Baby is breech at 31 weeks
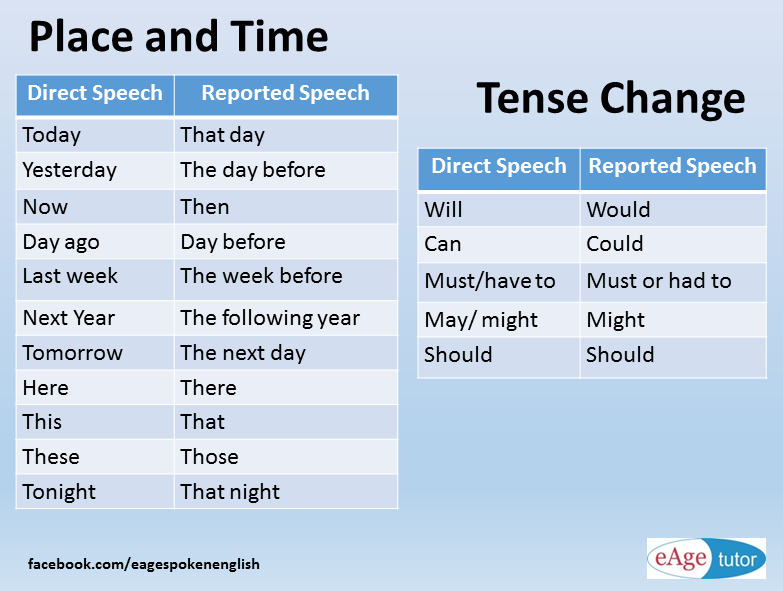
When Is Breech an Issue?
The later in pregnancy a baby is breech, the more difficult it is for the baby to flip head down. The baby’s size grows in relation to the uterus and there is a smaller percentage of amniotic fluid for the baby to move freely. The more complicated past births were due to fetal position, the earlier I suggest starting to get your muscles unwound and your pelvis aligned. If a previous baby remained either breech or posterior until birth, I suggest bodywork throughout the pregnancy.
In time, the breech baby’s head becomes heavy enough (between 5-7 months) for gravity to bring the head down in a symmetrical womb. The baby will move head down if there is room or if there is tone in the support to the uterus to direct the baby head down.
Common issues with breech:
- Health of the baby overall
- Safety of the birth
- Safety for the mother facing surgical birth
- Emotions of the birthing parent(s)
When should I be concerned about a breech position?
During the month before 30 weeks, about 15% of babies are breech. Since breech baby’s spine is vertical, the womb is “stretched” upwards. We expect babies to turn head down by 28-32 weeks.
Breech may not be an issue until 32-34 weeks. If you know your womb has an unusual limitation in shape or size, such as a bicornate uterus then begin body balancing before pregnancy and once 15 weeks in pregnancy. In this case, the baby needs to be head down much earlier so that the uterus still has the room for baby to turn. Every unique womb is unique so these dates are theoretical, not absolute.
The timeline for breech
This is a timeline of what to do and when to do it in order to help a breech baby move head down:
- Before 24-26 weeks, most babies lie diagonally or sideways in the Transverse Lie position.
- Between 24-29 weeks, most babies turn vertical and some will be breech.
- By 30-32 weeks, most babies flip head down and bottom-up.
- By 34 weeks pregnant, the provider expects the baby to be head down.
- Between 36-37 weeks, a provider may suggest an external cephalic version.
- Full term is from 37-42 weeks gestation, and about 3-4% of term babies are breech.
The medical model of care addresses the breech position between 36-37 weeks, when baby’s survival outside the womb won’t include special nursery care to breathe or suck. Physicians Oxorn and Foote, however, recommend helping babies turn head down at 34 weeks. Some home birth midwives suggest interacting with a baby at 30-34 weeks to encourage a head-down position (vertex).
Women who have had difficult previous births due to posterior, asynclitism, or a labor that didn’t progress, may want to begin bodywork and the Forward-leaning Inversion as soon as the second trimester of pregnancy (after morning sickness is gone and extra things like fetal positioning activities can be thought about).
Here is a general guideline for the average pregnancy:
10-24 weeks gestationThis is the time when fetal position is generally determined, even though the baby’s final position isn’t typically set before 34 weeks gestation. How can this be? The body has a habit, so to speak, of how the soft tissues, ligaments, muscles, and alignment of the pelvis and whole body is set. The baby simply follows this basic pattern. By adding body balancing now, the baby has an increased chance of ideal positioning for labor at 34 weeks and beyond.
24-30 weeksRoutine good posture with walking and exercise will help most babies be head down as the third trimester gets underway. A 30-second inversion is good practice for everyone. Unless you have a medical reason not to, please consider the Forward-leaning Inversion. If you have a history of car accidents, falls, uncomfortable pregnancies, hormonal imbalance, or a previous breech or posterior baby, then begin the inversion and body work before or during early pregnancy.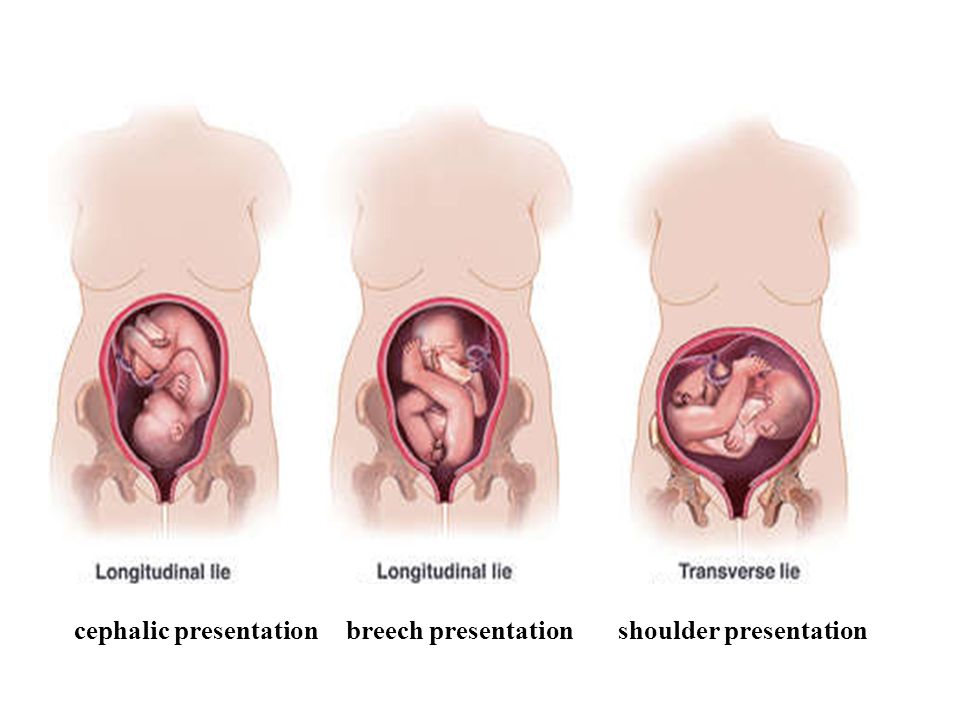
Oxorn and Foote recommend external version at 34 weeks, but most doctors want to wait for the baby’s lungs and suck reflex to be more developed in case the maneuver goes wrong and starts labor or pulls the placenta off the uterine wall. There is often enough amniotic fluid for an easy flip before 35 weeks.
- Inversion: Use of maternal positions that put the mother upside down may help a baby use gravity to flip. Get i
Dad’s the hero in this “over the top” support to help his mate do a Breech Tilt in the comfort of a bed!
nto the position you want your baby to be in. Inversions give a static stretch to uterine ligaments which, when followed by a swing back up to sitting tall over a neutral pelvis helps realign cervical ligaments and may make more room for the baby’s head. Start with a 30-seconds to 2 minutes of Forward-leaning Inversion.
- Breech Tilt: Follow the FLI with the Breech Tilt for 10-20 minutes.
 This allows you to tuck your chin while upside down on a similar slanted surface. Use an ironing board against the couch, for instance.
This allows you to tuck your chin while upside down on a similar slanted surface. Use an ironing board against the couch, for instance. - Open-knee Chest: Open-knee Chest has been studied and shown to help breeches flip. I like inversion positions that allow the mother to tuck her own chin. Myofascial workers tell me this relaxes her pelvis, whereas extending the chin tightens the pelvis.
- Professional bodywork: Acupuncture and Moxibustion both have good statistics for flipping breeches. Find out if there’s a Spinning Babies® Aware Practitioner in your area.
- Therapeutic massage: There are muscle/fascia attachments at the base of the skull, respiratory diaphragm, inguinal ligament, and even the hip sockets! We are whole organisms, not machines with reproductive parts.

- Chiropractic or Osteopathic: Spinal adjustmentsof the neck do improve pelvic alignment, especially if accompanied by fascial release. Not all chiropractors are trained in soft tissue body work, however. And not all soft tissue work is equal. This is why we promote our Aware Practitioner Workshops for bodyworkers.
Should manual external cephalic version be done earlier?
A few midwives recommend version (manually turning the breech baby to head down) at 30 –31 weeks. Anne Frye, author of Holistic Midwifery, reported a very low incidence of breech at term when her midwifery group manually rotated babies during this gestational age.
Attempting to turn the baby now is over a month before the medical model of turning breeches. Utmost gentleness must be the protective factor. If forcing a baby to turn harms the baby or placenta, the baby is too young to be cared for outside of the Neonatal Intensive Care Unit.
Midwives who turn babies now believe there is less chance of hurting a baby and proceed very carefully, stopping at once if there is resistance. Typically, there is less resistance from the uterus because there is more fluid and the baby is still very small.
Body work is suggested before attempting this, especially for first-time moms or women who had a difficult time with their first birth. There are risks to a manual version, so the baby should be monitored closely in between each 10-30 degrees of rotation.
35-36 weeksIf your baby is breech during this time your doctor or midwife will begin to talk about how to help the baby flip head down, and possibly about scheduling a manual version for 36-37 weeks. Getting body work and having acupuncture or homeopathy may help soften the ligaments and a tense uterus to either help the baby flip spontaneously or to allow more success in an attempt at a version.
Moxibustion has its highest success rate this week. 36-37 weeks
36-37 weeksDuring this time, you can continue with the suggestions in the “Professional Help” page. Also, an obstetrician may suggest manually flipping the baby to a head down position at this time. A few midwives will also offer this, perhaps even earlier, at 30-34 weeks.
NOTE: Don’t let someone manually flip your baby without using careful monitoring of the baby’s heartbeat. Accidents can occur, even when there is good intention. The baby must be listened to and the version stopped immediately if the heart rate drops.
External cephalic version near the end of pregnancy
You may also agree to go through with a cephalic version at this time. The baby is in the womb with the cord and placenta and there is a small risk in turning the baby manually. This maneuver should be done with monitoring by experienced professionals, in a setting ready for a cesarean if needed.
There is about a 40-50% chance this will be successful. Sometimes the baby moves easily and sometimes the procedure is painful. I believe it’s important who performs it, and that ligament tightness would make this more uncomfortable. I suggest getting chiropractic, myofascial, acupuncture, homeopathy, or moxibustion (or all of these) before and after the version.
Sometimes the baby moves easily and sometimes the procedure is painful. I believe it’s important who performs it, and that ligament tightness would make this more uncomfortable. I suggest getting chiropractic, myofascial, acupuncture, homeopathy, or moxibustion (or all of these) before and after the version.
Doing the Three Sisters of BalanceSM (or following the Turning Your Breech Baby guidelines) daily beforehand and just before the procedure would be relaxing and helpful. More birth professionals are using our approach in the hours or the week before the procedure and report that fewer procedures are necessary and those that are seem to be easier than average to do when the baby is able to be turned.
38-40 weeksSometimes a woman and her caregiver don’t know the baby is breech until this point or until labor. Rarely does a baby flip to breech this late in pregnancy but they can. Parents and providers may learn that baby is breech during a routine bio-physical ultrasound exam during this time or later in pregnancy.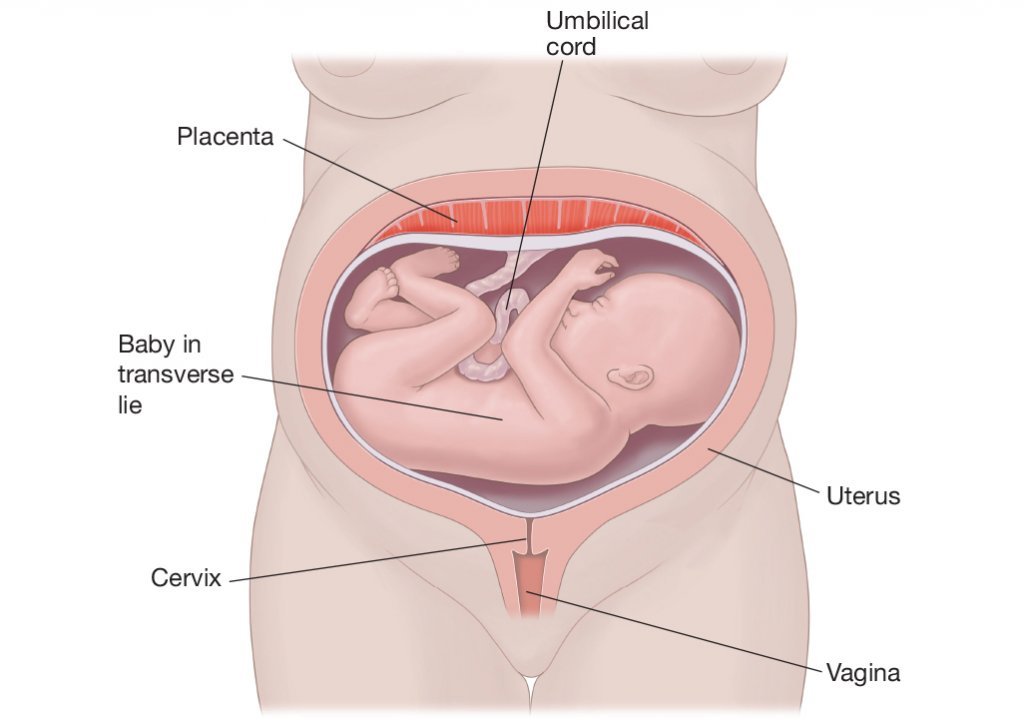
An external cephalic version may yet be successful, depending on the fluid level and the flexibility of the uterus, the baby’s head position and location, a uterine septum, where the placenta is, etc.
It is still possible that the baby flips doing body balancing activities or even labor itself (contractions might be the very action that turns baby in about 1% of breeches). You may find turning easier if you keep doing the activities listed above.
40-41 weeksThough many breeches are born about 37-39 weeks gestation, some will happily go to 41 or 42 weeks. For a head down baby, 41 weeks and 1 to 3 days is a common time for labor to begin on its own. SStarting labor at this gestation can certainly be normal for a healthy breechling, too.
If the pregnant person has a tendency to be somewhat overweight or lower energy, which can indicate low thyroid function, a longer pregnancy may be more likely. This tendency deserves looking after. Well-nourished and peppy women may also go a full pregnancy length, of course.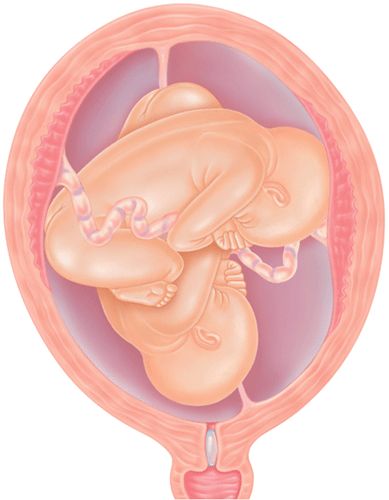
Going into labor and then having a planned cesarean is recommend by Dr. Michel Odent in his book, Cesarean. Going into labor spontaneously is safer for the breech vaginal birth, as well. Women who are trying to flip their baby often find it necessary to slow down the efforts and come to terms with a breech birth.
When facing a cesarean, it can be nurturing to you and your baby to plan a cesarean with skin-to-skin, delayed cord clamping, and breastfeeding on the operating room table or in the recovery room. Give yourself some time and compassion to feel your feelings and explore your options to adapt to the options you have available to you.
Postdates (after your due date) with a breechWith a breech, going all the way to 42 weeks may or may not be more of an issue. Some providers will have to end any plans for a vaginal birth by now. Midwifery statutes often limit midwifery care out of the hospital to 37-42 weeks (or 36-43, depending on where you live).
After 42 weeks, the baby’s skull bones are setting up more firmly and a vaginal birth is less favorable. I’ve been to a few breech births after 42 weeks gestation and everything went very well. But, I do sometimes wonder why labor isn’t starting and if metabolism is a reason, especially when there’s been regular bodywork for weeks.
For a person carrying a breech baby who does show signs of low thyroid function or otherwise a “sloshy” metabolism, I am inclined to transfer care to a kind hospital provider at 41.5 weeks. Intelligent and experienced monitoring may rule out issues that arise post dates that may complicate labor. With slow metabolism postdates issues with breech position may need extra attention before 42 weeks.
If Baby Does Not Turn
Not every breech baby will turn on their own. Not every attempt at an External Cephalic Version works (It’s often 50-50). Adding body balancing has abundant anecdotal reporting to show success. But this balancing should be individualized if the pregnant person has followed general guidelines closely for 1-2 weeks without success.
Be compassionate to you and your baby. You are both doing the best you can with the resources you have.
Choose your path. Sometimes it may feel like you don’t have a choice. Consider why it feels that way. Perhaps your choice is safety over manner of birth? That’s totally valid. Just because a vaginal birth might be available to some doesn’t mean it is your first choice, too.
Sometimes babies choose, too. The labor goes too fast to do surgery for the birth. Or, the baby doesn’t come into the pelvis and surgical birth is necessary. (Remember reaching in and pulling out the baby is not reasonable if a cesarean is available in the region unless this is a second twin (subsequent triplet) or travel is impossible due to weather, war, or whatever reason. Life is real. Babies don’t follow a script. Be real with your own experience.
Inducing a breech
Inducing a breech is not recommended in out of hospital settings. Even in the hospital, the risk rises. In some areas where breech is common, Pitocin/Syntocin inductions are done with outcomes that are good enough to keep the options open. Induction by herbs is also considered out of scope for breech.
Induction by herbs is also considered out of scope for breech.
We need to respect the breech and not stress the baby, especially in settings where we don’t have the rescue setup to solve any potential problems. Try body balancing and see if labor begins on its own. That would be a non-invasive, non-manipulating approach.
The Breech Turned During LaborIt is a rare possibility that the baby flips to head down during labor. I once assisted a midwife who’s laboring mother’s water had released. Her labor was mild and not picking up, so after 24 hours we transferred and found that the baby had flipped. The doctor thought we’d misdiagnosed, but the mother’s abdomen was so thin we could feel the baby’s knuckles and elbow and found the baby in the opposite direction after entering the hospital!
Another mother had Dynamic Body Balancing in early labor with one of Dr. Carol Phillips students who was also a midwife. Her breech baby turned head down during transition phase of labor!
If the plan is to have a cesarean once labor begins, call the hospital and alert them of labor immediately. Go to the hospital right away. Breech births can go quite quickly and you want to be where people are ready to help you. If you plan to have a vaginal birth, don’t delay in getting to your birth location or getting your birth team to you.
Go to the hospital right away. Breech births can go quite quickly and you want to be where people are ready to help you. If you plan to have a vaginal birth, don’t delay in getting to your birth location or getting your birth team to you.
While it can be totally normal to have a 24-hour or longer breech birth, many breech labors are quite short. Because the softer bottom is first, it may take you by surprise that you are progressing with such little pain (though some breech births are as painful as head down births). Just don’t base your decision to get to the hospital on your pain level!
A cesarean can be more complicated if the baby is wedged low in the pelvis. That is why there is a recommendation to have the cesarean in early labor. But cesareans are done everyday with head down babies low in the pelvis. Sometimes it’s how it is.
Starting labor in and of itself doesn’t make the surgery more dangerous. Rushing around and doing things in a hurry might. Alert your hospital before labor and again once you start labor. Be firm that you know what you are about and that they need to get the Operating Room ready while you are on your way.
Be firm that you know what you are about and that they need to get the Operating Room ready while you are on your way.
Mostly, a leisurely transition into the hospital can be sustained with a sense of humor and practicality. There can be a sense of calm while you and the staff take the steps to welcome your baby. This is your birth. Be present with how your experience unfolds.
After the birthWhile the concern about breech position is during the birthing, when the baby is breech for most of the third trimester, their skull bones become shaped by the inside of the upper womb (the fundus). This isn’t typically an issue but can be noticed.
Craniosacral therapy can gently (and without using force) reshape the baby’s head, ideally during the month or two after birth. Surgery on baby’s skull is seldom necessary after 3-6 sessions with a Craniosacral therapist. For most breech babies, this issue is not present. I list is here because I have heard some assumptions that can be dispelled.
A question about breech
Email from Wed, Feb 11, 2009:
…I’m 30 weeks and the baby is what I’d describe as oblique breech – his head is on my right side next to my belly button, his hips/butt are in my pelvis on the lower left side (my left) and his feet are in front of his face. I think he’s facing forward – towards my belly button. I’ve known this for weeks just because his big head is so hard I always bump that spot on accident. …. my first son was 9 lbs and born posterior, so I’m really hoping this baby is in the ideal position for delivery… so both of these things make me nervous that he won’t move. He has been in this position for a few weeks now. … Anyway, just wondering if I should worry and what, if anything, I can do to help him move now. My Midwife suggested a Chiropractor that can do some adjustments. I’d like to do the couch inversion too. Would it help for me to walk more? Also, should I sleep more on one side than the other? Thanks for your help! Great site!
Gail’s reply:
Hi….
now is a good time to take action, not so much that your baby is breech, but because your first baby was OP. You see, a pelvic misalignment and/or round ligament spasms (they often go together) can result in either a breech or a posterior fetal position. So, a breech will often flip to a posterior position and may stay that way unless you resolve the underlying issue. Maternal positioning is often not enough by itself to correct a posterior fetal position when there is a history of previous posterior or breech babies. While certainly most breech babies flip head down, it’s beneficial to help correct the symmetry of your uterine ligaments now, while the baby is still small enough to have plenty of room to flip head down once the reason for the previous posterior position is remedied. See some things a Chiropractor can do for breech and posterior by reading Professional Help.
Videos
Daily Essentials
Daily Essentials can be practiced daily throughout pregnancy to help bring balance and comfort — and an easier, shorter birth.
Learn More
Spinning Babies® Parent Class
Spinning Babies® Parent Class provides clear instructions on how to use Spinning Babies® for a more comfortable and confident pregnancy and labor.
Learn More
Featured Products
Shop Spinning Babies®
7 ways to turn a breech baby
You just found out your baby’s in the breech position and you’re panicking. Before you search the internet for “how to turn a breech baby,” read this.
First of all, don’t stress out. Just because your care provider thinks the baby is breech doesn’t mean you’ll automatically have to have a C-section, especially if you’re not yet 36 weeks along. Somewhere around the 34-week mark my midwife thought my son might be breech, and all of a sudden every midwife in the whole practice seemed to crowd into the exam room to chime in about acupuncture, yoga, confusing acronyms I’d never heard of, and something called moxibustion. I felt totally overwhelmed by all the options and techniques they were suggesting. (Eventually, an ultrasound revealed that what the midwives thought was the baby’s head was actually his bum—phew. Crisis averted.)
I felt totally overwhelmed by all the options and techniques they were suggesting. (Eventually, an ultrasound revealed that what the midwives thought was the baby’s head was actually his bum—phew. Crisis averted.)
It’s also important to know that the easiest technique for turning a breech baby is extremely low-effort: just give it time. Most babies do turn on their own before their due date. In fact, your chances of having a breech baby decrease with each passing week. While about 30 per cent of babies are breech at 30-32 weeks, only 3 per cent are still breech at term (37 weeks), says OB-GYN Ellen Giesbrecht, a doctor at BC Women’s Hospital in Vancouver.
You may have also heard that yoga positions, swimming, belly dancing, spending time upside down, or doing exercises like pelvic tilts can help. “Many of these are just about using the principle of gravity to get the baby’s bum up and out of the pelvis,” explains Giesbrecht.
Interestingly, the majority of babies will turn at night, when you’re sleeping, due to your reclined position. “Many moms don’t even notice when the baby turns,” says Ruth Comfort, a registered midwife at the South Community Birth Program and Assistant Head of Midwifery at BC Women’s Hospital and St. Paul’s Hospital in Vancouver.
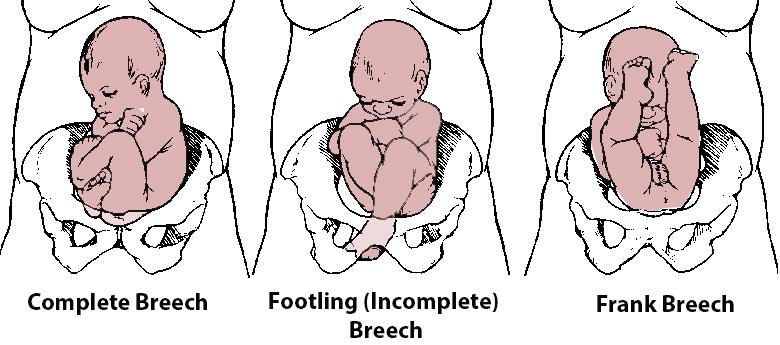
There are several types of breech presentation: frank breech (the baby’s bum—and not his head—is over your cervix, and his feet are way up near his face folded in a jackknife position instead of tucked in), footling breech (one or both feet are below the baby’s bum and sitting above your cervix) and complete breech (instead of being head-down, the baby’s bum is over your cervix, and his knees are tucked up against his chest, in a ball). Bum-first or feet-first is not the optimal position for a vaginal delivery. Many hospitals and OBs will not allow women to attempt vaginal breech births (though some do specialize in this—ask your provider), and midwives in Canada don’t typically deliver breech babies, either. Attempting a home birth with a breech baby is not recommended.
Midwife Ruth Comfort advises women to start by having a conversation with their provider about what kind of breech you’re dealing with. “That affects the efficacy of alternative techniques. It’s tricky because every woman is so different, and the reason her baby is breech may be different, too.”
First-time moms, or women who are extremely fit, may have more trouble getting a baby to move out of a breech position due to tighter pelvic and abdominal muscles, says Comfort. Women having a second or third child may have more luck with babies who turn spontaneously. (However, says Giesbrecht, “the more babies you have, the higher your chances of having a breech baby—that’s just statistics.”)
A uterine fibroid or the specific shape of your pelvis may mean the baby does not have room to turn, and that there’s little chance that any of the following methods will work. It could be that the cord is tangled around the baby’s leg or shoulder. (Unfortunately, this is not easily ascertained in an ultrasound, so sometimes there’s no way to know. ) It could be that the baby went through a growth spurt and got trapped in a bum-down position.
) It could be that the baby went through a growth spurt and got trapped in a bum-down position.
“If the cord isn’t an issue and the baby isn’t deeply engaged or wedged in the pelvis, the goal is to give the baby the space to turn on their own,” explains Comfort.
Here’s a breakdown of the most common techniques for turning a breech baby.
1. ECVThis intimidating-sounding acronym stands for external cephalic version, and it’s an intervention performed at a hospital, clinic or birth-care centre under ultrasound guidance. The doctor would use her hands to manipulate the baby’s position by carefully pushing on your belly and abdomen. ECV is usually best performed between 35-38 weeks, after nothing else has worked. The baby’s vital signs are monitored before and after the procedure. According to the medical literature, says Giesbrecht, ECV has about a 40 to 70 per cent success rate. But in her professional experience as an OB, she sees about a 50 per cent success rate. The procedure only takes a few minutes, but it can be very uncomfortable for women. “It’s painful,” says Giesbrecht, “but it’s less painful than recovering from a C-section if the baby does not turn.” Spinal epidurals for pain relief are an option, but your epidural would last much longer than the 2- to 5-minute ECV procedure. (Epidurals during ECV do not improve success rates, adds Giesbrecht.)
The procedure only takes a few minutes, but it can be very uncomfortable for women. “It’s painful,” says Giesbrecht, “but it’s less painful than recovering from a C-section if the baby does not turn.” Spinal epidurals for pain relief are an option, but your epidural would last much longer than the 2- to 5-minute ECV procedure. (Epidurals during ECV do not improve success rates, adds Giesbrecht.)
These are postures that Comfort recommends to all pregnant women for optimal fetal positioning as your due date approaches—whether you’re carrying a breech baby or not. For 10 to 15 minutes before bed, or while watching TV, rest in child’s pose or rock back and forth on your hands and knees, if you’re comfortable. This helps with relaxing the pelvic muscles and the gravitational pull inside your uterus. Comfort says that while this technique is not “evidence-based,” it’s also not harmful. You might also try some gentle pelvic rotations—gyrating your hips as if you’re trying to belly-dance—to encourage the baby to move around.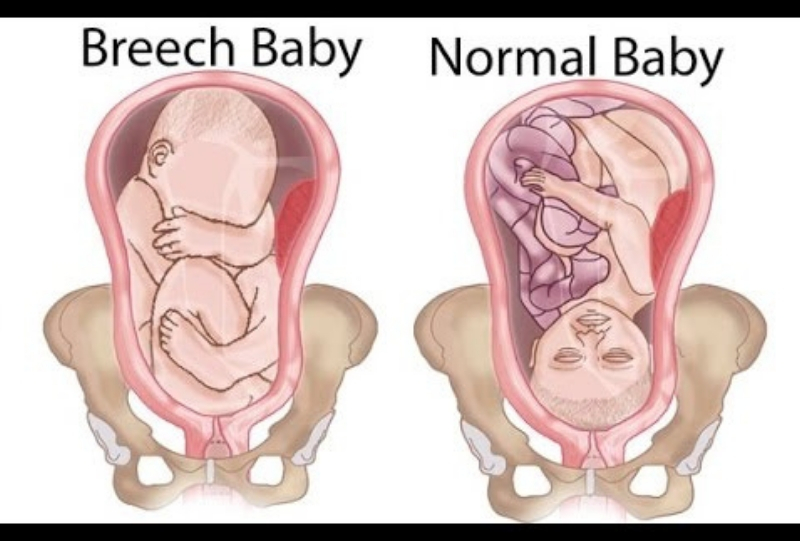
Moxibustion is a form of Chinese medicine and acupuncture, but instead of acupuncture needles, a practitioner applies gentle heat in the form of a mugwort stick, which looks a bit like a cigar. Only one end is lit, and the other (unlit!) end is gently applied to a pressure point on a pregnant woman’s baby toe (known as BL67). Giesbrecht, the OB, says that meta-analyses of acupuncture and moxibustion show there’s no adverse effects, but that these techniques aren’t necessarily proven to help, either. “There are no clear benefits or risks. It’s no better than waiting, but it does no harm,” she says.
Midwife Ruth Comfort, however, points to research from Europe. “There are some really good European studies proving efficacy of acupuncture on fetal position, as early as 32 weeks of gestation.”
4. Chiropractics: the Webster techniqueChiropractics and, more specifically, the Webster technique (you can watch videos online), are about addressing asymmetry in the pelvis and hipbones.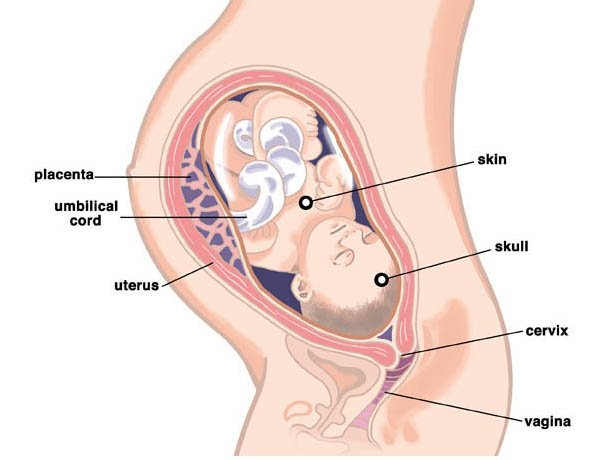 If you’re used to visiting a chiropractor regularly, ask him or her to check for tighter or shorter ligaments. “This method is about realigning the pelvis and optimizing space for fetal descent, but trust your instincts,” says Comfort. “Don’t do anything you’re not comfortable with.”
If you’re used to visiting a chiropractor regularly, ask him or her to check for tighter or shorter ligaments. “This method is about realigning the pelvis and optimizing space for fetal descent, but trust your instincts,” says Comfort. “Don’t do anything you’re not comfortable with.”
The breech tilt, or pelvic tilt, essentially means lying on the floor and raising your hips, with your feet planted on the ground and your knees bent. Or, some women position an ironing board so that one end is on the edge of a couch, and the other end is on the floor, creating a sloping bridge. Lie on the ironing board with your head resting on a pillow and your feet elevated, for a 20-minute period. (How you get your pregnant self onto, and off, this ironing board is definitely not going to be graceful. Ask for help.) “Other than the risk of a headache—and one of my patients busting an ironing board while she was lying on it—there are no adverse effects of this method,” Giesbrecht laughs.
Swimming, says Comfort, may not have proven results for turning breech babies, but can be quite relaxing for women. It’s therapeutic for tired joints and achy muscles late in pregnancy anyway, and it won’t hurt the baby.
7. MusicHave you heard old wives’ tales about playing music to your belly? The theory is that directing tunes toward the base of your bump might coax a baby whose head is near your ribs to turn toward a head-down (also known as vertex) position, closer to the cervix and birth canal. There is no medical evidence to support this method, however. “I’m not even going to comment on that,” says Giesbrecht.
What happens if you have to give birth to a breech babyDepending on how many weeks pregnant you are, and what kinds of alternative therapies you’re comfortable with, you may consider all—or none—of the above suggestions before it’s time to adapt your birth plan.
“Between 34 and 36 weeks we encourage as many natural techniques as you want to try—that, plus simply giving it time,” says Comfort. “It’s only at the 36- or 37-week mark that you’d book an ECV, begin to plan a C-section, or pursue a vaginal breech birth, if it’s an option for you.”
This can, of course, be frustrating: after a pregnancy that felt like smooth sailing, a flurry of decisions may need to be made last-minute, depending on fetal size, breech position, and—once the big day arrives—the length of your labour. Some pregnant women have difficulty adjusting to the reality that they can no longer go forward with the kind of birth they’d always envisioned.
“There’s a lot of grief around giving up the idea that you’re low-risk, that you’re no longer having a ‘normal’ pregnancy, and that you can’t have the delivery you expected,” says Comfort. “But I tell my patients not to worry too much and not to feel guilty if the baby won’t turn. Trust the baby—he or she may be breech for a good reason. ”
”
Watch Baby Grow!
Subscribe to Today’s Parent’s baby newsletter and find out what to expect for every stage and milestone, from birth to two years.- Email*
- Baby's due/birth date*
Month223456789101112
Day12345678910111213141516171819202122232425262728293031
Year2024202320222021
- CAPTCHA
- Consent*
Yes, I would like to receive Today's Parent's Baby newsletter. I understand I can unsubscribe at any time.**
FILED UNDER: C-section Giving birth health service seo Labour and delivery Pregnancy
Breech presentation - how to turn the baby
Vatagina Maria Alexandrovna
Obstetrician-gynecologist
Lapino-1 Clinical Hospital "Mother and Child"
Do not worry and worry if a child under 36 weeks is "ass forward": this is completely normal and the crumbs still have time to roll over.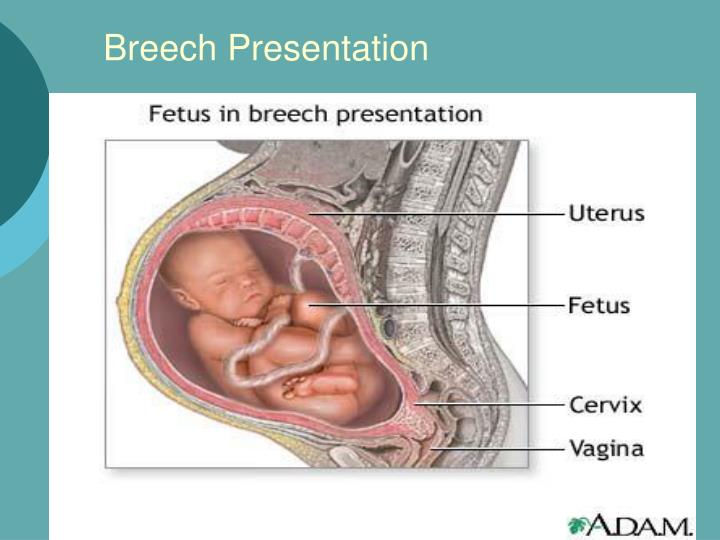 By the way, it happens that the baby turns upside down and immediately before the birth, and even in the birth itself
By the way, it happens that the baby turns upside down and immediately before the birth, and even in the birth itself
Try to get the baby to turn into the desired position. Tell everything in detail: why he should turn around, what it will give both mother and child in childbirth. You can talk out loud, or you can talk to yourself, the main thing is to talk to the baby about it all the time
In the water, the mother’s body relaxes, which means that the muscles of the uterus relax, its volume increases somewhat, and as a result, the child has a little more space “for maneuvers ".
Talk to him
There is always a connection between a child and a mother. And mother is the first person whom the baby believes and obeys. Therefore, try to persuade the baby to turn into the desired position. Tell everything in detail: why he should turn around, what it will give both mother and child in childbirth. You can talk out loud, or you can talk to yourself, the main thing is to talk to your baby about it all the time. Be gentle and at the same time persistent. Be sure to connect the future dad to the conversation, children obey men even more. When you persuade the baby, additionally stroke the stomach, as if instructing the child how to turn around. Great option: dad talks and strokes his stomach with you.
Be gentle and at the same time persistent. Be sure to connect the future dad to the conversation, children obey men even more. When you persuade the baby, additionally stroke the stomach, as if instructing the child how to turn around. Great option: dad talks and strokes his stomach with you.
Imagine
Visualization is a way in which a person imagines a picture he needs. So the expectant mother just needs to imagine the baby in the right position. If you don't know what it looks like or you just can't imagine a baby in your belly - find a beautiful photo from a magazine, book, Internet. Some kind of anatomical accuracy is not important here, just a pleasant and understandable picture is enough: the baby lies upside down inside the mother's belly. Look at the illustration more often and imagine that inside you the baby is also in the correct position. But you must not only look at someone else's photo, but imagine yourself and your child.
Lure him
Another way is to lure the baby. Children, especially small ones, are very curious, so make the baby turn around by showing him something interesting. But the baby is still in the stomach, how can he see something? We do not know exactly how the baby reacts to the world outside the mother's stomach, but it is believed that he, for example, can hear sounds. Place headphones with pleasant music in the lower abdomen, this can also encourage the child to turn towards the sound. Music should be calm, melodic and not loud so that the baby is not scared.
Children, especially small ones, are very curious, so make the baby turn around by showing him something interesting. But the baby is still in the stomach, how can he see something? We do not know exactly how the baby reacts to the world outside the mother's stomach, but it is believed that he, for example, can hear sounds. Place headphones with pleasant music in the lower abdomen, this can also encourage the child to turn towards the sound. Music should be calm, melodic and not loud so that the baby is not scared.
You can also turn on the flashlight and put it against the mother's stomach in the place where the baby's head is, and then, while talking, slowly move the flashlight to the side and down, dragging the baby along with you.
Swim and relax
Swimming also helps your baby get into head presentation. In the water, the mother’s body relaxes, which means that the muscles of the uterus also relax, its volume increases somewhat, and as a result, the child has a little more space “for maneuvers”. But swimming should be pleasant for mom, if a woman is afraid of water or she is not warm enough, then there will be no relaxation. Therefore, you must want to swim, plus the water must be at a comfortable temperature.
But swimming should be pleasant for mom, if a woman is afraid of water or she is not warm enough, then there will be no relaxation. Therefore, you must want to swim, plus the water must be at a comfortable temperature.
Do the exercises
There are very simple exercises , that will help the baby to fit correctly. But first, check with your doctor if you can do such exercises. Gymnastics to turn the baby into head presentation is not carried out if there is gestosis, the threat of termination of pregnancy, a scar on the uterus after a previous cesarean section, placenta previa.
Turns. Lying on the couch, turn from side to side 3-4 times in 10 minutes. Perform 3 times a day. The turn usually occurs within the first week.
Force of attraction. Lie on your back with a large pillow under your lower back and a small one under your head. Bend your knees, placing your feet on the floor. Lie like this for 10 minutes.
Knee-elbow position. Stand on your knees and elbows, at this time the pelvis is located above the head. Stay in this position for 15 minutes several times a day.
Stand on your knees and elbows, at this time the pelvis is located above the head. Stay in this position for 15 minutes several times a day.
Consult a specialist
If exercises and psychological methods do not work, there is another way – prophylactic external rotation performed by an experienced obstetrician-gynecologist in the maternity hospital. First, the mother is injected with drugs that relax the uterus, then the doctor tries to turn the child with certain hand movements, acting on his head and pelvis through the belly of the expectant mother. All this takes place under the control of ultrasound, and usually a woman does not experience any discomfort during this manipulation.
True, external rotation is now rarely performed: firstly, not all obstetricians and gynecologists can do it, and not all doctors believe that it is needed; secondly, not every woman is psychologically tuned in to him, and, besides, there are not always indications for him.
Psychological methods may seem questionable, but they often help. And if you add gymnastics and swimming, then the likelihood that the baby will turn into the correct position only increases. So if you don’t want to do a cesarean section with a breech presentation or give birth “ass first”, then you should try all the methods that are suitable and allowed for you.
Make an appointment
to the doctor - Vatagina Maria Aleksandrovna
Lapino-1 Clinical Hospital "Mother and Child"
Gynecology
By clicking on the submit button, I consent to the processing of personal data
consequences for the child in case of incorrect position
January 18, 2022
18.01
5 min.
47728
36
6
Breech presentation for most expectant mothers is a very disturbing moment - how the child will be born, is a caesarean section always indicated in such cases, what complications are possible. Let's answer these and many other questions in this article.
Let's answer these and many other questions in this article.
Breech presentation of the fetus is one of the options for the location of the child in the uterus of the mother. If we could look into a woman's belly, we would see a child who seems to be "sitting" in the uterus, and his head is pointing up. Normally, breech presentation lasts up to 32 weeks, and then the baby, as a rule, turns over and directs the head to the birth canal.
Article content
- Can a woman determine the presentation of the fetus?
- What is breech presentation
- Common causes of presentation
- How to determine breech presentation
- What to do to make the child roll over
- What can a woman do
- What can an obstetrician do
- What can a doctor do
- FAQ
Can a woman identify fetal presentation?
Only an experienced doctor who leads the pregnancy can determine the breech presentation, and the assumption is confirmed with the help of ultrasound.
In the event that the baby is positioned “incorrectly”, the doctor may recommend special exercises to turn the baby over into the optimal position for childbirth. This is important, because it is at 32-34 weeks that you need to undergo an examination and make sure that the baby has taken the right direction.
What is breech presentation
Doctors distinguish two types of breech presentation:
| Gluteal | In such a situation, during childbirth at the birth of a baby, the buttocks are the first to be born. The legs are located along the body. This option is the most favorable, rarely gives complications, so childbirth is most often carried out naturally. |
| foot | At birth, the legs appear first, such a presentation. |
Common causes of presentation
Of course, any expectant mother has a question - why does breech presentation occur. There are many reasons for this, the main ones are:
There are many reasons for this, the main ones are:
- multiple pregnancy - when there are two or three babies in the uterus, it is difficult for them to move and turn over head down
- polyhydramnios - in such a situation, the baby can move a lot and simply not take the correct position before childbirth
- oligohydramnios - in a situation where there is little amniotic fluid, the child simply cannot take the correct position
- cord entanglement
- fibroids or other diseases of the uterus
How to determine breech presentation
It is impossible to independently determine the position of the child.
To understand what kind of presentation a child has, you can use:
| Visual examination and palpation of the abdomen by an experienced specialist | So he determines where the head is and where the legs of the fetus are |
| Feeling the baby through the vagina | This method is used if a woman has entered an emergency delivery and is already in them. |
| ultrasound | The most reliable way to determine the position of the baby. The procedure is carried out at 32-34 weeks, when the baby takes its final position |
Example
A pregnant woman at 38 weeks was diagnosed with breech presentation. The woman was advised certain exercises in order to delicately turn the fetus over. The task was unsuccessful, so the specialist tried to make an obstetric coup, however, this did not lead to the desired result. As a result, the doctor decided to carry out the delivery by surgery and perform a caesarean section. The operation was successful, mother and child are doing well.
How to make a child roll over
In this matter, three directions need to be considered: what the woman herself can do, what her obstetrician-gynecologist can do, and what the doctor in charge of childbirth can do.
What a woman can do
Let's figure out what may depend on the future mother herself, and what she can do.
- First, tune in a positive way. The state of the child largely depends on the psychological state of the mother, so it is not recommended to be nervous and anxious.
- Second, talk to your child and ask him to roll over. Skeptics may scoff at such advice, but experienced psychologists and obstetricians say that this method works.
- And finally, do special exercises, for example, turns. Starting position - lying on your back, legs slightly bent at the knees. Gently and smoothly, without jerking, you need to turn on your right side and lie down in this position for 2 minutes. After that, roll over to your left side and also lie down. Repeat 5 times for each side. All movements should be as delicate as possible.
What a midwife can do
If mom did not succeed in stimulating the coup, this is absolutely normal. At a period of more than 35 weeks, an obstetrician takes over, who tries to make the so-called obstetric coup. During the procedure, with the help of special manipulations, he acts on the woman's stomach, trying to give the fetus the optimal position for childbirth. However, it is impossible not to notice that most of the babies "inverted by the midwife" will soon return to the breech presentation.
However, it is impossible not to notice that most of the babies "inverted by the midwife" will soon return to the breech presentation.
What a doctor can do
Quite often, in order to reduce the risks for both the mother and her baby, the doctor decides to perform a caesarean section. However, many women give birth naturally.
The choice of birth management is always personalized, taking into account the individual characteristics of the mother and her child. It is important to choose a good specialist at the initial stage of pregnancy.
FAQ
Breech presentation of the fetus at the 20th week of pregnancy - is it dangerous?
+
Absolutely not. We begin to talk about the fact that breech presentation is a conditional pathology no earlier than 32 weeks. Until this time, the child may roll over, and sometimes more than once. I will say even more - at this time the child is most often located with his legs down and this is absolutely normal.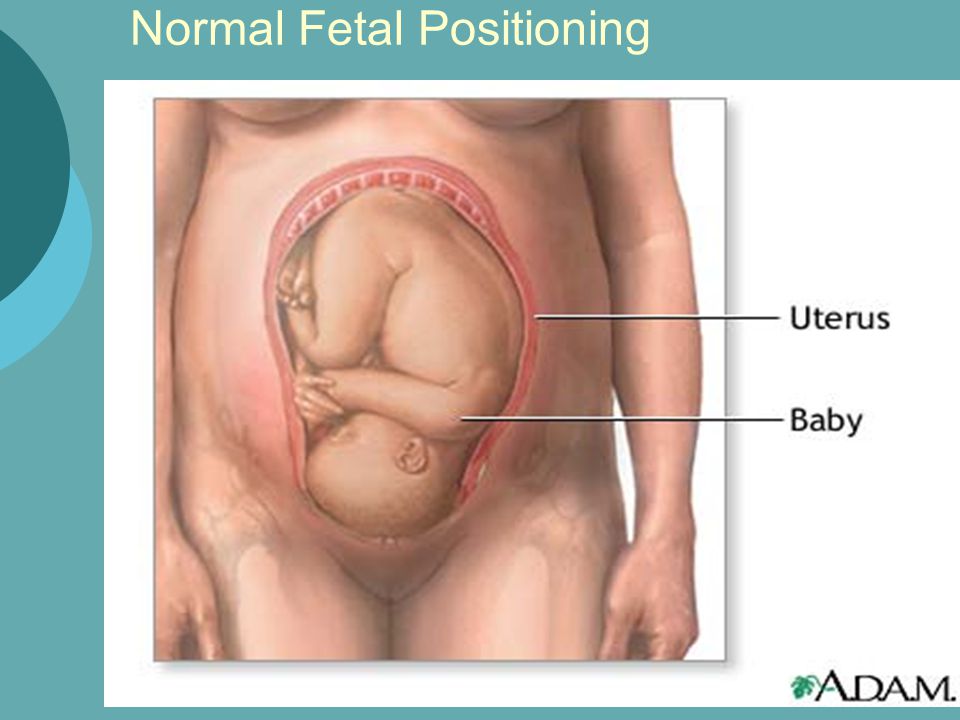
Foot presentation - is it the wrong position of the fetus?
+
What gestational age are we talking about? Initially, the child “tumbles” in his mother’s stomach, then most often he is just the same in a foot or breech presentation, when his legs are down and his head is up. And only closer to childbirth, a coup usually occurs and the child is located head down - at the entrance to the birth canal. If this does not happen, we can talk about the breech / foot / breech presentation.
What are the consequences of breech presentation for a child?
+
In general, with the correct management of childbirth, there will be no negative consequences for the child. He can suffer only if the doctor chooses the wrong method of obstetric care. In all other respects, there are no problems, the fetus develops absolutely normally.
How to understand that the child turned upside down?
+
The position of the child in the womb can only be determined by a competent specialist. The most effective and reliable method is ultrasound.
The most effective and reliable method is ultrasound.
And is there an unstable position of the fetus?
+
The fetus rotates many times during the entire pregnancy, at the end of the third trimester it usually turns head down and takes this position until delivery. However, it also happens that the child rolls over several times. In this case, we can talk about the unstable position of the fetus.
What is an obstetric revolution?
+
During the procedure, with the help of special manipulations, he acts on the woman's stomach, trying to give the fetus the optimal position for childbirth. However, it is impossible not to notice that most of the babies "inverted by the midwife" will soon return to the breech presentation.
Breech presentation of the fetus at 34 weeks of gestation - normal or pathological?
+
Breech presentation at this time is not a "final verdict.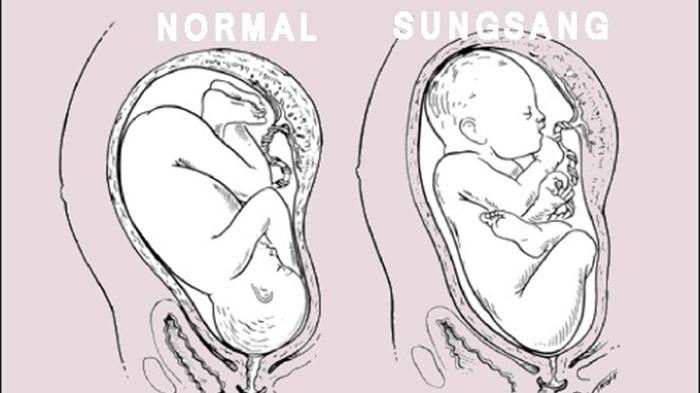 " the baby can still roll over. If this does not happen, the doctor will assess the size and position of the child closer to the MDD and decide on the tactics of childbirth.
" the baby can still roll over. If this does not happen, the doctor will assess the size and position of the child closer to the MDD and decide on the tactics of childbirth.
How to understand if the child turned upside down?
+
You yourself will not be able to understand this, or at least be sure that the coup has happened. I would recommend that you do an ultrasound - with the help of this study it will become known in which presentation your baby is.
We publish only verified information
Article author
Menshikova Maria Viktorovna obstetrician-gynecologist
Experience 38 years
Consultations 1816
Art. 46
46
Specialist with extensive practical experience. He has a certificate of a mammologist, a certificate of professional certification. Participates in foreign business trips and individual training programs (Los Angeles).
- 1982 - 1986 NPO MONIIAG - obstetrician-gynecologist
- 1987 - 1989 VNITs OZMIR - obstetrician-gynecologist
- 1989 - 1992 departmental polyclinic st. Moscow - Kurskaya - obstetrician-gynecologist
- 1992 - 2001 NPO MONIIAG - obstetrician-gynecologist
- 2007 - 2008 NP KMIKM - doctor administrator
- 2009 - 2013 Pereslavl Central District Hospital, women's consultation - obstetrician-gynecologist
- 2020 to present Teledoctor24 LLC - doctor - consultant (gynecologist)
Sources
- ... Savelyeva G.M., Shalina R.I., Panina O.B.
 "Obstetrics" - M .: "GEOTAR - Media", 2010
"Obstetrics" - M .: "GEOTAR - Media", 2010 - ... Chernukha E.A., Puchko T.K. "Pelvic presentation of the fetus", a guide for doctors - M .: "GEOTAR - Media", 2007
- ... Clinical protocol "Management of pregnancy and childbirth in breech presentation of the fetus" // Institute of Health and Family. Project "Mother and Child" - 2011
Share:
Category: Pregnancy and childbirth
About health Pregnancy and childbirth About children healthy lifestyle Psychology Neurology Gastroenterology Personal care Medicines and dietary supplementsPrevious article
Salt room
Next article
Diastasis after childbirth
Other related articles
Cherepenko Lyudmila Vikentievna
12.