, do not require additional equipment, the presence of a doctor and are easily reproducible by any woman.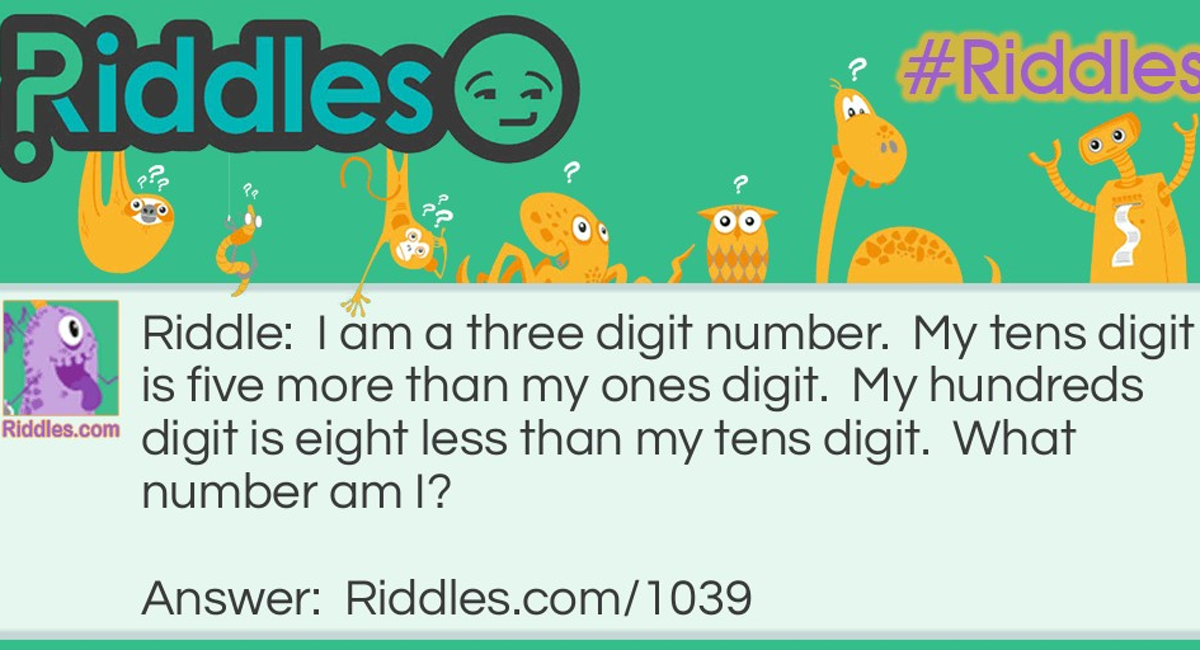 Their disadvantages are that each woman has different thresholds of susceptibility.
Their disadvantages are that each woman has different thresholds of susceptibility.
Count to ten
The most common method for assessing fetal movements is called count to ten . It can be carried out after 28 weeks of pregnancy, when the fetus is mature enough for active movements. Its essence lies in the fact that the expectant mother counts the movements of the fetus for a 12-hour time interval, for example, from 9 am to 9 pm. The time when a pregnant woman catches the tenth movement is recorded on a tablet. If the fetus makes less than 10 movements in 12 hours, this is a reason to consult a doctor for an additional examination.
Sadowski method
In the evening after dinner (approximately between 7until 11 p.m.), the woman lies on her left side and counts the movements of the fetus. At the same time, everything is considered, even the smallest movements. If 10 or more movements are noted within an hour, this indicates that the baby is moving quite actively and feels good. If the fetus moved less than 10 times in an hour, then the movements are counted for the next hour. Evening time for this assessment method was not chosen by chance. It is in the evening hours, especially after dinner and the associated increase in glucose, that the greatest activity of the fetus is noted. If the number of fetal movements during this test is less than 10 per two hours, this should be considered as a sign of a violation of his condition and additional studies should be carried out.
If the fetus moved less than 10 times in an hour, then the movements are counted for the next hour. Evening time for this assessment method was not chosen by chance. It is in the evening hours, especially after dinner and the associated increase in glucose, that the greatest activity of the fetus is noted. If the number of fetal movements during this test is less than 10 per two hours, this should be considered as a sign of a violation of his condition and additional studies should be carried out.
For an obstetrician-gynecologist, fetal movements are also an important diagnostic criterion for some deviations in the course of pregnancy from the norm. Too active, violent, painful fetal movement or weak, rare movements may indicate its unfavorable condition.
Changes in fetal activity
Changes in fetal activity may be associated with external influences. For example, if a pregnant woman lies on her back for a long time, then the enlarged uterus compresses a large vessel - the inferior vena cava, the blood flow to the fetus is disrupted, which immediately causes its violent reaction - active movements.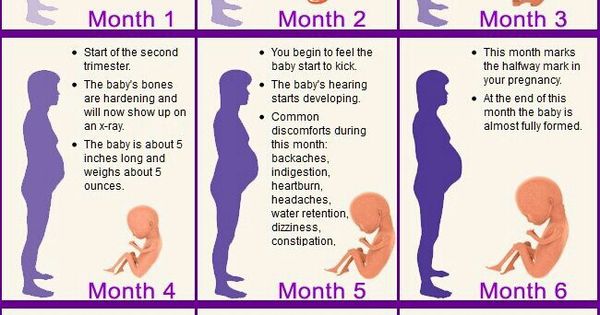 The same changes in the activity of the baby can occur in any other uncomfortable position of the mother - if she leans forward, squeezing her stomach, sits with her legs crossed, the child forces her mother to change her position with her activity. A similar situation occurs if the baby himself squeezes or presses the loops of the umbilical cord, limiting the flow of blood through it. He begins to move more actively, changes his position and relieves pressure on the umbilical cord. However, in some cases, an increase or vice versa, a subsidence of fetal movements can be a sign of a serious pathology.
The same changes in the activity of the baby can occur in any other uncomfortable position of the mother - if she leans forward, squeezing her stomach, sits with her legs crossed, the child forces her mother to change her position with her activity. A similar situation occurs if the baby himself squeezes or presses the loops of the umbilical cord, limiting the flow of blood through it. He begins to move more actively, changes his position and relieves pressure on the umbilical cord. However, in some cases, an increase or vice versa, a subsidence of fetal movements can be a sign of a serious pathology.
After 28 weeks of pregnancy, if your baby does not let you know for 3-4 hours, he may just be sleeping. In this case, the expectant mother needs to eat something sweet and lie down on her left side for half an hour. If these simple manipulations do not lead to a result, it is worth repeating them again after 2-3 hours. If this time the baby does not make itself felt, this is an occasion to consult a doctor. Rare and weak movements can also indicate a fetal problem, most often a lack of oxygen for the baby, that is, fetal hypoxia.
Rare and weak movements can also indicate a fetal problem, most often a lack of oxygen for the baby, that is, fetal hypoxia.
Determining the condition of the fetus
To determine the condition of the fetus, the doctor conducts a series of examinations:
Auscultation (listening)
The simplest is auscultation (listening) with a special wooden tube (obstetric stethoscope) or a special apparatus that captures the fetal heartbeat, doctor listens to the baby's heartbeat. Normally, it is about 120-160 beats per minute. A decrease in heart rate less than 120 or an increase of more than 160 indicates intrauterine suffering of the child.
Ultrasound and dopplerometry
During ultrasound, the doctor visually assesses the size of the fetus, the compliance of the development of the fetus with the gestational age, because with oxygen starvation, the growth rate of the fetus slows down and its size lags behind the norm for each period of pregnancy. Also important is the structure of the placenta, the presence of signs of aging in it, as a result of which the function of transferring blood, oxygen and nutrients to the fetus usually worsens. During ultrasound, the amount and type of amniotic fluid is assessed, which can also change with intrauterine fetal suffering. Dopplerometry of the vessels of the placenta and umbilical cord is a method for studying blood flow velocities in these vessels. With a decrease in the speed of blood flow in any vessel, one can speak of fetal malnutrition of varying severity.
Also important is the structure of the placenta, the presence of signs of aging in it, as a result of which the function of transferring blood, oxygen and nutrients to the fetus usually worsens. During ultrasound, the amount and type of amniotic fluid is assessed, which can also change with intrauterine fetal suffering. Dopplerometry of the vessels of the placenta and umbilical cord is a method for studying blood flow velocities in these vessels. With a decrease in the speed of blood flow in any vessel, one can speak of fetal malnutrition of varying severity.
Cardiotocography (CTG)
This is an important method for assessing the condition of the fetus. CTG is performed at a gestational age of 33 weeks or more, since only in this period of intrauterine development of the baby is a full-fledged regulation of the activity of the cardiovascular system of the fetus by the centers of the spinal cord and brain. Recording of fetal heartbeats is carried out for at least 40 minutes, and if necessary, the study can be extended up to one and a half hours. The device registers and records the baby's heart rate. For example, with a decrease in the concentration of oxygen in the blood of the fetus, the supply of oxygen to the cells of the nervous system decreases, which in turn affects the heart rate, especially during the period of wakefulness of the child. The obstetrician-gynecologist evaluates the heartbeat recording curve, episodes of slowing down and a sharp increase in the fetal heart rate, and based on these data, makes a conclusion about how comfortable the baby feels in the mother's stomach.
The device registers and records the baby's heart rate. For example, with a decrease in the concentration of oxygen in the blood of the fetus, the supply of oxygen to the cells of the nervous system decreases, which in turn affects the heart rate, especially during the period of wakefulness of the child. The obstetrician-gynecologist evaluates the heartbeat recording curve, episodes of slowing down and a sharp increase in the fetal heart rate, and based on these data, makes a conclusion about how comfortable the baby feels in the mother's stomach.
If during additional methods for assessing the condition of the fetus, initial disturbances in the supply of oxygen to the baby are detected, drug treatment is carried out aimed at increasing the access of blood and oxygen through the placenta and mandatory control examinations against the background of ongoing therapy. If the changes are profound and the baby experiences a pronounced deficiency of oxygen and nutrients, his condition suffers, an emergency delivery of such a patient is performed.
Fetal movements are not only an indicator of his condition, it is a way of communication between the baby and parents. The movements of the crumbs in the mother's tummy are unforgettable sensations that a woman can experience only in this short, but such a happy period of her life.
Center for Fetal Medicine in Moscow:
The main activities of our center are the early detection of congenital malformations in the fetus, prenatal screening for the detection of chromosomal abnormalities in the fetus, as well as pregnancy complications such as preeclampsia, fetal growth retardation and threatened abortion.
Our center is organized in such a way that the whole range of services is concentrated in one place, where a woman receives the results of various types of examinations, including ultrasound, biochemical, and specialist consultation within 1-1.5 hours. In the presence of a high risk for chromosomal diseases in the fetus, invasive diagnostics and genetics consultation are carried out here in the center.
Fetal echocardiography is given special attention in our center, since congenital heart defects in the fetus are increasingly common today, but, unfortunately, are often missed during ultrasound during pregnancy.
In view of the ever-increasing number of multiple pregnancies, which requires more time and a special approach, the observation of women with multiple pregnancies has been allocated to us in a separate clinic for multiple pregnancies.
All examinations in the center are carried out according to the international standards FMF (Fetal Medicine Foundation) and ISUOG (International Society for Ultrasound in Obstetrics and Gynecology). In complex clinical cases, we can consult with specialists from King's College Hospital, King's College Hospital (London, UK).
The team is a special pride of the center. Our doctors are not only one of the leading specialists, professors, doctors and candidates of medical sciences, doctors of the highest categories, they are also a team of like-minded people and real enthusiasts in their field. All ultrasound diagnostic doctors in our center have international FMF certificates. Having extensive experience in prenatal diagnostics, we share our knowledge with our colleagues by conducting training courses.
All ultrasound diagnostic doctors in our center have international FMF certificates. Having extensive experience in prenatal diagnostics, we share our knowledge with our colleagues by conducting training courses.
The Center is equipped with the most modern diagnostic equipment: these are the latest generation ultrasound machines, GE Voluson E8 Expert, with a complete set of modern technologies, including three-dimensional ones, this is a biochemical analyzer, Delfia Xpress, these are workplaces with professional computer programs.
Fetal movements during pregnancy | When do the first movements appear
When do the first movements appear?
The baby begins to move very early in the womb - at 7-8 weeks of gestation. But the first movement of the fetus goes unnoticed, since during this period it is very tiny, a little larger than a marigold.
The first tangible movements of the child, as a rule, appear in the second trimester - between 16 and 22 weeks of pregnancy, when the baby has already grown and grown stronger. The week in which the movement is felt depends on many factors:
The week in which the movement is felt depends on many factors:
- First or second child. During the first pregnancy, the movements of the baby become noticeable closer to the 20-22nd week. If the pregnancy is the second or third, the movements begin to be felt on average at 18 weeks or even earlier, because the woman already knows what sensations to expect.
- Placenta placement. If the placenta is closer to the back wall of the uterus, then the woman may feel movements later, if to the front - earlier.
- The physique of the expectant mother. Sometimes physique plays a role: fragile girls can feel the first tremors 2 weeks earlier.
- Lifestyle. In the midst of the working day, in noise or shaking, fetal movement is easy to miss. It is more likely to feel the first movement of the crumbs in a calm position, sitting or lying down.
In what part of the abdomen do you feel the first movements? Usually timid first movements are felt in the lower abdomen. At first, it is easy to confuse them with other internal processes, such as rumbling and bouts of hunger. But the baby grows and the movements become more intense, more diverse and “travel” along the tummy along with the tumbling baby.
At first, it is easy to confuse them with other internal processes, such as rumbling and bouts of hunger. But the baby grows and the movements become more intense, more diverse and “travel” along the tummy along with the tumbling baby.
Features of fetal movements at different stages of pregnancy
The nature and frequency of movements of the child change as it grows and develops. At first they are weak and irregular, but then the activity increases, and the movements become stronger and more intense.
Let's take a closer look at how the baby moves at different times and how the mother feels it.
First trimester
Toward the end of the first trimester, the baby begins to make its first movements, light as the flutter of a butterfly. But it is still very small, so in most cases the movements go unnoticed. The maximum that can be felt is a light, light, barely noticeable flutter in the lower abdomen or something resembling bubbles.
Second trimester
At the 16th week of pregnancy, some women begin to feel the baby move.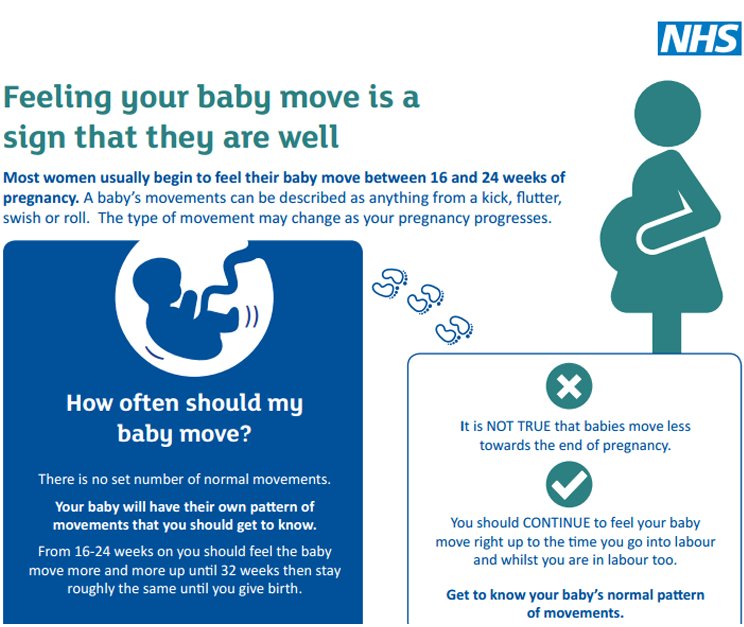 Someone describes them as the flutter of small wings or the movement of a fish wagging its tail, while someone describes them as twitching of a vein pulsating inside or blows of a small hammer.
Someone describes them as the flutter of small wings or the movement of a fish wagging its tail, while someone describes them as twitching of a vein pulsating inside or blows of a small hammer.
By 20 weeks, most pregnant women already feel the baby's light movements. At week 24, they become more pronounced and intense, sometimes accompanied by a slight twitch during hiccups. By the end of the second trimester, active fetal movement begins - the child somersaults and pushes more and more clearly, more often and stronger.
Third trimester
At week 28, the baby moves up to 30 times an hour, and some of his kicks and pokes can be so strong that the mother takes her breath away. During this period, obstetricians recommend starting to count the movements of the child. The nature of the activity helps the doctor understand what is happening with the baby and how he is developing.
At this stage of development, the baby develops a certain pattern of sleep and wakefulness. Peak activity tends to occur in the evening and at night—between 9:00 PM and 01:00 AM—just when mom is trying to sleep. This surge is due to changes in blood sugar levels. In addition, the movements of the baby can react to touch, bright light, loud noises or an uncomfortable posture of the mother.
Peak activity tends to occur in the evening and at night—between 9:00 PM and 01:00 AM—just when mom is trying to sleep. This surge is due to changes in blood sugar levels. In addition, the movements of the baby can react to touch, bright light, loud noises or an uncomfortable posture of the mother.
Your baby's activity continues to increase until 32 weeks. But after that, the grown-up child becomes more and more crowded in the fetal sac and the number of movements is reduced.
Tip
If you want your baby to make itself felt and move around, eat something sweet and lie on your side. An increase in blood glucose will cheer up the baby and he will begin to push.
Due to lack of space, fetal movements before childbirth become slower and more and more constrained. However, the baby should continue to move regularly throughout the day.
Important!
If the child's activity changes abruptly for unexplained reasons: he calms down or vice versa - the movements are too intensified and more frequent - tell your doctor as soon as possible.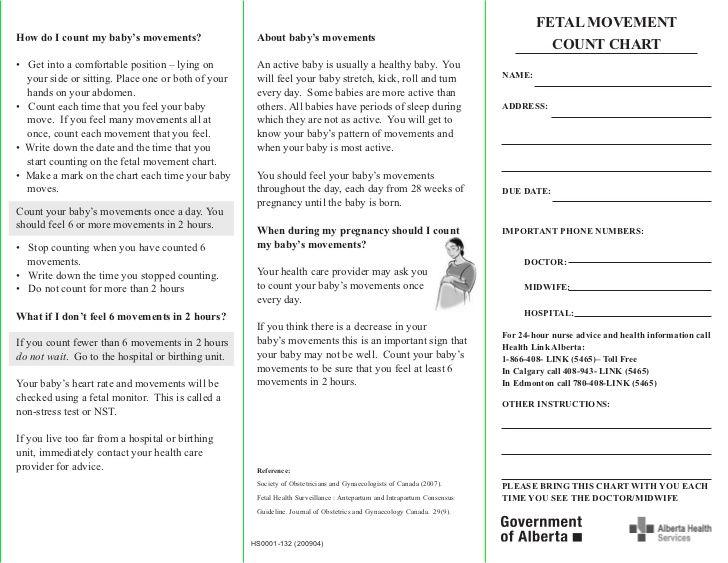 A change in the motor activity of the fetus may be a symptom of a violation of its condition and necessarily requires additional examination.
A change in the motor activity of the fetus may be a symptom of a violation of its condition and necessarily requires additional examination.
How to correctly calculate fetal movements?
Starting from the 28th week of pregnancy, the child's physical activity should be monitored every day. Until this time, the movements of the baby are not so noticeable, so the calculation will be uninformative.
So, how many movements should be per day? And how to count them correctly?
To determine the characteristics of the child's activity at home, use a special test of fetal movement by D. Pearson - "Count to ten". To do this, you need to mark in a special table every tenth movement of the baby from 9:00 to 21:00. If the child develops normally, then in 12 hours you will count at least 10 movements.
Important!
Not every push is considered a movement, but a series of movements (from the start of pushes to a pause).
After the 10th movement, you need to write down the time and start counting the next day. And if the baby moves much less or does not make itself felt within 12 hours, contact your doctor as soon as possible!
And if the baby moves much less or does not make itself felt within 12 hours, contact your doctor as soon as possible!
In addition to the Pearson test, there is another way to count the child's movements. Choose an hour during which you will count movements every day. It is very important to do it at the same time. Focus on the baby's movements and see how long it takes the baby to complete 10 kicks. If you counted 10 shocks in an hour, you can be calm - everything is in order.
If you still don't get 10 pushes within an hour, try eating, changing your position, and then try counting the number of pushes again.
Tip
Keep a movement diary to keep track of all changes. You can write everything in a notebook, or you can use a special mobile application that will help you track and record movements.
What should alert the future mother?
Be sure to contact your gynecologist if:
- You are past 22 weeks and you still don't feel your baby move.
 Perhaps you just did not notice them, but you need to make sure that the pregnancy is proceeding normally.
Perhaps you just did not notice them, but you need to make sure that the pregnancy is proceeding normally. - Tracking the activity of the child, you notice that for more than 12 hours there is no movement at all or they have become significantly less during the day.
- For several hours in a row, the baby behaves too actively, the intensity of the shocks has changed so much that it hurts you because of his movements.
- A sharp change in the nature and frequency of movements is monitored, although there are no apparent reasons for this. This may indicate a violation of the condition of the fetus, its heartbeat, or an infection.
Advice
In the third trimester of pregnancy, it is not recommended to sleep on your back. In this position, the vena cava can be clamped, which provides the baby with oxygen.
See also: Cord entanglement: causes and consequences for the baby
To make sure your baby is okay, your doctor may do several tests, such as auscultation, cardiotocography (CTG), and Doppler ultrasound.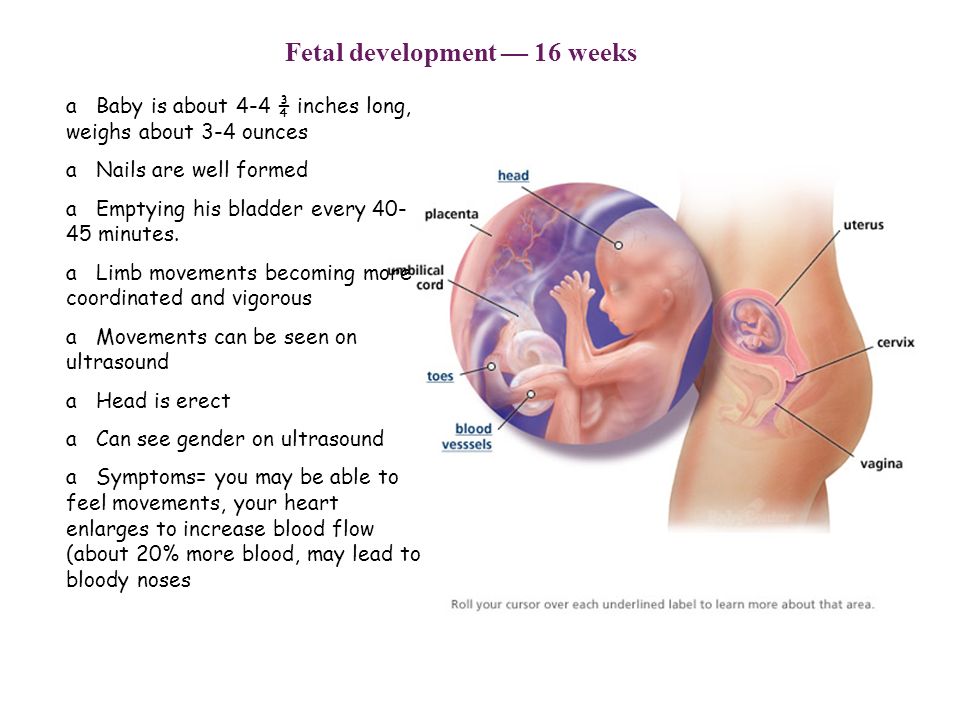
Auscultation is a method of assessing the condition of the baby by the sounds that he makes in the womb. The doctor listens to the tone and rhythm of the heartbeat, different noises, monitors their sequence and duration.
CTG (cardiotocography) is an ultrasound examination of the fetus. But unlike conventional ultrasound, during CTG, the tone of the uterus, the heartbeat and the movements of the baby are recorded. Based on the results of this study, the doctor can determine how comfortable the child feels, check the work of his heart and the level of development. If there are deviations in CTG, the specialist may recommend an assessment of the fetal blood flow - dopplerometry.
If indicated, your doctor can choose the right treatment, recommend that the mother rest and get more rest, or even prescribe bed rest.
Pregnancy not only changes the life of a future mother, but also causes many doubts. We will help you deal with all the fears and find answers to the most important questions about motherhood.