How many joules to defibrillate a child
Defibrillation in children - PMC
1. Atkins DL, Everson-Stewart S, Sears GK, Daya M, Osmond MH, Warden CR, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: The Resusctation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009;119:1484–91. [PMC free article] [PubMed] [Google Scholar]
2. Mogayzel C, Quan L, Graves JR, Tiedeman D, Fahrenbruch C, Herndon P. Out-of-hospital ventricular fibrillation in children and adolescents: causes and outcome. Ann Emerg Med. 1995;25:484–91. [PubMed] [Google Scholar]
3. Hickey RW, Cohen DM, Strausbaugh S, Dietrich AM. Pediatric patients requiring CPR in the prehospital setting. Ann Emerg Med. 1995;25:495–501. [PubMed] [Google Scholar]
4. Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–7. [PubMed] [Google Scholar]
5. Samson RA, Nadkarni VM, Meaney PA, Carey SM, Berg MD, Berg RA. Outcomes of in-hospital ventricular fibrillation in children. N Engl J Med. 2006;354:2328–39. [PubMed] [Google Scholar]
6. Cummins RO. CPR and ventricular fibrillation: lasts longer, ends better. Ann Emerg Med. 1995;25:833–6. [PubMed] [Google Scholar]
7. Acosta P, Varon J, Sternbach GL, Baskett P. Kouwenhoven, Jude and Knickerbocker: The introduction of defibrillation and exteranl chest compressions into modern resuscitation. Resuscitation. 2005;64:139–43. [PubMed] [Google Scholar]
8. Moulton C, Dreyer C, Dodds D, Yates DW. Placement of electrodes for defibrillation - a reveiw of the evidence. Eur J Emerg Med. 2000;7:135–43. [PubMed] [Google Scholar]
9. Sternbach GL, Varon J, Fromm RE. The resuscitation greats. Claude Beck and ventricular defibrillation. Resuscitation. 2000;44:3–5. [PubMed] [Google Scholar]
10. Lown B, Amarasingham R, Neuman J. New method for terminating cardiac arrhythmias. Use of synchronized capacitor discharge. JAMA. 1962;182:548–55. [PubMed] [Google Scholar]
11. Lown B, Neuman J, Amarasingham R, Berkovits BV. Comparison of alternating current with direct electroshock across the closed chest. Am J Cardiol. 1962;10:223–33. [PubMed] [Google Scholar]
Lown B, Neuman J, Amarasingham R, Berkovits BV. Comparison of alternating current with direct electroshock across the closed chest. Am J Cardiol. 1962;10:223–33. [PubMed] [Google Scholar]
12. Stults KR, Brown DD, Schug VL, Bean JA. Prehospital defibrillation performed by emergency medical technicians in rural communities. N Engl J Med. 1984;310:219–23. [PubMed] [Google Scholar]
13. Lerman BB, Deale OC. Relation between transcardiac and transthoracic current during defibrillation in humans. Circ Res. 1990;67:1420–6. [PubMed] [Google Scholar]
14. Caterine MR, Yoerger DM, Spencer KT, Miller SG, Kerber RE. Effect of electrode position and gel-application technique on predicted transcardiac current during transthoracic defibrillation. Ann Emerg Med. 1997;29:588–95. [PubMed] [Google Scholar]
15. Mower MM, Mirowski M, Spear JF, Moore EN. Patterns of ventricular activity during catheter defibrillation. Circulation. 1974;49:858–61. [PubMed] [Google Scholar]
16. Zipes DP, Fischer J, King RM, Nicoll AD, Jolly WW. Termination of ventricular fibrillation in dogs by depolarizing a critical amount of myocardium. Am J Cardiol. 1975;36:37–44. [PubMed] [Google Scholar]
Termination of ventricular fibrillation in dogs by depolarizing a critical amount of myocardium. Am J Cardiol. 1975;36:37–44. [PubMed] [Google Scholar]
17. Chen PS, Swerdlow CD, Hwang C, Karagueuzian HS. Current concepts of ventricular defibrillation. J Cardiovasc Electrophysiol. 1998;9:553–62. [PubMed] [Google Scholar]
18. Schneider T, Martens PR, Paschen H, Kuisma M, Wolcke B, Gliner BE, et al. Multicenter, randomized, controlled trial of 150-J biphasic shocks compared with 200- to 360-J monophasic shocks in the resuscitation of out-of-hospital cardiac arrest victims. Optimized Response to Cardiac Arrest (ORCA) Investigators. Circulation. 2000;102:1780–7. [PubMed] [Google Scholar]
19. Martens PR, Russell JK, Wolcke B, Paschen H, Kuisma M, Gliner BE, et al. Optimal response to cardiac arrest study: defibrillation waveform effects. Resuscitation. 2001;49:233–43. [PubMed] [Google Scholar]
20. Hess EP, Atkinson EJ, White RD. Increased prevalence of sustained return of spontaneous circulation following transition to biphasic waveform defibrillation. Resuscitation. 2008;77:39–45. [PubMed] [Google Scholar]
Resuscitation. 2008;77:39–45. [PubMed] [Google Scholar]
21. Kudenchuk PJ, Cobb LA, Copass MK, Olsufka M, Maynard C, Nichol G. Transthoracic incremental monophasic versus biphasic defibrillation by emergency responders (TIMBER): A randomized comparison of monophasic with biphasic waveform ascending energy defibrillation for the resuscitation of out-of-hospital cardiac arrest due to ventricular fibrillation. Circulation. 2006;114:2010–8. [PubMed] [Google Scholar]
22. Clark CB, Zhang Y, Davies LR, Karlsson G, Kerber RE. Pediatric transthoracic defibrillation: biphasic versus monophasic waveforms in an experimental model. Resuscitation. 2001;51:159–63. [PubMed] [Google Scholar]
23. Berg RA, Chapman FW, Berg MD, Hilwig RW, Banville I, Walker RG, et al. Attenuated adult biphasic shocks compared with weight-based monophasic shocks in a swine model of proplonged pediatric ventricular fibrillation. Resuscitation. 2004;61:189–97. [PubMed] [Google Scholar]
24. Berg MD, Banville IL, Chapman FW, Walker RG, Gaballa MA, Hilwig RW, et al. Attenuating the defibrillation dosage decreases postresuscitation myocardial dysfunction in a swine model of pediatric ventricular fibrillation. Pediatr Crit Care Med. 2008;9:429–34. [PMC free article] [PubMed] [Google Scholar]
Attenuating the defibrillation dosage decreases postresuscitation myocardial dysfunction in a swine model of pediatric ventricular fibrillation. Pediatr Crit Care Med. 2008;9:429–34. [PMC free article] [PubMed] [Google Scholar]
25. Geddes LA, Tacker WA, Rosborough JP, Moore AG, Cabler PS. Electrical dose for ventricular defibrillation of large and small animals using precordial electrodes. J Clin Invest. 1974;53:310–9. [PMC free article] [PubMed] [Google Scholar]
26. Tacker WA, Jr, Ewy GA. Emergency defibrillation dose: Recommendations and rationale. Circulation. 1979;60:223–5. [PubMed] [Google Scholar]
27. Tacker WA, Guinn GA, Geddes LA, Bourland JD, Korompai FL, Rubio PA. The electrical dose for direct ventricular defibrillation in man. J Thorac Cardiovas Surg. 1978;75:224–6. [PubMed] [Google Scholar]
28. Gutgesell HP, Tacker WA, Geddes LA, Davis JS, Lie JT, McNamara DG. Energy dose for ventricular defibrillation of children. Pediatrics. 1976;58:898–901. [PubMed] [Google Scholar]
29. Atkins DL, Jorgenson DB. Attenuated pediatric electrode pads for automated external defibrillator use in children. Resuscitation. 2005;66:31–7. [PubMed] [Google Scholar]
Atkins DL, Jorgenson DB. Attenuated pediatric electrode pads for automated external defibrillator use in children. Resuscitation. 2005;66:31–7. [PubMed] [Google Scholar]
30. Berg MD, Samson RA, Meyer RJ, Clark LL, Valenzuela TD, Berg RA. Pediatric defibrillation doses often fail to terminate prolonged out-of-hospital ventricular fibrillation in children. Resuscitation. 2005;67:63–7. [PubMed] [Google Scholar]
31. Rodriguez-Nunez A, Lopez-Herce J, Garcia C, Dominguez P, Carrillo A, Bellon JM, et al. Pediatric defibrillation after cardiac arrest: initial response and outcome. Crit Care. 2006;10:R113. [PMC free article] [PubMed] [Google Scholar]
32. Rossano JW, Quan L, Kenney MA, Rea TD, Atkins DL. Energy dosing for attempted defibrillation of out of hospital pediatric ventricular fibrillation. Resuscitation. 2006;70:80–9. [PubMed] [Google Scholar]
33. Biarent D, Bingham R, Richmond S, Maconochie I, Wyllie J, Simpson S, et al. European Resuscitation Council guidelines for resuscitation 2005. Section 6. Paediatric life support. Resuscitation. 2005;67:S97–133. [PubMed] [Google Scholar]
Section 6. Paediatric life support. Resuscitation. 2005;67:S97–133. [PubMed] [Google Scholar]
34. Babbs CF, Tacker WA, VanVleet JF, Bourland JD, Geddes LA. Therapeutic indices for transchest defibrillator shocks: effective, damaging, and lethal electrical doses. Am Heart J. 1980;99:734–8. [PubMed] [Google Scholar]
35. Gaba DM, Talner NS. Myocardial damage following transthoracic direct current countershock in newborn piglets. Pediatr Cardiol. 1982;2:281–8. [PubMed] [Google Scholar]
36. Berg RA. Attenuated adult biphasic shocks for prolonged pediatric ventricular fibrillation: Support for pediatric automated defibrillators. Crit Care Med. 2004;32:S352–5. [PubMed] [Google Scholar]
37. Tang W, Weil MH, Jorgenson D, Klouche K, Morgan C, Yu T, D, et al. Fixed-energy biphasic waveform defibrillation in a pediatric model of cardiac arrest and resuscitation. Crit Care Med. 2002;30:2736–41. [PubMed] [Google Scholar]
38. Gurnett CA, Atkins DL. Successful use of a biphasic waveform automated external defibrillator in a high-risk child. Am J Cardiol. 2000;86:1051–3. [PubMed] [Google Scholar]
Am J Cardiol. 2000;86:1051–3. [PubMed] [Google Scholar]
39. Bar-Cohen Y, Walsh E, Love B, Cecchin F. First appropriate use of automated external defibrillator in an infant. Resuscitation. 2005;67:135–7. [PubMed] [Google Scholar]
40. Divekar A, Soni R. Successful parental use of an automated external defibrillator for an infant with Long-QT Syndrome. Pediatrics. 2006;118:e-526–9. [PubMed] [Google Scholar]
41. ECC Committee, Task Forces of the American Heart Association. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112:13. [PubMed] [Google Scholar]
42. Stiell IG, Walker RG, Nesbitt LP, Chapman FW, Cousineau D, Christenson J, et al. BIPHASIC Trial. A randomized comparison of fixed lower versus escalating higher energy levels for defibrillation in out-of-hospital cardiac arrest. Circulation. 2007;115:1511–7. [PubMed] [Google Scholar]
43. Atkins DL, Kerber RE. Pediatric defibrillation: Current flow is improved by using “adult” paddle electrodes. Pediatrics. 1994;94:90–3. [PubMed] [Google Scholar]
Pediatrics. 1994;94:90–3. [PubMed] [Google Scholar]
44. Atkins DL, Sirna S, Kieso R, Charbonnier F, Kerber RE. Pediatric defibrillation: Importance of paddle size in determining transthoracic impedance. Pediatrics. 1988;82:914–8. [PubMed] [Google Scholar]
45. Samson RA, Atkins DL, Kerber RE. Optimal size of self-adhesive preapplied electrode pads in pediatric defibrillation. Am J Cardiol. 1995;75:544–5. [PubMed] [Google Scholar]
46. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112:IV1–203. [PubMed] [Google Scholar]
47. Cornwell L, Mukherjee R, Kelsall AW. Problems with the use of self-adhesive electrode pads in neonates. Resuscitation. 2006;68:425–8. [PubMed] [Google Scholar]
48. Garcia LA, Kerber RE. Transthoracic defibrillation: does electrode adhesive pad position alter transthoracic impedance? Resuscitation. 1998;37:139–43. [PubMed] [Google Scholar]
49. Dodd TE, Deakin CD, Petley GW, Clewlow F. External defibrillation in the left lateral position-a comparison of manual paddles with self-adhesive pads. Resuscitation. 2004;63:283–6. [PubMed] [Google Scholar]
External defibrillation in the left lateral position-a comparison of manual paddles with self-adhesive pads. Resuscitation. 2004;63:283–6. [PubMed] [Google Scholar]
50. Deakin CD, Sado DM, Petley GW, Clewlow F. Is the orientation of the apical defibrillation paddle of importance during manual external defibrillation? Resuscitation. 2003;56:15–8. [PubMed] [Google Scholar]
51. Diack AW, Welborn WS, Rullman RG, Walter CW, Wayne MA. An automatic cardiac resuscitator for emergency treatment of cardiac arrest. Med Instrum. 1979;13:78–83. [PubMed] [Google Scholar]
52. Weisfeldt ML, Kerber RE, McGoldrick RP, Moss AJ, Nichol G, Ornato JP, et al. Public access defibrillation - A statement for healthcare professionals from the American Heart Association Task Force on Automatic External Defibrillation. Circulation. 1995;92:2763. [PubMed] [Google Scholar]
53. Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, et al. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–46. [PubMed] [Google Scholar]
N Engl J Med. 2004;351:637–46. [PubMed] [Google Scholar]
54. Sanna T, La Torre G, de Waure C, Scapigliati A, Ricciardi W, Dello Russo A, et al. Cardiopulmonary resuscitation alone vs. cardiopulmonary resuscitation plus automated external defibrillator use by non-healthcare professionals: A meta-analysis on 1583 cases of out-of-hospital cardiac arrest. Resuscitation. 2008;76:226–32. [PubMed] [Google Scholar]
55. Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206–9. [PubMed] [Google Scholar]
56. Atkins DL, Hartley LL, York DK. Accurate recognition and effective treatment of ventricular fibrillation by automated external defibrillators in adolescents. Pediatrics. 1998;101:393–7. [PubMed] [Google Scholar]
57. Cecchin FC, Perry JC, Berul CI, Jorgenson DB, Duncan BW, Lyster T, et al. Is AED arrhythmia detection accurate for children? Sensitivity and specificity of an AED algorithm in 696 pediatric arrhythmias. Circulation. 2001;103:2483–8. [PubMed] [Google Scholar]
Circulation. 2001;103:2483–8. [PubMed] [Google Scholar]
58. Atkinson E, Mikysa B, Conway JA, Parker M, Christian K, Deshpande J, et al. Specificity and sensitivity of automated external defibrillators rhythm analysis in infants and young children. Ann Emerg Med. 2003;42:185–96. [PubMed] [Google Scholar]
59. Atkins DL, Scott WA, Blaufox AD, Law IH, Dick II M, Geheb F, et al. Sensitivity and specificity of an automated external defibrillator algorithm designed for pediatric patients. Resuscitation. 2008;76:168–74. [PubMed] [Google Scholar]
60. Samson RA, Berg RA, Bingham R, Biarent D, Coovadia A, Hazinski MF, et al. Use of automated external defibrillators for children: An update: An Advisory Statement From the Pediatric Advanced Life Support Task Force, International Liaison Committee on Resuscitation. Circulation. 2003;107:3250–5. [PubMed] [Google Scholar]
Automatic external defibrillation in a 6 year old
Article Text
Article menu
- Article
Text - Article
info - Citation
Tools - Share
- Rapid Responses
- Article
metrics - Alerts
Acute paediatrics
Automatic external defibrillation in a 6 year old
- B König1,
- J Benger2,
- L Goldsworthy1
- 1Department of Paediatric Emergency Medicine, Bristol Royal Hospital for Children, UK
- 2Department of Emergency Medicine, Bristol Royal Infirmary, UK
- Correspondence to:
Dr J Benger
Paediatric Emergency Department. Bristol Royal Hospital For Children, Paul O’Gorman Building, Upper Maudlin Street, Bristol BS2 8BJ, UK; jonathan.bengerubht.swest.nhs.uk
Bristol Royal Hospital For Children, Paul O’Gorman Building, Upper Maudlin Street, Bristol BS2 8BJ, UK; jonathan.bengerubht.swest.nhs.uk
Abstract
A case is reported in which an automatic external defibrillator (AED) was used during the successful resuscitation of a 6 year old child in out-of-hospital cardiac arrest, despite the fact that these devices are not recommended in children under 8 years. The interpretation of resuscitation protocols is discussed and new developments in this area reported.
- automatic external defibrillation
http://dx.doi.org/10.1136/adc.2004.054981
Statistics from Altmetric.com
Request Permissions
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- automatic external defibrillation
Widespread introduction of automatic external defibrillators (AEDs) has resulted in improved outcome from ventricular fibrillation (VF). 1 These devices are designed to be used by people with little or no training, and their placement in strategic public areas (such as airports and casinos) has been reported favourably.2 AEDs are now commonly used in pre-hospital care.
1 These devices are designed to be used by people with little or no training, and their placement in strategic public areas (such as airports and casinos) has been reported favourably.2 AEDs are now commonly used in pre-hospital care.
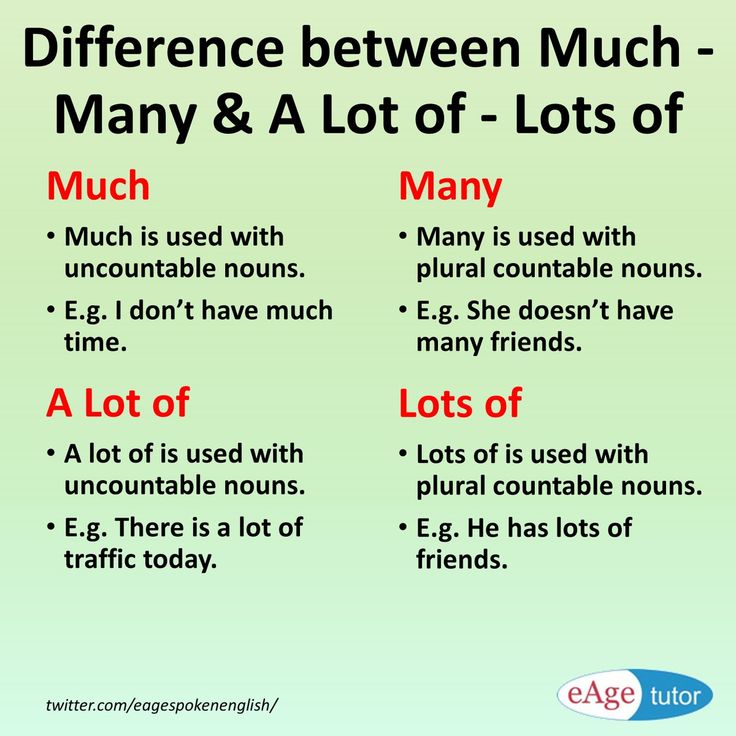
In children, the recommended first shock for VF is 2 J/kg using a monophasic defibrillator,3 but the data supporting this are scant.4 AEDs are designed for use in adults, and commonly deliver between 150 J and 200 J using a biphasic waveform. In younger children this could exceed the 10 J/kg that is thought to be potentially damaging to the myocardium, and as a result AEDs are not recommended in children under 8 years.5 Although ventricular fibrillation is less frequent in children than in adults, deciding whether or not to use an available AED on any child under 8 has been described as a “terrible dilemma”,6 particularly in a protocol driven clinical environment.
CASE REPORT
Our local ambulance despatch centre received an emergency call regarding a 6 year old girl (weight 20. 4 kg), who had collapsed and appeared to be in cardiac arrest. Basic life support was initiated by the girl’s mother according to instructions given over the telephone. The first paramedic, a “rapid response unit”, arrived within 4 minutes. The child was apnoeic and pulseless. A Heartstream FR2 (Agilent Technologies, Palo Alto, CA, USA) automatic external biphasic defibrillator was attached to the child’s chest and the monitor showed asystole. Cardiopulmonary resuscitation (CPR) was commenced, and the child ventilated with oxygen. After one minute a rhythm change to VF was noted and the AED analysed this as a shockable rhythm. One shock of 150 Joules* was delivered, following which a rhythm change to asystole occurred. CPR was continued.
4 kg), who had collapsed and appeared to be in cardiac arrest. Basic life support was initiated by the girl’s mother according to instructions given over the telephone. The first paramedic, a “rapid response unit”, arrived within 4 minutes. The child was apnoeic and pulseless. A Heartstream FR2 (Agilent Technologies, Palo Alto, CA, USA) automatic external biphasic defibrillator was attached to the child’s chest and the monitor showed asystole. Cardiopulmonary resuscitation (CPR) was commenced, and the child ventilated with oxygen. After one minute a rhythm change to VF was noted and the AED analysed this as a shockable rhythm. One shock of 150 Joules* was delivered, following which a rhythm change to asystole occurred. CPR was continued.
On the arrival of paramedic colleagues circulatory access was gained, the first dose of adrenaline was given, three cycles of the asystole protocol were completed, and endotracheal intubation was performed. After the third dose of adrenaline a rhythm change to VF was noted. A second shock of 150 J was delivered via the AED, again followed by asystole. One minute later a narrow complex bradycardia emerged with a palpable carotid pulse. The heart rate gradually increased and spontaneous respiratory effort occurred.
A second shock of 150 J was delivered via the AED, again followed by asystole. One minute later a narrow complex bradycardia emerged with a palpable carotid pulse. The heart rate gradually increased and spontaneous respiratory effort occurred.
On arrival at the hospital the child had a palpable pulse of 80 beats/min, a respiratory rate of six, and reactive pupils. Assisted ventilation was continued. A 12 lead electrocardiogram showed a prolonged QT interval. She was initially admitted to our paediatric intensive care unit. Computed tomography of her brain and an electroencephalogram were unremarkable. Six days after her cardiac arrest the patient was conversing and self-caring. An implantable defibrillator was inserted on the assumption that her arrest was secondary to prolonged QT interval causing ventricular fibrillation. She has subsequently returned to school.
DISCUSSION
This is the second recorded case of successful resuscitation following defibrillation with an AED in a child younger than 8 years. Neither the previously reported 3 year old,7 nor our 6 year old child, had evidence of any myocardial damage, though in our case this is supported by echocardiographic evidence rather than additional cardiac enzyme analysis.
Neither the previously reported 3 year old,7 nor our 6 year old child, had evidence of any myocardial damage, though in our case this is supported by echocardiographic evidence rather than additional cardiac enzyme analysis.
The existing monophasic 2 J/kg recommendation was deduced from a study of 71 transthoracic defibrillations performed on 27 children.4 Subsequent clinical experience suggests that this dose is effective, but the optimal dose is unknown.4 In addition, evidence is emerging to suggest that damage to the myocardium may be less with modern biphasic rather than traditional monophasic waveforms.8
Defibrillation is employed to depolarise the fibrillating heart, causing a temporary halt to electrical activity and providing an opportunity for a cardiac rhythm to be re-established. Use of higher energies may cause a prolonged depolarisation (asystole), and this may explain why the second shock was initially followed by apparent asystole before the emergence of a perfusing rhythm.
Current research in adult and animal defibrillation explores the analysis of both the defibrillation waveform and the transthoracic impedance, potentially enabling a shock with optimal energy, timing, and waveform to be delivered.9 Application of these principles is leading to development of paediatric defibrillators using lower energies. In the current absence of such equipment, however, professionals facing VF arrest in young children with an “adult” AED to hand will continue to face a “dilemma”.
Most practitioners are now familiar with the initial part of current recommendations: “set voltage AEDs should not be used in children under the age of 8 years”. Until new “child friendly” AEDs become available, we would use this case to draw attention to the additional statement that: “withholding use of an AED if no other defibrillator is available could cause harm”.10
Acknowledgments
The parents of the child, and the staff of the Children’s Emergency Department, take this opportunity to wholeheartedly praise the skills and the professionalism of the ambulance personnel, who we believe saved this girl’s life.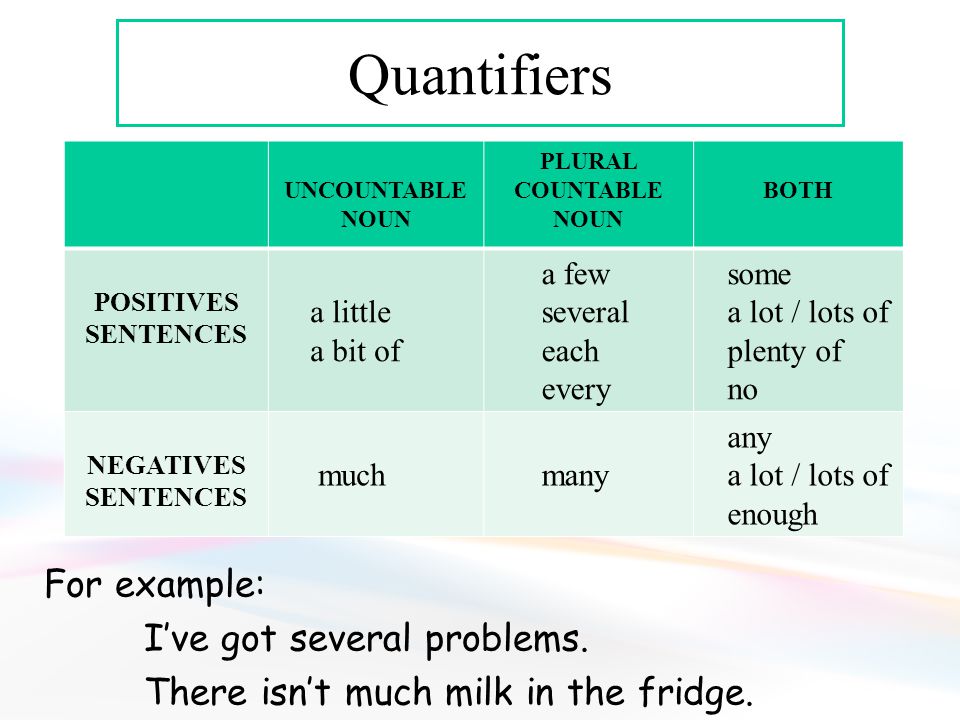
REFERENCES
- ↵
Marenco JP, Wang PJ, Link MS, et al. Improving survival from sudden cardiac arrest: the role of the automated external defibrillator. JAMA2001;285:1193–2000.
- ↵
Liddle R, Davies CS, Colquhoun M, et al. ABC of resuscitation: the automated external defibrillator. BMJ2003;327:1216–18.
- ↵
Molyneux EM, Mackway-Jones K (Advanced Life Support Group). Advanced paediatric life support: the practical approach, 3rd edn. London: BMJ Books, 2001.
- ↵
Gutgesell HP, Tacker WA, Geddes LA, et al. Energy dose for ventricular defibrillation of children. Pediatrics1976;58:898–901.
- ↵
Resuscitation Council (UK) Guidelines, 2001. Available from: http://www.resus.org.uk/pages/aed.htm#child (accessed 31 December 2003).
- ↵
Senior K . Automatic external defibrillation is safe in small children.
 Lancet2001;357:1678.
Lancet2001;357:1678. - ↵
Gurnett CA, Atkins DL. Successful use of a biphasic waveform automated external defibrillator in a high-risk child. Am J Cardiol2000;86:1051–3.
- ↵
Tang W, Weil MH, Sun S, et al. The effects of biphasic and conventional monophasic defibrillation on post resuscitation myocardial function. J Am Coll Cardiol1999;34:815–22.
- ↵
Niemann JT. Defibrillation waveforms. Ann Emerg Med2001;37:59–61.
- ↵
Biarent D, Coovadia A, Hazinski MF, et al. Use of automated external defibrillators for children: an update. An advisory statement from the Pediatric Advanced Life Support Task Force, International Liaison Committee on Resuscitation. Resuscitation2003;57:237–43.
Footnotes
↵* The Agilent Heartstream FR2 AED is a biphasic defibrillator that adjusts the waveform and delivered charge according to the measured chest impedance, but the delivered energy can only vary from 140 to 161 Joules.
Competing interests: none declared
Read the full text or download the PDF:
Subscribe
Log in using your username and password
For personal accounts OR managers of institutional accounts
Username *
Password *
Forgot your log in details?Register a new account?
Forgot your user name or password?
Defibrillation discharges - articles Medex-Inter
Warning To provide a high level of service, this site uses cookies. By continuing to use it, you agree that cookies will be stored on your computer: Accept
22/10/2021
Defibrillation is an emergency resuscitation measure, the essence of which is the impact on the myocardial area with a powerful electrical discharge. The procedure is used for atrial fibrillation, which is not amenable to medical correction, as well as other critical conditions accompanied by heart rhythm disturbances. Electrical defibrillation is carried out by the impact on the heart muscle of a single pulse generated by the resuscitator. Its strength and duration is determined by the type of pathology. The discharge is applied sequentially, if necessary, its power is increased. nine0005
Its strength and duration is determined by the type of pathology. The discharge is applied sequentially, if necessary, its power is increased. nine0005
The essence of electrical defibrillation
Electrical defibrillation is sometimes the only resuscitative measure that can restore the heart and save the patient's life. By itself, it is not capable of restarting the heart. It causes short-term asystole and complete dipolarization of the myocardial muscle, after which the natural pacemakers can resume their normal work.
Defibrillation force
For defibrillation, shocks with a power of 200-300 J are usually used. The power is determined by the type of pathology and the model of the equipment itself. In this case, the electrical impulse is applied sequentially, with increasing force:
- The first shock - 200 J. After 1-2 minutes, the doctor evaluates the heart rate. If ineffective, the procedure is repeated. For this, a higher power discharge is used.
- Second shock - 300 J. As in the first case, after 1-2 minutes it is necessary to evaluate the heart rate. If ineffective, the procedure is repeated.
- Third shock - 360 J. This is the maximum electrical shock recommended for defibrillation.
If the first series of three consecutive pulses is ineffective, then a second series of the same sequence is carried out against the background of continued mechanical ventilation, chest compressions and drug therapy. nine0005
Pediatric defibrillation shock power
Pediatric defibrillation power of the first shock is 2 J/kg. Each subsequent one increases in relation to the previous one by 0.5 J/kg. Maximum power - 5 J / kg. As with CPR in adults, a series of three shocks is also given to children. If the first series did not bring results, then against the background of ongoing artificial pulmonary ventilation, heart massage and drug therapy, a second series is carried out with the same sequence. nine0005
nine0005
You may be interested:
- What does an electrocardiogram show?
- What is ECHOCG
- What does fluid therapy include?
- Infusion route of administration
- ECG and EchoCG, what is the difference between
Features of defibrillation in cardiopulmonary resuscitation
Electrical impulse therapy, or rather its variety - electrical defibrillation is one of the main resuscitation measures in case of sudden death. Ventricular fibrillation is known to be the most common cause of cardiac arrest. Based on this, the outcome of resuscitation often depends on the possibility of defibrillation as soon as possible. nine0005
If an adult patient is in cardiac arrest and a defibrillator is available immediately, it is advisable to use it as soon as possible. If the cardiac arrest occurs unattended or a defibrillator is not available, it is wise to initiate cardiopulmonary resuscitation (CPR) while looking for a defibrillator to assess the rhythm and deliver shock if necessary.
In practice, defibrillation during CPR is as follows. While continuing to perform cardiac massage, defibrillator pads or self-adhesive defibrillator electrodes are applied to the patient's chest and the heart rate is quickly assessed. Evaluation of heart rate from defibrillator pads or self-adhesive electrodes is faster than ECG recording. Briefly interrupt chest compressions to assess the rhythm. Indications for defibrillation are ventricular fibrillation and pulseless ventricular tachycardia. Asystole and electromechanical dissociation are not indications for defibrillation. nine0005
The applicability of double sequential defibrillation in a sustained shock rhythm has not been justified. Dual sequential defibrillation is the nearly simultaneous application of two shocks using two defibrillators. Although some reports cite favorable outcomes, a 2020 systematic review found no evidence to support dual sequential defibrillation and did not recommend its use in routine medical practice. Existing studies are subject to a variety of biases, and observational studies have shown no improvement in outcome. nine0005
Existing studies are subject to a variety of biases, and observational studies have shown no improvement in outcome. nine0005
If using a manual defibrillator: charge the defibrillator (charge), then pause compressions and deliver one shock, then immediately resume compressions. Defibrillation should not interfere with the performance of quality compressions; pauses between stopping and resuming compressions should be no more than 5 seconds. The level of energy required for each specific defibrillator is determined by its instruction manual. Typically, the first shock level for a biphasic defibrillator is at least 150 J, for a monophasic defibrillator - 360 J. Before applying the shock, make sure that no one is touching the patient. The defibrillation health worker directs the resuscitation team. nine0005
Please note that medical examination gloves do not protect personnel from electric shock when a shock is applied.
When using an automated external defibrillator (hereinafter referred to as AED), follow its instructions, trying to minimize pauses in compressions.
After defibrillation is performed, CPR is continued for 2 minutes, then the heart rate is quickly assessed again. If ventricular fibrillation or ventricular tachycardia persists without a pulse, apply a second shock (150–200 J for a biphasic defibrillator or 360 J for a monophasic defibrillator), then immediately resume CPR (without a pause to reassess the rhythm and determine the pulse), starting with chest compressions ( ratio with rescue breaths 30:2). Continue CPR for 2 minutes, then quickly evaluate the rhythm. If ventricular fibrillation or pulseless ventricular tachycardia persists, a 3rd shock is applied (150–200 J for a biphasic defibrillator or 360 J for a monophasic defibrillator). After that, CPR is immediately resumed (without a pause to reassess the rhythm and determine the pulse), starting with chest compressions (ratio to rescue breaths 30:2). nine0005
If there is no recovery of cardiac activity after the 3rd shock, with venous (or intraosseous) access, 1 mg of epinephrine (may improve blood flow in the myocardium and increase the chances of success of a subsequent shock) and 300 mg of amiodarone are administered.