Can you walk after giving birth
Postpartum Exercise | Right as Rain by UW Medicine
If you’ve recently had a baby, chances are you’re getting bombarded with messages that go like this: Lose that post-pregnancy belly! Get your body back! Shed the excess baby weight!
Cue the side-eye.
Real talk? You’re exhausted, stressed and hurting in places you didn’t even know you had. Getting out of bed — let alone attempting some form of physical activity — can feel like someone is asking you to hike up Mount Rainier.
“Postpartum, there’s just so much,” explains Tina Allen, P.T., a physical therapist at the University of Washington Medical Center’s Urology Clinic. “Moms aren’t getting enough sleep, they have this new being that they’re looking after and their bodies and muscles don’t work like they used to.”
On top of that, you’re navigating your new family dynamic with a little one and have a whole ton of hormones to boot. So, yes, while you know that exercising after giving birth is good for you, it’s way easier said than done.
“Our bodies change from being pregnant,” adds Sarah Prager, M.D., M.A.S., an obstetrician-gynecologist at the Women’s Health Care Center at University of Washington Medical Center-Roosevelt and a professor in the Department of Obstetrics and Gynecology at the UW School of Medicine. “The pelvic floor is going to be in a slightly different location. Breasts are going to be different. Things might not look or feel exactly the same.”
To help you navigate your new postpartum self and safely get moving again after birth, Allen and Prager share their top tips for getting back into the fitness swing of things.
Listen to your postpartum bodyWhile celebrity moms may be posting pictures of their flat stomachs shortly after delivery — insert another side-eye here — that’s just not realistic.
Frame your physical fitness expectations with long-term goals in mind.
In those first few weeks after giving birth, it’s most important to prioritize your general recovery, well-being and sleep needs over any exercise routine.
And just like your labor and delivery is unique, how quickly you heal after having a baby is highly dependent on your personal birth experience.
Moms who have a smooth delivery with minimal complications may have an easier time resuming physical activity than those who need major interventions like a caesarean.
“Your ability to start activities is largely based on what your body is telling you,” Prager says.
That means paying close attention to how much pain you feel after doing certain movements, your level of bleeding and the amount of extra energy you can muster up between diaper changes and feedings.
Once your doctor clears you for more intense physical activity at your final check-up — usually around 6 to 8 weeks postpartum — you can progress to other types of exercise.
How quickly and intensely you start exercising again also depends on your previous fitness level. If your idea of a good workout before pregnancy was a brisk walk, you won’t have the same starting point as, say, a marathon runner — and that’s totally fine.
The most important thing is to find a level of physical activity that you feel comfortable with and go from there.
“I recommend starting at 75 percent effort of what your baseline had been,” Prager says. “If it feels like too much, back it off a bit more. If it feels OK, increase it a little bit.”
Start easy with short walksIt may not seem like much, but taking a short walk can help tremendously during your postpartum recovery.
“I encourage patients to be getting up and walking around almost immediately after delivery,” Prager says. “Even if it’s a 10-minute walk around the block, it can be extremely helpful for the healing process. It can decrease that risk of blood clots that is even more prominent postpartum if a woman has had surgery.”
Walking not only lets you test out how well your body feels after delivery — looking at you, vaginal tears — it also eases you back into physical activity without risking major injury.
“Walking is great,” Allen adds. “In general, movement helps everything.”
“In general, movement helps everything.”
A simple stroll — with or without baby — can also provide a huge mood boost, something that’s especially helpful during those first few exhausting weeks.
An analysis of 16 different studies found that light exercise during the postpartum period helped reduce the odds of developing mild to moderate depressive symptoms by as much as 54 percent.
From a short walk around the block, you can work your way up to longer distances, faster speeds or steeper inclines.
Don’t push yourself too far too fastWhile it’s good to work in some exercise, trying to do too much too quickly is not.
“There’s a difference between a good pain like, ‘Yes, I’ve worked my muscles hard and that feels great,’ versus ‘I’m straining my muscles in a way that they’re not ready for,’” Prager explains.
This is an especially important distinction to make if you’ve had a C-section, which means you shouldn’t lift anything heavier than your baby for the first 6 to 8 weeks.
“If you have increased urine leakage after exercising or any kinds of swelling happening, that’s something you should talk to your doctor about,” Allen notes. “If you’re having shooting pain, ripping, tearing or a sharp feeling, that’s really an indication to stop what you’re doing and back off. You’re being too intense too soon.”
When a red flag pops up, ease back on the physical activity until you feel better. From there, you can slowly build back up the duration or intensity of your exercise.
But if the pain doesn’t go away or get better on its own, talk to your doctor or physical therapist to check on your injury.
Another thing to watch out for? Your hydration and nutrition needs, particularly if you’re breastfeeding.
To keep those sudden hunger pangs at bay, it’s a good idea to tuck a water bottle and some snacks into your purse or stroller, just in case you suddenly feel depleted in the middle of a walk.
Make safe adjustments to postpartum exercisesOnce your doctor gives you the green light to get your sweat on, you might be tempted to dive back into your usual workout routine. But remember, your body is different now and still healing in various ways.
But remember, your body is different now and still healing in various ways.
To avoid injury, focus on exercises that won’t damage sensitive areas like your core or pelvic floor and adjust them as needed.
CoreRemember that whole celebrity mom comparison thing? This is where those unrealistic expectations can get you into trouble.
Don’t launch right into aggressive core exercises in an effort to lose your post-pregnancy belly as quickly as a Kardashian.
“Ab muscles are like big rubber bands that have been stretched out for 40 weeks,” Prager says. “If you immediately start exercising with dynamic exercises, you can damage them.”
That means avoiding crunches, jumps, twists and leg lifts. Instead, focus on more gentle, static core exercises like planks, bridges and pelvic tilts.
“Think about how you hold in your core as you zip up a tight pair of pants and how that keeps your core engaged,” Allen says. “Now try keeping your core engaged like that while breastfeeding, washing dishes or engaging with your little one. ”
”
Another common post-pregnancy concern is incontinence, courtesy of your still-healing pelvic floor. Gee, thanks.
Incontinence, when you can’t control urine leakages, is an issue that most moms have after giving birth. Usually, this will improve on its own over time.
Basic balance exercises and yoga can help, as well as another tried-and-true favorite: Kegels.
Allen says its best to do Kegels in various situations and positions — while lying down, sitting in your car or standing at the sink — to maximize their impact.
But when incontinence doesn’t go away on its own, specialized care like pelvic floor physical therapy can make a huge difference. Ask your doctor for a referral if you’re still experiencing issues several weeks postpartum.
BreastsAnother postpartum issue you may need to accommodate? Those extra-tender (and sometimes leaky) breasts.
Make it a point to breastfeed or pump before you exercise to alleviate some of the discomfort. Nursing pads are also helpful to prevent any embarrassing wet spots from appearing mid-yoga pose.
Nursing pads are also helpful to prevent any embarrassing wet spots from appearing mid-yoga pose.
And if your chest still feels a little unsupported, try doubling up on sports bras or opting for ones specifically made for nursing moms.
Alignment“I frequently have women who say they have back pain, neck pain and headaches postpartum,” Prager says. “That’s because the common position they are in is breastfeeding or looking down at their baby.”
When you sit or stand, focus on having a straight alignment, rolling your shoulders back and keeping your rib cage down. Adding props like breastfeeding pillows to support your arms and baby can help ensure you’re not hunched over for long periods of time, too.
Prager also suggests adding in chest-opening stretches and gentle neck rolls to your daily routine to help keep the tightness at bay.
“It’s still possible to gaze adoringly at your child and stretch your neck out a bit,” she says.
Finding time for self-care while nurturing your little one? Well, that’s the definition of #momlife.
Six ways you're sabotoging your postpartum recovery
Having a baby is a big emotional and physical transition. Go easy on yourself, and please don't try to "do it all."
The happy pictures of glowing new moms and hours-old babies you see on social media make childbirth seem easy, like it’s totally NBD. But giving birth is a life-altering event, and many women have unrealistic expectations about how fast they can (and should) get back to “normal.” When you have a hungry or fussy newborn and birth injuries to contend with at the same time, you have to adjust your recovery timeline and go easy on yourself.
“Respect the fact that you are going through a massive life change and a massive recovery,” says Batya Grundland, a family doctor who focuses on obstetrics and perinatal care at Women’s College Hospital in Toronto. If you want to get back on your feet and feeling better, faster, here are some things to watch out for.
1. Trying to do it allFrom booking a newborn photoshoot to hosting family who want to meet the baby (and cleaning the whole house before all the visitors arrive), it’s common to overdo it in those first few weeks. But even if you had a relatively easy delivery and didn’t get many stitches, you’ve just gone through a major physical trauma—experts say that for those first few weeks, rest is key. For at least the first 24 to 72 hours post-birth, spend as much time as possible in bed, skin-to-skin with the baby, especially if you’re trying to get the hang of breastfeeding, says Jennifer Brewer, a registered midwife in Toronto. Many midwives recommend a full week of bed rest, but Brewer understands that a week isn’t always possible for most women (especially if you have other children). Try for at least a few days, if you can. Staying horizontal, not walking around too much, and keeping pressure off your pelvic floor will help with healing and minimize postpartum bleeding.
But even if you had a relatively easy delivery and didn’t get many stitches, you’ve just gone through a major physical trauma—experts say that for those first few weeks, rest is key. For at least the first 24 to 72 hours post-birth, spend as much time as possible in bed, skin-to-skin with the baby, especially if you’re trying to get the hang of breastfeeding, says Jennifer Brewer, a registered midwife in Toronto. Many midwives recommend a full week of bed rest, but Brewer understands that a week isn’t always possible for most women (especially if you have other children). Try for at least a few days, if you can. Staying horizontal, not walking around too much, and keeping pressure off your pelvic floor will help with healing and minimize postpartum bleeding.
Impose limits on yourself and others. If a messy house drives you insane, ask someone else (like your partner or mother-in-law) to help with household tasks. Or set a timer and clean for 10 minutes, but no more. When family and friends come to visit, give them a specific window for when they can come and ask them to bring their own food and refreshments, or any supplies you might need. (Hint for your visitors: nipple cream, a pack of pads, baby wipes, fancy coffee delivery or snacks for a ravenously hungry nursing mom may be way more useful to you and your partner than overloading on cute baby outfits and blankets.)
When family and friends come to visit, give them a specific window for when they can come and ask them to bring their own food and refreshments, or any supplies you might need. (Hint for your visitors: nipple cream, a pack of pads, baby wipes, fancy coffee delivery or snacks for a ravenously hungry nursing mom may be way more useful to you and your partner than overloading on cute baby outfits and blankets.)
“Don’t invite people who are going to come in and just expect you to get up and make them something,” says Brewer.
Visitors often want to pass the baby around, too. While it’s nice to have your hands free for a bit, the fights over who gets to hold the baby make it especially hard for you to learn your new baby’s hunger cues. It can take three to five days (or more) for your milk to come in, which means some of your first well-wishers might arrive while you’re still trying to get into a good feeding rhythm. If you’re worried about your baby’s weight (the rule of thumb is that they should regain their birthweight by week two), minimize the amount of time the baby spends cuddling in others’ laps. (Sorry, Grandma!)
(Sorry, Grandma!)
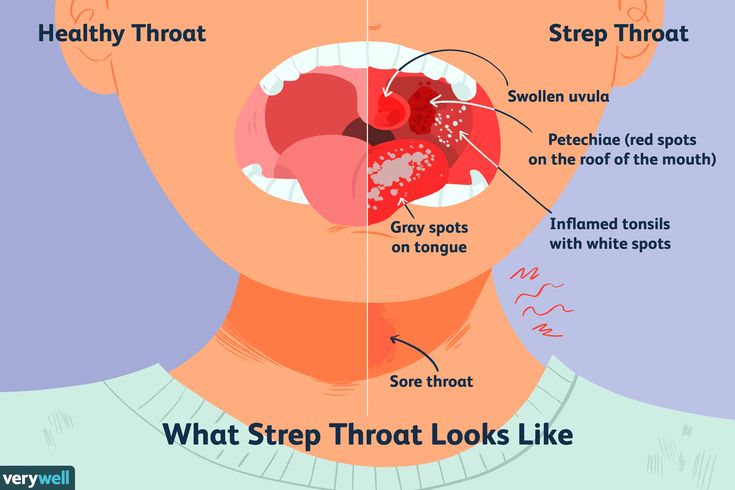
Also, make sure to ask everyone to wash their hands. Newborns are especially vulnerable to germs, as their immune systems are still forming.
2. Ignoring physical and mental red flagsKeep an eye on how you feel overall, and identify red flags early. If your post-birth pain is no longer being controlled by medication, if you begin seeing discharge from your stitches, or you experience heavy bleeding that’s persisting or getting worse, call your doctor as soon as possible, recommends Grundland.
Beyond the physical symptoms, it’s also important to monitor your mood. If you’re unable to feel a sense of connection with your baby, or if you can’t sleep at night—not because of your newborn, but because your worries are keeping you awake—you need to seek help early. This is especially essential if you’re having suicidal thoughts or thinking about harming your baby, says Grundland. Brewer agrees: The number one concern she sees in new mothers is mood issues that aren’t being addressed.
Brewer agrees: The number one concern she sees in new mothers is mood issues that aren’t being addressed.
Maybe you read the term “self-care” and rolled your eyes. Who has the time for self-care at this stage of motherhood? But try to take at least half an hour of time to yourself every day, even if it’s just to have a shower or to go to the bathroom alone, says Brewer. Ask your partner or a family member to come and take the baby for that solid chunk of time, so you’re not standing in the shower, unable to relax, wondering if that sound you’re hearing is your baby crying in the other room.
17 mind-blowing ways your body changes after giving birthIf you’ve had a vaginal birth, use this time to take an epsom salt bath in lukewarm water for 15 to 20 minutes, which will help promote healing. (Separate sitz baths that attach to the toilet work as well, but they’re not nearly as relaxing, and can put pressure on an already sore area. ) Applying frozen pads soaked in witch hazel will help soothe a sore perineum or ay hemorrhoids. Or, if you’re feeling up for it, go outside for some fresh air or a coffee shop visit, or just find a quiet place to read a magazine solo. “Around the six week mark, if people really aren’t yet doing these mental health things—like handing off the baby for a half-hour—I start to see issues,” says Brewer.
) Applying frozen pads soaked in witch hazel will help soothe a sore perineum or ay hemorrhoids. Or, if you’re feeling up for it, go outside for some fresh air or a coffee shop visit, or just find a quiet place to read a magazine solo. “Around the six week mark, if people really aren’t yet doing these mental health things—like handing off the baby for a half-hour—I start to see issues,” says Brewer.
It’s not selfish—it’s self-care that might save your sanity, and hasten your physical recovery as well.
4. Eating (and drinking) poorlyWhile you might be tempted to grab whatever carbs you can eat with one hand, try your hardest to keep healthy foods stocked. (Almonds, apples and protein bars are easy, one-handed snacks to add to your shopping list.) The first six weeks are about survival—it’s not about losing the baby weight. Eating well will help you manage your energy levels and mitigate any constipation.
“All women are a little bit constipated postpartum,” says Grundland. When you’re in labour (and if you’ve had surgery, such as a C-section) your digestion slows down, and constipation can cause painful bowel movements, or cause or worsen hemorrhoids. Eat lots of fibrous veggies, consider taking some flax supplements, and drink lots of water. (If dietary interventions don’t work, Grundland says it may be worth speaking with your healthcare provider about stool softeners.) If you’re breastfeeding, try to eat full-fat foods such as fish, yogurt and avocados to satiate your hunger.
When you’re bone-tired, your first instinct might be to reach for a cup of joe, but Brewer doesn’t recommend having more than one cup a day. Coffee dehydrates you, and small amounts of it end up in your breast milk, which can ultimately cause even more sleep deprivation. Instead, hydrate throughout the day with lots of water, or you can try lactation teas or coconut water for additional electrolytes.
Until your six-week postpartum check up, you shouldn’t be doing any serious exercise, says Amy Gildner, an orthopaedic physiotherapist and certified pelvic floor physiotherapist at West End Mamas in Toronto. “It’s definitely a time to rest and repair,” she says.
Once your healthcare provider gives you the green light, don’t go out and join a hardcore baby bootcamp right away. When you’ve got a six-week-old, you likely won’t be ready or able to do squats and planks like the mom of a six-month-old. One of the biggest mistakes women make is returning to exercise that is too challenging, says Gildner. Even if you were in great shape before (or even during) your pregnancy, you need to recognize that it won’t feel the same afterward. Approach your exercise goals like you’re coming back from an injury—which you are—and ease into it slowly, she recommends. And remember that the often-repeated “no pain, no gain” workout philosophy does not apply to postpartum healing.
And remember that the often-repeated “no pain, no gain” workout philosophy does not apply to postpartum healing.
So, skip sit ups and crunches—those aren’t great for anyone, especially postpartum, says Gildner. Avoid heavy lifting or straining during those first few months. Activities like spinning can be great for postpartum women who are having trouble walking, but be wary of leaning over and putting too much strain on a C-section scar.
“I don’t think it’s good to stay stagnant either,” says Gildner. She recommends that women begin getting active in a way that isn’t painful, as soon as they are able. Start off with walking, then add in some hills and gauge how you’re feeling before taking it to the next level. If you’re feeling the need to stretch and move, look into more gentle methods, like guided parent-and-baby yoga classes or moderate Pilates classes specifically designed for postpartum women.
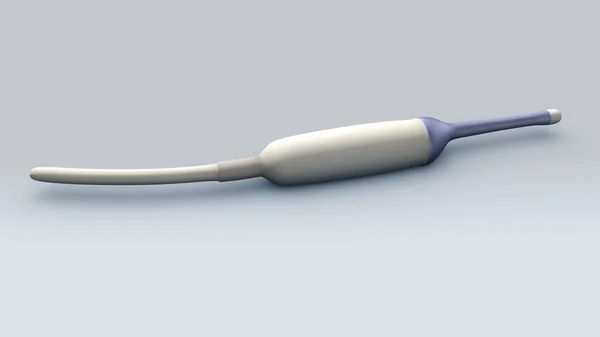
6. Skipping pelvic physiotherapyAt the six-week mark, most women, whether they had a vaginal birth or a C-section, will benefit from being assessed by a pelvic floor physiotherapist.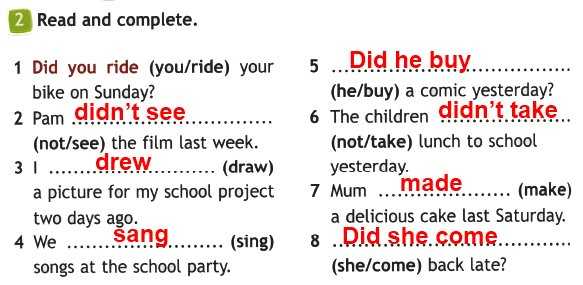 (This is separate from your six-week checkup with your primary care provider, and may cost you out of pocket, unless you have extended health benefits.) While a pelvic floor physio is an added cost, “it’s so worth it,” says Brewer. The physio will assess your core and back muscles, check on the healing of any scar tissue, and they’ll examine your pelvic floor, the sling of muscles holding up your pelvic organs. Be forewarned—this involves an internal vaginal exam. Pelvic physiotherapists can also help with healing diastasis recti, which is the thinning of the linea alba tendon in between your abs (making it seem like they are separating), caused by intra-abdominal pressure.
(This is separate from your six-week checkup with your primary care provider, and may cost you out of pocket, unless you have extended health benefits.) While a pelvic floor physio is an added cost, “it’s so worth it,” says Brewer. The physio will assess your core and back muscles, check on the healing of any scar tissue, and they’ll examine your pelvic floor, the sling of muscles holding up your pelvic organs. Be forewarned—this involves an internal vaginal exam. Pelvic physiotherapists can also help with healing diastasis recti, which is the thinning of the linea alba tendon in between your abs (making it seem like they are separating), caused by intra-abdominal pressure.
“One hundred percent of pregnant women have diastasis,” says Gildner. “It’s completely normal.” But getting the extent of your diastasis assessed, and managing it with personalized at-home exercises the physio recommends for you, is important for proper healing. Most physios will recommend deep core work such as Pilates moves or oblique exercises, as well as pelvic floor exercise cues, similar to doing Kegels.
It can be a tricky skill to master, especially after childbirth. To isolate your pelvic floor muscles, pretend you are scooping up a marble with your vagina and then pulling the marble up to your bellybutton. Don’t tense up your whole body, though. “I find some women brace even their neck muscles when I get them to do a Kegel. It’s a more subtle movement, focusing only on the vaginal muscles,” says Gildner. To help get the mind-muscle connection back, aim to do 10 to 15 Kegels per day, but don’t go overboard, either. Doing too many per day while you’re healing will do more harm than good.
C-section moms should also get assessed, says Gildner. “The biggest myth of C-sections is that your pelvic floor is fine because you didn’t deliver vaginally. Nothing could be further from the truth.” You are still pregnant for nine months, your core is often weak, and scar tissue can create a lot of issues with your abdominal muscles in your core. C-sections often cause women to experience back pain, stemming from a weak core. “We often don’t see [C-section] clients until a few months afterward, when the issues are chronic and harder to fix,” she says.
“We often don’t see [C-section] clients until a few months afterward, when the issues are chronic and harder to fix,” she says.
The fourth trimester asks a lot of your body: constantly reaching down to get your newborn from the bassinet, nursing in awkward positions, or babywearing, which can put a lot of strain on both your back and abdominals. The lack of sleep can make it even harder to recover.
Remember to take it easy. You don’t have to be Superwoman, but you do need to try and look after yourself (both physically and mentally) as much as you’re looking after your newborn. Remember to feed your body well—not just your baby’s—and snuggle up with your little one as much as possible. All this quiet, restful time will pay off in the long run, making you a happier parent who’s able to fully enjoy her baby.
Read more:
How postpartum doulas can help parents through the first few weeks with a new baby
Six things every mom should know about postpartum recovery
Watch Baby Grow!
Subscribe to Today’s Parent’s baby newsletter and find out what to expect for every stage and milestone, from birth to two years.
- Email*
- Baby's due/birth date*
Month223456789101112
Day12345678910111213141516171819202122232425262728293031
Year2025202420232022
- CAPTCHA
- Consent*
Yes, I would like to receive Today's Parent's Baby newsletter. I understand I can unsubscribe at any time.**
FILED UNDER: Maternal health Postpartum Postpartum care Self-care
The first days after childbirth
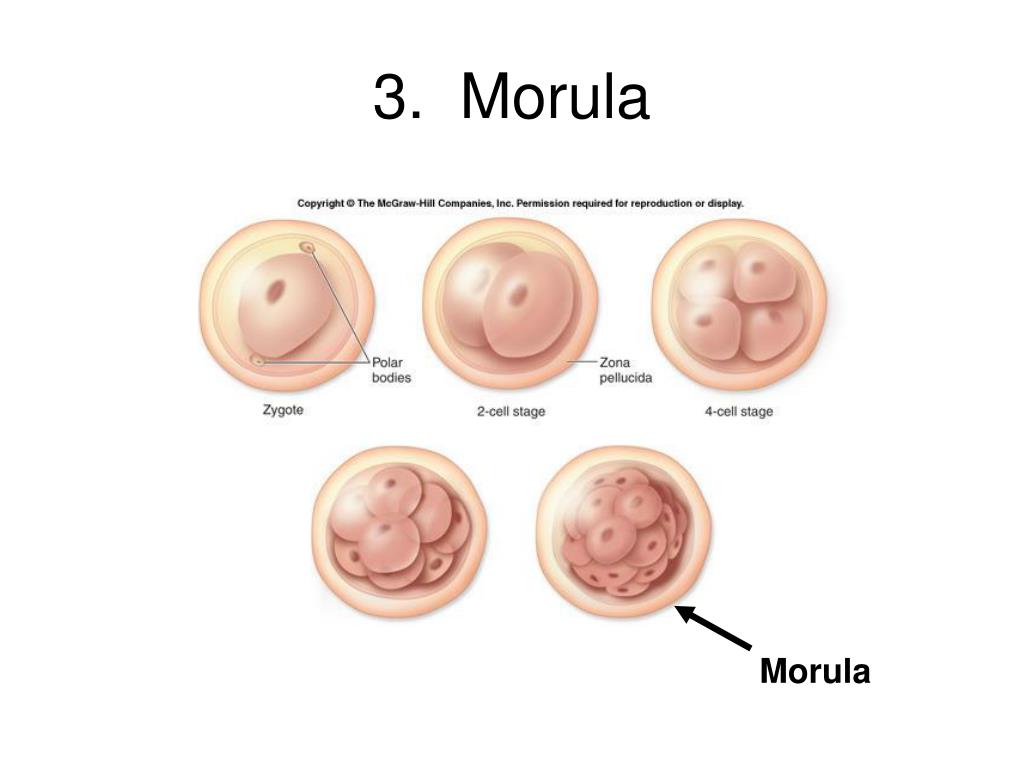
Pregnancy and childbirth is a serious burden for the body of any mother. After childbirth, significant changes occur in the body, but it must be said that restructuring cannot occur instantly. A woman will feel some changes right away, but quite significant changes will occur for several more weeks. What should change?
First days after childbirth (postnatal ward)
In the first days after childbirth, there may be hemorrhages in the eyes - red eyes, on the face - numerous bluish dots, similar to moles that appear during the second
childbirth. If a woman pushes incorrectly (holds her breath, screams, pushes “in the face”) or has features of the vascular wall, during attempts there is an increase in pressure in the vessels of the head, which can lead to rupture of blood vessels in and around the eyes . What to do with such red eyes?
If a woman pushes incorrectly (holds her breath, screams, pushes “in the face”) or has features of the vascular wall, during attempts there is an increase in pressure in the vessels of the head, which can lead to rupture of blood vessels in and around the eyes . What to do with such red eyes?
Cold tea compresses on the eyes (for 10 minutes) applied several times a day will have a calming effect and speed up recovery, which will occur in a maximum of 6-10 days. In about a week, the hemorrhages on the face will also pass. nine0003
Cramping abdominal pain worsens during breastfeeding associated with normal postpartum uterine contractions, which should shrink and return to pre-pregnancy size. Painful contractions of the uterus are more typical for repeated births and for twins. In primiparous women, such pains may not be present and uterine contraction is painless. Painful contractions may be more noticeable when breastfeeding, as suckling releases the hormone oxytocin, which stimulates uterine contractions. nine0003
nine0003
After childbirth, in addition to reducing the size of the uterus, the mucous membrane of the uterus - the endometrium - should be restored. Therefore, immediately after childbirth, lochia appear from the genital tract - the discharge of blood, mucus and tissue residues from the uterus. In the first three days after childbirth, they are usually bloody and as plentiful (and sometimes more plentiful) as during menstruation. Increased discharge when standing up and other movements is a normal process.
Muscle pain in different parts of the body can also disturb a woman in the first days after childbirth. These pains are associated with the physical stress that a woman experiences during childbirth. These pains go away on their own within a few days. nine0003
Pain in the perineum and the discomfort associated with it - and this feeling is also normal, because it is unrealistic to expect a 3-3.5 kg child to pass through the perineum without any consequences. Even if you avoided tears during childbirth and did not have an episiotomy (an incision in the perineum), this area was still stretched and squeezed. The pain will go away in a few days.
Even if you avoided tears during childbirth and did not have an episiotomy (an incision in the perineum), this area was still stretched and squeezed. The pain will go away in a few days.
In the case of an episiotomy, pain may increase, especially when laughing, coughing, sneezing, defecation. Like any wound, it does not heal immediately - it usually takes 5 to 7 days. At this time, the woman is forbidden to sit so that the seams do not come apart. At the same time, they are allowed to sit on the toilet, to perform regular sexual hygiene (after each visit to the toilet, it is necessary to wash the perineum with warm water, you can do it without soap, you should take a shower 2 times a day). While you are in the hospital, your midwife and doctor will examine your stitches for inflammation or other signs of infection. The stitches are usually removed on the 5th day. nine0003
In the first time after childbirth, only colostrum is excreted from the breast - a thick yellowish liquid, and milk appears on the 2-3rd day. By the 3rd day, the mammary glands often acquire hypersensitivity, sometimes bursting pain is felt in the chest , a feeling of compaction of the mammary glands may appear. With significant breast engorgement, it is necessary to limit the amount of fluid consumed (but not less than 1 liter per day), increase the frequency and duration of feeding the baby. To prevent nipple cracks and when they appear, you will need BEPANTEN, DEXPANTHENOL, SOLCOSERYL ointment. nine0003
By the 3rd day, the mammary glands often acquire hypersensitivity, sometimes bursting pain is felt in the chest , a feeling of compaction of the mammary glands may appear. With significant breast engorgement, it is necessary to limit the amount of fluid consumed (but not less than 1 liter per day), increase the frequency and duration of feeding the baby. To prevent nipple cracks and when they appear, you will need BEPANTEN, DEXPANTHENOL, SOLCOSERYL ointment. nine0003
During the first day after childbirth, there may be difficulties with urination . Some women do not have the urge to urinate; others feel the need but cannot empty their bladder. Despite all the difficulties, it is necessary that the bladder be emptied in the first 6-8 hours after childbirth. This is done so that the enlarged bladder does not interfere with the normal contraction of the uterus after childbirth. As a last resort, if you still cannot empty your bladder within 4 hours after giving birth, a woman may have a catheter placed. After giving birth, you need, regardless of desire, to urinate every 4 hours. Bladder function returns to normal after 3-7 days. nine0003
After giving birth, you need, regardless of desire, to urinate every 4 hours. Bladder function returns to normal after 3-7 days. nine0003
The causes of stool problems can be several factors, both physical and psychological. Getting your bowels back on track is rarely easy or quick, and takes a few days.
Include more fiber in your daily diet: fermented milk products, beets, high-fiber fruits, dried fruits. This will soften the stool, but make sure that there are no allergens among vegetables and fruits: remember that before the arrival of milk and the establishment of lactation, you should not drink a lot of liquid. Try to move more if your condition allows. And don't worry about your stitches coming apart - they won't. Since a woman is often given a cleansing enema before childbirth, there is usually no stool in the first 2-3 days. nine0003
Immediately after childbirth, you must not get out of bed on your own for 6 hours (only in the presence and with the help of a midwife), as there may be dizziness .
After childbirth the abdomen looks distended and somewhat pendulous and does not immediately return to its original shape, because the muscles and skin need time to contract. In order to quickly return to its former shape, you can use breathing exercises (traditional gymnastics can be performed only 6-8 weeks after childbirth). Breathing exercises are breathing with the stomach: while inhaling, inflate the stomach, while straining the muscles of the perineum, while exhaling, blow it off. Repeat 10-20 times, 4-5 times a day. nine0003
After a caesarean section: on the first day after the operation, it is only allowed to drink water up to 2-3 liters per day. But already on the second day, the mother is transferred to the postpartum department, where she immediately begins to lead an active lifestyle - she gets up and walks, feeds her baby, unsweetened bread, broth without meat are allowed. From the third day, after a cleansing enema, it is allowed to take boiled food (porridge, boiled meat, sour-milk products, cottage cheese, tea without sugar), butter cookies, buns, fresh fruits and vegetables are prohibited. nine0003
nine0003
First week after birth
Continued vaginal discharge : within 1-2 weeks after birth the discharge gradually becomes watery pink, then brown and finally yellowish white. During this period, you should use sanitary pads (and not tampons: they can provoke inflammatory diseases of the uterus and appendages). Allocations may stop after two weeks, and may continue up to the 6-8th. If after the first week there is a profuse bloody discharge, or discharge with an unpleasant odor, or a fever, you should consult a doctor. In this case, hospitalization and possibly curettage of the uterus may be necessary. You should also see a doctor if brownish or yellowish lochia persists for more than 6 weeks, as this may be the result of an infection, especially if accompanied by fever or pain, and tenderness in the abdomen. nine0003
The suture area after episiotomy must be kept dry and clean. You can wash the external genitalia and perineum with a decoction of chamomile, calendula, eucalyptus. For the first 2 months after childbirth, get out of bed carefully, first turning on your side, bypassing a sitting position (this will reduce pressure on the muscles of the perineum), and feed the baby lying on your side or half-sitting; you can't lift weights.
For the first 2 months after childbirth, get out of bed carefully, first turning on your side, bypassing a sitting position (this will reduce pressure on the muscles of the perineum), and feed the baby lying on your side or half-sitting; you can't lift weights.
The birth of a child is a very significant event for a woman, not only physically, but also psychologically. Firstly, childbirth itself exhausts the mother, and secondly, hormone production changes during and after childbirth. Therefore, it is natural that at this time comes period of mental instability .
The most typical feeling in the first days after childbirth is elation, but in the following days, and sometimes weeks, some women become sad, despondent, withdrawn and lethargic. It is worth noting that these are the usual postpartum emotions associated with the normalization of hormonal levels. In this situation, close people (spouse, parents) should come to your aid to help you cope with negative emotions. nine0003
nine0003
Within 7 days after the caesarean section (before removing the sutures), the nurse daily treats the postoperative suture with antiseptic solutions (for example, iodine, "potassium permanganate") and changes the bandage. The skin scar is formed approximately on the 5-7th day after the operation; already a week after the caesarean section, you can safely take a shower. Just do not rub the seam with a washcloth - this can be done in another week. Discharged from the maternity hospital in the absence of any complications on the 5-7th day after operative delivery. Since the pain in the scar area can persist for up to several weeks, it can be difficult for a woman to bend over, so it is easier to sit down, bending her legs at the knee and hip joints. nine0003
Remember that recovery after childbirth is usually about 6-8 weeks. However, the female body is individual. Therefore, each woman can feel the physical and emotional changes described above in her own way. Report any unusual or very severe symptoms to your nurses or your doctor.
Prepared by: Ass. obstetrics and gynecology Pavlyukova S.A. Head postpartum ward Dvornik E. V.
Recovery after childbirth: the first hours. nine0001
The joy of the birth of a baby is over, the hormonal cocktail that raged during childbirth is gradually changing its composition and the body is rebuilding to a new life stage - motherhood. But, having experienced the happiness of childbirth, what should mom do next? How to quickly restore strength and always enjoy communicating with the baby? Specific recommendations on how to help yourself in the first hours or days after childbirth are given by an experienced CTA obstetrician and childbirth preparation course leader Svetlana Luzikhina:
“The first day after childbirth, you can lie not only on your back, but also in any other position. Even on the stomach! But in this case, put a small pillow under the stomach so that there is no deflection in the back. Try not to lie in one position for a long time, change positions. It is advisable to get up only when absolutely necessary, for example, to the toilet, but you can eat in bed - let others take care of you! When walking, do not take long steps, but imagine that you are in a long, tight, evening dress, move smoothly and in small steps. nine0003
It is advisable to get up only when absolutely necessary, for example, to the toilet, but you can eat in bed - let others take care of you! When walking, do not take long steps, but imagine that you are in a long, tight, evening dress, move smoothly and in small steps. nine0003
In order for the pelvic bones to recover properly after childbirth, fix them in a supine position with a wide bandage or any long scarf (diaper) so that you can tie around - from the upper edge of the thigh to the middle of the thigh. This is especially important if you are planning to do something around the house, like cooking.
After giving birth, drink as much as your body requires. We recommend drinking a decoction of herbs (nettle, yarrow, shepherd's purse - brew in a thermos, each herb 2 tbsp per liter). This collection has an anti-inflammatory, hemostatic effect, helps to reduce the walls of the uterus after childbirth. We drink during the day, about a liter. On the first day, honey, lemon, two tablespoons of wine or rose hips (to increase hemoglobin) can be added to this herbal cocktail to taste, and we drink the main cocktail 5-7 days after childbirth. On the first day, you can eat and drink whatever you want to restore strength. Eat what you ate during pregnancy, the child is familiar with this food. Limit fresh vegetables and fruits, and be careful with those foods that personally cause gas formation in you, it is from them that the baby can have colic. nine0003
On the first day, you can eat and drink whatever you want to restore strength. Eat what you ate during pregnancy, the child is familiar with this food. Limit fresh vegetables and fruits, and be careful with those foods that personally cause gas formation in you, it is from them that the baby can have colic. nine0003
Eat easily digestible food: cereals, soups, stewed vegetables, etc. Add natural vegetable oils to food (porridge, soup) (2-3 tablespoons per day) to prevent constipation. If this does not help, you can use glycerin or sea buckthorn suppositories. Sea buckthorn suppositories also help heal cracks if they have formed, and they can also be used to treat hemorrhoids. With hemorrhoids, you can use the ointment "esculus" and "hamamelis" (there are also candles). In case of any complications, you can get individual recommendations from the specialists of our center (obstetrician-gynecologists, midwives, homeopaths, hirudotherapeutist, etc.). nine0003
Breastfeeding:
Contact with the baby is very important (emotional, physical, visual): skin-to-skin contact is important, do not hold back your emotions! Hug the baby, kiss! You stroke the baby, admire it, and the body immediately begins to release hormones that promote uterine contraction and stimulate the production of milk (colostrum). Don't worry about whether you have colostrum or not, breastfeed your baby on demand. Try to do it right right away so that the baby completely captures the areola. Teach your baby to open his mouth wide by teasing him by touching the baby's chin or lower lip with your finger or nipple. It shouldn't hurt when you suckle, and notice that the baby's jaw moves up and down, the lips are turned, and the tip of the spout is pressed against the breast. nine0003
Don't worry about whether you have colostrum or not, breastfeed your baby on demand. Try to do it right right away so that the baby completely captures the areola. Teach your baby to open his mouth wide by teasing him by touching the baby's chin or lower lip with your finger or nipple. It shouldn't hurt when you suckle, and notice that the baby's jaw moves up and down, the lips are turned, and the tip of the spout is pressed against the breast. nine0003
When breastfeeding, no matter what position you are in, make sure you feel comfortable. If you feel good, your baby will too. The child should lie confidently in your hands, it is not so important for him how correctly you are doing something - the children really need the confident hands of their parents! Subject to the above, milk will come at the right time for the baby. Difficulties arise if the mother had problems with prolactin before pregnancy, there was a long-term use of oxytocin, during separation after childbirth.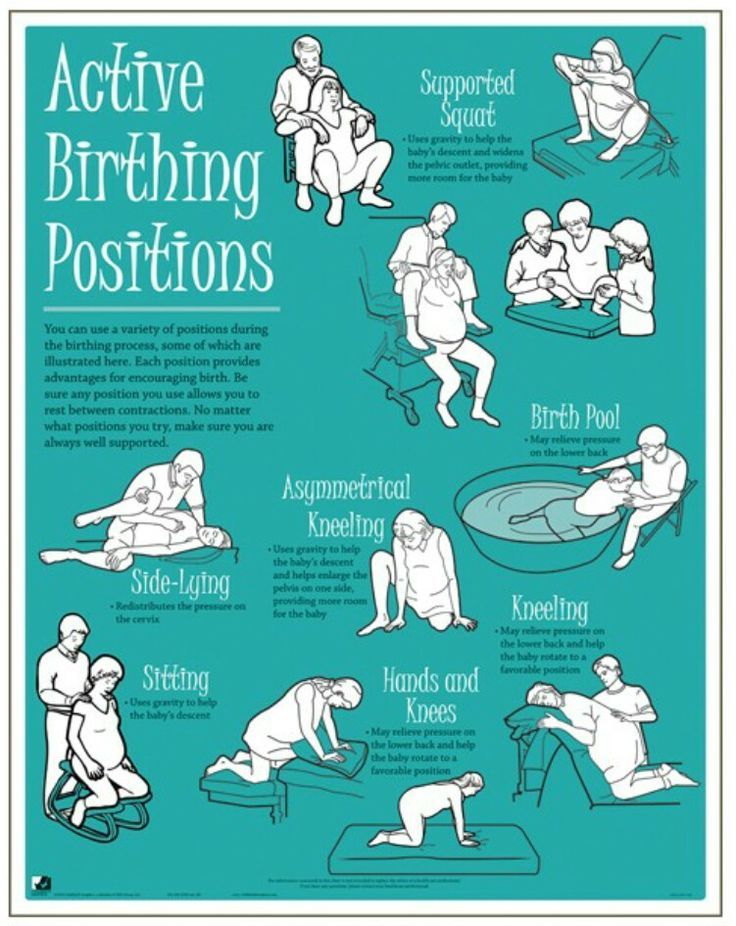 However, this may not affect in any way - everything is individual! nine0003
However, this may not affect in any way - everything is individual! nine0003
Wear a knitted or cotton bra, sports tops to support your bust. It is important that you feel comfortable and not press anywhere.
For nipple healing, use 100% lanolin (purilan) or bepanthen, sea buckthorn oil can also be used. Starting from the 38th week of pregnancy, you can start wiping the areola with a frozen decoction of oak bark (alternately, we wipe the left and right areola for 2-3 seconds, repeating 10-15 times). Thanks to tannins and temperature contrast, the skin on the chest will become a little rougher. Sponging is good to continue after childbirth, as long as there is a need. nine0003
To avoid congestion in the chest, from the end of the second day, try to completely exclude everything hot, eat and drink everything at room temperature. It is better to drink water often, but in small sips, in order to understand the body's need for water. Try not to drink sweet drinks (compotes, tea with sugar, etc.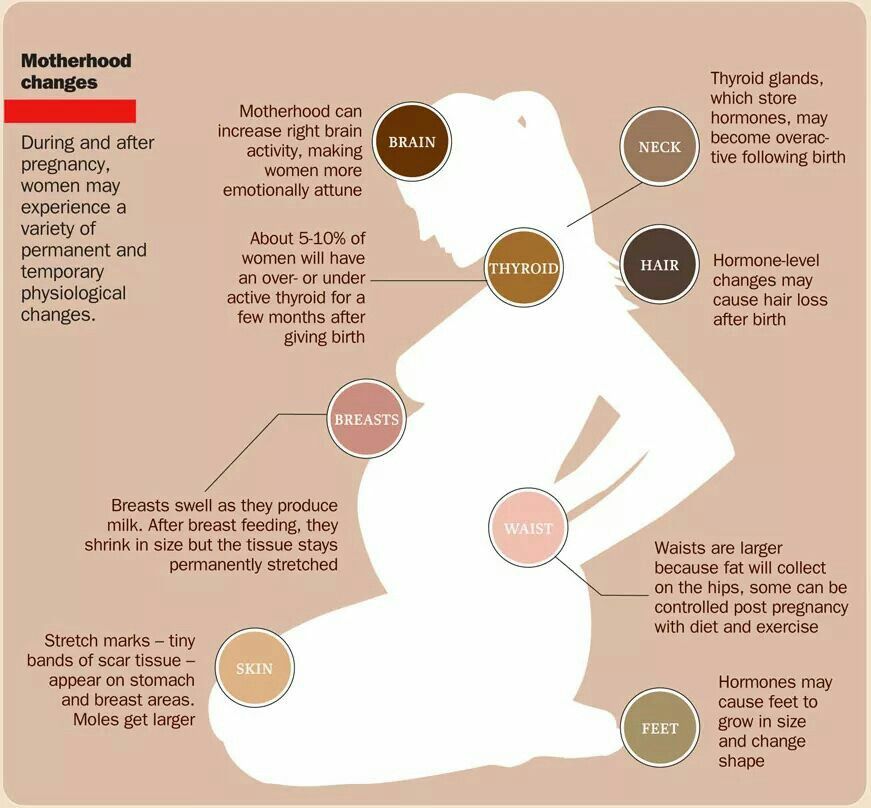 drinks), they require additional liquid. As soon as you begin to feel that milk is coming (the chest becomes hotter than usual and there are sensations of fullness), start doing exercises for the chest. Where there is movement, there is no stagnation! Let me remind you of a few exercises, for example: when you put your hands on your shoulders and rotate your elbows away from you; arms are bent at the elbows in front of us and we squeeze our palms, we also move them from side to side, up. A cat good and evil - this exercise will not only improve blood circulation in the chest, but also help the uterus contract better. nine0003
drinks), they require additional liquid. As soon as you begin to feel that milk is coming (the chest becomes hotter than usual and there are sensations of fullness), start doing exercises for the chest. Where there is movement, there is no stagnation! Let me remind you of a few exercises, for example: when you put your hands on your shoulders and rotate your elbows away from you; arms are bent at the elbows in front of us and we squeeze our palms, we also move them from side to side, up. A cat good and evil - this exercise will not only improve blood circulation in the chest, but also help the uterus contract better. nine0003
Massage your breasts with gentle massaging movements. We put the child to the breast at the request of the mother, if he asks more often - that's great! In no case do not express your breasts “completely”, if such a situation suddenly arises that you need to express, do it until the chest is relieved. But the chest should remain full. Milk comes on demand, if you express, then the body will not establish the correct rhythm of milk production, and you will turn into a dairy factory. nine0003
nine0003
As soon as you understand that milk comes at the request of the baby, start drinking what you want and at the temperature you like.
Personal care:
Use cotton underwear or maternity disposable panties. Change pads after every trip to the toilet. Also, every time it would be good to wash with a decoction of oak bark or yarrow, chamomile. In case of perineal injury (rupture or episiotomy), after treatment with an antiseptic, wound healing ointments for the mucosa (sea buckthorn oil, calendula ointment, arnica, solcoseryl, etc.) can be used. Empty your bladder more often, you can't stand it. If suddenly you do not feel the urge, then go to the toilet every 3 hours, as if on an alarm clock. nine0003
A contrast shower is useful (if not on the whole body, then at least on the area of the uterus). Change the temperature of the water so that you are comfortable, water yourself for 30-40 seconds, while trying not to get burned or get cold.
Gymnastics:
Exercises to strengthen the muscles of the perineum and pelvic floor can be done from 2-3 days after childbirth (if there are no injuries, and if there is, then not earlier than a week later), or when you remember about it ☺. We strengthen the muscles from the bottom up, starting with the famous Kegel exercise. Next, we add exercises for the abdominal muscles - “rinsing the abdomen” (lying on your back, with your legs bent at the knees, put one hand under your lower back and then raise the pelvis due to the tension of the gluteal muscles and help with breathing while inhaling, pull the perineum up, while exhaling we relax) . Also useful are “twisting” - to improve the work of intestinal motility, exercises on all fours (cat - with bent knees, we move our legs to the side and back, strengthening the gluteal muscles, etc.). Toward the end of the first month, exercises can be done with the baby. nine0003
We strengthen the muscles from the bottom up, starting with the famous Kegel exercise. Next, we add exercises for the abdominal muscles - “rinsing the abdomen” (lying on your back, with your legs bent at the knees, put one hand under your lower back and then raise the pelvis due to the tension of the gluteal muscles and help with breathing while inhaling, pull the perineum up, while exhaling we relax) . Also useful are “twisting” - to improve the work of intestinal motility, exercises on all fours (cat - with bent knees, we move our legs to the side and back, strengthening the gluteal muscles, etc.). Toward the end of the first month, exercises can be done with the baby. nine0003
Mood:
A favorable psychological background in the family is very important. It’s good if there are assistants next to you for the first few days who can cook food, clean the house (but don’t overdo it! the child needs cleanliness, not sterility!). Then the mother will be able to calmly deal only with the child and herself: tune in to breastfeeding, get used to the new role, and, of course, eat well and rest - sleep when the baby sleeps.