How many breaths per minute for a child while sleeping
Normal Respiratory Rates for Children
Written by Steven Brown
In this Article
- Normal Breathing Rate for Kids
- If Your Child Is Breathing Fast
- If Your Child's Breathing Is Irregular
- Get Used to This
Sickness that affects breathing crops up often during childhood. Naturally, you want to watch out for any sign that your youngster is coming down with something.
How fast they breathe can be a signal. If it's a bit too quick, that can be one of the first symptoms of a lung infection, especially for a baby or small child. Children younger than 3 need extra-close attention because this type of illness can be especially hard on them.
First, you need to know what counts as typical, healthy breathing.
Normal Breathing Rate for Kids
The thing to watch is how fast they breathe when they’re at rest. For children, the normal rate depends on their age:
To measure how fast your child is breathing, count how many times their chest rises in 1 full minute. If they're outside the normal range for their age, something may be wrong.
If Your Child Is Breathing Fast
If you have a baby or toddler, call 911 if:
- They're less than 1 year old and takes more than 60 breaths a minute.
- They're 1 to 5 years old and takes more than 40 breaths per minute.
If your child is older than that, call the doctor if they get winded more than usual after exercise, or even ordinary activities. If their quick breathing keeps coming back, that’s another reason to check with your doctor.
Rapid breathing can be a symptom of several things. Some of the most common are:
Bronchiolitis: This lung infection affects children under 2 years old. They generally get it in winter or early spring. It makes the airways inside their lungs get more narrow. That makes it hard for them to breathe. Other symptoms may include:
- Runny nose
- Cough
- Slight fever
- Wheezing
- Loss of appetite
It usually comes on during the winter or early spring, and the first symptoms look like a cold. Then, RSV spreads into the lungs, where it can lead to things like bronchiolitis and pneumonia.
Then, RSV spreads into the lungs, where it can lead to things like bronchiolitis and pneumonia.
Asthma: Kids who have this usually show the first signs of it by the time they’re 5 years old. Besides fast breathing, symptoms can include coughing or wheezing.
Pneumonia: This may come after your child has a cold or flu. It can be from a virus or bacteria.
Other symptoms include:
- Struggling to breathe
- Wheezing
- Coughing
Kids who are 2 or younger are more vulnerable. They should go to a doctor if they show symptoms.
If Your Child's Breathing Is Irregular
It's normal for a child to stop breathing for 5 or 10 seconds, then pick back up again on their own. But if it goes longer than 10 seconds or they start to turn blue, call 911.
If your child’s breathing pauses while they're asleep, that might be a sign of sleep apnea. This can crop up in kids between 2 and 8 and years old. There usually are other symptoms, too, such as snoring.
Get Used to This
Breathing issues are common in kids, especially if they go to daycare or have brothers and sisters. It’s normal for them to get as many as 12 infections a year. Each one may take a couple of weeks to clear up.
Different conditions have similar symptoms, so it may be hard for you to figure out which one your child has. That’s where the doctor will help.
Normal Respiratory Rate for Adults and Children
- Respiratory rate is the number of breaths taken per minute.
- In adults, the normal respiratory rate is roughly 12 to 20 breaths per minute.
- In children, the normal respiratory rate varies by age.
Respiratory rate is one of the main vital signs of the human body. It refers to the number of breaths you take in one minute.
The speed, pattern, and depth of your breaths indicate how well your body is working to deliver oxygen to all your vital organs and tissues.
Normal respiratory rate in a healthy adult is about 12 to 20 breaths per minute.
Your respiratory rate can be affected by many different factors such as alcohol consumption, sleep apnea, infections, or heart conditions.
Read on to learn more about why respiratory rate is important, how to measure it, what affects it, and when to see a doctor.
Respiration is the metabolic process of oxygen intake and carbon dioxide release. It’s controlled by a body system called the respiratory drive. The respiratory drive can be broken down into three systems:
- Neural central control: The neural central control system sets the ventilation rate and air intake volume. This affects exhalation, inhalation, and breathing pattern.
- Sensory input system: The sensory system sends information back to the central nervous system to indicate how much volume and at what rate to breathe. It also recognizes chemical changes such as irritants.
- Muscular system: The muscular system moves the lungs in accordance with signals from the other systems. It controls the mechanics of breathing.
These systems work together to create a process that exchanges oxygen and carbon dioxide.
When we breathe out, we release low oxygen and high carbon dioxide. When we breathe in, we take in high oxygen and low carbon dioxide. The exchange of these elements is important for metabolic processes to continue at the cellular level.
The respiratory drive is tied closely to the central nervous system. When the central nervous system is altered or damaged, it can affect the rate of respiration.
For example, a stroke that causes brain stem damage can affect breathing. Narcotics, such as opioids, can also depress the central nervous system and affect breathing.
There are also other factors that can affect your respiratory rate, as we’ll explore further in this article.
A normal respiratory rate in healthy adults is roughly 12 to 20 breaths per minute. Your respiratory rate is an important vital sign. It can potentially indicate a more serious condition, such as cardiac arrest.
Your respiratory rate is an important vital sign. It can potentially indicate a more serious condition, such as cardiac arrest.
If your respiratory rate is below average, it could indicate central nervous system dysfunction. If your respiratory rate is above average, it could indicate another underlying condition.
Some variation in respiratory rate may occur with aging. As we get older, we become more prone to certain health conditions. Changes to your respiratory health or other organ systems can change your respiratory rate.
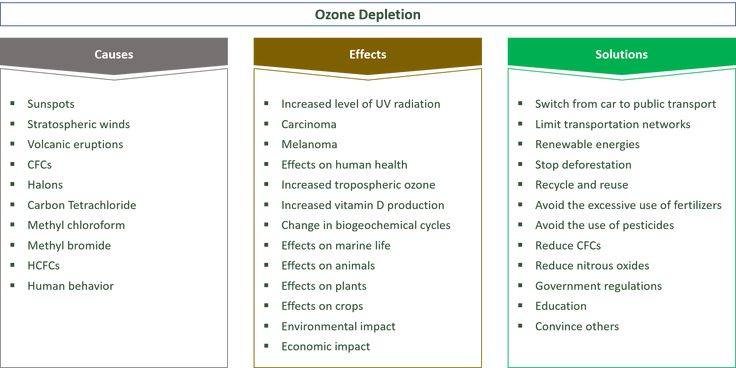
The normal respiratory rate for children varies by age.
| Age | Rate (in breaths per minute) |
| Birth to 6 months | 30 to 60 |
| 6 months to 1 year | 30 to 50 |
| 1 to 3 years | 24 to 40 |
| 3 to 5 years | 22 to 34 |
| 5 to 12 years | 16 to 30 |
| 12 to 18 years | 12 to 20 |
Your respiratory rate can be measured in three steps:
- Set a timer for 1 minute.
- Sit or lie down to get yourself in a state of rest. Avoid strenuous activity beforehand.
- Start the timer and measure the amount of breaths taken in 1 minute. This can be done by counting how many times your chest rises.
Sometimes focusing on trying to count your own breaths can cause feelings of stress. These feelings can affect your respiratory rate. If this is the case, you can ask a family member or friend to count your breaths for 1 minute. They should do this while you’re relaxed and focusing on something else.
The most common factors that can affect your measured respiratory rate include:
- emotional state
- physical fitness
- internal temperature
- your health status and any other conditions you may have
In some cases, a doctor or nurse may use sensors or other diagnostic tools to check your respiratory rate.
Alcohol
Alcohol is a depressant that affects your central nervous system. The effects of alcohol continue to increase the more you consume.
Alcohol poisoning slows your breathing and heart rate, which can contribute to life threatening complications.
Opioids
Opioids have a depressant effect on the central nervous system. The effects can be seen system-wide, from blood pressure to respiration rate.
Deaths from opioid overdose, which claim as many as 68,630 lives every year in the United States, are often caused by altered or dysfunctional breathing.
Medications
Other medications also act as central nervous system depressants, which means they can slow your respiratory rate.
These mediations include:
- benzodiazepines
- barbiturates
- certain sleeping medications, including zolpidem (Ambien)
Combining these medications with each other, or with other depressant substances such as alcohol or opioids, can lead to life threatening side effects.
Metabolic issues
Hypothyroidism is caused by an underactive thyroid gland. The thyroid hormone plays an important role in many body processes, including respiration.
Hypothyroidism can weaken the muscles of the lungs, making it harder to breathe. This can slow down your normal respiratory rate.
Brain injuries or stroke
Each year, 795,000 people have a stroke in the United States, according to the Centers for Disease Control and Prevention (CDC). One common complication of stroke is respiratory system dysfunction.
Changes in the respiratory rate can be minor to severe, depending on the stroke. Minor respiratory changes can lead to sleep disorders, such as sleep apnea. Major respiratory disturbances can lead to more serious complications, such as the need for a breathing tube.
In some cases, these respiratory changes are temporary and may improve with ongoing recovery from stroke.
Sleep apnea
Sleep apnea is a condition in which your breathing pattern is disrupted during sleep. Obstructive sleep apnea and central sleep apnea are the two main types of this condition.
Central sleep apnea occurs when the area of the central nervous system that controls breathing does not send the proper signals while you sleep. This can be caused by underlying factors, such as stroke, heart disease, or certain medications.
This can be caused by underlying factors, such as stroke, heart disease, or certain medications.
Fever
A fever is one of the reactions your body experiences when fighting an infection. There are many signs and symptoms of fever, including hot skin, sweating, and shivering. A fever can cause an increased respiratory rate as your body attempts to cool itself down.
Dehydration
Dehydration occurs when your body does not take in enough water to meet its needs.
When you’re severely dehydrated, low fluid levels can lead to a range of serious complications. These complications can speed up your breathing rate.
Asthma
Asthma is a condition characterized by narrow, inflamed, and mucus-filled airways. With asthma, there are times when it becomes difficult to get enough air into your lungs.
This can cause increased respiration as your body attempts to compensate for the lack of air exchange.
COPD and other lung conditions
Chronic obstructive pulmonary disease (COPD) is a set of conditions that are characterized by long-term lung damage. The following conditions fall under the umbrella of COPD:
The following conditions fall under the umbrella of COPD:
- emphysema
- chronic bronchitis
- refractory asthma
With COPD, damage or irritation in the lining of the lungs makes it difficult to get enough oxygen. As your body attempts to increase oxygen consumption, respiration increases.
Heart conditions
The heart is closely tied to respiration. The role of the heart, working in conjunction with the lungs, is to circulate oxygenated blood to the vital organs of your body.
With heart disease, heart function deteriorates and it cannot pump as much blood. When this happens, your body does not get the oxygen it needs and respiration increases.
Stimulants
Stimulants include many common ADHD medications. These drugs act on certain neurotransmitter chemicals in the brain. In turn, stimulants can have a range of effects in the body.
When taking stimulants, one potential side effect is an increased breathing rate.
Infections
Lung infections can cause inflammation of the airways and the lungs. This inflammation can make it difficult to breathe. When your body is unable to take long, deep breaths, it makes your breathing faster to try to get more oxygen.
This inflammation can make it difficult to breathe. When your body is unable to take long, deep breaths, it makes your breathing faster to try to get more oxygen.
Anxiety or panic attacks
Hyperventilation is a common symptom of anxiety and panic attacks. During a panic attack, the fight-or-flight response is activated. This response prepares the body to fight or flee, and heart rate, blood pressure, and respiratory rate can increase.
Transient tachypnea (infants)
This acute condition occurs in newborns and is characterized by fast, sometimes labored, breathing.
As newborns take their first few breaths, the fluid that was in their lungs is expelled out. When the baby cannot expel the fluid out entirely, the respiratory rate may increase to take in more oxygen.
Transient tachypnea requires treatment in hospital, but with treatment, it usually clears up within a few days.
If your breathing rate is low for too long, it can cause complications such as low blood oxygen, acidosis, or respiratory failure. In addition, increased or decreased respiratory rates often indicate underlying conditions that need to be treated.
In addition, increased or decreased respiratory rates often indicate underlying conditions that need to be treated.
If you or your child is experiencing the following symptoms, it’s important to see a doctor:
- rapid breathing of over 20 breaths per minute in adults
- slow breathing of under 12 breaths per minute in adults
- a breathing rate that falls outside of normal in children
- symptoms of asthma or a lung infection, such as coughing, wheezing, and increased mucus
- symptoms of thyroid disorder, such as dry skin, hair changes, and fatigue
If you or your child is struggling to breathe, or you suspect the change in breathing is due to an overdose, poisoning, or medical emergency, get emergency medical help right away.
Vital signs are measurements of your body’s basic functions. They’re called “vital” because they reflect the most important functions needed to sustain life.
Every medical evaluation starts with measuring these signs. This helps healthcare professionals determine the care and treatment you need.
This helps healthcare professionals determine the care and treatment you need.
Respiratory rate is one of the four vital signs. The other three vital signs are:
Body temperature
Your body needs to stay at a certain temperature to support its basic functions. In a healthy adult, body temperature is around 98.6°F (37°C), but it can range between 97.7°F to 99°F (36.5°C to 37.2°C).
Body temperature is affected by conditions such as fever, when body temperature increases due to infection, and hypothermia, when your body temperature becomes too low. When your body temperature is too high or too low, your body’s basic systems cannot function effectively.
To measure your temperature, you’ll need to use a thermometer. Digital thermometers that take measurements from the mouth, armpit, or rectum are commonly available. Each device is different, so it’s important to follow the instructions on your thermometer carefully.
Blood pressure
Blood pressure measures the force of your blood pushing against your artery walls when your heart beats and contracts. Healthy blood pressure for adults is considered to be 120/80 millimeters of mercury (mm Hg) or less.
Healthy blood pressure for adults is considered to be 120/80 millimeters of mercury (mm Hg) or less.
High blood pressure is known as hypertension. It can be caused by many different factors, such as age and certain health conditions.
Low blood pressure is known as hypotension. It can be caused by situations like standing up quickly, or health conditions such as a heart attack.
High blood pressure can lead to health complications, and in some cases the same is true of low blood pressure.
Your doctor or a nurse will typically measure your blood pressure during a routine health check. If your doctor recommends it, you can also use a measuring cuff to check your blood pressure at home.
Pulse rate
Your pulse rate, or heart rate, is the number of times your heart beats in one minute. In adults, the healthy range is 60 to 100 beats per minute.
The speed and pattern of your pulse rate provide an indication of your heart rhythm and how well your heart is pumping blood.
Slow, fast, or irregular heart rate is called arrhythmia. It can be caused by medications, high blood pressure, or other factors.
Your doctor can measure your heart rate during a simple physical exam, or they may use diagnostic tools like an electrocardiogram. You can also measure your heart rate at home by counting your pulse for 15 seconds, then multiplying that number by 4 to get your heart rate.
The normal respiratory rate of adults falls within the range of 12 to 20 breaths per minute. For children, a normal respiratory rate will depend on their age.
If you’re concerned that your breathing is not typical, visit your doctor. They can diagnose any other underlying conditions and causes.
Read this article in Spanish.
Pneumonia (Child)
Pneumonia is an infection that causes deep damage to the lungs. It can be caused by a virus or bacteria.
Symptoms of pneumonia in children may include the following:
Pneumonia caused by bacteria is usually treated with antibiotics. Your child should feel better within 2 days of starting the antibiotic. Pneumonia will pass in 2 weeks. Pneumonia caused by a virus is not treated with antibiotics. It can last up to 4 weeks.
Your child should feel better within 2 days of starting the antibiotic. Pneumonia will pass in 2 weeks. Pneumonia caused by a virus is not treated with antibiotics. It can last up to 4 weeks.
Home Care
Follow the guidelines below when treating your child at home.
Fluids
Fever causes the child to lose more water than usual. For children under 1 year old:
-
Continue regular breastfeeding or formula feeding.
-
Between feeds, give your child an oral rehydration solution as recommended by your child's healthcare provider. This solution can be purchased at grocery stores and pharmacies without a prescription.
For children over 1 year:
-
Give your child plenty of liquids such as water, juices, decaffeinated sodas, ginger ale, lemonade, fruit drinks, or popsicles.

Food
Don't worry if your child refuses to eat solid food for several days. This is fine. Make sure the child is drinking plenty of fluids.
Physical activity
Children who have a fever should stay at home, rest or play quiet games. Try to get your child to sleep more often. When the fever passes, the child will feel better, and his appetite will return, he will be able to go back to kindergarten or school.
Dream
There are frequent periods of drowsiness and excitability. A child with a stuffy nose will sleep better if their head and upper body are elevated. You can also raise the head of the bed by placing it on a 6 inch (15 cm) high block.
Cough
The illness is usually accompanied by a cough. It is recommended to install a cold steam humidifier by the bed. Over-the-counter cough and cold medicines (cold) have not been proven to be more effective than placebo (sweet, drug-free syrup). However, these drugs can cause severe side effects, especially in children younger than 2 years of age. Do not give over-the-counter cough and cold medicines to children under 6 years of age unless instructed to do so by your doctor.
However, these drugs can cause severe side effects, especially in children younger than 2 years of age. Do not give over-the-counter cough and cold medicines to children under 6 years of age unless instructed to do so by your doctor.
Do not smoke around your child and do not allow others to smoke. Cigarette smoke can make coughing worse.
Nasal congestion
Cleanse the nose of infants with a douche. Before cleansing the nose, you can put 2-3 drops of salt water (saline solution) into each nostril. This will help remove the highlights. Saline nose drops are available without a prescription. You can make your own saline solution by adding 1/4 teaspoon of table salt to 1 cup of water.
Medicines
If no other drug has been prescribed, use acetaminophen to reduce fever and relieve anxiety or discomfort. Children older than 6 months can take ibuprofen (ibuprofen) instead of acetaminophen. If your child has chronic liver disease or kidney disease, talk to your doctor before taking these medicines. Also check with your doctor if your child has ever had a stomach ulcer (stomach ulcer) or GI bleeding. Do not give aspirin to children under 18 who have a fever. It can cause severe liver damage.
Also check with your doctor if your child has ever had a stomach ulcer (stomach ulcer) or GI bleeding. Do not give aspirin to children under 18 who have a fever. It can cause severe liver damage.
If an antibiotic is prescribed, give it as directed until it runs out. You must continue to take it even if your child already feels better. Give the child exactly the dose of antibiotic that was prescribed, no more and no less.
Follow-up
If your child does not get better in the next 2 days (or as directed), see the doctor again.
If x-rays have been taken, they will be reviewed by a radiologist. You will be informed of any findings that may affect your child's treatment.
When to Seek Medical Care
Seek immediate medical attention if:
-
If your baby is less than 12 weeks old and has a temperature of 100.4°F (38°C) or higher. Your child may need to see a doctor.
-
A child of any age repeatedly has a temperature above 104°F (40°C).
-
The child is less than 2 years old and has a fever for more than 24 hours. The child is 2 years old or older and has had a fever for more than 3 days.
In addition, seek medical attention immediately if you experience any of the following:
-
Rapid breathing. A newborn under 6 weeks old has more than 60 breaths per minute. A child aged 6 weeks to 2 years has more than 45 breaths per minute. A child aged 3 to 6 years has more than 35 breaths per minute. A child aged 7 to 10 years has more than 30 breaths per minute. In a child older than 10 years - more than 25 breaths per minute.
-
Wheezing or labored breathing
-
Earache, sinus pain, neck stiffness or pain, headache, diarrhea or repeated vomiting
-
Unusually restless behavior, drowsiness or confusion
-
Appearance of a new rash
-
No tears when crying, sunken eyes or dry mouth, not urinating for 8 hours in infants, or decreased urine output in older children
-
Pale or bluish skin
-
Grunting sounds
© 2000-2022 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Was this helpful?
Yes no
Tell us more.
Check all that apply.
Wrong topic—not what I was looking for.
It was hard to understand.
It didn't answer any of my questions.
I still don't know what to do next.
other.
NEXT ▶
Last question: How confident are you filling out medical forms by yourself?
Not at all A little Somewhat Quite a bit Extremely
Marathon according to the norms
Everyone knows that an adult body differs significantly from a child's body. But not everyone knows what the baby’s pressure should be, what is the normal level of hemoglobin, whether it is worth sounding the alarm, noticing that the baby has a fever. The fact is that the norms for children and adults are very different. Especially to inform a wide range of patients, we held a marathon on the norms in the social networks of MedVedika. Every day, parents got acquainted with the main parameters that determine human health. Now marathon materials are available to you. Read and save useful information!
But not everyone knows what the baby’s pressure should be, what is the normal level of hemoglobin, whether it is worth sounding the alarm, noticing that the baby has a fever. The fact is that the norms for children and adults are very different. Especially to inform a wide range of patients, we held a marathon on the norms in the social networks of MedVedika. Every day, parents got acquainted with the main parameters that determine human health. Now marathon materials are available to you. Read and save useful information!
Pulse
Parents often ask us the question: “What is the normal heart rate for a child”? The heartbeat is one of the main vital parameters that is used to detect a number of pathologies. By observing the nature of the changes, specialists can draw a conclusion about the state of the human heart and the whole organism as a whole.
The normal pulse in a child is significantly different from the norm for an adult. Want to check if your child's pulse is normal? See the table of norms by age, the average value and the limits of the norm are indicated here.
Any concerns? You can always consult a pediatrician or a cardiologist at the MedVedik Children's Health Clinic.
Arterial pressure
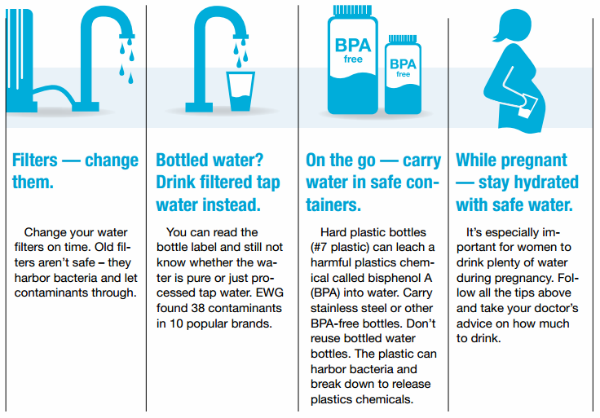
Blood pressure (BP) is one of the few health markers that can be measured at home. Today, a device for self-measurement of blood pressure is available in almost every family. But not all adults know that the norm indicators for children differ from the usual "120 to 80" for all of us.
"MedVedik" recalls that the blood pressure indicator depends on the age of the baby. The younger the child, the lower his normal pressure. This is due to the fact that the circulatory system and heart of the child continue to develop after birth, therefore, initially, the vessels and capillaries of the child have a lower tone than in adults.
Keep a helpful BP table for children. These are generalized indicators that are the result of many years of research. They correspond to the working pressure at 95% of healthy children.
Have you noticed a significant discrepancy between the readings of blood pressure in the child and in the table? Now that's a reason to see a doctor. He will calculate the individual rate specifically for your child and, if necessary, select the treatment.
P.S. By the way, to obtain an accurate measurement result, the size of the tonometer cuff is important. A large cuff on a small child's hand can distort the readings somewhat.
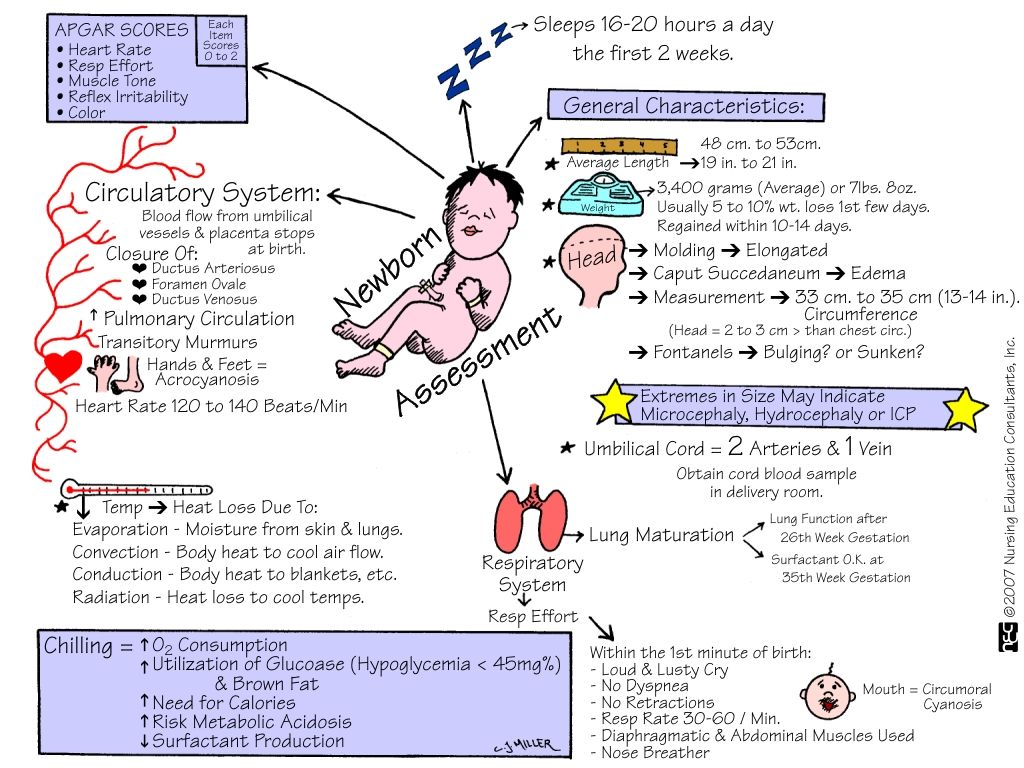
Respiratory rate
Counting respiratory movements is one of the actions performed by a pediatrician when examining a child. Do not underestimate this seemingly simple indicator. The frequency of respiratory movements (RR) per minute can provide important information about the state of the whole organism as a whole and about the functioning of the respiratory system and the cardiovascular system in particular.
Do you want to independently calculate the respiratory rate in a child? This will require a stopwatch (available in almost every mobile phone) and following simple rules. The child should be in a comfortable position and in a calm state (in infants, we recommend counting the respiratory rate during sleep). You can observe the breathing visually or by placing your hand on the baby's stomach. Be sure to count your breaths for a full minute. For the most accurate result, it is recommended to carry out three counts and calculate the average value.
The child should be in a comfortable position and in a calm state (in infants, we recommend counting the respiratory rate during sleep). You can observe the breathing visually or by placing your hand on the baby's stomach. Be sure to count your breaths for a full minute. For the most accurate result, it is recommended to carry out three counts and calculate the average value.
Did the findings surprise you? Indeed, the NPV per minute in children is several times higher than the same indicator in adults. The younger the child, the higher the respiratory rate. As they grow older, their number decreases, and by the age of 15 it is compared with the norm for adults.
See the age table. The NPV for boys and girls does not differ.
Leukocyte formula
Consider the indicators of the leukocyte formula in children under 5 years of age. Many modern parents prefer to take blood tests in specialized laboratories that hand out the results or send them by e-mail.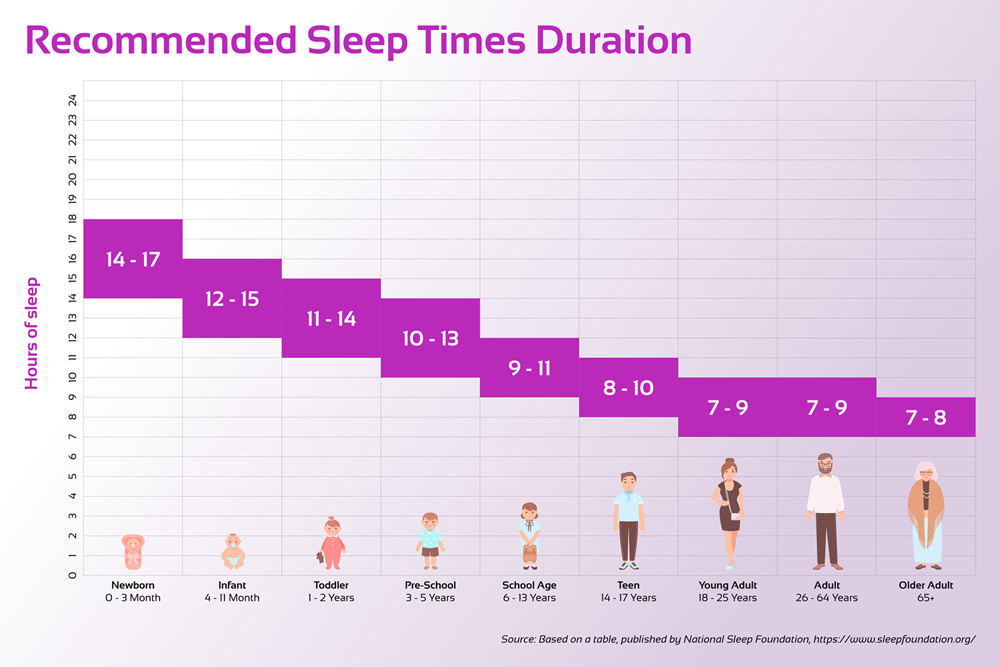 Having received the data, fathers and mothers begin to analyze the numbers, compare them with reference values, and sometimes panic.
Having received the data, fathers and mothers begin to analyze the numbers, compare them with reference values, and sometimes panic.
Don't worry ahead of time. In infants, the leukocyte formula is somewhat different from the same formula in adulthood. As in previous cases, this is due to the fact that the child's body is in the developmental stage.
"MedVedik" urges to trust the interpretation of the results of analyzes to professionals.
The number of leukocyte cells is constantly changing, and for this, a leukocyte formula was created, which helps doctors assess the general condition of the patient, in a timely manner to identify this or that deviation. The norms of the content of different bodies belonging to the group of leukocytes vary depending on age. The number of some cells increases, others - decreases even with normal development. At certain moments, the number of different leukocytes equalizes. Experts call all this a cross formula and do not attribute it to pathologies. Most often, the crossover occurs during the first year of a child's life.
Most often, the crossover occurs during the first year of a child's life.
In our clinic you are ready to consult on all emerging issues.
Hemoglobin
Health is made up of many components, each of which plays a specific role. One of the important indicators is the level of hemoglobin in the blood of a child. You will hardly be surprised to learn that hemoglobin norms in children of different ages differ significantly from adults. Almost always their values are higher.
Every cell in the human body needs oxygen to survive. Hemoglobin is a complex protein that is part of red blood cells and plays a key role in enriching the body with oxygen.
The highest level of hemoglobin in newborns, it ranges from 145 to 220 g / l. This is due to the fact that during pregnancy, the body of the expectant mother creates the necessary supply of iron for the child. At the age of one month, the supply is gradually depleted and the level of hemoglobin decreases. By three months, it can drop to 90 g/l. Proper nutrition is essential to maintain it. The best source of replenishment of iron and other useful elements is mother's milk. Therefore, if possible, do not stop breastfeeding for at least a year. Further, the level of hemoglobin in children begins to gradually increase.
By three months, it can drop to 90 g/l. Proper nutrition is essential to maintain it. The best source of replenishment of iron and other useful elements is mother's milk. Therefore, if possible, do not stop breastfeeding for at least a year. Further, the level of hemoglobin in children begins to gradually increase.
After the onset of puberty (12-15 years), depending on the sex of the child, hemoglobin values begin to differ. As a rule, this is slightly higher in boys than in girls. By adulthood, the value of hemoglobin in the blood approaches the "adult" indicator.
In our plate you can see the norms of hemoglobin content in the blood of children from birth to 18 years.
Body temperature
Young parents are often concerned about the question, what temperature in a child can be considered the norm?
An increase in readings on a thermometer should always be taken seriously, and even more so when it comes to a baby.