Should breastfeeding hurt
Breastfeeding FAQs: Pain and Discomfort (for Parents)
Breastfeeding is natural, but it takes practice to get it right. Here's how to handle pain and discomfort during nursing.
Is It Normal to Have Cramps While Breastfeeding?
Yes. During the first few days to weeks after delivery, you may feel strong, menstrual-like cramps in your uterus when your milk “lets down” (starts to flow). This is your uterus shrinking back to a smaller size.
Is It Normal for My Breasts to Get Engorged?
During the first 2–5 days after birth, it’s normal to have engorged (very full) breasts as your milk supply increases. But if your baby nurses (or you pump) every 2–3 hours, your breasts should not feel engorged.
Engorgement can lead to sore, painful breasts or a breast infection. So it’s best to try to avoid it. The longer you wait to breastfeed or pump, the more uncomfortable and engorged your breasts may get.
If you can't feed your baby right away, use warm compresses and try to pump or manually express your milk. One way to express milk is to put your thumb on top of your areola and a finger below it. Gently but firmly press your thumb and fingers back against your chest wall. Then compress your fingers together to express (push out) your milk.
Is It Normal to Feel Pain During or After Breastfeeding?
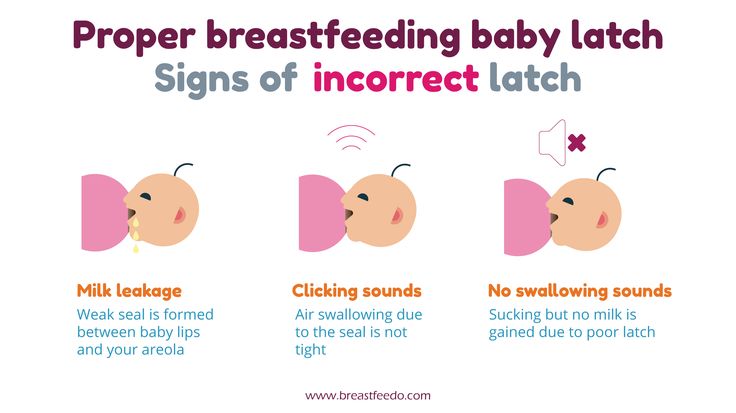
When babies latch on properly, some moms feel a few moments of discomfort at the very beginning of a nursing session. After that, discomfort should ease. You may feel a gentle tug on your breasts while your baby feeds, but it shouldn’t hurt.
If you feel discomfort during nursing, stop nursing and reposition your baby to get a better latch. Your nipple areola (the ring around the nipple) should be mostly in your baby’s mouth. When babies are latched on wrong, it can hurt or feel like a pinch each time your baby sucks. Over time, this can lead to painful, sore, cracked nipples.
If you have pain during breastfeeding, talk to your doctor or lactation consultant to make sure your baby is properly latched or that something else isn't going on.
What Else Can Cause Breast Pain?
The most common causes of breast pain include:
A plugged milk duct. Sometimes milk ducts get plugged. You may feel pain in an area of your breast or a lump may form under the skin where the duct is plugged. To help unclog the duct and ease pain:
- Take warm showers or use warm compresses on the area. Massage the area several times a day. Then, breastfeed your baby right away.
- Position your baby’s chin so that it points toward the clogged area during feeding. This will help that area of the breast empty sooner.
- Gently massage the lump while your baby feeds. It may take 2 to 3 feedings for the lump to go away. You also can use a manual (hand) or electric pump for a few minutes to help draw out the clogged milk while gently massaging the area.
- Apply cold compresses (ice wrapped in a thin towel) between feedings.
- If the lump doesn't go away within a couple of days, or if you have a fever, chills, aches, or red streaking, call your doctor.
Mastitis. This is an inflammation of the breast. If your breasts are sore; have red streaks; or have a hard, red area, you may have mastitis. Some women also get a fever and chills. If you think you have mastitis, call your doctor. In the meantime, continue to breastfeed or pump to drain the milk from your breasts. Switch between warm compresses and gentle massage right before breastfeeding and then apply cold compresses after a session. Mastitis caused by an infection may need treatment with antibiotics.
Oral thrush. Sometimes babies develop a yeast infection in the mouth called oral thrush. Babies with this have cracked skin in the corners of the mouth, and whitish or yellowish patches on the lips, tongue, or inside the cheeks. The infection can spread to your breast and cause:
- shooting or burning breast pain either during or after feedings
- pain deep within your breast
- strong pain in the breasts or nipples that doesn't get better after your baby properly latches on or you reposition your baby
- nipples that are cracked, itchy, burning, or are pink, red, shiny, flaky, or have a rash with little blisters
Call your doctor if you or your baby have any of these symptoms.
Inverted or flat nipples. Women who have inverted nipples (nipples that turn in rather than stick out) or flat nipples (that don't become as erect as they should when a baby is nursing) may have a harder time breastfeeding or have nipple pain. If either is the case, talk to your doctor or a lactation consultant about ways to make nursing easier and reduce any pain.
How Can I Ease Breast or Nipple Pain?
During Feedings
- Nurse first on the side that's less sore and vary breastfeeding positions.
- Make sure your baby latches onto your breasts correctly. If breastfeeding is too painful, it may be more comfortable to drain your breasts by pumping the milk.
- If you have sore nipples, ask a lactation consultant or your health care provider if a nipple shield is a good idea. Nipple shields go over the areola and nipple during a feeding to protect sore or cracked nipples. They should only be used when recommended by your care team as they can sometimes affect milk supply.

- Gently break the suction when removing your baby from your breast. Slip your finger in the side of your baby's mouth, between the gums, and then turn your finger a quarter turn to do so.
- At the end of a feeding, massage some breast milk onto your nipples, and then let them air dry.
Between Feedings
- Gently massage the sore area before nursing.
- Use wet or dry heat on your breasts (a warm shower, water bottle, heating pad, or warm washcloth) right before feeding. But if you have a yeast infection in your breast, you'll need to keep your nipples dry because yeast thrives on moisture. Get plenty of rest and fluids.
- Put ice packs or cool compresses on engorged breasts after feedings.
- Make the area where you feed your baby comfortable. Sit in a glider or a cozy chair with armrests. Footstools and pillows can give extra support. Some women like wraparound nursing pillows or "husband" back pillows with arms on each side for nursing in bed.
If breastfeeding is painful or uncomfortable for you, callyour doctor or lactation consultant for help.
6 breastfeeding problems in the first week – solved
Having trouble breastfeeding your newborn? Read our expert tips and watch videos to solve common breastfeeding problems in the first week.
Share this content
Cathy Garbin, child health nurse, midwife and lactation consultant:
For seven years, Cathy was a Research Associate with the renowned Hartmann Human Lactation Research Group, while supporting breastfeeding mothers in their homes and in hospitals. The mum of two still works with families, and also conducts study days for healthcare professionals and speaks at international conferences.
Breastfeeding isn’t always easy and if you’re experiencing difficulties you’re not alone. In fact a US study of more than 500 mums found that 92% reported breastfeeding challenges by day three1. Thankfully, many early breastfeeding difficulties are simple to deal with – here are my solutions to the most common problems mums experience in the first week.
Thankfully, many early breastfeeding difficulties are simple to deal with – here are my solutions to the most common problems mums experience in the first week.
I have sore nipples what should I do?
Problem 1: Breastfeeding hurts!
Pain while breastfeeding is usually down to sore, tender nipples, especially once your milk ‘comes in’ around two to four days after giving birth.2 Your baby will be feeding every couple of hours, which means the problem can worsen quickly, with some mums finding their nipples crack, bleed or become blistered. Ouch!
Solutions3
- Check your baby’s latch. Your baby not latching correctly is the most likely cause of breastfeeding pain. Your newborn should have a large portion of the lower part of the areola (the dark skin around your nipple) in her mouth when she feeds, with your nipple against the roof of her mouth, cupped gently underneath by her tongue.

- See a lactation consultant or breastfeeding specialist to make sure your baby’s mouth and body are positioned correctly and that there are no other latching problems. They can also check inside your baby’s mouth to see if there is a physical problem.
- Try different breastfeeding positions. A laid-back, cross-cradle, underarm (‘rugby ball’) or lying-down hold may take the pressure off the most painful areas of your breast.
- Wipe damaged nipples gently with several pieces of water-moistened cotton wool after feeding to remove any debris that could lead to infection.
- Air-dry nipples or dab with a very clean, soft muslin or flannel, as infection can flourish in damp conditions. Use either disposable or washable nursing pads to absorb any milk leakage, remembering to change them regularly.
- Soothe your nipples. Relieve soreness and any dry skin with ultra-pure lanolin cream or gently apply a few drops of your own breast milk – you won’t have to remove either before the next feed.
 You could also try hydrogel pads straight from the fridge. These nipple dressings cool and provide instant breastfeeding pain relief, while creating ideal conditions for healing.
You could also try hydrogel pads straight from the fridge. These nipple dressings cool and provide instant breastfeeding pain relief, while creating ideal conditions for healing. - Protect your nipples. Breast shells prevent your clothes from rubbing against sore areas.
- Be patient. Soreness normally settles down after a few days as your body gets used to breastfeeding and your baby’s sucking becomes more efficient.
- Consult a healthcare professional, lactation consultant or breastfeeding specialist if the pain while breastfeeding doesn’t subside after a few days. Ongoing nipple soreness can be a sign of an infection that may require medication.
Problem 2: My baby is not latching properly
Some newborns just don’t seem to manage to get a great latch – perhaps because you both need a little more time to get breastfeeding coordinated, or because they were born prematurely, are uncomfortable after a difficult birth, or their mum has flat or inverted nipples.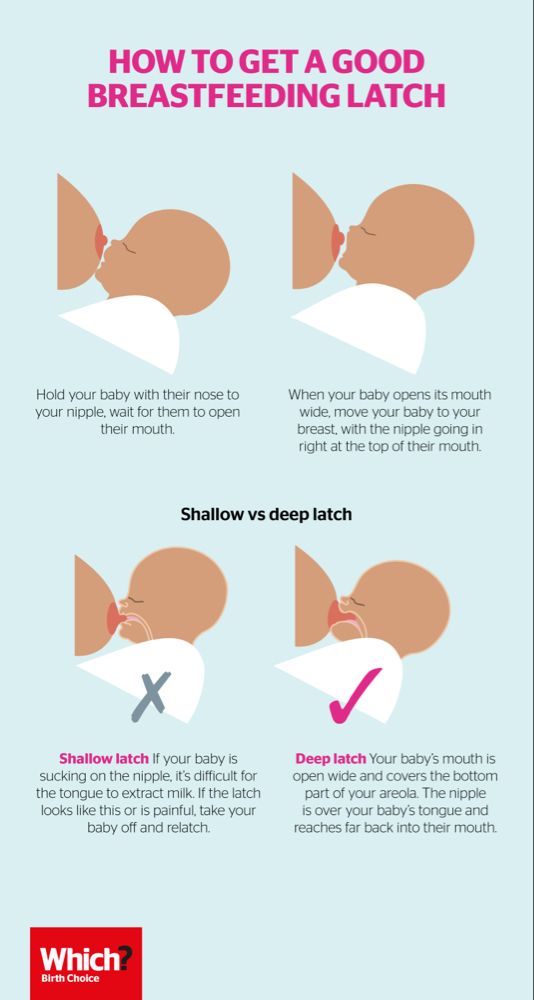
Solutions
- Get support from a lactation consultant or breastfeeding specialist who can diagnose the cause of the problem and develop a plan to help you overcome it.
- Draw out inverted or flat nipples. Nipple formers fit comfortably inside your bra, and apply a gentle pressure that can help draw out your nipples to support breastfeeding.
- Adopt different holds to make things easier for your newborn. She needs to feel supported, comfortable, and able to breathe in order to feed effectively. Make sure you’re not holding her head or pushing it. A laid-back, baby-led feeding style encourages your baby to use her innate reflexes, making it easier for her to reach your breast and latch on.4
- Make tiny adjustments while feeding. Rather than take your baby on and off the breast, creating frustration for you both, try ensuring she’s well positioned and comfortable.
 Keep her body and bottom close to you, support her across her shoulder girth, and hold her firmly so she feels secure. Let her head rest on your wrist so it can tilt back slightly and allow more space for her nose to breathe. Her chin should be close to your breast. If minor adjustments don’t seem to be improving your baby’s comfort, seek support from a lactation consultant or breastfeeding specialist.
Keep her body and bottom close to you, support her across her shoulder girth, and hold her firmly so she feels secure. Let her head rest on your wrist so it can tilt back slightly and allow more space for her nose to breathe. Her chin should be close to your breast. If minor adjustments don’t seem to be improving your baby’s comfort, seek support from a lactation consultant or breastfeeding specialist. - Feed through nipple shields. If your baby will not latch on, a lactation consultant or breastfeeding specialist may recommend using nipple shields to give your baby a larger, firmer target to attach to. In general, nipple shields should be considered a short-term solution.
The top 8 tips if your baby has lost too much weight
Problem 3: I do not have enough breast milk
Initially you’ll make a small amount of breast milk because the hormonal changes that trigger your milk production happen slowly, and won’t be finished until around day two to four. 2 This may cause you to worry your baby isn’t getting enough, but as her stomach is only tiny at first and she feeds frequently, it’s not a problem. During the first few days you only need to be concerned if your baby is losing more weight than expected and producing too few wet and dirty nappies, or is showing signs of dehydration. For a full explanation of how often your newborn should be weeing and pooing, read breastfeeding a newborn: what to expect in the first week.
2 This may cause you to worry your baby isn’t getting enough, but as her stomach is only tiny at first and she feeds frequently, it’s not a problem. During the first few days you only need to be concerned if your baby is losing more weight than expected and producing too few wet and dirty nappies, or is showing signs of dehydration. For a full explanation of how often your newborn should be weeing and pooing, read breastfeeding a newborn: what to expect in the first week.
Solutions
- Seek support from a lactation consultant, breastfeeding specialist or healthcare professional, who’ll be able to assess if you have a milk supply problem. The earlier you get help, the better.
- Feed on demand, not to a schedule. In the first week after birth your newborn will want to feed at least every two to three hours (maybe more!) throughout the day and night. This frequency helps to build your milk production.
- Look after yourself.
 It’s not always easy with a newborn, but try to rest when you can, eat well, and get as much help as possible with chores and any older children so you can focus on breastfeeding.
It’s not always easy with a newborn, but try to rest when you can, eat well, and get as much help as possible with chores and any older children so you can focus on breastfeeding. - Try expressing. If your baby is feeding often and still not putting on weight, a lactation consultant or breastfeeding specialist may recommend pumping to build your milk supply. If your milk hasn’t come in yet, the Medela Symphony hospital-grade double electric breast pump has an ‘Initiate’ program that mimics the way a newborn feeds in the first few days.
Problem 4: My breasts are really full and hard
When your milk comes in, your breasts will become fuller and firmer. If your baby is feeding well and frequently, this should pass without problems. However, some women’s breasts become rock hard, and they may also be tender, uncomfortable, even painful – a condition called breast engorgement. Engorged breasts may also feel fairly hot due to all the activity inside – it’s like a traffic jam in there! Although it’s only temporary, often lasting 24 to 48 hours, engorgement can also make it difficult for your baby to latch, as your nipples may become flattened. 5
5
Solutions
- Feed your baby frequently. Aim to feed at least eight to 12 times every 24 hours. This is the primary treatment for this condition – for more tips and advice read our article on breast engorgement.6,7
- See a healthcare professional, lactation consultant or breastfeeding specialist if the symptoms last more than 48 hours, you have a fever, or your baby is unable to breastfeed because of the engorgement.
Problem 5: My breasts are leaking
Leaky breasts are very common in the early days of breastfeeding, once your milk has come in. You may leak from one breast when you’re feeding your baby from the other, when lying on your front while sleeping, or when something stimulates your let-down reflex unexpectedly – like another baby crying in the supermarket. Leaking usually settles down after six weeks or so.
Solutions
- Protect your clothes by wearing disposable or washable nursing pads inside your bra day and night.

- Don’t waste a drop! Milk collection shells fit inside your bra to collect any leaked milk. They’re helpful when the leakage is too much for nursing pads, or if one nipple tends to drip while you’re feeding from the other. If you want to save the collected milk, you can, but only use milk you’ve collected during a breastfeed. Store in a sterile container and, if you’re not feeding it to your baby straight away, place in the fridge immediately and use within 24 hours. Don’t wear collection shells for more than two to three hours at a time.
Problem 6: I think I’m producing too much milk
Sometimes when your milk comes in, it really comes in! You may have a temporary oversupply for the first few weeks but it should settle down soon.7 Until then your breasts may feel painful and hard most of the time, even straight after a feed, and you might be leaking a lot of milk. Your baby may cough and splutter with the force of your let down, vomit as soon as she is moved after feeds, and have an uncomfortable tummy or explosive, frothy, greenish poos. All this suggests you may have too much milk, but this issue may resolve itself as soon as your breasts adjust to their new job.
All this suggests you may have too much milk, but this issue may resolve itself as soon as your breasts adjust to their new job.
Solutions
- Express a little milk by hand at the start of each feed to reduce the force of your let down.
- Try the laid-back breastfeeding position so your baby can better control the flow of milk. Or use the cradle position: holding her across her shoulders, ensuring your baby’s head is tilting back slightly and resting on your wrist. Her body will be resting on yours, sloping down diagonally.
- Be gentle and patient. Allow your baby to rest and digest her milk, both during and after a feed. Moving her around too much or too quickly could make her feel sick. As she grows, she’ll get better at coping with the flow, which is likely to slow in any case.
- Use a towel or muslin cloth to soak up the surge if your baby gets overwhelmed when your milk starts to flow, and put a milk collection shell on your other breast to catch any leaks.

- Seek advice from a lactation consultant or breastfeeding specialist if you’re still having difficulties after several weeks. They will assess you, and may advise on one-sided feeding or block feeding if you need to reduce your milk supply.
Read on: Breastfeeding difficulties in the next few weeks and breastfeeding challenges after the first month
References
1 Wagner EA et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics. 2013:peds-2013.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching‐On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women’s Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev. 2008;84(7):441-449.
Early Hum Dev. 2008;84(7):441-449.
5 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd. 2013;73(12):1202-1208.
6 Amir LH. Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol# 4: Mastitis, revised March 2014. Breastfeed Med. 2014;9(5):239-243.
7 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol# 20: Engorgement. Breastfeed Med. 2009;4(2):111-113.
Solutions to six breastfeeding problems in the first week
Are you having difficulty breastfeeding your newborn baby? Read on for expert advice on tackling the main challenges of the first week of breastfeeding.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is not always easy, so if
you are having difficulty, know that you are not alone. A US study found that out of 500 new mothers surveyed, 92% experienced breastfeeding problems by the third day. 1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding.
Problem #1. Breastfeeding hurts!
Pain during feeding is usually associated with tenderness or inflammation of the nipples, especially when milk "comes" on the second to fourth day after birth. 2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: some mothers' nipples crack, bleed, or blister. This is, of course, very annoying.
Solutions 3
- Check how the baby latch on.
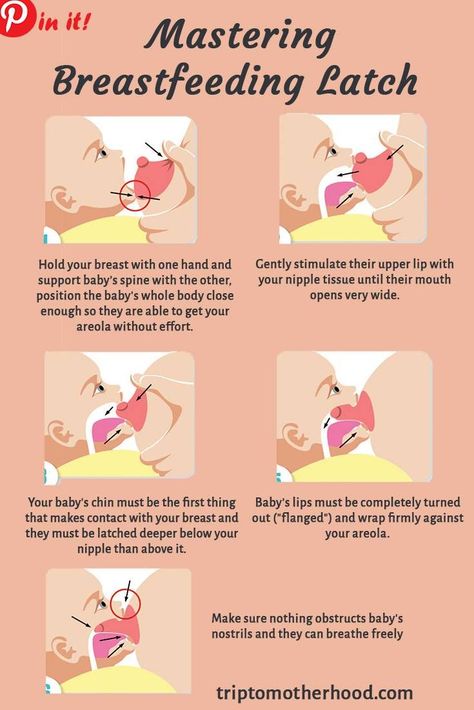 An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue.
An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue. - Contact a lactation consultant or healthcare professional to make sure your baby's mouth and torso are properly positioned during feeding and there are no other latch-on problems. The doctor may also examine the baby's mouth for physical abnormalities.
- Try other feeding positions. Reclining, cross cradle, underarm, or lying positions can relieve pressure on the most painful areas of your breasts.
- Gently wipe soaked nipples with water-soaked cotton swabs after each feed to remove milk residues that can cause infection.
- Air dry nipples or blot with a clean, soft muslin or flannel cloth to prevent bacterial growth in a humid environment.
 Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly.
Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly. - Soften your nipples. An ultra-pure lanolin treatment will help relieve inflammation and dry skin. You can also apply a few drops of your own breast milk to your nipples. In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing.
- Protect your nipples. Nipple shields* protect the sore area from rubbing against clothing.
- Be patient. The inflammation usually resolves after a few days as your body adjusts to breastfeeding and your baby learns to suckle.
- Seek medical attention, if pain during feeding does not go away after a few days. Constant inflammation of the nipples may indicate an infection that requires prompt treatment.

Problem #2. Baby doesn't latch on properly
Some newborns do not latch on properly right away. Maybe both of you just need more time to learn how to breastfeed, or maybe the baby was born prematurely, feels unwell after a difficult birth, or mom has flat or inverted nipples.
Solutions
- Contact a lactation consultant or healthcare professional who can help identify the cause of the problem and suggest solutions.
- Flat or inverted nipples must be pulled out. Nipple formers* fit comfortably in the bra and apply gentle pressure to the nipples to help them come out for easier feeding.
- Try different positions and ways to support your newborn. The baby needs to feel supported. He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead.
 This stimulates his natural reflexes and helps him find and latch on to his breasts. 4
This stimulates his natural reflexes and helps him find and latch on to his breasts. 4 - When feeding, try to find the optimal position. Instead of putting your baby on and off, stressing both of you, try to position him in a way that is easy and comfortable for him. Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional.
- Use nursing pads. If your baby is having difficulty latch-on, a lactation consultant or healthcare professional may suggest trying nursing pads*. A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.

Problem #3. Not enough breast milk
You will produce little breast milk at the very beginning, as the hormonal changes that trigger milk production occur slowly and do not end until the second or fourth day after birth. 2 You may be worried that your baby is not getting enough milk, but in the early days his stomach is still too small and feedings are frequent, so don't worry. The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
Solutions
- Contact a Lactation Consultant or your healthcare provider who can determine if you have problems with milk production. The sooner you do this, the better.
- Feed your baby on demand, not on a schedule. In the first week after birth, your baby will ask to breastfeed every two to three hours (or more often!), both day and night.
 Such frequent feeding helps to establish the production of breast milk.
Such frequent feeding helps to establish the production of breast milk. - Take care of yourself. It's not always easy with a newborn, but try to rest whenever you can, eat right, and accept any help around the house or with older children that your loved ones can give you to fully focus on breastfeeding.
- Try expressing milk. If a baby is feeding frequently but not gaining any weight, a lactation consultant or doctor may recommend pumping to increase breast milk production. If milk is not coming out at all, you can try the Medela Symphony Dual Electric Clinical Breast Pump**. It features an Initiate program that mimics a baby's natural sucking rhythm for the first few days.
Problem #4. Breast full and heavy
Your breasts will become fuller and heavier as milk comes in.
If the baby suckles well and often, this should not cause any problems. However, in some women, the breasts become so full that they become hard and painful. This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on. 5
This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on. 5
Solutions
- Feed your baby often. Try to breastfeed at least 8-12 times a day. This is the main way to alleviate this condition. For more tips and tricks, see the article on Breast Swelling. 6.7
- Call your healthcare provider, if symptoms persist for more than 48 hours, you have a fever, or your baby is unable to breastfeed due to swelling.
Problem #5. Milk is leaking
Breast leakage is very common in the early days of breastfeeding when milk production begins. Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Solutions
- Protect clothes from stains will help disposable or reusable bra pads to be used day and night.
- Don't waste precious drops! Breast milk collection pads* fit inside the bra and allow you to collect any leaking milk. This is a very useful thing when there is too much milk and the pads are not absorbing well, or when one breast is leaking while you are feeding the other. If you want to save the collected milk, use only the milk collected at the feeding. Place it in a sterile container and refrigerate immediately if you are not supplementing with it right away. Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.

Problem #6. There seems to be too much milk
Sometimes when milk comes in, too much is produced! In the first few weeks there may be an overabundance of milk, but usually everything returns to normal soon. 7 Up to this point, the breasts may be heavy and sore almost all the time, even immediately after a feed, and a lot of milk may leak. A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
Solutions
- Express some milk by hand at the beginning of each feed to ease the force of the flush.
- Try to feed while leaning back: this will help your baby control the flow of milk. The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm.
 The torso of the baby will be located diagonally on you.
The torso of the baby will be located diagonally on you. - Be kind and patient. Let your baby rest and absorb milk both during and after feeding. Don't move your baby too much or too fast, as this can make him nauseous. As the baby grows, he will learn to better cope with the rush of milk, which is likely to weaken anyway.
- Use the towel or swaddle to soak up spilled milk if the baby can't handle the flush, and place the breast milk collection pad on the other breast to catch any spilled milk.
- Contact a lactation consultant or doctor if problems persist after a few weeks . He will examine you and may suggest one-sided feedings or hourly breast changes (“breast duty”) to reduce your milk supply.
Related materials: Difficulties in breastfeeding in the next few weeks and problems with breastfeeding after the first month
Literature
1 Wagner EA et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
— Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 2008;84(7):441-449.
5 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. . ABM Clinical Protocol# 4: Mastitis , Revised MARCH 2014. Breastfeed : 5): 5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
Breastfeed : 5): 5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
7 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med . 2009;4(2):111-113. - Protocol Committee of the Academy of Breastfeeding Medicine, "AVM Clinical Protocol No. 20: Engorgement, Revision 2016". Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
Read instructions before use. Consult a specialist about possible contraindications.
* RU No. ФСЗ 2010/07352 of 07/19/10
** RU No. ФСЗ 2010/06525 of 03/17/2021
. And future mothers, having read a bunch of special literature during pregnancy, are very determined to feed their child with their own milk.
But the happy event finally happened: the baby was born. Some time passes, and suddenly the young mother with the same determination refuses to breastfeed. Why? What's happened? Turns out it hurts!
Some time passes, and suddenly the young mother with the same determination refuses to breastfeed. Why? What's happened? Turns out it hurts!
Calluses
Let's see why pain can occur during feeding and what it means.
So, when a newborn baby is first applied to the mother's breast, new sensations arise not only for him, but also for the mother. This is especially true for firstborns. But even if a woman has already had the experience of motherhood and breastfeeding, her breasts have already managed to “forget” how a tiny tongue and strong gums work. The skin on the nipple and around it is very thin and delicate, so the mother is guaranteed quite strong sensations.
The baby instinctively "grinds" her mother's nipple, and gradually the skin becomes harder and less vulnerable, a kind of callus is formed. If you have ever learned to play the guitar, then you probably remember how each string leaves an imprint on the soft fingertips in the beginning. Then the traces of the guitar strings simply “burn”, and, finally, the skin becomes rough, and protective calluses allow you to play the guitar almost painlessly.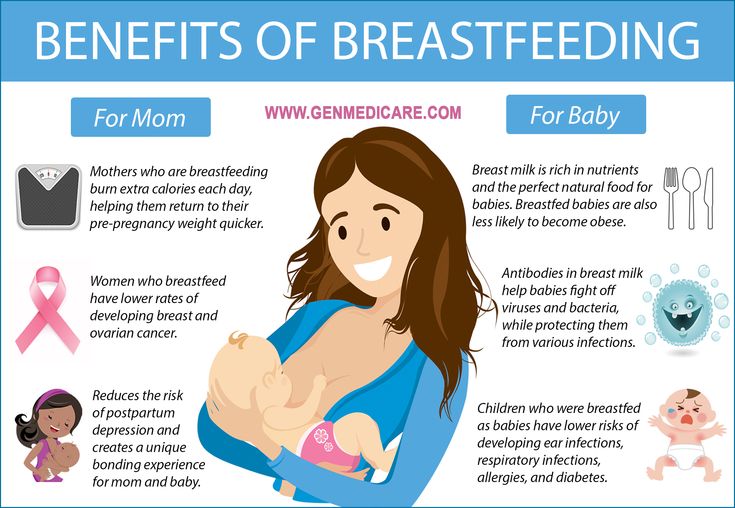
Something similar happens during breastfeeding. In the first days after childbirth, the skin may slightly crack, turn white, and white crusts appear on it. This is how “labor calluses” are formed, this process can take from a couple of days to a couple of weeks.
Pain may occur when the nipple is caught. But as soon as the baby began to actively suck, the pain disappears. Such pain (and sometimes not even pain, but just a strong sensation) occurs under the influence of hormones and does not require special therapeutic measures.
Torment or joy?
Alas, most of our maternity hospitals do not teach breastfeeding. Moreover, they teach how to turn breastfeeding into hellish torment. Judge for yourself. First, a nurse comes and in a stern voice tells the newly-made mother to wash her breasts with soap and then wipe dry. The breast is supposed to be given to the baby in the “scissors” grip (the peripapillary region is pinched with the index and middle fingers).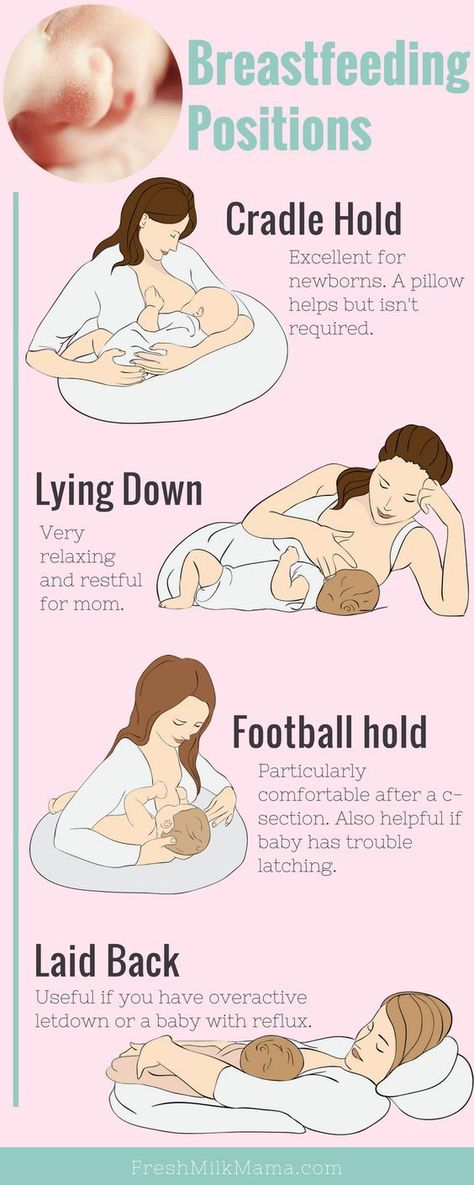 At the end of feeding, the instruction, which has passed all medical instances, again requires washing the breast with water, and if there is irritation, grease the nipple with brilliant green.
At the end of feeding, the instruction, which has passed all medical instances, again requires washing the breast with water, and if there is irritation, grease the nipple with brilliant green.
Where does this path lead? To dry out the natural lubricant around the nipple, inflammation of the skin and cracks. It is not surprising that feeding according to such instructions becomes an inhuman feat in the name of motherhood. Having bitten the end of the blanket so as not to scream in pain, the young mother feeds the baby with all her strength. How long will her heroism last?
If the skin around the nipple is reddened and inflamed, if there is no protective callus on the nipple and the pain increases during feeding, this is an alarming sign. In more advanced cases, the skin on the inflamed area becomes white (a water bubble appears) or dark red (this is a nipple abrasion). Both a water bladder and an abrasion are forms of nipple inflammation that can occur for several reasons.
- Incorrect attachment to the breast. Almost all women who have had maternity hospital experience put the baby to the breast incorrectly. The very capture of the “scissors” of millions of Russian women has been brought to automatism. Meanwhile, he is dangerous. Firstly, the breast is constricted, and milk, instead of flowing freely, stagnates in certain areas, resulting in often lactostasis. Secondly, in this position, the baby's mouth "slips" from the peripapillary region onto the nipple itself. And this is absolutely unacceptable! In the mouth, the crumbs should have not only the nipple, but also the areola. The position of the baby during feeding also matters. Physiologically correct is the prone position and from under the arm.
- Overdrying of the skin. It occurs as a result of washing the chest with soap, and even more so after using alcohol-containing solutions.
- Use of waterproof pads for leaking milk. Such pads create a favorable environment for the development of inflammation.
- Incorrect weaning of the baby from the breast at the end of feeding. If the baby is torn off the breast during sucking, he will instinctively compress the breast with his gums and may injure her.
- Tight clothing that constricts the chest.
Inflammation Prevention
- Make sure the baby is properly attached to the breast. If the baby correctly captures the breast, then the frequency and duration of breastfeeding is not limited. Do not let the child suck only the nipple, "drive" it back and forth in the mouth or from side to side, bite the mother's breast (even with a toothless mouth).
- There is no dirty breast. In any case, if at this moment you are not lying bare-chested in the sandbox. And therefore it is quite enough to wash it without soap once or twice a day.
- Do not use waterproof pads. At home, you can do without pads at all, you just need to change T-shirts more often, and “on the way out” get ventilated pads with holes.

- Wean the baby correctly. Either wait until he releases the nipple, or carefully insert your little finger into the corner of his mouth. The baby will slightly open his mouth, and then you can painlessly pull out your chest from him.
- If inflammation still occurs, the injured nipple can be treated with Purelan, Bepanten, Solcoseryl ointments.
Entry gate for infections
Inflammation of the nipples, if left untreated, can lead to cracks.
Fissures cause sharp, burning pain during feeding, ichor flows from the fissure, and blood may ooze during feeding. Such a chest injury is dangerous, because an open wound becomes an entrance gate for infection, and from here it is already just one step to mastitis.
And therefore, if you have cracks, the matter is urgent.
- The first step is to call a lactation consultant. He will determine how often you need to express, for how long you will have to stop feeding from a sore breast.
 Unfortunately, this issue cannot be resolved over the phone, it is necessary to examine the chest and determine the scale of the disaster.
Unfortunately, this issue cannot be resolved over the phone, it is necessary to examine the chest and determine the scale of the disaster. - At the time of treatment, you need to stop feeding the baby from the diseased breast. Depending on the size and depth of the crack, it can take from 12 hours to 2-3 days. During this time, milk from a diseased breast must be expressed 3 to 6 times.
- The baby should be fed from a healthy breast. If necessary, you can supplement with expressed milk from a spoon. Never use a bottle with a pacifier for this purpose.
- Cracks require special treatment. The consultant will recommend gels for wound healing. It is very important that these are gels, not ointments. After all, we need the wound to heal as quickly as possible, and ointments can only worsen the condition.
- After the cracks have healed, you will once again learn how to put the baby to the chest, properly wean it from the chest and find a comfortable position for feeding.
 It is better to do this together with a consultant so as not to step on the same rake twice.
It is better to do this together with a consultant so as not to step on the same rake twice. - By the way, during the treatment and after the resumption of feeding, be sure to inform the consultant by phone about your condition. If there is a deterioration, then one or two more meetings will be needed in order to find out what is wrong.
Of course, any disease is easier to prevent than to cure. So pay attention,
How to properly care for your breasts while breastfeeding
First of all, forget the instructions about washing your breasts often, especially with soap. If during a hygienic shower you rinse your chest, this will be enough.
Soap and detergents of any kind will remove the special protective lubricant produced by Montgomery's glands from the breasts. But in nature, nothing is done just like that: this lubricant has bactericidal properties, prevents the occurrence of abrasions, scuffs, excessive drying out and protects the skin from pathogenic microorganisms.